Abstract
Chronic disease is a growing concern for research, policy and clinical care. While the global burden of HIV for transgender populations has been comprehensively covered in recent systematic reviews, the same is not true for the burden of other chronic disease. The objective of this study was to review the literature on non-HIV chronic disease burden for transgender populations worldwide. A systematic review was conducted of Medline, Embase, CINAHL, PsycINFO and LGBT Life bibliographic databases for peer-reviewed scientific studies with non-HIV chronic disease prevalence data for transgender populations published any date up to February 15, 2019 without restriction on country or study design. A total of 93 studies and 665 datapoints were included in this review, comprising 48 distinct chronic disease outcomes in seven groups (cancer, cerebro/cardiovascular conditions, chronic liver and kidney disease, mental health and substance use conditions, metabolic and endocrine disorders, musculoskeletal and brain disorders, respiratory conditions, and unspecified and other conditions). The empirical literature on chronic disease among global transgender populations focuses on mental health morbidity, demonstrating an evidence gap on chronic physical health morbidity, particularly beyond that of sexual health. This review identified important gaps including in age-related conditions, inflammation-related disease and studies designed explicitly to investigate chronic disease burden among transgender populations. There is a need for high quality evidence in this area, including longitudinal population-based studies with appropriate comparison groups, and consistent measurement of both transgender status and chronic conditions.
Keywords: Transgender persons, Chronic disease, Health, Systematic review
1. Introduction
1.1. Chronic disease as a public health issue
Chronic disease is a leading cause of morbidity and mortality globally, accounting for 63% of deaths annually— with cardiovascular disease, diabetes, cancer, and chronic respiratory conditions responsible for much of the disease burden (80%) (World Health Organization. Global Status Report on Noncommunicable Diseases, 2010). In addition to premature mortality, consequences of chronic disease include medical complications, elevated risk of other co-morbidities, and disability (World Health Organization, 2010, Forouzanfar et al., 2016). At the population level, chronic disease morbidity impacts growing healthcare system burden and cost, healthcare-cost related poverty, and larger economic effects (World Health Organization, 2010), such that each 10% increase in chronic disease burden corresponds with a 0.5% lower rate of annual economic growth globally (Stuckler, 2008). Despite advances in medicine, technology and healthcare systems that have eradicated many serious threats to human health, chronic disease burden continues to rise worldwide, increasingly so in middle and low-income countries (Forouzanfar et al., 2016). Mounting chronic disease burden is further fueled by population growth and ageing as the global population increasingly lives in a post epidemiologic transition context (Kivimäki et al., 2015). Importantly, key drivers of chronic disease include modifiable risk factors such as environmental exposures (e.g. workplace risks, sanitation services), access to social and material resources (e.g. healthy food, freedom from violence, adequate income) and health behaviours (e.g. substance use, exercise), and thus may be more intervenable than risk factors for acute and other illnesses. (Forouzanfar et al., 2016)This is therefore an important area for public health focus.
1.2. Transgender populations and chronic disease
While chronic disease for transgender populations has been recognized as a priority research area (IOM, 2011), there is scarce literature in this area, particularly outside of HIV and mental health conditions (Reisner et al., 2016, Marshall et al., 2019). HIV among transgender populations has been well reviewed recently and globally (Reisner et al., 2016, Baral et al., 2013, Poteat et al., 2016, Reisner and Murchison, 2016, Herbst et al., 2008, Becasen et al., 2019, MacCarthy et al., 2017). A review of research on the global health burden of transgender populations published from 2008 to 2014 found only 7% of included data on general health (e.g. chronic disease, mortality), mostly in the United States (US) (Reisner et al., 2016). Of the limited research, there is evidence transgender people experience poorer physical health compared to cisgender people (Reisner et al., 2016). Much of the existing research, beyond sexual and mental health, has focused on cardiovascular conditions among transgender people accessing gender affirming hormone therapy (GAHT), again largely in the US, although also in Europe (Streed et al., 2017). Studies have shown that transgender people have higher prevalence of any chronic disease (Witten, 2014)as well as multimorbidity, compared to cisgender groups (Downing and Przedworski, 2018). Chronic disease burden may also be exacerbated for transgender people who are racialized (Seelman et al., 2017, Brown and Jones, 2014), older (Swartz et al., 2019), of lower socioeconomic status (Seelman et al., 2017), have poor access to other social determinants of health (Blosnich et al., 2017), and live with co-morbidities (Proctor et al., 2016).
1.3. Rationale and objectives for this review
No systematic review of the literature has been conducted of chronic disease burden for transgender populations. This study sought to systematically review and synthesize all available epidemiologic data on chronic disease burden, primarily prevalence in this case, among transgender populations, to identify areas for future research, and inform healthcare practice, policy focus and action. Initially, we also aimed to assess whether chronic illness burden was greater for transgender populations living with HIV compared to those living with HIV as data were available; however, the number of studies reporting HIV chronic co-morbidities for transgender people captured in this review was too few to warrant a sub-analysis.
2. Methods
2.1. Protocol and registration
The protocol has been registered with the International Prospective Register of Systematic Reviews (PROSPERO, https://www.crd.york.ac.uk/prospero), registration number CRD42020104077. The review is reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines (Moher et al., 2009).
2.2. Eligibility criteria
This review included peer-reviewed journal articles reporting quantitative data on the prevalence of chronic disease among transgender people. Studies with a very small transgender sample sizes (n < 10) and those published in languages other than English, French, Spanish, Italian, or Portuguese were excluded. Given the evidence need, no restrictions were placed on publication date, study country, or type of study design. If multiple publications reported the same chronic disease outcomes from a single study, the article reporting the most chronic disease data was included. For reported mental health and substance use outcomes, those based on symptomology assessments were excluded (e.g. psychometric scales for depression), for consistency with study outcomes in other chronic disease groups.
2.3. Information sources
MEDLINE, Embase, CINAHL, PsycINFO, and LGBT Life bibliographic databases were electronically searched for peer-reviewed literature published through Feburary 15, 2019.
2.4. Literature search
The search strategy was developed in consultation with a research librarian at the University of British Columbia and included Medical Subject Headings (MeSH terms) and keywords related to the two main search concepts: transgender persons and chronic disease. Commonly used terms for both concepts were included as subject headings and keywords, such as “transsexual”, or “gender minority” for transgender; and “long-term illness”, “chronic disease”, or “diabetes” for chronic conditions. The MEDLINE search strategy is included in Supplementary material.
2.5. Study selection
Studies were screened in parallel by two independent reviewers (AJR, AIS) using Covidence (Veritas Health Innovation, Melbourne). Reviewers rated studies for inclusion or exclusion at the title and abstract level first, then at the full text level. Disagreements at each screening phase were resolved through discussion and reasons for exclusion recorded.
2.6. Data extraction
Data elements extracted included participant characteristics, study design, sample size, and outcomes. One reviewer (AJR) extracted data from included publications using a predetermined extraction form. The second reviewer (AIS) assessed a 10% sample of extracted data for accuracy and any discrepancies were resolved through discussion between the two reviewers (Inter-rater reliability, percent agreement: 97%). Both the number of unique studies and the number of relevant datapoints reported in each study were captured. For example, a study reporting cancer outcomes for transgender people counted as n = 1 at the study level. If this study reported the prevalence of multiple cancer types (e.g. lung cancer and skin cancer), it counted as n = 2 at the datapoint level. Further, if the study reported cancer outcomes for multiple transgender sub-groups (e.g. by gender, race), each reported outcome was counted as a unique datapoint. For mental health and substance use outcomes, only diagnoses based on self-report, provider-report, or structured clinical interviews were included as most reliable measures of chronic disease conditions; assessments of symptomology (e.g., depression symptom scales) were excluded.
3. Results
3.1. Study selection
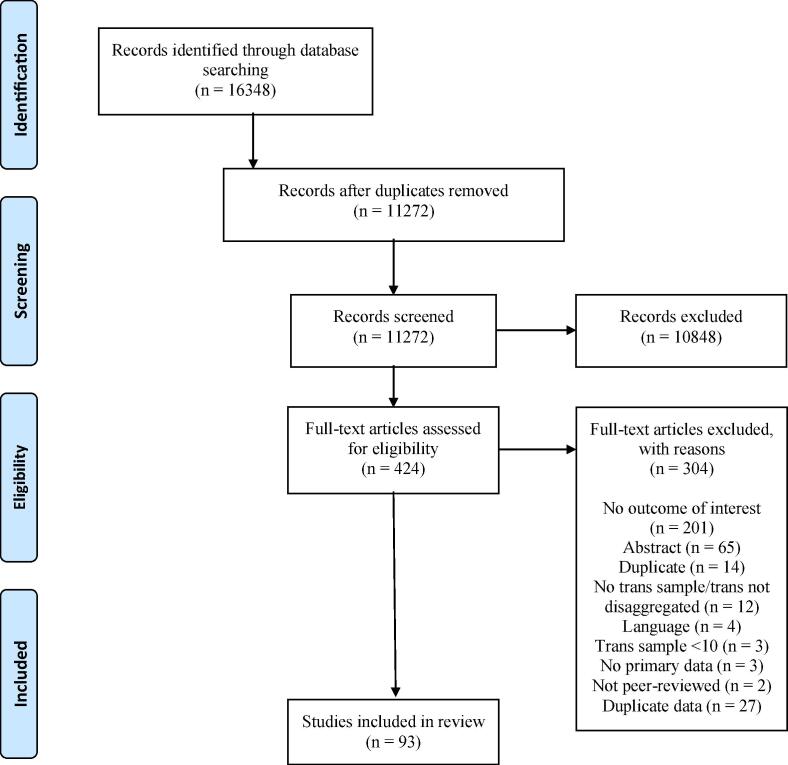
As shown in Fig. 1, 11,272 unique records were identified from the electronic database search. After title and abstract screening, 10,848 records were excluded with 424 articles assessed for eligibility via full text review. Of these, 93 articles were eligible for the review.
Fig. 1.
PRISMA flowchart for study screening for systematic search.
3.2. Study characteristics
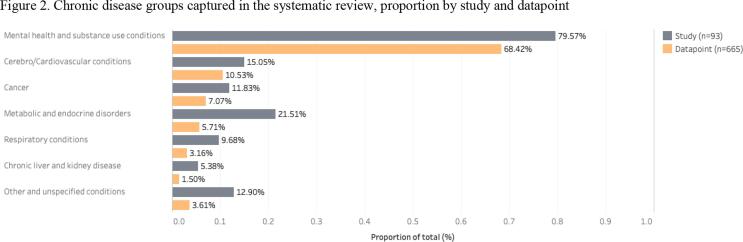
The 93 studies included 665 datapoints, reporting 48 unique chronic disease outcomes. Outcomes were grouped into seven chronic condition groups, adapted from the (World Health Organization. Global Status Report on Noncommunicable Diseases, 2010), for the purpose of narrative synthesis (Fig. 2, Supplementary material) (Popay et al., 2006).
Fig. 2.
Chronic disease groups captured in the systematic review, proportion by study and datapoint.
As summarized in Table 1, articles were published between 1980 and 2019: 57% were published in the five years preceding the search (2015–2019) and 85% in the decade preceding the search (2010–2019). Nearly half of included studies were clinical samples (44%), nearly one-quarter convenience samples (23%), 22% electronic medical record (EMR), 6% respondent-driven sampling (RDS) or snowball sampling methods, and 5% probability-based samples. A majority of studies employed cross-sectional designs (77%), nearly one-fifth longitudinal designs (17%), one a case-control design, and one a randomized controlled trial (RCT). Only 6.46% employed matching of any kind. Study design was classified based on analytic design (e.g. if a study used data from a retrospective cohort but treated the sample as cross-sectional in analysis, it was categorized as cross-sectional).
Table 1.
Studies and study characteristics included in systematic review.
| Study ID | Study sample | Country | Sampling method | Study design | Trans sample size | Chronic condition outcomes |
|---|---|---|---|---|---|---|
| ASIA | ||||||
| (Chen et al., 2019) | Transgender people | China | Convenience | Cross-sectional | 1309 | Mental health and substance use disorders |
| (Kalra and Shah, 2013) | Hijras accessing an STI clinic | India | Clinical | Cross-sectional | 50 | Mental health and substance use disorders |
| (Baba et al., 2011) | Transgender men patients at a GID clinic | Japan | Clinical | Cross-sectional | 178 | Metabolic and endocrine disorders |
| (Hoshiai et al., 2010) | GID clinic patients | Japan | Clinical | Cross-sectional | 579 | Mental health and substance use disorders |
| (Rutledge et al., 2018) | Transgender women | Malaysia | Convenience | Cross-sectional | 199 | Mental health and substance use disorders |
| (Lim et al., 2019) | Transgender OBGYN clinic patients | South Korea | EMR | Cross-sectional | 54 | Mental health and substance use disorders |
| EUROPE | ||||||
| (Cuypere et al., 1995) | Applicants for GAS at a gender identity clinic | Belgium | Clinical | Cross-sectional | 35 | Mental health and substance use disorders |
| (Defreyne et al., 2017) | Transgender endocrine clinic patients starting GAHT | Belgium | Clinical | Cross-sectional | 1081 | Metabolic and endocrine disorders |
| (Weyers et al., 2009) | Transsexual women accessing GAS | Belgium | Clinical | Cross-sectional | 50 | Unspecified and other diseases |
| (Wierckx et al., 2013) | Transgender gender clinic patients accessing GAHT, with cisgender control group | Belgium | Clinical | Cross-sectional | 352 | Cerebro/Cardiovascular diseases |
| (Simonsen et al., 2016) | Transsexual people accessing GAS at a public GID clinic | Denmark | EMR | Retrospective cohort | 104 | Cancer; Cerebro/Cardiovascular diseases; Chronic liver and kidney disease; Other and unspecified diseases; Respiratory disease |
| (Simonsen et al., 2016) | Transsexual people accessing GAS at a public GID clinic | Denmark | EMR | Retrospective cohort | 104 | Mental health and substance use disorders |
| (Holt et al., 2016) | Youth referred to a gender identity clinic | England | Clinical | Cross-sectional | 218 | Mental health and substance use disorders |
| Judge et al. (Judge et al., 2014) | Endocrine clinic patients with suspected or confirmed GD referred for GAHT | Ireland | Clinical | Cross-sectional | 218 | Cerebro/Cardiovascular conditions; Metabolic and endocrine disorders; Mental health and substance use disorders |
| (Colizzi et al., 2014) | Transgender patients at a gender identity clinic | Italy | Clinical | Prospective cohort | 118 | Mental health and substance use disorders |
| (Fisher et al., 2013) | Patients with GID at a GID clinic, without previous GAS | Italy | Clinical | Cross-sectional | 140 | Mental health and substance use disorders |
| (Madeddu et al., 2009) | Transsexual GID psychiatric clinic patients seeking GAS | Italy | Clinical | Cross-sectional | 50 | Mental health and substance use disorders |
| (Heylens et al., 2014) | Adults with GID seeking GAHT/GAS at gender clinics | Multiple (The Netherlands, Belgium, Germany, Norway) | Clinical | Cross-sectional | 305 | Mental health and substance use disorders |
| (Haraldsen and Dahl, 2000) | Transsexual patients with GAS history and cisgender personality disorder patients and cisgender healthy controls | Norway | Clinical | Cross-sectional | 86 | Mental health and substance use disorders |
| (Duišin et al., 2014) | Transgender psychiatric clinic patients and cisgender heterosexual comparison group | Serbia | Clinical | Cross-sectional | 30 | Mental health and substance use disorders |
| (Becerra-Fernandez et al., 2014) | Transgender men patients with GD diagnosis at GID clinic | Spain | Clinical | Cross-sectional | 77 | Metabolic and endocrine disorders |
| (Bergero-Miguel et al., 2016) | Transgender patients with GD at a public gender identity clinic | Spain | Clinical | Cross-sectional | 210 | Mental health and substance use disorders |
| (Gómez-Gil et al., 2009) | Transsexual patients with GD seeking GAS/GAHT | Spain | Clinical | Cross-sectional | 230 | Mental health and substance use disorders |
| (Guzmán-Parra et al., 2016) | Transsexual patients of a gender identity clinic | Spain | Clinical | Cross-sectional | 197 | Mental health and substance use disorders |
| (Vilas et al., 2014) | Transgender gender disorder clinic patients accessing GAHT | Spain | Clinical | Prospective cohort | 157 | Metabolic and endocrine disorders |
| (Bodlund and Kullgren, 1996) | Transsexual patients accessing GAS | Sweden | Clinical | Prospective cohort | 19 | Mental health and substance use disorders |
| (Hepp et al., 2005) | Psychiatric clinic patients with GID | Switzerland | Clinical | Cross-sectional | 31 | Mental health and substance use disorders |
| (de Vries et al., 2011) | Adolescent gender identity clinic patients with GID | The Netherlands | Clinical | Cross-sectional | 105 | Mental health and substance use disorders |
| (Gooren et al., 2013) | Transsexual patients accessing GAHT | The Netherlands | EMR | Retrospective cohort | 3102 | Cancer |
| (Gooren and Morgentaler, 2014) | Transsexual women gender clinic patients with history of GAHT and orchiectomy | The Netherlands | EMR | Retrospective cohort | 2306 | Cancer |
| (Van Kesteren et al., 1997) | Transsexuals receiving GAHT | The Netherlands | EMR | Retrospective cohort | 1109 | Cerebro/Cardiovascular diseases |
| (Wallien et al., 2007) | Dutch children referred to a GID clinic, and a comparison group of children referred to an ADHD clinic | The Netherlands | Clinical | Cross-sectional | 120 | Mental health and substance use disorders |
| LATIN AMERICA | ||||||
| (Fontanari et al., 2018) | Transgender women patients at a GD clinic | Brazil | Clinical | Cross-sectional | 289 | Mental health and substance use disorders |
| (Lobato et al., 2007) | Transsexual patients in a GID program | Brazil | Clinical | Cross-sectional | 138 | Mental health and substance use disorders |
| MIDDLE EAST AND NORTHERN AFRICA REGION | ||||||
| (Aghabikloo et al., 2012) | Patients with GID seeking GAS | Iran | Clinical | Cross-sectional | 69 | Mental health and substance use disorders |
| (Havar et al., 2015) | Patients with GID accessing GAS | Iran | Clinical | Cross-sectional | 108 | Mental health and substance use disorders |
| (Mazaheri Meybodi et al., 2014) | Transsexual psychiatric clinic patients with GID | Iran | Clinical | Cross-sectional | 83 | Mental health and substance use disorders |
| (Ibrahim et al., 2016) | Transgender and cisgender adult controls | Lebanon | RDS/Snowball | Cross-sectional | 20 | Mental health and substance use disorders |
| (Basar and Oz, 2016) | GD diagnosed psychiatric clinic patients | Turkey | Clinical | Cross-sectional | 116 | Mental health and substance use disorders |
| (Yildirim et al., 2017) | Children and adolescent psychiatric clinic patients with GID and a matched control group with non-GID diagnoses | Turkey | Clinical | Matched cross-sectional | 20 | Mental health and substance use disorders |
| NORTH AMERICA | ||||||
| (Chiniara et al., 2018) | Adolescents presenting to a transgender youth clinic | Canada | Clinical | Cross-sectional | 203 | Mental health and substance use disorders |
| (Drummond et al., 2018) | Assigned female sex at birth patients referred to a gender identity clinic as youth | Canada | Clinical | Prospective cohort | 25 | Mental health and substance use disorders |
| (Heard et al., 2018) | Transgender youth patients of a GD program | Canada | Clinical | Cross-sectional | 174 | Mental health and substance use disorders |
| (Rotondi et al., 2011) | Transfeminine adults | Canada | RDS/Snowball | Cross-sectional | 186 | Mental health and substance use disorders |
| (Rotondi et al., 2011) | Transmasculine adults | Canada | RDS/Snowball | Cross-sectional | 205 | Mental health and substance use disorders |
| (Williams et al., 2017) | Women and transgender/gender liminal people | Canada | Convenience | Cross-sectional | 193 | Mental health and substance use disorders |
| (Becerra-Culqui et al., 2018) | Transgender youth patients | United States | EMR | Matched cross-sectional | 1333 | Mental health and substance use disorders |
| (Beckwith et al., 2017) | HIV-positive adults with criminal justice system involvement history | United States | Convenience | Randomized controlled trial | 20 | Mental health and substance use disorders |
| (Beckwith et al., 2017) | Transgender patients at an LGBT community clinic | United States | EMR | Cross-sectional | 145 | Mental health and substance use disorders |
| (Brocksmith et al., 2018) | Pediatric endocrine clinic patients with GD diagnosis | United States | Clinical | Cross-sectional | 78 | Metabolic and endocrine disorders |
| (Brown and Jones, 2016) | Veterans | United States | EMR | Matched case-control | 5135 | Cancer; Cerebro/Cardiovascular diseases; Chronic liver and kidney disease; Mental health and substance use disorders; Metabolic and endocrine disorders; Other and unspecified diseases; Respiratory disease |
| (Chen et al., 2016) | Pediatric endocrinology clinic patients referred for GD | United States | Clinical | Retrospective cohort | 38 | Mental health and substance use disorders |
| (Cole et al., 1997) | Individuals presenting to a gender clinic with GD or transsexualism | United States | Clinical | Cross-sectional | 435 | Mental health and substance use disorders |
| (Dai and Hao, 2019) | Adults | United States | Probability-based | Cross-sectional | 669 | Cancer; Cerebro/Cardiovascular diseases; Chronic liver and kidney disease; Mental health and substance use disorders; Metabolic and endocrine disorders; Other and unspecified chronic diseases; Respiratory conditions |
| (Dawson et al., 2017) | Amazon Mechanical Turk workers | United States | Convenience | Cross-sectional | 54 | Mental health and substance use disorders |
| (Dragon et al., 2017) | Medicare beneficiaries | United States | EMR | Cross-sectional | 7454 | Cancer; Cerebro/Cardiovascular conditions; Chronic liver and kidney disease; Mental health and substance use disorders; Metabolic and endocrine disorders; Other and unspecified diseases; Respiratory disease |
| (Flentje et al., 2014) | People entering publicly funded substance abuse treatment | United States | EMR | Cross-sectional | 199 | Mental health and substance use disorders |
| (Flentje et al., 2016) | Urban homeless sexual and gender minorities | United States | Convenience | Cross-sectional | 49 | Mental health and substance use disorders; Unspecified and other diseases |
| (Gaither et al., 2017) | Transgender women patients seeking GAS from a high-volume surgeon | United States | Clinical | Cross-sectional | 330 | Cerebro/Cardiovascular diseases; Mental health and substance use disorders; Metabolic and endocrine disorders; Respiratory disease; Unspecified and other diseases |
| (Hill et al., 2016) | Transgender veterans and active duty service members | United States | Convenience | Cross-sectional | 106 | Cancer; Cerebro/Cardiovascular diseases; Mental health and substance use disorders; Metabolic and endocrine disorders; Other and unspecified diseases; Respiratory disease |
| (Hutchison et al., 2018) | Transgender patients in a state cancer registry | United States | EMR | Retrospective cohort | 230 | Cancer |
| (Jarin et al., 2017) | Adolescent patients with GD on GAHT | United States | EMR | Retrospective cohort | 116 | Mental health and substance use disorders |
| (Katz-Wise et al., 2017) | Transgender and gender non-conforming adults | United States | Convenience | Cross-sectional | 452 | Mental health and substance use disorders |
| (Katz-Wise et al., 2018) | Transgender and gender non-conforming youth and their families | United States | Convenience | Cross-sectional | 33 | Mental health and substance use disorders |
| (Keuroghlian et al., 2015) | Transgender and gender non-conforming adults | United States | Convenience | Cross-sectional | 452 | Mental health and substance use disorders |
| (Klemmer et al., 2018) | Transgender women | United States | RDS/Snowball | Cross-sectional | 233 | Mental health and substance use disorders |
| (Lindsay et al., 2016) | Transgender veterans of Iraq or Afghanistan accessing the VHA | United States | EMR | Cross-sectional | 332 | Mental health and substance use disorders |
| (Liu et al., 2019) | College students | United States | Probability-based | Cross-sectional | 301 | Mental health and substance use disorders |
| (Lothstein, 1980) | Adolescent gender identity clinic patients seeking GAS | United States | Clinical | Prospective cohort | 27 | Mental health and substance use disorders |
| (Lytle et al., 2016) | College students | United States | Probability-based | Cross-sectional | 123 | Mental health and substance use disorders |
| (Mustanski et al., 2010) | LGBT youth | United States | Convenience | Cross-sectional | 20 | Mental health and substance use disorders |
| (Nahata et al., 2017) | Transgender adolescents at an urban clinical gender program, referred for GAHT | United States | EMR | Cross-sectional | 79 | Mental health and substance use disorders |
| (Nokoff et al., 2018) | Adults | United States | Probability-based | Cross-sectional | 764 | Cerebro/Cardiovascular diseases; Metabolic and endocrine disorders |
| (Nuttbrock et al., 2015) | Transgender women | United States | Convenience | Prospective cohort | 230 | Mental health and substance use disorders |
| (Odo and Hawelu, 2001) | Native Hawaiian transgender women HIV prevention program clients and general population comparison group | United States | Clinical | Cross-sectional | 100 | Metabolic and endocrine disorders |
| (Quinn et al., 2017) | Transgender health system patients, and cisgender matched comparison group | United States | EMR | Matched cross-sectional | 6456 | Cancer; Cerebro/Cardiovascular diseases; Mental health and substance use disorders; Metabolic and endocrine disorders |
| (Qureshi et al., 2018) | LGBT adults | United States | Convenience | Cross-sectional | 27 | Cerebro/Cardiovascular diseases |
| (Reisner et al., 2013) | Transmasculine adult attendees of a transgender health conference | United States | Convenience | Cross-sectional | 73 | Mental health and substance use disorders; Metabolic and endocrine disorders; Respiratory disease |
| (Reisner et al., 2014) | Transgender men accessing STI testing at an LGBT community clinic | United States | EMR | Cross-sectional | 23 | Mental health and substance use disorders |
| (Reisner et al., 2015) | Transgender youth/young adult patients of an adolescent urban community health center, and matched cisgender controls | United States | EMR | Matched cross-sectional | 180 | Mental health and substance use disorders |
| (Reisner et al., 2016) | Young transgender women | United States | Convenience | Cross-sectional | 298 | Mental health and substance use disorders |
| (Reisner et al., 2016) | Transmasculine adults who have sex with cisgender men | United States | Convenience | Cross-sectional | 173 | Mental health and substance use disorders |
| (Seelman et al., 2017) | Transgender and gender non-conforming adults | United States | Convenience | Cross-sectional | 417 | Cerebro/Cardiovascular diseases; Mental health and substance use disorders; Metabolic and endocrine disorders; Respiratory disease |
| (Silverberg et al., 2017) | Transgender health system patients, and cisgender matched comparison group | United States | EMR | Matched retrospective cohort | 4889 | Cancer |
| (Spack et al., 2012) | Children and adolescents with GID referred for care to a multidisciplinary gender clinic | United States | Clinical | Cross-sectional | 97 | Mental health and substance use disorders |
| (Vankim et al., 2014) | College students | United States | Probability-based | Cross-sectional | 53 | Metabolic and endocrine disorders |
| (Warren et al., 2016) | LGBT adults | United States | Convenience | Cross-sectional | 208 | Metabolic and endocrine disorders |
| (White Hughto and Reisner, 2018) | Transgender and gender non-conforming older adults | United States | Convenience | Cross-sectional | 452 | Unspecified and other diseases |
| (Wilson et al., 2015) | Transgender women | United States | RDS/Snowball | Cross-sectional | 314 | Mental health and substance use disorders |
| OCEANIA | ||||||
| (Bolger et al., 2014) | Transgender men | Australia | Convenience | Cross-sectional | 279 | Mental health and substance use disorders |
| (Cheung et al., 2018) | New patients with GD at an endocrine and a primary care clinic | Australia | EMR | Cross-sectional | 540 | Cancer; Cerebro/Cardiovascular diseases; Chronic liver and kidney disease; Mental health and substance use disorders; Respiratory disease |
| (Pitts et al., 2009) | Transgender people | Multiple: Australia, New Zealand | Convenience | Cross-sectional | 253 | Mental health and substance use disorders |
| MULTIPLE/GLOBAL | ||||||
| (Witten, 2014) | Transgender adults | Multiple (24 countries including primarily United States, Canada, Australia, Sweden, United Kingdom) | RDS/Snowball | Cross-sectional | 1963 | Unspecified and other disease |
Abbreviations: STI = sexually transmitted infections; GID = Gender Identity Disorder; OBGYN = obstetrician/ gynecologist; EMR = electronic medical record; GAS = gender affirming surgery; GAHT = gender affirming hormone treatment; GD = gender dysphoria; ADHD = Attention-Deficit/ Hyperactivity Disorder; HIV = human immunodeficiency virus; LGBT = lesbian, gay, bisexual, trans; VHA = Veterans Health Administration
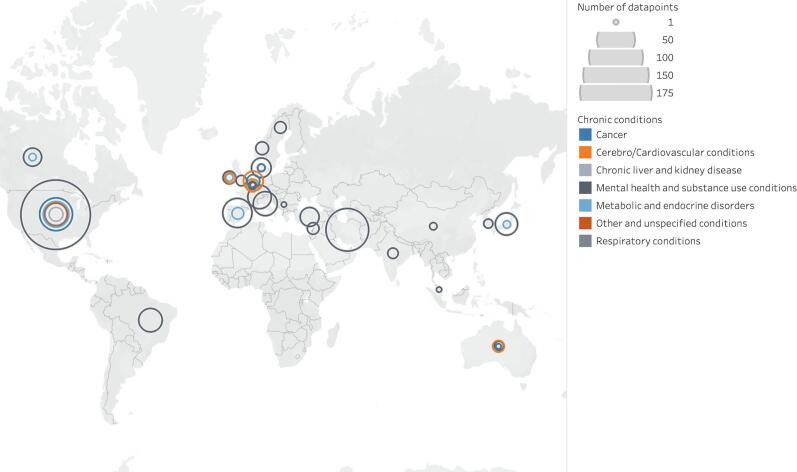
Studies were conducted primarily in the US (46%), with 6% published in Canada, 5% each in Spain and The Netherlands, and all other countries contributing less than 5% of included studies (Fig. 3). The global distribution of studies spanned Asia (6%), Europe (28%; including one study conducted in multiple countries in the region), Latin America (2%), the Middle Eastern and North African (MENA) region (6%), North America (53%), Oceania (3%; including one study conducted in multiple countries in the region); and one study spanning multiple regions (1%) conducted in 24 countries including primarily the US, Canada, Australia, Sweden and the United Kingdom. None were conducted in sub-Saharan Africa.
Fig. 3.
Global distribution of chronic disease outcomes among transgender populations.
A third of studies (33%) reported results for transgender samples without disaggregating by gender. Of those that did disaggregate by gender, nearly all included transgender women (89%) while 21% were conducted exclusively with transgender women. More than three-quarters (77%) of studies included transgender men, while 13% were conducted exclusively with transgender men. Only one study reported disaggregated chronic disease outcomes for gender non-conforming or non-binary people (2%). Included studies employed a diversity of transgender status measures, but the predominant measure was diagnosis-based ascertainment using the Diagnostic and Statistical Manual of Mental Disorders (DSM III-IV; 54%), with an additional 5% using a combination of DSM diagnoses and clinical notes. A third of included studies used an identity measure and 8% used a two-step measure that assessed sex assigned at birth and current gender (The GenIUSS Group. Best Practices for Asking Questions to Identify Transgender and Other Gender Minority Respondents on Population-Based Surveys. The Williams Institute;, 2014). The majority of studies sampled adult populations (67%), 16% were among youth, and 17% included mixed age groups.
3.3. Synthesis of results
3.3.1. Mental health and substance use disorders
Mental health and substance use disorders comprised the majority of included data (80% of studies, n = 74; 68% of datapoints, n = 455). Mood, anxiety, and substance use disorders were the most commonly studied outcomes in this category (21%, 18%, and 10% of datapoints, respectively). Overall, the lowest prevalence for mood and anxiety disorders was reported in clinical studies with some finding no prevalence among the study samples. The highest prevalence was reported in EMR studies - specifically in US studies of transgender adolescents accessing gender affirming care in an urban center, Medicare beneficiaries, and Veteran Health Administration patients (mood disorder: up to 82%; anxiety disorder: up to 67%) (Nahata et al., 2017). However, substance use disorder estimates varied more by study type, with the highest prevalence (50%) reported by a lifetime measure among transgender women (n = 20) with a gender identity diagnosis in a Swiss cross-sectional clinical study of psychiatric morbidity (Hepp et al., 2005).
3.3.2. Cerebrovascular and/or cardiovascular diseases
A total of 15% of studies (n = 14) and 11% of datapoints (n = 70) included cerebrovascular and/or cardiovascular diseases. The most commonly reported outcomes in this area were cardiovascular disease (7%), hypertension (2%), and hyperlipidemia (1%). Most datapoints in this area were provided via clinical or EMR studies (43%), with 19% from the US probability-based Behavioral Risk Factor Surveillance System (BRFSS) study (Dai and Hao, 2019, Nokoff et al., 2018), and 6% from several convenience samples. Prevalence of cardiovascular disease ranged from no cases in some studies to as high as 30% among a sample of 7,454 transgender adults in an EMR study of Medicare beneficiaries (Dragon et al., 2017). Hyperlipidemia prevalence ranged from 9% to 64%, and hypertension from less than 1% to 60%, with no discernable pattern in terms of study design, sample, gender, or chronic condition measures or definitions. Cerebrovascular disease comprised three datapoints (0.45%), and prevalence ranged from < 1% in a Netherlands EMR study of transgender people accessing GAHT (Van Kesteren et al., 1997)to 8% in a matched case-control EMR study of US veterans (Brown and Jones, 2016).
3.3.3. Cancer
Cancer outcomes were included in 12% of studies (n = 11) and 7% of datapoints (n = 47). The most reported cancer conditions were general or unspecified cancer, breast cancer, and viral infection-induced cancers, prostate cancer, and endocrine cancer (<2% of datapoints respectively). Three of the 11 studies reported incidence estimates for cancer outcomes, the remaining 73% reported prevalence exclusively. Of the studies in this area, 55% included cisgender comparators for transgender groups, with mixed evidence on the comparative cancer burden for transgender individuals, both for overall cancer morbidity and specific cancer types (i.e. some studies found cancer disparity for transgender compared to cisgender people, some did not). EMR studies provided the majority of cancer estimates (82%), and many were longitudinal studies (45%). Nearly all cancer outcomes were measured directly via provider diagnosis (i.e. in clinical or EMR studies; 91%), with the remaining measured via self-report diagnosis.
3.3.4. Metabolic and endocrine disorders
Metabolic and endocrine disorders represented 6% of datapoints (n = 38) and 22% of studies (n = 20). The most common outcome studied in this area was obesity (3% of datapoints), followed by diabetes (2%), and polycystic ovary syndrome (PCOS) and metabolic syndrome (<1% each). Diabetes prevalence ranged widely from <1% to 6% in clinical studies using self-report and provider diagnosis for condition ascertainment, to 27% to 31% in EMR studies relying on clinical diagnosis. Of the two clinical studies reporting PCOS prevalence for transgender men, one in Japan and one in Spain, estimates were comparable (32–36%) and both used the 2003 Rotterdam criteria for condition measurement (Baba et al., 2011, Becerra-Fernandez et al., 2014).
3.3.5. Respiratory disease
Respiratory diseases were included in 10% of studies (n = 9) and 3% of datapoints (n = 21). The most frequently reported respiratory outcomes were chronic lung disease (2% of datapoints) and asthma (1%). One-third of respiratory outcomes came from convenience samples, 29% EMR and probability-based samples respectively, and 10% clinical. Asthma prevalence was as high as 33% for an age-standardized estimate via self-report in a community-based convenience sample of 73 transmasculine adults attending a transgender health conference in the US (Reisner et al., 2013). Asthma prevalence was as low as 6%, via self-report in a clinical study of 330 transgender women seeking gender-affirming surgery from a high-volume US surgeon (Gaither et al., 2017).
3.3.6. Chronic liver and kidney disease
The lowest proportion of studies (5%, n = 5) and 2% of datapoints (n = 10) included chronic liver and kidney disease. All studies in this group were EMR-based except for one, using data from the probability-based BRFSS study in the US. Geographically, data was contributed from Europe, Oceania, and the US. Chronic kidney and liver disease were equally reported outcomes (0.75% of all datapoints), with prevalence estimates ranging widely from 3% by self-report provider diagnosis among transgender and gender non-conforming adults in a US probability sample (Dai and Hao, 2019), to 23% by provider diagnosis in an EMR study of transgender Medicare beneficiaries for chronic kidney disease (Dragon et al., 2017). Chronic liver disease was as high as 12% by provider diagnosis, in the same EMR Medicare study (Dragon et al., 2017). In studies that reported outcomes disaggregated by gender (40% of studies in this group), transgender women and men had a similar prevalence of chronic liver and kidney disease.
3.3.7. Other and unspecified diseases
Unspecified chronic diseases and other chronic diseases not otherwise grouped were included in 4% of datapoints (n = 24) and 13% of studies (n = 12). Arthritis and unspecified chronic diseases were the most commonly reported outcomes in this group (0.75% of datapoints each). Remaining “other” chronic diseases not included in any other group included pain disorders, osteoporosis, organic brain disorders and injuries, musculoskeletal diseases, gastroesophageal reflux disease, epilepsy, and benign prostatic hyperplasia. Of the five available arthritis datapoints, most were based on self-report diagnosis in probability-based or convenience sample surveys (80%). The remaining arthritis datapoint was the highest prevalence estimate (39%) based on a direct provider diagnosis from an EMR study of Medicare beneficiaries that included 7454 transgender patients (Dragon et al., 2017). Studies providing prevalence estimates of unspecified chronic conditions (e.g. “any chronic condition”, “chronic health condition”) used a diversity of sampling strategies but the majority were self-report measures (53%). Estimates ranged from 26% in a clinical study of 50 Dutch transgender women accessing gender-affirming hormone and surgical care (Weyers et al., 2009), to 50% among transgender women in a convenience sample from a point-in-time population count survey of 1027 homeless sexual and gender minorities in the US (Flentje et al., 2016).
4. Discussion
4.1. Summary of evidence, gaps and future directions
4.1.1. Chronic conditions
This review of global chronic disease burden among transgender populations included 93 studies and 665 datapoints, reporting on 48 unique outcomes and spanning 23 countries and four decades of research. Findings include a predominance of research on mental health. This is consistent with known trends in transgender health research (Marshall et al., 2019), including a 2016 review of the global health burden for transgender populations that found mental health to be the most commonly studied area in transgender health (31% of articles published between 2008 and 2014) and called for research focused on neglected and urgent health areas for transgender populations (e.g. physical health) (Reisner et al., 2016). Our review indicates the focus on mental health research among transgender people persists to the exclusion of other chronic disease.
The continued focus on mental health in transgender research is in part a legacy of the historical psycho-pathologization of transgender status (Bockting, 2009). Transgender-related diagnoses were only recently removed from the World Health Organization International Classification of Diseases (11th edition) chapter on mental and behavioural disorders in 2018, taking effect clinically in 2022 (GATE - » Joint Statement on ICD-11 process for trans gender diverse people. Published May 24, 2019). Hopefully, this change will contribute to a growing shift away from a disproportionate focus on the mental health of transgender people.
There is a specific need for future research on understudied chronic physical health conditions in transgender populations. This review found gaps in research on age-related chronic conditions including dementia, cancer, hypertension and osteoporosis and inflammation-related chronic illness such as cardiovascular disease, diabetes, and arthritis. For example, in addition to the elevated prevalence of cardiovascular morbidity found in a previous review (Wierckx et al., 2013), there is evidence transgender women are more likely to experience cardiovascular risk factors as well as mortality compared to cisgender adults (Asscheman et al., 2011). Future research on inflammation-related chronic physical conditions is especially relevant for transgender populations. Inflammatory processes implicated in chronic disease morbidity may be compounded by exogenous sex hormone use (an important part of gender-affirming care for many transgender people) (Scheim and Bauer, 2015), by HIV disease that disproportionately affects transgender populations (Poteat et al., 2016), and by chronic disease drivers such as stress, stigma and discrimination (DuBois et al., 2017, Jackson et al., 2010, Busse et al., 2017). The impact of GAHT on health outcomes, including chronic disease, is an important area for future research (Poteat et al., 2014).
The prevailing focus on the sexual and mental health of transgender people has ignored some conditions with a high burden among transgender populations. For example, PCOS, which was reported by only two studies in this review, may affect a third of transgender men (Baba et al., 2011, Becerra-Fernandez et al., 2014). Even within the mental health group, there is a disproportionate focus on mood, anxiety and substance use disorders, to the exclusion of other conditions such as PTSD (affecting up to 23%, in an EMR study of transgender adolescents accessing gender affirming care in a US urban center) (Nahata et al., 2017). The current review found an increase in PTSD research compared to Reisner et al.’s 2016 global health burden review (n = 24, n = 3 datapoints, respectively), but there remains disproportionally little epidemiological evidence in this area. Many studies included in the current review were broad descriptive epidemiological studies characterizing the overall health of transgender samples that further highlights the limited number of studies (n = 3) with an explicit focus on investigating the burden of specific chronic disease among transgender people.
4.1.2. Sampling and study design
Caution is warranted when interpreting prevalence estimates from the existing body of evidence. The majority of included studies were cross-sectional, within-group analyses, using non-representative sampling. Fewer than a third (28%) included cisgender comparator groups to investigate health disparity by gender identity, with only five employing matching for more robust estimates. Much of the data in this review was based on transgender populations in the US, with a predominance of EMR-based studies, primarily those conducted among Medicare beneficiaries (Proctor et al., 2016), veterans receiving care through the Veterans Health Administration system (Blosnich et al., 2013), and those insured through the Kaiser Permanente system (Quinn et al., 2017). The health of transgender individuals in these systems may not reflect the health status of the transgender general population, either in the US or in other regions. There is the need for the inclusion of core gender identity measures in nationally-representative probability-based studies (Waite and Denier, 2017, Baker, 2019).
4.1.3. Chronic disease measurement
Consistent with findings from Reisner et. al’s 2016 review (Reisner et al., 2016), heterogeneity in chronic disease measures (e.g. DSM diagnosis, structural clinical interview for mental health conditions, ICD, treatment history, clinical thresholds for physical conditions) and definitions (e.g. variety in DSM editions, ICD revisions, structured clinical interview instruments) were found in the current review of the literature. Included studies also used varied recall periods (e.g. lifetime, current, past-year, past two-years, past six-months) and prevalence measures, with more than a third (37%) reporting only frequencies and proportions. Additionally, many outcome measures were developed for use with other populations and may not have been validated for use with transgender samples (King et al., 2020). This may affect chronic disease prevalence estimates, particularly prevalence of conditions defined by sex-based clinical measures for transgender people on GAHT.
4.1.4. Transgender status measurement
This review found heterogeneity of transgender status measures across studies (e.g. DSM diagnosis, self-report) with few employing recommended two-step measures (Bauer et al., 2017). The currently evolving context of transgender measurement in clinical and EMR studies is of particular relevance given the preponderance of EMR and clinical studies in this review (Ewald et al., 2019). Studies that reported results disaggregated by gender for transgender groups largely used binary operationalizations of gender. While gender minority health research generally suffers from small sample sizes, there is a growing recognition of the diversity of lived experience among transgender populations and an urgent need for evolution in how gender identity is measured to reflect the lived realities of gender diverse people (Lagos, 2018, Reisner and Hughto, 2019, Streed et al., 2018). Gender non-conforming and non-binary people may experience mental health and substance use disparities even compared to binary-identified transgender groups (Reisner and Hughto, 2019, Streed et al., 2018). Rigorous, standardized transgender status measurement that reflects population gender diversity is key for future research.
4.2. Limitations
The results of this review should be considered in light of its limitations. Importantly, this review sought to map the available evidence in the area of chronic disease among global transgender populations, employing narrative synthesis largely at the datapoint level. As such, this review did not endeavor to synthesize or meta-analyze chronic disease prevalence estimates and thus results may be limited in the extent to which they can inform direct clinical practice. The primary intent was to identify research gaps and evidence needs. Findings may also have been skewed by the ability of one study with many datapoints to disproportionately contribute data to this synthesis. In this review of published studies reporting quantitative prevalence estimates for transgender populations. there was also heterogeneity of quality of evidence, including in study design and prevalence measures used across studies. As such, evidence from this review may be susceptible to information and selection bias, threatening study validity, speaking to the need for more rigorous epidemiological research. Though, importantly, the quality of the captured studies does not negate the identification of significant research gaps and evidence needs with regards to chronic disease, particularly physical chronic disease.
Finally, the focus of this synthesis was on chronic disease outcomes and not chronic disease risk factors. Only 40% (n = 37) of studies in this review reported significant correlates of chronic disease, including sociodemographics (e.g. sexual orientation, gender, age, race/ethnicity, socioeconomic status, country of origin) and psychosocial factors (e.g. history of violence, lifetime suicidal ideation), as well as trans-specific factors (e.g. experiences of transphobic victimization, access to a trans-affirming healthcare provider, social/medical transition status). A growing number of studies have demonstrated the importance of stigma, healthcare access, violence and syndemic or co-occurring factors in shaping health outcomes for transgender people (Reisner et al., 2016, Poteat et al., 2016, White Hughto et al., 2015). Future research is needed that can shed light on these drivers of disease burden, as well as the moderating and mediating impacts of intersecting social locations. Specifically, only approximately half (48%) of studies in this review reported race or ethnicity characteristics of the study sample, though, 22% of included studies were conducted in countries with majority or entirely non-white samples. Given evidence of racial disparities in chronic mental and physical health for transgender people, (Brown and Jones, 2014)the intersection of race, ethnicity, and gender diversity is an important area of focus for future chronic disease research.
4.3. Conclusions
This systematic review makes an important contribution as the first to focus on chronic disease among global transgender populations. Findings from this review point to a number of critical gaps in the existing transgender health literature landscape in terms of chronic disease burden knowledge, and important areas for future research. In particular, there is a need for research in areas other than sexual and mental health (Reisner et al., 2016), areas with unique vulnerability for transgender people such as inflammation-related disease, and areas with little evidence to date such as age-related chronic conditions. There is also a need for well-designed longitudinal studies (particularly important for incident cancer and other age-related conditions); research making use of large, population-representative data and appropriate comparison groups (Reisner et al., 2016), and use of consistent measurement for both transgender status (Reisner et al., 2016) and chronic disease ascertainment (Swartz et al., 2019). The alignment of funding mechanisms to these research priorities is fundamental to continued progress in transgender chronic health research. Finally, research with an explicit focus on chronic disease in transgender populations, including multimorbidity, is warranted (Swartz et al., 2019), as well as studies designed to investigate multi-level drivers of chronic disease burden. Given links between factors such as poverty, stigma, discrimination and barriers to healthcare access for transgender people (Reisner et al., 2016, Poteat et al., 2016, White Hughto et al., 2015), future research in this area should be rigorously designed to enable disentangling of the effects of these important determinants of health and point to opportunities for multi-level interventions to attenuate their effects in transgender populations.
Funding
AJR is supported by a Frederick Banting and Charles Best Doctoral Research Award from the Canadian Institutes of Health Research (#152382).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101259.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Aghabikloo A., Bahrami M., Saberi S.M., Emamhadi M.A. Gender identity disorders in Iran; request for sex reassignment surgery. Int. J. Med. Toxicol. Forensic Med. 2012;2(4):128–134. [Google Scholar]
- Asscheman H., Giltay E.J., Megens J.A., de Ronde W.P., van Trotsenburg M.A., Gooren L.J. A long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. Eur. J. Endocrinol. 2011;164(4):635–642. doi: 10.1530/EJE-10-1038. [DOI] [PubMed] [Google Scholar]
- Baba T., Endo T., Ikeda K. Distinctive features of female-to-male transsexualism and prevalence of gender identity disorder in Japan. J. Sex. Med. 2011;8(6):1686–1693. doi: 10.1111/j.1743-6109.2011.02252.x. [DOI] [PubMed] [Google Scholar]
- Baker, K., 2019. Leveraging the Behavioural Risk Factor Surveillance System for Transgender Health Research. In: 2019. Accessed March 17, 2020. https://apha.confex.com/apha/2019/meetingapi.cgi/Paper/452150?filename=2019_Abstract452150.html&template=Word.
- Baral S.D., Poteat T., Strömdahl S., Wirtz A.L., Guadamuz T.E., Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infectious Dis. 2013;13(3):214–222. doi: 10.1016/S1473-3099(12)70315-8. [DOI] [PubMed] [Google Scholar]
- Basar K., Oz G. Resilience in individuals with Gender Dysphoria: association with perceived social support and discrimination. Turk. J. Psychiatry. 2016 doi: 10.5080/u17071. [DOI] [PubMed] [Google Scholar]
- Bauer, G.R., Braimoh, J., Scheim, A.I., Dharma, C., 2017. Transgender-inclusive measures of sex/gender for population surveys: Mixed-methods evaluation and recommendations. PLOS ONE 12(5):e0178043. [DOI] [PMC free article] [PubMed]
- Becasen J.S., Denard C.L., Mullins M.M., Higa D.H., Sipe T.A. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006–2017. Am J Public Health. 2019;109(1):e1–e8. doi: 10.2105/AJPH.2018.304727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becerra-Culqui T.A., Liu Y., Nash R. Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics. 2018;141(5):e20173845. doi: 10.1542/peds.2017-3845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becerra-Fernandez A., Perez-Lopez G., Roman M.M. Prevalence of hyperandrogenism and polycystic ovary syndrome in female to male transsexuals. Endocrinol. Nutr. 2014;61(7):351–358. doi: 10.1016/j.endonu.2014.01.010. [DOI] [PubMed] [Google Scholar]
- Beckwith, C., Castonguay, B.U., Trezza, C., et al., 2017. Gender differences in HIV care among criminal justice-involved persons: Baseline data from the CARE+ corrections study. PLoS ONE. 12(1):e0169078. DOI:10.1371/journal.pone.0169078. [DOI] [PMC free article] [PubMed]
- Beckwith N., Reisner S.L., Zaslow S., Mayer K.H., Keuroghlian A.S. Factors associated with gender-affirming surgery and age of hormone therapy initiation among transgender adults. Transgender Health. 2017;2(1):156–164. doi: 10.1089/trgh.2017.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergero-Miguel T., García-Encinas M.A., Villena-Jimena A. Gender dysphoria and social anxiety: an exploratory study in Spain. J. Sex. Med. 2016;13(8):1270–1278. doi: 10.1016/j.jsxm.2016.05.009. [DOI] [PubMed] [Google Scholar]
- Blosnich J.R., Brown G.R., Shipherd, PhD J.C., Kauth M., Piegari R.I., Bossarte R.M. Prevalence of gender identity disorder and suicide risk among transgender veterans utilizing veterans health administration care. Am. J. Public Health. 2013;103(10):e27–e32. doi: 10.2105/AJPH.2013.301507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blosnich J.R., Marsiglio M.C., Dichter M.E. Impact of social determinants of health on medical conditions among transgender veterans. Am. J. Prev. Med. 2017;52(4):491–498. doi: 10.1016/j.amepre.2016.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bockting W.O. Transforming the paradigm of transgender health: a field in transition. Sex. Relationship Ther. 2009;24(2):103–107. doi: 10.1080/14681990903037660. [DOI] [Google Scholar]
- Bodlund O., Kullgren G. Transsexualism—General outcome and prognostic factors: a five-year follow-up study of nineteen transsexuals in the process of changing sex. Arch. Sex. Behav. 1996;25(3):303–316. doi: 10.1007/BF02438167. [DOI] [PubMed] [Google Scholar]
- Bolger A., Jones T., Dunstan D., Lykins A. Australian trans men: development, sexuality, and mental health: Australian trans men. Australian Psychol. 2014;49(6):395–402. doi: 10.1111/ap.12094. [DOI] [Google Scholar]
- Brocksmith V.M., Alradadi R.S., Chen M., Eugster E.A. Baseline characteristics of gender dysphoric youth. J. Pediatr. Endocrinol. Metab. 2018;31(12):1367–1369. doi: 10.1515/jpem-2018-0250. [DOI] [PubMed] [Google Scholar]
- Brown G.R., Jones K.T. Racial health disparities in a cohort of 5,135 transgender veterans. J. Racial Ethnic Health Disparities. 2014;1(4):257–266. doi: 10.1007/s40615-014-0032-4. [DOI] [Google Scholar]
- Brown G.R., Jones K.T. Mental health and medical health disparities in 5135 transgender veterans receiving healthcare in the veterans health administration: a case–control study. LGBT Health. 2016;3(2):122–131. doi: 10.1089/lgbt.2015.0058. [DOI] [PubMed] [Google Scholar]
- Busse D., Yim I.S., Campos B. Social context matters: ethnicity, discrimination and stress reactivity. Psychoneuroendocrinology. 2017;83(Supplement C):187–193. doi: 10.1016/j.psyneuen.2017.05.025. [DOI] [PubMed] [Google Scholar]
- Chen M., Fuqua J., Eugster E.A. Characteristics of referrals for gender dysphoria over a 13-year period. J. Adolesc. Health. 2016;58(3):369–371. doi: 10.1016/j.jadohealth.2015.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Zhu X., Wright L. Suicidal ideation and attempted suicide amongst Chinese transgender persons: national population study. J. Affect. Disord. 2019;245:1126–1134. doi: 10.1016/j.jad.2018.12.011. [DOI] [PubMed] [Google Scholar]
- Cheung A.S., Ooi O., Leemaqz S. Sociodemographic and clinical characteristics of transgender adults in Australia. Transgender Health. 2018;3(1):229–238. doi: 10.1089/trgh.2018.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiniara L., Bonifacio H., Palmert M. Characteristics of adolescents referred to a gender clinic: are youth seen now different from those in initial reports? Horm. Res. Paediatr. 2018;89(6):434–441. doi: 10.1159/000489608. [DOI] [PubMed] [Google Scholar]
- Cole C.M., O’Boyle M., Emory L.E., Meyer W.J., III Comorbidity of gender dysphoria and other major psychiatric diagnoses. Arch. Sex Behav. 1997;26(1):13–26. doi: 10.1023/A:1024517302481. [DOI] [PubMed] [Google Scholar]
- Colizzi M., Costa R., Todarello O. Transsexual patients’ psychiatric comorbidity and positive effect of cross-sex hormonal treatment on mental health: results from a longitudinal study. Psychoneuroendocrinology. 2014;39:65–73. doi: 10.1016/j.psyneuen.2013.09.029. [DOI] [PubMed] [Google Scholar]
- Cuypere G., Jannes C., Rubens R. Psychosocial functioning of transsexuals in Belgium. Acta Psychiatr. Scand. 1995;91(3):180–184. doi: 10.1111/j.1600-0447.1995.tb09763.x. [DOI] [PubMed] [Google Scholar]
- Dai H., Hao J. Sleep deprivation and chronic health conditions among sexual minority adults. Behav. Sleep Med. 2019;17(3):254–268. doi: 10.1080/15402002.2017.1342166. [DOI] [PubMed] [Google Scholar]
- Dawson A.E., Wymbs B.T., Gidycz C.A., Pride M., Figueroa W. Exploring rates of transgender individuals and mental health concerns in an online sample. Int. J. Transgenderism. 2017;18(3):295–304. doi: 10.1080/15532739.2017.1314797. [DOI] [Google Scholar]
- de Vries, A.L.C., Doreleijers, T.A.H., Steensma, T.D., Cohen-Kettenis, P.T., 2011. Psychiatric comorbidity in gender dysphoric adolescents. J Child Psychol Psychiatry 52(11):1195-1202. DOI:10.1111/j.1469-7610.2011.02426.x. [DOI] [PubMed]
- Defreyne J., De Bacquer D., Shadid S., Lapauw B., T’Sjoen G. Is type 1 diabetes mellitus more prevalent than expected in transgender persons? A local observation. Sex. Med. 2017;5(3):e215–e218. doi: 10.1016/j.esxm.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downing J.M., Przedworski J.M. Health of transgender adults in the U.S., 2014–2016. Am. J. Prev. Med. 2018;55(3):336–344. doi: 10.1016/j.amepre.2018.04.045. [DOI] [PubMed] [Google Scholar]
- Dragon C.N., Guerino P., Ewald E., Laffan A.M. Transgender medicare beneficiaries and chronic conditions: exploring fee-for-service claims data. LGBT Health. 2017;4(6):404–411. doi: 10.1089/lgbt.2016.0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond K.D., Bradley S.J., Peterson-Badali M., VanderLaan D.P., Zucker K.J. Behavior problems and psychiatric diagnoses in girls with gender identity disorder: a follow-up study. J. Sex Marital Ther. 2018;44(2):172–187. doi: 10.1080/0092623X.2017.1340382. [DOI] [PubMed] [Google Scholar]
- DuBois L.Z., Powers S., Everett B.G., Juster R.-P. Stigma and diurnal cortisol among transitioning transgender men. Psychoneuroendocrinology. 2017;82:59–66. doi: 10.1016/j.psyneuen.2017.05.008. [DOI] [PubMed] [Google Scholar]
- Duišin D., Batinić B., Barišić J., Djordjevic M.L., Vujović S., Bizic M. Personality disorders in persons with gender identity disorder. Sci. World J. 2014;2014:1–7. doi: 10.1155/2014/809058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewald E.R., Guerino P., Dragon C., Laffan A.M., Goldstein Z., Streed C., Jr. Identifying medicare beneficiaries accessing transgender-related care in the Era of ICD-10. LGBT Health. 2019;6(4):166–173. doi: 10.1089/lgbt.2018.0175. [DOI] [PubMed] [Google Scholar]
- Fisher A.D., Bandini E., Casale H., Ferruccio N., Meriggiola M.C., Gualerzi A., Manieri C., Jannini E., Mannucci E., Monami M., Stomaci N., Delle Rose A., Susini T., Ricca V., Maggi M. Sociodemographic and clinical features of gender identity disorder: an Italian multicentric evaluation. J. Sex. Med. 2013;10(2):408–419. doi: 10.1111/j.1743-6109.2012.03006.x. [DOI] [PubMed] [Google Scholar]
- Flentje A., Heck N.C., Sorensen J.L. Characteristics of transgender individuals entering substance abuse treatment. Addict. Behav. 2014;39(5):969–975. doi: 10.1016/j.addbeh.2014.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flentje A., Leon A., Carrico A., Zheng D., Dilley J. Mental and physical health among homeless sexual and gender minorities in a major urban US City. J. Urban Health. 2016;93(6):997–1009. doi: 10.1007/s11524-016-0084-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanari A.M.V., Rovaris D.L., Costa A.B., Pasley A., Cupertino R.B., Soll B.M.B., Schwarz K., da Silva D.C., Borba A.O., Mueller A., Bau C.H.D., Lobato M.I.R. Childhood maltreatment linked with a deterioration of psychosocial outcomes in adult life for Southern Brazilian transgender women. J. Immigrant Minority Health. 2018;20(1):33–43. doi: 10.1007/s10903-016-0528-6. [DOI] [PubMed] [Google Scholar]
- Forouzanfar M.H., Afshin A., Alexander L.T. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaither T.W., Awad M.A., Osterberg E.C., Romero A., Bowers M.L., Breyer B.N. Impact of sexual orientation identity on medical morbidities in male-to-female transgender patients. LGBT Health. 2017;4(1):11–16. doi: 10.1089/lgbt.2016.0097. [DOI] [PubMed] [Google Scholar]
- GATE - » Joint Statement on ICD-11 process for trans & gender diverse people. Published May 24, 2019. Accessed March 16, 2020. https://transactivists.org/icd-11-trans-process/.
- Gómez-Gil E., Trilla A., Salamero M., Godás T., Valdés M. Sociodemographic, clinical, and psychiatric characteristics of transsexuals from Spain. Arch. Sex. Behav. 2009;38(3):378–392. doi: 10.1007/s10508-007-9307-8. [DOI] [PubMed] [Google Scholar]
- Gooren L., Morgentaler A. Prostate cancer incidence in orchidectomised male-to-female transsexual persons treated with oestrogens. Andrologia. 2014;46(10):1156–1160. doi: 10.1111/and.12208. [DOI] [PubMed] [Google Scholar]
- Gooren L.J., van Trotsenburg M.A.A., Giltay E.J., van Diest P.J. Breast cancer development in transsexual subjects receiving cross-sex hormone treatment. J. Sex. Med. 2013;10(12):3129–3134. doi: 10.1111/jsm.12319. [DOI] [PubMed] [Google Scholar]
- Guzmán-Parra J., Sánchez-Álvarez N., de Diego-Otero Y. Sociodemographic characteristics and psychological adjustment among transsexuals in Spain. Arch. Sex. Behav. 2016;45(3):587–596. doi: 10.1007/s10508-015-0557-6. [DOI] [PubMed] [Google Scholar]
- Haraldsen I., Dahl A. Symptom profiles of gender dysphoric patients of transsexual type compared to patients with personality disorders and healthy adults. Acta Psychiatr. Scand. 2000;102(4):276–281. doi: 10.1034/j.1600-0447.2000.102004276.x. [DOI] [PubMed] [Google Scholar]
- Havar E.S., Hassanzadeh R., Moshkani M., Kaboosi A., Yasrebi K. Personality disorders and psychiatric comorbidity among persons with gender identity disorder. J. Indian Acad. Appl. Psychol. 2015;41(3):142–148. [Google Scholar]
- Heard, J., Morris, A., Kirouac, N., Ducharme, J., Trepel, S., Wicklow, B., 2018. Gender dysphoria assessment and action for youth: Review of health care services and experiences of trans youth in Manitoba. Paediatr Child Health 1205-7088 23(3):179-184. DOI:10.1093/pch/pxx156. [DOI] [PMC free article] [PubMed]
- Hepp U., Kraemer B., Schnyder U., Miller N., Delsignore A. Psychiatric comorbidity in gender identity disorder. J. Psychosom. Res. 2005;58(3):259–261. doi: 10.1016/j.jpsychores.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Herbst J.H., Jacobs E.D., Finlayson T.J., McKleroy V.S., Neumann M.S., Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- Heylens G., Elaut E., Kreukels B.P.C. Psychiatric characteristics in transsexual individuals: multicentre study in four European countries. Br. J. Psychiatry. 2014;204(2):151–156. doi: 10.1192/bjp.bp.112.121954. [DOI] [PubMed] [Google Scholar]
- Hill B.J., Bouris A., Barnett J.T., Walker D. Fit to serve? Exploring mental and physical health and well-being among transgender active-duty service members and veterans in the U.S. Military. Transgender Health. 2016;1(1):4–11. doi: 10.1089/trgh.2015.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt V., Skagerberg E., Dunsford M. Young people with features of gender dysphoria: demographics and associated difficulties. Clin. Child Psychol. Psychiatry. 2016;21(1):108–118. doi: 10.1177/1359104514558431. [DOI] [PubMed] [Google Scholar]
- Hoshiai, M., Matsumoto, Y., Sato, T., et al., 2010. Psychiatric comorbidity among patients with gender identity disorder. Psychiatry Clin Neurosci. 64(5):514-519. [DOI] [PubMed]
- Hutchison L.M., Boscoe F.P., Feingold B.J. Cancers disproportionately affecting the New York state transgender population, 1979–2016. Am. J. Public Health. 2018;108(9):1260–1262. doi: 10.2105/AJPH.2018.304560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim C., Haddad R., Richa S. Les comorbidités psychiatriques dans le transsexualisme: Étude sur une population de transgenres Libanais = Psychiatric comorbidities in transsexualism: Study of a Lebanese transgender population. Encéphale Rev Psychiatr Clin Biol Thérapeutique. 2016;42(6):517–522. doi: 10.1016/j.encep.2016.02.011. [DOI] [PubMed] [Google Scholar]
- IOM (Institute of Medicine). The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding.; 2011. [PubMed]
- Jackson J.S., Knight K.M., Rafferty J.A. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am. J. Public Health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarin J., Pine-Twaddell E., Trotman G., Stevens J., Conard L.A., Tefera E., Gomez-Lobo V. Cross-sex hormones and metabolic parameters in adolescents with gender dysphoria. Pediatrics. 2017;139(5):e20163173. doi: 10.1542/peds.2016-3173. [DOI] [PubMed] [Google Scholar]
- Judge C., O’Donovan C., Callaghan G., Gaoatswe G., O’Shea D. Gender dysphoria - prevalence and co-morbidities in an Irish adult population. Front. Endocrinol. 2014;5(JUN):87. doi: 10.3389/fendo.2014.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalra G., Shah N. The cultural, psychiatric, and sexuality aspects of Hijras in India. Int. J. Transgenderism. 2013;14(4):171–181. doi: 10.1080/15532739.2013.876378. [DOI] [Google Scholar]
- Katz-Wise S.L., Reisner S.L., White Hughto J.M., Budge S.L. Self-reported changes in attractions and social determinants of mental health in transgender adults. Arch. Sex Behav. 2017;46(5):1425–1439. doi: 10.1007/s10508-016-0812-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz-Wise S.L., Ehrensaft D., Vetters R., Forcier M., Austin S.B. Family functioning and mental health of transgender and gender-nonconforming youth in the trans teen and family narratives project. J. Sex Res. 2018;55(4-5):582–590. doi: 10.1080/00224499.2017.1415291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keuroghlian A.S., Reisner S.L., White J.M., Weiss R.D. Substance use and treatment of substance use disorders in a community sample of transgender adults. Drug Alcohol Depend. 2015;152:139–146. doi: 10.1016/j.drugalcdep.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King W.M., Hughto J.M.W., Operario D. Transgender stigma: a critical scoping review of definitions, domains, and measures used in empirical research. Soc. Sci. Med. 2020;250:112867. doi: 10.1016/j.socscimed.2020.112867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivimäki M., Vineis P., Brunner E.J. How can we reduce the global burden of disease? Lancet. 2015;386(10010):2235–2237. doi: 10.1016/S0140-6736(15)00129-4. [DOI] [PubMed] [Google Scholar]
- Klemmer, C.L., Arayasirikul, S., Raymond, H.F., 2018. Transphobia-based violence, depression, and anxiety in transgender women: The role of body satisfaction. J Interpers Violence. Published online March 11, 088626051876001. DOI:10.1177/0886260518760015. [DOI] [PubMed]
- Lagos D. Looking at population health beyond “male” and “female”: implications of transgender identity and gender nonconformity for population health. Demography. 2018;55(6):2097–2117. doi: 10.1007/s13524-018-0714-3. [DOI] [PubMed] [Google Scholar]
- Lim H.H., Jang Y.H., Choi G.Y., Lee J.J., Lee E.S. Gender affirmative care of transgender people: a single center’s experience in Korea. Obstet. Gynecol. Sci. 2019;62(1):46–55. doi: 10.5468/ogs.2019.62.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay J.A., Keo-Meier C., Hudson S., Walder A., Martin L.A., Kauth M.R. Mental health of transgender veterans of the Iraq and Afghanistan conflicts who experienced military sexual trauma: MST and mental health of transgender veterans. J. Trauma. Stress. 2016;29(6):563–567. doi: 10.1002/jts.22146. [DOI] [PubMed] [Google Scholar]
- Liu C.H., Stevens C., Wong S.H.M., Yasui M., Chen J.A. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: Implications for addressing disparities in service use. Depress Anxiety. 2019;36(1):8–17. doi: 10.1002/da.22830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobato M.I., Koff W.J., Schestatsky S.S., Chaves C.P.d.V., Petry A., Crestana T., Amaral J.T., Onófrio F.d.Q., Salvador J., Silveira E., Henriques A.A. Clinical characteristics, psychiatric comorbidities and sociodemographic profile of transsexual patients from an outpatient clinic in Brazil. Int. J. Transgenderism. 2007;10(2):69–77. doi: 10.1080/15532730802175148. [DOI] [Google Scholar]
- Lothstein L.M. The adolescent gender dysphoric patient: an approach to treatment and management. J. Pediatr. Psychol. 1980;5(1):93–109. doi: 10.1093/jpepsy/5.1.93. [DOI] [PubMed] [Google Scholar]
- Lytle M.C., Blosnich J.R., Kamen C. The association of multiple identities with self-directed violence and depression among transgender individuals. Suicide Life Threat. Behav. 2016;46(5):535–544. doi: 10.1111/sltb.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCarthy S., Poteat T., Xia Z. Current research gaps: a global systematic review of HIV and sexually transmissible infections among transgender populations. Sex. Health. 2017;14(5):456. doi: 10.1071/SH17096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madeddu F., Prunas A., Hartmann D. Prevalence of axis II disorders in a sample of clients undertaking psychiatric evaluation for sex reassignment surgery. Psychiatr. Q. 2009;80(4):261–267. doi: 10.1007/s11126-009-9114-6. [DOI] [PubMed] [Google Scholar]
- Marshall Z., Welch V., Minichiello A., Swab M., Brunger F., Kaposy C. Documenting Research with Transgender, Nonbinary, and Other Gender Diverse (Trans) individuals and communities: introducing the global trans research evidence map. Transgender Health. 2019;4(1):68–80. doi: 10.1089/trgh.2018.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazaheri Meybodi A., Hajebi A., Ghanbari Jolfaei A. Psychiatric axis I comorbidities among patients with gender dysphoria. Psychiatry J. 2014;2014:1–5. doi: 10.1155/2014/971814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Mustanski B.S., Garofalo R., Emerson E.M. Mental health disorders, psychological distress, and suicidality in a diverse sample of Lesbian, Gay, Bisexual, and Transgender Youths. Am. J. Public Health. 2010;100(12):2426–2432. doi: 10.2105/AJPH.2009.178319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahata L., Quinn G.P., Caltabellotta N.M., Tishelman A.C. Mental health concerns and insurance denials among transgender adolescents. LGBT Health. 2017;4(3):188–193. doi: 10.1089/lgbt.2016.0151. [DOI] [PubMed] [Google Scholar]
- Nokoff N.J., Scarbro S., Juarez-Colunga E., Moreau K.L., Kempe A. Health and cardiometabolic disease in transgender adults in the United States: Behavioral Risk Factor Surveillance System 2015. J. Endocr. Soc. 2018;2(4):349–360. doi: 10.1210/JS.2017-00465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuttbrock, L., Bockting, W., Rosenblum, A., et al., 2015. Transgender community involvement and the psychological impact of abuse among transgender women. Psychol Sex Orientat Gend Divers. 2(4):386-390. DOI:10.1037/sgd0000126.
- Odo C., Hawelu A. Eo Na Mahu o Hawai’i: the extraordinary health needs of Hawai’i’s Mahu. Pac Health Dialog. 2001;8(2):327–334. [PubMed] [Google Scholar]
- Pitts M.K., Couch M., Mulcare H., Croy S., Mitchell A. Transgender People in Australia and New Zealand: health, well-being and access to health services. Feminism Psychol. 2009;19(4):475–495. doi: 10.1177/0959353509342771. [DOI] [Google Scholar]
- Popay, J., Roberts, H., Sowden, A., et al., 2006. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product from the ESRC Methods Programme. Lancaster University; DOI:10.13140/2.1.1018.4643.
- Poteat T., Reisner S.L., Radix A. HIV epidemics among transgender women. Curr. Opin. HIV AIDS. 2014;9(2):168–173. doi: 10.1097/COH.0000000000000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat T., Scheim A., Xavier J., Reisner S., Baral S. Global Epidemiology of HIV infection and related syndemics affecting transgender people. J. Acquir. Immune Defic. Syndr. 2016;72:S210–S219. doi: 10.1097/QAI.0000000000001087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor K., Haffer S.C., Ewald E., Hodge C., James C.V. Identifying the transgender population in the medicare program. Transgender Health. 2016;1(1):250–265. doi: 10.1089/trgh.2016.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn V.P., Nash R., Hunkeler E. Cohort profile: Study of Transition, Outcomes and Gender (STRONG) to assess health status of transgender people. BMJ Open. 2017;7(12):e018121. doi: 10.1136/bmjopen-2017-018121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qureshi R.I., Zha P., Kim S., Hindin P., Naqvi Z., Holly C., Dubbs W., Ritch W. Health care needs and care utilization among lesbian, gay, bisexual, and transgender populations in New Jersey. J. Homosex. 2018;65(2):167–180. doi: 10.1080/00918369.2017.1311555. [DOI] [PubMed] [Google Scholar]
- Reisner, S.L., Hughto, J.M.W., 2019. Comparing the health of non-binary and binary transgender adults in a statewide non-probability sample. in: Shiu C-S, ed. PLOS ONE.14(8):e0221583. DOI:10.1371/journal.pone.0221583. [DOI] [PMC free article] [PubMed]
- Reisner S.L., Gamarel K.E., Dunham E., Hopwood R., Hwahng S. Female-to-male transmasculine adult health: a mixed-methods community-based needs assessment. J. Am. Psychiatr. Nurses Assoc. 2013;19(5):293–303. doi: 10.1177/1078390313500693. [DOI] [PubMed] [Google Scholar]
- Reisner S.L., White J.M., Mayer K.H., Mimiaga M.J. Sexual risk behaviors and psychosocial health concerns of female-to-male transgender men screening for STDs at an urban community health center. AIDS Care. 2014;26(7):857–864. doi: 10.1080/09540121.2013.855701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner S.L., Vetters R., Leclerc M., Zaslow S., Wolfrum S., Shumer D., Mimiaga M.J. Mental health of transgender youth in care at an adolescent urban community health center: a matched retrospective cohort study. J. Adolesc. Health. 2015;56(3):274–279. doi: 10.1016/j.jadohealth.2014.10.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner S.L., White Hughto J.M., Pardee D., Sevelius J. Syndemics and gender affirmation: HIV sexual risk in female-to-male trans masculine adults reporting sexual contact with cisgender males. Int. J. STD AIDS. 2016;27(11):955–966. doi: 10.1177/0956462415602418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner S.L., Murchison G.R. A global research synthesis of HIV and STI biobehavioural risks in female-to-male transgender adults. Global Public Health. 2016;11(7-8):866–887. doi: 10.1080/17441692.2015.1134613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner S.L., Poteat T., Keatley J. Global health burden and needs of transgender populations: a review. Lancet. 2016;388(10042):412–436. doi: 10.1016/S0140-6736(16)00684-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner S.L., Biello K.B., White Hughto J.M. Psychiatric diagnoses and comorbidities in a diverse, multicity cohort of young transgender women: baseline findings from project lifeskills. JAMA Pediatr. 2016;170(5):481. doi: 10.1001/jamapediatrics.2016.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner S.L., Radix A., Deutsch M.B. Integrated and gender-affirming transgender clinical care and research. J. Acquired Immune Defic. Syndr. 2016;72:S235–S242. doi: 10.1097/QAI.0000000000001088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotondi N.K., Bauer G.R., Travers R., Travers A., Scanlon K., Kaay M. Depression in male-to-female transgender ontarians: results from the Trans PULSE Project. Can. J. Community Mental Health. 2011;30(2):113–133. [Google Scholar]
- Rotondi N.K., Bauer G.R., Scanlon K., Kaay M., Travers R., Travers A. Prevalence of and risk and protective factors for depression in female-to-male transgender Ontarians: results from the Trans PULSE Project. Can. J. Commun. Ment. Health. 2011;30(2):135–155. doi: 10.7870/cjcmh-2011-0021. [DOI] [Google Scholar]
- Rutledge R., Morozova O., Gibson B.A., Altice F.L., Kamarulzaman A., Wickersham J.A. Correlates of recent HIV testing among transgender women in Greater Kuala Lumpur, Malaysia. LGBT Health. 2018;5(8):484–493. doi: 10.1089/lgbt.2018.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheim A.I., Bauer G.R. Sex and gender diversity among transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. J. Sex Res. 2015;52(1):1–14. doi: 10.1080/00224499.2014.893553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seelman K.L., Colón-Diaz M.J.P., LeCroix R.H., Xavier-Brier M., Kattari L. Transgender noninclusive healthcare and delaying care because of fear: connections to general health and mental health among transgender adults. Transgender Health. 2017;2(1):17–28. doi: 10.1089/trgh.2016.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seelman K.L., Young S.R., Tesene M., Alvarez-Hernandez L.R., Kattari L. A comparison of health disparities among transgender adults in Colorado (USA) by race and income. Int. J. Transgenderism. 2017;18(2):199–214. doi: 10.1080/15532739.2016.1252300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverberg M.J., Nash R., Becerra-Culqui T.A. Cohort study of cancer risk among insured transgender people. Ann. Epidemiol. 2017;27(8):499–501. doi: 10.1016/j.annepidem.2017.07.007. [DOI] [PubMed] [Google Scholar]
- Simonsen R.K., Giraldi A., Kristensen E., Hald G.M. Long-term follow-up of individuals undergoing sex reassignment surgery: Psychiatric morbidity and mortality. Nord. J. Psychiatry. 2016;70(4):241–247. doi: 10.3109/08039488.2015.1081405. [DOI] [PubMed] [Google Scholar]
- Simonsen R.K., Hald G.M., Kristensen E., Giraldi A. Long-term follow-pp of individuals undergoing sex-reassignment surgery: Somatic morbidity and cause of death. Sex. Med. 2016;4(1):e60–e68. doi: 10.1016/j.esxm.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spack N.P., Edwards-Leeper L., Feldman H.A., Leibowitz S., Mandel F., Diamond D.A., Vance S.R. Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics. 2012;129(3):418–425. doi: 10.1542/peds.2011-0907. [DOI] [PubMed] [Google Scholar]
- Streed C.G., Jr., Harfouch O., Marvel F., Blumenthal R.S., Martin S.S., Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: a narrative review. Ann. Intern. Med. 2017;167(4):256. doi: 10.7326/M17-0577. [DOI] [PubMed] [Google Scholar]
- Streed C.G., Jr., McCarthy E.P., Haas J.S. Self-reported physical and mental health of gender nonconforming transgender adults in the United States. LGBT Health. 2018;5(7):443–448. doi: 10.1089/lgbt.2017.0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuckler D. Population causes and consequences of deading chronic diseases: a comparative analysis of prevailing explanations. Milbank Q. 2008;86(2):273–326. doi: 10.1111/j.1468-0009.2008.00522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz, J.A., Ducheny, K., Holloway, T., Stokes, L., Willis, S., Kuhns, L.M., 2019. A latent class analysis of chronic health conditions among HIV-Positive transgender women of color. AIDS Behav. Published online May 29, DOI:10.1007/s10461-019-02543-3. [DOI] [PubMed]
- The GenIUSS Group. Best Practices for Asking Questions to Identify Transgender and Other Gender Minority Respondents on Population-Based Surveys. The Williams Institute; 2014.
- Van Kesteren P.J.M., Asscheman H., Megens J.A.J., Gooren L.J.G. Mortality and morbidity in transsexual subjects treated with cross-sex hormones. Clin. Endocrinol. 1997;47(3):337–343. doi: 10.1046/j.1365-2265.1997.2601068.x. [DOI] [PubMed] [Google Scholar]
- Vankim N.A., Erickson D.J., Eisenberg M.E., Lust K., Rosser B.R.S., Laska M.N. Weight-related disparities for transgender college students. Health Behav. Policy Rev. 2014;1(2):161–171. doi: 10.14485/HBPR.1.2.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilas M.V.A., Rubalcava G., Becerra A., Para M.C.M. Nutritional status and obesity prevalence in people with gender dysphoria. AIMS Public Health. 2014;1(3):137–146. doi: 10.3934/publichealth.2014.3.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite, S., Denier, N., 2017. Data and discrimination: A research note on sexual orientation in the Canadian labour market. Can Stud Popul. 43(3-4):264-271.
- Wallien M.S.C., Swaab H., Cohen-Kettenis P.T. Psychiatric comorbidity among children with gender identity disorder. J. Am. Acad. Child Adolesc. Psychiatry. 2007;46(10):1307–1314. doi: 10.1097/chi.0b013e3181373848. [DOI] [PubMed] [Google Scholar]
- Warren J.C., Smalley K.B., Barefoot K.N. Differences in psychosocial predictors of obesity among LGBT subgroups. LGBT Health. 2016;3(4):283–291. doi: 10.1089/lgbt.2015.0076. [DOI] [PubMed] [Google Scholar]
- Weyers S., Elaut E., De Sutter P. Long-term assessment of the physical, mental, and sexual health among transsexual women. J. Sex. Med. 2009;6(3):752–760. doi: 10.1111/j.1743-6109.2008.01082.x. [DOI] [PubMed] [Google Scholar]
- White Hughto J.M., Reisner S.L., Pachankis J.E. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc. Sci. Med. 2015;147:222–231. doi: 10.1016/j.socscimed.2015.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White Hughto J.M., Reisner S.L. Social context of depressive distress in aging transgender adults. J. Appl. Gerontol. 2018;37(12):1517–1539. doi: 10.1177/0733464816675819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wierckx, K., Elaut, E., Declercq, E., et al., 2013. Prevalence of cardiovascular disease and cancer during cross-sex hormone therapy in a large cohort of trans persons: A case-control study. Eur J Endocrinol. 169(4):471-478. DOI:10.1530/EJE-13-0493. [DOI] [PubMed]
- Williams C.C., Curling D., Steele L.S., Gibson M.F., Daley A., Green D.C., Ross L.E. Depression and discrimination in the lives of women, transgender and gender liminal people in Ontario, Canada. Health Soc Care Community. 2017;25(3):1139–1150. doi: 10.1111/hsc.12414. [DOI] [PubMed] [Google Scholar]
- Wilson E.C., Chen Y.-H., Arayasirikul S., Wenzel C., Raymond H.F. Connecting the dots: examining transgender women’s utilization of transition-related medical care and associations with mental health, substance use, and HIV. J. Urban Health. 2015;92(1):182–192. doi: 10.1007/s11524-014-9921-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witten T.M. End of life, chronic illness, and trans-identities. J. Social Work End-Of-Life Palliat. Care. 2014;10(1):34–58. doi: 10.1080/15524256.2013.877864. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Global Status Report on Noncommunicable Diseases 2010. World Health Organization; 2011:1-176. Accessed March 6, 2020. https://www.who.int/nmh/publications/ncd_report2010/en/.
- Yildirim B., Perdahli Fis N., Yazkan Akgul G., Ayaz A.B. Gender dysphoria and attention problems: possible clue for biological underpinnings. Psychiatry Clin. Psychopharmacol. 2017;27(3):283–290. doi: 10.1080/24750573.2017.1354417. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.