Abstract
Objectives
Programmes to ensure doctors’ maintenance of professional competence (MPC) have been established in many countries. Since 2011, doctors in Ireland have been legally required to participate in MPC. A significant minority has been slow to engage with MPC, mirroring the contested nature of such programmes internationally. This study aimed to describe doctors’ attitudes and experiences of MPC in Ireland with a view to enhancing engagement.
Participants
All registered medical practitioners in Ireland required to undertake MPC in 2018 were surveyed using a 33-item cross-sectional mixed-methods survey designed to elicit attitudes, experiences and suggestions for improvement.
Results
There were 5368 responses (response rate 42%). Attitudes to MPC were generally positive, but the time, effort and expense involved outweighed the benefit for half of doctors. Thirty-eight per cent agreed that MPC is a tick-box exercise. Heavy workload, travel, requirement to record continuing professional development activities and demands placed on personal time were difficulties cited. Additional support, as well as higher quality, more varied educational activities, were among suggested improvements. Thirteen per cent lacked confidence that they could meet requirements, citing employment status as the primary issue. MPC was particularly challenging for those working less than full-time, in locum or non-clinical roles, and taking maternity or sick leave. Seventy-seven per cent stated a definite intention to comply with MPC requirements. Being male, or having a basic medical qualification from outside Ireland, was associated with less firm intention to comply.
Conclusions
Doctors need to be convinced of the benefits of MPC to them and their patients. A combination of clear communication and improved relevance to practice would help. Addition of a facilitated element, for example, appraisal, and varied ways to meet requirements, would support participation. MPC should be adequately resourced, including provision of high-quality free educational activities. Systems should be established to continually evaluate doctors’ perspectives.
Keywords: medical education & training, health policy, health services administration & management
Strengths and limitations of this study.
Strong response rate for a national online survey of all doctors (n=5368, 42%).
Representativeness of the respondents.
Diverse stakeholders involved in the research, including patient representation.
Survey design was undertaken in accordance with best practice, informed by literature and theory. Post-hoc analysis of the survey confirmed its validity.
Although the response rate to the survey was excellent, there were still large numbers of non-responders. We cannot be sure that the findings presented here represent the views of non-responders.
Introduction
Historically, once a doctor entered independent practice, career-long maintenance of professional knowledge and skills was assumed.1 In recent decades, evolving doctor–patient relationships, a drive for accountability and high-profile cases of malpractice2 have led medical regulators to put continuous evaluative processes in place to ensure that doctors are up to date and fit to practise.3 A variety of terms are used to describe these programmes: revalidation, recertification, relicensing, maintenance of certification and maintenance of licensure.4 5 In this paper, we will use the term maintenance of professional competence (MPC).
MPC programme requirements vary from country to country but, in general, involve educational and assessment elements such as evidence of good professional standing; participation in knowledge self-assessments; examinations; quality improvement projects or audits; appraisal; peer and patient feedback; and continuing professional development (CPD).3 5–7 The intended outcomes of these activities are manifold and include improving patient safety and the quality of patient care, encouraging doctors to commit to lifelong learning and enhancing the CPD of doctors.5 8 While there is evidence that some MPC activities, such as interactive continuing medical education (CME)/CPD, appraisal, review of patient complaints and multisource feedback, have an impact on doctors’ knowledge, skills, attitudes and behaviours, it is less clear that MPC significantly impacts patient’s outcomes.3 This has led to much debate about whether and how MPC programmes should be implemented.
In keeping with international trends, in Ireland, doctors have been legally mandated to participate in MPC since 2011. The Medical Council, the regulator for doctors in Ireland, has established a range of Professional Competence Schemes (PCS) to administer the process through 13 national bodies responsible for postgraduate medical training. Doctors are required to enrol in and submit evidence of educational activities annually through a PCS. Each doctor is expected to obtain a minimum of 50 credits per year (1 credit=1 hour) through CPD activity. A minimum requirement of 20 credits each is set for external and internal CPD, with the remainder coming from personal learning and research/teaching categories. In addition, each doctor is required to complete one quality improvement (clinical/non-clinical) audit per year.9
Following its introduction in Ireland, a significant minority of doctors were slow to engage with MPC. By 2016, 16.3% had still not enrolled in a PCS despite a legal requirement to do so. Active measures by the Medical Council have addressed enrolment reducing this figure to 1.7% in 2018.10 Nonetheless, engagement remains a problem, with one postgraduate training body reporting 30% of doctors not meeting the requirements laid down by the Medical Council.11 Failure among doctors to engage fully with a legal requirement linked to competence has the potential to undermine the trust the public have in their doctors. It also creates risk for employers, indemnifiers and a significant challenge for the regulator.
This paper reports a national survey of doctors in Ireland, funded by the Health Research Board Ireland. The aim of this study was to describe doctors’ attitudes, experiences and suggestions for improvement in relation to current systems for MPC in Ireland. The research was underpinned by an integrated approach to knowledge translation. The research team included representation from a range of stakeholders: the regulator, postgraduate training bodies, the health service and patients.
Methods
Study design and setting
As the regulatory body for the medical profession in Ireland, the Medical Council has among its roles maintenance of the Register of Medical Practitioners and must satisfy itself as to medical practitioners’ ongoing MPC. The Register of Medical Practitioners is comprised of four divisions listed in table 1. Those registered in the general, supervised and specialist division are required to participate in MPC.
Table 1.
Divisions of the Register of Medical Practitioners
| Division | Registrants |
| General division | Medical practitioners who have not completed specialist training and do not occupy a postgraduate training post. Nineteen per cent of doctors in this division are GPs. |
| Specialist division | Medical practitioners who have completed specialist training recognised by the Medical Council and can practise independently as a specialist. Thirty-nine per cent of doctors in this division are GPs. |
| Supervised division | Medical practitioners who have been offered a post that has been approved by the national health service executive, which has specific supervisory arrangements. |
| Trainee specialist division | Trainee specialist registration is specifically for medical practitioners who practise in individually numbered, identifiable postgraduate training posts. |
GPs, general practitioners.
This study was a cross-sectional mixed-methods survey of all registered medical practitioners in Ireland mandated to participate in MPC in 2018 (n=12 920).
Survey instrument
We designed a questionnaire to elicit doctors’ experience, attitudes and suggestions for improvement of MPC. We drew on several sources to develop the questionnaire. We reviewed the literature, held a focus group with doctors undertaking MPC and sought input from our knowledge-user research partners to identify key areas of interest. The theory of planned behaviour (TPB)12 acted as a sensitising concept in the design of the survey. TPB posits that an individual’s attitude towards a behaviour, the subjective norms relating to that behaviour and the individual’s perceived control of the behaviour, shape behavioural intentions and the behaviour itself.12 In the case of MPC, this focused attention not only on doctors’ attitudes to MPC, and the barriers to participation they encountered, but also on their perceptions of the attitudes of others such as patients and colleagues, and the consequences of failure to participate. The questionnaire was piloted with a further group of doctors’ (n=30) representative of our target population, following which it was further revised and refined to improve clarity and length. The final version of the questionnaire consisted of 30 statements relating to MPC and 3 free text questions. A Likert-type format was used for the statements with five response codes ranging from 1=strongly agree to 5=strongly disagree. A copy of the questionnaire can be found in online supplemental appendix A.
bmjopen-2020-042183supp001.pdf (275KB, pdf)
Patient involvement
The research team included Mrs Margaret Murphy, a patient safety advocate and then External Lead Advisor, WHO Patients for Patient Safety, a network of 200+ patient safety champions from 51 countries. Mrs Murphy was a member of the project steering committee. She approved the design and conduct of the study and contributed to design of the questionnaire. Patient perspectives were reflected in items addressing the impact of MPC on patient outcomes, doctors’ perceptions of the importance of MPC to patients and the possibility of patient feedback contributing to doctors’ MPC.
Data collection
All doctors registered with the Medical Council are required to complete an online annual retention of registration process. In June/July 2018, information about the survey and a link to complete it were included in the process as a pop-up targeting those in the relevant divisions of the register. The information and link were also sent in email reminders to doctors in the weeks following the annual retention process. Survey responses were linked to demographic data held by the Medical Council using registration numbers. Once the data was collated, the registration numbers were removed and replaced with participant numbers to anonymise the data.
Data analysis
Descriptive statistics (frequencies and percentages) were generated to describe both the demographic characteristics of respondents and responses to each survey item. Proportional odds regression models were used to formally test the associations between responses to attitudinal items and intention to comply with the requirements of MPC. To validate the survey instrument, we estimated a full confirmatory factor analysis model with four latent factors based on the various Likert response survey questions organised under headings drawn from the TPB: attitudes; facilitators; barriers and social norms. To accommodate the ordered categorical nature of the indicators, we used a robust weighted least squares estimator. We calculated factor scores for each participant based on the model result and explored associations between these factor scores and demographic characteristics with confidence of capability to comply with requirements of MPC and intention to comply. Thematic analysis13 was conducted on the responses to the open-ended survey questions.
Results
There were 5368 responses to the survey from a population of 12 920, giving a response rate of 41.5%. Men accounted for 61% of responses. Median age was 47 years (IQR: 38–56 years). Fifty-eight per cent were in the specialist division of the register, 39% were in the general division and 0.7% in the supervised division. Fifty-six per cent had gained their basic medical qualification (BMQ) in Ireland and a further 14% within the European Union. Respondents were representative of the survey population, with slight over representation of men (61.2% vs 57.7%) and doctors registered in the general division (39.3% vs 36.5%). There was a good representation across specialties and countries of BMQ. Graduates of Irish medical schools were slightly under-represented in the General Division (29.4% vs 27.4%) and over-represented in the specialist division (73.8% vs 79.4%).
The majority of respondents held positive views on the general benefits of MPC, agreeing that it reassures patients and the public (65%), encourages doctors to continually learn and keep up to date (77%) and raises the standard of practice of all doctors (62%). At a more personal level, being encouraged to participate in educational activities was the most agreed benefit (70%), followed closely by being encouraged to reflect more on one’s professional development (67%).
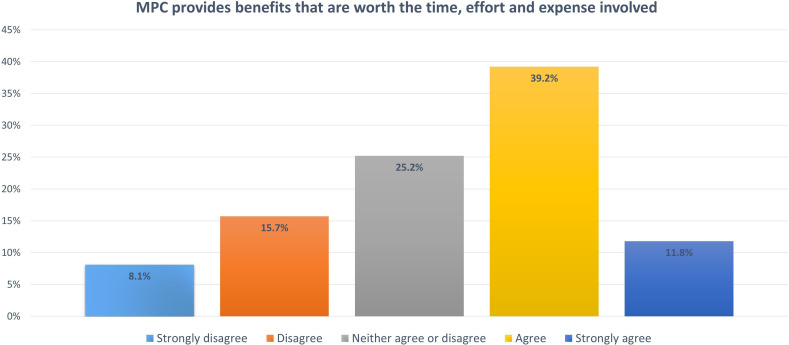
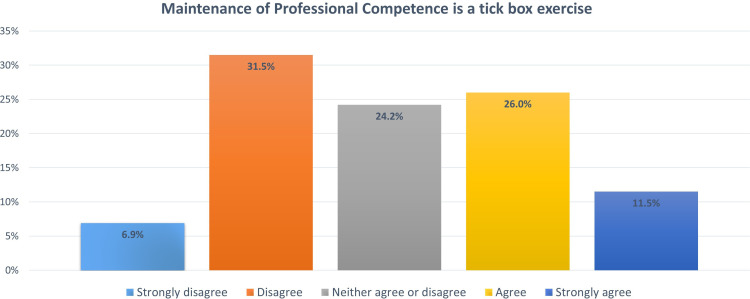
When the benefits were set against the time, effort and expense involved in the process, only 51% agreed that MPC was a worthwhile exercise (see figure 1) and 38% agreed with the statement that MPC was a tick-box exercise (see figure 2). MPC was considered to have resulted in changes in practice by a small majority (53%). MPC was not seen as being particularly important to patients (57%) or to colleagues (56%) and only 58% felt that non-compliance risked removal from the register.
Figure 1.
Distribution of responses to the statement that MPC provides benefits that are worth the time, effort and expense involved. MPC, maintenance of professional competence.
Figure 2.
Distribution of responses to the statement that maintenance of professional competence is a tick-box exercise.
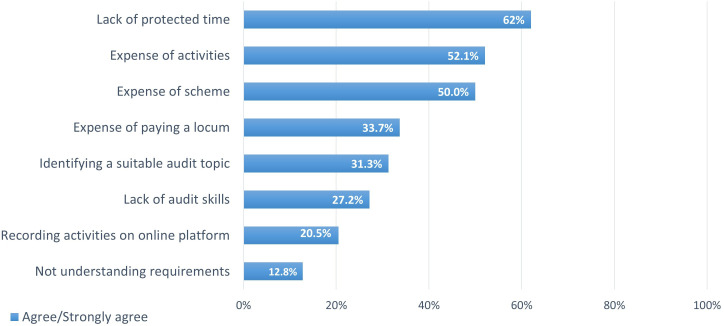
Barriers to participation in MPC
The main barriers to participation were lack of protected time and expense (see figure 3). Expense of locum cover to allow participation in CPD was also a significant barrier. Audit skills were lacking in a significant minority (27.2%). Doctors ≤34 years of age or over 55 years were more likely to report these difficulties (35% and 32%, respectively, p<0.001).
Figure 3.
Barriers to meaningful engagement with maintenance of professional competence.
A small group of doctors (12.8%) did not understand what they were required to do to maintain professional competence. A small majority (55%) agreed that current arrangements and information were sufficient. A significant minority expressed ambivalence or dissatisfaction with their ability to access high-quality CPD. Fourty-nine per cent disagreed or were ambivalent towards the statement that they match their choice of CPD to their learning needs.
Respondents provided over 1300 comments relating to barriers to meaningful participation in MPC. Six themes, with associated subthemes, were identified, and are outlined in table 2, ranked by frequency. Illustrative quotes are shown along with the respondent’s area of practice, area of BMQ (Ireland, other EU and non-EU) and division of the register.
Table 2.
Barriers to meaningful engagement with MPC—themes and subthemes
| Barriers | Barrier subthemes |
| Time involved in meeting the requirements of MPC | Time for participation in MPC activities
|
| MPC time vs personal time | |
| Expense of participation in MPC | Cumulative expense of MPC |
| Impact of expense on the selection of CPD activities | |
| Insufficient CPD funding | |
| Expense related to specific groups of doctors | |
| Availability and quality of CPD activities | Lack of relevance of CPD courses to scope of practice
Difficulty of accessing CPD course
|
| Employment status | Working abroad
|
| Not employed in Ireland (looking for jobs) | |
| Non-full-time employment | |
| Maternity or sick leave | |
| Non-clinical role | |
| Record keeping | Tedious and time-consuming process |
| Cumbersome online platform | |
| Audit | Lack of skills, training and support |
| Frequency of audit | |
| Lack of relevance to scope of practice | |
| Time-consuming process |
CPD, continuing professional development; MPC, maintenance of professional competence.
Consistent with the Likert-scaled responses, the time and expense of participation in MPC were the most frequently cited barriers.
Time involved in meeting the requirements of MPC
‘After a 10–12 hour very difficult day it can really interfere with personal time leading to stress and reduces time for family and friends. Due to increased pressures in primary care, paper work on call practice management etc. CPD while obviously very worthwhile has to be squeezed in and this leads to some resentment and less time for personal reading of which only 5 points are allocated.’ (GP, BMQ Ireland, specialist division)
Expense of participation in MPC
‘I am forced to usually only choose free events and local to me due to time and financial constraints, so I do not get to actually choose the things that would be most beneficial educationally. This is because locum costs or costs from family life/babysitters etc. is too much and if there are also course fees it is just not financially viable.’ (GP, BMQ Ireland, specialist division)
Some felt that the allowance or subsidy that they receive for CPD activity was inadequate. Specific groups of doctors such as those on maternity leave, non-partner general practitioners (GPs), non-consultant hospital doctors (NCHDs) and locums found it particularly challenging to cover the cost related to meeting the requirements of MPC.
‘I feel that non-partner/non-[principal] GPs are at a significant disadvantage, the cost of CPD in addition to paying out of pocket for Medical council etc. None of these costs are tax deductible for us. Everything is straight out of our pocket. We do not get a payment for study leave as [GP principals/ partners] do. We also face discrimination. as we have to continue to complete CPD with no maternity leave payments.’ (GP, BMQ Ireland, specialist division)
Availability and quality of CPD materials
The availability of CPD to match doctors’ scope of practice, and the quality of the CPD, were the main barriers under this theme. Repetitive content, the geographical concentration of events in Dublin and poor availability of online courses were cited.
‘The standard of educational activities provided by the relevant training bodies can be quite weak and repetitive in Ireland.’ (Psychiatry, BMQ Ireland, specialist division)
Employment status
Doctors not in full-time clinical employment in Ireland found it challenging to meet the requirements of MPC.
‘Working as a locum or as a sessional doctor for short periods is a barrier to carrying out audit. Maternity leave - possible to get external points but internal points and audit difficult to impossible. I was informed that I could make it up in later years. I do not think it is fair to ask people to do an extra audit to make up for time off on maternity leave. I moved city yearly since starting the CPD scheme and worked as locum, sessional work and other jobs. In that time, I also had a maternity leave… I found it difficult in those years to make up points’. (GP, BMQ Ireland, general division)
Record keeping
Recording of CPD activities on cumbersome online platforms was identified as a further barrier.
‘The process of recording activity through the online portal is a very tedious and time consuming. ….sitting down to spend a considerable amount of time engaging with the process is demoralising’. (Obstetrics and gynaecology, BMQ Ireland, specialist division)
Audit
Participants cited the audit as a barrier to participation in MPC. Issues relating to the audit included the lack of training, skills and information provided on how to conduct an audit. Many participants regarded audit as a pointless exercise with no clear benefit. Others believed audit was irrelevant to their practice and ‘only suitable for academics’. Some participants thought that the yearly audit was excessive and onerous, and would prefer an audit spread over a number of years.
Suggestions for improvement of MPC processes
The majority of respondents (58%) were not in favour of using patient feedback as part of MPC. Using feedback from colleagues also received a tepid reception with 51% agreeing that they would welcome it. Sixty-one per cent would like to see a quality improvement initiative option. Recommendations for improvement mirrored the barriers identified. Suggestions for improvement captured by the open-ended survey question are thematically outlined in table 3, and ranked by frequency.
Table 3.
Suggestions for improvement of MPC processes ranked by frequency
| Suggestion | Subthemes |
| Remove or change audit | Remove audit |
| Reduce audit frequency | |
| Audit alternative | |
| Provide additional support | Make allowances for individual circumstances |
| Provide more information | |
| Increase the quality and range of CPD activities | Provide more online courses |
| Increase the quantity, quality and variety of local CPD courses | |
| Reduce the expense of PCS and CPD courses | Subsidise CPD activities |
| Provide locum cover | |
| Make expenses tax deductible | |
| Changes to current scheme | Change points system |
| Introduce new methods | |
| Place more emphasis on learning | |
| Make participation voluntary | |
| More protected time | |
| Tailor PCS to specialty or scope of practice | Specialty specific requirements and courses |
| Recognition of non-clinical roles (ie, credit for teaching) |
CPD, continuing professional development; MPC, maintenance of professional competence; PCS, Professional Competence Scheme.
The most frequent suggested improvement was to remove or change the audit component.
‘The requirement to complete a full audit cycle within one year every single year encourages you to pick a subject dealing with small numbers so that it can all be completed in time. In my opinion, you should be allowed to carry out larger audits over a period of two or three years which would provide more useful and comprehensive information and therefore be much more beneficial. You could easily show evidence of working on the audit every year and this should be enough to satisfy the Medical Council in my view.’ (GP, BMQ Ireland, specialist division)
Participants felt that additional support should be provided by making allowances for individual circumstances and providing more information.
‘Allow excess points to be carried over from one year to the next. I feel the Colleges should be more aware and sensitive to individuals’ circumstances for example, illness, bereavement etc.’ (Radiology, BMQ Ireland, specialist division)
Provision of more online CPD, as well as improving the quality and quantity of offerings would make MPC a more useful experience for participants.
‘The body should be responsible for providing mandatory free online and in person educational activities, seminars and meetings covering all medical updates and specialties.’ (Psychiatry, BMQ non-EU, general division)
There were a variety of suggestions as to how expense of MPC could be reduced, including greater subsidies, provision of locum cover and making expenses tax deductible. Further suggestions included making changes to how CPD points are awarded, introduction of new methods to evaluate doctors and placing more emphasis on learning.
‘The basic premise of most educational activities being offered in these schemes as being of educational value is flawed. There is little value in sitting in a conference from an educational point of view. Learning needs to be more active and self-directed. Most CPD schemes to not facilitate this in any meaningful way.’ (Medical specialty, BMQ non-EU, general division)
In Ireland, doctors’ entitlement to study leave varies according to role. Those not currently entitled to such leave identified this as an area to be addressed.
‘We should have protected time included in our contract. It’s ridiculous having to go at night in the winter and give up weekend family time to go to meetings.’ (GP, BMQ Ireland, general division)
Finally, respondents suggested greater tailoring of the requirements of MPC to doctors’ scope of practice.
‘PCS at the moment is general and you can fill education or courses you like. I think it would be more productive if stratified into subspecialties, that might help people stay more focused and sharp into one speciality and relevant education.’ (Medical specialty, BMQ non-EU, general division)
Confidence in ability to meet requirements of MPC
Eighty-seven per cent of respondents agreed that they were confident that they could meet the requirements of MPC. A proportional odds regression model showed that confidence in meeting requirements was related to more positive attitudes to MPC, but not related to respondent characteristics, for example, gender or division of the register.
In total, over 700 doctors said that they were not confident that they could meet requirements. Of these, 315 provided comments explaining why they lacked confidence. Five main reasons and associated subthemes were identified, which are outlined in table 4 and ranked by frequency.
Table 4.
Reasons for lacking confidence in ability to meet requirements of MPC
| Reason | Subthemes |
| Employment status | Not in full-time practice |
| Non-clinical role | |
| Maternity leave | |
| Working abroad | |
| Sick leave | |
| Career break | |
| Lack of time | Cover for clinical work |
| Busy clinical workload | |
| Personal/family time | |
| Audit | Time |
| Lack of skills, training and support | |
| Employment status | |
| Expense | |
| Quantity and quality of CPD courses | Lack of relevant CPD courses |
| Not enough online courses |
CPD, continuing professional development; MPC, maintenance of professional competence.
Intention to comply with MPC
Seventy-seven per cent stated that they intended to comply with requirements. Twenty-three per cent were either unsure or disagreed.
Associations between Likert-scaled survey items and intention to comply were estimated using proportional odds regression models. This confirmed the relationship between intention to comply and positive attitudes to MPC, weaker endorsement of barriers to MPC, stronger endorsement of facilitators and stronger endorsement of social norms, for example, importance to patients. This was similar to the findings in relation to confidence of ability to comply.
Relationship between gender, region of BMQ, division of the register, role, service model, nationality and intent was significant only for gender and region of BMQ. Men and those who obtained their BMQ outside Ireland were more uncertain of their intention to comply with the requirements of MPC.
Discussion
This study was the first national survey of doctors’ attitudes towards MPC since its introduction in Ireland in 2011. While attitudes to MPC were generally positive, up to one-third of doctors were unconvinced of its impact. The time, effort and expense involved in MPC outweighed any perceived benefit for half of doctors. A significant minority (38%) felt that MPC is a tick-box exercise and over 40% did not view MPC as important to patients or colleagues, or consequential in terms of sanction from the Medical Council. Seventy-seven per cent of respondents stated a definite intention to comply with the requirements of MPC, which is surprisingly low in the context of the legal requirement to do so. Those who were less certain of intention to comply held more negative views of the process, in terms of general attitudes, perception of impact on own practice and endorsement of the presence of multiple barriers to participation. These findings point to the importance of convincing doctors that MPC is worthwhile. Being male, or having a BMQ from outside Ireland, also predicted greater likelihood of not expressing firm intention to comply.
Engaging doctors in MPC in a meaningful way requires clear communication of the purpose of the process and explicit linkage of the mandated activities to that purpose. Confusion about the objectives of MPC and lack of evidence of its effectiveness have hampered doctors’ commitment to the process internationally.6 14 The findings of this research suggest that a similar situation prevails in Ireland. While promotion of MPC and the PCS schemes in Ireland refer to doctor competence, quality of care and patient safety,9 the requirements currently in place are aimed primarily at assuring doctors’ attendance at approved CPD sessions. The relationship between CPD and competence, quality of care and patient safety is supported by limited evidence,3 15 which may explain the significant minority of doctors who were unconvinced of its impact in enhancing standards of medical practice and reassuring the public.
Furthermore, 49% of respondents to our survey disagreed or were ambivalent towards the statement that they match their choice of CPD to their learning needs. Qualitative comments suggest that convenient timing and location, availability and expense contribute to the choice of CPD undertaken. Thus, MPC can become a tick-box exercise, focused on scoring the required points before the annual deadline rather than meeting learning needs. While the compulsory annual audit might have been expected to be a useful activity embedded in doctors’ day-to-day practice, our findings suggest that, on the contrary, it is seen by many a time consuming and ineffective exercise. Comments suggested that the single year timeframe forces a decision to do small-scale audits that have little perceived impact. This goes some way to explaining why only 53% of respondents agreed that their own practice had been impacted by participation in MPC. Removal of the audit, or change to the requirements relating to it, was the most frequent suggestion to improve MPC. The literature suggests that any model of MPC that seeks to impact practice should feature a facilitated approach through activities such as regular performance review, appraisal, mentoring, etc,3 something that is lacking in the current Irish system. Facilitation can involve exploration of learning needs, targeted choice of CPD and linking audit to practice. It has also been shown to provide emotional support and to enhance engagement with the process.16
Inadequate resourcing of MPC was evident in the barriers to engagement identified by respondents. Time associated with participating in the MPC process was the greatest barrier. Heavy workload, requirement to travel and to record CPD activities, and the demands this placed on personal time were among the difficulties arising. Respondents repeatedly referred to the need for funded protected time for MPC, including provision of locum cover. The current strain in the Irish health system, with short staffing and heavy service demands, can make it challenging for those entitled to study leave to take it. Time constraints are cited internationally as a barrier to MPC.17 18
Expense of participation in MPC was the second-most endorsed barrier. Internationally, the question of who should bear the expense of MPC is a hotly contested topic. Our respondents’ comments echo the concerns of doctors in other jurisdictions that MPC is a money-making exercise for those who regulate and run programmes.15 Doctors pay annual registration fees to the Medical Council, membership or fellowship fees to postgraduate training bodies and professional indemnity fees. The addition of a fee for enrolment in a PCS, fees for CPD activities and the associated locum cover, travel and accommodation add up to significant expense. Respondents indicated that this is an issue particularly for doctors for whom professional expenses are not tax deductible and who may not have a CPD allowance, those working less than full-time, as NCHDs or salaried GPs and those taking maternity/parental or sick leave. While some doctors do have an allowance for CPD activities, this varies across different groups and is not universal.
If MPC programmes are to be successful, CPD to match learning needs must be readily available and of high quality. Respondents commented that available CPD was of limited range and tended to be repetitive. Geographical location, excessive expense, inadequate advertising/notice and limited places all contributed to inaccessibility of current CPD offerings. A strong preference for greater availability of online learning was expressed, as well as greater variety and better quality courses outside Dublin. Recent work in the Irish context has documented the broad CPD needs of both GPs and hospital consultants and provides useful information to support more effective provision of CPD.19–22
The vast majority of doctors understood what the requirements for MPC were, but many did not find PCS sufficiently flexible or information provided adequate. Foremost among suggestions for improvement was the provision of more information and support for doctors. Greater flexibility, reflecting recognition of the individual circumstances of doctors, for example, sick leave, was also felt to be important. This included allowing greater flexibility between categories of points and requiring fewer points from part-time workers. The arbitrary nature of the threshold of 50 CPD points would suggest that these are reasonable suggestions.
There is a subgroup of doctors for whom the combination of expense and the specific requirements of MPC present a real challenge. Thirteen per cent of respondents expressed lack of confidence in their ability to meet MPC requirements. The main reason cited for lack of confidence was employment status. Meeting the requirements of MPC is particularly challenging for those working less than full time, in locum posts, in non-clinical roles, taking maternity or sick leave and those living outside Ireland for part of the year. Again, this is something that is common across other jurisdictions.23 Greater flexibility in requirements would support participation among this group.
Strengths and limitations
Among the strengths of this study are the diverse stakeholders involved in the research, the strong response rate to the questionnaire and the representativeness of the respondents. Survey design was undertaken in accordance with best practice, informed by literature and theory. Post-hoc analysis of the survey confirmed its validity. Although the response rate to the survey was excellent, there were still large numbers of non-responders. We cannot be sure that the findings presented here represent the views of non-responders.
Conclusions
We have presented the views of over 5000 doctors participating in MPC in Ireland. The problems with implementation of MPC identified in this study are not unique to the Irish context. As MPC continues to evolve internationally, other jurisdictions grapple with the same challenges. Enhancing doctors’ engagement in MPC in Ireland will require a comprehensive strategy focused on better communication, adequate resourcing and ongoing evaluation of the process.
Supplementary Material
Acknowledgments
We would like to acknowledge the support of the Health Research Board, Ireland, and the contribution of our research partners: Professor Hilary Hoey, Director of Professional Competence, Royal College of Physicians of Ireland, Dublin, Ireland; Dr Philip Crowley, National Director for Quality, Health Service Executive, Dublin, Ireland; Mrs Margaret Murphy, External Lead Advisor, World Health Organisation Patients for Patient Safety Ireland; Professor Dubhfeasa Slattery, formerly Head of Clinical Risk at the State Claims Agency, Dublin, Ireland, currently Professor of Professionalism, Royal College of Surgeons of Ireland, Dublin, Ireland; Professor Ellen O’Sullivan, Chair, Irish Forum of Postgraduate Training Bodies, Dublin, Ireland; Professor Mary Horgan, President of the Royal College of Physicians of Ireland, Dublin, Ireland; and Dr Graham McMahon, President and Chief Executive Officer, Accreditation Council for Continuing Medical Education, USA. We are grateful to Ireland’s doctors who shared their perspectives with us on this important topic in great numbers.
Footnotes
Twitter: @statsepi, @DeirdreMBennett
Contributors: DB designed the study. JO'F, AW, JC and DB designed the questionnaire. JO'F and JC administered the questionnaire and collected the data. DD performed the statistical analysis. All authors contributed to the analysis and interpretation of the data, have agreed both to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved and the resolution documented in the literature. EG, AW and DB drafted the paper which was edited and approved by all authors.
Funding: This work was supported by the Health Research Board, Ireland, grant number APA-2016–1869.
Competing interests: Two of the authors, JO'F and JC, are employed by the Medical Council of Ireland. The Medical Council of Ireland is the regulatory body for doctors responsible for the maintenance of competence programme that is the focus of this research.
Patient consent for publication: Not required.
Ethics approval: Ethical approval was granted by the Social Research Ethics Committee, University College Cork (reference no. 2017–118). Informed consent was obtained from all participants.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. The datasets generated and/or analysed during the study are not publicly available due to participants not having consented to public availability, but are available from the corresponding author on reasonable request: d.bennett@ucc.ie.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Sklar DP. What happens after medical school? current controversies about licensure, maintenance of certification, and continuing professional development. Acad Med 2016;91:1–3. 10.1097/ACM.0000000000001011 [DOI] [PubMed] [Google Scholar]
- 2.Dixon-Woods M, Yeung K, Bosk CL. Why is U.K. medicine no longer a self-regulating profession? The role of scandals involving "bad apple" doctors. Soc Sci Med 2011;73:1452–9. 10.1016/j.socscimed.2011.08.031 [DOI] [PubMed] [Google Scholar]
- 3.Archer J, Pitt R, Nunn S, et al. . The evidence and options for medical revalidation in the Australian context. UK: Plymouth, 2015. [Google Scholar]
- 4.Horsley T, Lockyer J, Cogo E, et al. . National programmes for validating physician competence and fitness for practice: a scoping review. BMJ Open 2016;6:e010368. 10.1136/bmjopen-2015-010368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shaw K, Cassel CK, Black C, et al. . Shared medical regulation in a time of increasing calls for accountability and transparency. JAMA 2009;302:jama.2009.1620:2008–14. 10.1001/jama.2009.1620 [DOI] [PubMed] [Google Scholar]
- 6.Tazzyman A, Ferguson J, Walshe K, et al. . The evolving purposes of medical revalidation in the United Kingdom. Acad Med 2017;93:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miller SH. American Board of medical specialties and repositioning for excellence in lifelong learning: maintenance of certification. J Contin Educ Health Prof 2005;25:151–6. 10.1002/chp.22 [DOI] [PubMed] [Google Scholar]
- 8.Merkur S, Mossialos E, Long M, et al. . Physician revalidation in Europe. Clin Med 2008;8:371–6. 10.7861/clinmedicine.8-4-371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Medical Council Professional competence; promoting quality assurance. Dublin, Ireland, 2010. [Google Scholar]
- 10.Medical Council Maintenance of professional competence. Report of progress 2011-2018. Dublin, Ireland, 2018. [Google Scholar]
- 11.Hanlon H, Prihodova L, Russel T. Benefits and barriers to participating in mandatory continuing professional development scheme in doctors in Ireland : Association for medical education in Europe annual scientific meeting. 8 Vienna: AMEE, 2019. [Google Scholar]
- 12.Ajzen I. From intentions to actions: A theory of planned behavior : Kuhl J, Beckman J, Action-control: from cognition to behavior. Heidelberg: Springer, 1985: 11–39. [Google Scholar]
- 13.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 14.Archer J, Regan de Bere S, Nunn S, et al. . "No one has yet properly articulated what we are trying to achieve": a discourse analysis of interviews with revalidation policy leaders in the United Kingdom. Acad Med 2015;90:88–93. 10.1097/ACM.0000000000000464 [DOI] [PubMed] [Google Scholar]
- 15.Teirstein PS. Boarded to death--why maintenance of certification is bad for doctors and patients. N Engl J Med 2015;372:106–8. 10.1056/NEJMp1407422 [DOI] [PubMed] [Google Scholar]
- 16.NHS England, NHS Improvement . Medical Appraisal : Feedback from GPs in 2018-19. London, 2019. [Google Scholar]
- 17.Cook DA, Holmboe ES, Sorensen KJ, et al. . Getting maintenance of certification to work: a grounded theory study of physicians' perceptions. JAMA Intern Med 2015;175:35–42. 10.1001/jamainternmed.2014.5437 [DOI] [PubMed] [Google Scholar]
- 18.Ikenwilo D, Skåtun D. Perceived need and barriers to continuing professional development among doctors. Health Policy 2014;117:195–202. 10.1016/j.healthpol.2014.04.006 [DOI] [PubMed] [Google Scholar]
- 19.Maher B, O'Neill R, Faruqui A, et al. . Survey of Irish general practitioners' preferences for continuing professional development. Educ Prim Care 2018;29:13–21. 10.1080/14739879.2017.1338536 [DOI] [PubMed] [Google Scholar]
- 20.Maher B, Faruqui A, Horgan M, et al. . Continuing professional development and Irish Hospital doctors: a survey of current use and future needs. Clin Med 2017;17:307–15. 10.7861/clinmedicine.17-4-307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dowling S, Last J, Finnegan H, et al. . Does locally delivered small group continuing medical education (CME) meet the learning needs of rural general practitioners? Educ Prim Care 2019;30:145–51. 10.1080/14739879.2019.1573109 [DOI] [PubMed] [Google Scholar]
- 22.Dowling S, Last J, Finnegan H, et al. . What are the current “top five” perceived educational needs of Irish general practitioners? Ir J Med Sci 2019. [DOI] [PubMed] [Google Scholar]
- 23.Agius S, Baron R, Lewis B, et al. . What do GP educators perceive to be the opportunities and challenges of introducing revalidation? Educ Prim Care 2011;22:386–92. 10.1080/14739879.2011.11494041 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-042183supp001.pdf (275KB, pdf)