Abstract
Introduction
Early access to adequate antenatal care (ANC) from skilled providers is crucial for detecting and preventing obstetric complications of pregnancy. We aimed to assess factors associated with the utilisation of the new WHO ANC guidelines including the recommended number, on time initiation and adequate components of ANC contacts in Myanmar.
Methods
We examined data from 2943 mothers aged 15–49 years whose most recent birth occurred in the last 5 years prior to the 2015–2016 Myanmar Demographic and Health Survey. Factors associated with utilisation of the new WHO recommended ANC were explored using multinomial logistic regression and multivariate models. We used marginal standardisation methods to estimate the predicted probabilities of the factors significantly associated with the three measures of ANC.
Results
Approximately 18% of mothers met the new WHO recommended number of eight ANC contacts. About 58% of the mothers received adequate ANC components, and 47% initiated ANC within the first trimester of pregnancy. The predicted model shows that Myanmar could achieve 70% coverage of adequate components of ANC if all women were living in urban areas. Similarly, if ANC was through private health facilities, 63% would achieve adequate components of ANC. Pregnant women from urban areas (adjusted risk ratio (aRR): 4.86, 95% CI 2.44 to 9.68) were more than four times more likely to have adequate ANC components compared with women from rural areas. Pregnant women in the highest wealth quintile were three times more likely to receive eight or more ANC contacts (aRR: 3.20, 95% CI 1.61 to 6.36) relative to mothers from the lowest wealth quintile. On time initiation of the first ANC contact was fourfold for mothers aged 30–39 years relative to adolescent mothers (aRR: 4.07, 95% CI 1.53 to 10.84).
Conclusion
The 2016 WHO ANC target is not yet being met by the majority of women in Myanmar. Our results highlight the need to address health access inequity for women who are from lower socioeconomic groups, or are younger, and those living in rural areas.
Keywords: maternal health, child health, health systems, cross-sectional survey
Key questions.
What is already known?
Pregnant women in the lower socioeconomic strata are known to be at higher risk for not initiating adequate ANC early and not receiving at least four ANC visits.
What are the new findings?
We demonstrate that Myanmar could achieve 63% coverage of adequate ANC components if the minimum ANC standards were available from the public health facilities at the same rate as those of private health facilities.
Also, if women in rural areas had the same access to ANC as women in urban areas, the country would achieve 70% coverage for adequate components of ANC.
What do the new findings imply?
Efforts to prioritise capacity, including infrastructure and resourcing in rural public health facilities, will improve ANC quality and equity for pregnant women from lower socioeconomic groups and those living in rural areas.
Introduction
Despite global efforts to expand the coverage of maternal and child healthcare services, most women in low-income and middle-income countries (LMICs) still experience a high-risk of death related to pregnancy and childbirth.1 2 Coverage of essential healthcare services such as adequate ANC and skilled birth attendance are among the key indicators to track progress of the Sustainable Development Goals (SDG).3 4 SDG-3 aims to reduce maternal mortality to less than 70 per 100 000 live births and neonatal mortality to less than 12 per 1000 live births by 2030.5 Early access to adequate ANC services from skilled providers is crucial to ensure the best care for women, including promoting awareness, detection and prevention of complications during pregnancy, labour and the postnatal period and to avoid stillbirths and newborn deaths.6–8 Although in 2017 an estimated 62% of women globally received four ANC contacts with skilled health providers,9 the quality of care provided, the skill level of the healthcare provider and early initiation of the first contact remains low and hinders improving health outcomes for women and her offspring.10 11
In 2010, a Cochrane systematic review of randomised trials in Thailand, Cuba, Saudi Arabia and Argentina found a borderline significant increase in perinatal mortality for women randomised to four ANC visits compared with eight model of care.12 13 Based on the recommendation, in 2016, the WHO released the new ANC guidelines for routine ANC to complement the existing WHO guidelines released since 2000 on the management of pregnancy-related complications. The new WHO guidelines recommend eight standard ANC contacts, which previously was only four focus ANC visits.14 As well as increasing the number of contacts, the new guideline aims to provide pregnant women with respectful, individualised, person-centred care at every ANC contact.15 This is a major shift in focus that puts pregnant women at the centre of care. It also emphasises that the first ANC contact should be initiated during the first trimester at <12 weeks gestational age.15 Furthermore, the guideline highlighted the importance of quality of care provided to pregnant women at each ANC contact.16
In 2015, Myanmar was among the Southeast Asian countries with the highest maternal mortality, estimated at 178 per 100 000 live births.2 Postpartum haemorrhage (31%), eclampsia (11%) and abortion-related complications (10%) were the leading cause of maternal mortality in the country.17 Improving the quality and accessibility of maternal and child healthcare services is a priority of the government of Myanmar, as outlined in the Myanmar National Health Plan 2017–2021.18 Previous research investigating ANC in Myanmar has identified factors associated with utilisation and access to care during pregnancy,19–21 birth and postbirth22 23 and highlighted the need to improve the quality of maternal and newborn care services.24 However, these studies did not investigate the new WHO recommended ANC guidelines. In 2018, the Myanmar Ministry of Health and Sports issued a national guideline for ANC based on the 2016 WHO guideline for delivery of ANC services.25 The goal of the national guideline for ANC was to enable service providers at all levels of the health system to use evidence-based knowledge and skills to deliver quality ANC services. In line with the new WHO standard guidelines, this study aims to assess the factors associated with the recommended initiation, number of contacts and adequate components of ANC in order to inform policy and health services of their capacity and compliance with the WHO recommended standard ANC.
Methods
We examined data from the 2015–2016 Myanmar Demographic and Health Survey (MDHS), which is a stratified national-level household survey conducted in seven states and eight regions of Myanmar.26 The 2015–2016 MDHS is the first ever Demographic and Health Survey conducted by the Myanmar Ministry of Health and Sports and funded by the US Agency for International Development. A two-stage stratified sampling design was conducted for the selection of the sample in urban and rural areas and for each of the seven states and eight regions of Myanmar. The first stage involved selecting sample points (clusters) consisting of enumeration areas or ward/village tracts with a total of 442 clusters (123 urban and 319 rural). At the second stage, equal probability systematic sampling was used for selection of a fixed number of 30 households from each of the selected clusters. Detailed information of the 2015–2016 MDHS sampling design have been reported elsewhere.26 The survey collected information on access and utilisation of ANC services based on the focused ANC model, which recommended four ANC contacts. During the survey, women were asked about their access to ANC during pregnancy, such as a number of contacts, initiation and the components of ANC they received. The relevant information on ANC services were obtained from 3176 (2943 weighted) women aged 15–49 years who had ANC contacts from skilled providers during pregnancy for their most recent birth in the 5 years prior to the survey. We included only the most recent birth because these births had the most detailed information on maternal and child healthcare services and are less subject to recall bias. We also excluded 460 (13%) of mothers who did not receive any ANC and 180 (5%) of those mothers who had ANC from unskilled providers.
Study variables
There are three study outcomes for this analysis that assess the new WHO standard ANC guidelines using the 2015–2016 MDHS dataset. The first study outcome was the recommended initiation of the first ANC contact expressed as the number of women with a live birth in the last 5 years prior to the survey who initiated their first ANC contact during the first trimester of pregnancy from skilled providers. We categorised ANC initiation as: (1) on-time initiation (defined as the number of pregnant women who initiated the first ANC contact during the first trimester ≤3 months); (2) late initiation (defined as those pregnant women who initiated their first ANC contact during the second trimester 4–6 months); and (3) very late initiation (defined as the number of pregnant women who initiated their first ANC contact during the third trimester 7–9 months); month is the unit of measurement in the Demographic and Health Survey. The second outcome was the new recommended number of ANC contacts defined as the number of women with a live birth in the 5 years prior to the survey who have had at least eight or more ANC contacts from skilled providers during pregnancy. We defined the number of ANC contacts as: (1) number of pregnant women who had 1–3 ANC contacts, (2) number of pregnant women with 4–7 ANC contacts and (3) number of pregnant women with eight or more ANC contacts. The third outcome was adequacy of ANC. It is expressed as the number of women with a live birth in the last 5 years prior to the survey who received adequate components of ANC from skilled providers during pregnancy. In this analysis, we included only seven components of ANC. These components were available from the list of the indicators collected during 2015–2016 MDHS such as blood pressure measurement, urine analysis, blood analysis, tetanus vaccination, iron supplementation, intestinal parasite medication and counselling on potential complications of pregnancy. Women receiving ANC components were categorised into: (1) adequate ANC (classified as the number of women who received between six and seven ANC components); (2) inadequate ANC (classified as the number of women who received between four and five ANC components); and (3) severely inadequate ANC (classified as the number of women who received less than four ANC components).
Explanatory variables for this analysis were selected based on the literature27–29 and included household characteristics; cluster type and location (representing the characteristics of a cluster); and the household wealth quintile (representing the economic status of the household). The maternal and partner factors (describing individual-level circumstances of a pregnant woman and of her partner) included maternal characteristics such as mother’s current age, mother’s education, mother’s working status, and partner characteristics such as husband’s working status, and education.30 31 We also, included exposure to mass media, including radio, television, newspapers or magazines,32 and birth rank, birth interval, place of ANC services, place of birth, mode of birth, type of birth assistance and postnatal care services.33 34
Statistical analysis
All analyses were carried out using STATA/MP V.12.35 The ‘Svy’ survey commands were used to allow for adjustments for the cluster sampling design and sampling weights. The frequency tabulations were generated to describe the characteristics of study variables.35 Since each of the outcome variables had more than two categories, we conducted univariable multinomial logistic regressions to determine the unadjusted risk ratios (aRRs) for the outcome variables. This was followed by conducting multivariable multinomial logistic regression analysis to examine risk ratios for factors associated with each of the outcomes. At the initial stage, we included all the predictor variables, with (p<0.2). This was followed by a manual backward procedure to eliminate non-significant variables but retaining those significant (p<0.05) factors. The final model included all the variables with p<0.05.
To estimate the predicted probabilities of the factors significantly associated with the outcomes, we used marginal standardisation methods describe by Muller and MacLehose.36 According to this method, the estimated odds of outcome is proportionally adjusted according to a weight for each level of the covariates following confounder-adjusted logistic regression. The following formula was used to examine the marginal standardisation:
Whereas (pΛez) is the predicted probabilities of the study outcome for any (E=e and Z=z) assuming that all respondents (target population) in the dataset had the single set values of the exposure level donated to Set[E=e] and with the same distribution of a given set of observed values for the covariate vector donated to (Z=z). Thus, the logistic regression coefficients were used to calculate predicted probabilities for every respondent at their observed covariate pattern and newly exposure value. The marginal probabilities obtained from this method indicate a weighted average over the distribution of the covariates, which are equivalent to estimates obtained by standardising to the total population. In this analysis, we used the STATA margins command to compute the predicted probability of the factors associated with on time initiation of first ANC contact, receiving the recommended number of eight or more ANC contacts and receiving adequate ANC components after performing a logistic regression model.
Ethical approval consent
Verbal informed consent was taken from each respondent before the interview. The Demographic Health Survey programme gave permission to access and use the data for this research.
Patient and public involvement statement
This study is based on the analysis of secondary data of the 2015–2016 MDHS, which is available in the public domain. The participants were not involved in the design or implementation of this analysis, and there are no plans to disseminate the results of the analysis to study participants due to the deidentified data.
Results
We found 59% (95% CI 56.0% to 62.5%) of mothers met the previous WHO guidelines for the minimum recommended number of 4 or more ANC contacts, of those mothers 42% (95% CI 39.0% to 44.1%) had a minimum number of 4–7 ANC contacts and 18% (95% CI 15.6% to 20.2%) had received the new recommended number of eight or more ANC contacts. About 58% (95% CI 55.1% to 61.2%) of mothers had an adequate number of ANC components. ANC contact was initiated within the first trimester of pregnancy by 47% of women (95% CI 41.1% to 49.5%) (figure 1).
Figure 1.
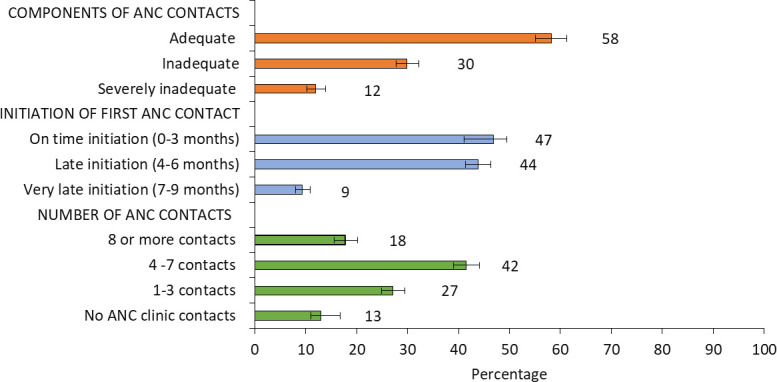
The recommended number, initiation and adequacy of ANC components and contacts (percentage and 95%CI), Myanmar Demographic and Health Survey, 2015–2016. ANC, adequate antenatal care.
Almost three quarters (73%) of the study population lived in a rural area and 23% of the study population were in the lowest wealth quintiles. Three per cent of mothers were adolescents (<20 years). Public health facilities were the main ANC service providers, accounting for 71% of ANC. About half (53%) of all live births were in non-health facilities, and almost a quarter of all births (23%) were attended by unskilled providers (table 1).
Table 1.
Baseline characteristics of the study participants analysis of Myanmar Demographic and Health Survey, 2015–2016 (n=2943)
| N | Weighted N (%) | |
| Household factors | ||
| Location of household | ||
| Rural | 2347 | 2158 (73.3) |
| Urban | 829 | 784 (26.7) |
| Geographical zone | ||
| Hilly zone | 1099 | 553 (19.4) |
| Coastal zone | 563 | 344 (12.0) |
| Delta zone | 609 | 1002 (35.1) |
| Central plain zone | 815 | 959 (33.5) |
| Household wealth status | ||
| Lowest quintile | 742 | 680 (23.1) |
| Second lowest quintile | 680 | 613 (20.8) |
| Middle quintile | 602 | 528 (18.0) |
| Fourth quintile | 635 | 584 (19.8) |
| Highest quintile | 517 | 539 (18.3) |
| Maternal/partner factors | ||
| Mother’s current age (years) | ||
| Under 20 | 78 | 74 (2.5) |
| 20–29 | 1339 | 1228 (41.7) |
| 30–39 | 1385 | 1325 (45.0) |
| 40 and over | 374 | 315 (10.7) |
| Mother’s education | ||
| No education/primary | 1747 | 1676 (56.9) |
| Secondary or higher | 1429 | 1267 (43.1) |
| Mother’s working status | ||
| Not working | 1136 | 1032 (35.2) |
| Agriculture-related work | 444 | 369 (12.6) |
| Non-agriculture related work | 1588 | 1533 (52.3) |
| Husband’s working status | ||
| Agriculture-related work | 2491 | 1758 (60.3) |
| Non-agriculture related work | 1340 | 1157 (39.7) |
| Husband’s education | ||
| No education/primary | 1560 | 1485 (51.3) |
| Secondary or higher | 1551 | 1409 (48.7) |
| Exposure to mass media | ||
| Reading newspaper or magazine | ||
| No | 1955 | 1792 (60.9) |
| Yes | 1221 | 1150 (39.1) |
| Listening to radio | ||
| No | 1910 | 1740 (59.1) |
| Yes | 1266 | 1202 (40.9) |
| Watching television | ||
| No | 1132 | 762 (25.9) |
| Yes | 2735 | 2181 (74.1) |
| Birth history | ||
| Birth rank | ||
| 4th birth rank and over | 1043 | 566 (19.2) |
| 2nd–3rd birth rank | 1599 | 1277 (43.4) |
| 1st birth rank | 1225 | 1099 (37.4) |
| Preceding birth interval | ||
| Birth interval >3 years | 864 | 453 (15.4) |
| Birth interval <3 years | 1766 | 1379 (47.0) |
| First child | 1225 | 1099 (37.5) |
| Pregnancy, birth and postbirth care | ||
| Place of antenatal care | ||
| Home/other | 1136 | 485 (16.5) |
| Public health facility | 2335 | 2100 (71.4) |
| Private health facility | 396 | 358 (12.2) |
| Birth assistant | ||
| None/traditional birth attendants/other untrained | 1363 | 686 (23.3) |
| Health professional | 2504 | 2257 (76.7) |
| Place of birth | ||
| Non-health facility | 2403 | 1552 (52.7) |
| Health facility | 1464 | 1391 (47.3) |
| Mode of birth | ||
| Non-caesarean section | 3183 | 2272 (77.2) |
| Caesarean section | 684 | 671 (22.8) |
| Postnatal care | ||
| No | 2024 | 1467 (49.8) |
| Yes | 1842 | 1476 (50.2) |
Mothers aged 20–29 years (aRR: 2.85, 95% CI 1.07% to 7.58%), 30–39 years (aRR: 4.07, 95% CI 1.53% to 10.84%) and 40–49 years (aRR: 3.79, 95% CI 1.29% to 11.11%) were at least twofold more likely to initiate ANC during the first trimester of pregnancy relative to adolescent mothers. Mothers assisted by skilled healthcare providers at birth were twofold more likely to have initiated ANC in the first trimester than mothers unassisted at birth or assisted by unskilled healthcare providers (aRR: 2.34, 95% CI 1.45% to 3.77%, table 2).
Table 2.
Adjusted and unadjusted risk ratios for initiation of first antenatal care contact, analysis of Myanmar Demographic and Health Survey, 2015–2016 (n=2943)
| Initiation of first antenatal care contact | ||||||||||||
| Late initiation within second trimester (4–6 months) | On time initiation within first trimester (0–3 months) | |||||||||||
| Study variables | RR* | 95% CI‡ | P value | aRR‡ | 95% CI‡ | P value | RR* | 95% CI‡ | P value | aRR‡ | 95% CI‡ | P value |
| Household factors | ||||||||||||
| Location of household | ||||||||||||
| Rural | 1.00 | 1.00 | ||||||||||
| Urban | 1.79 | (1.22 to 2.64) | 0.003 | 1.32 | (0.87 to 1.99) | 0.191 | ||||||
| Geographical zone | ||||||||||||
| Hilly zone | 1.00 | 1.00 | ||||||||||
| Coastal zone | 1.03 | (0.62 to 1.72) | 0.905 | 1.12 | (0.65 to 1.94) | 0.68 | ||||||
| Delta zone | 1.09 | (0.69 to 1.72) | 0.704 | 1.00 | (0.60 to 1.65) | 0.996 | ||||||
| Central plain zone | 1.10 | (0.67 to 1.81) | 0.709 | 1.49 | (0.84 to 2.64) | 0.168 | ||||||
| Household wealth status | ||||||||||||
| Lowest quintile | 1.00 | 1.00 | ||||||||||
| Second lowest quintile | 1.13 | (0.75 to 1.71) | 0.563 | 1.21 | (0.80 to 1.82) | 0.367 | ||||||
| Middle quintile | 1.10 | (0.70 to 1.73) | 0.682 | 1.06 | (0.68 to 1.65) | 0.802 | ||||||
| Fourth quintile | 1.95 | (1.21 to 3.16) | 0.006 | 1.74 | (1.05 to 2.87) | 0.030 | ||||||
| Highest quintile | 2.45 | (1.43 to 4.17) | 0.001 | 2.88 | (1.68 to 4.17) | <0.001 | ||||||
| Maternal/partner factors | ||||||||||||
| Mother’s current age (years) | ||||||||||||
| Under 20 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 20–29 | 1.39 | (0.68 to 2.83) | 0.361 | 1.28 | (0.60 to 2.72) | 0.527 | 3.00 | (1.20 to 7.51) | 0.019 | 2.85 | (1.07 to 7.58) | 0.00 |
| 30–39 | 1.99 | (0.99 to 3.99) | 0.053 | 1.66 | (0.77 to 3.58) | 0.192 | 4.26 | (1.77 to 10.25) | 0.001 | 4.07 | (1.53 to 10.84) | 0.00 |
| 40 and over | 1.44 | (0.65 to 3.18) | 0.364 | 1.34 | (0.56 to 3.22) | 0.506 | 3.31 | (1.27 to 8.59) | 0.014 | 3.79 | (1.29 to 11.11) | 0.00 |
| Mother’s education | ||||||||||||
| No education/primary | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Secondary or higher | 1.79 | (1.29 to 2.48) | 0.001 | 1.64 | (1.12 to 2.40) | 2.02 | (1.45 to 2.83) | <0.001 | 1.73 | (1.16 to 2.56) | ||
| Mother’s working status | ||||||||||||
| Not working | 1.00 | 1.00 | ||||||||||
| Agriculture-related work | 0.80 | (0.49 to 1.33) | 0.392 | 1.02 | (0.64 to 1.63) | 0.933 | ||||||
| Non-agriculture related work | 1.10 | (0.78 to 1.55) | 0.601 | 1.12 | (0.79 to 1.61) | 0.520 | ||||||
| Husband’s working status | ||||||||||||
| Agriculture-related work | 1.00 | 1.00 | ||||||||||
| Non-agriculture related work | 1.41 | (0.99 to 1.99) | 0.054 | 1.22 | (0.84 to 1.76) | 0.282 | ||||||
| Husband’s education | ||||||||||||
| No education/primary | 1.00 | 1.00 | ||||||||||
| Secondary or higher | 1.41 | (1.05 to 1.90) | 0.023 | 1.52 | (1.13 to 2.04) | 0.005 | ||||||
| Exposure to mass media | ||||||||||||
| Reading newspaper or magazine | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Yes | 1.57 | (1.14 to 2.17) | 0.006 | 1.20 | (0.84 to 1.70) | 0.309 | 2.06 | (1.48 to 2.86) | <0.001 | 1.51 | (1.06 to 2.14) | 0.022 |
| Listening to radio | ||||||||||||
| No | 1.00 | 1.00 | ||||||||||
| Yes | 0.98 | (0.69 to 1.40) | 0.913 | 1.31 | (0.93 to 1.85) | 0.119 | ||||||
| Watching television | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Yes | 1.68 | (1.21 to 2.33) | 0.002 | 1.47 | (1.04 to 2.09) | 0.028 | 1.49 | (1.06 to 2.10) | 0.023 | 1.22 | (0.85 to 1.76) | 0.283 |
| Birth history | ||||||||||||
| Birth rank | ||||||||||||
| 4th birth rank and over | 1.00 | 1.00 | ||||||||||
| 2nd–3rd birth rank | 1.30 | (0.88 to 1.92) | 0.19 | 1.42 | (0.91 to 1.99) | 0.082 | ||||||
| 1st birth rank | 1.09 | (0.72 to 1.65) | 0.689 | 1.58 | (0.87 to 2.05) | 0.045 | ||||||
| Preceding birth interval | ||||||||||||
| Birth interval >3 years | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Birth interval <3 years | 1.97 | (1.33 to 2.90) | 0.001 | 1.71 | (1.15 to 2.54) | 0.008 | 1.81 | (1.21 to 2.71) | 0.004 | 1.47 | (0.97 to 2.22) | 0.070 |
| First child | 1.49 | (0.99 to 2.23) | 0.056 | 1.26 | (0.80 to 2.00) | 0.320 | 1.67 | (1.06 to 2.58) | 0.020 | 1.47 | (0.90 to 2.40) | 0.121 |
| Pregnancy, birth and postbirth care | ||||||||||||
| Place of antenatal care | ||||||||||||
| Home/other | 1.00 | 1.00 | ||||||||||
| Public health facility | 1.01 | (0.56 to 1.89) | 0.961 | 1.10 | (0.70 to 2.74) | 0.673 | ||||||
| Private health facility | 0.81 | (0.44 to 1.48) | 0.491 | 1.11 | (0.60 to 2.07) | 0.731 | ||||||
| Birth assistant | ||||||||||||
| None/traditional birth attendants/other untrained | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Health professional | 1.84 | (1.29 to 2.62) | 0.001 | 1.84 | (1.19 to 2.83) | 0.006 | 2.27 | (1.57 to 3.28) | <0.001 | 2.34 | (1.45 to 3.77) | 0.001 |
| Place of birth | ||||||||||||
| Non-health facility | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Health facility | 1.15 | (0.82 to 1.61) | 0.414 | 0.65 | (0.42 to 1.03) | 0.064 | 1.13 | (0.80 to 1.60) | 0.482 | 0.55 | (0.34 to 0.88) | 0.013 |
| Mode of birth | ||||||||||||
| Non-caesarean section | 1.00 | 1.00 | ||||||||||
| Caesarean section | 0.92 | (0.62 to 1.36) | 0.684 | 1.24 | (0.85 to 1.79) | 0.263 | ||||||
| Postnatal care | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Yes | 1.25 | (0.91 to 1.72) | 0.171 | 1.22 | (0.88 to 1.68) | 0.235 | 1.71 | (1.24 to 2.37) | 0.001 | 1.60 | (1.16 to 2.23) | 0.005 |
*Unadjusted risk ratio (RR).
†Adjusted risk ratio (aRR) and the risk ratio adjusted for all other variables in the table.
‡Confidence interval (CI).
Urban women were more than fourfold more likely to receive an adequate number of ANC components compared with rural women (aRR: 4.86, 95% CI 2.44 to 9.68). Pregnant women attending private facilities for ANC (aRR: 2.24, 95% CI 1.24 to 4.42) and those attending public facilities for ANC (aRR: 2.37, 95% CI 1.54 to 3.65) were twice more likely to have adequate components of ANC compared with their counterparts who received ANC from home/other informal source (table 3).
Table 3.
Adjusted and unadjusted risk ratio for adequacy of antenatal care component, analysis of Myanmar Demographic and Health Survey, 2015–2016 (n=2943)
| Components of antenatal care | ||||||||||||
| Inadequate | Adequate | |||||||||||
| Study variables | RR* | 95% CI‡ | P value | aRR‡ | 95% CI‡ | P value | RR* | 95% CI‡ | P value | aRR‡ | 95% CI‡ | P value |
| Household factors | ||||||||||||
| Location of household | ||||||||||||
| Rural | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Urban | 2.31 | (1.30 to 4.08) | 0.004 | 1.80 | (0.90 to 3.61) | 0.099 | 7.31 | (4.06 to 13.17) | <0.001 | 4.86 | (2.44 to 9.68) | <0.001 |
| Geographical zone | ||||||||||||
| Hilly zone | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Coastal zone | 0.64 | (0.38 to 1.08) | 0.097 | 0.59 | (0.34 to 1.04) | 0.069 | 0.48 | (0.26 to 0.89) | 0.02 | 0.43 | (0.22 to 0.84) | 0.014 |
| Delta zone | 0.87 | (0.52 to 1.47) | 0.612 | 0.68 | (0.39 to 1.21) | 0.193 | 1.23 | (0.66 to 2.28) | 0.519 | 0.79 | (0.40 to 1.56) | 0.490 |
| Central plain zone | 0.70 | (0.44 to 1.10) | 0.121 | 0.57 | (0.34 to 0.95) | 0.032 | 0.71 | (0.40 to 1.25) | 0.236 | 0.53 | (0.28 to 1.02) | 0.058 |
| Household wealth status | ||||||||||||
| Lowest quintile | 1.00 | 1.00 | ||||||||||
| Second lowest quintile | 0.99 | (0.66 to 1.50) | 0.962 | 1.30 | (0.88 to 1.93) | 0.184 | ||||||
| Middle quintile | 1.26 | (0.80 to 2.97) | 0.323 | 1.76 | (1.12 to 2.75) | 0.014 | ||||||
| Fourth quintile | 1.66 | (0.95 to 2.89) | 0.077 | 3.53 | (2.12 to 5.88) | <0.001 | ||||||
| Highest quintile | 2.17 | (1.17 to 4.02) | 0.014 | 6.44 | (3.33 to 12.45) | <0.001 | ||||||
| Maternal/partner factors | ||||||||||||
| Mother’s current age (years) | ||||||||||||
| Under 20 | 1.00 | 1.00 | ||||||||||
| 20–29 | 0.91 | (0.41 to 1.98) | 0.805 | 1.86 | (0.84 to 4.99) | 0.124 | ||||||
| 30–39 | 0.84 | (0.37 to 1.91) | 0.678 | 1.96 | (0.88 to 4.91) | 0.098 | ||||||
| 40 and over | 0.72 | (0.30 to 1.69) | 0.443 | 1.34 | (0.59 to 3.40) | 0.483 | ||||||
| Mother’s education | ||||||||||||
| No education/primary | 1.00 | 1.00 | ||||||||||
| Secondary or higher | 1.55 | (1.10 to 2.17) | 0.018 | 2.75 | (2.02 to 3.73) | <0.001 | ||||||
| Mother’s working status | ||||||||||||
| Not working | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Agriculture-related work | 0.74 | (0.48 to 1.14) | 0.17 | 0.79 | (0.49 to 1.26) | 0.319 | 0.44 | (0.28 to 0.68) | <0.001 | 0.64 | (0.40 to 1.04) | 0.070 |
| Non-agriculture related work | 0.78 | (0.57 to 1.08) | 0.131 | 0.73 | (0.52 to 1.03) | 0.072 | 0.67 | (0.48 to 0.93) | 0.017 | 0.62 | (0.43 to 0.90) | 0.011 |
| Husband’s working status | ||||||||||||
| Agriculture-related work | 1.00 | 1.00 | ||||||||||
| Non-agriculture related work | 1.68 | (1.22 to 2.31) | 0.002 | 3.01 | (2.18 to 4.16) | <0.001 | ||||||
| Husband’s education | ||||||||||||
| No education/primary | 1.00 | 1.00 | ||||||||||
| Secondary or higher | 1.21 | (0.87 to 1.68) | 0.264 | 2.12 | (1.56 to 2.90) | 0.074 | ||||||
| Exposure to mass media | ||||||||||||
| Reading newspaper or magazine | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Yes | 1.91 | (1.36 to 2.70) | <0.001 | 1.77 | (1.24 to 2.51) | 0.002 | 3.71 | (2.18 to 4.15) | <0.001 | 2.12 | (1.50 to 2.99) | <0.001 |
| Listening to radio | ||||||||||||
| No | 1.00 | 1.00 | ||||||||||
| Yes | 1.24 | (0.91 to 1.68) | 0.174 | 1.41 | (1.06 to 1.88) | 0.018 | ||||||
| Watching television | ||||||||||||
| No | 1.00 | 1.00 | ||||||||||
| Yes | 1.69 | (1.28 to 2.24) | <0.001 | 2.37 | (1.77 to 3.17) | <0.001 | ||||||
| Birth history | ||||||||||||
| Birth rank | ||||||||||||
| Fourth birth rank and over | 1.00 | 1.00 | ||||||||||
| 2nd–3rd birth rank | 1.32 | (0.93 to 1.86) | 0.122 | 1.91 | (1.37 to 2.66) | <0.001 | ||||||
| First birth rank | 1.30 | (0.88 to 1.91) | 0.186 | 2.03 | (1.43 to 2.88) | <0.001 | ||||||
| Preceding birth interval | ||||||||||||
| Birth interval >3 years | 1.00 | 1.00 | ||||||||||
| Birth interval <3 years | 0.82 | (0.53 to 1.26) | 0.368 | 0.97 | (0.63 to 1.50) | 0.905 | ||||||
| First child | 0.95 | (0.63 to 1.42) | 0.807 | 1.30 | (0.85 to 1.97) | 0.223 | ||||||
| Pregnancy, birth and postbirth care | ||||||||||||
| Place of antenatal care | ||||||||||||
| Home/other | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Public health facility | 1.92 | (1.37 to 2.69) | <0.001 | 1.61 | (1.11 to 2.34) | 0.012 | 3.77 | (2.55 to 5.57) | <0.001 | 2.37 | (1.54 to 3.65) | <0.001 |
| Private health facility | 2.80 | (1.53 to 5.14) | <0.001 | 1.65 | (0.87 to 3.13) | 0.125 | 7.88 | (4.22 to 14.74) | <0.001 | 2.24 | (1.24 to 4.42) | <0.020 |
| Birth assistant | ||||||||||||
| None/traditional birth attendants/other untrained | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Health professional | 1.91 | (1.43 to 2.57) | <0.001 | 1.65 | (1.19 to 2.30) | 0.003 | 5.42 | (3.93 to 7.48) | <0.001 | 3.38 | (2.38 to 4.81) | <0.001 |
| Place of birth | ||||||||||||
| Non-health facility | 1.00 | 1.00 | ||||||||||
| Health facility | 1.98 | (1.39 to 2.82) | <0.001 | 4.39 | (3.07 to 6.28) | <0.001 | ||||||
| Mode of birth | ||||||||||||
| Non-caesarean section | 1.00 | 1.00 | ||||||||||
| Caesarean section | 2.11 | (1.32 to 3.39) | 0.002 | 3.66 | (2.34 to 5.71) | <0.001 | ||||||
| Postnatal care | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Yes | 1.26 | (0.91 to 1.73) | 0.158 | 1.36 | (0.98 to 1.90) | 0.066 | 1.72 | (1.23 to 2.39) | 0.001 | 2.22 | (1.57 to 3.14) | <0.001 |
*Unadjusted risk ratio (RR).
†Adjusted risk ratio (aRR) and the risk ratio adjusted for all other variables in the table.
‡Confidence interval (CI).
Pregnant women in the highest wealth quintile were threefold more likely of having eight and more ANC contacts (aRR: 3.20, 95% CI 1.61 to 6.36) relative to mothers from the lowest wealth quintile. Mothers who gave birth in a health facility were twofold more likely to have received eight or more ANC contacts (aRR: 2.35, 95% CI 1.54 to 3.28) compared with those mothers who gave birth in non-health facility. Receiving eight or more ANC contacts was threefold more likely for women attending a private facility for ANC (aRR: 3.62, 95% CI 1.86 to 6.97), compared with home/other informal sources of ANC (table 4).
Table 4.
Adjusted and unadjusted risk ratios for recommended number of antenatal care contacts, analysis of Myanmar Demographic and Health Survey, 2015–2016 (n=2943)
| Study variables | Number of antenatal care contacts | |||||||||||
| 4–7 ANC contacts | 8 or more ANC contacts | |||||||||||
| RR* | 95% CI‡ | P value | aRR‡ | 95% CI‡ | P value | RR* | 95% CI‡ | P value | aRR‡ | 95% CI‡ | P value | |
| Household factors | ||||||||||||
| Location of household | ||||||||||||
| Rural | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Urban | 3.42 | (2.44 to 4.79) | <0.001 | 1.84 | (1.29 to 2.62) | 0.001 | 9.62 | (6.30 to 14.68) | <0.001 | 2.56 | (1.64 to 4.00) | <0.001 |
| Geographical zone | ||||||||||||
| Hilly zone | 1.00 | 1.00 | ||||||||||
| Coastal zone | 0.88 | (0.61 to 1.28) | 0.501 | 1.10 | (0.64 to 1.88) | 0.739 | ||||||
| Delta zone | 1.43 | (1.02 to 2.01) | 0.039 | 1.32 | (0.78 to 2.23) | 0.296 | ||||||
| Central plain zone | 1.15 | (0.83 to 1.57) | 0.389 | 1.24 | (0.74 to 2.07) | 0.421 | ||||||
| Household wealth status | ||||||||||||
| Lowest quintile | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Second lowest quintile | 1.30 | (0.99 to 1.72) | 0.058 | 1.09 | (0.82 to 1.46) | 0.551 | 1.93 | (1.26 to 2.93) | 0.002 | 1.41 | (0.90 to 2.21) | 0.137 |
| Middle quintile | 1.77 | (1.30 to 2.40) | <0.001 | 1.19 | (0.87 to 1.64) | 0.278 | 3.59 | (2.30 to 5.61) | <0.001 | 1.85 | (1.14 to 3.00) | 0.013 |
| Fourth quintile | 2.34 | (1.77 to 3.29) | <0.001 | 1.21 | (0.83 to 1.78) | 0.306 | 6.56 | (4.23 to 10.18) | <0.001 | 2.04 | (1.25 to 3.33) | 0.005 |
| Highest quintile | 5.52 | (3.13 to 9.73) | <0.001 | 1.70 | (0.92 to 3.13) | 0.087 | 27.65 | (14.58 to 52.44) | <0.001 | 3.20 | (1.61 to 6.36) | 0.001 |
| Maternal/partner factors | ||||||||||||
| Mother’s current age (years) | ||||||||||||
| Under 20 | 1.00 | 1.00 | ||||||||||
| 20–29 | 1.62 | (0.86 to 3.06) | 0.134 | 1.94 | (0.84 to 4.50) | 0.120 | ||||||
| 30–39 | 1.97 | (1.06 to 3.64) | 0.032 | 2.37 | (1.04 to 5.38) | 0.039 | ||||||
| 40 and over | 1.40 | (0.72 to 2.73) | 0.322 | 1.08 | (0.45 to 2.61) | 0.864 | ||||||
| Mother’s education | ||||||||||||
| No education/primary | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Secondary or higher | 2.51 | (2.00 to 3.15) | <0.001 | 1.33 | (1.03 to 1.73) | 0.032 | 4.92 | (3.72 to 6.51) | <0.001 | 1.19 | (0.84 to 1.68) | 0.322 |
| Mother’s working status | ||||||||||||
| Not working | 1.00 | 1.00 | ||||||||||
| Agriculture-related work | 0.62 | (0.45 to 0.85) | 0.003 | 0.38 | (0.24 to 0.60) | <0.001 | ||||||
| Non-agriculture related work | 0.95 | (0.74 to 1.21) | 0.671 | 1.13 | (0.84 to 1.54) | 0.418 | ||||||
| Husband’s working status | ||||||||||||
| Agriculture-related work | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Non-agriculture related work | 1.98 | (1.55 to 2.53) | <0.001 | 1.09 | (0.83 to 1.41) | 0.542 | 5.26 | (3.91 to 7.09) | <0.001 | 1.63 | (1.18 to 2.25) | 0.003 |
| Husband’s education | ||||||||||||
| No education/primary | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Secondary or higher | 2.04 | (1.64 to 2.53) | <0.001 | 1.20 | (0.94 to 1.55) | 0.145 | 4.98 | (3.72 to 6.67) | <0.001 | 1.76 | (1.27 to 2.43) | 0.001 |
| Exposure to mass media | ||||||||||||
| Reading newspaper or magazine | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Yes | 1.95 | (1.56 to 2.43) | <0.001 | 1.29 | (1.01 to 1.66) | 0.042 | 2.80 | (2.15 to 3.64) | <0.001 | 1.21 | (0.91 to 1.60) | 0.197 |
| Listening to radio | ||||||||||||
| No | 1.00 | 1.00 | ||||||||||
| Yes | 1.32 | (1.05 to 1.65) | 0.016 | 1.19 | (0.91 to 1.56) | 0.193 | ||||||
| Watching television | ||||||||||||
| No | 1.00 | 1.00 | ||||||||||
| Yes | 1.87 | (1.47 to 2.39) | <0.001 | 2.61 | (1.97 to 3.47) | <0.001 | ||||||
| Birth history | ||||||||||||
| Birth rank | ||||||||||||
| 4th birth rank and over | 1.00 | 1.00 | ||||||||||
| 2nd–3rd birth rank | 1.31 | (1.03 to 1.68) | 0.029 | 2.96 | (1.92 to 4.24) | <0.001 | ||||||
| 1st birth rank | 1.73 | (1.34 to 2.24) | <0.001 | 5.16 | (3.14 to 6.96) | <0.001 | ||||||
| Preceding birth interval | ||||||||||||
| Birth interval >3 years | 1.00 | 1.00 | ||||||||||
| Birth interval <3 years | 1.43 | (1.10 to 1.86) | 0.008 | 1.85 | (1.27 to 2.71) | 0.002 | ||||||
| First child | 1.90 | (1.41 to 2.55) | <0.001 | 3.48 | (2.29 to 5.29) | <0.001 | ||||||
| Pregnancy, birth and postbirth care | ||||||||||||
| Place of antenatal care | ||||||||||||
| Home/other | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Public health facility | 2.16 | (1.63 to 2.88) | <0.001 | 1.62 | (1.19 to 2.20) | 0.002 | 4.41 | (2.78 to 6.99) | <0.001 | 2.08 | (1.24 to 3.50) | 0.006 |
| Private health facility | 4.03 | (2.42 to 6.71) | <0.001 | 1.88 | (1.10 to 3.23) | 0.022 | 20.40 | (11.20 to 37.12) | <0.001 | 3.62 | (1.86 to 6.97) | <0.001 |
| Birth assistant | ||||||||||||
| None/traditional birth attendants /other untrained | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Health professional | 2.78 | (2.17 to 3.55) | <0.001 | 1.59 | (1.21 to 2.09) | 0.001 | 8.76 | (5.66 to 13.56) | <0.001 | 2.20 | (1.32 to 368) | 0.003 |
| Place of birth | ||||||||||||
| Non-health facility | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Health facility | 2.40 | (1.88 to 3.06) | <0.001 | 1.26 | (0.93 to 1.71) | 0.140 | 7.34 | (5.38 to 10.01) | <0.001 | 2.35 | (1.54 to 3.28) | <0.001 |
| Mode of birth | ||||||||||||
| Non-caesarean section | 1.00 | 1.00 | ||||||||||
| Caesarean section | 1.97 | (1.47 to 2.60) | <0.001 | 4.97 | (3.65 to 6.76) | <0.001 | ||||||
| Postnatal care | ||||||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Yes | 1.30 | (1.06 to 1.60) | 0.011 | 1.45 | (1.17 to 1.80) | 0.001 | 1.33 | (1.00 to 1.76) | 0.044 | 1.83 | (1.35 to 2.47) | <0.001 |
*Unadjusted risk ratio (RR).
†Adjusted risk ratio (aRR) and the risk ratio adjusted for all other variables in the table.
‡Confidence interval (CI).
In the predictive model keeping the distribution of all covariates the same, except making urban residence universal, we would expect 70% of women to receive an adequate number of components of ANC during their pregnancy (online supplementary file 1). Alternatively, if all women received ANC from private healthcare facilities keeping all other covariates unchanged, 63% would receive the adequate number of ANC components (online supplementary file 1). Similarly applying the same methods but all women were aged between 15 years and 19 years, we would expect that 30% of women would initiate the first ANC contact during the first trimester of pregnancy. Whereas if all women were 20–29 years, this would be increased to 46% of women initiating the first ANC contact during the first trimester of pregnancy (online supplementary file 2). The best model for the predictive margins for the recommended number of eight ANC contacts were as high as 27% for pregnant women receiving ANC from a private health facility (online supplementary file 3).
bmjgh-2019-002169supp001.pdf (48.7KB, pdf)
bmjgh-2019-002169supp002.pdf (63.7KB, pdf)
bmjgh-2019-002169supp003.pdf (51.3KB, pdf)
Discussion
Our results demonstrate that Myanmar is similar to many other LMICs, with 59% of the pregnant women meeting the previous WHO minimum number of four or more ANC contacts, compared with the global LMIC proportion of 55%.1 37 We found that about 18% of pregnant women in Myanmar met the new recommended number of eight or more ANC contacts. Less than half of women initiated ANC by 12 weeks gestational age as recommended by WHO.14 Our estimate of the likelihood of pregnant women receiving the recommended number, adequacy and on time initiation of ANC contacts was significantly higher for urban residents, women aged between 20 years and 49 years and women from the wealthiest households. Our findings highlight that Myanmar has made slow progress over the period of the Millennium Development Goals era with regards to coverage of the new focus ANC model. This needs to be considered in the context of the civil unrest, internal conflicts and of course that the ANC model in place was based on the previous WHO ANC module.38 We also found that there remains inequity in ANC utilisation.
Socioeconomic inequality in ANC contacts exists in Myanmar, as it does in almost all countries around the world.24 28 39 40 In this study, pregnant women in the lower socioeconomic strata were at a higher risk for not initiating ANC early, not receiving the recommended number of ANC contacts or receiving adequate ANC components. We demonstrated that Myanmar could achieve ~51% coverage of up to seven ANC contacts, if all women were in the highest wealth quintile households. Evidence of improving access to ANC has included cash transfer schemes, housing finance schemes and community mortgage programmes for low-income women.41 Such initiatives benefit poorer women by improving their living conditions and status within the household through providing them with access to capital, resources, credit, land, technology and information.42 43 Thus, intervening with similar programmes are likely to benefit women to access ANC, and these interventions may be worth considering for Myanmar.
Pregnant women who received the adequate number of components and recommended number of eight ANC contacts were more likely to use skilled healthcare providers at birth and postbirth care services than women who did not. Late initiation of ANC precludes sufficient time to access the sufficient number of ANC contacts thus missing opportunities for early intervention, and this has been previously identified.44–46 In other settings such as South-eastern Tanzania and Afghanistan, a counselling intervention of early ANC initiation that involved training community health volunteers to provide ANC information to women within their own communities has been shown to improve on-time initiation of ANC.47 48
Urban residence was predictive of women receiving adequate ANC components, consistent with a previous study in 91 LMICs.49 In Myanmar, inadequate ANC components could be explained by poor healthcare infrastructure particularly in rural areas. Our findings demonstrate that, if the minimum standards of ANC components such as diagnostic tests were available from the public health facilities at the same rate as those of private health facilities, the country would achieve 63% coverage of adequate components of ANC. In addition to our findings, a lack of availability and distribution of health resources such as a sufficient supply chain, financial resources and infrastructure particularly in rural and hard-to-reach conflict and postconflict areas are among the challenges facing the health system as indicated in the Myanmar National Health Plan 2017–2021.50 Thus, building capacity, infrastructure and resourcing public health facilities in rural areas needs to be prioritised.50–52
In Myanmar, the risk of late initiation of ANC was higher among adolescent mothers. These adolescent mothers were generally primiparous, living in poorer and rural households. As in many LMICs, late initiation of ANC could be explained by the inability of pregnant adolescents to recognise the signs and symptoms of pregnancy, or trying to conceal their pregnancies, leading to delays in initiating antenatal care.21 53 54 Adolescent pregnancy has poorer outcomes thus, an intervention that promotes delayed childbirth for married adolescents and more broadly promotes the use of contraception for adolescents could effectively reduce the risk of adolescent pregnancy and improve maternal and child health outcomes.
The study strengths include a representative national sample with a high response for women (96%). Data on birth history were restricted to the most recent birth in order to minimise recall bias. The study was however a cross-sectional survey that restricts the interpretation of causality. The reliance on maternal recall for the data is also a weakness; however, any bias is likely to be non-differential. Not all ANC service indicators, measurement and information on pregnancy, birth and postbirth complications or measurement of knowledge and attitude were collected during the 2015–16 MDHS, and this could have affected the result. However, these data are the best nationally representative data available from Myanmar.
Conclusion
Myanmar has made slow progress towards the previous WHO guidelines of four or more ANC contacts. The overall findings from this analysis show that the county is still far from attaining the new recommended number of eight and more ANC contacts. The main factors associated with on-time initiation, adequacy and recommended eight or more ANC contacts were urban residence, women aged between 20 years and 49 years and women from the wealthiest households. Interventions that address the persistent health access inequity for younger, poorer and rural women need to be prioritised in order for the country to improve access to recommended care throughout pregnancy and for a positive pregnancy experience thus improving maternal health and birth outcomes.
Footnotes
Handling editor: Sanni Yaya
Contributors: NSM and CR-G designed the study. NSM performed the analysis and prepared the first draft of the manuscript. CR-G revised drafts of the manuscript and provided advice on data analysis. KSM revised the manuscript and analysis. All authors read and approved the final manuscript.
Funding: CR-G is funded by the National Health and Medical Research Council GNT1127074 and a Robinson Fellowship, The University of Sydney. NSM is funded by SOAR funding, The University of Sydney.
Competing interests: The authors declare no conflicts of interest.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: The Ethics Review Committee on Medical Research, including Human Subjects in the Department of Medical Research, Ministry of Health and Sports and ICF Institutional Review Board reviewed and approved the survey protocol.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository. Currently, the data are available from the Demographic and Health Surveys website (https://dhsprogram.com).
References
- 1.WHO World health statistics 2016: monitoring health for the SDGs, sustainable development goals. Switzerland; 2016. [Google Scholar]
- 2.WHO, UNICEF, UNFPA, World Bank Group, United Nations Trends in maternal mortality: 1990 to 2015: estimates by who, UNICEF, UNFPA, world bank group and the United nations population division. Geneva, Switzerland, 2015. [Google Scholar]
- 3.United Nations The sustainable development goals report 2016. New York; 2016. [Google Scholar]
- 4.Raynes-Greenow C. Gaps and challenges underpinning the first analysis of global coverage of early antenatal care. Lancet Glob Health 2017;5:e949–50. 10.1016/S2214-109X(17)30346-7 [DOI] [PubMed] [Google Scholar]
- 5.UNICEF Indicator and monitoring framework for the global strategy for women's, children's and adolescent's health (2016-2030); 2016.
- 6.Lawn JE, Blencowe H, Waiswa P, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet 2016;387:587–603. 10.1016/S0140-6736(15)00837-5 [DOI] [PubMed] [Google Scholar]
- 7.Owolabi OO, Wong KLM, Dennis ML, et al. Comparing the use and content of antenatal care in adolescent and older first-time mothers in 13 countries of West Africa: a cross-sectional analysis of demographic and health surveys. Lancet Child Adolesc Health 2017;1:203–12. 10.1016/S2352-4642(17)30025-1 [DOI] [PubMed] [Google Scholar]
- 8.Uneke CJ, Uro-Chukwu HC. Improving quality of antenatal care through provision of medical supply kits. Lancet Glob Health 2018;6:e4–5. 10.1016/S2214-109X(17)30471-0 [DOI] [PubMed] [Google Scholar]
- 9.NICEF global databases Antenatal care, 2018. Available: https://data.unicef.org/topic/maternal-health/antenatal-care/
- 10.Leslie HH, Malata A, Ndiaye Y, et al. Effective coverage of primary care services in eight high-mortality countries. BMJ Glob Health 2017;2:e000424. 10.1136/bmjgh-2017-000424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mbuagbaw L, Medley N, Darzi AJ, et al. Health system and community level interventions for improving antenatal care coverage and health outcomes. Cochrane Database Syst Rev 2015;12:CD010994. 10.1002/14651858.CD010994.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vogel JP, Habib NA, Souza JP, et al. Antenatal care packages with reduced visits and perinatal mortality: a secondary analysis of the WHO antenatal care trial. Reprod Health 2013;10:19. 10.1186/1742-4755-10-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carroli G, Villar J, Piaggio G, et al. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet 2001;357:1565–70. 10.1016/S0140-6736(00)04723-1 [DOI] [PubMed] [Google Scholar]
- 14.Tunçalp Ӧ, Pena-Rosas JP, Lawrie T, et al. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG 2017;124:860–2. 10.1111/1471-0528.14599 [DOI] [PubMed] [Google Scholar]
- 15.WHO WHO recommendations on antenatal care for a positive pregnancy experience Switzerland World Health Organization; 2016. [PubMed] [Google Scholar]
- 16.de Masi S, Bucagu M, Tunçalp Özge, et al. Integrated person-centered health care for all women during pregnancy: implementing World Health organization recommendations on antenatal care for a positive pregnancy experience. Glob Health Sci Pract 2017;5:197–201. 10.9745/GHSP-D-17-00141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Department of Health - Ministry of Health Myanmar,, UNICEF . Nationwide cause specific maternal mortality survey 2004–2005; 2005.
- 18.Ministry of Health and Sports (MoHS) Myanmar National Health Plan 2017 - 2021; 2016.
- 19.Oo K, Win LL, Saw S, et al. Challenges faced by skilled birth attendants in providing antenatal and intrapartum care in selected rural areas of Myanmar. WHO South East Asia J Public Health 2012;1:467–76. 10.4103/2224-3151.207049 [DOI] [PubMed] [Google Scholar]
- 20.Wangmo S, Patcharanarumol W, Nwe ML, et al. Hard-To-Reach villages in Myanmar: challenges in access to health services and interim solutions. Qual Primary Care 2017;25:187–92. [Google Scholar]
- 21.Sein KK. Maternal health care utilization among ever married youths in Kyimyindaing township, Myanmar. Matern Child Health J 2012;16:1021–30. 10.1007/s10995-011-0815-8 [DOI] [PubMed] [Google Scholar]
- 22.Wai KM, Shibanuma A, Oo NN, et al. Are husbands involving in their spouses' utilization of maternal care services?: a cross-sectional study in Yangon, Myanmar. PLoS One 2015;10:e0144135. 10.1371/journal.pone.0144135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Than KK, Mohamed Y, Oliver V, et al. Prevention of postpartum haemorrhage by community-based auxiliary midwives in hard-to-reach areas of Myanmar: a qualitative inquiry into acceptability and feasibility of task shifting. BMC Pregnancy Childbirth 2017;17:146. 10.1186/s12884-017-1324-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okawa S, Win HH, Leslie HH, et al. Quality gap in maternal and newborn healthcare: a cross-sectional study in Myanmar. BMJ Glob Health 2019;4:e001078. 10.1136/bmjgh-2018-001078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maternal and Reproductive Health Division, Ministry of Health and Sports, UNICEF National guidelines for antenatal care: for service providers USAID; 2018. [Google Scholar]
- 26.Ministry of Health and Sports (MoHS), ICF Myanmar demographic and health survey 2015-16. Nay Pyi Taw, Myanmar and Rockville, Maryland USA: Ministry of Health and Sports and ICF, 2017. [Google Scholar]
- 27.Heredia-Pi I, Servan-Mori E, Darney BG, et al. Measuring the adequacy of antenatal health care: a national cross-sectional study in Mexico. Bull World Health Organ 2016;94:452–61. 10.2471/BLT.15.168302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Islam MM, Masud MS. Determinants of frequency and contents of antenatal care visits in Bangladesh: assessing the extent of compliance with the who recommendations. PLoS One 2018;13:e0204752. 10.1371/journal.pone.0204752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yaya S, Bishwajit G, Ekholuenetale M, et al. Timing and adequate attendance of antenatal care visits among women in Ethiopia. PLoS One 2017;12:e0184934. 10.1371/journal.pone.0184934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mugo NS, Dibley MJ, Agho KE. Prevalence and risk factors for non-use of antenatal care visits: analysis of the 2010 South Sudan household survey. BMC Pregnancy Childbirth 2015;15:68. 10.1186/s12884-015-0491-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haftu A, Hagos H, Mehari M-A, et al. Pregnant women adherence level to antenatal care visit and its effect on perinatal outcome among mothers in Tigray public health institutions, 2017: cohort study. BMC Res Notes 2018;11:872. 10.1186/s13104-018-3987-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Titaley CR, Dibley MJ. Factors associated with not using antenatal iron/folic acid supplements in Indonesia: the 2002/2003 and 2007 Indonesia demographic and health survey. Asia Pac J Clin Nutr 2015;24:162–76. 10.6133/apjcn.2015.24.1.10 [DOI] [PubMed] [Google Scholar]
- 33.Bishanga DR, Drake M, Kim Y-M, et al. Factors associated with institutional delivery: findings from a cross-sectional study in Mara and Kagera regions in Tanzania. PLoS One 2018;13:e0209672. 10.1371/journal.pone.0209672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dhakal P, Shrestha M, Baral D, et al. Factors affecting the place of delivery among mothers residing in jhorahat VDC, Morang, Nepal. Int J Community Based Nurs Midwifery 2018;6:2. [PMC free article] [PubMed] [Google Scholar]
- 35. StataCorp. Stata: release 13. statistical software. College Station, TX: StataCorp LP, 2013. [Google Scholar]
- 36.Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol 2014;43:962–70. 10.1093/ije/dyu029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.WHO and International Center for Equity in Health/Pelotas State of inequality: reproductive, maternal, newborn and child health. Geneva; 2015. [Google Scholar]
- 38.Saw YM, Win KL, Shiao LW-S, et al. Taking stock of Myanmar's progress toward the health-related millennium development goals: current roadblocks, paths ahead. Int J Equity Health 2013;12:78. 10.1186/1475-9276-12-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Houweling TAJ, Ronsmans C, Campbell OMR, et al. Huge poor-rich inequalities in maternity care: an international comparative study of maternity and child care in developing countries. Bull World Health Organ 2007;85:745–54. 10.2471/BLT.06.038588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Victora CG, Matijasevich A, Silveira M, et al. Socio-Economic and ethnic group inequities in antenatal care quality in the public and private sector in Brazil. Health Policy Plan 2010;25:253–61. 10.1093/heapol/czp065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.The World Bank World development report 2012: gender equality and development. Washington: The World Bank; 2011. [Google Scholar]
- 42.Heaman MI, Sword W, Elliott L, et al. Barriers and facilitators related to use of prenatal care by inner-city women: perceptions of health care providers. BMC Pregnancy Childbirth 2015;15:2. 10.1186/s12884-015-0431-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Obare F, Warren C, Njuki R, et al. Community-Level impact of the reproductive health vouchers programme on service utilization in Kenya. Health Policy Plan 2013;28:165–75. 10.1093/heapol/czs033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saad-Haddad G, DeJong J, Terreri N, et al. Patterns and determinants of antenatal care utilization: analysis of national survey data in seven countdown countries. J Glob Health 2016;6:010404. 10.7189/jogh.06.010404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moller A-B, Petzold M, Chou D, et al. Early antenatal care visit: a systematic analysis of regional and global levels and trends of coverage from 1990 to 2013. Lancet Glob Health 2017;5:e977–83. 10.1016/S2214-109X(17)30325-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Benova L, Tunçalp Özge, Moran AC, et al. Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries. BMJ Glob Health 2018;3:e000779. 10.1136/bmjgh-2018-000779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gross K, Alba S, Glass TR, et al. Timing of antenatal care for adolescent and adult pregnant women in south-eastern Tanzania. BMC Pregnancy Childbirth 2012;12:16. 10.1186/1471-2393-12-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Edmond KM, Yousufi K, Anwari Z, et al. Can community health worker home visiting improve care-seeking and maternal and newborn care practices in fragile states such as Afghanistan? a population-based intervention study. BMC Med 2018;16:106. 10.1186/s12916-018-1092-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arsenault C, Jordan K, Lee D, et al. Equity in antenatal care quality: an analysis of 91 national household surveys. Lancet Glob Health 2018;6:e1186–95. 10.1016/S2214-109X(18)30389-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.World Health Organization The Republic of the Union of Myanmar health system review. Contract No.: 3 2014. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 51.O'Neill K, Takane M, Sheffel A, et al. Monitoring service delivery for universal health coverage: the service availability and readiness assessment. Bull World Health Organ 2013;91:923–31. 10.2471/BLT.12.116798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Leslie HH, Spiegelman D, Zhou X, et al. Service readiness of health facilities in Bangladesh, Haiti, Kenya, Malawi, Namibia, Nepal, Rwanda, Senegal, Uganda and the United Republic of Tanzania. Bull World Health Organ 2017;95:738–48. 10.2471/BLT.17.191916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Godia PM, Olenja JM, Hofman JJ, et al. Young people's perception of sexual and reproductive health services in Kenya. BMC Health Serv Res 2014;14:172. 10.1186/1472-6963-14-172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bwalya BC, Sitali D, Baboo KS, et al. Experiences of antenatal care among pregnant adolescents at Kanyama and Matero clinics in Lusaka district, Zambia. Reprod Health 2018;15:124. 10.1186/s12978-018-0565-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2019-002169supp001.pdf (48.7KB, pdf)
bmjgh-2019-002169supp002.pdf (63.7KB, pdf)
bmjgh-2019-002169supp003.pdf (51.3KB, pdf)


