Abstract
The COVID-19 pandemic poses significant challenges to patients with end-stage kidney disease who receive treatment in outpatient dialysis centers. These patients represent a fragile population that is at higher risk for both infection and transmission. At the start of the pandemic, many suspected COVID-19 dialysis patients were diverted to the emergency department (ED) for testing/treatment, placing a tremendous burden on the ED and inpatient dialysis units. Several recommendations and guidelines have been established to optimize patient care while also decreasing the burden on the ED and inpatient dialysis units and maximizing the ability to perform outpatient hemodialysis. As the pandemic continues, dialysis facilities will have an increasing burden to provide safe and accessible dialysis, while also being able to direct patients to the ED for either emergent dialysis or COVID-19 treatment/testing. We reviewed opinions, recommendations and guidelines developed by professional organizations and dialysis facilities for the management of “patients under investigation” (PUIs) and COVID-19 positive patients that depend on whether the suspicion occurs while the patient is at home vs. at the dialysis center.
Keywords: COVID-19, Hemodialysis, Emergency department, End-stage kidney disease, Nephrology, Dialysis
1. Introduction
The COVID-19 pandemic poses significant challenges to dialyze patients who are treated with hemodialysis (HD) in outpatient dialysis centers. Dialysis centers are poised to have an unusually high disease burden given the high density of patients in a dialysis center and the immunocompromised state of the dialysis patient [[1], [2], [3]]. Dialysis patients are a particularly susceptible population to the novel virus because of their combined risk factors for disease; including age, comorbid disease, and less efficient immune systems [4,5]. It has even been suggested that due to the lack of a robust immune system, dialysis patients will have only mild symptoms in early stages of the disease and therefore have a higher risk of spreading the infection [3,6]. Dialysis patients are required to travel to-and-from dialysis sessions, despite their COVID-19 status, and be in close contact with one another during treatments, increasing the risk of disease exposure and transmission to fellow patients. Therefore, the outpatient dialysis center is a paradox to “social distancing,” especially for an extremely fragile patient population.
Early in the pandemic, emergency physicians noted there was a high propensity to divert suspected COVID-19 positive patients to emergency department (ED) for COVID-19 testing, or for dialysis treatment itself. This is largely because a dialysis patient infected with the virus places significant strain on the dialysis center's resources due to requirements for isolation, control and prevention, thus limiting the ability to comply [7]. Mt. Sinai Hospital in New York City developed a peritoneal dialysis program to “maximize the ability to provide dialysis resources for the [coronavirus] surge” in April 2020 due to the “increase in hospital demands for HD” because of the large volumes of patients showing up to the ED after missing their regularly scheduled dialysis sessions. [8] In a paper published in May 2020, Kliger and Silberzweig discuss the American Society of Nephrology's (ASN) establishment of a “COVID-19 Response Team” due to United States emergency departments and hospitals becoming overwhelmed with symptomatic dialysis patients. This response team was established to “provide evidence-based guidance to patients, healthcare professionals and dialysis facilities” regarding screening, patient placement, personal protective equipment (PPE) guidelines, environmental disinfection, communication with the health department, etc. [9] Later in the pandemic, the Centers for Disease Control and Prevention (CDC) established guidelines that recommended any symptomatic dialysis patient be transported to a tertiary care facility, unless full compliance with CDC isolation and protection recommendations could be achieved [10]. However, despite this expected resultant surge in patients to the ED, there was high variability in emergency plans and preparedness [11].
However, as the extent and longevity of the virus became more apparent, outpatient HD centers across the globe developed strict disease control and prevention protocols to minimize the risk of transmission to other patients and healthcare personnel. There have also been several policies/guidelines, regarding dialysis patients and other patient populations, established to aid health care providers in their decision of when to direct a patient to the ED when suspected of COVID-19. These policies continue to evolve globally and in the United States, and have the potential to reduce the burdens placed on both EDs and HD centers.
In this article, we discuss guidelines that have been established with the objective to optimize patient care while also decreasing the burden on the ED and inpatient dialysis units and maximizing the ability to perform outpatient HD. We also highlight important strategies utilized by various dialysis centers across the globe to minimize the transmission of COVID-19 in outpatient HD units and adequately utilize available resources to protect both health care workers and patients. With our recommendations in mind, our goal is to unite emergency medicine providers throughout the world to develop a plan for the management of end -stage kidney disease (ESKD) patients on dialysis during a global pandemic.
2. Methods
The authors searched PubMed, SCOPUS, and Google Scholar for articles using key terms related to COVID-19, “SARS-COV-2”, adult hemodialysis, and emergency department, a combination of keywords “COVID-19”, and “Dialysis”, “hemodialysis, and “Emergency Department”. Articles were not included if they were not primarily in English or did not have an English translation, were focused on pediatric patients or were preliminary/unpublished results. We included studies such as letters, perspectives, clinical guidelines, and retrospective studies. The reference lists of selected articles were reviewed for additional studies. We include several primary references from sources deemed reputable by the authors including the CDC and policies accessible to the public from national dialysis companies.
3. Results
3.1. Testing/screening for COVID-19 in United States dialysis centers
Guidelines for managing “persons under investigation” (PUIs) and COVID-19 positive patients vary across outpatient HD facilities. The CDC established guidelines for patient screening at dialysis, which are being followed by several prominent outpatient HD facilities in the United States [12] to optimize PPE usage and protect COVID-19 negative patients, while also properly treating COVID-19 positive patients requiring dialysis. In an editorial from late March 2020, Weiner and Watnick pointed out that there are two options for both PUIs and clinically stable COVID-19 patients who present to their dialysis centers - either dialyze in place (which requires adequate PPE, staffing, appropriate social distancing, etc.) or refer to the hospital for testing or treatment [13]. This editorial also explores the option of home dialysis. Although transitioning a large number of hemodialysis patients from the outpatient in-center setting to the home setting would significantly decrease the burden on hemodialysis facilities, this would be extremely resource intensive and not feasible due to the need for peritoneal dialysis (PD) catheter placement. At this point in the pandemic, PD catheter placement was not considered a “priority procedure.” Although resource intensive, the authors discussed how critical increasing the use of home dialysis will be throughout the pandemic to “reduce the risk for COVID-19 infection in both patients with kidney failure and the staff needed to care for them, thereby reducing the risk to the entire community [13].
The CDC guidelines stress the importance of prompt identification of PUIs, dialyzing PUIs separately, monitoring exposure of the healthcare personnel, and adequate communication among all persons within the dialysis facility to minimize the spread of infection [12]. They recommend screening dialysis patients at the door by asking about recognized symptoms of COVID-19 seen in Table 1 to include; cough, diarrhea, fever, muscle aches, etc., and measuring their temperature at the door. They also recommend that dialysis centers implement a phone triaging system to limit the risk of disease transmission and exposure. Healthcare personnel should call patients on the day of dialysis to screen them over the phone for COVID-19 symptoms/exposure. If a patient screens positive, the facility's healthcare provider (nephrologist) should be notified. At the discretion of the dialysis center providers, patients will be directed to the emergency room/urgent care for further evaluation and treatment. The aim of referral is to identify and treat any patients who may require immediate and/or emergent treatment for their COVID-19 infection [12].
Table 1.
CDC recognized symptoms of COVID-19
| Fever (> 38 °C or 100.4 °F) or chills |
| Cough |
| Shortness of breath |
| Fatigue |
| Muscle or body aches |
| Headache |
| New loss of taste or smell |
| Sore throat |
| Congestion or runny nose |
| Nausea or vomiting |
| Diarrhea |
As the pandemic has evolved, the CDC has added recommendations on the assessment of asymptomatic patients who have been exposed to a suspected or lab-confirmed case of COVID-19. Like symptomatic patients, asymptomatic persons are an importance cause for the spread of the virus. These persons are also considered PUIs. The CDC stresses the importance of interviewing the asymptomatic close contact by phone or video conference. If this is not possible, the healthcare personnel must stay at least 6 ft away from the close contact while both are wearing facemasks. If the healthcare personnel has to enter the close contact's home, take their temperature, or swab them for the virus, the guidelines discuss the importance of adequate PPE and proper hand hygiene. If the asymptomatic patient has come into contact with a lab-confirmed case of COVID-19, they must self-isolate for 14 days after contact for testing and symptom monitoring [14].
Using the CDC guidelines as a foundation, Ikizler and Kliger published recommendations on how to minimize the transmission of COVID-19 in outpatient dialysis centers in March 2020. They stressed the importance of each facility designing a site-specific triage plan for the disposition of their patients, whether it be to dialyze in place, transfer to a site with testing capabilities, or transfer to the ED [15]. One issue they observed is that patients were transferred to the ED with the goal of minimizing exposure of infected patients in the dialysis facilities. This occurred without realization that hospital resources are very likely to reach capacity [15]. Therefore, dialysis facilities must anticipate this likelihood, and develop policies to manage clinically stable patients with confirmed or suspected COVID-19 in-center.
A large US dialysis organization providing dialysis services to ~190,000 patients in over 2400 nationwide facilities has developed both in-center and patient safety policies for COVID-19 using the CDC guidelines as a basis [16]. All individuals (patients, visitors, healthcare workers) are screened for COVID-19 symptoms and exposure before entering the center. Visitors are not permitted in the centers to reduce disease transmission. All patients are provided with surgical masks both in the waiting room and in the treatment area, and strict hand washing policies (upon entry and exit) have been established. Staff members are required to wear full PPE when in contact with a dialysis patient, to include mask, gown, gloves, and eye protection. Patients who screen positive for COVID-19 (based on CDC guidelines) will either be dialyzed in place in a separate area, or if deemed necessary by their organization's policy, will be sent to the hospital for further testing/treatment. This has the potential to significantly decrease the burden on the ED and the inpatient dialysis units by not referring every PUI to the hospital. They have also developed a telehealth option for routine appointments with nephrologists, social workers, dialysis nurses, dieticians to limit disease exposure. Patients are urged to contact their nephrologist or their dialysis center if they have advanced symptoms of COVID-19, to include fever >100.4 °F, shortness of breath or general malaise. Lastly, all isolation centers or centers with isolation shifts must undergo a thorough cleaning after each dialysis shift [16].
In the US, it is currently recommended that patients with symptoms should be dialyzed in hospitals rather than in isolation rooms at hemodialysis facilities unless the facility can comply with CDC guidelines [17]. However, one major concern is the possibility of inpatient hemodialysis units reaching capacity, requiring dialysis of even symptomatic patients at outpatient facilities. In this instance, patients should be placed in face masks as soon as they arrive in the facility and should be dialyzed in a separate room with the door closed [17].
Akbarialiabad and Kavousi published a systematic review on COVID-19 and maintenance hemodialysis in November 2020. They reviewed multiple papers, mostly from the United States and Italy, which discussed the patient-related, staff-related and dialysis facility-related policies and guidelines developed by dialysis centers to “guide future prevention of infection and management of patients with ESRD and COVID-19.” The authors found that many of the recommendations overlapped but did note some unique differences worth mentioning. In regard to screening, the authors discussed the importance of changing the screening questions as the pandemic evolves, having the patients call the dialysis unit prior to their session to respond to screening questions, and initiating temperature checks both before entering the unit and during the dialysis session [18].
3.2. International approach to dialysis patients in the COVID-19 era
3.2.1. Europe
The European Dialysis (EUDIAL) Working Group of European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) established guidelines for the “prevention, mitigation and containment” of the COVID-19 pandemic in outpatient dialysis centers [7].
The goal of the ERA-EDTA's guidelines was to “minimize the risk for other patients and personnel taking care of these patients,” in outpatient dialysis centers, which, in turn, reduces ED and hospital burden [7]. (Table 2 ) If isolation rooms for confirmed positive patients were unavailable in outpatient centers, they should be transported to the nearest emergency department for admission for dialysis [7]. In these patients, the ED provider must determine the threshold for dialysis. This places the patient, the transporters, and emergency department staff at greater risk of exposure.
Table 2.
Summary of European Renal Association-European Dialysis and Transplant Association recommendations to reduce transmission of COVID-19 in dialysis centers
| Dialysis Patients | Healthcare Team | |
|---|---|---|
| Education |
|
|
| Infection Control |
|
|
| Communication |
|
|
| Isolation |
|
|
Adapted from Basile C, et al. Nephrol Dial Transplant. 2020;35(5):737–741. [7].
Both the Italians and Belgians used these guidelines as a basis to further expand these recommendations to develop their own approaches to managing dialysis patients during this era [19].
The Belgians highlighted the significance of early detection of infected patients and minimizing the need for hospitalization of dialysis patients [19]. To isolate positive cases prior to patients entering the dialysis center, patients with symptoms were encouraged to discuss their symptoms by phone regardless of their clinical condition. All symptomatic dialysis patients suspected of having the virus – based on symptoms of cough/fever/muscle aches – were not allowed to enter the dialysis ward and instead were directed to the ED for reverse transcriptase-polymerase chain reaction (RT- PCR) testing, electrolyte panel and possible computed tomography (CT) scan. On non-dialysis days, symptomatic patients received point-of-care COVID-19 testing to have results before the next dialysis day. If patients were asymptomatic, but had contact with a known positive patient, then they were isolated and received a swab test, but not directed to the ED [19].
In order to determine the need for hospitalization, a dialysis patient's social situation (for example, ability to isolate from vulnerable family members and transportation means) and clinical condition must be considered. A majority of symptomatic, yet stable, dialysis patients may not be candidates for outpatient dialysis given their disability to recover at home, and therefore may require ED visit and hospitalization to receive treatment [19]. The balance of determining who needs hospitalization in a dialysis unit vs. those who can undergo outpatient dialysis has placed a significant burden on the ED as well as the in-hospital staff of the dialysis units.
Two dialysis centers in Lombardy, Italy utilized early point-of-care testing to identify and isolate 22/370 COVID-19 positive patients and subsequently prevented spread to other patients and staff, while delivering dialysis to the positive patients [20]. The authors described their policy of performing dialysis on COVID-19 positive or suspected patients while in isolation areas. It is important to note that patients in these centers were only tested if they were symptomatic - at the discretion of the facility [20]. However, all patients were advised to wear surgical masks regardless of their clinical condition. If emergent dialysis was indicated, the patient was required to be hospitalized [19]. They also recommended “hospitalization until full recovery,” which is not always necessary if the patient becomes clinically stable, but is still mildly symptomatic.
3.2.2. China
In May 2020, physicians in China developed a set of “practical management recommendations” for healthcare providers, dialysis patients, and dialysis facilities for the management of ESKD patients on dialysis during the COVID-19 pandemic. These include recommendations for the screening of dialysis patients, handwashing and PPE training, dialyzing patients under investigation in separate units, equipment decontamination, avoidance of public transportation, and avoidance of unnecessary hospital visits [21].
In Wuhan, China, they were able to set up COVID-19 designated hospitals to centrally isolate and manage COVID-19 positive dialysis patient [22]. If it was not possible for the patient to be transferred to a COVID-19 designated hospital, the patient was referred to a center with a designated COVID-19 positive shift, preferably at the end of the day to further limit exposure. All of the patients in the designated COVID-19 hospitals received chest CTs as a means of diagnosing disease severity and prognosis [22]. This puts a huge burden on EDs and could be considered a waste of hospital resources.
In June 2020, a leading university hospital in Beijing China, Peking Union Medical College Hospital, published recommendations for urgent hemodialysis for ESKD patients referred to the emergency department during the COVID-19 pandemic. The hospital developed a “dialysis consult” from the emergency department. The first step was to screen the patients for possible contact, fever, respiratory symptoms, or abnormal chest imaging. If the patients screened positive, they would then have an infectious disease consultation. The ID provider would determine if the patient was stable enough for outpatient COVID testing. If positive, the patient would then be transferred to a designated COVID-19 hospital, similar to those discussed above in Wuhan. If the patient tested negative for the virus, they were to be dialyzed separate from other ESKD patients for 14 days. After fourteen days, these patients resumed routine dialysis [23].
3.3. Emergency department referral for dialysis patients
As demonstrated in the previous sections, ultimately many dialysis patients with concern for infection or exposure to COVID-19 will be transferred to the ED for further management, whether it be for COVID-19 testing or for dialysis treatment. However, policies of ED referrals have varied considerably based on; geographic location, time in the pandemic, and system resource availability.
In collaboration with the American Society of Nephrology (ASN), the American College of Emergency Physicians (ACEP) developed guidelines on when to direct patients to the ED. The organization recommended that if a patient has mild symptoms of COVID-19 infection that would not otherwise require hospitalization, then centers should follow infection control guidelines as provided by the CDC and perform dialysis at the center as normal, with proper isolation precautions [12,24,25] If a patient is referred to the ED, then ACEP recommends discussing this first with an accepting physician to deliver care most optimally and timely [25].
The ACEP and ASN issued a joint statement on appropriate use of the ED during the pandemic [26]. The recommendation is that patients with suspected or confirmed COVID-19 should follow CDC guidelines on infection prevention and control [12,26]. However, the recommendation is that patients with “… mild symptoms that do not require hospitalization should not be referred to the ED.” If the patient is to be referred for a non-emergent complaint then the “… dialysis center should discuss the case with their medical director and the ED before sending the patient” [26].
The Pandemic Respiratory Infection Emergency System Triage (PRIEST) study was performed by the University of Sheffield's School of Health and Related Research in the United Kingdom as a response to the COVID-19 pandemic to “optimize the triage of people with suspected respiratory infections during a pandemic [and] to identify the most accurate triage method for predicting severe illness among patients attending the emergency department with suspected respiratory infection.” [27]. The study used patient data from early phases of the COVID-19 pandemic to “test how well existing triage methods predict serious complications or recommended necessary hospital admissions.” As a result of the study, the authors developed the PRIEST COVID-19 clinical severity score, which is a triage method based upon the following: “(a) presenting clinical characteristics alone and (b) presenting clinical characteristics, electrocardiogram, chest x-ray and routine blood test results. The PRIEST score utilizes the National Early Warning Score (NEWS) as a basis for its scoring system. The NEWS score was developed by the Royal College of Physicians (RCP) in 2012 to “improve the identification, monitoring and management of unwell patients in the hospital.” The score is based on a logistic regression model designed to predict “in-hospital patient mortality within 24 hours of a set of vital signs observations” [28]. The results of the PRIEST score can be used to determine patient disposition and to determine which individual patients may develop serious complications from the virus. The PRIEST score can be utilized by dialysis facilities to determine a patient's disease severity and need for ED evaluation [29].
The Quick COVID-19 Severity Index (qCSI) is a risk stratification index developed by emergency medicine physicians in May 2020 after retrospectively studying “adult patients admitted from the emergency department who tested positive for COVID-19 up to 24 hours after initial presentation” in a nine-hospital health system in the Northeastern US [30].The qCSI index uses only physical exam and vital sign measurements (SPO2, respiratory rate, nasal flow cannula rate). The index predicts critical respiratory illness at 24-h as defined by high oxygen requirements, non-invasive ventilation, invasive ventilation, or death. This model can be utilized by dialysis facilities to determine risk of critical respiratory illness in symptomatic ESKD patients [30].
In Italy, patients who were either symptomatic or known to be COVID-19 positive were primarily dialyzed within the HD facility with proper isolation precautions. Patients were referred to the ED for evaluation and work-up if they had fever and signs of significant or worsening/unstable airway disease. If a patient was in “... respiratory distress or failure ER staff must be summoned…” [20].
The Japanese Society of Nephrology highlighted the utilization of lung ultrasound as a “valuable tool for the assessment of dialysis patients with COVID-19 [31].”They note that the detection of focal B-lines on ultrasound may be more sensitive and efficient than CT findings, especially in early disease. They proposed that outpatient dialysis facilities adopt lung ultrasound as a bedside tool to diagnose and monitor disease severity, while also differentiating COVID-19 from other possible causes of dyspnea. Using lung ultrasound in outpatient facilities would also limit hospital staff exposure to potential COVID-19 patients, thereby providing infection control. Advantages of lung ultrasound are summarized in Table 3 . The society also highlighted that the greatest barrier to having lung ultrasound in outpatient facilities is that dialysis units lack trained staff for performing and interpreting the imaging studies [31].
Table 3.
Advantages of using lung ultrasound over CT-scan
| Findings are comparable to that of CT-Scan |
| Hand-held ultrasound devices are available and adequate and portable |
| Infection control – easier and quicker to disinfect portable ultrasound than a CT-scan |
| Bedside imaging study with immediate interpretation that can be repeated |
| Limits patient transport, thereby reducing disease exposure and transmission |
| No ionizing radiation with ultrasound |
Adapted from Reisinger N, et al. Clin Exp Nephrol. 2020;24(9):850–852. [31].
3.4. Emergency dialysis
There exists few reports on how emergency or emergent dialysis was performed in either COVID-19 positive or suspected COVID-19 patients. Patients who required urgent, but not emergent, dialysis were screened for fever, evaluated by an infectious disease provider, received full chest imaging workup, and then dialyzed on an isolated ward until verification of disease status. If emergent dialysis was required, on either unknown status patients or known COVID-19 patients, the patients would be transferred to designated hospitals capable of performing dialysis with proper isolation precautions. Patients were then isolated on COVID-19 units [23].
4. Discussion
As the coronavirus pandemic continues, dialysis facilities will have an increasing burden to both provide both safe and accessible dialysis, while also being able to direct patients to the ED for either emergent dialysis or COVID-19 treatment/testing. This discussion, expressing the authors' opinions based on the interpretation of available literature, will provide recommendations on two different designs related to hemodialysis patients who dialyze in outpatient centers.
4.1. The patient at home
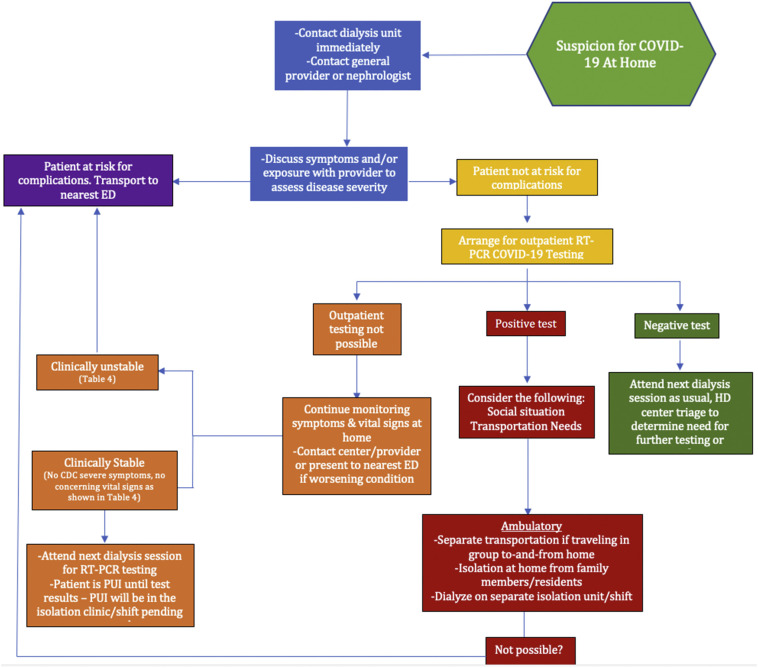
The first design provides guidelines on the approach to the dialysis patient with whom there is suspicion for COVID-19 infection while the patient is at home. (Fig. 1 ).
Fig. 1.
Algorithm for the dialysis patient who has suspicion for COVID-19 at home.
If the patient, family member, or caregiver suspects that the patient has been exposed to or is exhibiting symptoms of COVID-19 infection, it is very important that the HD center becomes aware as soon as possible. The patient or caregiver should then contact their nephrologist and/or general practitioner to discuss their symptoms or exposure. The provider will then assess disease severity by asking the patient questions. We recommend they ask the patient the CDC's Recognized Severe Symptoms of COVID-19 shown in Table 4 [32]. If the patient answers yes to any of these questions, they are therefore at risk for worsening clinical condition and should be transported to the nearest ED.
Table 4.
Assessing clinical instability of COVID-19 patients
| CDC Recognized Severe Symptoms of COVID-19 | Concerning vital signs |
|---|---|
| Trouble breathing | Intractable Fever (≥ 38 °C or 100.4 °F) |
| Cyanosis | Respiratory rate ≥ 24 breaths/min |
| Inability to wake or stay awake (lethargy) | Heart rate persistently over 100 beats/min |
| Persistent chest pain or pressure | Systolic blood pressure persistently <90 mmHg |
| New confusion | O2 saturation persistently <92% on room air |
If the patient answers “no” to all of the CDC's recognized severe symptoms, the patient's nephrologist or primary care provider should then arrange for outpatient COVID-19 testing, preferably at the patient's primary care office [19]. If outpatient testing is not available, the patient should continue to monitor their symptoms and vital signs at home for worsening clinical condition. Symptoms of worsening clinical condition and concerning vital signs are shown in Table 4. If their condition worsens, patient should present to the nearest ED and inform their nephrologist and/or general practitioner. If the patient's symptoms do not worsen and continue to have stable vital signs at home, we recommend that they present to their next scheduled dialysis session. At this point, the patient is a PUI, and the dialysis center will determine the need for testing or transport based on screening and vital signs.
If the patient tests positive for the virus, their social situation, transportation needs, and clinical condition must be considered. For the patient to safely present to their scheduled outpatient dialysis session, they must ensure that they can transport to-and-from the center individually, that they can isolate at home from family members or other residents, and that they can dialyze on a separate COVID-19 isolation shift or unit [19]. If any of these things are not possible for the patient, we recommend transport to the ED for testing, determination of emergency need for dialysis and disposition. If the patient tests positive for the virus, can travel individually, isolate at home, and has the ability to dialyze in isolation, they will be scheduled for dialysis in either a designated isolation center or shift.
If the patient tests negative for COVID-19, they can attend their next dialysis session as usual, and the dialysis center will determine if further testing is needed.
4.2. The patient at the dialysis unit
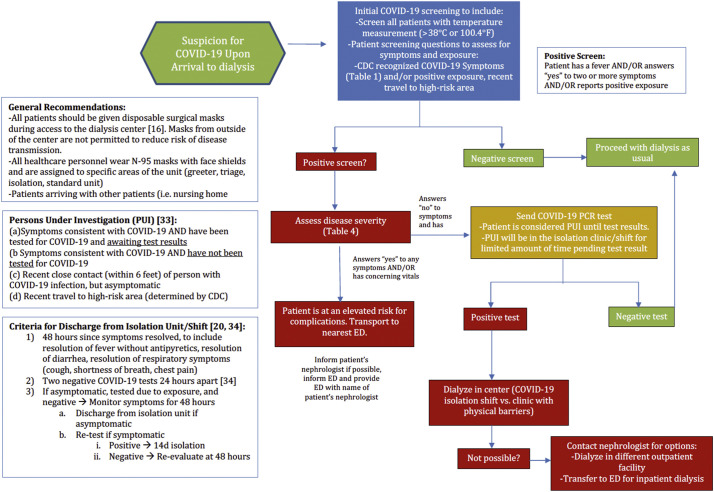
The second design (Fig. 2 ) provides guidelines on the approach to the dialysis patient with whom there is suspicion for COVID-19 infection when the patient arrives to the dialysis center. Based on guidelines reviewed so far [16, 19,22,32,33,34], we recommend that every dialysis center provide surgical masks for all patients and that patients should not be permitted to bring masks from home to reduce disease transmission. We also recommend that all healthcare personnel have access to N-95 masks and face-shields to wear at all times, and that all members of the healthcare team have designated areas and/or shifts that they will work in (greeter, triage, regular unit, isolation unit, isolation shift) [19]. Lastly, patients arriving to the unit in groups from nursing homes should be triaged separately to reduce risk of disease transmission.
Fig. 2.
Algorithm for the dialysis patient with whom there is suspicion for COVID-19 in the dialysis unit.
Every dialysis patient arriving for their dialysis session should be screened for COVID-19 before entering the unit. The greeter outside of the unit should ask questions about specific symptoms concerning for COVID-19 based on the CDC recognized symptoms for COVID-19 shown in Table 1, as well as possible exposures to the virus and recent travel to high-risk areas. If the patient answers “yes” to two or more symptoms OR answers “yes' to exposure, they are immediately considered a PUI and have a positive screen [33]. See Fig. 2 for a list of these criteria, inspired by the CDC guidelines [33]. If the patient answers “no” to symptoms and exposure, they have a negative screen and can proceed with dialysis as usual [16,19,22,32,33].
Patients who screen positive must be assessed for disease severity using the CDC's Recognized Severe COVID-19 symptoms criteria shown in Table 4. If the patient answers “no” to all of the CDC “severe” criteria and has normal vital signs, a COVID-19 PCR test should be sent immediately. The patient will then be considered a PUI until the test results, and will be placed in the isolation center/shift pending test results [19]. If the test is negative, the patient can dialyze as usual in the non-isolation unit with appropriate social distancing and physical barriers. Those who reported positive exposure without symptoms can dialyze in the normal unit, however must also be physically isolated from the other asymptomatic patients (6 ft apart with physical barriers).
If the patient answers “yes” to any of the CDC severe COVID-19 criteria and/or has abnormal vital signs, they are considered clinically unstable, are at risk for further complications of the disease, and should be transported to the ED for further evaluation. The dialysis center should notify the ED that the patient is coming, and also provide the patient with a form including the patient's name, dialysis schedule and name of their nephrologist.
If the test is positive, but the patient is either asymptomatic with exposure or deemed clinically stable, they will dialyze in-center in a designated isolation shift/unit. If it is not possible to dialyze in a designated shift/unit, this patient will be transferred to the ED for inpatient dialysis and symptom monitoring, or transferred to an isolation center. This will be at the discretion of the patient's nephrologist.
4.3. The patient discharged from an isolated COVID-19 dialysis center/shift
We recommend that patients who are being dialyzed on an isolation center/shift due to COVID-19 exposure with symptoms or a positive test must be dialyzed in this center/shift for 14 days either after exposure or positive test [22]. Following this fourteen-day period, symptoms that include respiratory symptoms, diarrhea, and resolution of fever without use of antipyretics, must be resolved for 48 h and must have two negative COVID-19 PCR tests twenty-four hours apart in order for a patient to be considered for discharge from an isolation unit/shift [34]. The CDC guidelines allow discharge just twenty-four hours from symptom resolution [34]. However, given that dialysis patients are at higher risk for complications from the virus, we recommend an additional twenty-four hours of symptom monitoring [34] prior to disposition. Secondly, if the patient reported a positive exposure with symptoms and tested negative and has been completely asymptomatic for ~48 h, the patient can resume dialysis as usual without re-testing. [22,34].
4.4. The patient referred to the emergency department
The CDC and other medical societies have provided guidelines on how to prevent the spread of COVID-19 in dialysis facilities [10]. However, there is little guidance on when to refer dialysis patients to the emergency departments for management of COVID-19. Kliger et al. recommended that “sick patients” be referred to the ED for emergent treatment [35]. Other guidances indicated referral should be done at the provider's discretion [12,13,15,26], which can lead to a large degree of practice variance.
Two distinct situations relevant to the dialysis patient in the ED during the COVID-19 pandemic arise. The first is how and when to refer a patient to the ED from a dialysis center with COVID-19 symptoms and the second is how to handle a dialysis patient in the ED who requires emergent dialysis.
If a dialysis patient shows signs of severe illness at the outpatient dialysis facility, a referral to a nearby ED can then be done for further assessment. In symptomatic patients, the dialysis facility can use the qCSI index to determine their risk of severe respiratory illness. The receiving ED should be contacted to be informed that they will be receiving a potential COVID-19 positive patient.
If the patient's nephrologist feels that the patient is clinically stable by assessing vital signs despite answering yes to one of the CDC's criteria, and have a portable ultrasound present in the facility, the nephrologist should consider looking for B-lines to evaluate fluid status before transferring the patient to the ED as recommended by the Japanese [31]. [Unfortunately, there is not always a nephrologist present in the dialysis unit, and dialysis unit nurses and other providers may not know how to diagnose and interpret ultrasound studies.] Therefore, we recommend that dialysis centers invest in at least one portable ultrasound and undergo training on point-of-care lung ultrasound to determine fluid status and to possibly save the patient a trip to the hospital and a CT scan.
If a dialysis patient arrives to an emergency department with symptoms that may require emergency dialysis, the patient should be triaged and screened for risk of COVID-19 infection based on CDC recognized symptoms [32]. If a patient screens positive, they should be isolated and tested in accordance with hospital policy - giving preference to rapid testing, as the patient will likely require inpatient admission and should avoid being on a COVID-19 ward given their immunocompromised state. The emergency department providers can also utilize the PRIEST score to help determine patient disposition and disease severity [29]. The patient in the ED should be evaluated for dialysis. If emergent dialysis is required, the patient's nephrologist or the hospital's nephrology team should be contacted to prepare for emergent dialysis. If the patient's COVID-19 status is still unknown at the time emergency dialysis is deemed necessary, the patient should be considered a COVID-19 PUI until proven otherwise on the basis of clinical emergency.
5. Limitations
There are some limitations to consider when reviewing our recommendations for the management of ESKD patients during the COVID-19 pandemic. First and foremost, COVID-19 is not fully understood and the pandemic continues to evolve; new discoveries are made daily regarding the symptoms, clinical presentation, complications and management of this novel virus. Therefore, our recommendations are built from studying literature reviews, retrospective observational studies, expert opinions, and dialysis center guidelines rather than less biased, better designed studies such as randomized control trials (RCTs). However, given the novelty of the virus and therefore lack of available data, there have been only a handful of RCTs conducted during the COVID-19 era, and none specific to ESKD patients.
Another limitation is that many of the papers we reviewed are from different countries with different patient populations and economic systems. For example, Wuhan, China established a COVID-19 designated hospital for their ESKD patients in which every single patient received a CT scan to monitor disease progression. These things have not happened in the United States since the beginning of the pandemic and unlikely to occur in other countries of less economic status or with fewer healthcare resources. Therefore, when making our recommendations, we had to consider what is most realistic here in the US for our ESKD patients.
One of the main focuses of our paper relates to emergency department referral of the ESKD patient. Although we are limited in data from the emergency medicine literature given the lack of papers on dialysis patients in the ED during a pandemic, our goal is to assist emergency medicine providers in the development of a united plan for the management of ESKD patients presenting to the emergency department during a global pandemic by reviewing the experiences, recommendations and ideas of different medical specialties in a multitude of countries worldwide. It is important to note that our recommendations above are limited by the dynamic evolution of the pandemic. For example, COVID-19 vaccines are entering their final stages of clinical trials and many patients have known antibodies to the virus. Variables such as the vaccine and development of antibodies have the potential to alter our above recommendations.
6. Conclusions
As the COVID-19 pandemic evolves, we encourage ongoing dialogues between the ED and the dialysis units it serves to communicate best practices in COVID-19 testing and hemodialysis treatments for PUI and COVID-19 positive dialysis patients.
Financial support
This is a non-funded study, with no compensation or honoraria for conducting the study.
Declaration of competing interest
The authors do not have a financial interest or relationship to disclose regarding this research project.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [doi:10.10d6/NEJMoa2001017] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naicker S., Yang C.W., Hwang S.J., Liu B.C., Chen J.H., Jha V. The novel coronavirus 2019 epidemic and kidneys. Kidney Int. 2020;97(5):824–828. doi: 10.1016/j.kint.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Syed-Ahmed M., Narayanan M. Immune dysfunction and risk of infection in chronic kidney disease. Adv Chronic Kidney Dis. 2019;26(1):8–15. doi: 10.1053/j.ackd.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Betjes M.G. Immune cell dysfunction and inflammation in end-stage renal disease. Nat Rev Nephrol. 2013;9(5):255–265. doi: 10.1038/nrneph.2013.44. [DOI] [PubMed] [Google Scholar]
- 6.Albalate M., Arribas P., Torres E. High prevalence of asymptomatic COVID-19 in haemodialysis: learning day by day in the first month of the COVID-19 pandemic. Nefrologia. 2020;40(3):279–286. doi: 10.1016/j.nefro.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basile C., Combe C., Pizzarelli F. Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in haemodialysis centers. Nephrol Dial Transplant. 2020;35(5):737–741. doi: 10.1093/ndt/gfaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El Shamy O., Sharma S., Winston J., Uribarri J. Peritoneal Dialysis during the coronavirus Disease-2019 (COVID-19) pandemic: acute inpatient and maintenance outpatient experiences. Kidney Med. 2020;2(4):377–380. doi: 10.1016/j.xkme.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kliger A.S., Silberzweig J. Mitigating risk of COVID-19 in Dialysis facilities. Clin J Am Soc Nephrol. 2020;15(5):707–709. doi: 10.2215/CJN.03340320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention Interim Guidance for Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed COVID-19 in Outpatient Hemodialysis Facilities. 2020. https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/dialysis.html Available from. [accessed 08.26.2020]
- 11.Bressan S., Buonsenso D., Farrugia R. Preparedness and response to pediatric CoVID-19 in European emergency departments: a survey of the REPEM and PERUKI networks. Ann Emerg Med. 2020 doi: 10.1016/j.annemergmed.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.“Screening Dialysis Patients for COVID-19 .” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention. www.cdc.gov/coronavirus/2019-ncov/hcp/dialysis/screening.html Available from.
- 13.Weiner D.E., Watnick S.G. Hemodialysis and COVID-19: an Achilles’ heel in the pandemic health care response in the United States. Kidney Med. 2020;2(3):227–230. doi: 10.1016/j.xkme.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Interim Infection Control Guidance for Public Health Personnel Evaluating Persons Under Investigation (PUIs) and Asymptomatic Close Contacts of Confirmed Cases at Their Home or Non-Home Residential Settings. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/php/guidance-evaluating-pui.html April 2020. Available from.
- 15.Ikizler T.A., Kliger A.S. Minimizing the risk of COVID-19 among patients on dialysis. Nat Rev Nephrol. 2020;16(6):311–313. doi: 10.1038/s41581-020-0280-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.In-Center Dialysis and Coronavirus (COVID-19): Protecting Your Health. Fresenius Kidney Care. 2020. https://www.freseniuskidneycare.com/thrive-central/in-center-dialysis-and-coronavirus Available from. [accessed 5.20.2020]
- 17.Ikizler T.A. COVID-19 and Dialysis units: what do we know now and what should we do? Am J Kidney Dis. 2020;76(1):1–3. doi: 10.1053/j.ajkd.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akbarialiabad H., Kavousi S., Ghahramani A., Bastani B., Ghahramani N. COVID-19 and maintenance hemodialysis: a systematic scoping review of practice guidelines. BMC Nephrol. 2020;21(1):470. doi: 10.1186/s12882-020-02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meijers B., Messa P., Ronco C. Safeguarding the maintenance hemodialysis patient population during the coronavirus disease 19 pandemic. Blood Purif. 2020;49(3):259–264. doi: 10.1159/000507537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rombolà G., Heidempergher M., Pedrini L. Practical indications for the prevention and management of SARS-CoV-2 in ambulatory dialysis patients: lessons from the first phase of the epidemics in Lombardy. J Nephrol. 2020;33(2):193–196. doi: 10.1007/s40620-020-00727-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li J., Li S.X., Zhao L.F., Kong D.L., Guo Z.Y. Management recommendations for patients with chronic kidney disease during the novel coronavirus disease 2019 (COVID-19) epidemic. Chronic Dis Transl Med. 2020;6(2):119–123. doi: 10.1016/j.cdtm.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li J., Xu G. Lessons from the experience in Wuhan to reduce risk of COVID-19 infection in patients undergoing long-term hemodialysis. Clin J Am Soc Nephrol. 2020;15(5):717–719. doi: 10.2215/CJN.03420320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen G., Hu R., Wang Y. Recommendation from Peking union medical college hospital for urgent hemodialysis during the COVID-19 pandemic. Int Urol Nephrol. 2020;52(9):1809–1810. doi: 10.1007/s11255-020-02532-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.COVID-19 & Dialysis. American College of Emergency Physicians. 2020. www.acep.org/corona/COVID-19-alert/covid-19-articles/covid-19--dialysis/ Available from. [accessed 5.20.2020]
- 25.“Infection Control: Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2).” Centers for Disease Control and Prevention. 2020. www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Finfection-control%2Fcontrol-recommendations.html Available from. [accessed 4.12.2020]
- 26.Joint Statement from ASN and ACEP on Appropriate Use of Emergency Departments during the COVID-19 Pandemic | Kidney News, American College of Emergency Physicians & American Society of Nephrologists. 2020. https://www.kidneynews.org/policy-advocacy/leading-edge/joint-statement-from-asn-and-acep-on-appropriate-use-of-emergency-departments-during-the-covid-19 Available from. [accessed 5.29.2020]
- 27.PRIEST Study | ScHARR | The University of Sheffield. Published October 22, 2020. https://www.sheffield.ac.uk/scharr/research/centres/cure/priest Available from:
- 28.NEWS (or NEWS2) Score When Assessing Possible COVID-19 Patients in Primary Care? The Centre for Evidence-Based Medicine. 2020. https://www.cebm.net/covid-19/should-we-use-the-news-or-news2-score-when-assessing-patients-with-possible-covid-19-in-primary-care/ Available from. [accessed on 11.12.2020]
- 29.The PRIEST COVID-19 Clinical Severity Score | ScHARR | The University of Sheffield. Published October 22, 2020. https://www.sheffield.ac.uk/scharr/research/centres/cure/priest/priest-covid-19 Available from.
- 30.Haimovich A.D., Ravindra N.G., Stoytchev S. Development and validation of the quick COVID-19 severity index: a prognostic tool for early clinical decompensation. Ann Emerg Med. 2020;76(4):442–453. doi: 10.1016/j.annemergmed.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reisinger N., Koratala A. Lung ultrasound: a valuable tool for the assessment of dialysis patients with COVID-19. Clin Exp Nephrol. 2020;24(9):850–852. doi: 10.1007/s10157-020-01903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.“Symptoms of Coronavirus.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention. 2020. www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html Available from. [accessed 5.12.2020]
- 33.Overview of Testing for SARS-Cov-2 (COVID-19). Centers for Disease Control. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html Available from. [accessed 8.27.2020]
- 34.Discontinuation of Transmission-Based Precautions and Disposition of Patients with COVID-19 in Healthcare Settings (Interim Guidance). Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html Available from. [accessed 8.27.2020]
- 35.Kliger A.S., Cozzolino M., Jha V., Harbert G., Ikizler T.A. Managing the COVID-19 pandemic: international comparisons in dialysis patients. Kidney Int. 2020;98(1):12–16. doi: 10.1016/j.kint.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]