ABSTRACT
Vaccination is recommended for healthcare professionals (HCPs) to protect them against vaccine-preventable diseases (VPDs); however, uptake rates are low. This study aimed to evaluate HCPs’ influenza, hepatitis B, and measles vaccine uptake in all healthcare levels in Crete, Greece. We conducted a questionnaire–based, cross-sectional multicenter study in 2018, including HCPs employed at 18 primary care centers and 3 hospitals. Overall, 2,246 HCPs responded (57.2% of the target population). The influenza vaccine uptake rate was 36.1% (810/2,246), with the annual vaccination rate at 14.8% (332/2,246) over the previous 5 years. Concurrently, the hepatitis B 3-dose vaccine uptake rate was 60.3% (1,316/2,181). Among the participating HCPs, 70.7% (1,457/2,061) had measles immunity due to previous illness (959/2,061, 46.5%), a 2-dose vaccination scheme (461/2,061, 22.4%), or serological confirmation (37/2,061, 1.8%). Vaccine uptake rates differed between groups depending on age, profession, and workplace setting. Logistic regression analysis revealed that risk factors for no influenza vaccine uptake during the previous season were younger age (≤45 years; odds ratio [OR] 1.35, 95% confidence interval [CI]: 1.08–1.66), profession other than physician (OR 2.94, 95%CI: 2.09–4.12), and working in hospitals (OR 1.39, 95%CI 1.02–1.89). Older age (>45 years) was an independent risk factor for not receiving a measles (OR 26.74, 95%CI: 17.41–41.06) or hepatitis B vaccine (OR 1.36, 95%CI 1.09–1.7). Working in primary care was an independent risk factor for not getting a hepatitis B vaccine (OR 1.52, 95%CI: 1.15–2.1). Our findings indicate that individualized and targeted interventions should be implemented to increase vaccine uptake among HCPs.
KEYWORDS: Influenza, measles, hepatitis B, vaccine-preventable diseases, healthcare professionals, vaccination uptake
Introduction
Vaccine-preventable diseases (VPDs) are a significant cause of morbidity and mortality.1 Transmission of VPDs remains a challenge in healthcare settings despite immunization programs.2 Efforts to eliminate healthcare-acquired infections are important for patients’ safety and infection control.1
Vaccination of healthcare professionals (HCPs) is one of the most successful preventive tools for VPD control.3 Evidence from the recent measles epidemic in Europe as well as other VPD outbreaks reported in hospital settings has shown that non-immune HCPs can facilitate disease spread and, in some cases, serve as the primary source of infection.2–5 HCPs are at high risk of VPD exposure,3 and might transmit VPDs to patients who have contraindications to vaccinations or for whom vaccinations are less effective (e.g., infants, patients who are immunocompromised, and older adults).3,6–8 Vaccination of HCPs against influenza is essential for their own and their patients’ safety, as well as to prevent hospital-based disease outbreaks.9,10 Other than influenza, HCPs are susceptible to hepatitis B, which is the most efficiently transmissible blood-borne infection,11 and measles, which is a highly transmissible disease with documented HCP involvement as index cases and causes of transmission.4,12
Public health authorities strongly recommend and, in some cases, mandate vaccinations for HCPs.7 In Greece, such vaccinations are not mandatory but strongly recommended as part of the national vaccination program.7,13 Over the last 3 years, additional measures have been introduced to promote influenza and measles vaccine uptake among HCPs, including the establishment of a national steering committee for influenza and the issuance of new detailed guidelines for measles vaccination and immune status assessment.13,14
Despite these recommendations, suboptimal compliance and low vaccination rates among HCPs remain a problem in many countries.5,14–19 The World Health Organization working group on vaccine hesitancy considers evaluation of vaccine uptake as essential to detecting the extent of the problem and designing interventions tailored to the needs of local communities.15 To address the low rate of vaccine uptake among HCPs in Crete, Greece, we conducted a large cross-sectional multicenter survey with HCPs from 18 primary care centers and 3 hospitals, focusing on influenza, hepatitis B, and measles. We evaluated differences in vaccination uptake rates among HCPs and identified predictors of no-vaccine uptake among them.
Materials and methods
A cross-sectional multicenter study was conducted during March-September 2018 and included HCPs employed at 18 primary care centers and 3 hospitals (hospital A: Rethymnon General Hospital, hospital B: Heraklion University Hospital and hospital C: General Hospital of Chania) in Crete, the largest island of Greece. Although all of Crete’s 23 primary care centers and 5 hospitals were invited to participate, the present study included only the facilities that responded to our invitation. Among them, hospital A was a secondary hospital with 220 beds; hospital C was a secondary hospital with 430 beds; hospital B was a referral tertiary teaching hospital, the largest on the island, with 760 beds. Ethical approval was obtained from the Ethics Committee of the 7th Health Municipality of Greece.
For the purpose of this study, an anonymous questionnaire was developed, which included the following items: a) measles (history of previous illness, 2-dose vaccination, 1-dose vaccination, no vaccination, unknown status), b1) hepatitis B (history of previous illness, 3-dose vaccination, <3-dose vaccination, no vaccination, carrier status, unknown status), b2) hepatitis B serology (known/unknown status; if known, protective or not based on the threshold of anti-HBs 10 IU/ml), and c) influenza vaccination (vaccine uptake in the previous year, and vaccine uptake during the last 5 years: always, occasionally or never).
Prior to its distribution, the questionnaire underwent preliminary pilot testing and validity evaluation by the study authors. Subsequently, the 7th Health Municipality invited the healthcare facilities to distribute the questionnaire among their HCPs. A reminder was sent to the healthcare facilities that did not respond to the first notice. In the case of the General Hospital of Rethymnon, the questionnaire data were withdrawn anonymously by the existing updated hospital’s HCP vaccination registry. During the study period, no vaccination campaigns were conducted within primary care centers or hospitals except for the routine processes that take place annually, organized by public health authorities. These processes include vaccination recommendations made to HCPs as part of the national vaccination program,13 distribution of influenza vaccination posters, and educational activities alongside regular vaccination reminders sent to healthcare facilities. Furthermore, new national recommendations regarding measles vaccination among HCPs, issued in 2017, were distributed to all facilities, stating that all HCPs without demonstrable evidence of measles immunity should receive two doses of the measles, mumps and rubella (MMR) vaccine. Additional systematic interventions were delivered in hospital A, where a vaccination registry had been created and sent regular reminders and made recommendations regarding VPD to encourage annual influenza vaccination among all employees. All HCPs that refused vaccination were required to wear a face mask during the flu season.
The variables of interest included demographic characteristics, profession, workplace setting, flu vaccination status during the previous influenza season (2017–2018), flu vaccination status during the past 5 years (2013–18), vaccination/infection history against measles and hepatitis B, and self-reported immunity to these diseases.
The HCPs that were unvaccinated or received <3 doses of the hepatitis B vaccine were considered susceptible/nonimmune to hepatitis B. The HCPs that reported having had neither 2-dose scheme of measles/MMR vaccine nor a history of measles (or serologically proven immunity) were considered susceptible/non-immune to measles.
Quantitative variables (such as age in years) were reported as a median and range while categorical variables (such as sex, professional profile, working center, vaccination status, age group ≤45 years and >45) were reported as absolute and relative frequencies. The age cutoff was chosen based on the median age of all HCPs in our study, which was 47 years, rounded up to the nearest 5, yielding 45 years.
To assess the association between vaccination status and other variables of interest, a univariate analysis was performed using a chi-squared test. Determinants of vaccination uptake were further assessed by multivariate logistic regression using the MedCalc 19.1.3 software (MedCalc Software Ltd, Belgium). The results were expressed as odds ratio (ORs) with 95% confidence intervals (95% CI). A p-value <0.05 was considered statistically significant. The participants that did not report their sex, age, or profession, or reported unknown vaccination and immunity status for a specific VPD were excluded from univariate and multivariate analyses.
Results
Participants’ characteristics
Out of 23 primary care centers and 5 hospitals on the island, 18 primary care facilities and 3 hospitals replied to the study invitation. From these facilities, 2,246 HCPs responded to the questionnaire (57.2% among all employed HCPs). Among the responders, 572/2,246 (25.5%) did not report their profession, 421/2,246 (18.7%) their sex, and 90/2,246 (4%) their age. Participants’ median age was 47 years (range 21–67), and 443/1825 (24.3%) participants were men. Among the responders, 313/1,674 (18.7%) participants were physicians, 880/1,674 (52.6%) were nurses, 236/1,674 (14.1%) were paramedics, and 245/1,674 (14.6%) belonged to other non-medical professional categories. Overall, 18.6% (418/2,246) of the HCPs were working in primary care centers and 20.4% (458/2,246), 36.6% (823/2,246), and 24.4% (547/2,246) in hospital A, B, and C respectively (Table 1).
Table 1.
Participants’ characteristics and vaccination status
| Sex | ||
| Males | 443/1,825 | (24.3%) |
| Age (years) | ||
| (median, range) | 47 (21–67) | |
| Age groups | ||
| ≤45 years | 914/2,156 | (42.4%) |
| >45 years | 1,242/2,156 | (57.6%) |
| Profession | ||
| Physician | 313/1,674 | (18.7%) |
| Nurse | 880/1,674 | (52.6%) |
| Paramedical | 236/1,674 | (14.1%) |
| Other | 245/1,674 | (14.6%) |
| Workplace | ||
| Primary Care Centers | 418/2,246 | (18.6%) |
| Hospital A | 458/2,246 | (20.4%) |
| Hospital B | 823/2,246 | (36.6%) |
| Hospital C | 547/2,246 | (24.4%) |
| Vaccine/Immune Status | ||
| Influenza | ||
| 2017-18 season | 810/2,246 | (36.1%) |
| Annually (last 5 years) | 332/2,246 | (14.8%) |
| Occasionally (last 5 years) | 732/2,246 | (32.6%) |
| No vaccination (last 5 years) | 1,182/2,246 | (52.6%) |
| Hepatitis B | ||
| 3 doses vaccine uptake | 1,316/2,181 | (60.3%) |
| 1 or 2 doses vaccine uptake | 232/2,181 | (10.6%) |
| No vaccine | 626/2,181 | (28.7%) |
| ΗΒsAg(+) | 7/2,181 | (0.3%) |
| Susceptible to hepatitis B | 858/2,181 | (39.3%) |
| Measles | ||
| History of illness | 959/2,061 | (46.5%) |
| Positive serology only | 37/2,061 | (1.8%). |
| 2 doses vaccine uptake* | 461/1,065 | (43.3%) |
| 1 dose vaccine uptake* | 62/1,065 | (5.8%) |
| No vaccine* | 542/1,065 | (50.9%) |
| Susceptible to measles | 604/2,061 | (29.3%) |
*Among HCPs without a history of illness or serologically proven immunity.
Influenza
Among the 2,246 participants, 810 (36.1%) had received the quadrivalent inactivated influenza vaccine during the 2017–2018 season, which was the only vaccine type available in Greece during that period. Only 332 HCPs (14.8%) reported that they had received either the trivalent or quadrivalent inactivated influenza vaccine annually every year in the preceding 5 years (2013–2018), while 732 (32.6%) reported having occasionally received these vaccines in the last 5 years (Figure 1a). Finally, 1,181 (52.6%) of HCPs reported not having been vaccinated against influenza during 2013–2018.
Figure 1.
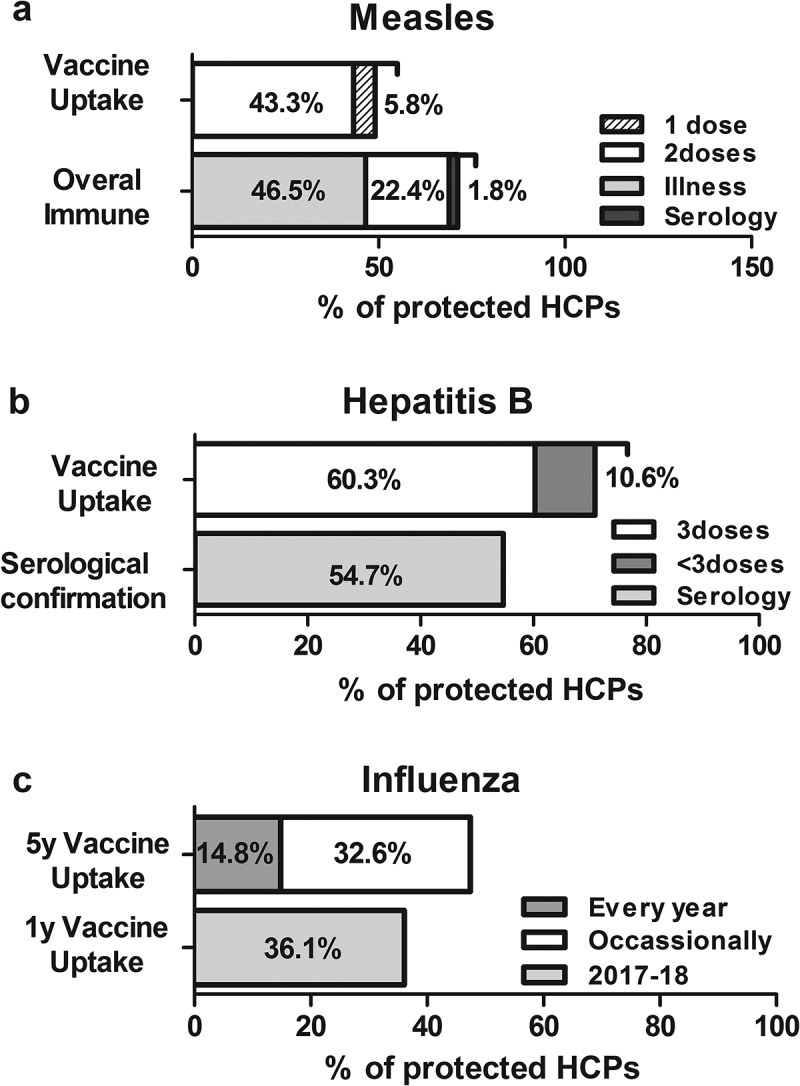
Vaccine uptake and overall protection against (a) influenza, (b) hepatitis B, and (c) measles among all healthcare professionals included in the present study
Hepatitis B
Among the 2,246 participants, 65 (2.9%) reported “unknown vaccination or immunity status” to hepatitis B and were excluded from analysis. Among the remaining participants, 1,316/2,181 (60.3%) reported having received at least 3 doses of the hepatitis B vaccine (Figure 1b), and 1,192/2,181 (54.7%) reported having evaluated their anti-HBs levels. Moreover, 7/2,181 HCPs (0.3%) reported being ΗΒsAg carriers. Overall, 39.3% (858/2,181) of HCPs were vulnerable to hepatitis B (Table 1).
Measles
Among all participants, 185/2,246 (8.2%) reported “unknown vaccination or immunity status” to measles and were excluded from analysis. Among the remaining HCPs, 959/2,061 (46.5%) reported history of measles, and 37/2,061 (1.8%) reported positive serology despite unknown history of illness. Among the remaining 1,065 participants, only 461 (43.3%) received 2 doses of the vaccine (Figure 1c). Overall, 29.3% (604/2,061) of HCPs were vulnerable to measles (Table 1).
Differences in coverage rates
HCPs were stratified based on sex, age (≤ 45 and >45 years), profession (physicians, nurses, paramedics, other), and workplace setting (either primary care centers or hospitals). Univariate analysis was performed to identify differences in coverage rates between these groups (Table 2), revealing higher influenza vaccine uptake among men (p < .0001), professionals >45 years-old (p < .0001), physicians (p < .001), HCPs working in primary care centers (p < .0001), and HCPs working in hospital A and C (p < .0001).
Table 2.
Vaccine uptake and overall protection for influenza, hepatitis B and measles in different categories of HCPs. Univariate analysis based on demographic and other characteristics of HCPs
| Influenza |
Hepatitis B |
Measles |
||||||
|---|---|---|---|---|---|---|---|---|
| 1-yearvaccine uptake | p value | 5-yearvaccine uptake | p value | 3 dosesvaccine uptake | p value | 2 dosesvaccine uptake* | p value | |
| Sex | ||||||||
| Males | 42.8% | 16.7% | 44.9% | 33.1% | ||||
| Females | 32.2% | p < .001 | 9.2% | p < .001 | 61.3% | p < .001 | 40.5% | p .04 |
| Age | ||||||||
| ≤45 years | 30.8% | 12.4% | 66.0% | 71.4% | ||||
| >45 years | 40.6% | p < .001 | 16.5% | p .011 | 59.0% | p .013 | 13.3% | p < .001 |
| Profession | ||||||||
| Physician | 55.6% | 23.5% | 46.1% | 40.6% | ||||
| Nurse | 29.1% | 8.2% | 74.5% | 45.8% | ||||
| Paramedical | 32.1% | 10.6% | 45.7% | 22.4% | ||||
| Other | 31.3% | ap < .001 | 6.2% | ap < .001 | 49.4% | ap < .001 | 25.5% | ap < .001 |
| Workplace | ||||||||
| Primary Care | 48.0% | 21.3% | 47.5% | 70.0% | ||||
| All hospitals | 33.1% | p < .001 | 13.2% | p < .001 | 63.1% | p < .001 | 39.4% | p < .001 |
| Hospital | ||||||||
| Hospital A | 44.5% | 28.6% | 69.1% | 83.3% | ||||
| Hospital B | 20.2% | 6.1% | 80.9% | 39.2% | ||||
| Hospital C | 47.1% | p < .001 | 11.3% | p < .001 | 32.0% | p < .001 | 27.4% | p < .001 |
*The percentage of nonimmune HCPs that received the vaccine (without any history of illness or positive serology). Chi square test was performed. For different professional categories two different analyses were conducted; either a) comparison among two groups: physicians compared to other professions or b) comparison among “physicians and nurses” and “paramedical and others” HCPs.
Concurrently, hepatitis B vaccine uptake was higher among women (p < .0001), professionals ≤45 years-old (p = .013), physicians and nurses (p < .0001), and HCPs working in hospitals (p < .0001), especially in hospital B (p < .0001).
Finally, measles vaccine uptake among HCPs without history of illness and/or negative anti-measles serology was higher among women (p = .04), professionals ≤45 years-old (p < .0001), physicians and nurses (p < .0001), and HCPs working in hospitals (p < .0001), in particular, hospital A (p < .0001). Older HCPs had higher rates of natural immunity, but the overall immunity to measles (vaccination, history of measles, or positive serology) was greater among younger HCPs [660/826, (79.9%) vs. 718/1,144 (62.7%), p < .0001].
Multivariate analysis of risk factors for inadequate vaccine uptake among HCPs
Multivariate logistic regression models were further performed, taking into consideration variables that differed significantly between groups in the univariate analysis. HCPs that had not received influenza vaccine during the previous influenza season, never received influenza vaccine during the last five years, never received any dose of hepatitis B vaccine and never received any dose of measles vaccine (among non -immune HCPs) were considered unvaccinated against influenza, hepatitis B and measles respectively). The dependent variables were either no influenza vaccine uptake in the previous and in the last five years or no hepatitis B or no measles vaccine uptake. Independent variables were age (≤45 and >45 years), profession (physicians, nurses, paramedics, other), and workplace setting (either primary care centers or hospitals; and work in hospital A. B or C). Age, profession, and workplace setting had a significant impact on vaccination uptake (Table 3). Specifically, important risk factors for no influenza vaccine uptake during the 2017–2018 season were younger age (OR 1.35, 95% CI: 1.08–1.66), profession other than physician (OR 2.94, 95% CI: 2.09–4.12), and working in hospitals instead of primary care centers (OR 1.39, 95% CI: 1.02–1.89), in particular, hospital B (OR 3.56, 95% CI: 2.7–4.7). Similarly, important risk factors for never receiving influenza vaccine in the past 5 years were profession other than physician (OR 2.67, 95% CI: 1.94–3.67), and working in a hospital rather than primary care center (OR 1.84, 95% CI: 1.36–2.48), in particular, hospital B (OR 4.5, 95% CI: 3.45–6.03). Older age was an important risk factor for no vaccine uptake against measles or hepatitis B vaccine among the nonimmune HCPs (OR 26.74, 95% CI: 17.41–41.06 and OR 1.36, 95% CI: 1.09–1.70, respectively). Moreover, participants who had not received a vaccine against hepatitis B were more likely to have a profession other than physician or nurse (OR 1.75, 95% CI: 1.38–2.21). Finally, working in a primary care center was an independent risk factor of inadequate vaccine uptake against hepatitis B (OR 1.52, 95% CI: 1.15–2.1).
Table 3.
Risk factors for vaccine non – uptake among HCPs’ categories
| Vaccine non-uptake for* | Odds ratio (95% CI) | P |
|---|---|---|
| Influenza (2017–18 season) | ||
| Age ≤ 45 years | 1.35 (1.08–1.66) | 0.0071 |
| Non–physician only | 2.94 (2.09–4.12) | 0.0001 |
| Work in hospitals | 1.39 (1.02–1.89) | 0.035 |
| Work in hospital B | 3.56 (2.71–4.71) | 0.0001 |
| Influenza (last 5 years) | ||
| Non-physician only | 2.67 (1.94–3.67) | 0.0001 |
| Work in hospitals | 1.84 (1.36–2.48) | 0.0001 |
| Work in hospital B | 6.41 (4.92–8.51) | 0.0001 |
| Measles †‡ | ||
| Age >45 years | 26.74 (17.41–41.06) | 0.0001 |
| Work in hospitals | 59.16 (25.81–135.6) | 0.0001 |
| Hepatitis B‡ | ||
| Age >45 years | 1.36 (1.09-–1.70) | 0.0071 |
| Non–physician or nurse | 1.75 (1.38–2.21) | 0.0001 |
| Work in primary care | 1.52 (1.15-2.-1) | 0.0027 |
*The dependent variables (no vaccination against influenza for either season 2017–2018 or the last five years, no hepatitis B vaccine uptake or no measles vaccine uptake) were adjusted for sex, age (≤ 45 years old and >45 years old), profession (physicians, nurses, paramedics, other) and workplace (either primary care centers or hospitals).
‡ No vaccine uptake of measles and hepatitis b was evaluated versus any dose of vaccine uptake.
† Analysis of no measles vaccine uptake among the HCPs that reported to be nonimmune to measles.
Discussion
The present study has revealed low vaccine uptake rates among HCPs alongside a great proportion of HCPs susceptible to influenza, hepatitis B, and measles. The presently reported influenza vaccine uptake rates are far below the European target of 75%,20 despite recommendations and annual nationwide campaigns.10,21 In the absence of proof of vaccination for hepatitis B, a 3-dose vaccine series is recommended for all HCPs, as well as testing anti-HBs serology 1 to2 months after the 3rd dose.22 In the present study, one-third of the HCPs were susceptible to hepatitis B and only half of HCPs evaluated their anti-HBs levels, suggesting that poor compliance with recommendations is not limited to vaccinations. The observed susceptibility rates were consistent with previously reported data for Greece,16,18,19,23 but were lower than the rates reported elsewhere.3,24–27
High measles vaccination uptake (up to 95%) is required for herd immunity;28 nevertheless, HCPs who participated in our study, similar to their European counterparts,18,29 remain far from this target, despite updates to national guidelines on measles vaccination and immunity assessment by HCPs, released in 2017, during the measles epidemic.13
In the present study, in HCPs older than 45 years, immunity to measles was mainly due to previous history of measles. High rates of naturally acquired immunity have been reported previously in Greece; in fact, they are expected since the measles vaccine was introduced in 1978, while the 2-dose MMR schedule was implemented in 1989.30 Several measles outbreaks during the last 15 years in Greece have also contributed to HCPs’ exposure to the wild type virus.4 Nevertheless, despite these high rates of naturally acquired immunity, older HCPs had lower overall immunity than did younger HCPs due to low vaccination rates. Missed opportunities to be vaccinated during childhood might account for this age-related immunity gap, which has also been reported in other studies on HCPs’ vaccinations in Europe.7,24,31
The present study has identified likely determinants of no vaccine uptake by HCPs. Sex did not play a significant role in multivariate analysis. However, previously published evidence is inconclusive regarding the role of sex in vaccine uptake, as higher coverage rates have been observed among either sex.5,32 However, profession, age, and workplace setting were important determinants of HCPs’ vaccination coverage in the present study. Paramedics and participants in other professional categories were more likely to not receive vaccines; meanwhile, nurses were at a higher risk for not receiving the influenza vaccine. These findings are consistent with previous studies, which have reported higher vaccination rates among physicians compared to other HCP groups.5,33–35
Regarding age, HCPs ≤45 years-old were at higher risk of not being vaccinated against influenza; in contrast, older HCPs were at higher risk of not being vaccinated against measles and hepatitis B. These findings are consistent with the literature.16,18,36–39 Nevertheless, the described vaccination patterns might also be attributed to the Greek national vaccination guidelines, whereby influenza vaccination is recommended for people aged >60 years or people with chronic diseases; older HCPs are more likely to belong to either of these categories. Concurrently, older HCPs might have missed childhood vaccination programs for hepatitis B and measles.
There was substantial variability in vaccination uptake among healthcare facilities. Hospital-based HCPs received the influenza and measles vaccines less frequently; meanwhile, primary care canters-based HCPs were more susceptible to hepatitis B. These findings are consistent with previous studies, reporting higher rates of hepatitis B vaccination in HCPs working in surgical departments or HCPs with frequent direct contact with blood or other body secretions.5 The higher rates of influenza vaccination uptake observed in primary care-based HCPs are probably the result of decade-long continuous efforts by the Greek Ministry of Health to reform primary care services.40 In addition, a nationwide influenza vaccine campaign has been rolled out during the last decade, including communication with all primary healthcare centers and free influenza vaccine to all HCPs at their workplace.40
Considerable differences in vaccination uptake rates were noted among the staff of three included hospitals. For example, among all hospitals, hospital A had the highest while hospital B had the lowest influenza vaccination rates. This finding might be attributed to the fact that, in hospital A, additional interventions have been implemented locally; specifically, a vaccination registry has been launched, which sends regular reminders and makes specific recommendations regarding VPDs to susceptible HCPs. Moreover, wearing a face mask during the flu season, was required for the staff that refused influenza vaccination. Furthermore, hospital A was the smallest in the number of beds and personnel, while hospital B was the largest, based on these metrics. These factors might play a significant role in the effectiveness of pro- vaccination measures; other factors might have contributed to these substantial discrepancies and further research is required to identify them.
However, these findings indicated that each facility might need to develop and implement its own vaccination policies to increase the vaccination uptake among its employees. The United States Task Force on Community Preventive Services has recommended a combination of widespread community-based interventions to increase vaccine coverage in targeted populations.41 Further research is required to evaluate the role of these recommendations at different locations and investigate whether individualized interventions provide additional benefits over general measures targeted at specific HCP groups and healthcare facility types.
Our study has several limitations. The majority of data were self–reported, and vaccine uptake rates might have been over- or underestimated, in particular, among older participants who might be less likely to accurately recall their vaccination status. However, the use of self-reported questionnaire-based data is a broadly accepted method in studies assessing vaccine coverage of HCPs.42,43 In fact, self-reported vaccination status has been reported to correlate with actual vaccination status for influenza,42 as well as with hepatitis B and measles seroprevalence.43 Nevertheless, self-reporting of anti-HBs status might result in HCPs having assessed their anti-HBs levels >2 months post-vaccination. As vaccine-induced anti-HBs levels decrease over time, we cannot make any correlations among anti-HBs and hepatitis B immunity. A considerable portion of HCPs did not report their age, sex, or profession and were excluded from univariate and multivariate analyses. A major strength of the present study is that the questionnaire was distributed by an official health authority and included a large number of HCPs based at 21 different sites, including hospitals and primary care centers.
In conclusion, this study underscores that national recommendations do not suffice and more robust measures are required to increase vaccination uptake among HCPs. Vaccination uptake rates may well vary and specific, quite well defined groups of HCPs are more vulnerable. We suggest that different vaccines might require individualized approach to increase uptake based on age, profession, and working sites of the HCPs; different healthcare facilities might also require an individualized approach; since one size is unlikely to fit all.
Funding Statement
This work was supported by the Special Account for Research Funds of University of Crete (SARF UoC) [Grant No 4491].
References
- 1.Fernando SA, Gray TJ, Gottlieb T.. Healthcare-acquired infections: prevention strategies. Intern Med J. 2017;47:1341–51. [DOI] [PubMed] [Google Scholar]
- 2.Increased transmission and outbreaks of measles-European region, 2011. MMWR Morb Mortal Wkly Rep. Centers for Disease Control and Prevention. 2011;60:1605–10. [PubMed] [Google Scholar]
- 3.Maltezou HC, Poland GA. Immunization of health-care providers: necessity and public health policies. Healthcare (Basel). 2016;4(3):47. doi: 10.3390/healthcare4030047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Georgakopoulou T, Horefti E, Vernardaki A, Pogka V, Gkolfinopoulou K, Triantafyllou E, Tsiodras S, Theodoridou M, Mentis A, Panagiotopoulos T. Ongoing measles outbreak in Greece related to the recent European-wide epidemic. Epidemiol Infect. 2018;146(13):1692–98. doi: 10.1017/S0950268818002170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Genovese C, Picerno IAM, Trimarchi G, Cannavo G, Egitto G, Cosenza B, Merlina V, Icardi G, Panatto D, Amicizia D, et al. Vaccination coverage in healthcare workers: a multicentre cross-sectional study in Italy. J Prev Med Hyg. 2019;60(1):E12–E17.doi: 10.15167/2421-4248/jpmh2019.60.1.1097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haviari S, Benet T, Saadatian-Elahi M, Andre P, Loulergue P, Vanhems P. Vaccination of healthcare workers: a review. Hum Vaccin Immunother. 2015;11(11):2522–37.doi: 10.1080/21645515.2015.1082014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maltezou HC, Poland GA. Vaccination policies for healthcare workers in Europe. Vaccine. 2014;32(38):4876–80.doi: 10.1016/j.vaccine.2013.10.046 [DOI] [PubMed] [Google Scholar]
- 8.Rapisarda V, Ledda C, Maltezou HC. Vaccination in healthcare workers: risk assessment, planning, strategy of intervention and legal implications. Future Microbiol. 2019;14(9s):1–3.doi: 10.2217/fmb-2018-0235 [DOI] [PubMed] [Google Scholar]
- 9.Paget J, Spreeuwenberg P, Charu V, Taylor RJ, Iuliano AD, Bresee J, Simonsen L, Viboud C. Global mortality associated with seasonal influenza epidemics: new burden estimates and predictors from the GLaMOR project. J Glob Health. 2019;9(2):020421.doi: 10.7189/jogh.09.020421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strategies to achieve the healthy people . 2020 annual influenza vaccine coverage goal for health-care personnel: recommendations from the national vaccine advisory committee. Public Health Rep. 2013;128:7–25.doi: 10.1177/003335491312800103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewis JD, Enfield KB, Sifri CD. Hepatitis B in healthcare workers: transmission events and guidance for management. World J Hepatol. 2015;7(3):488–97.doi: 10.4254/wjh.v7.i3.488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hiller U, Mankertz A, Köneke N, Wicker S. Hospital outbreak of measles - evaluation and costs of 10 occupational cases among healthcare worker in Germany, February to March 2017. Vaccine. 2019;37(14):1905–09.doi: 10.1016/j.vaccine.2019.02.068 [DOI] [PubMed] [Google Scholar]
- 13.Maltezou HC, Botelho-Nevers E, Brantsæter AB, Carlsson RM, Heininger U, Hübschen JM, Josefsdottir KS, Kassianos G, Kyncl J, Ledda C, et al. Vaccination of healthcare personnel in Europe: update to current policies. Vaccine. 2019;37(52):7576–84.doi: 10.1016/j.vaccine.2019.09.061 [DOI] [PubMed] [Google Scholar]
- 14.Maltezou HC, Katerelos P, Protopappa K, Dounias G. Seasonal influenza vaccination in healthcare personnel in Greece: 3-year report. Future Microbiol. 2019;14(9s):55–58.doi: 10.2217/fmb-2018-0266 [DOI] [PubMed] [Google Scholar]
- 15.Lane S, MacDonald NE, Marti M, Dumolard L. Vaccine hesitancy around the globe: analysis of three years of who/unicef joint reporting form data-2015-2017. Vaccine. 2018;36(26):3861–67.doi: 10.1016/j.vaccine.2018.03.063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karaivazoglou K, Triantos C, Lagadinou M, Bikas C, Michailidou M, Kalafateli M, Thomopoulos K, Assimakopoulos K, Nikolopoulou V, Jelastopulu E, et al. Acceptance of hepatitis b vaccination among health care workers in western Greece. Arch Environ Occup Health. 2014;69(2):107–11.doi: 10.1080/19338244.2012.750586 [DOI] [PubMed] [Google Scholar]
- 17.Toska A, Saridi M, Wozniak G, Souliotis K, Korovesis K, Apostolopoulou E. Influenza vaccination among nurses in Greece. Am J Infect Control. 2012;40(3):276–78.doi: 10.1016/j.ajic.2011.04.050 [DOI] [PubMed] [Google Scholar]
- 18.Maltezou HC, Katerelos P, Poufta S, Pavli A, Maragos A. Theodoridou M. Attitudes toward mandatory occupational vaccinations and vaccination coverage against vaccine-preventable diseases of health care workers in primary health care centres. Am J Infect Control. 2013;41(1):66–70.doi: 10.1016/j.ajic.2012.01.028 [DOI] [PubMed] [Google Scholar]
- 19.Maltezou HC, Gargalianos P, Nikolaidis P, Katerelos P, Tedoma N, Maltezos E, Lazanas M. Attitudes towards mandatory vaccination and vaccination coverage against vaccine-preventable diseases among health-care workers in tertiary-care hospitals. J Infect. 2012;64(3):319–24.doi: 10.1016/j.jinf.2011.12.004 [DOI] [PubMed] [Google Scholar]
- 20.Nicoll A. A new decade, a new seasonal influenza: the council of the European Union recommendation on seasonal influenza vaccination. Euro Surveill. 2010;15(1):19458.doi: 10.2807/ese.15.01.19458-en [DOI] [PubMed] [Google Scholar]
- 21.Wicker S, Marckmann G. Vaccination of health care workers against influenza: is it time to think about a mandatory policy in Europe? Vaccine. 2014;32(38):4844–48.doi: 10.1016/j.vaccine.2013.09.062 [DOI] [PubMed] [Google Scholar]
- 22.Schillie S, Murphy TV, Sawyer M, Ly K, Hughes E, Jiles R, de Perio MA, Reilly M, Byrd K, Ward JW. CDC guidance for evaluating health-care personnel for hepatitis b virus protection and for administering postexposure management. MMWR Recomm Rep. 2013;62:1–19. [PubMed] [Google Scholar]
- 23.Rachiotis G, Goritsas C, Alikakou V, Ferti A, Roumeliotou A. Vaccination against hepatitis b virus in workers of a general hospital in Athens. Med Lav. 2005;96:80–86. [PubMed] [Google Scholar]
- 24.Leung V, Harper S, Slavin M, Thursky K, Worth L. Are they protected? Immunity to vaccine-preventable diseases in healthcare workers at an Australian hospital. Aust N Z J Public Health. 2014;38(1):83–86.doi: 10.1111/1753-6405.12163 [DOI] [PubMed] [Google Scholar]
- 25.Dannetun E, Tegnell A, Torner A, Giesecke J. Coverage of hepatitis B vaccination in Swedish healthcare workers. J Hosp Infect. 2006;63(2):201–04.doi: 10.1016/j.jhin.2006.01.014 [DOI] [PubMed] [Google Scholar]
- 26.De Schryver A, Claesen B, Meheus A, van Sprundel M, Francois G. European survey of hepatitis b vaccination policies for healthcare workers. Eur J Public Health. 2011;21(3):338–43.doi: 10.1093/eurpub/ckq122 [DOI] [PubMed] [Google Scholar]
- 27.Yuan Q, Wang F, Zheng H, Zhang G, Miao N, Sun X, Woodring J, Chan PL, Cui F. Hepatitis B vaccination coverage among health care workers in China. PLoS One. 2019;14(5):e0216598.doi: 10.1371/journal.pone.0216598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Plans-Rubió P. Low percentages of measles vaccination coverage with two doses of vaccine and low herd immunity levels explain measles incidence and persistence of measles in the European Union in 2017-2018. Eur J Clin Microbiol Infect Dis. 2019;38(9):1719–29.doi: 10.1007/s10096-019-03604-0 [DOI] [PubMed] [Google Scholar]
- 29.Simone B, Carrillo-Santisteve P, Lopalco PL. Healthcare workers role in keeping MMR vaccination uptake high in Europe: a review of evidence. Euro Surveill. 2012;17:20206. [PubMed] [Google Scholar]
- 30.Gioula G, Exindari M, Melidou A, Minti F, Sidiropoulou E, Dionisopoulou S, Kiriazi M, Tsintarakis E, Malisiovas N. Seroprevalence of measles in Northern Greece. Acta Microbiologica Hellenica. 2017;62:145–50. [Google Scholar]
- 31.Lengyel G, Marossy A, Anosi N, Farkas SL, Kele B, Nemes-Nikodem E, Szentgyorgyi V, Kopcso I, Matyus M. Screening of more than 2000 Hungarian healthcare workers’ anti-measles antibody level: results and possible population-level consequences. Epidemiol Infect. 2019;147:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kahn KE, Black CL, Ding H, Williams WW, Lu PJ, Fiebelkorn AP, Havers F, D’Angelo DV, Ball S, Fink RV, et al. Influenza and Tdap vaccination coverage among pregnant women - United States, April 2018. MMWR Morb Mortal Wkly Rep. 2018;67(38):1055–59.doi: 10.15585/mmwr.mm6738a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Black CL, Yue X, Ball SW, Fink RV, de Perio MA, Laney AS, Williams WW, Graitcer SB, Fiebelkorn AP, Lu PJ, et al. Influenza vaccination coverage among health care personnel - United States, 2017-18 influenza season. MMWR Morb Mortal Wkly Rep. 2018;67(38):1050–54.doi: 10.15585/mmwr.mm6738a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bonaccorsi G, Lorini C, Santomauro F, Guarducci S, Pellegrino E, Puggelli F, Balli M, Bonanni P. Predictive factors associated with the acceptance of pandemic and seasonal influenza vaccination in health care workers and students in Tuscany, central Italy. Hum Vaccin Immunother. 2013;9:2603–12.doi: 10.4161/hv.26036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guthmann JP, Fonteneau L, Ciotti C, Bouvet E, Pellissier G, Levy-Bruhl D, Abiteboul D. Vaccination coverage of health care personnel working in health care facilities in France: results of a national survey, 2009. Vaccine. 2012;30(31):4648–54.doi: 10.1016/j.vaccine.2012.04.098 [DOI] [PubMed] [Google Scholar]
- 36.Haridi HK, Salman KA, Basaif EA, Al-Skaibi DK. Influenza vaccine uptake, determinants, motivators, and barriers of the vaccine receipt among healthcare workers in a tertiary care hospital in Saudi Arabia. J Hosp Infect. 2017;96(3):268–75.doi: 10.1016/j.jhin.2017.02.005 [DOI] [PubMed] [Google Scholar]
- 37.Alicino C, Iudici R, Barberis I, Paganino C, Cacciani R, Zacconi M, Battistini A, Bellina D, Di Bella AM, Talamini A, et al. Influenza vaccination among healthcare workers in Italy. Hum Vaccin Immunother. 2015;11(1):95–100.doi: 10.4161/hv.34362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Castilla J, Martinez-Baz I, Godoy P, Toledo D, Astray J, Garcia S, Mayoral JM, Martin V, Gonzalez-Candelas F, Guevara M, et al. Trends in influenza vaccine coverage among primary healthcare workers in Spain, 2008-2011. Prev Med. 2013;57(3):206–11.doi: 10.1016/j.ypmed.2013.05.021 [DOI] [PubMed] [Google Scholar]
- 39.Riphagen-Dalhuisen J, Gefenaite G, Hak E. Predictors of seasonal influenza vaccination among healthcare workers in hospitals: a descriptive meta-analysis. Occup Environ Med. 2012;69(4):230–35.doi: 10.1136/oemed-2011-100134 [DOI] [PubMed] [Google Scholar]
- 40.Dedoukou X, Nikolopoulos G, Maragos A, Giannoulidou S, Maltezou HC. Attitudes towards vaccination against seasonal influenza of health-care workers in primary health-care settings in Greece. Vaccine. 2010;28(37):5931–33.doi: 10.1016/j.vaccine.2010.06.108 [DOI] [PubMed] [Google Scholar]
- 41.Jacob V, Chattopadhyay SK, Hopkins DP, Murphy Morgan J, Pitan AA, Clymer JM. Community preventive services task force. Increasing coverage of appropriate vaccinations: a community guide systematic economic review. Am J Prev Med. 2016;50(6):797–808.doi: 10.1016/j.amepre.2015.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Llupia A, Garcia-Basteiro AL, Mena G, Rios J, Puig J, Bayas JM, Trilla A. Vaccination behaviour influences self-report of influenza vaccination status: a cross-sectional study among health care workers. PLoS One. 2012;7(7):e39496.doi: 10.1371/journal.pone.0039496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Trevisan A, Frasson C, Morandin M, Beggio M, Bruno A, Davanzo E, Di Marco L, Simioni L, Amato G. Immunity against infectious diseases predictive value of self-reported history of vaccination and disease. Infect Control Hosp Epidemiol. 2007;28(5):564–69.doi: 10.1086/516657 [DOI] [PubMed] [Google Scholar]


