Abstract
Among youth with diabetes mellitus, elevated blood pressure represents one of the most common co-morbidities. Hence, exploring dietary factors that may help prevent or control hypertension in this population is of paramount importance. We investigated whether adherence to the Dietary Approaches to Stop Hypertension (DASH) is associated with hypertension in youth with diabetes from the SEARCH for Diabetes in Youth Study. Between 2001 and 2005, 2,830 youth aged 10 to 22 years (2,440 with type 1,390 with type 2 diabetes) completed a study visit. For each of the 8 DASH food groups, a score of 10 was assigned when the DASH recommendation was met. Lower intakes were scored proportionately, and the 8 individual scores were summed. The association between the overall DASH score and hypertension was evaluated using multiple logistic regression. The crude prevalence of hypertension was 6.8% for youth with type 1 and 28.2 % for type 2 diabetes. In youth with type 1, a higher adherence to DASH was inversely related to hypertension, independent of demographic, clinical, and behavioral characteristics (tertile 2 vs. 1: OR 0.7, 95% CI 0.5–1.0; 3 vs. 1: 0.6, 0.4–0.9; ptrend=0.007). For type 2 diabetes, the DASH diet was not associated with hypertension (tertile 2 vs. 1: 0.8, 0.5–1.4; 3 vs. 1: 0.9, 0.5–1.5; ptrend=0.6). Prospective observational studies or clinical trials are needed to investigate whether adherence to the DASH guidelines may help prevent hypertension in youth with type 1 diabetes. In type 2 diabetes, more research with a larger sample is necessary.
Keywords: DASH, diabetes mellitus, hypertension, dietary pattern, nutrition
INTRODUCTION
Hypertension represents one of the most common co-morbidities in persons with diabetes mellitus (DM) and seriously affects morbidity and mortality1, 2. Recent evidence from the SEARCH for Diabetes in Youth Study suggests that 30% of adolescents aged 10–19 years with type 1 or type 2 DM (T1DM, T2DM) have elevated blood pressure (BP), with a particularly high proportion in those with T2DM3.
Dietary modification is a central part of any treatment strategy for (pre)hypertensive youth4. The Dietary Approaches to Stop Hypertension (DASH) trials demonstrated that a dietary pattern rich in vegetables, fruits and low-fat dairy products can effectively lower systolic and diastolic BP in normo- and hypertensive adults5. However, subsequent attempts to evaluate the importance of the DASH diet have yielded mixed results6–8. It has also been suggested that higher intakes of fruit, vegetables and dairy might be related to lower BP in children9. Studies investigating the total DASH pattern in youth, in particular in the critical population of youth with DM, are lacking2, 10, 11.
The aim of the present analysis was to examine the association between adherence to the DASH dietary pattern and hypertension in youth with DM, using cross-sectional data from the SEARCH for Diabetes in Youth Study.
METHODS
Study population
SEARCH for Diabetes in Youth is a multi-center, observational study of physician-diagnosed DM in children, adolescents and young adults <20 years of age. A detailed description has been published previously12. Population-based ascertainment included youth with DM prevalent in 2001 and incident from 2002 through the present. Diabetes cases are being identified in geographically defined populations (Ohio, Washington, South Carolina, Colorado), among health plan enrollees (Hawaii, California), and among several American Indian populations.
The study was reviewed and approved by the local Institutional Review Board(s) and complied with the privacy rules of the Health Insurance Portability and Accountability Act. DM cases were asked to complete an initial survey including age at diagnosis and self-reported race/ethnicity and subsequently invited to a study visit. Written informed consent was obtained from participants ≥18 years of age, or from a parent in participants <18 years. Minors provided written assent.
In this analysis, DM type as assigned by the health care provider was used for classification into T1DM (combining T1A, T1B and T1) and T2DM based on information collected from the health care providers at the time of the case report or from medical records.
Blood pressure and anthropometry
Physical examinations at the study visits included measurements of height, weight, and BP and were conducted according to standardized protocols by trained and certified staff members. Three BP measurements were obtained at the right arm with a mercury manometer after the patient had been sitting for at least 5 minutes, with a break of at least 30 seconds between readings. Five cuff sizes were available. The mean of the three measurements was calculated for this analysis.
In accordance with the 4th Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in children and adolescents4, hypertension was defined as having a diastolic or systolic BP (SBP, DBP) ≥95th percentile for age, height and sex (in participants ≥18 years, 140 mmHg and 90 mmHg served as cut-offs for SBP and DBP), or taking antihypertensive medication1, 13.
Standard deviation scores (SDS) of anthropometric parameters were constructed according to the U.S. Centers for Disease Control and Prevention (CDC) 2000 growth standards14, with interpolations made for those who were older than 20 years of age at the time of the measurement. Obesity was defined as having a BMI ≥95th percentile for age and sex15.
Dietary assessment
At study visits, dietary intake was assessed in participants ≥10 years with a food frequency questionnaire (FFQ), which represented a modified version of the Block Kid’s Food Questionnaire16. Details of the dietary assessment methodology in SEARCH can be found elsewhere17. The SEARCH FFQ incorporates 85 food lines, and for each food, the participants indicated whether it was consumed in the past week, on how many days, and the average portion. Portion size was queried either as a number (e.g., number of slices) or in relation to pictures of food in bowls or plates. The nutrient and portion-size databases were based on the Nutrition Data System for Research (database 3, version 4.05/33, 2002, University of Minnesota, Minneapolis), and industry sources.
Table 3.
Median energy, food group and nutrient intakes according to diabetes type and DASH adherence.
| Type 1 Diabetes (n=2,440) | Type 2 Diabetes (n=390) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Tertiles of DASH score | Tertiles of DASH score | ||||||||
| Diet characteristic | 1 (lowest) |
2 | 3 (highest) |
p* | 1 (lowest) |
2 | 3 (highest) |
p* | |
| Mean DASH score | 29.9 | 39.9 | 50.0 | - | 26.7 | 36.5 | 46.6 | - | |
| Energy (kcal/day) | 1752.2 | 1753.1 | 1783.6 | 0.5 | 1709.7 | 1579.4 | 1634.2 | 0.4 | |
| Food groups (servings/1000 kcal) | |||||||||
| Total grains | 2.05 | 2.15 | 2.15 | 0.01 | 1.93 | 2.13 | 2.09 | 0.08 | |
| High fiber grains† | 22.4 | 24.3 | 32.4 | <0.0001 | 22.3 | 29.2 | 33.9 | 0.1 | |
| Vegetables | 0.94 | 0.96 | 1.06 | <0.0001 | 1.11 | 1.14 | 1.33 | 0.03 | |
| Fruit | 0.53 | 0.81 | 1.16 | <0.0001 | 0.50 | 0.85 | 1.04 | <0.0001 | |
| Total dairy | 0.76 | 0.91 | 1.10 | <0.0001 | 0.46 | 0.59 | 0.82 | <0.0001 | |
| Low-fat dairy | 0.20 | 0.42 | 0.70 | <0.0001 | 0 | 0.13 | 0.44 | <0.0001 | |
| Meat | 1.57 | 1.26 | 1.04 | <0.0001 | 1.70 | 1.49 | 1.33 | 0.003 | |
| Nuts & seeds | 0 | 0.18 | 0.44 | <0.0001 | 0 | 0.09 | 0.35 | <0.0001 | |
| Fats & oils | 2.25 | 1.79 | 1.39 | <0.0001 | 2.08 | 1.93 | 1.60 | 0.005 | |
| Sweets | 0.89 | 0.85 | 0.68 | <0.0001 | 1.02 | 0.91 | 0.65 | 0.002 | |
| Nutrients (per 1000 kcal) | |||||||||
| CHO (g) | 114.4 | 118.2 | 124.4 | <0.0001 | 113.7 | 117.8 | 119.0 | 0.02 | |
| Fat (g) | 43.7 | 42.2 | 40.4 | <0.0001 | 43.7 | 42.7 | 41.3 | 0.04 | |
| Saturated fat (g) | 16.1 | 15.3 | 14.4 | <0.0001 | 15.9 | 15.0 | 14.1 | <0.0001 | |
| Protein (g) | 40.2 | 39.6 | 39.4 | 0.004 | 40.0 | 38.0 | 39.2 | 0.5 | |
| Fiber (g) | 6.0 | 6.6 | 7.8 | <0.0001 | 5.8 | 6.8 | 8.2 | <0.0001 | |
| Calcium (mg) | 501.0 | 588.3 | 669.4 | <0.0001 | 326.7 | 392.0 | 436.0 | <0.0001 | |
| Magnesium (mg) | 121.0 | 135.4 | 152.6 | <0.0001 | 105.8 | 119.8 | 138.6 | <0.0001 | |
| Potassium (mg) | 1166.5 | 1286.1 | 1461.6 | <0.0001 | 1048.2 | 1170.7 | 1348.6 | <0.0001 | |
CHO, carbohydrates.
χ2-Test for categorical, Kruskal Wallis-Test for continuous variables.
Frequency of consumption (%).
Staff certified on the SEARCH protocol instructed study participants on the completion of the SEARCH FFQ, which was generally self-administered with interviewer assistance. However, interview administration was offered if necessary.
DASH score
Adherence to the DASH Eating Plan was assessed with an index variable that comprised the 8 DASH food groups (grains, vegetables, fruits, dairy, meat, nuts/seeds/legumes, fats/oils, and sweets)18,19. For each food group, a maximum score of 10 could be achieved when the intake met the recommendation19, while lower intakes were scored proportionately. If lower intakes are favored by DASH, reverse scoring was applied, and a score of 0 was applied to intakes ≥200% the upper recommended level. The resulting 8 component scores were summed to create the overall DASH adherence score, which could range from 0 to 80.
Details of the index components and the score standards are summarized in Table 1. In order to more closely reflect the recommendations of DASH18–20, the grain and dairy components consisted of two items and addressed a qualitative goal in addition to an absolute quantitative one.
Table 1.
Components of the DASH index*.
| Score Component | Maximum score | Standard for maximum score | Standard for minimum score of 0 |
|---|---|---|---|
| 1) Grains | |||
| a) total | 5 | ≥6 servings/day | 0 servings/day |
| b) high fiber | 5 | ≥50% of daily servings | 0% of daily servings |
| 2) Vegetables | 10 | ≥4 servings/day | 0 servings/day |
| 3) Fruit | 10 | ≥4 servings/day | 0 servings/day |
| 4) Dairy | |||
| a) total | 5 | ≥2 servings/day | 0 servings/day |
| b) low-fat | 5 | ≥75% of daily servings | 0% of daily servings |
| 5) Meat, poultry, fish, eggs | 10 | ≤2 servings/day | ≥ 4 servings/day |
| 6) Nuts, seeds, legumes | 10 | ≥4 servings/week | 0 servings/week |
| 7) Fats, oils | 10 | ≤3 servings/day | ≥ 6 servings/day |
| 8) Sweets | 10 | ≤5 servings/week | ≥ 10 servings/week |
For 2,000 kcal/day. Intakes between minimum and maximum levels scored proportionally.
Wherever possible, we adjusted the standard serving sizes in SEARCH to those of the DASH Eating Plan. Adjustments were not feasible for a variety of mixed (meat) dishes, but usually 1 (medium) piece or portion represented 1 serving. Because the DASH Eating Plan of the National Heart, Lung, and Blood Institute (NHLBI) gives recommendations for four levels of daily energy intake (1,600/2,000/2,300/3,100 kcal/day), we assigned each individual the energy level that was closest to the estimated energy requirement based on age, sex, and physical activity level (PAL)21. Physical activity in SEARCH was assessed by questions derived from the Youth Risk Behavior Surveillance System22. Youth who reported neither moderate nor vigorous physical activity ≥5 days/week were classified as sedentary, those who were either moderately or vigorously physically active ≥5 days/week as low active, and those who were both moderately and vigorously physically active ≥5 days/week as active.
Statistical analysis
We considered all youth whose DM was prevalent in 2001 or incident between 2002 and 2005. Of 8,031 registered youth that met these criteria, 3,707 attended a study visit and were aged ≥10 years at that time. Youth with other or unknown clinical DM type (n=39) were excluded. Among the remaining 3,668 participants, 462 did not fill out the FFQ, and 159 were excluded because of serious quality problems with the dietary data. This number was further reduced after excluding those without measured blood pressure (n=151). Other information relevant to this analysis, such as physical activity or parental education, was missing in 156. The final sample size thus was 2,830 (2,440 with T1DM, 390 with T2DM).
Proportionately more youth with T2DM than T1DM were excluded (n=248 vs. n=590; 39% vs. 19.5%), mainly due to lack or limited quality of the dietary data. Excluded youth with T1DM were more likely to be male than those with T1DM in the final dataset, while excluded youth with T2DM were older and characterized by a longer diabetes duration (p<0.05).
We investigated the relation between DASH adherence and hypertension by calculating crude and adjusted prevalence of hypertension in tertiles of DASH adherence. In addition, odds ratios (OR) with 95% confidence intervals (CI) were calculated, relative to the lowest tertile. Potential confounders were evaluated on an individual basis and in full models. BMI-SDS and energy intake (kcal/day) were considered as potential mediators, since they might lie on the pathway between the DASH diet pattern and hypertension. Linear trends across categories were performed by assigning each individual the median value of the category and modeling this variable continuously.
Because of the differences in both etiology and management, the analyses were undertaken separately for youth with T1DM and T2DM, further justified by an interaction between DASH adherence and DM type (p=0.046). In addition, potential effect modifiers were evaluated. All analyses were carried out using SAS (version 9.1), and a p-value <0.05 was considered statistically significant.
RESULTS
The overall prevalence of hypertension in the study sample was 9.8%, however, marked differences existed between youth with T1DM and T2DM (6.8% vs. 28.2%; p<0.0001). Adherence to DASH was slightly higher in T1DM than in T2DM (39.9±9.1 vs. 36.6±9.1; p<0.0001) (data not shown).
General characteristics of the study sample according to DASH adherence are summarized in Table 2. In both T1DM and T2DM, a greater adherence to DASH was associated with younger age, a higher parental education, less experience with smoking and higher physical activity. No clear relationship existed between the DASH score and obesity or BMI-SDS. As expected however, more youth with T2DM than with T1DM were obese (76.2% vs. 12.1%, p<0.0001) (data not shown).
Table 2.
General characteristics according to diabetes type and DASH adherence.
| Type 1 Diabetes (n=2,440) | Type 2 Diabetes (n=390) | ||||||
|---|---|---|---|---|---|---|---|
| Tertiles of DASH score | Tertiles of DASH score | ||||||
| Characteristic | 1 (lowest) |
3 (highest) |
p* | 1 (lowest) |
3 (highest) |
p* | |
| Demographics | |||||||
| Female (%) | 55.4 | 47.7 | 0.006 | 66.2 | 60.8 | 0.5 | |
| Age at examination (years) | 14.9 ± 2.9 | 14.7 ± 3.1 | 0.07 | 16.6 ± 2.7 | 15.5 ± 2.8 | 0.003 | |
| Race/ethnicity (%) | |||||||
| Non-Hispanic White | 71.8 | 80.9 | 0.0001 | 20.0 | 20.8 | 0.04 | |
| African American | 12.1 | 4.7 | 40.8 | 28.5 | |||
| Hispanic | 11.3 | 11.1 | 13.9 | 27.7 | |||
| Native American | 1.0 | 0.3 | 11.5 | 15.4 | |||
| All Other | 3.8 | 3.1 | 13.9 | 7.7 | |||
| Highest parental education ≥ Bachelor’s degree (%) | 38.6 | 54.5 | <0.0001 | 13.8 | 22.3 | 0.2 | |
| Clinical variables | |||||||
| Diabetes duration (years) | 3.4 (1.1;7.5) | 3.0 (1.0;6.9) | 0.2 | 1.4 (0.8;3.2) | 1.2 (0.6;2.4) | 0.2 | |
| BMI-SDS (SD)† | 0.6 ± 0.9 | 0.6 ± 0.9 | 0.5 | 2.1 ± 0.7 | 1.9 ± 0.8 | 0.09 | |
| Obesity (%)‡ | 12.7 | 10.5 | 0.2 | 81.5 | 72.3 | 0.2 | |
| Family history of hypertension (%) | 77.1 | 79.7 | 0.2 | 83.9 | 87.7 | 0.6 | |
| Behavioral Variables | |||||||
| Ever smoked (%) | 27.4 | 17.5 | <0.0001 | 39.2 | 26.2 | 0.04 | |
| Vigorous physical activity <5 d/wk (%) | 75.5 | 58.4 | <0.0001 | 84.6 | 64.6 | 0.0006 | |
Consumption of all food groups comprised in our DASH index differed significantly between tertiles (p<0.05) (Table 3). In particular, youth in the highest tertiles consumed twice as many servings of fruits and low-fat dairy products than those in the lowest. Achieving a higher DASH score was associated with a lower intake of total and saturated fat, but higher intakes of carbohydrates, fiber, calcium, magnesium and potassium (p<0.05). A higher adherence to DASH was not related to total energy intake. Despite being in the highest tertile of the DASH score, the average single food scores were still remarkably low at 0.4 out of 5 (whole grains), 3.6 out of 5 (low-fat dairy), 5.1 out of 10 (fruits), 5.3 out of 10 (vegetables) and 8.4 out of 10 for meat (data not shown).
In youth with T1DM, mean DBP decreased across tertiles of DASH adherence (p=0.04, Table 4). A similar tendency in SBP existed for both T1DM and T2DM (p=0.1), but was eliminated by adjusting for potential confounders (data not shown). Comparable results were obtained for the prevalence of hypertension: With increasing adherence to DASH, the crude prevalence declined markedly for youth with T1DM. Adjustment for confounders did not change this result (Figure 1). A decreasing tendency in the crude hypertension prevalence across tertiles of DASH adherence could also be observed in T2DM, but the differences did not reach statistical significance. Adjusting for confounders further attenuated this tendency.
Table 4.
Blood pressure characteristics overall and according to diabetes type and DASH adherence.
| Type 1 Diabetes (n=2,440) | Type 2 Diabetes (n=390) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tertiles of DASH score | Tertiles of DASH score | ||||||||||
| Characteristic | Total (n=2,830) |
1 (lowest) |
2 | 3 (highest) |
p* |
1 (lowest) |
2 | 3 (highest) |
p* | ||
| SBP (mmHg) | 107.7 ± 11.7 | 106.6 ± 11.2 | 105.7 ± 10.9 | 106.6 ± 10.6 | 0.1 | 118.1 ± 12.5 | 116.3 ± 12.2 | 115.0 ± 14.0 | 0.1 | ||
| DBP (mmHg) | 68.3 ± 10.0 | 68.2 ± 9.7 | 67.2 ± 9.7 | 67.2 ± 9.7 | 0.04 | 73.9 ± 10.9 | 72.6 ± 10.4 | 72.2 ± 10.0 | 0.4 | ||
| Hypertension | |||||||||||
| Elevated BP (%)† | 6.4 | 5.7 | 4.4 | 3.1 | 0.04 | 20.8 | 18.5 | 16.9 | 0.7 | ||
| BP medication (%) | 4.1 | 3.9 | 2.2 | 2.1 | 0.04 | 15.4 | 10.0 | 13.1 | 0.4 | ||
| Elevated BP and/or BP medication (%) | 9.8 | 9.0 | 6.4 | 5.2 | 0.01 | 31.5 | 26.2 | 26.9 | 0.6 | ||
BP, blood pressure; SBP/DBP, systolic/diastolic blood pressure. Numbers are frequencies, or means ± SD.
χ2-test for categorical, ANOVA for continuous variables.
SBP and/or DBP≥95th percentile4.
Figure 1. Adjusted* hypertension prevalence according to diabetes type and DASH adherence.
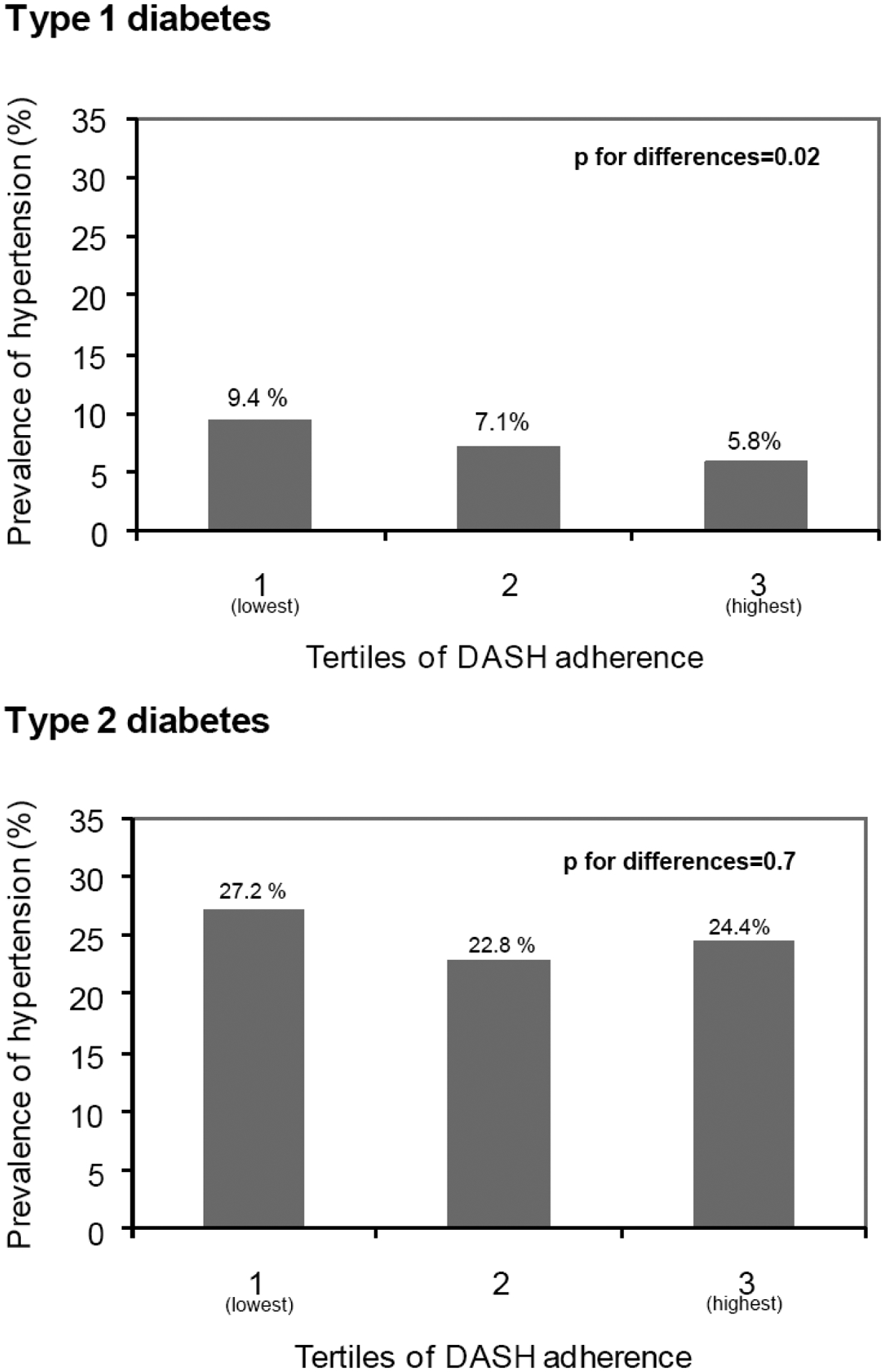
*Adjusted for sex, age, study center, race/ethnicity, diabetes duration, family history of high BP, vigorous physical activity (<5 days/week yes/no).
We next evaluated the association in multiple logistic regression models. After adjustment for demographic, clinical, and behavioral characteristics, the odds of having hypertension among youth in the highest tertile of DASH adherence was 40% lower than in the lowest tertile (model 1, 95%CI: 0.38; 0.86) (Table 5). In addition, a statistically significant trend towards decreasing odds existed across tertiles (p=0.007). Additional inclusion of energy intake (model 2) and BMI-SDS (model 3) did not affect these results. In youth with T2DM, the crude OR indicated a slightly decreasing trend across tertiles of DASH adherence too, but it did not reach statistical significance (p=0.4). Adjusting for demographic, clinical, behavioral factors, energy intake, and BMI-SDS (models 1–3) further reduced these differences.
Table 5.
Odds Ratios (95% confidence intervals) for hypertension according to diabetes type and DASH adherence.
| Type 1 Diabetes (n=2,440) | Type 2 Diabetes (n=390) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Tertiles of DASH score | Tertiles of DASH score | ||||||||
| Model | 1 (lowest) |
2 | 3 (highest) |
ptrend | 1 (lowest) |
2 | 3 (highest) |
ptrend | |
| Crude | 1.00 | 0.69 (0.48; 1.00) | 0.55 (0.37; 0.82) | 0.003 | 1.00 | 0.77 (0.45; 1.32) | 0.80 (0.47; 1.37) | 0.4 | |
| Model 1* | 1.00 | 0.71 (0.49; 1.04) | 0.57 (0.38; 0.85) | 0.006 | 1.00 | 0.81 (0.46; 1.42) | 0.87 (0.49; 1.57) | 0.6 | |
| Model 2† | 1.00 | 0.71 (0.49; 1.04) | 0.56 (0.37; 0.84) | 0.005 | 1.00 | 0.81 (0.46; 1.42) | 0.87 (0.49; 1.57) | 0.6 | |
| Model 3‡ | 1.00 | 0.70 (0.48; 1.03) | 0.57 (0.38; 0.85) | 0.006 | 1.00 | 0.97 (0.54; 1.75) | 0.98 (0.53; 1.81) | 0.9 | |
Adjusted for sex, age, study center, race/ethnicity, diabetes duration, family history of high blood pressure, vigorous physical activity (<5 days/week yes/no).
Model 1+energy intake.
Model 2+BMI standard deviation score (BMI-SDS).
Finally, adjustment for the micronutrients potassium, calcium or magnesium did not attenuate the findings in T1DM, and the association remained statistically significant (data not shown). In addition, we evaluated potential effect modification by sex, age, race/ethnicity, and obesity by conducting stratified analyses and including interaction terms in models. No evidence for effect modification existed (p-values for interaction terms>0.1).
DISCUSSION
To the best of our knowledge, this is the first study to examine the association between the DASH diet pattern and hypertension in persons with DM, and the first to focus on youth. A greater adherence to DASH was associated with markedly decreased odds of hypertension in youth with T1DM. It is noteworthy that the effect size was large compared to observational studies that focused on single nutrients or food groups only when assessing diet-disease relationships, a potential advantage of dietary pattern analysis discussed previously.
We did not observe a significant association between DASH adherence and hypertension in youth with T2DM. The most likely reason for this is limited statistical power. Our sample size was sufficient to detect an OR of 0.41 between two tertiles with 80% power (alpha=0.05, two-tailed). However, the absence of a relation might also stem from the differences in hypertension pathophysiology in T2DM, compared to T1DM1. In addition, most youth with T2DM were obese (76.8%). It is possible that in the obese state, quantitative aspects of diet, in particular energy balance, are of greater relevance than qualitative ones. Finally, the DASH adherence scores were statistically significantly lower in youth with T2DM than in T1DM.
Since the publication of the DASH trial results in 19975, the DASH dietary pattern has been widely recommended to prevent and treat hypertension23 and is now part of the 2005 Dietary Guidelines for Americans24. However, its practical application has recently been questioned25. While the DASH trials were designed as feeding studies and thus represented a best case scenario with optimal adherence, intervention studies in free-living populations have been inconsistant6, 25.
Only a limited number of studies have assessed adherence to DASH in observational settings. In the EPIC-Potsdam Study, women in the third, but not the highest quartile of a DASH score had a lower risk for hypertension26. A higher DASH score was associated with lower BP increases in the SU.VI.MAX cohort too, but the effect was not stronger than that of fruit and vegetables alone27. Although fat quality was evaluated in SU.VI.MAX, the DASH index used in both studies only included standardized intakes of vegetables, fruits and dairy. This might be an important shortcoming, because each DASH food group contributes critical nutrients20. More comprehensive applications of the DASH diet to observational data were used in the Iowa Womeńs Health Study (IWHS)7 and the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial28. In the IWHS, no association between DASH adherence and incidence of (self-reported) hypertension and cardiovascular mortality existed. However, their DASH index was positively associated with energy and sodium intake, thus perhaps not capturing a truly favorable overall diet. By contrast, the cross-sectional analysis of the PLCO Study focused on distal colorectal adenoma. A reduced risk with increasing DASH adherence existed in the group of male former smokers only.
Overall, the limited number of observational studies was almost exclusively based on adult study populations. One of the few studies focusing on children has demonstrated that an increased intake of fruits, vegetables and dairy in the pre-school years might be related to lower BP levels during childhood9. In fact, it is generally assumed that a greater DASH adherence would equally benefit pediatric age groups. An increased intake of central food groups are accordingly recommended for (pre)hypertensive youth, and prevention purposes4. With regards to DM, the current ADA guidelines on Medical Nutrition Therapy (MNT) in DM advocate a diet low in sodium and high in fruits, vegetables and low-fat dairy products to lower BP in normo- and hypertensive diabetic persons, with DASH being explicitly mentioned29. Furthermore, a joint scientific statement by the American Heart Association (AHA) and the ADA, targeting primary prevention of cardiovascular disease in DM, recommends lifestyle therapy, including a diet pattern similar to DASH, for (pre)hypertensive patients2. However, only studies in general populations served as references.
Until today, it is unclear through which mechanism(s) the DASH diet exerts its antihypertensive properties, although a natriuretic action has been proposed30. Reduced sodium and increased potassium intake represent dietary factors that seem to lower BP, at least in adults23. However, the original DASH trial held sodium intake constant, although a combination of DASH and sodium restriction was even more effective31. Other dietary factors targeted by the DASH diet (fiber, saturated fat, magnesium) differed significantly between tertiles of DASH adherence in our study, but the evidence for BP lowering properties is inconclusive for them23. Only a higher protein intake yielded promising results in observational and intervention studies, in particular when substituting carbohydrates32, 33. However, differences in protein intake between tertiles of DASH adherence in our study were small, and intake of carbohydrates was positively associated with adherence to DASH. To summarize, it is most likely that DASH exerts a beneficial effect beyond that of single dietary factors, as has been hypothesized earlier34. Accordingly, adjusting for several nutrients that could function as mediators did not explain our results in T1DM.
Our study has several limitations. First, our results are based on cross-sectional data, and youth diagnosed with hypertension might have changed their dietary habits accordingly. However, taking into account awareness of hypertension did not change our results. Second, our BP data was based on three averaged BP measurements, taken at one visit instead of at least three different occasions4. In addition, our definition of hypertension included taking antihypertensive medication, as is common practice in general35 as well as diabetic36–38 populations. It is possible that some of the SEARCH participants will have been prescribed these medications for reasons other than to reduce BP levels, in particular for renal protection. However, changing our definition of hypertension to a) having elevated SBP or DBP (≥95th percentile), or b) having a diagnosis of hypertension and/or elevated SBP or DBP (≥95th percentile), did not change our conclusions. Third, as already stated above, overall adherence to DASH was low, but will most likely have resulted in an underestimation of effects. Fourth, no consensus exists about how to best create a DASH index, i.e. which items to include, whether to consider food groups and/or nutrients, or how to weight components. Fifth, we were not able to adjust for sodium intake, which might have mediated the association between DASH adherence and hypertension, but estimation of sodium from a FFQ is questionable39. A final limitation is that applying a FFQ to estimate dietary intake is prone to measurement error. Since obese study participants tend to greater underreporting of dietary intakes40, the lack of an association in T2DM could also stem from less valid dietary data. However, currently no biomarker capturing dietary patterns as a whole is available.
Perspectives
In conclusion, a higher adherence to the DASH Eating Plan was associated with decreased odds of hypertension in youth with T1DM. Prospective studies are needed to investigate whether advocating central aspects of DASH may help prevent and control elevated BP levels in this population. In T2DM, DASH adherence was not associated with hypertension, perhaps because of inadequate sample size.
Acknowledgements:
The SEARCH for Diabetes in Youth Study is indebted to the many youth and their families, and their health care providers, whose participation made this study possible.
Furthermore, the authors wish to acknowledge the involvement of General Clinical Research Centers (GCRC) at the following institutions in the SEARCH for Diabetes in Youth Study: Medical University of South Carolina (Grant Number M01 RR01070); Cincinnati Children’s Hospital (Grant Number M01 RR08084); Children’s Hospital and Regional Medical Center and the University of Washington School of Medicine (Grant Number M01RR00037 and M01RR001271); Colorado Pediatric General Clinical Research Center (Grant Number M01 RR00069).
Funding: ALB Günther was supported by the Heinrich Hertz-Foundation (Ministry of Innovation, Science, Research and Technology, North Rhine-Westphalia, Germany).
SEARCH for Diabetes in Youth is funded by the Centers for Disease Control and Prevention (CDC) (PA number 00097 and DP-05-069) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Site Contract Numbers: California (U01 DP000246); Colorado (U01 DP000247); Hawaii (U01 DP000245); Ohio (U01 DP000248); South Carolina (U01 DP000254); Washington (U01 DP000244); Coordinating Center (U01 DP000250).
Footnotes
The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the CDC and the NIDDK.
Disclosures: None
REFERENCES
- 1.Arauz-Pacheco C, Parrott MA, Raskin P. Hypertension management in adults with diabetes. Diabetes Care. 2004; 27 Suppl 1:S65–67. [DOI] [PubMed] [Google Scholar]
- 2.Buse JB, Ginsberg HN, Bakris GL, Clark NG, Costa F, Eckel R, Fonseca V, Gerstein HC, Grundy S, Nesto RW, Pignone MP, Plutzky J, Porte D, Redberg R, Stitzel KF, Stone NJ. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care. 2007;30:162–172. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez BL, Fujimoto WY, Mayer-Davis EJ, Imperatore G, Williams DE, Bell RA, Wadwa RP, Palla SL, Liu LL, Kershnar A, Daniels SR, Linder B. Prevalence of cardiovascular disease risk factors in U.S. children and adolescents with diabetes: the SEARCH for diabetes in youth study. Diabetes Care. 2006;29:1891–1896. [DOI] [PubMed] [Google Scholar]
- 4.National High Blood Pressure Education Program Working Group on Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576. [PubMed] [Google Scholar]
- 5.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–1124. [DOI] [PubMed] [Google Scholar]
- 6.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289:2083–2093. [DOI] [PubMed] [Google Scholar]
- 7.Folsom AR, Parker ED, Harnack LJ. Degree of concordance with DASH diet guidelines and incidence of hypertension and fatal cardiovascular disease. Am J Hypertens. 2007;20:225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Obarzanek E, Vollmer WM, Lin PH, Cooper LS, Young DR, Ard JD, Stevens VJ, Simons-Morton DG, Svetkey LP, Harsha DW, Elmer PJ, Appel LJ. Effects of individual components of multiple behavior changes: the PREMIER trial. Am J Health Behav. 2007;31:545–560. [DOI] [PubMed] [Google Scholar]
- 9.Moore LL, Singer MR, Bradlee ML, Djousse L, Proctor MH, Cupples LA, Ellison RC. Intake of fruits, vegetables, and dairy products in early childhood and subsequent blood pressure change. Epidemiology. 2005;16:4–11. [DOI] [PubMed] [Google Scholar]
- 10.Couch SC, Daniels SR. Diet and blood pressure in children. Curr Opin Pediatr. 2005;17:642–647. [DOI] [PubMed] [Google Scholar]
- 11.Simons-Morton DG, Obarzanek E. Diet and blood pressure in children and adolescents. Pediatr Nephrol. 1997;11:244–249. [DOI] [PubMed] [Google Scholar]
- 12.SEARCH for Diabetes in Youth Writing Group. SEARCH for Diabetes in Youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials. 2004;25:458–471. [DOI] [PubMed] [Google Scholar]
- 13.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., Jones DW, Materson BJ, Oparil S, Wright JT Jr., Roccella EJ. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 14.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002:1–190. [PubMed] [Google Scholar]
- 15.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164–192. [DOI] [PubMed] [Google Scholar]
- 16.Block G, Murphy M, Roullet J, Wakimoto P, Crawford P, Block T. Pilot validation of a FFQ for children 8–10 years Fourth International Conference on Dietary Assessment Methods. September 17, 2000; Tucson, AZ: (Abstract). [Google Scholar]
- 17.Mayer-Davis EJ, Nichols M, Liese AD, Bell RA, Dabelea DM, Johansen JM, Pihoker C, Rodriguez BL, Thomas J, Williams D. Dietary intake among youth with diabetes: the SEARCH for Diabetes in Youth Study. J Am Diet Assoc. 2006;106:689–697. [DOI] [PubMed] [Google Scholar]
- 18.Windhauser MM, Ernst DB, Karanja NM, Crawford SW, Redican SE, Swain JF, Karimbakas JM, Champagne CM, Hoben KP, Evans MA. Translating the Dietary Approaches to Stop Hypertension diet from research to practice: dietary and behavior change techniques. DASH Collaborative Research Group. J Am Diet Assoc. 1999;99:S90–95. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute. Your guide to lowering your blood pressure with DASH. DASH Eating Plan. Available at: http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf. Accessed February 10, 2008.
- 20.Lin PH, Aickin M, Champagne C, Craddick S, Sacks FM, McCarron P, Most-Windhauser MM, Rukenbrod F, Haworth L. Food group sources of nutrients in the dietary patterns of the DASH-Sodium trial. J Am Diet Assoc. 2003;103:488–496. [DOI] [PubMed] [Google Scholar]
- 21.Food and Nutrition Board of the Institute of Medicine, The National Academies. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids (macronutrients). Washington DC: National Academies Press; 2005. [DOI] [PubMed] [Google Scholar]
- 22.Grunbaum JA, Kann L, Kinchen S, Ross J, Hawkins J, Lowry R, Harris WA, McManus T, Chyen D, Collins J. Youth risk behavior surveillance--United States, 2003. MMWR Surveill Summ. 2004;53:1–96. [PubMed] [Google Scholar]
- 23.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. 2006;47:296–308. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Department of Health and Human Services and USDA. Dietary guidelines for Americans 2005. 6th ed Washington DC: U.S. Government Printing Office; 2005. [Google Scholar]
- 25.Logan AG. DASH Diet: time for a critical appraisal? Am J Hypertens. 2007;20:223–224. [DOI] [PubMed] [Google Scholar]
- 26.Schulze MB, Hoffmann K, Kroke A, Boeing H. Risk of hypertension among women in the EPIC-Potsdam Study: comparison of relative risk estimates for exploratory and hypothesis-oriented dietary patterns. Am J Epidemiol. 2003;158:365–373. [DOI] [PubMed] [Google Scholar]
- 27.Dauchet L, Kesse-Guyot E, Czernichow S, Bertrais S, Estaquio C, Peneau S, Vergnaud AC, Chat-Yung S, Castetbon K, Deschamps V, Brindel P, Hercberg S. Dietary patterns and blood pressure change over 5-y follow-up in the SU.VI.MAX cohort. Am J Clin Nutr. 2007;85:1650–1656. [DOI] [PubMed] [Google Scholar]
- 28.Dixon LB, Subar AF, Peters U, Weissfeld JL, Bresalier RS, Risch A, Schatzkin A, Hayes RB. Adherence to the USDA Food Guide, DASH Eating Plan, and Mediterranean dietary pattern reduces risk of colorectal adenoma. J Nutr. 2007;137:2443–2450. [DOI] [PubMed] [Google Scholar]
- 29.Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, Holzmeister LA, Hoogwerf B, Mayer-Davis E, Mooradian AD, Purnell JQ, Wheeler M. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2002;25:148–198. [DOI] [PubMed] [Google Scholar]
- 30.Akita S, Sacks FM, Svetkey LP, Conlin PR, Kimura G. Effects of the Dietary Approaches to Stop Hypertension (DASH) diet on the pressure-natriuresis relationship. Hypertension. 2003;42:8–13. [DOI] [PubMed] [Google Scholar]
- 31.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, Karanja N, Lin PH. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 32.Appel LJ. The effects of protein intake on blood pressure and cardiovascular disease. Curr Opin Lipidol. 2003;14:55–59. [DOI] [PubMed] [Google Scholar]
- 33.Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER 3rd, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, Charleston J, McCarron P, Bishop LM. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005;294:2455–2464. [DOI] [PubMed] [Google Scholar]
- 34.Appel LJ. Lifestyle modification as a means to prevent and treat high blood pressure. J Am Soc Nephrol. 2003;14:S99–S102. [DOI] [PubMed] [Google Scholar]
- 35.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. [DOI] [PubMed] [Google Scholar]
- 36.Collado-Mesa F, Colhoun HM, Stevens LK, Boavida J, Ferriss JB, Karamanos B, Kempler P, Michel G, Roglic G, Fuller JH. Prevalence and management of hypertension in type 1 diabetes mellitus in Europe: the EURODIAB IDDM Complications Study. Diabet Med. 1999;16:41–48. [DOI] [PubMed] [Google Scholar]
- 37.Geiss LS, Rolka DB, Engelgau MM. Elevated blood pressure among U.S. adults with diabetes, 1988–1994. Am J Prev Med. 2002;22:42–48. [DOI] [PubMed] [Google Scholar]
- 38.Maahs DM, Kinney GL, Wadwa P, Snell-Bergeon JK, Dabelea D, Hokanson J, Ehrlich J, Garg S, Eckel RH, Rewers MJ. Hypertension prevalence, awareness, treatment, and control in an adult type 1 diabetes population and a comparable general population. Diabetes Care. 2005;28:301–306. [DOI] [PubMed] [Google Scholar]
- 39.Khaw KT, Bingham S, Welch A, Luben R, O’Brien E, Wareham N, Day N. Blood pressure and urinary sodium in men and women: the Norfolk Cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk). Am J Clin Nutr. 2004;80:1397–403. [DOI] [PubMed] [Google Scholar]
- 40.Lissner L, Troiano RP, Midthune D, Heitmann BL, Kipnis V, Subar AF, Potischman N. OPEN about obesity: recovery biomarkers, dietary reporting errors and BMI. Int J Obes (Lond). 2007;31:956–961. [DOI] [PubMed] [Google Scholar]


