Abstract
Background
Pandemic planning has historically been oriented to respond to an influenza virus, with vaccination strategy being a key focus. As the current COVID-19 pandemic plays out, the Australian government is closely monitoring progress towards development of SARS-CoV2 vaccines as a definitive intervention. However, as in any pandemic, initial supply will likely be exceeded by demand due to limited manufacturing output.
Methods
We convened community juries in three Australian locations in 2019 to assess public acceptability and perceived legitimacy of influenza pandemic vaccination distribution strategies. Preparatory work included literature reviews on pandemic vaccine allocation strategies and on vaccine allocation ethics, and simulation modelling studies. We assumed vaccine would be provided to predefined priority groups. Jurors were then asked to recommend one of two strategies for distributing remaining early doses of vaccine: directly vaccinate people at higher risk of adverse outcomes from influenza; or indirectly protect the general population by vaccinating primary school students, who are most likely to spread infection.
Results
Thirty-four participants of diverse backgrounds and ages were recruited through random digit dialling and topic-blinded social media advertising. Juries heard evidence and arguments supporting different vaccine distribution strategies, and questioned expert presenters. All three community juries supported prioritising school children for influenza vaccination (aiming for indirect protection), one by 10–2 majority and two by consensus. Justifications included that indirect protection benefits more people and is likely to be more publicly acceptable.
Conclusions
In the context of an influenza pandemic, informed citizens were not opposed to prioritising groups at higher risks of adverse outcomes, but if resources and epidemiological conditions allow, achieving population benefits should be a strategic priority. These insights may inform future SARS-CoV-2 vaccination strategies.
Keywords: Pandemic Influenza vaccination, Health policy, Public deliberation, Public health ethics
1. Introduction
The challenges of managing pandemic have become newly pertinent in 2020, as countries around the world struggle to manage SARS-CoV-2 infection in their populations [1]. Healthcare capacity has been overwhelmed, even in high-income contexts, and shortages of critical health care resources have resulted in rationing in many jurisdictions [2]. Intensive mitigation and suppression measures have led to a significant reduction in new cases in several countries. However, the economic impact of such measures has been severe with those in lower socio-economic positions worse affected [3]. In the absence of effective treatment for COVID-19, populations will remain at risk requiring governments to balance the need to ease social and economic restrictions against the potential for surging case numbers [4]. The development of a safe and effective vaccine, typically an essential part of pandemic response plans, is now a shared global strategy for the longer-term control of COVID-19 [5], [6], [7].
More than a hundred vaccine candidates are in development as of late November 2020, with eleven already in phase III trials [8]. As new vaccines are licensed and become available, demand is expected to far outstrip supply in the early stages. One of the few precedents for vaccine distribution strategy in such a context is pandemic influenza planning; thus, governments are already looking to existing pandemic influenza management plans for guidance on strategies to distribute scarce vaccine [7], [9].
The WHO’s Pandemic Influenza Risk Management guidance advises member states to establish which groups should be prioritised for initial vaccination, guided by ethical considerations and informed by local risk assessment [10]. The current Australian Health Management Plan for Pandemic Influenza (AHMPPI) prioritises direct protection for groups who are considered likely to be at higher risk of severe illness, based on risk groups targeted by the seasonal influenza vaccination program [11]. Drawing on their plans for pandemic influenza, the World Health Organization (WHO) has published guidelines for managing scarce resources in COVID-19 prevention and care, recommending a framework for priority setting that considers context and extent of scarcity. It suggests equality of access, maximising best outcomes, prioritising those at greatest risk of becoming seriously ill, and prioritising essential workers, depending on scenario [7], [12].
Our paper is one of two in a series that aims to provide a framework for the prioritisation of vaccine allocation. In the companion paper, a cross-disciplinary research team was commissioned by the Australian Government Department of Health to undertake modelling and perform an ethical analysis to develop a flexible framework to guide the distribution of limited influenza vaccine supplies in the early phases of a pandemic response [13]. This framework recommends promotion of three overall objectives in health protection decision-making: (i) creating and maintaining trust; (ii) promoting equity; and (iii) focusing on outcomes. The first objective supports effective pandemic and post-pandemic healthcare management. The second attempts to redress pre-existing disadvantage so that disparities in pandemic burden are not socially patterned. The final objective focuses on reducing the negative impacts of the pandemic while it is occurring and into the future. Outcomes include both harms (broadly, things that threaten people’s essential interests) and benefits (things that impact positively on well-being of individuals and groups). The framework aims to achieve these objectives by establishing two priority levels for vaccine allocation. The first priority (Level 1) comprises two groups: frontline healthcare workers (HCW) and First Nations Australians. Vaccinating HCW who are likely to be in contact with COVID-19 patients reduces risk of infection and spread and ensures that the provision of care is not compromised by HCW who are ill or reluctant to attend work. Protected HCW maximises beneficial health outcomes for patients and promotes trust in healthcare settings. First Nations Australians are known to be at the highest risk of adverse outcomes in pandemics and experience considerable structural disadvantage [14]; prioritising this group promotes equity. Level 1 groups are prioritized irrespective of other evidentiary factors. Less clear, however, is which groups should receive ‘Level 2’ vaccine access (that is, which groups should be next). Following distribution to Level 1 groups, Level 2 priority groups need to be defined consistent with the three overall objectives.
Based on outcomes of the modeling on influenza pandemics described in the companion paper (see also supplementary materials), our framework proposed two strategies that could be used to distribute influenza vaccines among Level 2 groups and the remaining population [13]:
-
•
the ‘high-risk’ strategy – which aims to provide direct protection to individuals at higher risk of severe illness; and
-
•
the ‘school-based’ strategy – which aims to provide indirect protection to the population through vaccinating primary school children, who, in the case of influenza, are most likely to develop and spread infection.
In Australia the annual vaccination program for seasonal influenza prioritises direct protection for high risk groups [15]. This strategy is adopted by many other high-income countries, with the notable exception of the UK. Seasonal influenza vaccination has been offered to British children, in a phased roll-out since 2013, for the dual purpose of protecting the children themselves and reducing transmission across all age groups to protect those at risk of severe outcomes [16]. While school-based programs for delivery of some vaccines to teenagers have been in place in most Australian states and territories since the 1970s (e.g. rubella, and more recently hepatitis B followed by HPV), adoption of a ‘primary school’ strategy for seasonal or pandemic influenza vaccines would be a significant strategic shift in Australian immunisation policy. The primary school strategy serves as a useful proxy for evaluating the acceptability of indirect vaccination strategies in general. It is important to note, however, that the suitability of vaccination strategies is always dependent on underlying disease epidemiology. In the context of COVID-19, for example, epidemiology so far suggests that children are not significantly affected, or driving disease transmission [17], and so school-based vaccination should not be prioritised [2], [9], [12].
The disease model described in the companion paper was also designed to inform decisions about whether to base the pandemic vaccination program on a 1- or 2-dose strategy [13]. Decisions about dosing strategies depend on early clinical studies of a pandemic vaccine to show whether it produces antibody levels considered sufficient for protection. In past pandemics, a single dose has sometimes been sufficient for older individuals. But if two doses are needed for full protection, a vaccine program may a) use limited vaccine supplies to fully protect fewer people; or b) provide partial protection to more people with just one dose. These alternative pandemic vaccine distribution strategies require different approaches to implementation, have different goals and allocate the benefits and burdens of vaccination differently (Supplementary Textbox 1).
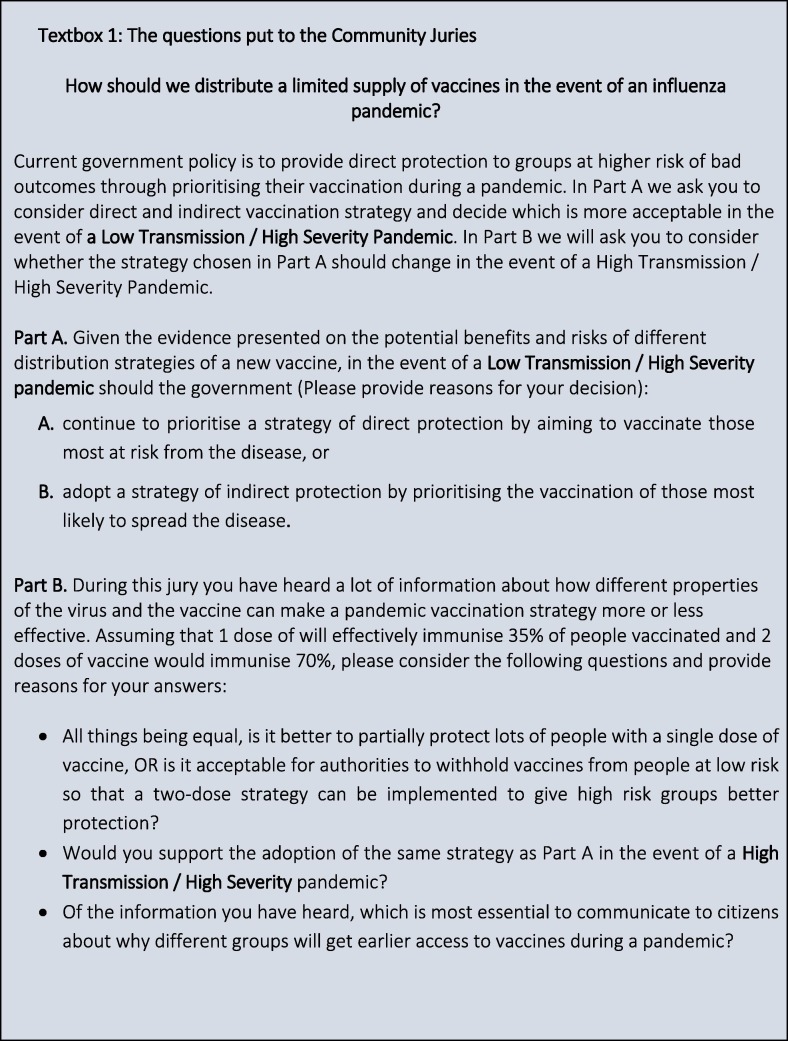
The WHO guidance document on pandemic preparedness emphasises the important role of the public in effective planning and response to an influenza pandemic [18]. Consistent with this, we conducted community juries in different parts of Australia to provide recommendations on how best to use limited vaccine resources in the event of an influenza pandemic, in collaboration with the Australian Government Department of Health Office of Health Protection. The modelling studies indicated that positive impacts from vaccine distribution strategy were only possible in the event of a pandemic with low virus transmissibility but high severity of illness among those infected (Supplementary Figs. 1 & 2). Although SARS-CoV2 is a highly transmissible virus in many contexts, including Australia, widespread suppression measures have reduced transmission significantly. Thus although the influenza virus has different characteristics to SARS-CoV2, the current policy context is to some extent comparable. Based on the preliminary work described above, the question put to the juries and supporting evidence focused on a low transmission, high severity scenario (Fig. 1 Textbox 1), the aim being to gather evidence about the acceptability and perceived legitimacy of two specific strategies for prioritising pandemic vaccine distribution in this situation, and reasons for acceptance or non-acceptance of these strategies.
Fig. 1.
Textbox 1 - The questions put to the Community Juries.
2. Methods and materials
A citizens’ or community jury meets for two to five days to carefully examine an issue of public significance [19]. Usually 10–15 members of the public serve on a jury, acting as a ‘mini-public’ or microcosm of the broader public [19], [20]. While a small group cannot statistically represent ‘the general public’, participants are recruited to capture a diversity of experiences and backgrounds in a community [21], and so can suggest what an inclusive and informed public would advise, given factual information and time to deliberate [20], [22], [23]. Community juries have been used in Australia and elsewhere to consider issues surrounding infectious disease control and prevention [24], [25], including the appropriateness of different measures that can be used in response to a pandemic [26], [27], [28], [29].
Formal deliberation is more than a dialogue and not just a debate. The deliberative process is designed to extend the thinking of participants beyond their own interests to think about whole-of-population good and the collective needs of the community. To be considered robust and reliable deliberative processes must (at a minimum):
-
(i)
provide participants with balanced factual information;
-
(ii)
ensure that a sufficiently diverse range of potentially conflicting, minority and marginal perspectives are considered; and
-
(iii)
create opportunities for free and open discussion and debate within and between citizens, experts and/or policy actors, to challenge and test competing claims.
The method assumes that people can think rationally and change their views should the evidence warrant it [30]. Community juries are usually directed to consider a specific issue – typically formulated as a ‘charge’ (as in a court hearing). They hear from a variety of expert witnesses, question those witnesses, and deliberate together on the issue. The process is like a legal proceeding, but the outputs are not legally binding and consensus is encouraged but not required. When conducted in this way, community juries can provide perspectives that can inform policy recommendations and evidence of public values, concerns and arguments. Juries thus reflect the likely acceptability and public legitimacy of different policy alternatives, and provide an indication of what an informed public thinks should be done to address a specific issue [19], [20], [31].
There is a longstanding debate about the relationship between empirical and theoretical work in bioethics, which is beyond the scope of this paper [32]. This project is an example of empirical bioethics, which assumes that the moral judgements of members of the public have an important place in final determinations of the right thing to do [33]. What role public judgements should have in final determinations differs between research traditions. In particular, deliberative research methods are different from perhaps more familiar social science methods. They “arise from political theory, enact an ideal form of democracy, and are intended to have direct and indirect consequences in governance” [34]. Jurors engage with normative questions when they consider evidence. They make value-based decisions about what matters and provide researchers with insight about public moral intuitions and judgements and how they are enacted. Researchers can combine a highly contextual understanding of a particular scenario with ethical deliberation to draw normative conclusions. As a result, projects such as this can report descriptive outcomes – what did juries decide? – and normative recommendations – what do well-informed, inclusive groups of people say we should do, and for what reasons?
2.1. Study settings
We convened three community juries: Jury 1 in Wollongong (NSW), Jury 2 in Melbourne (Victoria) and Jury 3 in Kalgoorlie (Western Australia) – representing regional, metropolitan, and rural populations, respectively. All were held over two days (Saturday-Sunday) in April and May 2019.
2.2. Juror recruitment
An independent research service was contracted to recruit jury participants, using randomly generated list-based samples of mobile and fixed-line telephone numbers, located in specific geographic areas, and a social media advertising strategy targeting those same areas. To reduce selection bias the social media advertisement was blinded as to the research topic area. The jurors were then selected purposively from the resulting pool of potential participants, to promote an approximate 50:50 gender split, and ensure a range of ages and socioeconomic and cultural diversity within each jury [22], [35]. Jurors were compensated $200 AUD for each day of their time.
2.3. Jury procedures
Each jury commenced with an orientation session to introduce the process, the questions for consideration and to seek consent. Day 1 focused on understanding: basic influenza virus biology (seasonal and pandemic strains); the individual and population impacts of influenza infection (during seasonal outbreaks and pandemics); different interventions to manage infection risks; influenza vaccinology including manufacturing pipeline and licensing; different pandemic vaccine distribution strategies; and different ethical perspectives on prioritising pandemic vaccine (Supplementary Table 1). Logistic considerations related to vaccine production and distribution were highlighted, as well as common challenges to vaccination program implementation.
Testimony from four experts was pre-recorded and shown to jurors as video presentations – and are available online [36]. Experts were selected on the basis of their institutional roles, experience and expertise to provide balanced, factual information supporting different expert perspectives on the potential impacts, benefits and costs of direct or indirect vaccine protection strategies. Each presentation ran for approximately 25–30 min. Pre-recording ensured the format of the evidence presented was standardised across juries. After each video presentation the expert was available by teleconference call or in person, for jurors to ask questions. These question and answer sessions, facilitated by a researcher, allowed jurors to clarify or question the evidence and opinions presented. Facilitation focused on promoting constructive dialogue and fair interaction amongst jurors. For the first hour of Day 2, jurors reflected on, discussed and debated the evidence, aided by a facilitator. Juries then deliberated for an hour, without facilitation, to reach a verdict on the questions posed. The verdicts, underpinning reasoning, and dissenting views were then reported to the research team in a final facilitated feedback session. Our research and reporting processes for these Community Juries were cross-checked against the CJChecklist protocol [37].
2.4. Data collection and analysis
The three deliberative groups (juries) are the units of analysis in this study. All jury deliberations (facilitated and un-facilitated) and expert question and answer sessions were audio-recorded and transcribed. To track changes in the positions held by individual jurors, participants completed an anonymous ballot at 4 time-points during jury proceedings: (i) before any evidence had been presented at the beginning of Day 1; (ii) after having considered the evidence at the end of Day 1; (iii) after reflecting on it at home overnight at the beginning of Day 2; and (iv) after the deliberation and delivery of the verdict at the end of Day 2. Jurors also completed a process evaluation exit survey at the conclusion of each event. During the final session a researcher/facilitator recorded the verdict and reasons on a flipchart. Each point was reviewed by the jury to ensure accuracy. In what follows the characteristics of each jury are described; a summary of jurors’ own descriptions of the rationale and reasoning that underpinned their responses to the questions is then provided.
3. Results
3.1. Participant characteristics
34 people were recruited across the three study settings (Table 1 ). All juries included participants of both genders and a range of ages, but those in Melbourne and Kalgoorlie had more male than female participants. Compared with the national average educational attainment, jurors in Wollongong were skewed towards either higher or lower levels and those in Melbourne towards a slightly higher level. Participants in each jury resided in postcodes representing a range of ‘socioeconomic indices for areas’ (SEIFA) scores (a measure of average socioeconomic status of local areas) largely consistent with those of each study setting.
Table 1.
Characteristics of Jury Participants.
| Jury 1 (n = 12) | Jury 2 (n = 12) | Jury 3 (n = 10) | |
|---|---|---|---|
| Age (years) | |||
| 18–34 | 3 | 4 | 2 |
| 35–54 | 5 | 4 | 6 |
| >55 | 4 | 4 | 2 |
| Gender | |||
| Male | 6 | 7 | 3 |
| Female | 6 | 5 | 7 |
| Highest Educational Attainment | |||
| High School | 4 | 3 | 3 |
| Trade / Diploma | 4 | 2 | 3 |
| Bachelor Degree | 1 | 5 | 2 |
| Postgraduate Degree | 3 | 2 | 2 |
| Socio-Economic status of suburb* | |||
| Low | 2 | 1 | 0 |
| Middle | 10 | 4 | 5 |
| High | 0 | 7 | 5 |
Based on Socio-economic Index for Area (SEIFA).
3.1.1. Community jury verdicts
PART A: At the end of jury proceedings all three Community juries voted to support a vaccine distribution strategy aimed at achieving indirect protection – Melbourne with an 10–2 majority and Wollongong and Kalgoorlie by consensus verdicts. The results of the time-point ballots represented in Table 2 demonstrate that the balance of the vote changed throughout each event, with support, after jurors had deliberated, swinging definitively behind strategies aimed at providing indirect protection.
Table 2.
Part A - Votes at different time-points during jury proceedings.
| CJ #1 (Wollongong) |
CJ #2 (Melbourne) |
CJ #2 (Kalgoorlie) |
||||
|---|---|---|---|---|---|---|
| Direct strategy | Indirect strategy | Direct strategy | Indirect strategy | Direct strategy | Indirect strategy | |
| #1 Saturday AM Before evidence delivered | 8 | 4 | 8 | 4 | 6 | 4 |
| #2 Saturday PM After evidence delivered | 6 | 6 | 5 | 7 | 2 | 8 |
| #3 Sunday AM After reflection overnight | 8 | 4 | 5 | 7 | 1 | 9 |
| #4 Sunday PM After deliberation | 0 | 12 | 2 | 10 | 0 | 10 |
3.2. Jurors’ reasons for their responses to PART A
Jurors supported the goal of indirect protection during a low transmissibility/high severity pandemic. The key reasons given were fairly consistent, although there was some underlying differences in the values underpinning the positions in the three locations. Based on the evidence presented, jurors preferred the ‘school-based’ strategy over prioritising high-risk groups because it was most effective for everyone: more people would benefit from the available resources, not just those vaccinated. This was not a decision to deny protection for those in high risk groups, but about prioritisation. People at higher risk would be protected indirectly and, eventually, have the opportunity to be vaccinated and protected directly.
Jurors argued that a strategy focused on protecting children would be more acceptable to the general public, and gave two central reasons for supporting the school-based strategy: maximising the utility of vaccine resources, and the moral significance of protecting children. The Wollongong group emphasised that “kids are important” and should be protected early; therefore indirect protection was construed as an “extra benefit”. The Melbourne group was more concerned with maximising the potential utility of vaccine resources and thereby building community trust and maintaining social cohesion. The overarching goal of the Kalgoorlie jury was to exploit the potential utility of vaccine resources for population benefit and to maximise the number of people protected. The logistical efficiency of schools-based vaccination was also more appealing to jurors than relying on members of vulnerable groups to access primary care for vaccination. All juries emphasized that compassion for those at greater risk of severe illness was important, and two of the 12 Melbourne jurors voted to prioritise high risk groups in the early stages of a pandemic, out of concern for those at greatest risk of a severe illness. However, on balance, all three juries voted to use vaccine resources to maximise population health outcomes.
PART B: At the end of proceedings, juries in Wollongong and Kalgoorlie voted in support of commencing the program with a 2-dose vaccine distribution strategy, whereas the Melbourne jury supported a 1-dose strategy. Table 3 shows that the juries were relatively evenly split on this question at the first ballot (before any evidence had been presented). The balance of the vote, at each poll, changed throughout proceedings, with 3–4 votes swinging definitively behind the preferred strategy, after each jury’s final deliberations.
Table 3.
Part B - Votes at different time-points during jury proceedings.
| CJ #1 (Wollongong) |
CJ #2 (Melbourne) |
CJ #2 (Kalgoorlie) |
||||
|---|---|---|---|---|---|---|
| 1-dose strategy | 2-dose strategy | 1-dose strategy | 2-dose strategy | 1-dose strategy | 2-dose strategy | |
| #1 Saturday AM Before evidence delivered | 6* | 5* | 7 | 5 | 5 | 5 |
| #2 Saturday PM After evidence delivered | 5 | 7 | 6 | 6 | 2 | 8 |
| #3 Sunday AM After reflection overnight | 3 | 9 | 5 | 7 | 5 | 5 |
| #4 Sunday PM After deliberation | 0 | 12 | 11 | 1 | 1 | 9 |
1 participant did not know whether they supported a 1- or 2-dose strategies at the first vote.
3.3. Pro-1-dose strategies
The Melbourne jury supported adoption of a 1-dose strategy during the early phases of vaccine roll-out. They concluded that giving more people some protection sooner was fairer, would make more people feel safer, promote trust in authorities and, ultimately, help to maintain social order and cohesion. They argued that some people would not present for a second dose, risking loss of an opportunity to protect more people sooner, and wastage of time and resources, especially if one dose was found to be sufficient.
3.4. Pro-2-dose strategies
In Wollongong and Kalgoorlie juries supported a 2-dose strategy during the early phases of vaccine roll-out, because starting with a 1-dose strategy without evidence of its effectiveness would risk wasting vaccine doses and may make the indirect strategy ineffective, and a 2-dose strategy would be more likely to promote public trust in vaccine effectiveness because fewer vaccinated people may become infected. Juries strongly argued that authorities should be transparent about uncertainty regarding dosage. While acknowledging that a 1-dose strategy might be seen as rapidly helping more people, these juries argued for maximising effectiveness until the efficacy of a single vaccine dose was known.
3.5. Advice on public communication
When asked what citizens should be told about why different groups will get earlier access to vaccines during a pandemic, jurors at all three sites told us that the population health value of the indirect approach - i.e. that it protects more people, including those at higher risk of severe illness - and why vaccine would be limited, initially, would need to be explained.
3.6. Responding to changes in the nature of the pandemic
Juries were also asked about strategies to manage a high transmission/high severity pandemic: a scenario that would more closely approximate an unmitigated SARS-CoV-2 outbreak. The Wollongong and Melbourne juries voted to retain an indirect protection strategy because: a) children are important and worthy of prioritization (given greater emphasis in Wollongong); b) a simple school-based (rather than risk-group based) strategy would be easier to defend, publicly (important for both Wollongong and Melbourne); and c) it was more likely to maintain trust and social stability (given greater emphasis in Melbourne). In contrast the Kalgoorlie jury drew on evidence they had heard that, in a high /high severity pandemic, an indirect protection strategy was unlikely to provide a transmissibility population benefit, and argued for directly protecting those most at risk of severe illness. Notably, the reasons given by each group for these different positions align quite closely with their key reasons for supporting an indirect protection strategy, namely: protecting children (Wollongong); maintaining social cohesion (Melbourne); and, maximising the potential utility of vaccine resources (Kalgoorlie).
4. Discussion
Most pandemic plans around the world do not substantively attend to ethical considerations in prioritising scarce pandemic vaccine. Those that do emphasise the need for procedural justice, usually explicated as a set of principles embedded in response decision-making and communication [13], [38]. Ethical justifications for prioritising particular groups tend to be utilitarian, maximising ‘good’ by minimising illness and death in those most at risk. The recommended framework in our companion paper for Australian priority vaccine allocation has three overarching objectives: (i) creating and maintaining trust; (ii) promoting equity; and, (iii) focusing on outcomes. These aims were communicated to each community jury in expert testimony, and ideas relevant to the priority that should be afforded to each of these aims also arose during jurors’ deliberations.
All juries affirmed that ensuring public trust was vitally important. Their decisions explicitly prioritised the need to create and maintain public trust in two key areas: public perceptions about effectiveness of pandemic vaccination; and, more broadly, how health authorities communicate with the public before and during a pandemic. Of relevance to the second and third objectives, all groups juxtaposed ideas of equity and best outcomes, saying that, while both were important, maximising population effectiveness was more critical in their decision making. All three juries supported providing indirect protection of the population, by vaccination of primary school children. They were not opposed, in principle, to prioritising groups at higher risks of adverse outcomes, but chose the indirect strategy based on evidence they had seen that it would be more effective and efficient. Given the apparently limited role of children in transmitting SARS-CoV2, alternative groups would need to be identified and vaccinated in an indirect protection strategy, based on best evidence of effectiveness and implementability. The current study supports the findings of previous deliberative research in Australia [26], [27], which indicates that while informed publics generally support prioritisation of high-risk groups on equity grounds, as in the current AHMPPI [11], given the opportunity to consider the trade-offs entailed, they prefer that vaccine resources be used, optimally, to maximise utility and benefit the broader population while also working to sustain social order.
Including members of the public in deliberation forums can provide local sources of evidence for those planning and implementing pandemic policy and anticipate local issues which may support or impede successful implementation. Decision-making during a pandemic must take into account both evidence-based models and likely community acceptability of the chosen policy [39], [40]. Unless they ask, decision-makers can only speculate on what the public's values are, and are likely to be unaware of the extent to which the perspectives of different groups in society might be aligned; for example, the potential for the school-based strategy to provide indirect population protection and a previously identified strong preference (measured by a population survey), among many people, to give highest priority to protecting children during a pandemic [41]. In the case of COVID-19, indirect immunisation strategies are unlikely to be targeted at children, potentially leading juries to reach different conclusions about such strategies. As our results show, a shared consensus in public deliberations is not necessary to enhance the basis for decision-making; the reasons jurors provided for their support of either 1- or 2-dose vaccination strategies were coherent, well-reasoned, and depended on how each group responded to the probability of vaccine efficacy (1 dose 35% / 2 dose 70%), which highlights how difficult the choice will be without knowledge of the efficacy of a single dose. Public deliberations should include diverse perspectives to understand what is at stake for different groups and develop possible pathways for action [22], [23]. Publicity, transparency and deliberation can promote greater social and political engagement, public accountability and confidence in difficult policy decisions.
4.1. Study strengths and limitations
Community juries are a deliberative method that involve a process of iterative two-way exchange of information between members of the public and experts. By providing extensive information from a range of experts, and ensuring conditions for reasonable and extended debate, independent community juries elicit more considered judgements than other social research methods such as surveys or focus groups. The sample size is small, but this is necessary for high-quality deliberation. Participants were asked to select between a pre-determined range of strategies. It is possible that there are other strategies participants would prefer. However, our design prioritised the direct policy relevance of the questions put to the jurors: that is, we put to the jurors the questions policymakers were asking, and wanted answers to. It is possible that other policy options would be more relevant for deliberation in other jurisdictions. A further limitation is that we did not collect data from participants regarding whether they were parents of school aged children such that we are unable to analyse any potential effect of this variable on jurors’ reasoning.
5. Conclusions
Defining clear and justifiable objectives for pandemic response in context aids development of flexible and adaptive decision support frameworks and facilitates clear communication and engagement activities. Previous deliberative research in Australia found public support for using limited pandemic vaccine resources to protect healthcare workers and maintain social services – largely driven by a desire to maintain societal functioning. The current study indicates the Australian public may also prefer distribution strategies aimed at maximising the utility of vaccines so as to provide population benefits through indirect protection, if time and resources allow. These findings have direct relevance for COVID-19, despite being undertaken for an influenza pandemic model, in that the initial supply of SARS-CoV-2 vaccines will be well short of demand and necessitate rationing. A key difference is the high susceptibility to infection in countries that achieved effective COVID-19 suppression, which will require vaccine prioritisation over a longer time period because more people may need to be vaccinated to achieve community protection. All groups agreed that transparency in communication and trust in authorities is paramount – a value given highest priority by our jury groups. Responsiveness to emerging evidence is also key, particularly in further identifying higher risk groups such as the elderly and those with co-morbidities [2], [12], [17], and in determining optimal vaccination schedules. Once available, governments should communicate their vaccine allocation plans effectively and transparently, both to other levels of government and the public.
6. Role of the funding source
This project was directly funded by the Australian Government Department of Health Office of Health Protection Approach to Market: Health/17–18/73536 Investigate and Model Initial Pandemic Influenza Vaccination Target Groups – extension to conduct Citizens’ Juries.
The Australian Partnership for Preparedness Research on Infectious Disease Emergencies is a Centre of Research Excellence funded by the Australian Government National Health and Medical Research Council (NHMRC) GNT1116530.
The Centre for Research Excellence in Emerging Infectious Disease (CREID) is funded by the Australian Government National Health and Medical Research Council (NHMRC) GNT1102962.
Jodie McVernon is supported by a NHMRC Principal Research Fellowship GNT1117140.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2020.12.010.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.World Health Organization. Coronavirus disease 2019 (COVID-19): situation report, 59. Geneva: WHO; 2020. p. https://apps.who.int/iris/bitstream/handle/10665/331597/nCoVsitrep19Mar2020-eng.pdf.
- 2.Emanuel E.J., Persad G., Upshur R., Thome B., Parker M., Glickman A. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 3.The Lancet. Redefining vulnerability in the era of COVID-19. Lancet (London, England). 2020;395:1089. [DOI] [PMC free article] [PubMed]
- 4.Ferguson NM LD, Nedjati-Gilani G, Imai N, Ainslie K, Baguelin M. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. 2020;DOI. 2020;10:77482. [DOI] [PMC free article] [PubMed]
- 5.Zhang S., Wang Y., Rauch A., Wei F. Unprecedented disruptions of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. medRxiv. 2020 doi: 10.1016/j.psychres.2020.112958. 2020.03.13.20034496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fernandes N. Economic Effects of Coronavirus Outbreak (COVID-19) on the World Economy. SSRN2020.
- 7.Yamey G., Schäferhoff M., Hatchett R., Pate M., Zhao F., McDade K.K. Ensuring global access to COVID-19 vaccines. The Lancet. 2020;395:1405–1406. doi: 10.1016/S0140-6736(20)30763-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Draft landscape of COVID-19 candidate vaccines. Geneva: WHO; 2020. p. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines.
- 9.Centres for Disease Control and Prevention (CDC). COVID-19 Vaccination Program Interim Playbook for Jurisdiction Operations. Version 20: U.S. Department of Health and Human Services; 2020. p. https://www.cdc.gov/vaccines/imz-managers/downloads/COVID-19-Vaccination-Program-Interim_Playbook.pdf.
- 10.Black A.J., Geard N., McCaw J.M., McVernon J., Ross J.V. Characterising pandemic severity and transmissibility from data collected during first few hundred studies. Epidemics. 2017;19:61–73. doi: 10.1016/j.epidem.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Australian Government Department of Health. Australian Health Management Plan for Pandemic Influenza. Canberra, Australia: Commonwealth Government of Australia; 2014.
- 12.Organization WH. Ethics and COVID-19: resource allocation and priority-setting. Geneva: WHO; 2020.
- 13.Fielding J, Sullivan S, Beard F, Macartney K, Williams J, Dawson A, et al. Constructing an ethical framework for priority allocation of pandemic influenza vaccines. Vaccine. 2020;under review. [DOI] [PMC free article] [PubMed]
- 14.Flint S.M., Davis J.S., Su J.Y., Oliver-Landry E.P., Rogers B.A., Goldstein A. Disproportionate impact of pandemic (H1N1) 2009 influenza on Indigenous people in the Top End of Australia's Northern Territory. Med J Aust. 2010;192:617–622. doi: 10.5694/j.1326-5377.2010.tb03654.x. [DOI] [PubMed] [Google Scholar]
- 15.National Immunisation Program. Statement on the Administration of Seasonal Influenza Vaccines in 2019 Australian Government Department of Health, Canberra Australian Technical Advisory Group on Immunisation (ATAGI); 2019. p. https://www.health.gov.au/resources/publications/atagi-advice-on-seasonal-influenza-vaccines-in-2019.
- 16.Pebody RG, Sinnathamby MA, Warburton F, Andrews N, Boddington NL, Zhao H, et al. Uptake and impact of vaccinating primary school-age children against influenza: experiences of a live attenuated influenza vaccine programme, England, 2015/16. Euro Surveill. 2018;23:pii=1700496. [DOI] [PMC free article] [PubMed]
- 17.Zhang J., Litvinova M., Liang Y., Wang Y., Wang W., Zhao S. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 2020 doi: 10.1126/science.abb8001. eabb8001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Pandemic influenza preparedness and response: a WHO guidance document: Geneva: World Health Organization; 2009. [PubMed]
- 19.Degeling C., Carter S., Rychetnik L. Which public and why deliberate? – A scoping review of public deliberation in public health and health policy research. Soc Sci Med. 2015;131:114–121. doi: 10.1016/j.socscimed.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 20.Street J., Duszynski K., Krawczyk S., Braunack-Mayer A. The use of citizens' juries in health policy decision-making: a systematic review. Soc Sci Med. 2014;109:1–9. doi: 10.1016/j.socscimed.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 21.Karpowitz C.F., Raphael C. Ideals of inclusion in deliberation. J Public Deliberation. 2016;12:1–24. [Google Scholar]
- 22.Burgess M.M. From ‘trust us’ to participatory governance: deliberative publics and science policy. Public Understand Sci. 2014;23:48–52. doi: 10.1177/0963662512472160. [DOI] [PubMed] [Google Scholar]
- 23.Degeling C., Rychetnik L., Street J., Thomas R., Carter S.M. Influencing health policy through public deliberation: lessons learned from two decades of Citizens'/community juries. Soc Sci Med. 2017;179:166–171. doi: 10.1016/j.socscimed.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 24.Degeling C., Gilbert G.L., Annand E., Taylor M., Walsh M.G., Ward M.P. Managing the risk of Hendra virus spillover in Australia using ecological approaches: a report on three community juries. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0209798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Degeling C., Johnson J., Iredell J., Nguyen K.-A., Norris J.M., Turnidge J.D. Assessing the public acceptability of proposed policy interventions to reduce the misuse of antibiotics in Australia: a report on two community juries. Health Expect. 2018;21:90–99. doi: 10.1111/hex.12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Braunack-Mayer A.J., Street J.M., Rogers W.A., Givney R., Moss J.R., Hiller J.E. Including the public in pandemic planning: a deliberative approach. BMC Public Health. 2010;10:501. doi: 10.1186/1471-2458-10-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Docter S.P., Street J., Braunack-Mayer A.J., van der Wilt G.-J. Public perceptions of pandemic influenza resource allocation: a deliberative forum using Grid/Group analysis. J Public Health Policy. 2011;32:350–366. doi: 10.1057/jphp.2010.49. [DOI] [PubMed] [Google Scholar]
- 28.Baum N.M., Jacobson P.D., Goold S.D. “Listen to the people”: public deliberation about social distancing measures in a pandemic. Am J Bioethics: AJOB. 2009;9:4–14. doi: 10.1080/15265160903197531. [DOI] [PubMed] [Google Scholar]
- 29.Rogers W.A., Street J.M., Braunack-Mayer A.J., Hitter J.E., FluViews T. Pandemic influenza communication: views from a deliberative forum. Health Expect. 2009;12:331–342. doi: 10.1111/j.1369-7625.2009.00562.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blacksher E., Diebel A., Forest P.-G., Goold S.D., Abelson J. What is public deliberation. Hastings Cent Rep. 2012;42:14–17. doi: 10.1002/hast.26. [DOI] [PubMed] [Google Scholar]
- 31.Karpowitz C.F., Deliberation R.C. Cambridge University Press; 2014. democracy, and civic forums: Improving equality and publicity. [Google Scholar]
- 32.Ives J., Dunn M., Molewijk B., Schildmann J., Bærøe K., Frith L. Standards of practice in empirical bioethics research: towards a consensus. BMC Med Ethics. 2018;19:68. doi: 10.1186/s12910-018-0304-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Feminist S.J., Bioethics E. Empirical bioethics: theoretical and practical perspectives. Cambridge University Press - Cambridge Bioethics and Law; Cambridge: 2016. pp. 195–221. [Google Scholar]
- 34.Carter S.M. Methodological challenges in deliberative empirical ethics. J Med Ethics. 2020;46:382–383. doi: 10.1136/medethics-2020-106185. [DOI] [PubMed] [Google Scholar]
- 35.Irwin A., Jensen T.E., Jones K.E. The good, the bad and the perfect: Criticizing engagement practice. Soc Stud Sci. 2013;43:118–135. [Google Scholar]
- 36.Australian Partnership for Preparedness Research on Infectious Disease Emergencies. Community perspectives on distributing an initially limited supply of vaccines in the event of an influenza pandemic. https://www.apprise.org.au/project/community-perspectives-on-distributing-a-limited-supply-of-vaccines-in-the-event-of-an-influenza-pandemic/: APPRISE; 2019.
- 37.Thomas R., Sims R., Degeling C., Street J.M., Carter S.M., Rychetnik L. CJCheck Stage 1: development and testing of a checklist for reporting community juries – Delphi process and analysis of studies published in 1996–2015. Health Expect. 2016 doi: 10.1111/hex.12493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vawter D.E., Garrett J.E., Gervais K.G., Prehn A.W., DeBruin D.A. Attending to social vulnerability when rationing pandemic resources. J Clin Ethics. 2011;22:42–53. [PubMed] [Google Scholar]
- 39.Grill K, Dawson A. Ethical frameworks in public health decision-making: defending a value-based and pluralist approach. Health Care Anal. 2015:1–17. [DOI] [PubMed]
- 40.Thomas J.C., Dasgupta N., Martinot A. Ethics in a pandemic: a survey of the state pandemic influenza plans. Am J Public Health. 2007;97:S26–S31. doi: 10.2105/AJPH.2006.093443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marshall H., Ryan P., Roberton D., Street J., Watson M. Pandemic Influenza and Community Preparedness. Am J Public Health. 2009;99:S365–S371. doi: 10.2105/AJPH.2008.153056. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.