Abstract
Yellow fever virus (YFV) is the etiological agent of yellow fever (YF), an acute hemorrhagic vector-borne disease with a significant impact on public health, is endemic across tropical regions in Africa and South America. The virus is maintained in two ecologically and evolutionary distinct transmission cycles: an enzootic, sylvatic cycle, where the virus circulates between arboreal Aedes species mosquitoes and non-human primates, and a human or urban cycle, between humans and anthropophilic Aedes aegypti mosquitoes. While the urban transmission cycle has been eradicated by a highly efficacious licensed vaccine, the enzootic transmission cycle is not amenable to control interventions, leading to recurrent epizootics and spillover outbreaks into human populations. The nature of YF transmission dynamics is multifactorial and encompasses a complex system of biotic, abiotic, and anthropogenic factors rendering predictions of emergence highly speculative. The recent outbreaks in Africa and Brazil clearly remind us of the significant impact YF emergence events pose on human and animal health. The magnitude of the Brazilian outbreak and spillover in densely populated areas outside the recommended vaccination coverage areas raised the specter of human — to — human transmission and re-establishment of enzootic cycles outside the Amazon basin. Herein, we review the factors that influence the re-emergence potential of YFV in the neotropics and offer insights for a constellation of coordinated approaches to better predict and control future YF emergence events.
Keywords: arbovirus, epizootics, outbreak, re-emergence, transmission cycles, yellow fever virus
Introduction
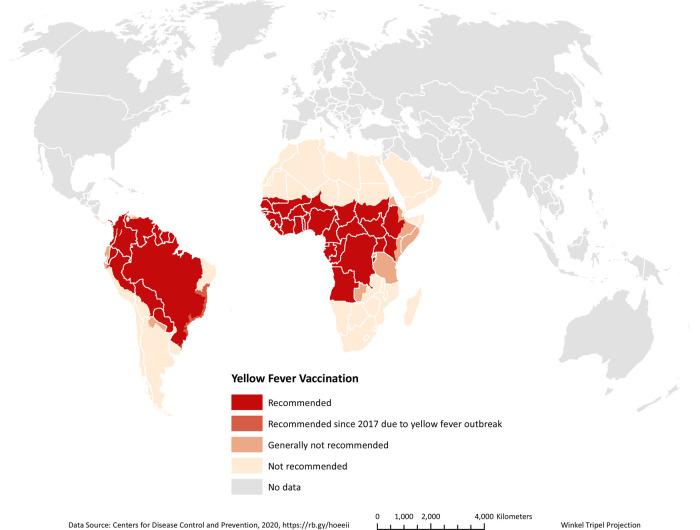
Yellow fever virus (YFV), the prototype member of the genus Flavivirus (family Flaviviridae), is the etiological agent of yellow fever (YF), an acute hemorrhagic vector-borne disease with occurrence in tropical regions of Africa and South America (Figure 1). Feared since the 17th Century [1], yellow fever was the first human disease to (i) be attributed to a virus [2], (ii) be transmitted by the anthropophilic Aedes aegypti mosquito [3], and (iii) have a licensed vaccine [4]. Undoubtedly, it is considered one of the most important infectious diseases of humans whose historical, financial, and medical significance has been well documented, as exemplified by the decimation of Caucasian colonists and their colonization campaigns in the Americas and the failure of early attempts to construct the Panama Canal.
Figure 1. Global distribution of yellow fever virus and recommended vaccination coverage areas.
The virus was introduced to the Americas from Africa in the 17th Century through the bilges of sailing ships carrying Ae. aegypti mosquitoes, which quickly established sustained transmission cycles in coastal cities, with the subsequent establishment of an enzootic, sylvatic cycle in the forests of Panama and South America. Until the eradication of its transmission cycle in North America in 1905 [5], successive YF epidemics caused significant mortality throughout the continent [1] (and reviewed in [6,7]). Sustained vector control programs under the auspices of the Pan American Health Organization (PAHO), undertaken to prevent urban epidemics of YF, led to the eradication of Ae. aegypti, the major vector of YFV transmission amongst human populations in almost all American countries [8]. This effort, coupled with massive immunization drives, led to significant declines in YF cases worldwide and no major urban outbreaks in the Americas for 80 years. However, discontinuation of the eradication program during the early 1970s allowed for the gradual reinfestation of the region by Ae. aegypti, which continued well into the present day [9–11].
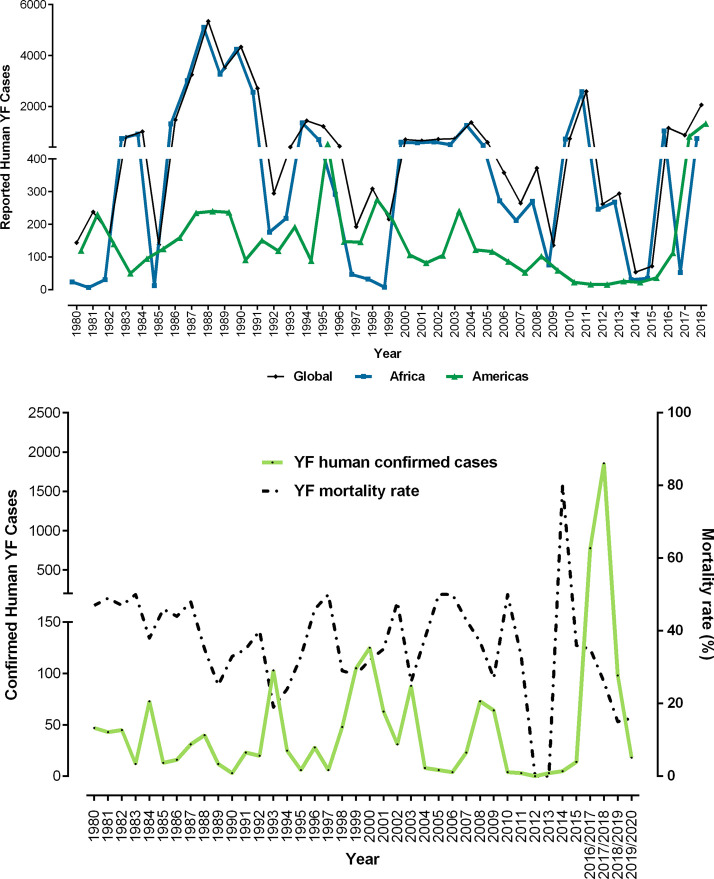
YFV outbreaks re-emerge from the forest every 7–8 years, and in the 2016–2019 outbreak in Brazil [12,13], the virus spilled over in areas without a history of acquired immunity or mandatory vaccination coverage [14], causing 2166 confirmed cases and 751 deaths [15] (Figure 2A). Similarly, a concurrent outbreak in Angola and the Democratic Republic of Congo resulted in 884 confirmed cases and 381 deaths, exporting cases as far as China [16]. Both outbreaks raised fears of initiation of urban transmission leading to massive immunization drives, severe global shortages of YF vaccines, and raising concerns for the establishment of transmission cycles in Asia [16–18]. To date, the failure to implement universal vaccination in areas at risk of transmission is a reflection of poverty, social and political instability, and access to rural areas where outbreaks are most likely to occur [19]. Moreover, the cause of YFV re-emergence events is multifactorial and involves increased densities of susceptible hosts and vectors, vector competence, climate change, viral genetic variation and fitness, insufficient vaccine coverage, uncontrolled urbanization, and deforestation [11,20].
Figure 2. Global disease burden of YFV.
(A) Human cases reported yearly by the World Health Organization (WHO), from 1980 to 2018. The numbers of cases by year for Africa (blue line) and the Americas (green line). Black line denotes the global disease burden of YFV. Data obtained from [76]. (B) Confirmed human yellow fever cases (green line) and mortality rate (black line) in Brazil, from 1980 to present day as reported by the Ministry of Health.
Epidemiology
Autochthonous (virus spread from one individual and acquired in another individual in the same place) YFV transmission occurs in 44 countries, putting nearly a billion people at risk of infection. There are ∼200 000 infections and 30 000 deaths every year, with nearly 90% of these occurring in Africa (Figure 2B), although these estimates may be inaccurate due to underreporting and misdiagnosis. Most YFV infections are asymptomatic or present as a mild undifferentiated febrile illness, with an incubation period lasting 3 to 6 days, characterized by an abrupt onset of chills, fever, headache, viremia, photophobia, lumbosacral pain, nausea, prostration, generalized myalgias, facial flushing, red tongue, and conjunctivitis. Recovery in moderately ill patients begins 3–4 days after the appearance of symptoms. However, in severe cases, this recovery is transient, also known as the period of remission, only to relapse with severe clinical manifestations, such as jaundice, albuminuria, oliguria, bradycardia (Faget's sign), delirium, stupor, metabolic acidosis, leading to shock and hemorrhage. This relapse is known as the intoxication period, and the prognosis in such cases is poor, as the case fatality rate is between 20 to 50% [11]. In South America, the mortality rate among symptomatic infections reaches 40–60% compared with 20% in West Africa, which has been attributed to cross protection by immunity to heterologous flaviviruses [19,21]. Despite the availability of a highly effective live-attenuated vaccine, sporadic human cases occur in settings of low population immunity, as well as in settings of high vaccine coverage. These likely represent spillover infection from the enzootic sylvatic transmission cycles. Since 2016, there has been a resurgence of significant YF outbreaks, notably in the Americas (Brazil) and Africa (Angola, The Democratic Republic of Congo, and Nigeria). These emergence events were directly attributed to spillover from the sylvatic cycle (Americas) or insufficient vaccine coverage due to limited health infrastructure (Africa).
In Africa, YF is distributed in West, Central, and East Africa, with the majority of YF cases and deaths taking place in sub-Saharan Africa, where YF is a major public health problem. As mentioned above, the region experiences periodic, yet unpredictable outbreaks of urban YF, spurring massive reactive vaccination campaigns. In the Americas, YF has historically been reported from North Panama to the northeast region of Argentina. However, in recent decades most of the YF activity has been reported in the Amazon Basin. YF usually occurs during the rainy season, when population densities of Haemagogus species mosquitoes are at their highest. Since 1985, the number of reported YF cases following sylvatic spillover has increased, including outbreaks in Peru [22], Bolivia [23], Paraguay [24], and Brazil [13,25] [reviewed in [26] and [27,28]] (Figure 2B). These re-emergence events are not surprising as regular epizootic activity in South America frequently results in large die-offs among susceptible non-human primate (NHP) populations and spillover into humans, especially unvaccinated agricultural and forest workers (e.g. loggers, hunters) who regularly come into contact with sylvatic mosquitoes.
Origins and evolution
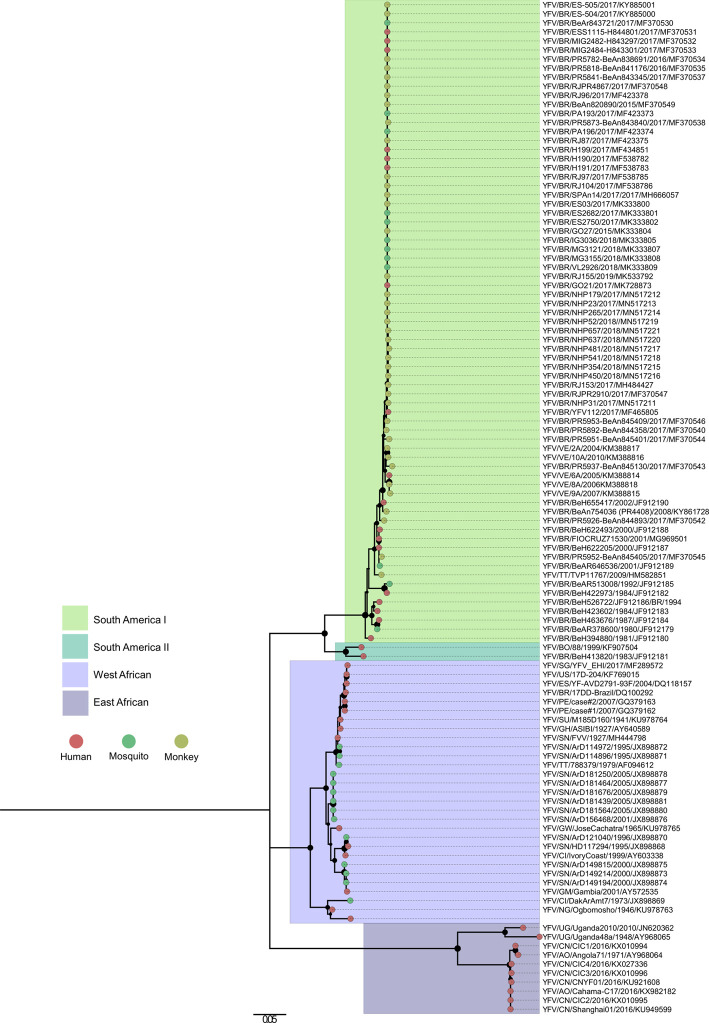
Phylogenetic analyses support the origin of YFV in the Old World, likely Central Africa [29]. While only one serotype is known for YFV, the species is genetically divided into four groups (genotypes) that differ at least 9% at the nucleotide sequence level (Figure 3). Of these, two genotypes circulate in Africa: West and East African. Ancestral strains from the West African genotype were introduced through the slave trade and seeded the American lineages, which through geographic expansion and diversification, gave rise to the two American genotypes, South America I (SA I) and South America II (SA II) [29].
Figure 3. Phylogeny of yellow fever virus.
Phylogeny of YFV virus inferred using the maximum likelihood method. The tree was obtained from a sequence dataset of 112 isolates using the General Time Reversible (GTR) substitution model. Branches are labeled with bootstrap values representing the percentage of 1000 replicates in which the members of a given clade were predicted to relate in the same topography. The scale shows a genetic distance of 0.05 or a 5% nucleotide sequence divergence. Evolutionary analyses were conducted in MEGA7 [77]. Abbreviations: VE, Venezuela; BR, Brazil; PE, Peru; TT, Trinidad and Tobago; US, USA; SU, Suriname; EC, Ecuador; BO, Bolivia; SG, Singapore; ES, Spain; GH, Ghana; SN, Senegal; GW, Guinea-Bissau; CI, Côte d'Ivoire; GM, The Gambia; NG, Nigeria; UG, Uganda; CN, China; AO, Angola.
The genetic clustering of YFV is congruent with its remarkable geographic distribution in Africa and the Americas. Like many arboviruses, YFV emergence and distribution are characterized by rapid radiation consistent with a pattern of intense diversification (‘boom and bust’ period) followed by lineage extinction (‘pruning’ period) and clade replacement. For example, in Africa the coinciding patterns of genotype and geographic clustering of YFV circulation reflect the distribution of both susceptible hosts and vectors in focal geographic areas and transmission cycles. Thus emergence events are mostly located around rainforest transition zones, supporting the notion of sylvatic maintenance with periodic spillover events causing outbreaks into human populations [30]. Similarly, the evolutionary dynamics of YFV in the Americas are well characterized by local circulation, in situ evolution, and sporadic re-emergence events between regions or countries. Here both genotypes, SA I and SA II, have diversified into several concurrent enzootic lineages that appear to persist and evolve within distinct geographic areas of Brazil, Bolivia, Peru, Venezuela, and the Caribbean for extended periods [12–14,29,31–35].
Ecology
Transmission cycles
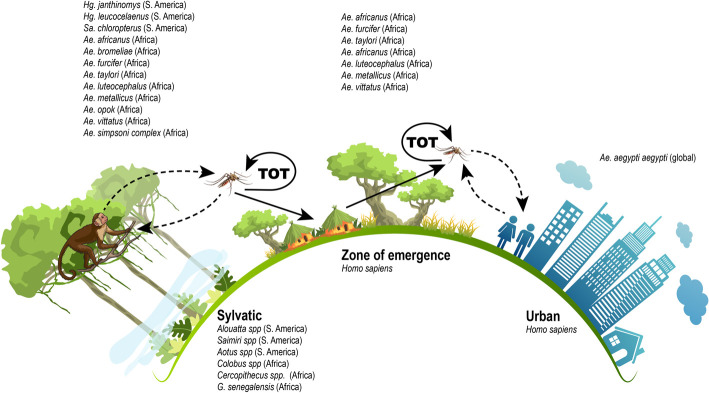
The transmission cycles of YFV include: (i) an enzootic sylvatic cycle, where the virus circulates between arboreal mosquitoes and NHPs; (ii) a human or urban cycle, between humans and peridomestic/domestic mosquitoes; and (iii) a zone of emergence, observed in rural areas of Africa and the Americas where enzootic vector(s) often reach high densities and YFV can transfer between NHPs and humans resulting in the onset of epidemic outbreaks. Transovarial transmission (transmission from parent to offspring via the ovaries) (ToT) of YFV in mosquitoes had been demonstrated in both human and sylvatic transmission cycles and may provide a mechanism for the maintenance of the transmission cycles in inter-epidemic periods [36,37] (Figure 4). In Africa, the virus is vectored exclusively by Aedes spp., whereas in the Americas it is also vectored by Haemagogus and Sabethes spp. mosquitoes. Several primate genera are involved in the maintenance of YFV: In Africa, Colobus, Cercopithecus, Erythrocebus, and Galago species), and in the Americas, Alouatta, Saimiri, and Aotus species serve as sylvatic hosts (Figure 4). Unlike New World monkeys, very few species of African monkeys succumb to lethal infection, which may explain the shorter interval between periods of YFV activity in the forests of Africa. In the human or urban transmission cycle, maintenance of the virus involves exclusively humans and the anthropophilic Ae. aegypti mosquitoes (Figure 4) (reviewed in [26]).
Figure 4. Transmission cycles of yellow fever virus.
Abbreviation: TOT, transovarial transmission.
Curiously, despite several opportunities for the introduction (as recently as 2016) and spread of YFV in Asia, where Ae. aegypti mosquitoes are abundant and over 2 billion of immunologically naïve human populations currently reside, the virus has failed to establish a detectable autochthonous transmission cycle. Several hypotheses have been proposed to account for this paradox, including (i) cross-protection afforded by immunity to heterologous flaviviruses endemic in the region, such as dengue, Japanese encephalitis, Zika, West Nile, and others [38]. (ii), competitive exclusion of YFV by these arboviruses in susceptible Asian mosquito populations may also play a role (reviewed in [26]); (iii) lower vector competence among Asian Ae. aegypti strains compared with those in Africa and the Americas [39,40]; and (iv) inherent differences among African YFV strains. Strains from East Africa are considered more likely to have entered Asia, whereas West African strains were successful in seeding autochthonous transmission in the Americas [29].
Factors shaping YFV transmission cycles
Typical among arboviral transmission cycles, YFV cycles are influenced by several extrinsic (e.g. biotic, abiotic, and anthropogenic) factors. The vectorial nature of YFV transmission implies an inherent dependence on (i) climatic factors, such as temperature, precipitation, and humidity, which have an impact on mosquito distributions, densities, and physiology, which consequently influence viral transmission; (ii) vegetation coverage, as well as biodiversity in a given area, which modulate vector–host–virus interactions; and (iii) anthropogenic influences, including urban expansion, alteration of land use, population densities and immunization coverage.
Documented rises in average temperatures and precipitation patterns are clear indications of global climate change [41]. A recent report by the ‘The Intergovernmental Panel on Climate Change' (IPCC) suggested that if current trends continue, the global mean temperatures will likely rise by 1.5°C between 2030 and 2052 [42]. Higher levels of precipitation create better conditions for the reproduction of mosquitoes. On the other hand, warmer temperatures accelerate the development of larvae, increase rates of YF viral replication, and aid in the wider dissemination of vectors such as Aedes and Haemagogus species [43–45]. Human behavior and alterations in land-use practices, including recent upticks in deforestation for agriculture, logging, and mining can culminate in the generation of new habitats for hosts and vectors, altering vector–host interactions, host utilization of particular species in particular land cover types, and thus their potential role in pathogen maintenance and spillover [44,46]. Although Hg. leucocelanus and Hg. janthinomys are considered primatophilic and typically found on the tree canopies, they can travel great distances and be found at ground level around forests or even feeding indoors in rural settings [45,47–49]. The proximity of sylvatic vectors to peri-urban and urban areas should be of particular concern to public health authorities, considering the total reinfestation of major urban centers by Ae. aegypti throughout Central and South America. Therefore, climate and environmental changes could have unprecedented and complex effects on the emergence of YF and other arboviral and zoonotic diseases [50].
Periodicity of epizootic outbreaks in the Americas
Historical epizootic outbreaks show a pattern of periodic or ‘wandering’ epizootic outbreaks characterized by the cyclical occurrence and disappearance of outbreaks within particular geographic areas [22]. It is hypothesized that maintenance of YFV in the enzootic transmission cycle is through NHPs that move continuously throughout their geographic range in the Amazon basin. The appearance of wandering epizootics is supported by localized foci of disease incidence peaks, where the virus sweeps through susceptible NHP populations, then disappears while the focus of transmission moves onward to a distant location along forest galleries in the vast river networks of the Amazon basin [51]. All neotropical NHP species are highly susceptible to YFV infection, leading to massive die-offs signaling the onset of epizootics. Surviving NHP populations develop solid immunity, and the length of inter-epidemic intervals between epizootics represents the time required for reconstruction of susceptible NHP populations (reviewed in [26]. In Brazil alone, several epizootics were reported all over the country occurring on average every 6–7 years from 1933 up to the recent outbreak of 2016–2019. However, reconstruction of susceptible NHP populations does not readily explain the documented occurrence of the 2008–2009 synchronous epizootics in widely separated locations in South America (Trinidad, Paraguay, Peru, Colombia, Venezuela, Argentina and Brazil). Possible factors that may have contributed to the synchronicity of these epizootics include rapid movement and initiation by infected humans or trafficking of infected monkeys and stochastic seeding by genetically distinct strains. Overall, a range of factors influences YF activity within enzootic cycles, including the presence of the virus, distribution and sizes of susceptible vector and, host populations and climatic conditions, such as duration of the rainy season, humidity, and temperature. Despite extensive efforts to study the YFV enzootic cycles in South America and reported associations between epizootic activity and multiple variables, the parameters most important for influencing the enzootic transmission cycle and the factors that trigger human outbreaks remain poorly understood.
Unlike the urban transmission cycle, complete eradication of the enzootic transmission cycle poses severe challenges since it is not amenable to typical control interventions. However, although there is supportive evidence that a monkey vaccination strategy could be effective in decreasing YFV infection, thus reducing viral circulation and consequently spillover risk for humans [52], it is considered logistically impossible to implement vaccination in the vast Amazon basin and Atlantic rainforest (but see [53]). While there is support that such a strategy will be effective in smaller areas (e.g. urban parks) [54], NHP vaccination will require additional studies for veterinary use approval.
Predictive modeling for YFV ecology
As with all zoonoses, predicting how YFV transmission risk changes over space and time remains a formidable challenge. Hosts and vectors that comprise the sylvatic cycles of mosquito-borne flaviviruses are dynamic and difficult to observe, and they are increasingly subject to anthropogenic disturbance. Zoonotic risk predictions for human spillover may be improved by drawing upon modeling methods that make use of empirical data describing wildlife hosts (NHPs), mosquito vectors, and environments that have supported historical spillover transmission. Statistical (machine) learning methods have leveraged robust covariation patterns in biological and ecological data to better estimate and identify drivers of zoonotic disease risk. For instance, Han et al. [55] applied machine learning to data describing traits of NHPs associated with mosquito-borne flaviviruses with the goal of predicting which species pose the greatest risk as future sources of spillover infection to humans. Similar approaches have been applied to mosquito traits associated with vector competence, and when combined with network approaches, these associations can point to unobserved NHP — mosquito vector relationships that may be contributing to enzootic cycles [56].
Given the inherent difficulty of observing pathogen transmission per se, machine learning methods combined with transmission models enable investigation of infection dynamics and comparisons of zoonotic risk posed by multiple host (or suspected host) species comprising the sylvatic cycle [57]. For instance, compartmental SIR-type models parameterized through data mining on host traits reveal differential contributions of host species to important epidemiological quantities such as outbreak size, equilibrium prevalence, and reproduction number (R0) [57]. Analyzing dynamical models in a comparative way (for instance, looking at the dynamics generated across multiple NHPs and vectors) may reveal parameters that are particularly influential for YFV transmission dynamics and species that are particularly important for spillover transmission. In addition to organismal factors, machine learning of environmental factors describing YFV spillover [58], in combination with transmission models of YFV transmission [59] can help distinguish the relative importance of multiple interacting factors contributing to the risk of spillover transmission.
Reflections on the recent Brazilian outbreak
The significance of the 2016–2018 Brazilian YFV outbreak was that it took place outside the endemic region of the Amazon basin, resulting in the largest epizootic/epidemic of sylvatic YF in Brazil since the 1940s. Viruses from two lineages fueled this outbreak, one represented by strains closely related to viruses sampled previously in Venezuela [60], and the other represented a newly emerged lineage, originating in the state of Goiás in 2014. The new lineage was introduced and circulated undetected into the state of Minas Gerais for almost two years prior to the explosive growth of the outbreak by the end of 2016, at which time it radiated out into the Southeast region of Brazil in at least two independent events and persisted at least up to 2019 [28,60,61]. From 2016 to 2020, the outbreaks reached YFV-free areas in the Southeast and South of Brazil (Figure 1), raising concerns for the re-establishment of sylvatic cycles [62].
Contrary to the previous spillover events, these outbreaks spread rapidly, extensively, and in proximity to densely populated regions. YFV-infected NHP carcasses were collected inside urban areas in different parts of the country [35,63]. In Minas Gerais state alone, high YF positivity was observed in NHP carcasses collected in urban areas with a widespread occurrence in 67 municipalities within the state, alarming public health authorities for the specter of urban YFV transmission vectored by Ae. aegypti [63], an occurrence last documented in 1942. However, no human cases were epidemiologically linked to YFV circulation in urban areas and there was no evidence of urban YFV transmission by Ae. aegypti [35]. Furthermore, several lines of evidence supported sylvatic origin and transmission in this outbreak: (i) distribution of human and NHP YF cases largely overlapped from 2016 to 2018 [62]; and (ii) despite co-circulation of multiple lineages during the outbreaks [60,61], there was no evidence of molecular signatures suggestive of adaptation for increased infectivity in humans [13].
The silent circulation of YFV outside the Amazon basin for almost two years before its detection at the end of 2016 and the vast geographical expansion of the outbreaks to previously considered YF-free areas, are of great concern leading the Brazilian authorities to revise their immunization policies for yellow fever. Control of outbreaks in human populations depends on the use of the safe and highly efficacious vaccine, requiring and maintaining a minimum of 80% coverage to achieve herd immunity [64,65]. Vaccination is recommended for persons of 9 months of age and older and a single dose of the vaccine with boosters every 10 years is highly efficacious and confers life-long protection against YFV [66]. However, recent studies suggested limited serologic protection in children after vaccination [67,68]. In 2013, WHO recommended that a single dose is sufficient to elicit life-long protection [69], and booster doses should be determined on a case-by-case basis and restricted to special populations, including young children, pregnant women, and immunocompromised individuals [70,71]. Moreover, the recent outbreaks resulted in massive immunization drives and consequently severe global shortages of YF vaccines, leading to the implementation of a fractional-dosing strategy to provide vaccination coverage to susceptible populations [72,73]. Fractional dosing involved giving vaccinees one-fifth of a vaccine dose containing no less than 1000 international units/dose and a number of studies demonstrated protective immune responses lasting years post-vaccination [17,74]. Consequently in 2017, Brazil implemented the use of either single or fractional dosing and expansion of geographic areas subject to mandatory vaccination. These strategies increased the vaccination coverage from 3526 cities and municipalities in 2010 to 4469 in 2018, which led to a significant reduction in subsequent outbreaks [62]. The strengthening of vaccination in Brazil's Southeast region during and immediately after the first wave in 2016/2017 seemed to impact outbreak dynamics with a southward displacement, but only after the second wave of the outbreak in 2017/2018, the number of cases had decreased significantly [62]. However, despite these immunization campaigns, as of June 2020, the average vaccination coverage stands at 40.14% of the population, with more than 116.2 million unvaccinated people at risk for YFV infection [75].
Collectively, the recent outbreaks reiterated the unpredictability of spillovers and their potential to cause significant outbreaks, reinforcing the need for sustained surveillance strategies and control strategies in both humans and NHPs, to better assist in the monitoring and understanding of YFV dynamics, to quantify and prevent the risk of spillover infection and future outbreaks, and to prevent re-establishment of a sylvatic transmission cycle in the Atlantic rainforest.
Conclusion
Several factors influence the re-emergence potential of YFV, such as inadequate vaccination coverage, inability to control sylvatic transmission cycles, reinfestation of major urban centers by Ae. aegypti, and inadequate vector control strategies. These factors represent a clear and present threat for the return of urban YF in the Americas. Enhanced surveillance of human and NHP populations at risk for YFV infection is crucial for the early detection and rapid containment of YFV transmission. Additionally, longitudinal studies of NHP and mosquito populations are urgently needed in order to understand the maintenance of YFV in the inter-epidemic periods and the mechanisms of emergence that drive epizootics and spillovers from susceptible hosts (NHPs and humans) via competent vectors of transmission. Given the overly optimistic WHO mandate for the elimination of yellow fever epidemics by 2026, it will require a global and coordinated constellation of elimination strategies. We are sanguine that a multifaceted approach encompassing basic research on virus — vector — host interactions, sustainable genomic and environmental surveillance, modeling tools, and community outreach will combine to offer a powerful coordinated approach to better predict and control YF emergence.
Summary
Yellow fever virus (YFV) is an arbovirus with a significant impact on human public health.
Enzootic, sylvatic, YFV transmission cycles are maintained among non-human vertebrate hosts and arboreal mosquitoes in a specific geographic region of Africa and the Americas. They are not amenable to control interventions and thus a constant source of virus spillovers.
There are still gaps in our knowledge about the factors that influence emergence of YFV, which include increased densities of susceptible hosts and vectors, vector competence, climate change, viral genetic variation and fitness, insufficient vaccine coverage, uncontrolled urbanization, and deforestation.
Progress toward understanding the drivers of emergence require statistical and dynamical modeling approaches informed by coordinated data collection, and model iteration with empirical data from field surveillance. These approaches have independently been shown to generate actionable predictions for zoonotic spillover, and may together deepen our understanding of how drivers combine to precipitate spillover transmission.
Finally, future prediction and control of YFV emergence events will require basic research on virus – vector – host interactions, sustainable genomic and environmental surveillance, novel vaccination strategies in controlling enzootic cycles, modeling tools, and community outreach.
Acknowledgements
We are grateful to the expert graphical design of Prof. Michaela Buenemann, Department of Geography, New Mexico State University (Figure 1) and Mrs. Mary Joe Singleton (Figure 4).
Abbreviations
- IPCC
The Intergovernmental Panel on Climate Change
- NHP
non-human primate
- PAHO
Pan American Health Organization
- SA I
South America I
- SA II
South America II
- TOT
transovarial transmission
- WHO
World Health Organization
- YF
yellow fever
- YFV
Yellow fever virus
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
This research was funded by the Centers for Research in Emerging Infectious Diseases “The Coordinating Research on Emerging Arboviral Threats Encompassing the Neotropics (CREATE-NEO)” grant U01 AI151807 from the U.S. National Institutes of Health (to N.V.) and grants 2013/21719-3 from FAPESP (Fundação de Amparo a Pesquisa do Estado de São Paulo)(to M.L.N.), APQ-01574-17 from FAPEMIG/SES-MG/SEPLAG-MG/FIOCRUZ (to B.P.D.). M.L.N. and B.P.D. are CNPq Research Fellows. B.A.H. acknowledges funding from the Ecology and Evolution of Infectious Disease (EEID) program from the U.S. National Science Foundation (DEB 1717282). The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Author Contributions
All authors contributed equally in the conceptualization, writing of the original draft, and the revision of this manuscript.
References
- 1.Rush A.B. (1789) An Account of the Bilious Remitting Fever, as it Appeared in Philadelphia in the Summer and Autumn of the Year 1780. Medical Inquiries and Observations, Prichard and Hall, Philadelphia [Google Scholar]
- 2.Stokes A., Bauer J.H. and Hudson N.P. (1928) Experimental transmission of yellow fever to Macacus rhesus. A preliminary note. J. Amer. Med. Assoc. 90, 253 10.1001/jama.1928.02690310005002 [DOI] [Google Scholar]
- 3.Reed W., Carroll J., Agramonte A. and Lazear J.W. (1900) The etiology of yellow fever. A preliminary note. Mil. Med. 166, 29–36 10.1093/milmed/166.suppl_1.29 [DOI] [PubMed] [Google Scholar]
- 4.Theiler M. and Smith H.H. (1937) The use of yellow fever virus modified by in vitro cultivation for human immunization. J. Exp. Med. 65, 787–800 10.1084/jem.65.6.787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carrigan J.A. (1967) Yellow fever in New orleans, 1905: the last epidemic. Bull. Tulane Med. Fac. 26, 19–28 PMID:16250373 [Google Scholar]
- 6.Duffy J. (1968) Yellow fever in the continental United States during the nineteenth century. Bull. N. Y. Acad. Med. 44, 687–701 PMID: [PMC free article] [PubMed] [Google Scholar]
- 7.Duffy J. (1953) Epidemics in Colonial America, Louisiana State University Press [Google Scholar]
- 8.Soper F.L., Wilson D.B., Lima S. and Antunes W.S. (1943) The Organization of Permanent Nationwide Anti-Aedes Aegypti Measures in Brazil, The Rockefeller Foundation, New York [Google Scholar]
- 9.Kraemer M.U.G., Reiner R.C. Jr, Brady O.J., Messina J.P., Gilbert M., Pigott D.M. et al. (2019) Past and future spread of the arbovirus vectors Aedes aegypti and Aedes albopictus. Nat. Microbiol. 4, 854–863 10.1038/s41564-019-0376-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kraemer M.U., Sinka M.E., Duda K.A., Mylne A.Q., Shearer F.M., Barker C.M. et al. (2015) The global distribution of the arbovirus vectors Aedes aegypti and Ae albopictus. eLife 4, e08347 10.7554/eLife.08347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Monath T.P. (1986) Yellow fever In The Arboviruses: Epidemiology and Ecology (Monath T.P., ed.), pp. 139–231, V. Boca Raton, FL, CRC Press, Inc [Google Scholar]
- 12.Giovanetti M., de Mendonca M.C.L., Fonseca V., Mares-Guia M.A., Fabri A., Xavier J. et al. (2019) Yellow fever virus reemergence and spread in southeast Brazil, 2016–2019. J. Virol. 94, e01623-19 10.1128/JVI.01623-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faria N.R., Kraemer M.U.G., Hill S.C., Goes de Jesus J., Aguiar R.S., Iani F.C.M. et al. (2018) Genomic and epidemiological monitoring of yellow fever virus transmission potential. Science 361, 894–899 10.1126/science.aat7115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cunha M.S., da Costa A.C., de Azevedo Fernandes N.C.C., Guerra J.M., Dos Santos F.C.P., Nogueira J.S. et al. (2019) Epizootics due to yellow fever virus in Sao Paulo state, Brazil: viral dissemination to new areas (2016–2017). Sci. Rep. 9, 5474 10.1038/s41598-019-41950-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.PAHO. Epidemiological update: yellow fever 25 January 2019 Available from: https://www.paho.org/hq/index.php?option=com_docman&view=download&category_slug=yellow-fever-2194&alias=47621-25-january-2019-yellow-fever-epidemiological-update-1&Itemid=270&lang=en
- 16.Song R., Guan S., Lee S.S., Chen Z., Chen C., Han L. et al. (2018) Late or lack of vaccination linked to importation of yellow fever from Angola to China. Emerg. Infect. Dis. 24, 1383–1386 10.3201/eid2407.171868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Casey R.M., Harris J.B., Ahuka-Mundeke S., Dixon M.G., Kizito G.M., Nsele P.M. et al. (2019) Immunogenicity of fractional-dose vaccine during a yellow fever outbreak - final report. N. Engl. J. Med. 381, 444–454 10.1056/NEJMoa1710430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kraemer M.U.G., Faria N.R., Reiner R.C. Jr, Golding N., Nikolay B., Stasse S. et al. (2017) Spread of yellow fever virus outbreak in Angola and the democratic republic of the Congo 2015-16: a modelling study. Lancet Infect. Dis. 17, 330–338 10.1016/S1473-3099(16)30513-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barrett A.D. and Higgs S. (2007) Yellow fever: a disease that has yet to be conquered. Annu. Rev. Entomol. 52, 209–229 10.1146/annurev.ento.52.110405.091454 [DOI] [PubMed] [Google Scholar]
- 20.Vasconcelos P.F., Rodrigues S.G., Degallier N., Moraes M.A., da Rosa J.F., da Rosa E.S. et al. (1997) An epidemic of sylvatic yellow fever in the southeast region of Maranhao State, Brazil, 1993–1994: epidemiologic and entomologic findings. Am. J. Trop. Med. Hyg. 57, 132–137 10.4269/ajtmh.1997.57.132 [DOI] [PubMed] [Google Scholar]
- 21.Calisher C.H., Karabatsos N., Dalrymple J.M., Shope R.E., Porterfield J.S., Westaway E.G. et al. (1989) Antigenic relationships between flaviviruses as determined by cross-neutralization tests with polyclonal antisera. J. Gen. Virol. 70, 37–43 10.1099/0022-1317-70-1-37 [DOI] [PubMed] [Google Scholar]
- 22.Bryant J., Wang H., Cabezas C., Ramirez G., Watts D., Russell K. et al. (2003) Enzootic transmission of yellow fever virus in Peru. Emerg. Infect. Dis. 9, 926–933 10.3201/eid0908.030075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van der Stuyft P., Gianella A., Pirard M., Cespedes J., Lora J., Peredo C. et al. (1999) Urbanisation of yellow fever in santa cruz, Bolivia. Lancet 353, 1558–1562 10.1016/S0140-6736(99)03291-2 [DOI] [PubMed] [Google Scholar]
- 24.Outbreak news. (2008) Yellow fever, Paraguay. Wkly Epidemiol. Rec. 83, 105 PMID: [PubMed] [Google Scholar]
- 25.Dietz J.M., Hankerson S.J., Alexandre B.R., Henry M.D., Martins A.F., Ferraz L.P. et al. (2019) Yellow fever in Brazil threatens successful recovery of endangered golden lion tamarins. Sci. Rep. 9, 12926 10.1038/s41598-019-49199-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanley K.A., Monath T.P., Weaver S.C., Rossi S.L., Richman R.L. and Vasilakis N. (2013) Fever versus fever: The role of host and vector susceptibility and interspecific competition in shaping the current and future distributions of the sylvatic cycles of dengue virus and yellow fever virus. Infect. Genet. Evol. 19C, 292–311 10.1016/j.meegid.2013.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paules C.I. and Fauci A.S. (2017) Yellow fever: once again on the radar screen in the Americas. N. Engl. J. Med. 376, 1397–1399 10.1056/NEJMp1702172 [DOI] [PubMed] [Google Scholar]
- 28.Rezende I.M., Sacchetto L., Munhoz de Mello E., Alves P.A., Iani F.C.M., Adelino T.E.R. et al. (2018) Persistence of yellow fever virus outside the Amazon basin, causing epidemics in southeast Brazil, from 2016 to 2018. PLoS Negl. Trop. Dis. 12, e0006538 10.1371/journal.pntd.0006538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bryant J.E., Holmes E.C. and Barrett A.D. (2007) Out of Africa: a molecular perspective on the introduction of yellow fever virus into the Americas. PLoS Pathog. 3, e75 10.1371/journal.ppat.0030075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beck A., Guzman H., Li L., Ellis B., Tesh R.B. and Barrett A.D. (2013) Phylogeographic reconstruction of African yellow fever virus isolates indicates recent simultaneous dispersal into east and West Africa. PLoS Negl. Trop. Dis. 7, e1910 10.1371/journal.pntd.0001910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li Y. and Yang Z. (2017) Adaptive diversification between yellow fever virus West African and South American lineages: a genome-wide study. Am. J. Trop. Med. Hyg. 96, 727–734 10.4269/ajtmh.16-0698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nunes M.R., Palacios G., Cardoso J.F., Martins L.C., Sousa E.C. Jr, de Lima C.P. et al. (2012) Genomic and phylogenetic characterization of Brazilian yellow fever virus strains. J. Virol. 86, 13263–13271 10.1128/JVI.00565-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mir D., Delatorre E., Bonaldo M., Lourenco-de-Oliveira R., Vicente A.C. and Bello G. (2017) Phylodynamics of yellow fever virus in the Americas: new insights into the origin of the 2017 Brazilian outbreak. Sci. Rep. 7, 7385 10.1038/s41598-017-07873-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Souza R.P., Foster P.G., Sallum M.A., Coimbra T.L., Maeda A.Y., Silveira V.R. et al. (2010) Detection of a new yellow fever virus lineage within the South American genotype I in Brazil. J. Med. Virol. 82, 175–185 10.1002/jmv.21606 [DOI] [PubMed] [Google Scholar]
- 35.Silva N.I.O., Sacchetto L., de Rezende I.M., Trindade G.S., LaBeaud A.D., de Thoisy B. et al. (2020) Recent sylvatic yellow fever virus transmission in Brazil: the news from an old disease. Virol. J. 17, 9 10.1186/s12985-019-1277-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beaty B.J., Tesh R.B. and Aitken T.H. (1980) Transovarial transmission of yellow fever virus in stegomyia mosquitoes. Am. J. Trop. Med. Hyg. 29, 125–132 10.4269/ajtmh.1980.29.125 [DOI] [PubMed] [Google Scholar]
- 37.Cornet M., Robin Y., Heme G., Adam C., Renaudet J., Valade M. et al. (1979) Une pousse epizootique de fievre selvatique au Senegal oriental. Isolement dur virus de lots de moustiques adultes males et femelles. Med. Mal. Infect 9, 63 10.1016/S0399-077X(79)80024-4 [DOI] [Google Scholar]
- 38.Ashcroft M.T. (1979) Historical evidence of resistance to yellow fever acquired by residence in India. Trans. R. Soc. Trop. Med. Hyg. 73, 247–248 10.1016/0035-9203(79)90232-3 [DOI] [PubMed] [Google Scholar]
- 39.Tabachnick W.J., Wallis G.P., Aitken T.H., Miller B.R., Amato G.D., Lorenz L. et al. (1985) Oral infection of aedes aegypti with yellow fever virus: geographic variation and genetic considerations. Am. J. Trop. Med. Hyg. 34, 1219–1224 10.4269/ajtmh.1985.34.1219 [DOI] [PubMed] [Google Scholar]
- 40.Aitken T.H., Downs W.G. and Shope R.E. (1977) Aedes aegypti strain fitness for yellow fever virus transmission. Am. J. Trop. Med. Hyg. 26, 985–989 10.4269/ajtmh.1977.26.985 [DOI] [PubMed] [Google Scholar]
- 41.Gaythorpe K.A., Hamlet A., Cibrelus L., Garske T. and Ferguson N.M. (2020) The effect of climate change on yellow fever disease burden in Africa. eLife 9, e55619 10.7554/eLife.55619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Masson-Delmotte V., Zhai P., Pörtner H.-O., Roberts D., Skea J., Shukla P.R. et al. (2018) IPCC, 2018: Summary for Policymakers. Global Warming of 1.5°C. An IPCC Special Report on the Impacts of Global Warming of 1.5°C Above pre-Industrial Levels and Related Global Greenhouse gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty, World Meteorological Organization, Geneva, Switzerland [Google Scholar]
- 43.Chouin-Carneiro T., David M.R., de Bruycker Nogueira F., Dos Santos F.B. and Lourenco-de-Oliveira R. (2020) Zika virus transmission by Brazilian Aedes aegypti and Aedes albopictus is virus dose and temperature-dependent. PLoS Negl. Trop. Dis. 14, e0008527 10.1371/journal.pntd.0008527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hendy A., Hernandez-Acosta E., Chaves B.A., Fe N.F., Valerio D., Mendonca C. et al. (2020) Into the woods: changes in mosquito community composition and presence of key vectors at increasing distances from the urban edge in urban forest parks in Manaus, Brazil. Acta Trop. 206, 105441 10.1016/j.actatropica.2020.105441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Possas C., Lourenco-de-Oliveira R., Tauil P.L., Pinheiro F.P., Pissinatti A., Cunha R.V.D. et al. (2018) Yellow fever outbreak in Brazil: the puzzle of rapid viral spread and challenges for immunisation. Mem. Inst. Oswaldo Cruz 113, e180278 10.1590/0074-02760180278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Young K.I., Medwid J.T., Azar S.R., Huff R.M., Drumm H., Coffey L.L. et al. (2020) Identification of mosquito bloodmeals collected in diverse habitats in Malaysian Borneo using COI barcoding. Trop. Med. Infect. Dis. 5, 51 10.3390/tropicalmed5020051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gomes Ade C., Torres M.A., Ferri L., da Costa F.R. and da Silva A.M. (2007) [Finding of haemagogus (Conopostegus) leucocelaenus (Diptera: Culicidae), in the municipality of Porto Alegre, state of Rio Grande do Sul]. Rev. Soc. Bras. Med. Trop. 40, 487–488 10.1590/S0037-86822007000400025 [DOI] [PubMed] [Google Scholar]
- 48.Abreu F.V.S., Ribeiro I.P., Ferreira-de-Brito A., Santos A., Miranda R.M., Bonelly I.S. et al. (2019) Haemagogus leucocelaenus and Haemagogus janthinomys are the primary vectors in the major yellow fever outbreak in Brazil, 2016–2018. Emerg. Microbes Infect. 8, 218–231 10.1080/22221751.2019.1568180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hendy A., Hernandez Acosta E., Valério D., Mendonça C., Rodrigues E., Júnior J.T.A. et al. (2020) The vertical stratification of known and potential vectors of sylvatic arboviruses at the Adolpho Ducke forest reserve in Manaus, Brazil. Sci. Rep. 10, 18254 10.1038/s41598-020-75178-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ryan S.J., Carlson C.J., Mordecai E.A. and Johnson L.R. (2019) Global expansion and redistribution of Aedes-borne virus transmission risk with climate change. PLoS Negl. Trop. Dis. 13, e0007213 10.1371/journal.pntd.0007213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Downs W.G. (1982) The known and the unknown in yellow fever ecology and epidemiology. Ecol. Dis. 1, 103–110 PMID: [PubMed] [Google Scholar]
- 52.Mason R.A., Tauraso N.M., Spertzel R.O. and Ginn R.K. (1973) Yellow fever vaccine: direct challenge of monkeys given graded doses of 17D vaccine. Appl. Microbiol. 25, 539–544 10.1128/AEM.25.4.539-544.1973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rushmore J., Caillaud D., Hall R.J., Stumpf R.M., Meyers L.A. and Altizer S. (2014) Network-based vaccination improves prospects for disease control in wild chimpanzees. J. R. Soc. Interface 11, 20140349 10.1098/rsif.2014.0349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Massad E., Miguel M.M. and Coutinho F.A.B. (2018) Is vaccinating monkeys against yellow fever the ultimate solution for the Brazilian recurrent epizootics? Epidemiol. Infect. 146, 1622–1624 10.1017/S0950268818002273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Han B.A., Majumdar S., Calmon F.P., Glicksberg B.S., Horesh R., Kumar A. et al. (2019) Confronting data sparsity to identify potential sources of Zika virus spillover infection among primates. Epidemics 27, 59–65 10.1016/j.epidem.2019.01.005 [DOI] [PubMed] [Google Scholar]
- 56.Evans M.V., Dallas T.A., Han B.A., Murdock C.C. and Drake J.M. (2017) Data-driven identification of potential zika virus vectors. eLife 6, e22053 10.7554/eLife.22053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Han B.A., O'Regan S.M., Paul Schmidt J. and Drake J.M. (2020) Integrating data mining and transmission theory in the ecology of infectious diseases. Ecol. Lett. 23, 1178–1188 10.1111/ele.13520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kaul R.B., Evans M.V., Murdock C.C. and Drake J.M. (2018) Spatio-temporal spillover risk of yellow fever in Brazil. Parasit. Vectors 11, 488 10.1186/s13071-018-3063-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Childs M.L., Nova N., Colvin J. and Mordecai E.A. (2019) Mosquito and primate ecology predict human risk of yellow fever virus spillover in Brazil. Philos. Trans. R. Soc. Lond. 374, 20180335 10.1098/rstb.2018.0335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Delatorre E., de Abreu F.V.S., Ribeiro I.P., Gomez M.M., Dos Santos A.A.C., Ferreira-de-Brito A. et al. (2019) Distinct YFV lineages co-circulated in the central-Western and southeastern Brazilian regions from 2015 to 2018. Front. Microbiol. 10, 1079 10.3389/fmicb.2019.01079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moreira-Soto A., Torres M.C., Lima de Mendonca M.C., Mares-Guia M.A., Dos Santos Rodrigues C.D., Fabri A.A. et al. (2018) Evidence for multiple sylvatic transmission cycles during the 2016–2017 yellow fever virus outbreak, Brazil. Clin. Microbiol. Infect. 24, 1019 e1–e4 10.1016/j.cmi.2018.01.026 [DOI] [PubMed] [Google Scholar]
- 62.de Thoisy B., Silva N.I.O., Sacchetto L., Trindade G.S. and Drumond B.P. (2020) Spatial epidemiology of yellow fever: identification of determinants of the 2016-2018 epidemics and at-risk areas in Brazil. PLoS Negl. Trop. Dis. 14, e0008691 10.1371/journal.pntd.0008691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sacchetto L., Silva N.I.L., Rezende I.M., Arruda M.S., Costa T.A., Mello E.M. et al. (2020) Neighbor danger: yellow fever virus epizootics in urban and urban-rural transition areas of Minas Gerais state, during 2017-2018 yellow fever outbreaks in Brazil. PLoS Negl. Trop. Dis. 14, e0008658 10.1371/journal.pntd.0008658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barrett A.D., Monath T.P., Barban V., Niedrig M. and Teuwen D.E. (2007) 17D yellow fever vaccines: new insights. A report of a workshop held during the world congress on medicine and health in the tropics, Marseille, France, Monday 12 September 2005. Vaccine 25, 2758–2765 10.1016/j.vaccine.2006.12.015 [DOI] [PubMed] [Google Scholar]
- 65.Ndeffo-Mbah M.L. and Pandey A. (2020) Global risk and elimination of yellow fever epidemics. J. Infect. Dis. 221, 2026–2034 10.1093/infdis/jiz375 [DOI] [PubMed] [Google Scholar]
- 66.Gotuzzo E., Yactayo S. and Cordova E. (2013) Efficacy and duration of immunity after yellow fever vaccination: systematic review on the need for a booster every 10 years. Am. J. Trop. Med. Hyg. 89, 434–444 10.4269/ajtmh.13-0264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Idoko O.T., Domingo C., Tapia M.D., Sow S.O., Geldmacher C., Saathoff E. et al. (2020) Serological protection 5-6 years post vaccination against yellow fever in African infants vaccinated in routine programmes. Front. Immunol. 11, 577751 10.3389/fimmu.2020.577751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.de Melo A.B., da Silva Mda P., Magalhaes M.C., Gonzales Gil L.H., Freese de Carvalho E.M., Braga-Neto U.M. et al. (2011) Description of a prospective 17DD yellow fever vaccine cohort in Recife, Brazil. Am. J. Trop. Med. Hyg. 85, 739–747 10.4269/ajtmh.2011.10-0496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.WHO. (2013) Vaccines and vaccination against yellow fever: WHO position paper — June 2013. Wkly Epidemiol Rec. 88, 269–283 PMID: [PubMed] [Google Scholar]
- 70.Barrett A.D.T. (2020) Yellow fever vaccine: the conundrum of 2 doses, one dose, or one-fifth dose to induce and maintain protective immunity. J. Infect. Dis. 221, 1922–1924 10.1093/infdis/jiz379 [DOI] [PubMed] [Google Scholar]
- 71.Kareko B.W., Booty B.L., Nix C.D., Lyski Z.L., Slifka M.K., Amanna I.J. et al. (2020) Persistence of neutralizing antibody responses Among yellow fever virus 17D vaccinees living in a nonendemic setting. J. Infect. Dis. 221, 2018–2025 10.1093/infdis/jiz374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.World Health Organisation. (2017) WHO position on the use of fractional doses — June 2017, addendum to vaccines and vaccination against yellow fever WHO: Position paper — June 2013. Vaccine 35, 5751–5752 10.1016/j.vaccine.2017.06.087 [DOI] [PubMed] [Google Scholar]
- 73.Wu J.T., Peak C.M., Leung G.M. and Lipsitch M. (2016) Fractional dosing of yellow fever vaccine to extend supply: a modelling study. Lancet 388, 2904–2911 10.1016/S0140-6736(16)31838-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.de Menezes Martins R., Maia M.L.S., de Lima S.M.B., de Noronha T.G., Xavier J.R., Camacho L.A.B. et al. (2018) Duration of post-vaccination immunity to yellow fever in volunteers eight years after a dose-response study. Vaccine 36, 4112–4117 10.1016/j.vaccine.2018.05.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Epidemiológico B. (2019) Monitoramento dos Casos de Arboviroses Urbanas Transmitidas Pelo Aedes (Dengue, Chikungunya E Zika) Até a Semana Epidemiológica 12 de 2019 E Levantamento Rápido dE Índices para Aedes Aegypti (LIRAa), Secretaria de Vigilância em Saúde Ministério da Saúde [Google Scholar]
- 76.Yellow Fever Reported by WHO region [Internet]. WHO. 2019. [cited September 18, 2020]. Available from: https://apps.who.int/gho/data/view.main.1520_50?lang=en
- 77.Kumar S., Stecher G. and Tamura K. (2016) MEGA7: molecular evolutionary genetics analysis version 7.0 for bigger datasets. Mol. Biol. Evol. 33, 1870–1874 10.1093/molbev/msw054 [DOI] [PMC free article] [PubMed] [Google Scholar]