Abstract
Background
The safety of surgery during and after the coronavirus disease-2019 (COVID-19) pandemic is paramount. Early reports of excessive perioperative mortality in COVID-positive patients promoted the widespread avoidance of operations. However, cancelling or delaying operations for cancer, trauma, or functional restitution has resulted in increased morbidity and mortality.
Methods
A national multicentre cohort study of all major reconstructive operations carried out over a 12-week period of the ‘COVID-19 surge’ in the United Kingdom and Ireland was performed. Primary outcome was 30-day mortality and secondary outcome measures were major complications (Clavien-Dindo grade ≥3) and COVID-19 status of patients and healthcare professionals before and after surgery.
Results
A total of 418 patients underwent major reconstructive surgery with a mean operating time of 7.5 hours and 12 days’ inpatient stay. Cancer (59.8%) and trauma (29.4%) were the most common indications. COVID-19 infection was present in 4.5% of patients. The 30-day post-operative mortality was 0.2%, reflecting the death of one patient who was COVID-negative. Overall complication rate was 20.8%. COVID status did not correlate with major or minor complications. Eight healthcare professionals developed post-operative COVID-19 infection, seven of which occurred within the first three weeks.
Conclusions
Major reconstructive operations performed during the COVID-19 crisis have been mostly urgent cases involving all surgical specialties. This cohort is a surrogate for all major operations across all surgical specialties. Patient safety and surgical outcomes have been the same as in the pre-COVID era. With adequate precautions, major reconstructive surgery is safe for patients and staff. This study helps counsel patients of COVID-19 risks in the perioperative period.
Keywords: COVID-19, Reconstructive surgery, Major surgery, Free flap, Pedicled flap, Revascularisation, Safety, Mortality
Introduction
Since the World Health Organisation officially declared coronavirus disease-2019 (COVID-19) a pandemic on 11 March 2020, healthcare systems and societies have been significantly disrupted.1 , 2 Globally, it is estimated that over 28 million (72.3%) planned operative procedures have been cancelled during the 12-week peak of the pandemic, which affected all main surgical specialties.3
In the UK and Ireland, a national directive was passed throughout the National Health Service (NHS) on March 17 to cancel all non-urgent elective operations for a period of at least three months.4 This was primarily intended to free up hospital beds and enable operating theatres and surgical staff to be re-deployed for treating COVID-19 patients.4 , 5 However, a significant side effect of this has been to deprive patients of life-changing operations,6 causing them increased pain, morbidity and mortality-risk,7 with restricted function and reduced quality of life.8 This will have a longer-term adverse impact for both individual patients and society as a whole.8, 9, 10
Recent reports of high mortality and complication rates associated with operating on COVID-positive patients11 , 12 have reinforced this national response to cancel or delay operations. Prior to the COVID-19 pandemic, 4.2 million patients were on waiting lists for NHS treatment. This has already increased significantly over the last three months9 and is expected to reach 10 million patients by the end of 2020.
This national collaborative study recruited consecutive data from all registered reconstructive surgical centres in the UK and Ireland during the peak months of the COVID-19 pandemic, to analyse the safety and efficacy of major reconstructive operations. These operations are typically undertaken with other surgical specialties and are lengthy with a prolonged inpatient stay. The aim was to establish whether it was safe to recommence surgical practice. This would provide guidance for surgeons to better counsel their patients within the UK and Ireland as compared to previously published work.11 , 12
Methods
Design
A national multicentre cohort study of all major reconstructive operations carried out in the UK and Ireland over a 12-week period, from 1 March 2020 to 23 May 2020, was performed.
Major reconstructive operations were defined as microsurgical tissue transfer, major pedicled flaps, replantations, and major limb revascularisations performed for elective, cancer or emergency indications, in both adults and children. Minor reconstructive or other surgical procedures were excluded.
The study was registered and approved as a clinical audit at the lead centre – University Hospitals of Leicester NHS Trust with registration number 10,596 – with Caldicott guardians’ approval. Confirmation was obtained from a local scientific committee that ethical approval was not required.
Data collection
Consultant reconstructive surgeons were contacted and allocated as principal collaborators in all 70 major reconstructive surgical centres within the UK and Ireland (Figs. 1 and 2 ). This included all centres listed within the British Association of Plastic and Reconstructive Surgeons (BAPRAS) directory13 as well as centres performing major reconstructive oral and maxillo-facial surgery. Collaborators were provided with written guidance and remote support throughout the study period.
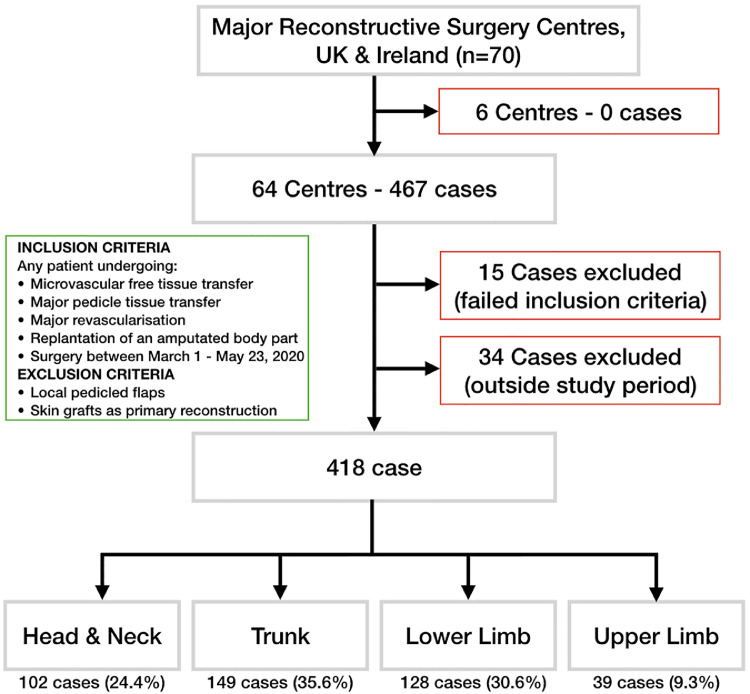
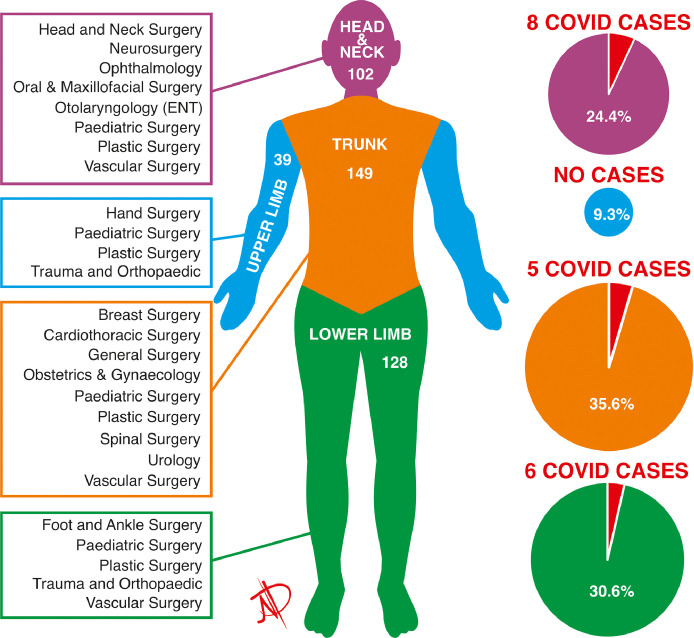
Fig. 1.
Study design.
Major reconstructive surgery centres and surgical cases included, according to pre-defined inclusion and exclusion criteria. Surgical case mix by anatomical region.
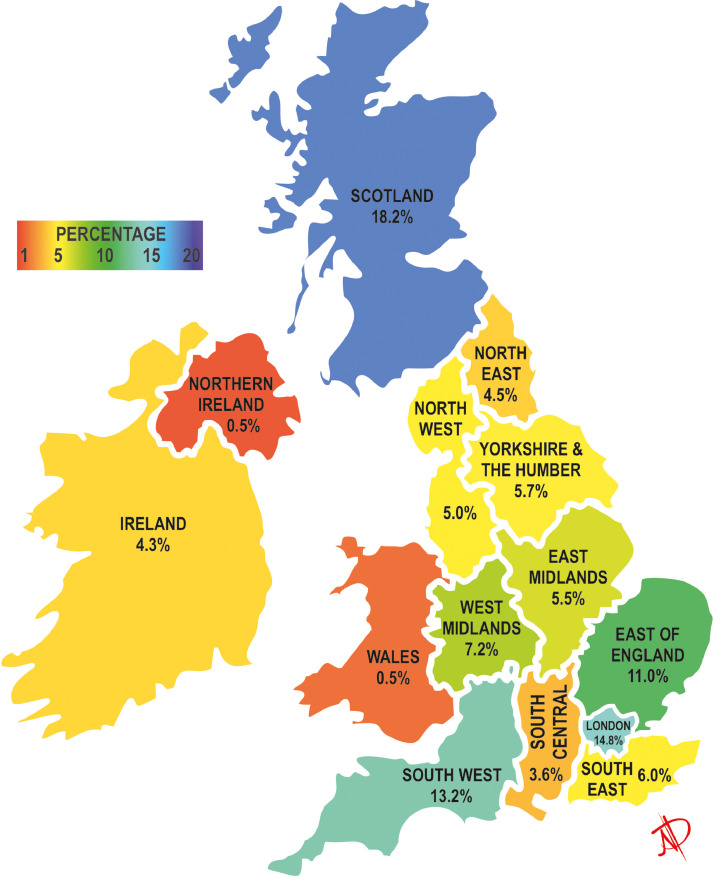
Fig. 2.
Geographical distribution of patients undergoing major reconstructive operations.
Major reconstructive surgical caseload as a percentage of the total 418 cases performed, by geographical region in the UK and Ireland.
A specifically designed proforma was developed and securely distributed to collect only pertinent, routine, anonymised data with no change to clinical care pathways (Appendix 3). This was completed and returned for each consecutive case that met inclusion criteria.
Before locking the dataset for analysis, the local principal collaborator for each hospital was asked to confirm data completeness, including 30-day follow-up, and that all eligible patients had been entered into the database.
Patients and healthcare professionals
Demographic variables recorded for patients included age, gender, ethnicity, comorbidities, smoking status, and American Society of Anesthesiologists (ASA) physical status classification I-V.14
Operative variables included diagnosis, operation, type of flap/replantation, reconstructed body part, and date. The priority level of surgery was classified according to the NHS England speciality-specific surgical priority levels15 on the basis of recommended time intervals from presentation to surgical treatment. Duration of the operating theatre episode (arrival of the patient in the anaesthetic room until leaving theatre) was also recorded, including total surgical time (knife-to-skin to last suture) and total non-surgical time (pre- and post-surgery).
Variables regarding the intraoperative use of personal protective equipment (PPE) and perioperative COVID-19 status were also collected. This included whether patients or healthcare professionals were clinically suspected of having COVID-19 before or within 2 weeks after surgery, and if they were tested for COVID-19 by swab test, chest x-ray or CT scan.
Outcomes
The primary outcome was all-cause 30-day post-operative mortality for all cases included in the study, with the day of surgery defined as day 0.
The key secondary outcome measures were major complications (Clavien-Dindo grade ≥3),16 and COVID-19 status before and after surgery for both patients and healthcare professionals. Additional secondary outcomes included minor post-operative complications (Clavien-Dindo grade ≤ 2), return to theatre and length of inpatient stay. Trends in the number of operations were also mapped against time and the national incidence of COVID-related deaths,18 throughout the 12-week study period (Fig. 3 ).
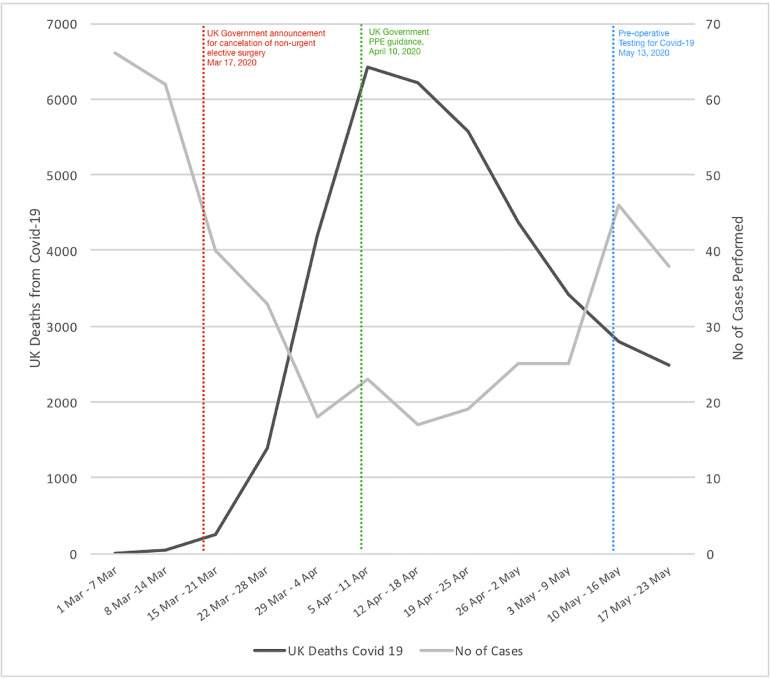
Fig. 3.
Major reconstructive surgery case numbers over time.
Number of major reconstructive surgeries performed over the 12-week study period (grey), alongside the national incidence of deaths associated with COVID-19 (black) and key time points regarding national policy changes in the UK and Ireland (red, green and blue).
In view of the national variations of perioperative testing during the study period,17 patients and healthcare professionals with symptoms of COVID-19 prior to the introduction of routine antigen swab testing in each centre were diagnosed based on clinical symptoms. After the introduction of testing in each centre, patients were diagnosed primarily based on results of their swab tests. However, if a patient had classical symptoms of COVID-19 either pre- or post-operatively but had a negative test result, they were also identified as COVID-positive, to account for the high false-negative rate of swab tests in use at the time.17
Statistical analysis
Data were interrogated according to STROBE guidelines for observational studies.18 Analysis was conducted using Statistical Product and Service Solutions (SPSS), IBM Corp, for Windows version 21•0, (SPSS Inc., Armonk, NY, USA).
Continuous data were tested for distribution. Non-normally distributed data were tested using the Mann-Whitney U test. The χ2 and Fisher's exact tests were used for categorical data. The cut-off for theatre time and length of stay was defined based on the receiver-operating characteristic (ROC) analysis. Relative risk (RR) and 95% confidence intervals (CI) were generated using the Stata for Windows version 15. P value <0.05 (two-sided) was considered statistically significant. Missing data were included in flowcharts and descriptive analyses, allowing denominators to remain consistent in calculations.
Results
Response rate from the 70 centres performing major reconstructive surgery in the UK and Ireland was 100% (Fig. 1). Six centres did not perform any major reconstructive operations during the study period. The remaining 64 centres submitted a total of 467 cases, of which 418 cases met the inclusion criteria for the study. By the date of final analysis (28 June 2020) 30-day follow-up data were available for all 418 patients.
Number of major reconstructive operations performed
Case numbers varied between the different geographical regions of the UK and Ireland (Fig. 2), with the largest number performed in Scotland (76/418 [18.2%]), followed by London, England (62/418 [14.8%]) and South West England (55/418 [13.2%]).
Case numbers also varied during the 12-week study period (Fig. 3). Initially, there was a sizeable decrease in the frequency of major reconstructive cases, which was most marked during the period from 1 March to 4 April 2020. Numbers remained low throughout the month of April and then increased again towards 40 cases per week by the end of May.
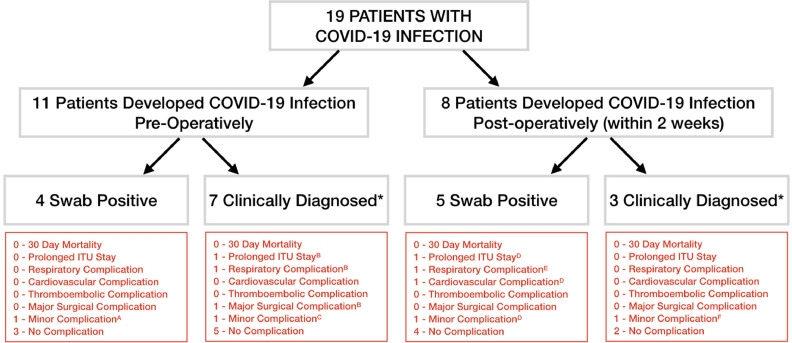
COVID-positive patients
Nineteen (4.5% [19/418]) patients were COVID-positive perioperatively (Fig. 4 ). Eleven (2.6% [11/418]) were diagnosed pre-operatively (four positive swab tests and seven clinically diagnosed). Surgery was deferred for a minimum of ten days in these patients, following which two minor and one major (flap failure) post-operative complications occurred. A further eight (2.0%) patients were diagnosed with COVID-19 post-operatively (five positive swab tests and three clinically diagnosed). Of these, two patients developed complications, one major (prolonged ITU stay) and one minor (seroma collection). No 30-day post-operative mortality occurred in association with COVID-19.
Fig. 4.
Patients diagnosed with COVID-19 perioperatively.
* Clinically diagnosed prior to established swab testing protocols. A,B,C,D,E,F Each letter refers to a single patient in the above descriptors for complication.
Comparisons between COVID-positive and COVID-negative patients
There was no significant gender difference in COVID status (p = 0.152) between male (219 [52.4%]) and female patients (199 [47.6%]) (Table 1 ). Mean age of the entire patient population was 51.6 years (range: 10–92 years), with COVID-positive patients having a significantly higher mean age of 63.4 years (range: 20–92 years and p = 0.005) than that of COVID-negative patients (mean 50.9 years and p = 0.005). The majority of patients (377 [90.2%]) were of white ethnic background and all COVID-positive patients were within this group.
Table 1.
Demographic data for all patients included in the study, in relation to their COVID-status perioperatively. p<0.05 (bold) denotes statistical significance.
| Study Characteristics | All Patients | COVID-positive | COVID-negative | p-value |
|---|---|---|---|---|
| 418 | 19(4.5) | 399(95.5) | ||
| Age (Years) | ||||
| Mean | 51.6 | 63.37 | 50.87 | 0.005 |
| Median | 54 | 71 | 54 | |
| Gender | ||||
| Male | 219(52.4) | 6(31.6) | 193(48.4) | 0.152 |
| Female | 199(47.6) | 13(68.4) | 206(51.6) | |
| Comorbidities | ||||
| Hypertension | 91(21.8) | 11(57.9) | 80(20.1) | 0.000 |
| Diabetic | 43(10.3) | 3(15.8) | 40(10) | 0.419 |
| COPD/Asthma | 43(10.3) | 6(31.6) | 37(9.3) | 0.008 |
| Chronic Kidney disease | 14(3.3) | 2(10.5) | 12(3) | 0.129 |
| Cardiovascular disorder | 40(9.6) | 5(26.3) | 35(8.8) | 0.026 |
| Cerebrovascular disorder | 12(2.9) | 3(15.8) | 9(2.3) | 0.014 |
| Ethnicity | ||||
| White | 377(90.2) | 19(100) | 358(89.7) | 0.339 |
| Non-White | 30(7.2) | 0(0) | 30(7.5) | |
| Unknown | 11(2.6) | 0(0) | 11(2.8) | |
| ASA Grade | ||||
| I | 79(18.9) | 2(10.5) | 77(19.3) | 0.000 |
| II | 227(54.3) | 7(36.8) | 220(55.1) | |
| III | 99(23.7) | 6(31.6) | 93(23.3) | |
| IV | 13(3.1) | 4(21.1) | 9(2.3) | |
| Diagnosis | ||||
| Benign | 24(5.7) | 0(0) | 24(6) | 0.485 |
| Cancer | 250(59.8) | 12(63.2) | 238(59.6) | |
| Infection | 21(5) | 2(10.5) | 19(4.8) | |
| Trauma | 123(29.4) | 5(26.3) | 118(29.6) | |
| Reconstruction Type | ||||
| Free Flap | 247(59.1) | 8(42.1) | 239(59.9) | 0.065 |
| Pedicled Flap | 145(34.7) | 11(57.9) | 134(33.6) | |
| Replant/Major revascularisation | 26(6.2) | 0(0) | 26(6.5) | |
| Length of Stay (Number of days) | ||||
| Mean | 11.98 | 16.1 | 11.79 | 0.031 |
| Median | 8 | 15 | 8 | |
| Theatre Time (min) | ||||
| Mean | 451.03 | 436.68 | 451.74 | 0.457 |
| Median | 450 | 400 | 450 | |
| Priority Level of Surgery | ||||
| 1a (within 24 h) | 28(6.7) | 0(0) | 28(7) | 0.236 |
| 1b (within 72 h) | 88(21.1) | 5(26.3) | 83(20.8) | |
| 2 (within 4 weeks) | 239(57.2) | 14(73.7) | 225(56.4) | |
| 3 (within 3 months) | 16(3.8) | 0(0) | 16(4) | |
| 4 (More than 3 months) | 47(11.2) | 0(0) | 47(11.8) | |
| Site of Surgery | ||||
| Head and neck cutaneous | 43(10.3) | 3(15.8) | 40(10) | 0.284 |
| Head and neck mucosal | 59(14.1) | 5(26.3) | 54(13.5) | |
| Lower limb | 128(30.6) | 6(31.6) | 122(30.6) | |
| Trunk | 149(35.6) | 5(26.3) | 144(36.1) | |
| Upper limb | 39(9.3) | 0(0) | 39(9.8) | |
| Mortality | ||||
| All-cause 30-day mortality rate | 1(0.2) | 0 | 1(0.3) | 0.955 |
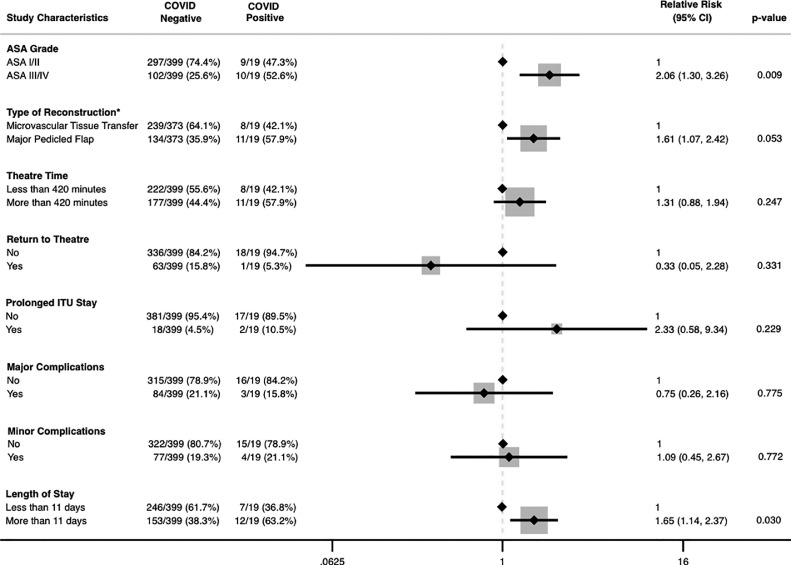
The most prevalent comorbidities amongst all patients were hypertension (21.8%), diabetes (10.3%), asthma/COPD (10.3%) and cardiovascular disorders (9.6%). COVID-positive patients had a significantly higher incidence of hypertension (p = 0.000), asthma/COPD (p = 0.008), cardiovascular disorders (p = 0.026) or cerebrovascular disease (p = 0.014) (Table 1). Most patients were ASA grade II (227 [54.3%]), and COVID-positive patients (10/19 [52.6%]) were more likely to have a higher ASA grade (III/IV) (RR: 2.06 [95% CI: 1.3–3.26], p = 0.009) than that of the COVID-negative group (102/399 [25.6%]) (Fig. 5 ).
Fig. 5.
Key patient, surgical and post-operative outcomes in relation to COVID-status.
Forest plot. Distribution of various study characteristics between COVID-positive and COVID-negative patients. Relative risk (RR) with 95% confidence intervals (CI). P-value <0.05 denotes statistical significance.
*Replantation cases (26 patients) were excluded from this analysis as no COVID-positive patients underwent replant operations.
The majority of patients underwent major surgery for cancer (250 [59.8%]) or trauma (123 [29.4%]) and the distribution of these categorical diagnoses was similar between COVID-positive and COVID-negative patients (p = 0.485) (Table 1). The majority of COVID-positive patients (63.2%) underwent cancer surgery. Sites of operations were heterogeneously distributed between head and neck (102 [24.4%]), trunk (149 [35.6%]), lower limb (128 [30.6%]) and upper limb (39 [9.3%]) with similar distribution between COVID-positive and COVID-negative patients (p = 0.284) (Figs. 1 and 6 ). Of these operations, 247 (59.1%) involved microsurgical tissue transfer, 145 (34.7%) involved major pedicled flap reconstruction and 26 (6.2%) were replantation or major revascularisation cases (Table 1). COVID-positive patients were more likely to undergo major pedicled flap reconstruction (RR: 1.61 [1.07–2.42] and p = 0.053).
Fig. 6.
Major reconstructive surgery case numbers according to anatomical site and surgical specialties involved in the patients’ care.
(A) Distribution of surgical case numbers according to anatomical site of the body. (B) Frequency of COVID-19-positive patients diagnosed perioperatively according to anatomical site of the body.
Overall, 85% of cases were priority level 1a, 1b or 2 according to the NHS England speciality-specific surgical priority levels.16 Of the 19 COVID-positive patients, 5 were priority level 1b (required surgery within 72 h) and 14 were priority level 2 (required surgery within 4 weeks).
All patients underwent major operations involving resection and/or reconstruction with a mean operating theatre duration of 7.5 h, with no significant difference between COVID-positive (mean 436.7 min) and COVID-negative patients (mean 451.7 min) (p = 0.457). However, COVID-positive patients had a significantly higher mean length of inpatient stay of 16.1 days than that of 11.8 days for COVID-negative patients (p = 0.031) (Fig. 5).
Post-operative complications of major reconstructive surgery
Of the 418 major reconstructive operations performed during this 12-week period, major complications (Clavien-Dindo classification ≥ 3) were observed in 87 (20.8%) patients. The incidence of major complications was 15.8% (3/19) in the COVID-positive group and 21.1% (84/399) in the COVID-negative group was (RR:0.75 [0.26–2.16] and p = 0.775). Of the 87 patients with major complications, 64 (15.3%) required return to theatre and 20 (4.8%) had a prolonged ITU stay. There was no significant difference in any of these parameters between the two groups (Fig. 5).
Minor complications (Clavien-Dindo grade ≤2) were noted in 81 (19.4%) cases, which were similarly distributed between the COVID-positive (4/19 [21.1%]) and COVID-negative patients (77/399 [19.3%]) (p = 0.772) (Fig. 5).
Mortality cases
The all-cause 30-day mortality rate was 0.2% (1/418). This accounted for a single patient who was COVID-negative throughout their treatment (Table 2 ). They were ASA grade IV, and underwent a 17.8 h neurosurgical resection involving craniectomy and reconstruction with microsurgical tissue transfer. On post-operative day 4, they had a cerebrovascular accident and died on day 7 post-operatively.
Table 2.
Key demographic and surgical factors related to mortality.
| Case 1 (7-day mortality) | Case 2 (31-day mortality) | |
|---|---|---|
| COVID-19 status | Swab test negative, no symptoms of COVID-19 | COVID-19 negative throughout initial hospital admission, including operation. Discharged home and later re-admitted, with subsequent COVID-positive swab test (day-10 post-operatively) |
| Age | >65 years old | >65 years old |
| ASA grade | IV | III |
| Urgency of surgery | NHS England priority level 2 | NHS England priority level 2 |
| Complexity of surgery | Neurosurgical resection, neck dissection and free flap reconstruction | Coronary artery bypass grafts complicated by sternal dehiscence and sternal osteomyelitis, requiring multiple repeat debridements and omental flap reconstruction through laparotomy |
| Surgical time | 17.8 h | 2.1 h |
| Post-operative complications | Clavien-Dindo grade 4 and 5 (stroke, respiratory failure requiring ventilation and death) | Clavien-Dindo grade 4 and 5 (COVID pneumonia, respiratory failure and death) |
| Death | Day 7 post-operatively | Day 31 post-operatively |
| Mortality rate | 0.2% 30-day mortality rate | 0.4% overall mortality rate |
Only one other death was reported, which occurred after the 30-day follow-up period. This occurred on post-operative day 31 in a patient who was ASA grade III and had undergone coronary artery bypass grafting complicated by sternal dehiscence, multiple surgical debridements and subsequent reconstruction with a pedicled omental flap. Following discharge from hospital, the patient was re-admitted and subsequently diagnosed with COVID-19 on post-operative day 10, before the patient 21 days later. The patient had multiple cardiac, respiratory and metabolic comorbidities (Table 2).
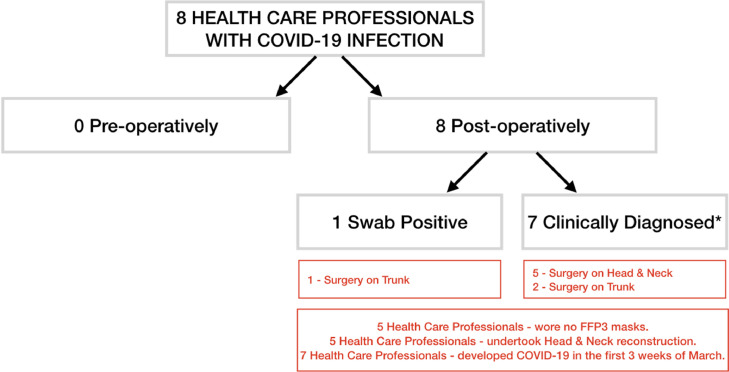
COVID-positive healthcare professionals
No healthcare professionals were known to be COVID-positive preoperatively. Eight healthcare professionals were diagnosed with COVID-19 within two weeks of treating eight separate patients (Fig. 7 ), giving a 1.9% infection rate for healthcare professionals. One was diagnosed with antigen swab test and seven were clinically diagnosed. Five of these were involved in potentially aerosol-generating procedures of the head and neck and four had not used their FFP3 (or equivalent) masque throughout the operation. Seven occurred within the first three weeks of March, prior to the introduction of PPE guidelines for healthcare professionals.
Fig. 7.
Healthcare professionals diagnosed with COVID-19 perioperatively.
* Clinically diagnosed prior to swab testing protocol.
Discussion
COVID-19 and associated national directives introduced during the pandemic have caused a significant reduction in surgical activity over this 12-week peak period throughout the UK and Ireland (Fig. 3). However, a sizeable cancer and trauma reconstructive caseload continued, providing a representative population in which to study the safety of major reconstructive surgery for consecutive patients.
The post-operative outcomes for patients nationally demonstrate the safety of major reconstructive surgery performed during the COVID-19 pandemic. These are comparable to published data from the pre-COVID era,19 , 20 including the UK national flap registry.21
Major reconstructive surgery has been performed to a high standard, despite the multiple challenges faced throughout the healthcare sector, both inside and outside the operating theatre. These included altered theatre environments, unfamiliar theatre teams, delayed start times, increased changeover times between cases, confusion regarding testing for patients and staff, evolving PPE requirements, and both communication and technical difficulties while wearing PPE in the theatre.
Furthermore, high-quality outcomes were maintained in this patient population with high incidence of factors known to be associated with increased morbidity and mortality,22 including urgency (85.0% priority levels 1a, 1b and 2), complexity (59.1% microsurgical tissue transfer), long duration (average duration 7.5 h), long inpatient stay (12 days), cancer (59.8%) or trauma (29.4%) diagnosis and raised ASA grade (81.1% ASA II-IV).
This is the first report of the all-cause 30-day mortality rate (0.2%) in a complete population in which the denominator is known. This stands in contrast to the 20.5%11 and 23.8%12 peri‑operative mortality risk published for COVID-positive patients only, which may be less representative of the overall population undergoing surgery during the pandemic.23 The current studied population had a COVID-19 incidence of 4.5% (19/418), which reflects the general population incidence at the time (6.8%).24 As a result, our data report a lower risk prediction for all consecutive patients undergoing major reconstructive surgery during the COVID-19 pandemic. COVID-19 positive status was not associated with increased mortality or morbidity risk throughout the healthcare systems of the UK and Ireland.
The all-cause 30-day post-operative mortality rate was 0.2% (1/418), with an additional death occurring after 30-days post-operatively (0.4% overall mortality) (Table 2). Both deaths were the result of multiple patient and surgical factors, in patients for whom a high mortality risk would have been predicted independently of COVID-19. These mortality rates are comparable to in-hospital mortality reported in the UK national flap registry21 (overall mortality 0.5% (16/3486)) and reported figures from the pre-COVID era of 4% in-hospital mortality19 and 7.4% 30-day mortality20 for all surgical specialties.
Furthermore, our results support those published from a large series of major cancer operations performed in a single centre in India25 during the same time period. Although unable to report 30-day mortality, no post-operative deaths were reported from 494 operations, and the complication rate was not increased in their six COVID-positive patients.
In deciding whether or not to offer appropriate surgery for patients during the COVID-19 pandemic, the potential risk of operating must be set against the known risk of not operating. Worldwide, over 2 million (37.7%) cancer operations are estimated to have been cancelled or delayed due to the pandemic.3 A 6-month delay in cancer surgery provision is known to cost each patient 2.19 of the life years they should have gained,7 resulting in the population losing 59% of the resource-adjusted life years gained by hospital treatment of an equivalent number of COVID-19 patients.7 In the UK, 27.8% of excess mortality during the pandemic did not involve COVID-19 infection.26 Moreover, prior to the pandemic, trauma accounted for over £3.5 billion annual lost economic activity within the UK.27 Without timely reconstructive surgery, the socio-economic cost, functional and psychological impact of cancer, trauma, and congenital abnormalities will significantly increase throughout the population.
Conclusion
Complex major reconstructive operations have been performed and continue to be performed throughout the COVID-19 pandemic in the UK and Ireland. Patient safety and post-operative outcomes have been demonstrated to be equivalent to the pre-COVID era. These data may inform patient-based discussion and decision-making regarding undergoing surgery during the pandemic and beyond.
Competing interest
None.
Transparency declaration
The authorship group confirms that this manuscript is an honest, accurate, and transparent account of the study. No important areas have been omitted.
Patient and Public Involvement
Not appropriate.
Funding sources
None.
Acknowledgements
The study was conceived and coordinated by Venkat Ramakrishnan and Nakul Gamanlal Patel.
Data coordination by Afshin Mosahebi, Maniram Ragbir, Henk Giele, Venkat Ramakrishnan and Nakul Gamanlal Patel.
Writing by Dimitris Reissis, Henk Giele, Afshin Mosahebi and Andrew Hart.
Data analysis, including tables and forest plots by Manish Mair.
Data interpretation by Manish Mair, Dimitris Reissis, Venkat Ramakrishnan and Nakul Gamanlal Patel.
Figures drawn by Nakul Gamanlal Patel.
Data Collection: ReconSurg Collaborative (Appendix 1).
Data entry: Kishan Patel, Ahmed Ibrahim, Dimitris Reissis, Vivek Sharma and Lucie Wright.
Major Reconstructive Centres included (Appendix 2).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.bjps.2020.12.032.
Appendix. Supplementary materials
References
- 1.Sipido K.R., Antoñanzas F., Celis J., Degos L., Frackowiak R., Fuster V., Ganten D., Gay S., Hofstraat H., Holgate S.T., Krestin G. Overcoming fragmentation of health research in Europe: lessons from COVID-19. Lancet. 2020;395:1970–1971. doi: 10.1016/S0140-6736(20)31411-2. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (2020) Coronavirus (COVID-19). Updated country preparedness and response status for COVID-19 as of 9 June 2020. June 9, 2020. https://www.who.int/publications/i/item/updated-country-preparedness-and-response-status-for-covid-19-as-of-9-june-2020. Accessed: June 16, 2020.
- 3.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;12 doi: 10.1002/bjs.11746. 10-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NHS England and NHS improvement . I. March 17, 2020. mportant and urgent – next steps on NHS response to covid-19.https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf Accessed: June 8, 2020. [Google Scholar]
- 5.Diaz A., Sarac B.A., Schoenbrunner A.R., Janis J.E., Pawlik T.M. Elective surgery in the time of COVID-19. Am J Surg. 2020;219:900–902. doi: 10.1016/j.amjsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.RCS England. Recovery of surgical services. May 26, 2020. https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/. Accessed: June 8, 2020.
- 7.Sud A., Jones M., Broggio J., Loveday C., Torr B., Garrett A., Nicol D.L., Jhanji S., Boyce S.A., Gronthoud F., Ward P. Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol. 2020 doi: 10.1016/j.annonc.2020.05.009. Published online May 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Søreide K., Hallet J., Matthews J.B., Schnitzbauer A.A., Line P.D., Lai P.B., Otero J., Callegaro D., Warner S.G., Baxter N.N., Teh C.S. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020 doi: 10.1002/bjs.11670. published online April 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.NHS Confederation. Getting the NHS back on track planning for the next phase of Covid-19. June 9, 2020. https://www.nhsconfed.org/-/media/Confederation/Files/Publications/Documents/REPORT_NHS-Reset_Getting-NHS-back-on-track_FNL.pdf. Accessed: June 14, 2020.
- 10.BAPRAS Breast reconstruction working group. Restarting breast reconstruction services - immediate reconstruction. June 17, 2020. http://www.bapras.org.uk/docs/default-source/default-document-library/restarting-breast-recon-pathways.pdf?sfvrsn=2. Accessed: June 18, 2020.
- 11.Lei S., Jiang F., Su W., Chen C., Chen J., Mei W., Zhan L.Y., Jia Y., Zhang L., Liu D., Xia Z.Y. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020 Apr 5 doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Surg COVID, Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)31182-X. published online May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.British Association of Plastic and Reconstructive Surgeons. Find a Unit. http://www.bapras.org.uk/home/find-a-unit. Accessed: May 12, 2020.
- 14.American Society of Anesthesiologists. ASA physical status classification system. October 23, 2019. https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system. Accessed: June 18, 2020.
- 15.NHS England Clinical guide to surgical prioritisation during the coronavirus pandemic. April 11, 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0221-specialty-guide-surgical-prioritisation-v1.pdf. Accessed: May 12, 2020</bib>.
- 16.Dindo D., Demartines N., Clavien P.A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watson J., Whiting P.F., Brush J.E. Interpreting a covid-19 test result. BMJ. 2020;369 doi: 10.1136/bmj.m1808. m1808. [DOI] [PubMed] [Google Scholar]
- 18.von Elm E., Altman D.G., Egger M., Pocock S.J., G tzsche P.C., Vandenbroucke J.P. The Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 19.Pearse R.M., Moreno R.P., Bauer P., Pelosi P., Metnitz P., Spies C., Vallet B., Vincent J.L., Hoeft A., Rhodes A. Mortality after surgery in Europe: a 7 day cohort study. Lancet. 2012;380:1059–1065. doi: 10.1016/S0140-6736(12)61148-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hackett N.J., De Oliveira G.S., Jain U.K., Kim J.Y. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg. 2015;18:184–190. doi: 10.1016/j.ijsu.2015.04.079. [DOI] [PubMed] [Google Scholar]
- 21.British Association of Plastic and Reconstructive Surgeons. UK National Flap Registry. https://rs2.e-dendrite.com/csp/bapras/frontpages/index.html. Accessed: June 28, 2020.
- 22.Pearse R.M., Harrison D.A., James P., Watson D., Hinds C., Rhodes A., Grounds R.M., Bennett E.D. Identification and characterisation of the high-risk surgical population in the United Kingdom. Crit. Care. 2006;10:1–6. doi: 10.1186/cc4928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tuech J.J., Schwarz L. Can we operate our patients without fear during the period of COVID-19 infection? EClinicalMedicine. 2020 doi: 10.1016/j.eclinm.2020.100382. May 17, 100382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Office for National Statistics (ONS). Coronavirus (COVID-19) infection survey pilot. 28 May 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveypilot/28may2020. Accessed: June 6, 2020.
- 25.Shrikhande S.V., Pai P.S., Bhandare M.S., Bakshi G., Chaukar D.A., Chaturvedi P., Goel M., Gulia A., Qureshi S.S., Maheshwari A., Moiyadi A. Outcomes of elective major cancer surgery during COVID 19 at Tata memorial centre: implications for cancer care policy. Ann Surg. 2020 doi: 10.1097/SLA.0000000000004116. published online June 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Office for National Statistics (ONS) Analysis of death registrations not involving coronavirus (COVID-19) England and Wales. 2020 28 December 2019 to 1 May 2020. June 5, 2020 https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/analysisofdeathregistrationsnotinvolvingcoronaviruscovid19englandandwales28december2019to1may2020/technicalannex. Accessed June 18. [Google Scholar]
- 27.NHS Confederation. Implementing trauma systems: key issues for the NHS. August 11, 2010. https://www.nhsconfed.org/∼/media/Confederation/Files/Publications/Documents/Implementing_trauma_systems_report.pdf. Accessed: June 28, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.