Abstract
In order to develop a novel scoring model for the prediction of coronavirus disease-19 (COVID-19) patients at high risk of severe disease, we retrospectively studied 419 patients from five hospitals in Shanghai, Hubei, and Jiangsu Provinces from January 22 to March 30, 2020. Multivariate Cox regression and orthogonal projections to latent structures discriminant analysis (OPLS-DA) were both used to identify high-risk factors for disease severity in COVID-19 patients. The prediction model was developed based on four high-risk factors. Multivariate analysis showed that comorbidity [hazard ratio (HR) 3.17, 95% confidence interval (CI) 1.96–5.11], albumin (ALB) level (HR 3.67, 95% CI 1.91–7.02), C-reactive protein (CRP) level (HR 3.16, 95% CI 1.68–5.96), and age ≥60 years (HR 2.31, 95% CI 1.43–3.73) were independent risk factors for disease severity in COVID-19 patients. OPLS-DA identified that the top five influencing parameters for COVID-19 severity were CRP, ALB, age ≥60 years, comorbidity, and lactate dehydrogenase (LDH) level. When incorporating the above four factors, the nomogram had a good concordance index of 0.86 (95% CI 0.83–0.89) and had an optimal agreement between the predictive nomogram and the actual observation with a slope of 0.95 (R2 = 0.89) in the 7-day prediction and 0.96 (R2 = 0.92) in the 14-day prediction after 1,000 bootstrap sampling. The area under the receiver operating characteristic curve of the COVID-19-American Association for Clinical Chemistry (AACC) model was 0.85 (95% CI 0.81–0.90). According to the probability of severity, the model divided the patients into three groups: low risk, intermediate risk, and high risk. The COVID-19-AACC model is an effective method for clinicians to screen patients at high risk of severe disease.
Keywords: COVID-19, severity, risk factors, scoring model, nomogram
Highlights
- The severity and mortality of COVID-19 patients urgently need to be resolved.
- Comorbidity, ALB, CRP, and age ≥60 years are independent risk factors for severe COVID-19.
- The COVID-19-AACC model is effective for screening patients at risk of severe disease.
Introduction
In December 2019, an increasing number of patients with pneumonia of unknown cause were found in Wuhan, China (1, 2). A novel coronavirus was identified by gene detection and virus isolation. On January 12, 2020, the World Health Organization (WHO) named the virus “2019-nCoV” (3), and on February 11, 2020, the WHO renamed it severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the disease it caused coronavirus disease 2019 (COVID-19) (4). The epidemic soon spread all over China and 212 other countries and areas around the world, resulting in more than 4.72 million people infected and over 300,000 deaths up to May 17, 2020. It has been shown that COVID-19 is more contagious than SARS-CoV seen in 2003, and that medical staff were also infected during the epidemic (5, 6).
Wu et al. (7) first reported that timely antiviral treatment may slow the progression of COVID-19 caused by SARS-CoV-2 and improve the prognosis. Nahama et al. (8) found that the use of resiniferatoxin could improve patient outcomes in those with advanced COVID-19. Omarjee et al. (9) demonstrated that targeting T-cell senescence and cytokine storm with rapamycin may prevent progression in COVID-19. However, up to the date of submission of this report, there are still no specific drugs for COVID-19 patients worldwide, and the severity and mortality of COVID-19 patients are urgent problems that still need to be resolved (10, 11). Hence, it is extremely important to understand the critical factors associated with the severity of COVID-19 and provide convenient and efficient diagnostic methods. Xiao et al. (12) developed an artificial intelligence-assisted tool using computed tomography (CT) imaging to predict disease severity and further estimate the risk of developing severe disease in patients suffering from COVID-19.
In the present study, we aimed to develop a novel scoring model for predicting patients at high risk of severe COVID-19, which would facilitate clinicians to manage COVID-19 patients.
Patients and Methods
Patients
In this study, 419 consecutive patients with confirmed COVID-19 were enrolled from the Shanghai Public Health Clinical Center (208 cases), the Wuhan Central Hospital, Tongji Medical College, Huazhong University of Science and Technology (130 cases), the third People's Hospital of Yancheng City (15 cases), the Fifth People's Hospital of Wuxi (46 cases), and the Second People's Hospital of Yancheng City (20 cases) from January 22 to March 30, 2020, and the follow-up ended on April 30, 2020. All patients admitted with severe COVID-19 to these five hospitals were excluded. This retrospective study was performed in accordance with the Helsinki Declaration and was approved by the Ethics Committee of the Shanghai Public Health Clinical Center (YJ-2020-S089-02).
Definition and Clinical Classification of Cases
All the enrolled COVID-19 patients were diagnosed based on the WHO criteria (13) and the National Health Commission of China criteria. We defined the COVID-19 patients according to epidemiological history consistent with any two clinical manifestations and pathogenic evidence. SARS-CoV-2 RNA was tested with samples from the nose, pharynx, and anus swabs, respectively, by real time-polymerase chain reaction (PCR). We defined the clinical classification and epidemiological history of COVID-19 patients as described previously (14): the first generation (Generation I): patients with a history of exposure to the south China seafood market in Wuhan, China; the second generation (Generation II): patients with Wuhan tourism experience; the third generation (Generation III): imported cases; and the fourth generation (Generation IV): patients infected by Generation III patients. The progression to severe COVID-19 during the observation period was diagnosed based on heart and pulmonary function recovery and lung CT findings. We divided the patients into the severe group and the stable group according to whether the patients had progression to severe COVID-19. In this study, all COVID-19 patients who also had other virus infections were excluded.
Data Collection
We retrospectively collected data from the patients' medical records and attending doctors, including clinical baseline data, laboratory parameters, length of stay, and so on. At the time of admission, all patients underwent laboratory examinations. All data were collected on the first day after admission. Clinical outcomes were followed up till April 30, 2020.
Statistical Analysis
Statistical analyses were performed by SPSS (version 25; IBM SPSS Statistics, United States) and R software, version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria). Continuous variables with normal distribution were expressed as mean ± standard deviation and were compared using the independent sample t-test. Data with non-normal distribution were expressed as median (IQR) and were compared using the non-parametric test. The classified variables were tested using the chi-square test. A value of P < 0.05 was considered statistically significant. The significance of each variable was assessed using the univariate and multivariate Cox proportional hazards model to investigate the independent high-risk factors for disease severity with their hazard ratio (HR) and 95% confidence interval (CI). The performance of the nomogram was evaluated by calibration with 1,000 bootstrap samples to decrease the overfit bias. The receiver operating characteristic (ROC) package in R software was used to compare the time-dependent area under the ROC curve (td-AUC). Orthogonal projections to latent structures discriminant analysis (OPLS-DA) was performed with SIMCA version 14.1.0.2047.
Results
Clinical Characteristics of COVID-19 Patients in the Severe Group and the Stable Group
A total of 419 eligible COVID-19 patients included in the stable group and the severe group were recruited from five hospitals in Shanghai, Jiangsu, and Hubei Provinces, China. The flowchart of patient enrollment is shown in Figure 1. The clinical characteristics of these patients are summarized in Table 1. In these 419 patients, the average age was 47.1 ± 16.0 years, 207 (49.4%) were male, 88 (21.0%) were older than 60 years, 139 (33.2%) had at least one underlying comorbidity, the average hospitalization time was 16.5 ± 7.9 days, and 87 (20.8%) patients became severe and critically ill during the observation period. Three hundred fourteen (74.9%) patients were Generations III and IV.
Figure 1.
Flowchart of COVID-19 patient enrollment including the stable group and the severe group.
Table 1.
Characteristics of COVID-19 patients in this study.
| Overall | Stable group | Severity group | P value | |
|---|---|---|---|---|
| (n = 419) | (n = 332) | (n = 87) | ||
| Age, years | 47.1 ± 16.0 | 44.6 ± 15.2 | 56.8 ± 15.4 | 0.000 |
| Gender (n, %) | 0.053 | |||
| Male | 207 (49.40) | 156 (46.99) | 51 (58.62) | |
| Female | 212 (50.60) | 176 (53.01) | 36 (41.38) | |
| Comorbidity (n, %) | 0.000 | |||
| Without | 280 (66.83) | 249 (75.00) | 31 (35.63) | |
| With | 139 (33.17) | 83 (25.00) | 56 (64.37) | |
| Lymphocyte, × 109/L | 1.2 (0.8–1.6) | 1.2 (0.9–1.7) | 0.8 (0.6–1.1) | 0.000 |
| D-dimer, mg/L | 0.28 (0.19–0.54) | 0.24 (0.17–0.45) | 0.51 (0.30–0.91) | 0.000 |
| ALT, U/L | 24 (15–38) | 23 (14–38) | 27 (18–39) | 0.072 |
| ALB | 40 (37–43) | 41 (38–44) | 37 (33–39) | 0.000 |
| TBIL, μmol/L | 10.4 (7.3–15.4) | 9.8 (7.0–14.5) | 13.4 (8.3–18.8) | 0.002 |
| LDH, U/L | 213 (172–281) | 204 (166–256) | 281 (212–346) | 0.000 |
| CRP | 8.0 (2.6–26.3) | 6.2 (1.8–18.4) | 39.0 (15.0–85.2) | 0.000 |
| PCT, μg/L | 0.05 (0.02–0.05) | 0.04 (0.02–0.05) | 0.05 (0.04–0.09) | 0.000 |
| D-dimer, mg/L | 0.000 | |||
| ≤0.55 | 318 (75.89) | 269 (81.02) | 49 (56.32) | |
| >0.55 | 101 (24.11) | 63 (18.98) | 38 (43.68) | |
| Lymphocyte, × 109/L (n, %) | 0.000 | |||
| >1.0 | 259 (61.81) | 230 (69.28) | 29 (33.33) | |
| ≤1.0 | 160 (38.19) | 102 (30.72) | 58 (66.67) | |
| Age, years (n, %) | 0.000 | |||
| ≤60 | 331 (79.00) | 287 (86.45) | 44 (50.57) | |
| >60 | 88 (21.00) | 45 (13.55) | 43 (49.43) | |
| LDH, U/L (n, %) | 0.000 | |||
| ≤250 | 272 (64.92) | 241 (72.59) | 31 (35.63) | |
| 250–500 | 138 (32.94) | 86 (25.90) | 52 (59.77) | |
| >500 | 9 (2.15) | 5 (1.51) | 4 (4.60) | |
| CRP, mg/L (n, %) | 0.000 | |||
| <10 | 229 (54.65) | 213 (64.16) | 16 (18.39) | |
| ≥10 | 190 (45.35) | 119 (35.84) | 71 (85.06) | |
| ALB, g/L (n, %) | 0.000 | |||
| ≥40 | 215 (51.31) | 202 (60.84) | 13 (14.94) | |
| <40 | 204 (48.69) | 130 (39.16) | 74 (85.06) |
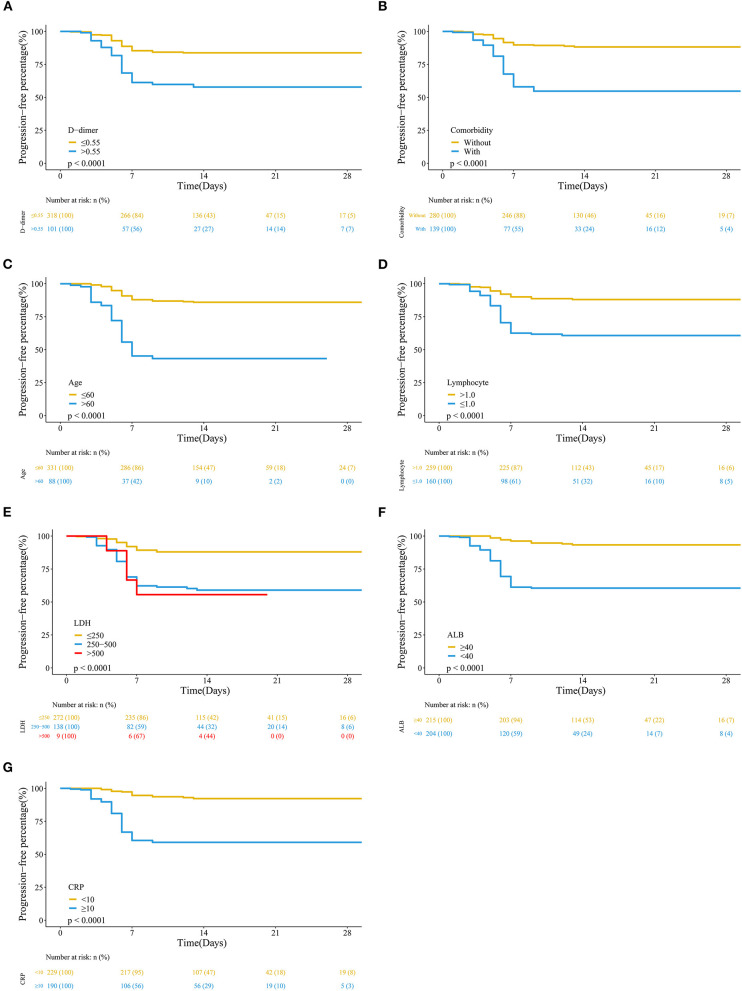
When the clinical characteristics in the stable group and the severe group were compared, the results showed that age, comorbidity, lymphocyte count, albumin (ALB), D-dimer, C-reactive protein (CRP), and lactate dehydrogenase (LDH) levels were significantly different between the two groups (Table 1 and Figure 2).
Figure 2.
Kaplan–Meier analysis of high-risk factors for severe COVID-19. We defined the time from admission after infection and days to severe disease development or discharge. (A) D-dimer; (B) comorbidity; (C) age; (D) lymphocyte count; (E) lactate dehydrogenase (LDH); (F) albumin (ALB); (G) C-reactive protein (CRP).
High-Risk Factors for Severe COVID-19
We performed Cox regression analysis, which demonstrated that comorbidity (HR 3.17, 95% CI 1.96–5.11), ALB level (HR 3.67, 95% CI 1.91–7.02), CRP level (HR 3.16, 95% CI 1.68–5.96), and age ≥60 years (HR 2.31, 95% CI 1.43–3.73) were independent risk factors for severe COVID-19 in these patients (Table 2).
Table 2.
The univariate and multivariate logistic regression analysis independent high-risk factors for severity of COVID-19 patients.
| Un COX analysis | Mul COX analysis | |||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| D-dimer (mg/L) | ||||
| ≤0.55 | 1 | – | 1 | – |
| >0.55 | 2.961 (1.936–4.529) | 0.000 | 1.070 (0.672–1.702) | 0.776 |
| Comorbidity | ||||
| Without | 1 | – | 1 | – |
| With | 4.617 (2.971–7.173) | 0.000 | 3.166 (1.960–5.114) | 0.000 |
| Age (years) | ||||
| ≤60 | 1 | – | 1 | – |
| >60 | 5.557 (3.633–8.499) | 0.000 | 2.307 (1.427–3.728) | 0.001 |
| Lymphocyte (×10/L) | ||||
| >1.0 | 1 | – | 1 | – |
| ≤1.0 | 3.814 (2.440–5.961) | 0.000 | 1.234 (0.741–2.054) | 0.419 |
| LDH (U/L) | ||||
| ≤250 | 1 | – | 1 | – |
| 250–500 | 3.944 (2.526–6.158) | 0.000 | 1.531 (0.918–2.553) | 0.103 |
| >500 | 4.215 (1.487–11.943) | 0.007 | 2.572 (0.869–7.612) | 0.088 |
| ALB (g/L) | ||||
| ≥40 | 1 | – | 1 | – |
| <40 | 7.899 (4.374–14.267) | 0.000 | 3.663 (1.912–7.018) | 0.000 |
| CRP (mg/L) | ||||
| <10 | 1 | – | 1 | – |
| ≥10 | 7.022 (4.076–12.098) | 0.000 | 3.161 (1.677–5.961) | 0.000 |
We also used OPLS-DA to evaluate the influence of parameters on the severity of COVID-19. The severe group was unambiguously distinguished from the stable group (Figures 3A,B). The top five parameters that influenced the severity of COVID-19 were CRP, ALB, age ≥60 years, comorbidity, and LDH (Figures 3C,D).
Figure 3.
OPLS-DA to evaluate the influence of parameters on the severity of COVID-19. (A) ROC of OPLS-DA. (B) In the three-dimensional scatter plot of all samples in the OPLS-DA model, the predictive component was used in the stable group and the severe group. (C) Loading plot showing the relationship of each parameter to the predictive component (x) and the first orthogonal component (y); parameters that deviated from zero on the x-axis were considered potentially predictive. (D) The higher predictive VIP (VIP pred) value.
Hence, comorbidity, ALB, CRP, and age ≥60 years were identified as the most influential risk factors for the severity of COVID-19 in these patients.
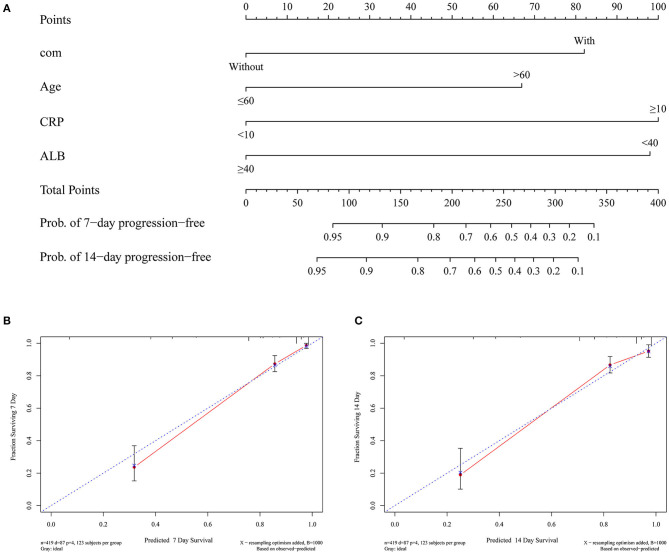
Development and Validation of a Predictive Nomogram for the Probability of Severe COVID-19
Based on the above independent risk factors associated with the severity of COVID-19, we developed a predictive nomogram and validated it using the bootstrap method (Figure 4A). Calibration tests were used to evaluate the predictive accuracy for progression of COVID-19 using the nomogram. The C-index for predicting the severity of COVID-19 with the nomogram was 0.86 (0.83–0.89), which indicated good accuracy. The calibration curve showed optimal agreement between the predictive nomogram and the actual observation with a slope of 0.95 (R2 = 0.89) in the 7-day prediction and 0.96 (R2 = 0.92) in the 14-day prediction after 1,000 bootstrap sampling (Figures 4B,C).
Figure 4.
Development and validation of a predictive nomogram for the probability of severe COVID-19. (A) A predictive nomogram was developed based on the independent risk factors associated with the severity of COVID-19. (B) The 7-day predictive performance of the nomogram with a slope of 0.95 (R2 = 0.89). (C) The 7-day predictive performance of the nomogram with a slope of 0.96 (R2 = 0.92).
Development and Assessment of the Novel Scoring Model for COVID-19 Severity
Based on the above nomogram, we further developed a novel scoring model, which may facilitate the clinical assessment of COVID-19 severity. We named the model COVID-19-American Association for Clinical Chemistry (AACC) (age ≥60 years, ALB, comorbidity, and CRP), and the score ranged from 0 to 5 points (Figure 5). CRP (<10 mg/L) and ALB (<40 g/L) were chosen as the cut-off values, respectively, to score the ALB and CRP.
Figure 5.
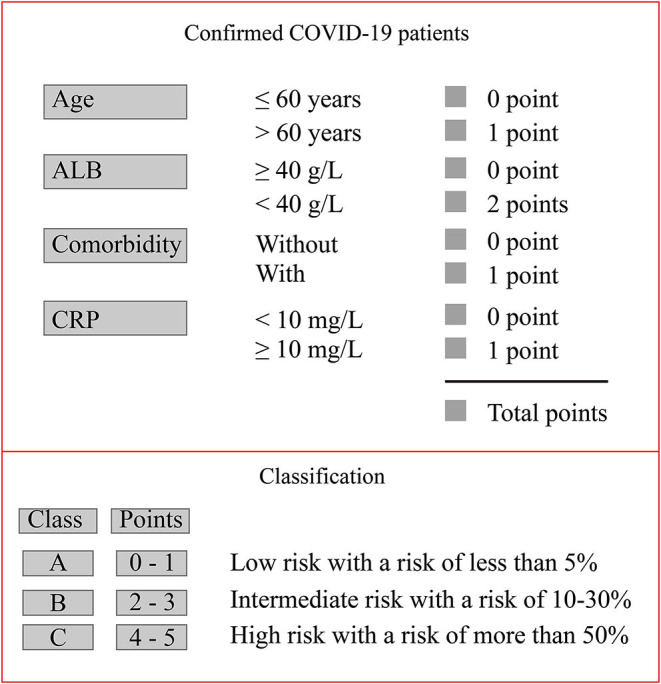
COVID-19-AACC model for risk stratification of the probability of severe COVID-19.
The AUROC of the COVID-19-AACC scoring model for predicting the probability of severe COVID-19 in these patients was 0.85 (95% CI 0.81–0.90).
With the cut-off value of 0 point, the positive predictive value and positive likelihood ratio of the scoring model were 27.2 (95% CI 22.3–32.5) and 1.42 (95% CI 1.3–1.5). The negative predictive value and negative likelihood ratio were 97.3 (95% CI 92.2–99.4) and 0.11 (95% CI 0.03–0.3), with a sensitivity of 96.6 (95% CI 90.3–99.3) and a specificity of 32.2 (95% CI 27.2–37.5).
Using a cut-off value of 4 points, the positive predictive value and positive likelihood ratio of the scoring model were 80.6 (95% CI 62.5–92.5) and 15.90 (95% CI 6.7–37.5). The negative predictive value and negative likelihood ratio were 84.0 (95% CI 80.0–87.5) and 0.73 (95% CI 0.6–0.8), with a sensitivity of 28.7 (95% CI 19.5–39.4) and a specificity of 98.2 (95% CI 96.1–99.3) (Table 3).
Table 3.
The performances of COVID-19-AACC model for risk stratification of probabilities for severity of COVID-19 patients.
| Variable | (n = 419) |
|---|---|
| AUROC | 0.85 (0.81–0.90) |
| Cutoff value (95% CI) | 0 |
| Sensitivity, % | 96.6 (90.3–99.3) |
| Specificity, % | 32.2 (27.2–37.5) |
| Positive predictive value, % | 27.2 (22.3–32.5) |
| Negative predictive value, % | 97.3 (92.2–99.4) |
| Positive likelihood ratio | 1.42 (1.3–1.5) |
| Negative likelihood ratio | 0.11 (0.03–0.3) |
| Cutoff value (95% CI) | 4 |
| Sensitivity, % | 28.7 (19.5–39.4) |
| Specificity, % | 98.2 (96.1–99.3) |
| Positive predictive value, % | 80.6 (62.5–92.5) |
| Negative predictive value, % | 84.0 (80.0–87.5) |
| Positive likelihood ratio | 15.90 (6.7–37.5) |
| Negative likelihood ratio | 0.73 (0.6–0.8) |
The following three risk groups according to their probability of severe COVID-19 were developed: low risk (Class A: 0–1 point) group, with a risk of severe disease of <5%; intermediate risk (Class B: 2–3 points) group, with a risk of 10–30%; and high-risk (Class C: 4–5 points) group, with a risk of more than 50% (Figure 5).
Discussion
Coronavirus is distributed throughout the world and has many subtypes. SARS in 2003 and Middle East respiratory syndrome (MERS) in 2013 were caused by coronavirus infection (15, 16). At present, the rapid spread of SARS-CoV-2 worldwide has resulted in a heavy burden to society. To date, the global control of COVID-19 was still not optimistic (17, 18). Although the overall mortality of COVID-19 is not high internationally, the mortality of patients with severe and critical disease is relatively high (19). According to the WHO, the death rate in critically ill patients was over 50% (20). Obviously, it is extremely important to manage these serious cases in a timely and appropriate manner. In fact, in the majority of regions and countries, rapid diagnosis of suspected cases has been possible (21). Thus, how to control the progression from mild to severe disease in these patients is the key to the treatment of COVID-19 by clinicians.
In view of this issue, several studies (22, 23) have shown the factors that may affect the severity of COVID-19. Ji et al. (24) showed that comorbidity, older age, lower lymphocyte count, and higher LDH level were associated with the progression of COVID-19. Yan et al. (25) described the clinical and laboratory characteristics of 193 patients with severe COVID-19. Of these patients, 48 with severe COVID-19 had diabetes. Diabetes was associated with an increased risk of death. Another study (26) showed that severe CO2 retention and acidosis prior to extracorporeal membrane oxygenation were confirmed to be risk factors for severe COVID-19 and poor prognosis.
In this study, we retrospectively studied 419 patients from five hospitals in Shanghai, Hubei, and Jiangsu Provinces and determined several risk factors for the severity of COVID-19 in these patients, including age ≥60 years, ALB level, comorbidity, and CRP level. Of the 419 enrolled cases, both median age and the proportion of patients over 60 years in the severe COVID-19 group were significantly higher than those in the stable group (Table 1). The above conclusions were consistent with most previous studies, such as those by Wang et al. (27). It is notable that patients with comorbidities, especially diabetes and cardiovascular diseases, were prone to severe COVID-19. Ji et al. (24) showed that comorbidity, older age, lower lymphocyte count, and higher LDH level at presentation were independent high-risk factors for COVID-19 progression. Zhang et al. (28) selected risk factors for severe and even fatal pneumonia and created a predictive scoring system, including age, white blood cell count, neutrophil count, glomerular filtration rate, and myoglobin level as candidates for the scoring system to predict the severity of COVID-19. We also considered the reasons for the decline in physical function and immune function in the elderly, which could increase the probability of severe COVID-19. The study by Cai et al. (29) indicated that CRP, procalcitonin (PCT), and D-dimer may predict the severity of COVID-19. The study by Zhou et al. (30) showed no significant differences in CRP between the non-aggravation group and the aggravation group. In our study, the levels of CRP in the severe group were significantly higher than those in the stable group, and the proportion of patients with CRP levels ≥10 mg/L was also significantly higher than that in the stable group. Mishra et al. (31) recommended serum ALB for the therapy of SARS-CoV-2. Bi et al. (32) showed that ALB was much lower in severe patients, but was not an independent risk factor for disease progression. Our study has confirmed that ALB is a risk factor for the severity of COVID-19. In the present study, we also assessed the critical factors for disease severity using logistic analysis and OPLS-DA, respectively. The results of both analyses showed that comorbidity, ALB, CRP, and age ≥60 years were the most influential risk factors for severe COVID-19 in these patients.
Based on the above risk factors, we developed a predictive nomogram for the probability of severe COVID-19. The nomogram had a good concordance index of 0.86 (95% CI 0.83–0.89) and well-fitted calibration curves in both the 7-day prediction and the 14-day prediction. We then constructed a scoring model (COVID-19-AACC) based on the above nomogram, which also had a good concordance index of 0.85 (95% CI 0.81–0.90). The COVID-19-AACC scoring model was used to identify COVID-19 patients at low risk (Class A), intermediate risk (Class B), and high risk (Class C) of severe disease. Of the 419 patients enrolled, 254 (60.6%) scored 0–1 point and were considered low risk, and 134 (32.0%) scored 2–3 points and were considered intermediate risk, whereas 31 (7.4) scored 4–5 points and were considered high risk. These high-risk patients should be transferred to tertiary centers as early as possible for appropriate treatment.
Of note, there were several limitations in the present study. Firstly, this study is a retrospective, multicenter study, and the possibility of recall bias cannot be completely excluded. The results from a limited sample size do not necessarily represent the overall results of patients in China or even in the world. Secondly, a validation group should be included to further validate the scoring model. Finally, more indicators, including genes and images, should be included to further optimize the model.
In summary, the COVID-19-AACC scoring model will be of significant help to clinicians in evaluating COVID-19 patients in the early stage, especially in non-tertiary hospitals. For high-risk groups, early intervention can effectively reduce the rate of severe disease and mortality.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the present retrospective study was performed in accordance with the Helsinki Declaration and was approved by the Ethics Committee of the Shanghai Public Health Clinical Center (YJ-2020-S089-02). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
ZD, DC, DW, and DZ contributed to the study concept and design, conducted the literature search, and wrote the manuscript. YF, JX, WG, and YY contributed to the data analysis and produced the tables and figures. YS, LZ, and XZ contributed to the collection of patient samples and medical information. JX and SS obtained funding. DL, YZ, MW, and AW contributed to the acquisition and analysis of data. HL and SS contributed to the study concept and critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Glossary
Abbreviations
- COVID-19
coronavirus disease-19
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- SARS
severe acute respiratory syndrome
- MERS
Middle East respiratory syndrome
- WHO
World Health Organization
- HR
hazard ratio
- CI
confidence interval
- OPLS-DA
orthogonal projections to latent structures discriminant analysis
- CRP
C-reactive protein
- ALB
albumin
- LDH
lactate dehydrogenase.
Footnotes
Funding. This study was supported by the Hospital Fund of Shanghai Public Health Clinical Center (Grant No. KY-GW-2020-13).
References
- 1.Chan JF, Kok KH, Zhu Z, Chu H, To KK, Yuan S, et al. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect. (2020) 9:221–36. 10.1080/22221751.2020.1719902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ren B, Yan F, Deng Z, Zhang S, Xiao L, Wu M, et al. Extremely high incidence of lower extremity deep venous thrombosis in 48 patients with severe COVID-19 in Wuhan. Circulation. (2020) 142:181–3. 10.1161/CIRCULATIONAHA.120.047407 [DOI] [PubMed] [Google Scholar]
- 3.Scott SE, Zabel K, Collins J, Hobbs KC, Kretschmer MJ, Lach M, et al. First mildly Ill, non-hospitalized case of Coronavirus disease 2019 (COVID-19) without viral transmission in the United States - Maricopa County, Arizona, 2020. Clin Infect Dis. (2020) 71:807–12. 10.1093/cid/ciaa374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of Coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. (2020) 172:577–82. 10.7326/M20-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ragni E, Mangiavini L, Viganò M, Brini AT, Peretti GM, Banfi G, et al. Management of osteoarthritis during COVID-19 pandemic. Clin Pharmacol Ther. (2020) 108:719–29. 10.1002/cpt.1910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schijns V, Lavelle EC. Prevention and treatment of COVID-19 disease by controlled modulation of innate immunity. Eur J Immunol. (2020) 50:932–8. 10.1002/eji.202048693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu J, Li W, Shi X, Chen Z, Jiang B, Liu J, et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J Intern Med. (2020) 288:128–38. 10.1111/joim.13063 [DOI] [PubMed] [Google Scholar]
- 8.Nahama A, Ramachandran R, Cisternas AF, Ji H. The role of afferent pulmonary innervation in poor prognosis of acute respiratory distress syndrome in COVID-19 patients and proposed use of resiniferatoxin (RTX) to improve patient outcomes in advanced disease state: a review. Med Drug Discov. (2020) 5:100033 10.1016/j.medidd.2020.100033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Omarjee L, Janin A, Perrot F, Laviolle B, Meilhac O, Mahe G. Targeting T-cell senescence and cytokine storm with rapamycin to prevent severe progression in COVID-19. Clin Immunol. (2020) 216:108464. 10.1016/j.clim.2020.108464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dhawan G, Kapoor R, Dhawan R, Singh R, Monga B, Giordano J, et al. Low dose radiation therapy as a potential life saving treatment for COVID-19-induced acute respiratory distress syndrome (ARDS). Radiother Oncol. (2020) 147:212–6. 10.1016/j.radonc.2020.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quaglino P, Fava P, Brizio M, Marra E, Rubatto M, Agostini A, et al. Metastatic melanoma treatment with check point inhibitors in the COVID-19 era: experience from an Italian skin cancer unit. J Eur Acad Dermatol Venereol. (2020) 34:1395–6. 10.1111/jdv.16586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xiao LS, Li P, Sun F, Zhang Y, Xu C, Zhu H, et al. Development and validation of a deep learning-based model using computed tomography imaging for predicting disease severity of Coronavirus disease 2019. Front Bioeng Biotechnol. (2020) 8:898. 10.3389/fbioe.2020.00898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (nCoV) Infection is Suspected: Interim Guidance. (2020). Available online at: https://www.who.int/internalpublications-detail/clinical-management-of-severe-acute-respiratoryinfection-when-novel-coronavirus-(ncov)-infection-is-suspected (accessed January 20, 2020).
- 14.Wu J, Liu J, Zhao X, Liu C, Wang W, Wang D, et al. Clinical characteristics of imported cases of covid-19 in Jiangsu province: a multicenter descriptive study. Clin Infect Dis. (2020) 71:706–12. 10.1093/cid/ciaa199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang Y, Peng F, Wang R, Yange M, Guan K, Jiang T, et al. The deadly coronaviruses: the 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J Autoimmun. (2020) 109:102434. 10.1016/j.jaut.2020.102434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al Hosani FI, Kim L, Khudhair A, Pham H, Al Mulla M, Al Bandar Z, et al. Serologic follow-up of middle east respiratory syndrome coronavirus cases and contacts-Abu Dhabi, United Arab Emirates. Clin Infect Dis. (2019) 68:409–18. 10.1093/cid/ciy503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garzotto F, Ceresola E, Panagiotakopoulou S, Spina G, Menotto F, Benozzi M, et al. COVID-19: ensuring our medical equipment can meet the challenge. Expert Rev Med Dev. (2020) 17:483–9. 10.1080/17434440.2020.1772757 [DOI] [PubMed] [Google Scholar]
- 18.Raamkumar AS, Tan SG, Wee HL. Measuring the outreach efforts of public health authorities and the public response on facebook during the COVID-19 pandemic in early 2020: cross-country comparison. J Med Internet Res. (2020) 22:e19334 10.2196/19334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shi Q, Zhang X, Jiang F, Zhang X, Hu N, Bimu C, et al. Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: a two-center, retrospective study. Diabetes Care. (2020) 43:1382–91. 10.2337/dc20-0598 [DOI] [PubMed] [Google Scholar]
- 20.Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the fleischner society. Chest. (2020) 158:106–16. 10.1148/radiol.2020201365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong SC, Leung M, Lee LL, Chung KL, Cheng VC. Infection control challenge in setting up a temporary test centre at Hong Kong international airport for rapid diagnosis of COVID-19 due to SARS-CoV-2. J Hosp Infect. (2020) 105:571–3. 10.1016/j.jhin.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu J, Liu Y, Xiang P, Pu L, Xiong H, Li C, et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med. (2020) 18:206. 10.1186/s12967-020-02374-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang X, Yu J, Pan LY, Jiang HY. ACEI/ARB use and risk of infection or severity or mortality of COVID-19: a systematic review and meta-analysis. Pharmacol Res. (2020) 158:104927 10.1016/j.phrs.2020.104927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ji D, Zhang D, Xu J, Chen Z, Yang T, Zhao P, et al. Prediction for progression risk in patients with COVID-19 pneumonia: the CALL score. Clin Infect Dis. (2020) 71:1393–9. 10.1093/cid/ciaa414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yan Y, Yang Y, Wang F, Ren H, Zhang S, Shi X, et al. Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diabetes Res Care. (2020) 8:e001343. 10.1136/bmjdrc-2020-001343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang X, Cai S, Luo Y, Zhu F, Hu M, Zhao Y, et al. Extracorporeal membrane oxygenation for Coronavirus disease 2019-induced acute respiratory distress syndrome: a multicenter descriptive study. Crit Care Med. (2020) 48:1289–95. 10.1097/CCM.0000000000004447 [DOI] [PubMed] [Google Scholar]
- 27.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang C, Qin L, Li K, Wang Q, Zhao Y, Xu B, et al. A novel scoring system for prediction of disease severity in COVID-19. Front Cell Infect Microbiol. (2020) 10:318. 10.3389/fcimb.2020.00318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cai Q, Huang D, Ou P, Yu H, Zhu Z, Xia Z, et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. (2020) 75:1742–52. 10.1111/all.14309 [DOI] [PubMed] [Google Scholar]
- 30.Zhou Y, Zhang Z, Tian J, Xiong S. Risk factors associated with disease progression in a cohort of patients infected with the 2019 novel coronavirus. Ann Palliat Med. (2020) 9:428–36. 10.21037/apm.2020.03.26 [DOI] [PubMed] [Google Scholar]
- 31.Mishra PM, Uversky VN, Nandi CK. Serum albumin-mediated strategy for the effective targeting of SARS-CoV-2.Med. Hypotheses. (2020) 140:109790. 10.1016/j.mehy.2020.109790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bi X, Su Z, Yan H, Du J, Wang J, Chen L, et al. Prediction of severe illness due to COVID-19 based on an analysis of initial fibrinogen to albumin ratio and platelet count. Platelets. (2020) 31:674–9. 10.1080/09537104.2020.1760230 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.