The lifetime risk of developing incident heart failure (HF) in the US is 20% for individuals older than 40 years.(1) Few HF scores rely solely on echocardiographic parameters of cardiac structure and function to determine the risk of incident HF. Among these, the Heart and Soul Study (HSS) developed a validated echocardiographic risk-stratification index (ERSI) in participants with stable coronary artery disease to predict the 4-year probability of incident HF among asymptomatic individuals, independent of and superior to clinical risk factors.(2)
Hispanics/Latinos are a large and fast growing subset of the US population and should be considered at high risk for incident HF based on the prevalence of clinical risk factors.(3) However, there is equipoise regarding their real HF risk, with some projection statistics estimating that Hispanics/Latinos will have the lowest HF prevalence in 2030.(4) This assertion feeds the so called “Hispanic paradox”, which remains poorly understood.(3) Nonetheless, it remains reasonable that Hispanics/Latinos will have a significant impact on the future prevalence and economic burden of HF in the US, as this population ages and continues to grow, but further data is needed.(5) We sought to better understand the burden that Hispanics/Latinos will have in the anticipated HF epidemic in the US by estimating the incident HF risk of a community-cohort of Hispanics/Latinos, based on echocardiographic parameters.
We used cross-sectional data from the population-based Echo-Study of Latinos (ECHO-SOL). Participants older than 40 years of age, with complete echocardiographic data and without a history of incident HF were selected. The ERSI was calculated from echocardiographic parameters as described by Stevens et al. and applied to estimate risk of incident HF. The index range was 0 to 8, with lower scores representing lower risk for incident HF. The scoring system included: 1 point for LV outflow tract velocity time integral <22cm, 1 point for left atrial volume index >29 ml/m2, 1 point for moderate or severe mitral regurgitation, 2 points for pseudonormal or restrictive diastolic dysfunction, 3 points for LV mass index ≥ 90 g/m2.(2). The cohort was divided into Low Risk (ERSI <3) and High Risk (ERSI ≥3), and analyzed by gender, age and Hispanic/Latino subpopulation. Survey statistics and weighted frequencies were used for all analyses.
A total of 1,769 participants [57% women, mean age 56.3 (±0.37)] were included. The largest Hispanic/Latino subpopulation was Cuban (31.9%), the smallest was South American (6.1%). The High Risk category represented 52% of the ECHO-SOL population. Obesity, hypertension and diabetes were significantly more prevalent in the High Risk subpopulation (198 vs. 311; 220 vs. 353; and 122 vs. 197 respectively. P < 0.0001 for all). The proportion of individuals in the High Risk category increased proportionally with older age; this held true for males and females (P = 0.034 and 0.027, respectively). However, more females tended to be in the High Risk subpopulation at a younger age as compared to males (Figure 1A). Puerto Rican had the highest proportion of High Risk individuals (58.4%), and Mexican the lowest (47.9%); however, this difference was not statistically significant (Figure 1B). The ERSI distribution was different across the four geographic locations, with the greatest proportion of High Risk individuals in Chicago and the lowest in San Diego (P = 0.013). Compared to the original cohort of the HSS in which the ERSI was validated, the ECHO-SOL target population was younger, with a higher proportion of female participants and a lower prevalence of coronary artery disease (3%); nonetheless the proportion of participants in the High Risk ERSI category is similar for both cohorts (56% in the HSS cohort). Moreover, 9.2% of the ECHO-SOL participants were classified in the highest ERSI category (scores 7–8) as compared to only 2% of the HSS participants.
Figure 1.
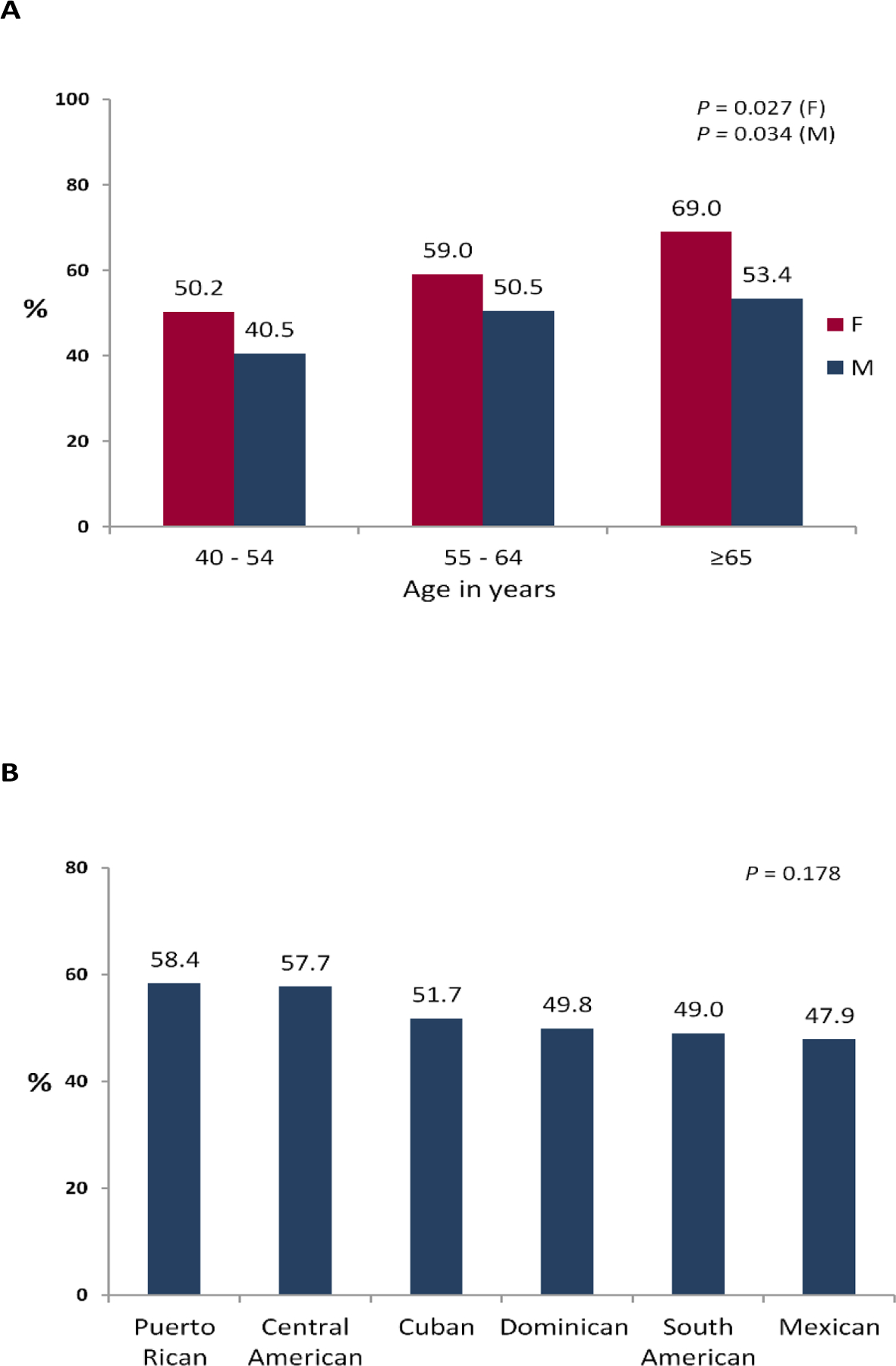
(A) Echocardiographic risk stratification index (ERSI) ≥3 by age and sex. (B) ERSI ≥3 by Hispanic/Latino subpopulation, echocardiographic risk stratification index; F, female; M, male.
This is the largest study of US Hispanics/Latinos, describing a high prevalence of abnormal LV structure and function based on the ERSI. This likely translates to a higher risk of future incident HF independently of clinical risk factors despite a relatively young mean age of this population. These estimations based on objective and reproducible data, highlight the significant role that the Hispanic/Latino population will likely have in the US HF epidemic. Since Hispanic/Latinos represent a large and growing subset of the US population, determining their HF risk is a critical step for designing appropriate cardioprotective strategies. There are limitations to our study. Although the application of the ERSI is a promising tool to estimate risk of incident HF, it was developed for evaluation of subjects with coronary artery disease, and at present we lack the outcome data necessary to validate it in ECHO-SOL. However, our study does represent an important first step in identifying HF risk in a large and relevant segment of our population.
Footnotes
Conflict of interest: The authors have reported that they have no relationships relevant to the contents of this manuscript to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Yancy CW, Jessup M, Bozkurt B et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology 2013;62:e147–239. [DOI] [PubMed] [Google Scholar]
- 2.Stevens SM, Farzaneh-Far R, Na B, Whooley MA, Schiller NB. Development of an echocardiographic risk-stratification index to predict heart failure in patients with stable coronary artery disease: the Heart and Soul study. JACC Cardiovascular imaging 2009;2:11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodriguez CJ, Allison M, Daviglus ML et al. Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States: a science advisory from the American Heart Association. Circulation 2014;130:593–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heidenreich PA, Albert NM, Allen LA et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 2013;6:606–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heidenreich PA, Trogdon JG, Khavjou OA et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011;123:933–44. [DOI] [PubMed] [Google Scholar]


