Falls are the leading cause of injury among adults aged ≥65 years (older adults) in the United States. In 2018, an estimated 3 million emergency department visits, more than 950,000 hospitalizations or transfers to another facility (e.g., trauma center), and approximately 32,000 deaths resulted from fall-related injuries among older adults.* Deaths from falls are increasing, with the largest increases occurring among persons aged ≥85 years (1). To describe the percentages and rates of nonfatal falls by age group and demographic characteristics and trends in falls and fall-related injuries over time, data were analyzed from the 2018 Behavioral Risk Factor Surveillance System (BRFSS) and were compared with data from 2012, 2014, and 2016. In 2018, 27.5% of older adults reported falling at least once in the past year, and 10.2% reported an injury from a fall in the past year. The percentages of older adults reporting a fall increased between 2012 and 2016 and decreased slightly between 2016 and 2018. Falls are preventable, and health care providers can help their older patients reduce their risk for falls. Screening older patients for fall risk, assessing modifiable risk factors (e.g., use of psychoactive medications or poor gait and balance), and recommending interventions to reduce this risk (e.g., medication management or referral to physical therapy) can prevent older adult falls (https://www.cdc.gov/steadi).
BRFSS is a landline and mobile telephone survey conducted annually in all 50 U.S. states, the District of Columbia (DC), and U.S. territories, with a median response rate of 49.9% in 2018. The survey collects information on health-related behavioral risk factors and chronic conditions among noninstitutionalized U.S. adults aged ≥18 years.† Information on falls and fall-related injuries is recorded every 2 years from adults aged ≥45 years by asking “In the past 12 months, how many times have you fallen?” If the response was one or more times, the respondent was asked “How many of these falls caused an injury? By an injury, we mean the fall caused you to limit your regular activities for at least a day or to go see a doctor.” Responses to each of these questions ranged from 0 to 76 falls or fall-related injuries. Rates were calculated as the average number of falls and fall-related injuries per 1,000 older adults. Both questions were dichotomized to calculate the percentage of older adults who reported having at least one fall or fall-related injury.
Using 2018 BRFSS data, percentages and rates were calculated by age group for demographic (sex and race/ethnicity) and geographic (urban/rural status) characteristics. Functional characteristics (blind/difficulty seeing, difficulty dressing/bathing, difficulty walking/climbing stairs, difficulty doing errands alone, and difficulty concentrating/making decisions) also were compared, as were self-reported health status and data on taking part in any physical activity/exercise in the past month. Analysis was restricted to respondents aged ≥65 years residing in the 50 states and DC. Any respondents with missing values or responses of “Don’t know/Not sure” or “Refused” for falls or fall-related injuries were excluded. Overall, 4.8% of respondents were excluded from the analysis of falls, leaving 142,834; and 4.9% were excluded from the analysis of fall-related injuries, leaving 142,591. Two-sample t-tests were used to compare percentages across characteristics. Linear trend tests were conducted for age group and self-reported health status. BRFSS data from 2012, 2014, 2016, and 2018 were used to examine trends in the percentages of adults aged ≥65 years who had fallen or had a fall-related injury and rates of falls overall and by age group. Polynomial linear regression was used to assess linearity of trends (2). Where nonlinear trends were detected, two-sample t-tests with Bonferroni adjustments for multiple comparisons were performed to determine differences between years (2). Because the BRFSS questions about falls differed in three states (Michigan, Oregon, and Wisconsin) for 2012, compared with other years, the trend analysis was limited to 47 states and DC. All results presented are weighted to represent the U.S. population. Analysis was conducted using SAS-callable SUDAAN (version 11; RTI International) to account for the complex survey design.
In 2018, 27.5% of adults aged ≥65 years reported at least one fall in the past year (Table 1), and 10.2 % of adults aged ≥65 years reported at least one fall-related injury (Table 2). In the preceding year, an average of 714 falls (Table 1) and an average of 170 fall-related injuries were reported per 1,000 older adults (Table 2), or approximately 35.6 million falls and 8.4 million fall-related injuries. The percentage of adults aged ≥65 years reporting a fall or a fall-related injury increased with age (p<0.001). Among adults aged ≥85 years, 33.8% reported a fall (Table 1) and 13.9% reported a fall-related injury (Table 2). Overall, a higher percentage of women reported at least one fall (29.1%; p<0.001) or fall-related injury (11.9%; p<0.001) than did men in the past year (25.5% reported a fall and 7.9% reported a fall-related injury). However, when stratified by age group, the percentages of adults aged ≥85 years reporting a fall (32.8% of women and 35.7% of men; p = 0.184) or fall-related injury (14.3% of women and 13.4% of men; p = 0.553) did not differ significantly by sex. A lower percentage of blacks (22.5%; p<0.001) and Asian/Pacific Islanders (15.6%; p<0.001) reported a fall than did whites (28.3%) (Table 1), and a higher percentage of American Indian/Alaska Natives (15.2%) reported a fall-related injury than did whites (10.2%; p = 0.008) (Table 2). The percentages of older adults reporting a fall decreased as health status improved (p<0.001) (Table 1). Overall, a higher percentage of older adults living in rural areas (29.5%) reported a fall compared with those living in urban areas (27.0%; p<0.001); however, when stratified by age group, this was only true for persons aged 65–74 years (Table 1). Regardless of age group, older adults reporting difficulties with functional abilities reported a higher percentage of falls and fall-related injuries than did those without these difficulties (p<0.001). A lower percentage of older adults who reported any physical activity in the past month reported a fall (24.9%) compared with those who did not report physical activity (33.1%; p<0.001), regardless of age group.
TABLE 1. Number of falls, percentages of adults reporting a fall, and rates* of self-reported falls in the past year among adults aged ≥65 years, by age group and selected characteristics (unweighted n = 142,834) — Behavioral Risk Factor Surveillance System, United States, 2018.
| Age group/Characteristic | No.† reporting a fall | % (95% CI)§ | Rate* of falls (95% CI) |
|---|---|---|---|
|
Total (all aged ≥65 years)
| |||
|
Overall
|
13,685,662
|
27.5 (26.9–28.0)
|
714 (689–739)
|
|
Sex
| |||
| Male |
5,629,838 |
25.5 (24.6–26.3) |
735 (694–775) |
| Female |
8,026,432 |
29.1 (28.3–29.8) |
695 (664–727) |
|
Race/Ethnicity
¶
| |||
| White |
10,898,569 |
28.3 (27.8–28.9) |
738 (710–765) |
| Black |
4,260,153 |
22.5 (20.4–24.7) |
526 (455–597) |
| American Indian/Alaska Native |
325,910 |
32.2 (27.3–37.5) |
1,169 (845–1494) |
| Asian/Pacific Islander |
237,985 |
15.6 (10.9–21.8) |
250 (167–334) |
| Hispanic |
1,039,618 |
28.1 (24.7–31.7) |
677 (555–799) |
| Multiple/Other |
193,208 |
29.6 (26.3–33.2) |
1,333 (859–1,807) |
|
Geography
| |||
| Urban |
11,024,283 |
27.0 (26.4–27.7) |
682 (653–710) |
| Rural |
2,661,031 |
29.5 (28.5–30.4) |
858 (805–910) |
|
Self-reported health
| |||
| Excellent |
974,558 |
16.4 (15.0–18.0) |
288 (254–323) |
| Very good |
3,201,506 |
21.9 (21.1–22.8) |
420 (393–446) |
| Good |
4,423,458 |
26.6 (25.6–27.7) |
615 (573–657) |
| Fair |
3,246,406 |
36.8 (35.2–38.3) |
1,102 (1,030–1,173) |
| Poor |
1,789,371 |
48.1 (45.8–50.5) |
2,057 (1,872–2,242) |
|
Functional characteristics
| |||
| Blind/Difficulty seeing | |||
| Yes |
1,611,580 |
42.1 (39.5–44.9) |
1,500 (1,343–1,658) |
| No |
12,013,980 |
26.2 (25.6–26.8) |
646 (622–670) |
| Difficulty concentrating | |||
| Yes |
2,398,304 |
48.5 (46.1–50.9) |
1,798 (1,660–1,936) |
| No |
11,133,899 |
25.0 (24.5–25.6) |
584 (562–607) |
| Difficulty walking/climbing stairs | |||
| Yes |
6,218,999 |
46.3 (45.0–47.6) |
1,562 (1,488–1,637) |
| No |
7,386,736 |
20.4 (19.9–21.0) |
397 (377–418) |
| Difficulty performing errands alone | |||
| Yes |
2,578,010 |
53.0 (50.6–55.3) |
1,994 (1,845–2,142) |
| No |
11,017,965 |
24.6 (24.1–25.2) |
573 (550–595) |
| Difficulty dressing/bathing | |||
| Yes |
1,584,599 |
58.7 (55.6–61.7) |
2,496 (2,258–2,735) |
| No |
12,068,592 |
25.6 (25.1–26.2) |
610 (588–633) |
| Any physical activity in past month | |||
| Yes |
8,431,996 |
24.9 (24.2–25.5) |
583 (555–612) |
| No |
5,227,220 |
33.1 (32.0–34.2) |
989 (938–1,040) |
|
65–74 years
| |||
|
Overall
|
7,619,118
|
25.9 (25.2–26.6)
|
700 (668–733)
|
|
Sex
| |||
| Male |
3,224,096 |
23.3 (22.2–24.4) |
702 (654–750) |
| Female |
4,378,780 |
28.2 (27.2–29.2) |
698 (654–741) |
|
Race/Ethnicity
¶
| |||
| White |
5,832,525 |
26.3 (25.6–27.0) |
721 (685–758) |
| Black |
588,611 |
21.7 (19.4–24.1) |
537 (437–638) |
| American Indian/Alaska Native |
72,207 |
33.9 (27.7–40.7) |
1,323 (856–1,790) |
| Asian/Pacific Islander |
182,037 |
17.8 (11.6–26.4) |
269 (160–378) |
| Hispanic |
685,669 |
28.5 (24.2–33.3) |
660 (544–776) |
| Multiple/Other |
112,714 |
28.2 (24.2–32.4) |
1,273 (766–1,781) |
|
Geography
| |||
| Urban |
6,107,062 |
25.4 (24.5–26.2) |
663 (627–698) |
| Rural |
1,511,825 |
28.2 (27.0–29.5) |
871 (798–944) |
|
Self-reported health
| |||
| Excellent |
572,626 |
15.2 (13.3–17.2) |
260 (228–292) |
| Very good |
1,831,360 |
20.3 (19.3–21.4) |
391 (361–421) |
| Good |
2,357,029 |
24.7 (23.4–26.0) |
589 (532–647) |
| Fair |
1,893,376 |
37.3 (35.2–39.4) |
1,180 (1,080–1,280) |
| Poor |
941,100 |
47.9 (45.1–50.8) |
2,255 (2,012–2,499) |
|
Functional characteristics
| |||
| Blind/Difficulty seeing | |||
| Yes |
828,168 |
42.7 (38.7–46.8) |
1,548 (1,341–1,754) |
| No |
6,758,376 |
24.6 (23.9–25.4) |
638 (607–670) |
| Difficulty concentrating | |||
| Yes |
1,362,936 |
50.9 (47.6–54.1) |
1,944 (1,773–2,115) |
| No |
6,175,049 |
23.2 (22.6–23.9) |
566 (536–597) |
| Difficulty walking/climbing stairs | |||
| Yes |
3,189,778 |
47.3 (45.4–49.1) |
1,735 (1,626–1,844) |
| No |
4,388,844 |
19.4 (18.8–20.1) |
389 (364–415) |
| Difficulty performing errands alone | |||
| Yes |
1,258,886 |
56.5 (52.9–60.0) |
2,366 (2,127–2,604) |
| No |
6,313,271 |
23.3 (22.6–24.0) |
561 (532–590) |
| Difficulty dressing/bathing | |||
| Yes |
855,277 |
59.6 (55.3–63.8) |
2,689 (2,365–3,014) |
| No |
6,749,735 |
24.1 (23.4–24.8) |
598 (568–627) |
| Any physical activity in past month | |||
| Yes |
4,900,264 |
23.3 (22.5–24.0) |
574 (538–610) |
| No |
2,707,832 |
32.5 (30.8–34.1) |
1,013 (946–1,079) |
|
75–84 years
| |||
|
Overall
|
4,424,372
|
28.5 (27.5–29.5)
|
707 (664–750)
|
|
Sex
| |||
| Male |
1,744,922 |
27.3 (25.6–28.9) |
748 (670–826) |
| Female |
2,671,039 |
29.4 (28.1–30.8) |
679 (631–728) |
|
Race/Ethnicity
¶
| |||
| White |
3,660,879 |
29.8 (28.7–30.8) |
742 (694–790) |
| Black |
289,006 |
23.4 (18.7–28.8) |
488 (397–579) |
| American Indian/Alaska Native |
24,161 |
29.2 (22.0–37.7) |
1,022 (657–1,386) |
| Asian/Pacific Islander |
45,914 |
—** |
— |
| Hispanic |
267,023 |
24.8 (19.7–30.6) |
498 (377–619) |
| Multiple/Other |
62,832 |
31.1 (24.8–38.2) |
— |
|
Geography
| |||
| Urban |
3,573,520 |
28.2 (27.0–29.4) |
683 (634–732) |
| Rural |
850,758 |
29.9 (28.3–31.6) |
816 (731–901) |
|
Self-reported health
| |||
| Excellent |
305,524 |
17.9 (15.5–20.7) |
328 (234–422) |
| Very good |
1,031,504 |
23.5 (21.9–25.2) |
443 (385–502) |
| Good |
1,528,297 |
28.8 (26.9–30.8) |
625 (569–682) |
| Fair |
959,740 |
34.5 (32.0–37.0) |
1,017 (892–1,143) |
| Poor |
579,025 |
44.9 (40.5–49.3) |
1,756 (1,454–2,058) |
|
Functional characteristics
| |||
| Blind/Difficulty seeing | |||
| Yes |
482,311 |
39.8 (35.9–43.8) |
1,461 (1,189–1,732) |
| No |
3,929,486 |
27.6 (26.5–28.6) |
643 (602–683) |
| Difficulty concentrating | |||
| Yes |
681,990 |
44.3 (40.8–47.8) |
1,672 (1,417–1,927) |
| No |
3,705,749 |
26.7 (25.6–27.8) |
599 (560–638) |
| Difficulty walking/climbing stairs | |||
| Yes |
2,134,694 |
45.1 (42.9–47.4) |
1,435 (1,314–1,556) |
| No |
2,264,615 |
21.1 (20.1–22.2) |
385 (353–416) |
| Difficulty performing errands alone | |||
| Yes |
814,654 |
50.3 (46.4–54.2) |
1,906 (1,642–2,169) |
| No |
3,590,020 |
25.9 (24.9–26.9) |
566 (529–603) |
| Difficulty dressing/bathing | |||
| Yes |
486,255 |
58.0 (52.6–63.3) |
2,423 (2,018–2,828) |
| No |
3,927,919 |
26.8 (25.8–27.8) |
608 (569–647) |
| Any physical activity in past month | |||
| Yes |
2,667,197 |
26.3 (25.0–27.6) |
571 (525–617) |
| No |
1,746,501 |
32.7 (31.0–34.5) |
963 (874–1,052) |
|
≥85 years
| |||
|
Overall
|
1,642,172
|
33.8 (31.8–35.9)
|
816 (719–913)
|
|
Sex
| |||
| Male |
660,820 |
35.7 (32.3–39.2) |
931 (755–1,107) |
| Female |
976,613 |
32.8 (30.3–35.4) |
733 (621–846) |
|
Race/Ethnicity
¶
| |||
| White |
1,405,165 |
35.3 (33.2–37.5) |
817 (737–897) |
| Black |
79,686 |
26.0 (20.3–32.6) |
580 (393–766) |
| American Indian/Alaska Native |
8,547 |
— |
— |
| Asian/Pacific Islander |
10,034 |
— |
— |
| Hispanic |
86,926 |
39.8 (26.6–54.7) |
— |
| Multiple/Other |
17,663 |
35.0 (22.3–50.2) |
789 (439–1,139) |
|
Geography
| |||
| Urban |
1,343,701 |
33.4 (31.1–35.8) |
795 (682–908) |
| Rural |
298,448 |
35.7 (31.8–39.9) |
916 (773–1,059) |
|
Self-reported health
| |||
| Excellent |
96,407 |
21.6 (17.1–26.9) |
373 (288–459) |
| Very good |
338,642 |
28.0 (24.6–31.6) |
544 (462–625) |
| Good |
538,133 |
30.9 (27.7–34.3) |
726 (549–902) |
| Fair |
393,290 |
40.5 (35.5–45.7) |
934 (791–1,078) |
| Poor |
269,246 |
58.1 (51.6–64.4) |
2,051 (1,418–2,685) |
|
Functional characteristics
| |||
| Blind/Difficulty seeing | |||
| Yes |
301,101 |
44.7 (37.8–51.8) |
1,435 (974–1,897) |
| No |
1,326,118 |
31.9 (29.8–34.1) |
714 (628–800) |
| Difficulty concentrating | |||
| Yes |
353,378 |
48.9 (41.0–56.8) |
1,527 (1,091–1,962) |
| No |
1,253,102 |
30.9 (29.0–32.8) |
654 (601–707) |
| Difficulty walking/climbing stairs | |||
| Yes |
894,527 |
45.8 (42.4–49.2) |
1,275 (1,094–1,457) |
| No |
733,277 |
25.8 (23.2–28.5) |
506 (395–617) |
| Difficulty performing errands alone | |||
| Yes |
504,470 |
49.5 (44.9–54.2) |
1,319 (1,073–1,565) |
| No |
1,114,674 |
29.4 (27.3–31.7) |
679 (575–783) |
| Difficulty dressing/bathing | |||
| Yes |
243,067 |
56.9 (49.4–64.1) |
1,991 (1,314–2,668) |
| No |
1,390,938 |
31.5 (29.4–33.7) |
701 (617–784) |
| Any physical activity in past month | |||
| Yes |
864,536 |
31.9 (29.2–34.7) |
704 (584–824) |
| No | 772,887 | 36.4 (33.4–39.5) | 960 (800–1,119) |
Abbreviation: CI = confidence interval.
* Weighted number of falls per 1,000 adults aged ≥65 years.
† Weighted number of adults aged ≥65 years reporting at least one fall in the past year. Because of varying question-specific nonresponse, sample sizes might vary among questions.
§ Weighted percentage of adults aged ≥65 years reporting at least one fall in the past year.
¶ Whites, blacks, American Indians/Alaska Natives, Asians/Pacific Islanders, and others/unknown were non-Hispanic; Hispanics could be of any race.
** Dashes indicate sample size <50 or relative standard error >30%.
TABLE 2. Number of fall-related injuries, percentage of adults reporting a fall-related injury, and rates* of self-reported fall-related injuries in the past year among adults ≥65 years by age group and select characteristics (unweighted n = 142,591) — Behavioral Risk Factor Surveillance System, United States, 2018.
| Age group/Characteristic | No.† reporting a fall-related injury | % of fall-related injuries§ (95% CI) | Rate* of fall-related injuries (95% CI) |
|---|---|---|---|
|
Total (all aged ≥65 years)
| |||
|
Overall
|
5,051,046
|
10.2 (9.8–10.6)
|
170 (160–179)
|
|
Sex
| |||
| Male |
1,753,182 |
7.9 (7.4–8.6) |
140 (125–155) |
| Female |
3,285,921 |
11.9 (11.4–12.5) |
193 (181–204) |
|
Race/Ethnicity
¶
| |||
| White |
3,927,593 |
10.2 (9.9–10.6) |
170 (161–178) |
| Black |
373,817 |
8.8 (7.1–10.8) |
122 (99–144) |
| American Indian/Alaska Native |
49,235 |
15.2 (11.4–19.9) |
360 (183–536) |
| Asian/Pacific Islander |
107,711 |
—** |
90 (39–142) |
| Hispanic |
422,695 |
11.5 (9.2–14.1) |
192 (132–251) |
| Multiple/Other |
73,334 |
11.3 (9.2–13.7) |
— |
|
Geography
| |||
| Urban |
4,112,951 |
10.1 (9.6–10.6) |
167 (157–178) |
| Rural |
937,957 |
10.4 (9.8–11.1) |
180 (161–199) |
|
Self-reported health
| |||
| Excellent |
322,006 |
5.4 (4.3–6.9) |
65 (51–79) |
| Very good |
972,529 |
6.7 (6.1–7.3) |
81 (74–89) |
| Good |
1,518,761 |
9.2 (8.5–9.8) |
133 (122–145) |
| Fair |
1,294,112 |
14.7 (13.6–15.9) |
263 (238–289) |
| Poor |
917,291 |
24.9 (23.0–26.9) |
624 (535–713) |
|
Functional characteristics
| |||
| Blind/Difficulty seeing | |||
| Yes |
742,101 |
19.6 (17.4–21.9) |
436 (354–519) |
| No |
4,281,945 |
9.4 (9.0–9.8) |
147 (140–155) |
| Difficulty concentrating | |||
| Yes |
1,104,754 |
22.5 (20.6–24.6) |
489 (425–552) |
| No |
3,888,940 |
8.7 (8.4–9.1) |
133 (125–141) |
| Difficulty walking/climbing stairs | |||
| Yes |
2,704,665 |
20.3 (19.2–21.3) |
407 (376–438) |
| No |
2,315,536 |
6.4 (6.0–6.8) |
82 (76–88) |
| Difficulty performing errands alone | |||
| Yes |
1,318,985 |
27.3 (25.1–29.7) |
587 (524–651) |
| No |
3,693,519 |
8.3 (7.9–8.6) |
124 (116–132) |
| Difficulty dressing/bathing | |||
| Yes |
833,239 |
31.2 (28.3–34.4) |
724 (619–829) |
| No |
4,198,368 |
8.9 (8.6–9.3) |
138 (130–145) |
| Any physical activity in past month | |||
| Yes |
2,918,250 |
8.6 (8.1–9.1) |
131 (121–140) |
| No |
2,120,902 |
13.5 (12.7–14.3) |
253 (232–274) |
|
65–74 years
| |||
|
Overall
|
2,743,633
|
9.3 (8.8–9.9)
|
160 (148–171)
|
|
Sex
| |||
| Male |
958,537 |
6.9 (6.3–7.6) |
123 (108–138) |
| Female |
1,775,596 |
11.4 (10.7–12.2) |
191 (175–208) |
|
Race/Ethnicity
| |||
| White |
1,999,023 |
9.0 (8.6–9.5) |
155 (144–166) |
| Black |
226,321 |
8.4 (6.9–10.2) |
126 (100–153) |
| American Indian/Alaska Native |
35,860 |
16.9 (11.9–23.9) |
452 (191–714) |
| Asian/Pacific Islander |
95,225 |
— |
— |
| Hispanic |
299,340 |
12.5 (9.5–16.3) |
180 (136–224) |
| Multiple/Other |
42,830 |
10.7 (8.6–13.3) |
— |
|
Geography
| |||
| Urban |
511,500 |
9.3 (8.7–9.9) |
160 (146–173) |
| Rural |
2,232,054 |
9.6 (8.8–10.4) |
161 (146–176) |
|
Self-reported health
| |||
| Excellent |
173,443 |
4.6 (3.1–6.8) |
54 (35–73) |
| Very good |
571,453 |
6.3 (5.6–7.1) |
79 (69–89) |
| Good |
744,975 |
7.8 (7.2–8.5) |
116 (103–128) |
| Fair |
765,642 |
15.1 (13.5–17.0) |
276 (238–314) |
| Poor |
477,503 |
24.5 (22.3–26.9) |
649 (540–758) |
|
Functional characteristics
| |||
|
Blind/Difficulty seeing
| |||
| Yes |
402,881 |
21.0 (17.5–24.9) |
486 (366–605) |
| No |
2,326,598 |
8.5 (8.0–9.0) |
136 (128–145) |
| Difficulty concentrating | |||
| Yes |
642,512 |
24.2 (21.4–27.3) |
529 (454–604) |
| No |
2,064,220 |
7.8 (7.3–8.3) |
121 (111–130) |
| Difficulty walking/climbing stairs | |||
| Yes |
1,408,428 |
21.0 (19.6–22.5) |
452 (407–496) |
| No |
1,324,451 |
5.9 (5.4–6.4) |
73 (67–80) |
| Difficulty performing errands alone | |||
| Yes |
650,112 |
29.4 (26.0–33.0) |
717 (600–834) |
| No |
2,072,807 |
7.6 (7.2–8.1) |
114 (106–121) |
| Difficulty dressing/bathing | |||
| Yes |
454,702 |
32.0 (28.4–35.9) |
766 (633–899) |
| No |
2,280,876 |
8.2 (7.7–8.7) |
128 (118–138) |
| Any physical activity in past month | |||
| Yes |
1,620,337 |
7.7 (7.2–8.3) |
121 (108–133) |
| No |
1,118,474 |
13.4 (12.3–14.7) |
258 (234–282) |
|
75–84 years
| |||
|
Overall
|
1,634,953
|
10.6 (9.8–11.3)
|
170 (156–185)
|
|
Sex
| |||
| Male |
547,968 |
8.6 (7.4–9.9) |
141 (118–164) |
| Female |
1,085,428 |
12.0 (11.1–12.9) |
192 (173–210) |
|
Race/Ethnicity
| |||
| White |
1,355,522 |
11.0 (10.3–11.8) |
179 (164–195) |
| Black |
115,601 |
9.3 (5.4–15.7) |
112 (61–162) |
| American Indian/Alaska Native |
7,702 |
9.4 (5.6–15.4) |
179 (78–280) |
| Asian/Pacific Islander |
9,402 |
— |
— |
| Hispanic |
90,085 |
8.4 (5.9–11.8) |
135 (82–187) |
| Multiple/Other |
21,322 |
10.6 (7.5–14.8) |
173 (99–246) |
|
Geography
| |||
| Urban |
1,338,288 |
10.6 (9.7–11.5) |
167 (151–183) |
| Rural |
296,606 |
10.4 (9.5–11.5) |
185 (149–222) |
|
Self-reported health
| |||
| Excellent |
112,211 |
6.6 (4.8–8.9) |
80 (56–103) |
| Very good |
301,804 |
6.9 (5.9–8.0) |
82 (69–94) |
| Good |
538,594 |
10.2 (8.7–11.8) |
139 (120–157) |
| Fair |
382,369 |
13.8 (12.3–15.4) |
260 (220–300) |
| Poor |
286,516 |
22.3 (19.2–25.7) |
527 (408–647) |
|
Functional characteristics
| |||
| Blind/Difficulty seeing | |||
| Yes |
190,201 |
15.8 (13.4–18.5) |
338 (258–419) |
| No |
1,440,008 |
10.1 (9.4–10.9) |
156 (142–170) |
| Difficulty concentrating | |||
| Yes |
294,225 |
19.2 (16.6–22.2) |
398 (324–472) |
| No |
1,326,930 |
9.6 (8.8–10.4) |
145 (131–159) |
| Difficulty walking/Climbing stairs | |||
| Yes |
889,083 |
18.9 (17.1–20.8) |
360 (320–401) |
| No |
731,862 |
6.8 (6.2–7.5) |
86 (76–96) |
| Difficulty performing errands alone | |||
| Yes |
404,429 |
25.2 (21.3–29.4) |
511 (432–591) |
| No |
1,222,743 |
8.8 (8.2–9.5) |
130 (118–143) |
| Difficulty dressing/Bathing | |||
| Yes |
248,895 |
30.1 (24.0–37.0) |
636 (524–749) |
| No |
1,379,549 |
9.4 (8.8–10.1) |
144 (130–157) |
| Any physical activity in past month | |||
| Yes |
964,611 |
9.5 (8.6–10.5) |
141 (125–157) |
| No |
665,922 |
12.5 (11.4–13.7) |
226 (198–254) |
|
≥85 years
| |||
|
Overall
|
672,460
|
13.9 (12.5–15.4)
|
227 (179–276)
|
|
Sex
| |||
| Male |
246,677 |
13.4 (11.0–16.2) |
265 (148–382) |
| Female |
424,896 |
14.3 (12.7–16.1) |
205 (175–236) |
|
Race/Ethnicity
| |||
| White |
573,048 |
14.5 (13.0–16.1) |
222 (186–257) |
| Black |
31,894 |
10.5 (7.1–15.2) |
119 (74–164) |
| American Indian/Alaska Native |
5,673 |
— |
— |
| Asian/Pacific Islander |
3,084 |
— |
— |
| Hispanic |
33,270 |
— |
— |
| Multiple/Other |
9,182 |
— |
— |
|
Geography
| |||
| Urban |
542,610 |
13.6 (12.1–15.2) |
216 (163–268) |
| Rural |
129,850 |
15.6 (12.1–19.8) |
283 (155–410) |
|
Self-reported health
| |||
| Excellent |
36,352 |
8.2 (5.3–12.3) |
96 (59–133) |
| Very good |
99,273 |
8.2 (6.5–10.4) |
100 (77–123) |
| Good |
235,192 |
13.6 (11.4–16.1) |
216 (150–282) |
| Fair |
146,101 |
15.1 (12.5–18.2) |
203 (165–241) |
| Poor |
153,272 |
33.4 (26.5–41.1) |
788 (367–1210) |
|
Functional characteristics
| |||
| Blind/Difficulty seeing | |||
| Yes |
149,020 |
22.4 (17.6–28.0) |
— |
| No |
515,339 |
12.5 (11.1–14.0) |
187 (154–221) |
| Difficulty concentrating | |||
| Yes |
168,017 |
23.4 (17.8–30.2) |
532 (234–831) |
| No |
497,790 |
12.3 (11.1–13.7) |
174 (150–198) |
| Difficulty walking/climbing stairs | |||
| Yes |
407,155 |
21.0 (18.5–23.7) |
366 (261–470) |
| No |
259,223 |
9.1 (7.6–10.9) |
133 (91–174) |
| Difficulty performing errands alone | |||
| Yes |
264,445 |
26.2 (22.1–30.7) |
424 (311–536) |
| No |
397,969 |
10.5 (9.3–11.9) |
174 (120–227) |
| Difficulty dressing/bathing | |||
| Yes |
129,643 |
30.9 (24.5–38.2) |
— |
| No |
537,943 |
12.2 (10.9–13.7) |
176 (144–207) |
| Any physical activity in past month | |||
| Yes |
333,302 |
12.3 (10.5–14.4) |
171 (142–201) |
| No | 336,507 | 15.9 (13.8–18.3) | 298 (194–403) |
Abbreviation: CI = confidence interval.
* Weighted number of fall-related injuries per 1,000 older adults.
† Weighted number of adults aged ≥65 years reporting at least one fall-related injury in the past year. Because of varying question-specific nonresponse, sample sizes might vary among questions.
§ Weighted percentage of older adults reporting at least one fall-related injury in the past year.
¶ Whites, blacks, American Indians/Alaska Natives, Asians/Pacific Islanders, and others/unknown were non-Hispanic; Hispanics could be of any race.
** Dashes indicate sample size <50 or relative standard error >30%.
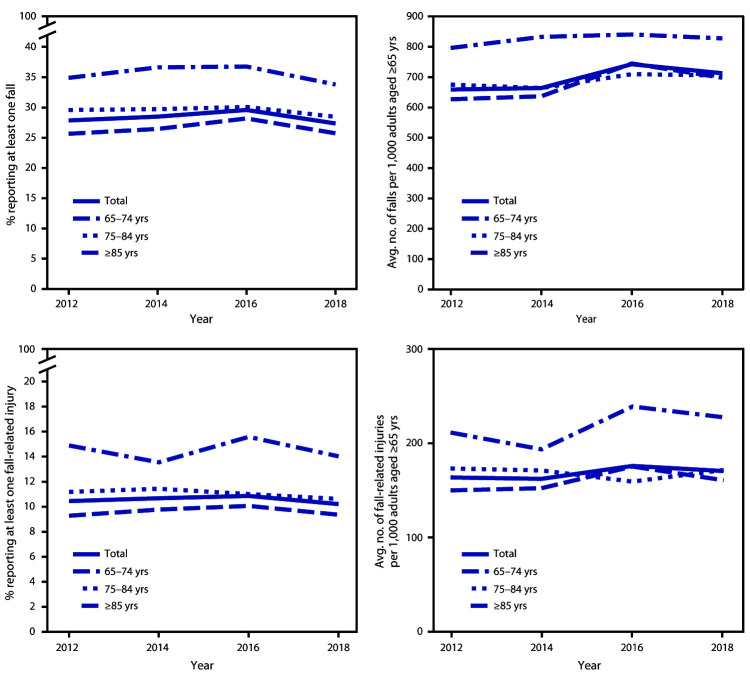
Among states in which falls and fall injuries were consistently reported across years (excluding Michigan, Oregon, and Wisconsin where data in 2012 were reported differently than in other years), the percentage of those older adults reporting a fall increased from 27.9% in 2012 to 29.6% in 2016 (p<0.001) and decreased to 27.4% in 2018 (p<0.001) (Figure). The rates of falls and fall-related injuries and the percentages of older adults reporting a fall-related injury did not significantly change from 2012 to 2018.
FIGURE.
Percentages and rates of self-reported falls and fall-related injuries among adults aged ≥65 years, by age group — Behavioral Risk Factor Surveillance System, United States,* 2012–2018
* Data from Michigan, Oregon, and Wisconsin were omitted because of the difference in the way these states collected information about falls during 2012, compared with the rest of the states.
Discussion
The percentage of older adults reporting a fall increased from 2012 to 2016, followed by a modest decline from 2016 to 2018. Although statistically significant, these changes were small. Even with this decrease in 2018, older adults reported 35.6 million falls. Among those falls, 8.4 million resulted in an injury that limited regular activities for at least a day or resulted in a medical visit. In the United States, health care spending on older adult falls has been approximately $50 billion annually (3). In 2018, approximately 52 million adults were aged ≥65 years§ by 2030, this number will increase to approximately 73 million.¶ Despite no significant changes in the rate of fall-related injuries from 2012 to 2018, the number of fall-related injuries and health care costs can be expected to increase as the proportion of older adults in the United States grows.
Adults aged ≥85 years were more likely to report a fall or fall-related injury in the preceding year than were those aged <85 years. Currently, adults aged ≥85 years account for <2% of the population; by 2050 this proportion is projected to increase to 5%. Many fall risk factors increase with age, including chronic health conditions related to falls, increased use of medications, and functional decline (4). More research is needed to determine how fall risk factors differ among persons aged ≥85 years and to identify targeted interventions that could adequately address the needs of these adults.
The findings in this report are subject to at least five limitations. First, because BRFSS data are self-reported, they are subject to recall bias, especially for falls that did not result in injury or that occurred several months before the survey (5). Second, this survey is cross-sectional. Although functional abilities, health status, and physical activity were all associated with falls and fall-related injuries, it is not possible to determine whether these factors preceded the fall or resulted from a fall. Third, BRFSS does not include older adults living in nursing homes, which might have led to an underestimation of falls and fall-related injuries, especially among adults aged ≥85 years (6). Fourth, the response rate (median response rate of 49.9%) could result in non-response bias, however BRFSS data are weighted to adjust for some of this bias. Finally, the results of the trend analyses were derived from only four time points. Future analyses with more time points might describe these trends with more certainty.
Regardless of age group, higher percentages of older adults who reported no physical activity in the past month or reported difficulty with one or more functional characteristics (difficulty walking up or down stairs, dressing and bathing, and performing errands alone) reported falls and fall-related injuries. These risk factors are frequently modifiable suggesting that, regardless of age, many falls might be prevented. Older adults of any age can, together with their health care providers, take steps to reduce their risk for falls. CDC created the Stopping Elderly Accidents, Deaths & Injuries (STEADI) initiative, which offers tools and resources for health care providers to screen their older patients for fall risk, assess modifiable fall risk factors, and to intervene with evidence-based fall prevention interventions (https://www.cdc.gov/steadi). These include medication management, vision screening, home modifications, referral to physical therapists who can address problems with gait, strength, and balance, and referral to effective community-based fall prevention programs. As the proportion of older adults living in the United States continues to grow, so too will the number of falls and fall-related injuries. However, many of these falls are preventable. To help keep older adults living independently and injury-free, reducing fall risk and fall-related injuries is essential.
Summary.
What is already known about this topic?
Falls are the leading cause of injury among adults aged ≥65 years, who in 2014 experienced an estimated 29 million falls, resulting in 7 million fall-related injuries.
What is added by this report?
In 2018, 27.5% of adults aged ≥65 years reported at least one fall in the past year (35.6 million falls) and 10.2% reported a fall-related injury (8.4 million fall-related injuries). From 2012 to 2016, the percentages of these adults reporting a fall increased, and from 2016 to 2018, the percentages decreased.
What are the implications for public health practice?
Falls and fall-related injuries are highly prevalent but are preventable. Health care providers play a crucial role and can help older adults reduce their risk for falls.
Acknowledgments
Mark Stevens, Gwen Bergen, National Center for Injury Prevention and Control, CDC.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
Footnotes
References
- 1.Burns E, Kakara R. Deaths from falls among persons aged ≥65 years—United States, 2007–2016. MMWR Morb Mortal Wkly Rep 2018;67:509–14. 10.15585/mmwr.mm6718a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ingram DD, Malec DJ, Makuc DM, et al. National Center for Health Statistics guidelines for analysis of trends. Vital Health Stat 2 2018;179:1–71. [PubMed] [Google Scholar]
- 3.Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc 2018;66:693–8. 10.1111/jgs.15304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas 2013;75:51–61. 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 5.Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc 2005;53:2190–4. 10.1111/j.1532-5415.2005.00509.x [DOI] [PubMed] [Google Scholar]
- 6.Becker C, Rapp K. Fall prevention in nursing homes. Clin Geriatr Med 2010;26:693–704. 10.1016/j.cger.2010.07.004 [DOI] [PubMed] [Google Scholar]