Abstract
Objectives
The effects of the comprehensiveness of sex education on sexual health measures have not been well-studied. We compared trends in comprehensive sex education and its relation to contraceptive use at first intercourse and current contraceptive use for women ages 15–24 in the United States between 2011 and 2017.
Study design
Analyses included females ages 15–24 from the 2011–2017 National Survey of Family Growth. We defined comprehensive sex education as including 6 topics queried in the NSFG (how to say no to sex, birth control methods, where to get birth control, how to use condoms, sexually transmitted infections, HIV/AIDS), and non-comprehensive sex education as including less than 6 topics. Multivariable regression models investigated associations with contraceptive indicators.
Results
Among 5445 respondents, percentages of women receiving comprehensive sex education in 2011–2013, 2013–2015, and 2015–2017 were 35%, 40%, and 34%. Across all periods, respondents reporting comprehensive sex education before first sex were less likely to report first sexual intercourse before age 15 (aOR 0.55; 95% CI: 0.40–0.74) and non-volitional first intercourse (aOR 0.42, 95% CI: 0.26–0.72) compared to those with non-comprehensive sex education. At first intercourse, those with comprehensive sex education were more likely to have used any (aOR = 1.63; 95% CI: 1.18–2.25) and very effective (aOR = 1.35; 95% CI: 1.04–1.75) contraception. Comprehensive sex education was unrelated to current contraceptive use (aOR = 0.87; 95% CI: 0.63–1.21).
Conclusions
Comprehensive sex education was associated with increased odds of contraceptive use at first intercourse, but not current contraceptive use.
Implications
Programs that promote comprehensive sex education may have a positive impact on preventive behaviors at sexual debut.
Keywords: Contraception, Sexual education, Adolescent, Coitarche, National Survey of Family Growth
1. Introduction
Comprehensive sex education describes a curriculum that teaches students a full range of topics including sexual consent, contraception, and sexually transmitted infections (STIs) including HIV/AIDS [1,2]. Sex education is associated with increased rates of contraceptive use at first sexual intercourse and 15–17 months after interventions [[3], [4], [5]]. Exposure to comprehensive sex education is associated with reduced teen pregnancy, HIV, and STIs [3,4,6].
Despite evidence showing its effectiveness, a significant proportion of adolescents do not receive comprehensive sex education. Alternatives range from abstinence-only education to non-comprehensive sex education, covering only some recommended topics. Programs that teach abstinence-only education do not delay sexual debut or decrease teenage pregnancy risk [[7], [8], [9], [10], [11]].
In 2016, only 14.1 percent of state sex education curricula in grades 6–8 covered all Center for Disease Control (CDC)-recommended topics addressing pregnancy, HIV, and STI prevention [1]. Current trends suggest a decline in support of comprehensive sex education [12]. In 2018, the Department of Health and Human Services cut grants to 81 programs that worked to decrease teenage pregnancy rates [13,14].
In this changing landscape, we sought to assess associations between comprehensive sex education and contraceptive behaviors. We specifically examined trends in comprehensive sex education, and assessed its association with age at first intercourse, voluntariness of first intercourse, contraceptive use at first intercourse, and contraceptive use at the time of the survey.
2. Methods
2.1. Study design and sample
We conducted a cross-sectional analysis of data from the National Survey of Family Growth (NSFG), 2011–2017. The dataset comes from the combined 2011–2013, 2013–2015 and 2015–2017 public-use data files of 30,715 face-to-face interviews [[15], [16], [17]]. The survey consisted of a multistage, stratified, national probability sample of respondents ages 15–44 living in US households, with 5601 women in 2011–2013, 5699 in 2013–2015 and 5554 in 2015–2017. Female participation rates in the 2011–2013, 2013–2015 and 2015–2017 surveys were 73.4%, 71.2% and 66.7%. The survey oversampled Hispanics, African-Americans, and teenagers, which are accounted for with survey weights to produce representative estimates. Study procedures, sample design, and variance estimation for the surveys were previously published [18]. The National Center for Health Statistics (NCHS)/CDC and University of Michigan Institutional Review Boards approved data collection. The Johns Hopkins University Institutional Review Board deemed this study exempt.
We analyzed data for all female respondents aged 15–24 years, as sex education questions are only asked of respondents in this age group. We selected female respondents because we were specifically interested in assessing relationships between comprehensive sexual education and patterns of contraception use. We included female respondents irrespective of sexual activity or sexual orientation.
2.2. Measurement of comprehensive sex education, sexual health behaviors, and contraception use
The NSFG measures sex education by asking participants if they ever received formal sex education at school, church, or a community center before age 18. The survey assesses seven topics: whether participants learned about how to say no to sex, methods of birth control, where to get birth control, how to use a condom, sexually transmitted infections, HIV/AIDS, and waiting until marriage to have intercourse. The survey also collects information on the grade that respondents first learned about each topic and whether they learned it before or after sexual debut.
We defined comprehensive sex education as learning about the following six topics: how to say no to sex, methods of birth control, where to get birth control, how to use a condom, sexually transmitted infections, and HIV/AIDS. We did not include waiting for marriage as a required topic in our definition of comprehensive sex education because it is not included in definitions provided by the American College of Obstetricians and Gynecologists and the CDC [1,2]. We defined non-comprehensive sex education as learning fewer than the six topics comprising comprehensive sex education, but one or more of the seven topics surveyed, including waiting until marriage. Thus, participants who learned about waiting until marriage but not about all six other topics were included in the non-comprehensive sex education category because learning about this topic demonstrates that they received some form of sex education, including abstinence-only or abstinence-based education. We classified respondents as receiving no sex education if they did not learn about any of the seven topics.
Dependent variables were age at first sex, voluntariness of first sex, contraception use at first sex and current contraceptive use. We used the SEX1AGE recoded variable, which describes age at first sex if the respondent had vaginal intercourse with a male partner since menarche. We used the SEX1AGE categories of 14 and under and 15 and above to be consistent with NSFG literature [19]. We used the VOLSEX1 variable to determine voluntariness of first sex. This survey question was asked to respondents aged 18 years and older if they ever had vaginal intercourse with a male partner. We used the SEX1MTHD1 recoded variable to determine the type of contraception used at first sex. For our analysis of age at first sex, volitional first sex, and contraceptive use at first sex, we defined comprehensive first sex as receiving all six key topics prior to first sex. We used the GRFSTSX variable, which determines the grade at first sex, along with variables for each topic that determined which grade they learned about the topic. In the case where the grade was the same for first sex and the topic learned, another variable (e.g. SEDNOSX for learning about saying no to sex) was used to distinguish whether the topic was learned before or after first sex. In our analysis of contraceptive use at first sex, we only included those who reported volitional first sex. We used the CONSTAT1 recoded variable for current contraceptive use status (within the month of the interview). In our analysis of current contraceptive use, we excluded individuals who were sterile for non-contraceptive reasons, pregnant, seeking pregnancy, postpartum up to 2 months, or not sexually active in the last 3 months. Contraceptive measures were categorized based on typical-use effectiveness rates: very effective (sterilization, IUDs, contraceptive implants, oral contraceptive pills [OCPs], contraceptive patch, contraceptive ring, and injectable contraception), and less effective (male condoms, female condoms, withdrawal, cervical cap, periodic abstinence, diaphragm, foam, sponge, jelly or cream without a diaphragm, suppository, and emergency contraception) [20]. In our analysis of contraceptive effectiveness at first sex, we excluded individuals who used vasectomy (n = 1) because it did not represent a female's contraceptive choice, and those who responded with other methods (n = 2) because we could not determine the efficacy of these other methods.
2.3. Statistical analysis
We conducted a descriptive analysis to assess trends in the prevalence of comprehensive sex education over three time periods. We then examined factors related to comprehensive sex education across the three periods after testing for potential interactions by survey year. In the absence of interactions, we pooled survey years for this analysis. Next, we assessed bivariate and multivariate associations between type of sex education (comprehensive sex education or non-comprehensive sex education) and age at first sex, voluntariness of first sex, contraceptive use at first sex, and current contraceptive use. We also analyzed the number of topics included in comprehensive sex education as our key independent measure to assess differences in the odds of outcome measures with each additional comprehensive sex education topic learned. Multivariable regression models adjusted for sociodemographic characteristics previously shown to be associated with contraceptive use and/or adolescent sexual behavior: age, race/ethnicity, income, education, place of residence, living with parents, insurance, religion and religiosity (defined as frequency of attending services at age 14). We checked for multicollinearity using the variance inflation factor. We analyzed data using Stata version 15.1, using the svy command to account for complex survey design and sampling weights.
3. Results
3.1. Sample characteristics
Altogether 5628 female respondents were 15–24 years (1997 in 2011–2013, 1963 in 2013–2015, 1668 in 2015–2017). Table 1 describes sample characteristics by time period. The mean age was 19.5 years, with little variation over time. Twenty-two percent of the sample was Hispanic, and 14.6% African American, with stable proportions over time. Approximately 40% of the sample had some college education or more.
Table 1.
Sociodemographic characteristics of all women 15–24 years in the United States in 2011–2013, in 2013–2015 and in 2015–2017
| Characteristic | N | 2011–2017 (%) | 2011–2013 (%) | 2013–2015 (%) | 2015–2017 (%) |
|---|---|---|---|---|---|
| Total (n) | 5628 | 1997 | 1963 | 1668 | |
| Age | |||||
| 15 | 532 | 8.2 | 8.0 | 8.3 | 8.4 |
| 16 | 588 | 9.3 | 9.9 | 7.4 | 10.7 |
| 17 | 624 | 9.9 | 10.1 | 9.8 | 9.8 |
| 18 | 639 | 10.1 | 8.9 | 9.6 | 12.1 |
| 19 | 588 | 9.9 | 10.6 | 9.3 | 9.8 |
| 20–21 | 959 | 20.4 | 22.1 | 21.2 | 17.6 |
| 22–24 | 1698 | 32.2 | 30.5 | 34.4 | 31.7 |
| Race/ethnicity | |||||
| Hispanic | 1511 | 22.2 | 21.4 | 22.2 | 23.1 |
| Non-Hispanic white | 2390 | 52.7 | 52.8 | 53.7 | 51.9 |
| Non-Hispanic black | 1182 | 14.6 | 15.1 | 14.3 | 14.1 |
| Non-Hispanic other or multiple | 545 | 10.5 | 10.8 | 9.8 | 10.9 |
| Income (% Federal poverty level) | |||||
| 0–99 | 2234 | 34.9 | 36.7 | 35.5 | 32.0 |
| 100–199 | 1374 | 23.8 | 23.9 | 22.1 | 24.9 |
| 200–299 | 822 | 16.0 | 14.9 | 16.7 | 16.5 |
| > 300 | 1198 | 25.5 | 24.5 | 25.8 | 26.6 |
| Education | |||||
| Currently in high school | 1920 | 30.1 | 29.9 | 30.2 | 31.5 |
| Did not complete 12th grade | 375 | 5.3 | 6.8 | 4.9 | 4.2 |
| High school | 1507 | 25.5 | 25.7 | 24.7 | 24.6 |
| Some college or higher | 1826 | 39.2 | 37.7 | 40.2 | 39.7 |
| Insurance | |||||
| Private or Medi-Gap | 2694 | 54.5 | 51.5 | 57.4 | 55.6 |
| Medicaid, CHIP, state sponsored | 1772 | 24.9 | 24.0 | 25.8 | 24.8 |
| Medicare, military, other government | 328 | 5.4 | 6.0 | 4.5 | 5.5 |
| No insurance, single service, Indian Health Service | 834 | 15.2 | 18.6 | 12.4 | 14.2 |
| Place of residence | |||||
| Metropolitan Statistical Area (MSA) | 2303 | 35.4 | 35.0 | 39.0 | 31.7 |
| Other MSA | 2479 | 48.7 | 49.6 | 47.0 | 51.9 |
| Not MSA | 846 | 15.9 | 15.5 | 14.0 | 16.4 |
| Mother (or mother figure's) education | |||||
| Less than high school | 1117 | 16.3 | 16.9 | 15.7 | 15.4 |
| High school | 1590 | 27.1 | 29.1 | 26.7 | 26.2 |
| Some college | 1553 | 28.3 | 30.3 | 26.4 | 27.6 |
| Bachelor's | 1313 | 27.7 | 23.1 | 30.1 | 30.3 |
| No mother-figure identified | 55 | 0.7 | 0.5 | 1.0 | 0.6 |
| Living with parents or parent-figures | |||||
| Both biological parents | 1693 | 31.5 | 30.3 | 31.9 | 32.5 |
| Other or no parental figures | 3935 | 68.6 | 69.7 | 68.1 | 67.5 |
| Religion | |||||
| No religion | 1314 | 24.0 | 21.5 | 25.2 | 25.5 |
| Catholic | 1280 | 22.5 | 22.1 | 22.5 | 22.3 |
| Protestant | 2625 | 45.2 | 47.5 | 45.4 | 43.0 |
| Other | 409 | 8.3 | 9.0 | 6.9 | 9.3 |
| Religiousness (frequency of attending religious services) at age 14 | |||||
| More than once a week | 1031 | 17.5 | 18.1 | 16.8 | 17.3 |
| Once a week | 1853 | 33.0 | 34.7 | 31.9 | 31.7 |
| 1–3 times a month | 876 | 15.8 | 15.4 | 15.7 | 16.9 |
| 1–11 times a year | 846 | 15.3 | 13.7 | 17.0 | 15.0 |
| Never or unknown | 1022 | 18.5 | 18.1 | 18.6 | 19.1 |
*All percentages are weighted.
According to our specified criteria, only 36% of respondents received comprehensive sex education over the study period 2011–2017, peaking at 40% in 2013–2015 and dropping to 34% in 2015–2017. A minority (2.8% - 3.3%) indicated receiving no sexual education. The percentage of respondents receiving non-comprehensive sex education increased from 57% to 63% between 2013–2015 and 2015–2017. Among respondents who received sex education, 24.8% reported receiving zero to three comprehensive sexual education topics, 38.7% reported receiving four or five, and 37% reported receiving all six topics. Thirty-nine percent of respondents who received non-comprehensive sex education did not report learning about contraceptive methods or where to receive contraception.
Table 2 presents pooled analysis of factors related to comprehensive sex education across survey years. Results indicate younger adolescents, living with their parents, and who were still enrolled in high school were less likely to have reported receiving comprehensive sex education (Table 2). Receipt of comprehensive sex education was not associated with race, income, insurance, or mother's education. Age was related to receipt of comprehensive sex education in the survey periods from 2011 to 2013 and 2013–2015, but not 2015–2017.
Table 2.
Sociodemographic characteristics associated with receipt of comprehensive sex education among women ages 15–24 in the United States between 2011 and 2017
| Characteristic | % Comprehensive sex education | p Value⁎ |
|---|---|---|
| Overall | 36.3 | |
| Age | <.001 | |
| 15–18 | 30.6 | |
| 19–21 | 38.8 | |
| 22–24 | 40.7 | |
| Race/ethnicity | .35 | |
| Hispanic | 39.4 | |
| Non-Hispanic white | 35.3 | |
| Non-Hispanic black | 37.1 | |
| Non-Hispanic other or multiple | 34.4 | |
| Income (% Federal poverty level) | .07 | |
| 0–99 | 33.8 | |
| 100–199 | 35.9 | |
| 200–299 | 35.4 | |
| > 300 | 40.8 | |
| Education | <.001 | |
| Currently in high school | 28.2 | |
| Did not complete 12th grade | 36.7 | |
| High school | 39.7 | |
| Some college or higher | 40.3 | |
| Insurance | .07 | |
| Private | 37.7 | |
| Medicaid, CHIP, state sponsored | 37.2 | |
| Medicare, military, other government | 28.3 | |
| No insurance, single service, Indian Health Service | 32.9 | |
| Place of residence | .08 | |
| Metropolitan Statistical Area (MSA) | 39.1 | |
| Other MSA | 34.1 | |
| No MSA | 37.0 | |
| Mother (or mother figure's) education | .57 | |
| Less than high school | 35.0 | |
| High school | 38.3 | |
| Some college | 36.9 | |
| Bachelor's | 34.6 | |
| No mother-figure identified | 36.7 | |
| Living with parents or parent-figures | <.001 | |
| Both biological parents | 30.9 | |
| Other or no parental figures | 38.8 | |
| Religion | 0.20 | |
| No religion | 38.4 | |
| Catholic | 38.0 | |
| Protestant | 35.8 | |
| Other | 29.1 | |
| Religiousness (frequency of attending religious services) | .37 | |
| More than once a week | 33.9 | |
| Once a week | 34.7 | |
| 1–3 times a month | 38.7 | |
| 1–11 times a year | 38.2 | |
| Never | 38.0 | |
%s are weighted.
chi-Square tests assessing the statistical differences in the percentage of respondents receiving comprehensive sex education by sociodemographic characteristics.
3.2. Characteristics of first sex
Overall, 16.6% of adolescents initiated sex before age 15, and 6.2% reported non-volitional first sexual intercourse, which remained stable over time. In our sample, 1830 adolescents reported receiving comprehensive sex education prior to first sex, 3367 reported receiving non-comprehensive sex education, and 431 reported learning no sex education topics prior to first sex. When analyzing differences according to type of sex education prior to first sex, 8.9% of adolescents who reported receiving comprehensive sex education initiated first sex before age 15, compared to 16.4% among those who reported receiving non-comprehensive sex education; this effect remained after sociodemographic adjustments (aOR 0.55; 95% CI 0.40–0.74). Adolescents who received comprehensive sex education prior to first sex were less likely to have experienced non-volitional first sex compared to non-comprehensive sex education (3.2% versus 7.6%, p = 0.0003); this effect remained after sociodemographic adjustments (aOR 0.42, 95% CI 0.26–0.72). Among adolescents who initiated sex before age 15, the adjusted odds of non-volitional first sex were not reduced among those who received comprehensive sexual education compared to those who had not (aOR = 0.31, 95% CI 0.09–1.04). For those who initiated sex at 15 years or above, the odds of non-volitional sex were reduced with receipt of comprehensive sex education in the adjusted model (aOR = 0.54, 95% CI 0.35–0.94).
Fig. 1 depicts the percentage of sexually active respondents reporting sexual activity and contraceptive use according to number of topics learned comprising comprehensive sex education. With each additional topic that participants reported learning prior to first sex, the adjusted odds of first sex at age 15 or above increased by 39% (aOR 1.39, 95% CI 1.30–1.48). Similarly, with each additional topic reported prior to first sex, the adjusted odds of volitional first sex increased by 42% (aOR 1.42, 95% CI 1.2–1.65).
Fig. 1.
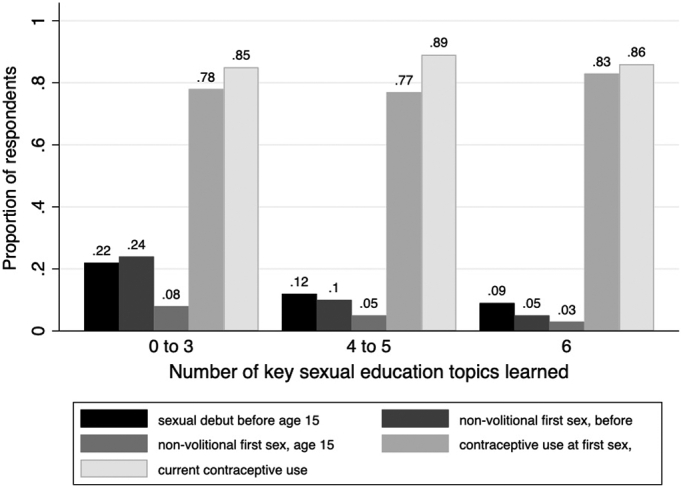
Percentage of women ages 15–24 in the United States who had first sexual intercourse before age 15, who reported non volitional first intercourse, who reported contraceptive use at first sex and who reported current use of contraception according to number of key sexual education topics learned*
*The six key topics include: How to say no to sex, methods of birth control, where to get birth control, how to use a condom, sexually transmitted infections, and HIV/AIDS. Age at sexual debut, non-volitional first sex, and contraceptive use at first sex measures are based on key topics learned prior to first sex.
**Non-volitional first sex and contraceptive use at first sex assessed among women who reported ever having had vaginal intercourse.
***Current contraceptive use evaluated among women in need of contraception at the time of the survey (sexually active in last 3 months, not pregnant or trying to conceive, not sterile or in the 2 months postpartum period).
3.3. Contraceptive use at volitional first sex
Altogether, 79% of respondents used contraception at volitional first sex, with little change over time: 63.6% used condoms, 29.3% used OCP and 2.6% used other hormonal methods, including LARC. Women who received comprehensive sex education prior to first sex were more likely to report contraception at volitional first sex than those who received non-comprehensive sex education (84.3% versus 76.8%, p < 0.004) (Table 3), even after adjusting for covariates (aOR 1.72, 95% CI 1.27–2.33). Among those who used contraception at volitional first sex, women who received comprehensive sex education were more likely to select a very effective method (hormonal contraception or LARC) than those who received non-comprehensive sex education even after sociodemographic adjustments (aOR 1.35, 95% CI 1.04–1.75). When comparing comprehensive sex education to non-comprehensive sex education before first sex, 28.0% versus 18.9% selected the pill and 0.2% versus 0.7% chose LARC at first sex. For each comprehensive sex education topic learned, the adjusted odds of using contraception at volitional first sex increased by 6% (aOR = 1.06, 95% CI 1.00–1.21) while the adjusted odds of using very effective contraception at volitional first sex increased by 13% (aOR = 1.13, 95% CI 1.05–1.21).
Table 3.
Sexual and contraceptive behaviors according to type of sex education received among women 15–24 years in the United States between 2011 and 2017, results from bivariate and multivariate logistic regression
| Comprehensive sex education⁎ (weighted %) | Non-comprehensive sex education⁎ ref. (weighted %) |
Total (weighted %) | Odds ratio (OR) (95% CI) | Adjusted odds ratio⁎⁎ (aOR) (95% CI) | |
|---|---|---|---|---|---|
| Age at first sex before age 15 | 8.9 | 16.4 | 13.6 | 0.45 (0.37–0.67) |
0.55 (0.40–0.74) |
| Non-volitional first sex (all) | 3.2 | 7.6 | 5.9 | 0.39 (0.24–0.66) |
0.42 (0.26–0.72) |
| Non-volitional first sex, age at first sex before age 15 | 4.5 | 18.1 | 14.1 | 0.22 (0.08–0.59) |
0.31 (0.09–1.04) |
| Non-volitional first sex, age at first sex 15 and above | 3.0 | 6.0 | 4.8 | 0.49 (0.28–0.85) |
0.54 (0.31–0.94) |
| Contraceptive use at volitional first sex | 84.3 | 76.8 | 79.8 | 1.62 (1.17–2.25) |
1.63 (1.18–2.25) |
| Use of very effective methods† at first sex among contraceptive users at volitional first sex | 36.3 | 30.4 | 32.9 | 1.30 (0.98–1.73) |
1.35 (1.04–1.75) |
| Current contraceptive use | 86.4 | 87.7 | 87.2 | 0.90 (0.64–1.26) |
0.87 (0.63–1.21) |
| Use of very effective methods among current contraceptive users† | 75.2 | 71.5 | 73.1 | 1.21 (0.93–1.56) |
1.22 (0.95–1.59) |
Notes: ref. = reference group.
Comprehensive sex education: participants learned about all of the following six topics before first sex (age at first sex, non-volitional first sex, contraceptive use at first sex) or prior to age 18 (current contraceptive use): how to say no to sex, methods of birth control, where to get birth control, how to use a condom, sexually transmitted infections, and HIV/AIDS; non-comprehensive sex education: participants learned one or more, but not all, of the sex education topics surveyed.
adjusted odds ratio adjusted for age, race, federal poverty level (%), education, mother's education, metropolitan statistical area (community type), insurance, religion, and religiosity at age 14.
Methods of hormonal contraception or long acting reversible contraception.
3.4. Current contraceptive use
The time elapsed between time of first sex and survey administration averaged 4.4 years. Eighty-seven percent of respondents in need of contraception had used contraception at the time of the survey, with no change over time (Table 3), with no difference between those who had received comprehensive sex education and those who had not (86.4% versus 87.7%, aOR = 0.87; 95% CI 0.63–1.21). The odds of using any contraception or very effective methods at the time of the survey did not change based on the number of topics learned. Among contraceptive users, choice of methods did not significantly differ based on type of sex education: 14.9% of those who received comprehensive sex education used LARC compared to 15.2% of those who had not, 58.1% of those who received comprehensive sex education used other hormonal methods compared to 54.4% of those who had not, and 15.9% of those who received comprehensive sex education used condoms compared to 19.6% of those who had not. Subgroup analysis showed no differences in contraceptive use between comprehensive sex education and non-comprehensive sex education by age groups, 15–19 or 20–24 years.
4. Discussion
Comprehensive sex education was associated with an increase in the likelihood of contraception at first sex compared to non-comprehensive sex education. Comprehensive sex education was also associated with a lower likelihood of non-volitional first sex and higher age at first sex. Both types of sex education have similar associations with current contraceptive use. The findings mirror previous articles that determine that birth control education is associated with delayed age at first sex, increased use of contraception at first sex and use of more reliable methods at first sex [3,4,10], but consolidates the generalizability of these results using recent data from a national sample. In addition, our results add to previous literature comparing abstinence-only education and comprehensive sex education by comparing the recalled content, rather than intent, of sex education and its effects on contraceptive use and showing that comprehensive sex education has an effect on the voluntariness of first sex.
Respondents who received non-comprehensive sex education were more likely to be younger, live with both parents, and have a lower education level, which may reflect the fact that comprehensive sex education is delivered at a later time in school curricula. Delayed programing is concerning given the fact that 58% of adolescents 15–16 years who had initiated sexual activity in our study had not received comprehensive sexual education. The lower proportion of respondents receiving comprehensive sex education at a younger age could be one of the factors contributing to lower levels of contraceptive protection at first sex when sexual activity starts at a younger age. Previous studies have shown age, race, education, and family income are related to likelihood of using contraception at first sexual intercourse among teenage girls [21,22].
Our study found that while the prevalence of formal sex education increased between 2011 and 2015, it decreased in 2015–2017. This may be due to decreased government support for comprehensive sex education programs and increased promotion of abstinence-only programs [23,24].
The variation in contraceptive use for individuals who received comprehensive versus non-comprehensive sex education suggests that comprehensive sex education informs contraceptive use at first sex. Previous studies report similar findings when comprehensive sex education is compared to abstinence-only education [1,3,8,10]. By applying stringent criteria to our comprehensive sex education category, we sought to emphasize the importance of receiving all major components of sex education, including sexual consent, pregnancy and STI prevention on young women's autonomy and protection at sexual initiation and its potential sustained effect over time.
A major limitation of this study is the recall of individuals reporting the sex education topics they received through formal education, which may be prone to recall bias and social desirability bias. There is also the potential for recall bias in the timing of sex education relative to sexual initiation, which in the case of cross-sectional data is difficult to address and therefore causality cannot be assumed. We also could not determine where individuals received sex education, as the question stem included school, church and community programs. In addition, other confounding variables such as region or state may have been missed in this analysis. Finally, we could not compare effects of any sex education to no sex education because the sample size of those who received no sex education was small.
Our study found that comprehensive sex education is associated with later, less non-volitional, and more protected sexual debut in adolescents and young adults, and that the proportion of individuals reporting receipt of comprehensive sex education has decreased in recent years. These results suggest that public health and policy efforts should aim to preserve comprehensive curricula and improve existing sex education curricula to cover essential components of decision-making regarding safe sex, STIs, and contraception.
Declaration of competing interests
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Anne Burke reports completed research support from Bayer, pending research support from Scope Intl, and ongoing support from NICHD, all mediated through Johns Hopkins University.
Footnotes
Declarations of interest: Anne Burke reports completed research support from Bayer, pending research support from Scope Intl, and ongoing support from NICHD, all mediated through Johns Hopkins University.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Brener N.D., Demissie Z., McManus T., Shanklin S.L., Queen B., Kann L. Centers for Disease Control and Prevention; Atlanta: 2017. School Health Profiles 2016: Characteristics of Health Programs Among Secondary Schools.http://www.cdc.gov/schoolhealthprofiles [Google Scholar]
- 2.American College of Obstetricians and Gynecologists' Committee on Adolescent Health Care. Committee Opinion No. 678: comprehensive sexuality educationObstet Gynecol. 2016;128(5):e227–e230. doi: 10.1097/AOG.0000000000001769. [DOI] [PubMed] [Google Scholar]
- 3.Lindberg L.D., Maddow-Zimet I. Consequences of sex education on teen and young adult sexual behaviors and outcomes. J Adolesc Health. 2012;51(4):332–338. doi: 10.1016/j.jadohealth.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 4.Kohler P.K., Manhart L.E., Lafferty W.E. Abstinence-only and comprehensive sex education and the initiation of sexual activity and teen pregnancy. J Adolesc Health. 2008;42(4):344–351. doi: 10.1016/j.jadohealth.2007.08.026. [DOI] [PubMed] [Google Scholar]
- 5.Lopez L.M., Bernholc A., Chen M., Tolley E.E. School-based interventions for improving contraceptive use in adolescents. Cochrane Database Syst Rev. 2016;6 doi: 10.1002/14651858.CD012249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chin H.B., Sipe T.A., Elder R., Mercer S.L., Chattopadhyay S.K., Jacob V. The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: two systematic reviews for the guide to community preventive services. Am J Prev Med. 2012;42(3):272–294. doi: 10.1016/j.amepre.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Borawski E.A., Trapl E.S., Adams-Tufts K., Hayman L.L., Goodwin M.A., Lovegreen L.D. Taking be proud! Be responsible! To the suburbs: a replication study. Perspect Sex Reprod Health. 2009;41(1):12–22. doi: 10.1111/j.1931-2393.2009.4111209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trenholm C., Devaney B., Fortson K., Clark M., Bridgespan L.Q., Wheeler J. Impacts of abstinence education on teen sexual activity, risk of pregnancy, and risk of sexually transmitted diseases. J Policy Anal Manage. 2008;27(2):255–276. doi: 10.1002/pam.20324. [DOI] [PubMed] [Google Scholar]
- 9.Kirby D.B. The impact of abstinence and comprehensive sex and STD/HIV education programs on adolescent sexual behavior. Sex Res Soc Policy. 2008;5(3):18. [Google Scholar]
- 10.Isley M.M., Edelman A., Kaneshiro B., Peters D., Nichols M.D., Jensen J.T. Sex education and contraceptive use at coital debut in the United States: results from cycle 6 of the National Survey of family growth. Contraception. 2010;82(3):236–242. doi: 10.1016/j.contraception.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 11.Stanger-Hall K.F., Hall D.F. Abstinence-only education and teen pregnancy rates: why we need comprehensive sex education in the US. PLoS One. 2011;6(10) doi: 10.1371/journal.pone.0024658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindberg L.D., Maddow-Zimet I., Boonstra H. Changes in adolescents’ receipt of sex education, 2006–2013. J Adolesc Health. 2016;58(6):621–627. doi: 10.1016/j.jadohealth.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.A. S. for Health (ASH) Teen Pregnancy Prevention Program Facts. 2017. https://www.hhs.gov/ash/about-ash/news/2017/teen-pregnancy-prevention-program-facts.html;
- 14.Santhanam L. Why the Federal Teen Pregnancy Prevention Program's fate is uncertain. 2018. https://www.pbs.org/newshour/health/why-the-federal-teen-pregnancy-prevention-programs-fate-is-uncertain
- 15.National Center for Health Statistics (NCHS) CDC National Center for Health Statistics; Hyattsville, MD: 2018. 2015–2017 National Survey of family growth public-use data and documentation. [dataset] [Google Scholar]
- 16.National Center for Health Statistics (NCHS) CDC National Center for Health Statistics; Hyattsville, MD: 2016. 2013–2015 National Survey of family growth public use data and documentation. [dataset] [Google Scholar]
- 17.National Center for Health Statistics (NCHS) CDC National Center for Health Statistics; Hyattsville, MD: 2014. 2011–2013 National Survey of family growth public use data and documentation. [dataset] [Google Scholar]
- 18.Groves R.M., Mosher W.D., Lepkowski J.M., Kirgis N.G. Planning and development of the continuous National Survey of Family Growth. Vital Health Stat. 2009;1(48):1–64. [PubMed] [Google Scholar]
- 19.Martinez G.M., Abma J.C. Sexual activity and contraceptive use among teenagers aged 15–19 in the United States, 2015–2017. NCHS Data Brief. 2020;366:1–8. [PubMed] [Google Scholar]
- 20.Sundaram A., Vaughan B., Kost K., Bankole A., Finer L., Singh S. Contraceptive failure in the United States: estimates from the 2006-2010 National Survey of Family Growth. Perspect Sex Reprod Health. 2017;49(1):7–16. doi: 10.1363/psrh.12017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abma J.C., Martinez G.M. Sexual activity and contraceptive use among teenagers in the United States, 2011-2015. Natl Health Stat Report. 2017;104:1–23. [PubMed] [Google Scholar]
- 22.Lee J., Berenson A., Patel P.R. Characteristics of females who use contraception at Coitarche: an analysis of the National Survey of family growth 2006-2010 database. J Womens Health. 2015;24(12):972–977. doi: 10.1089/jwh.2015.5219. [DOI] [PubMed] [Google Scholar]
- 23.Santelli J.S., Kantor L.M., Grilo S.A., Speizer I.S., Lindberg L.D., Heitel J. Abstinence-only-until-marriage: an updated review of U.S. policies and programs and their impact. J Adolesc Health. 2017;61(3):400–403. doi: 10.1016/j.jadohealth.2017.05.031. [DOI] [PubMed] [Google Scholar]
- 24.Schalet A.T., Santelli J.S., Russell S.T., Halpern C.T., Miller S.A., Pickering S.S. Invited commentary: broadening the evidence for adolescent sexual and reproductive health and education in the United States. J Youth Adolesc. 2014;43(10):1595–1610. doi: 10.1007/s10964-014-0178-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


