Abstract
Background: According to the clinical manifestation, tuberculosis (TB) is divided into pulmonary tuberculosis (PTB) and extrapulmonary tuberculosis (EPTB). The incidence rate of EPTB has increased in many countries. The demographic and clinical characteristics of EPTB in China remain still unclear.
Materials and methods: We retrospectively analyzed the medical records of 5,624 hospitalized patients with positive M. tuberculosis culture between January 2008 and June 2013 in Shandong province. We investigated the epidemiological, demographic, and clinical characteristics of patients with EPTB.
Results: Among 5,624 hospitalized TB patients with positive M. tuberculosis culture, 4,277 (76.05 %) had PTB, 618 (10.99 %) had EPTB, and 729 (12.96 %) had both PTB and EPTB. The proportion of EPTB increased significantly from 6.97 % in 2008 to 19.98 % in 2012 (p <0.001). The most frequent sites or foci of EPTB were pleura (63.27 %), followed by bone/joint (13.75 %), and lymph nodes (8.9 %). The mean duration of treatment for pleural TB was eight months and for EPTB in the other foci was more than 15 months.
Conclusion: The proportion of EPTB in Shandong province has significantly increased. Clinicians need to be aware of the trend and remain vigilant against EPTB. EPTB requires prolonged treatment, and clinical supervision should be strengthened to prevent drug resistance. HIPPOKRATIA 2020, 24(1): 27-32.
Keywords: Tuberculosis, extrapulmonary, epidemiology, clinical features, duration of treatment, Shandong, China
Introduction
The World Health Organization (WHO) estimated that ten million people were infected with tuberculosis (TB) in 2018. There were 1.2 million TB deaths among the HIV-negative people and 251,000 additional deaths among HIV-positive people in 20181. TB that affects the lungs is characterized as pulmonary TB (PTB), and TB, which affects other organs or tissues outside the lungs, is classified as extrapulmonary TB (EPTB). PTB is the most typical and common form of tuberculosis. The PTB patients who are sputum smear-positive on microscopy for acid–alcohol fast bacilli are the most contagious and have been a priority worldwide. However, available evidence on EPTB is limited and therefore needs more attention and action.
The proportion of EPTB among TB patients varies widely in different countries2-4. Moreover, an increased proportion of EPTB has been reported in studies originating from different countries4-6. Existing epidemiological studies have shown that the differences in gender, age, race, education level, and immune status were all associated with EPTB rates7-10. Therefore, the types and demographics of EPTB could be very different from region to region. In China, the proportion of EPTB in Beijing had increased to 31.4 %11, whilst in Tianjin, it was only 10.3 %12. At present, there are no reports on the proportion of EPTB in the Shandong Province.
EPTB is a severe clinical problem due to increased morbidity and mortality. Clinical manifestations of EPTB are diverse and atypical, and specimens for culture are difficult to obtain. Diagnosis is often based on radiological or histological features combined with symptoms and signs. However, positive culture of M. tuberculosis is the gold standard diagnosis13. Therefore, EPTB is often misdiagnosed. Also, prolonged treatment and lack of following-up specimens make diagnosis and treatment supervision for EPTB more challenging14,15. Early diagnosis and treatment improve the prognosis. The current study aimed to demonstrate the epidemiological, demographic, and clinical features of EPTB via retrospective data analysis from inpatients with positive M. tuberculosis culture.
Materials and methods
A definite case of tuberculosis refers to a patient with Mycobacterium tuberculosis complex identified from a clinical specimen, either by culture or by the newer molecular line probe assay method. We analyzed patients’ medical records with positive M. tuberculosis culture retrospectively from January 2008 to June 2013 in the hospitals responsible for TB prevention and control in the Shandong province. Approval for this study was obtained from the Ethics Committee of the First Affiliated Hospital of Shandong First Medical University (S320, 21/11/2019).
Patients of both gender, aged 15 years and older, were selected for the study regardless of the EPTB disease site. When a patient had several organs affected by EPTB, the patient was classified according to the most severely affected site. Other inclusion criteria were positive culture for M. tuberculosis of specimens obtained (sputum, bronchoalveolar fluid, hydrothorax, abdominal fluid, cerebrospinal fluid, urine, lymph nodes, puncture fluid, biopsy tissues, ect.) and utilizing the improved Lowenstein-Jensen medium for the culture. Lastly, availability for collection and evaluation of all admission and discharge records, intact results of clinical laboratory tests and accessory examinations, and all surgical operation notes. Patients who were under 15 years or had a negative culture for M. tuberculosis were excluded.
The patients’ demographic and clinical data were collected using standard data collection forms. The EpiData Entry software, version 3.1 (EpiData Association, Odense, Denmark) was used for data entry and management. We applied for statistical analysis Excel datasheets generated automatically by the system.
Statistical analysis
Frequencies and means were used to describe the distribution of qualitative and quantitative data, respectively. Pearson’s chi-squared test was performed to compare the distribution of the categorical variables among groups. If variance among groups was equal, one-way ANOVA was used to examine the difference of means of continuous variables; otherwise, the Wilcoxon rank-sum test was used. Trend chi-square test was used to explore the linear trend of the proportion of EPTB. Logistic regression was carried out to identify factors associated with EPTB. All reported probabilities (p values) were two sided and p <0.05 was considered statistically significant. Statistical analyses were performed using the IBM SPSS Statistics for Windows, Version 20.0 (IBM Corp., Armonk, NY, USA).
Results
From January 2008 to June 2013, 5,624 patients with positive M. tuberculosis culture were hospitalized. Of these patients, 76.05 % (4,277) had PTB, 10.99 % (618) had EPTB, and 12.96 % (729) had concurrent PTB and EPTB (Figure 1). The changes in EPTB proportion in the tuberculosis patients were compared between 2008 and 2012 after removing the cases of concurrent PTB and EPTB. The proportion of EPTB significantly increased from 6.97 % in 2008 to 19.98 % in 2012 (p <0.001, Figure 2).
Figure 1. Flow chart of data acquisition regarding patients’ medical records with positive M. tuberculosis culture retrospectively from January 2008 to June 2013 in the hospitals responsible for TB prevention and control in the Shandong province. PTB: pulmonary tuberculosis, EPTB: extrapulmonary tuberculosis, PCR: polymerase chain reaction.
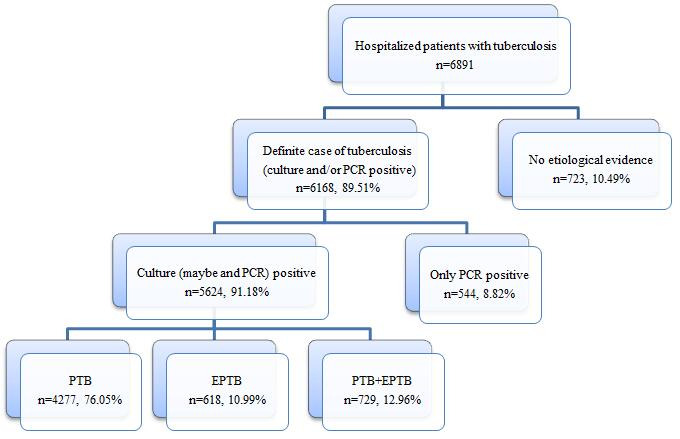
Figure 2. Relative rates of pulmonary tuberculosis and extrapulmonary tuberculosis over the years 2008-2013 in the Shandong province, China. PTB: pulmonary tuberculosis, EPTB: extrapulmonary tuberculosis.

Regarding patients with EPTB, their mean age was 30 years, 75.73 % were male, 55.99 % were urban residents, and 7.61 % had a tuberculosis history; one case was known to be HIV co-infected. Regarding patients with only PTB, their mean age was 37 years, 65.82 % were male, 28.71 % were urban residents, and 5.66 % had a tuberculosis history. The characteristics of TB cases and cases with concurrent PTB and EPTB are shown in Table 1.
Table 1. Demographic and clinical characteristics of patients with tuberculosis in Shandong province, China, during 2008-2013.
n: number, TB: tuberculosis, PTB: pulmonary tuberculosis, EPTB: extrapulmonary tuberculosis, IQR: interquartile range
Logistic regression was performed to identify the factors associated with EPTB. On multivariable analysis, EPTB patients were more likely to be male [odds ratio (OR): 1.34, 95 % CI: 1.16-1.55; p =0.007] and had a history of TB (OR: 9.05, 95 % CI: 6.88-11.9; p =0.005) compared with PTB patients (Table 2). They were also more likely to be urban residents and younger (p =0.002), while HIV co-infection was not associated with EPTB (p =0.709).
Table 2. Factors associated with extrapulmonary tuberculosis.
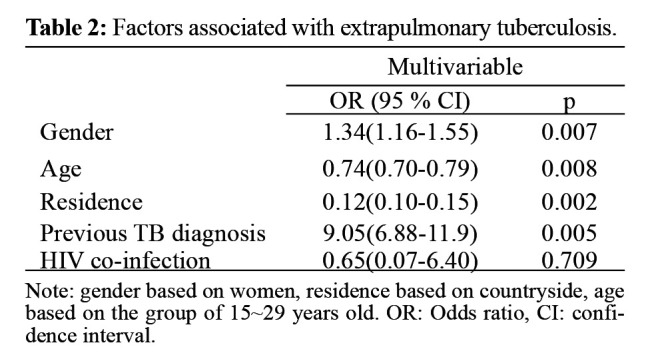
Note: gender based on women, residence based on countryside, age based on the group of 15~29 years old. OR: Odds ratio, CI: confidence interval
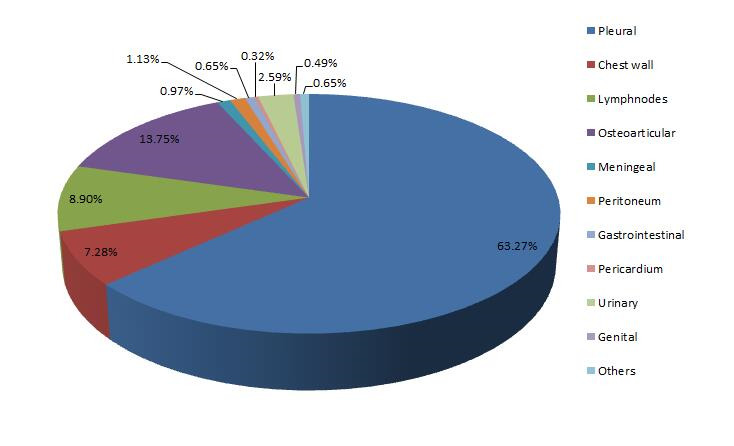
In the 618 EPTB cases, the most frequent infection focus was pleura (in 391 patients; 63.27 %), followed by bone/joint (85; 13.75 %). Additional foci of EPTB were lymph nodes (55; 8.9 %), chest wall (45; 7.28 %), and urinary system (16; 2.59 %) (Figure 3). The category of “other” was composed of four patients (0.65 % of EPTB cases) who had various sites affected, including liver, perianal, and skin.
Figure 3. Extrapulmonary tuberculosis disease sites among the 618 hospitalized patients in Shandong province, China, during 2008-2013.
Among the 391 pleural TB patients, in 375 (95.91 %), TB was limited to the pleura, while 16 (4.09 %) had other infected foci besides the pleura. For these patients, the male to female ratio was 2.93:1, and the mean age was 28 years. There were 224 (57.29 %) patients with right-side pleural lesions, 142 (36.32 %) with left-side pleural infection, and 25 (6.39 %) patients with bilateral pleural pathology. Thirty-two patients were lost to follow-up and were not included in the study; thus, we retrospectively analyzed 359 pleural TB patients’ complete clinical records. The most common clinical symptom was chest pain (320; 89.14 %), and more than half of the patients had no systemic TB symptoms (216; 60.17 %). Fever was the most common toxic TB symptom (125; 34.82 %). During their treatment, all patients underwent thoracentesis, 285 (79.39 %) had an indwelling chest drainage tube placed, and 40 (11.14 %) underwent decortication. Most patients received first-line anti-TB drugs (Table 3). The total treatment duration ranged from six to 19 months, with a mean time of eight months. Most patients were compliant, and the overall prognosis was good. However, 11 (3.06 %) patients had poor compliance resulting in their delayed cure and extended treatment duration.
Table 3. Information of treatment for the 618 hospitalized patients with extrapulmonary tuberculosis in Shandong province, China, during 2008-2013.
M: months.
Among the 85 osteoarticular TB patients, in 67 (78.82 %), TB was limited to the bone or joint, while 18 (21.18 %) had other foci. The male: female ratio was 1.28:1, and the mean age was 34 years. In total, 179 bone or joint lesions were involved, 143 of which were vertebral lesions (Figure 4). The most common clinical symptom was pain and tenderness (in 65 patients; 76.47 %), followed by functional limitation (41; 48.24 %). More than half of the patients had no systemic TB symptoms (49; 57.65 %). The most common toxic symptom (32; 37.65 %) was Night sweats, followed by fever (29; 34.12 %). During treatment, 81 (95.29 %) patients underwent surgery or invasive procedures. Two patients discontinued treatment (one for economic reasons) after three and eight months of treatment, respectively. The remainder 83 patients received the full course of medication treatment. The total treatment duration ranged from eight to 34 months, with a mean time of 19 months. The overall prognosis was good. However, eight (9.41 %) patients had a residual functional limitation.
Figure 4. Anatomic site affected, for the 85 hospitalized patients with osteoarticular tuberculosis in Shandong province, China, during 2008-2013.

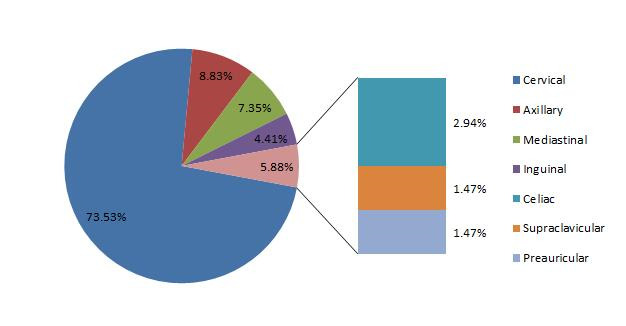
Among 55 lymphatic TB patients, in 53 (96.36 %), TB was limited to the lymph nodes, while two (3.64 %) also had other lesions. For these patients, the male to female ratio was 1.05:1, and the mean age was 26 years. A total of 68 lymph nodes were involved. The most frequent site was the cervical chain lymph nodes (50; 73.53 %) (Figure 5). One patient was lost to follow up and was not included in the analysis. More than half of the patients had no systemic TB symptoms (28; 51.85 %). Only three (5.55 %) patients had typical systemic TB symptoms. Most patients had multiple lymph node lesions (46; 85.19 %), and rarely (8 patients; 14.81%) a single lymph node was affected by TB. During treatment, 51 (94.44 %) patients received surgery or invasive procedures. One patient discontinued treatment after two months, and one succumbed. The other 52 patients had good compliance. The total treatment duration ranged from six to 42 months, with a mean duration of 15 months.
Figure 5. Anatomic site affected, for the 55 hospitalized patients with Lymphatic tuberculosis in Shandong province, China, during 2008-2013.
Among the 45 patients with TB of the chest wall, 25 (55.56 %) had only chest wall lesions, while 20 (44.44 %) had other sites’ involvement. The male to female ratio was 2.29:1, and the mean age was 29 years. There were 28 (62.22 %) patients with lesions on the right side of the chest wall and 17 (37.78 %) on the left side. The most frequent location of the chest wall TB was the right anterior (21; 46.67 %), followed by the left anterior (11; 24.44 %), and the right lateral (5; 11.11 %) chest wall. Most patients had no systemic TB symptoms (34; 75.56 %) and/or respiratory symptoms, but solely the chest wall mass. During treatment, 40 (88.89 %) patients received surgery or invasive procedures. All those patients completed drug therapy except for one patient who died. The total treatment duration ranged from eight to 36 months, and the mean treatment duration was 18 months.
Regarding the 16 patients with urinary tract TB, in the 12 (75 %), TB was localized to the urinary system, while four (25 %) also had other lesions. The male to female ratio was 1.24:1, and the mean age was 44 years. In total, 25 urinary tract sites were infected. The most frequent location was the kidney (13; 52 %), followed by the ureter (8; 32.0%). Only five patients had solely renal TB, and all the others were multiple lesions located at the kidney, ureter, and/or bladder. Systemic TB symptoms were relatively rare. The most common symptoms were frequent urination and urinary urgency (10; 62.5 %), followed by urodynia (7; 43.75 %). Macroscopic hematuria was relatively rare (2; 12.5 %). Two patients underwent renal abscess drainage during their treatment, one patient underwent ureterectomy and ureteral bladder transplantation, and the other 13 patients received only anti-TB drug therapy. One patient with M. tuberculosis resistant to amikacin and levofloxacin was treated for 24 months. The remaining patients completed treatment within 6 to 18 months, with a mean treatment duration of 15 months.
Discussion
Shandong is the second most populous province in China (100.7 million). The annual TB registration rate was 32.7 per 100,000 population, which was at a lower level in the country. In the present study, we analyzed the epidemiologic and clinical characteristics of EPTB in Shandong province, China. The proportion of EPTB had significantly increased in recent years. The possible reasons are correlated with the fact that the improvement of economic and medical levels enables more and more patients with EPTB seeking medical treatment, leading to an increase in the diagnostic rate. At the same time, the number of PTB had dropped. In previous reports, higher proportions of female patients were observed16. However, in agreement with the findings of a study originating from Saudi Arabia17, our study showed EPTB was more common among males with a high (2.93:1) male to female ratio of pleural TB.
The susceptible age for the development of EPTB has been reported variably in previous reports. Some studies have found the mean age of osteoarticular TB to be over 60 years of age18,19. However, similar to previous Chinese study20, we found osteoarticular TB to be more common in young subjects (mean age 34 years).
A recent study showed that EPTB patients were more often HIV-positive compared to PTB patients21. Among patients hospitalized with EPTB, patients co-infected with HIV and low CD4 counts were more likely to have severe disease22. In the present study, from the 5,624 TB patients included, only four were HIV positive. We found no correlation between EPTB and HIV infection. This may be due to the fact that Shandong has a low incidence of HIV infection.
Pang et al11 reported that the most frequent form of EPTB in China was osteoarticular TB. However, we observed the most common site to be pleura, followed by bone/joint, and lymph nodes. Specifically, most pleural TB was unilateral, and the right side was more commonly affected. Only 6.39 % of patients with pleural TB had bilateral pleural lesions. The spine is the most common osteoarticular TB site, but the most vulnerable vertebral region is unclear. Previous studies showed the lumbar vertebrae to be the most common20, while other the thoracic vertebrae23. We also found vertebrae to be the most common osteoarticular TB site, and thoracic vertebrae the most frequently affected, followed by lumbar vertebrae.
Our finding that the most frequent lymphatic TB site was the cervical chain lymph nodes is consistent with a previous report14, while most patients with urinary TB had complex lesions involving the kidney, ureter, and/or bladder. The chest wall location of EPTB was included in this study. We found that the most susceptible site was the anterior chest wall, of which the right anterior area was more commonly affected than the left.
In the current study, there were 78 patients with positive M. tuberculosis culture in the cerebrospinal fluid, including five (6.4 %) patients with only TB meningitis, 52 (66.7 %) patients with PTB and TB meningitis, and 21 (26.9 %) patients with concurrent TB meningitis and other EPTB; fact suggested that majority of TB meningitis would not occur as the only site of infection. The possibility of concurrent TB meningitis should be vigilant in diagnosing and treating other types of tuberculosis. Also, all 78 TB patients with meningeal involvement were tested by polymerase chain reaction (PCR) for M. tuberculosis in the cerebrospinal fluid (CSF), among which 42 (53.85 %) were positive; fact suggesting that the sensitivity of PCR in the diagnosis of TB meningitis is low, and in suspicious cases, the cause needs further investigating.
The general clinical manifestations of various EPTB are systemic TB symptoms (including fever, night sweats, loss of appetite, fatigue, and weight loss), which are also specific clinical manifestations of tuberculosis. In the current study, there were differences in the symptoms of the various types of EPTB. For example, fever was more common in patients with pleural TB, and night sweats were common in patients with osteoarticular TB. It is worthy of note that more than half of all patients had no systemic symptoms of TB. Therefore, clinical manifestations of EPTB were atypical and not enough to serve as the basis for diagnosis.
Because a drug sensitivity test was not routinely performed, a portion of the corresponding results were missing. There were two main reasons: i) some patients did not have a drug-susceptibility test due to economic or other reasons, and ii) few doctors failed to inform their patients timely to pay for the susceptibility test after receiving positive culture result. In the present study, among the 352 strains of M. tuberculosis tested for drug-susceptibility, five were drug-resistant, out of which one was multidrug-resistant (specimen from chest wall TB).
Anti-TB chemotherapy is the main treatment for EPTB. In the present study, most of the cases were treated with first-line anti-TB drugs, but levofloxacin and other second-line drugs were also utilized in a relatively high proportion. That was a phenomenon of drug abuse. Rifampicin is the first choice in clinical treatment with a change to rifapentine when there are apparent adverse reactions that cannot be tolerated. As a result, some patients were given both drugs during treatment. JieHeLing and YouFuNing are both Chinese patented medicines, and their main ingredients are both extracts of Euphorbia fischeriana Steud. However, China’s drug directions recommend different ranges of use, i.e., JieHeLing for lymphatic TB and YouFuNing for PTB and other TB types. These may be correlated with the different composition of wolfsbane extract.
There have been debates regarding optimal therapy. General guidelines recommend six months for EPTB patients, but tuberculous meningitis patients should have extended treatment duration. Previous studies found no significant difference in the outcomes between six and nine months24, and the course of treatment is often longer clinically. In our study, the mean duration of treatment for pleural TB was eight months; for the other sites was more than 15 months. In the case of osteoarticular TB, many experts prefer to complete treatment after 12 months or according to radiographic and/or pathological evidence. It is challenging to evaluate the efficacy and confirm cure. However, prolonged treatment is problematic, as compliance declines with longer treatment duration. Clinical supervision should be strengthened to ensure that cure is achieved and to prevent the emergence of drug-resistance.
Although anti-TB drugs have significantly reduced the need for surgery, this is still important for the treatment of EPTB. Most of the patients underwent drainage and/or focus cleaning in the study.
This study described the demographic and clinical characteristics of EPTB in Shandong province and demonstrated the current treatment status, which are areas of interest for clinical practice. However, there are also limitations in the study, i.e., we enrolled only hospitalized TB patients with positive M. tuberculosis culture but not included patients without positive culture and outpatients, which might bias the reported results. Furthermore, owing to the retrospective design, social and economic data were not captured and analyzed.
In conclusion, the study summarized the epidemiologic and clinical characteristics of patients with EPTB in Shandong province, China. A significantly increased proportion of EPTB has been demonstrated. Clinicians need to be aware of this increasing trend and raise awareness and vigilance of EPTB. There were still some problems in the treatment of EPTB, such as anti-TB drug abuse (especially second-line anti-TB drugs), prolongation of the treatment time, decreased compliance of patients, interruption of treatment, and even loss to follow-up. It is recommended to strengthen supervision during treatment to improve the disease’s treatment and prognosis, which may prevent the emergence of drug-resistant strains.
Conflicts of Interest
The authors declared no conflicts of interest.
Acknowledgements
The authors thank their colleagues: Baobao Feng, Meiyan Sheng, Lili Liu, Hongbo Liu, Qing Wang for data collection and Qiang Wang for guiding statistical analysis.
References
- 1.World Health Organization. Global tuberculosis report 2019. World Health Organization, Geneva, 2019. Avaliable at: https://www.who.int/publications/i/item/global-tuberculosis-report-2019.
- 2.Vachon J, Gallant V, Siu W. Tuberculosis in Canada, 2016. Can Commun Dis Rep. 2018;44:75–81. doi: 10.14745/ccdr.v44i34a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holden IK, Lillebaek T, Andersen PH, Bjerrum S, Wejse C, Johansen IS. Extrapulmonary Tuberculosis in Denmark From 2009 to 2014; Characteristics and Predictors for Treatment Outcome. Open Forum Infect Dis. 2014;6:ofz388. doi: 10.1093/ofid/ofz388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis. 2009;49:1350–1357. doi: 10.1086/605559. [DOI] [PubMed] [Google Scholar]
- 5.Kruijshaar ME, Abubakar I. Increase in extrapulmonary tuberculosis in England and Wales 1999-2006. Thorax. 2009;64:1090–1095. doi: 10.1136/thx.2009.118133. [DOI] [PubMed] [Google Scholar]
- 6.Sandgren A, Hollo V, van der Werf MJ. Extrapulmonary tuberculosis in the European Union and European Economic Area, 2002 to 2011. Euro Surveill. 2013;18:20431. [PubMed] [Google Scholar]
- 7.Tahseen S, Khanzada FM, Baloch AQ, Abbas Q, Bhutto MM, Alizai AW, et al. Extrapulmonary tuberculosis in Pakistan- A nation-wide multicenter retrospective study. PLoS One. 2020;15:e0232134. doi: 10.1371/journal.pone.0232134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sreeramareddy CT, Panduru KV, Verma SC, Joshi HS, Bates MN. Comparison of pulmonary and extrapulmonary tuberculosis in Nepal- a hospital-based retrospective study. BMC Infect Dis. 2008;8:8. doi: 10.1186/1471-2334-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang Z, Kong Y, Wilson F, Foxman B, Fowler AH, Marrs CF, et al. Identification of risk factors for extrapulmonary tuberculosis. Clin Infect Dis. 2004;38:199–205. doi: 10.1086/380644. [DOI] [PubMed] [Google Scholar]
- 10.Gomes T, Vinhas SA, Reis-Santos B, Palaci M, Peres RL, Aguiar PP, et al. Extrapulmonary tuberculosis: Mycobacterium tuberculosis strains and host risk factors in a large urban setting in Brazil. PloS One. 2013;8:e74517. doi: 10.1371/journal.pone.0074517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pang Y, An J, Shu W, Huo F, Chu N, Gao M, et al. Epidemiology of Extrapulmonary Tuberculosis among Inpatients, China, 2008-2017. Emerg Infect Dis. 2019;25:457–464. doi: 10.3201/eid2503.180572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang X, Yang Z, Fu Y, Zhang G, Wang X, Zhang Y, et al. Insight to the Epidemiology and Risk Factors of Extrapulmonary Tuberculosis in Tianjin, China during 2006-2011. PloS One. 2014;9:e112213. doi: 10.1371/journal.pone.0112213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Hazmi MM, Al-Otaibi FE. Predictors of pulmonary involvement in patients with extra-pulmonary tuberculosis. J Family Community Med. 2012;19:88–92. doi: 10.4103/2230-8229.98287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Golden MP, Vikram HR. Extrapulmonary tuberculosis: an overview. Am Fam Physician. 2005;72:1761–1768. [PubMed] [Google Scholar]
- 15.Kulchavenya E. Extrapulmonary tuberculosis: are statistical reports accurate? Ther Adv Infect Dis. 2014;2:61–70. doi: 10.1177/2049936114528173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sunnetcioglu A, Sunnetcioglu M, Binici I, Baran AI, Karahocagil MK, Saydan MR. Comparative analysis of pulmonary and extrapulmonary tuberculosis of 411 cases. Ann Clin Microbiol Antimicrob. 2015;14:34. doi: 10.1186/s12941-015-0092-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Hajoj S, Shoukri M, Memish Z, AlHakeem R, AlRabiah F, Varghese B. Exploring the sociodemographic and clinical features of extrapulmonary tuberculosis in Saudi Arabia. PloS One. 2015;10:e0101667. doi: 10.1371/journal.pone.0101667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruiz G, García Rodríguez J, Güerri ML, González A. Osteoarticular tuberculosis in a general hospital during the last decade. Clin Microbiol Infect. 2003;9:919–923. doi: 10.1046/j.1469-0691.2003.00671.x. [DOI] [PubMed] [Google Scholar]
- 19.Houshian S, Poulsen S, Riegels-Nielsen P. Bone and joint tuberculosis in Denmark: increase due to immigration. Acta Orthop Scand. 2000;71:312–315. doi: 10.1080/000164700317411942. [DOI] [PubMed] [Google Scholar]
- 20.Chen ST, Zhao LP, Dong WJ, Gu YT, Li YX, Dong LL, et al. The Clinical Features and Bacteriological Characterizations of Bone and Joint Tuberculosis in China. Sci Rep. 2015;5:11084. doi: 10.1038/srep11084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ohene SA, Bakker MI, Ojo J, Toonstra A, Awudi D, Klatser P. Extra-pulmonary tuberculosis: A retrospective study of patients in Accra, Ghana. PloS One. 2019;14:e0209650. doi: 10.1371/journal.pone.0209650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leeds IL, Magee MJ, Kurbatova EV, del Rio C, Blumberg HM, Leonard MK, et al. Site of extrapulmonary tuberculosis is associated with HIV infection. Clin Infect Dis. 2012;55:75–81. doi: 10.1093/cid/cis303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Procopie I, Popescu EL, Pleșea RM, Dorobanțu M, Mureșan RF, Lupașcu-Ursulescu CV, et al. Clinical-Morphological Aspects in Spinal Tuberculosis. Curr Health Sci J. 2018;44:250–260. doi: 10.12865/CHSJ.44.03.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park SH, Yang SK, Yang DH, Kim KJ, Yoon SM, Choe JW, et al. Prospective randomized trial of six-month versus nine-month therapy for intestinal tuberculosis. Antimicrob Agents Chemother. 2009;53:4167–4171. doi: 10.1128/AAC.00874-09. [DOI] [PMC free article] [PubMed] [Google Scholar]




