Abstract
Corona virus disease 2019 (COVID-19) has caused a global outbreak and severely posed threat to people’s health and social stability. Mounting evidence suggests that immunopathological changes, including diminished lymphocytes and elevated cytokines, are important drivers of disease progression and death in coronavirus infections. Cytokine storm not only limits further spread of virus in the body but also induces secondary tissue damage through the secretion of large amounts of active mediators and inflammatory factors. It has been determined that cytokine storm is a major cause of deaths in COVID-19; therefore, in order to reverse the deterioration of severe and critically ill patients from this disease, the cytokine storm has become a key therapeutic target. Although specific mechanisms of the occurrences of cytokine storms in COVID-19 have not been fully illuminated, hyper-activated innate immune responses, and dysregulation of ACE2 (angiotensin converting enzyme 2) expression and its downstream pathways might provide possibilities. Tailored immunoregulatory therapies have been applied to counteract cytokine storms, such as inhibition of cytokines, corticosteroids, blood purification therapy, and mesenchymal stem cell therapy. This review will summarize advances in the research of cytokine storms induced by COVID-19, as well as potential intervention strategies to control cytokine storms.
Keywords: COVID-19, cytokine storm, ACE2, IL-6, immunoregulatory therapy
Introduction
Pathogenic human coronavirus infections, such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), could cause fatal lower respiratory tract infections and extra-pulmonary manifestations (1–3). The Coronavirus Disease 2019 (COVID-19), first reported in Wuhan, China, has raised acute and grave global concern since December 2019 (4, 5). On March 11, 2020, the world health organization (WHO) officially declared a global pandemic status for COVID-19, which is a great threat to people’s health and social stability. In the early stages of COVID-19, severe acute respiratory infection symptoms occurred, and some patients rapidly developed acute respiratory distress syndrome (ARDS), acute respiratory failure, and other serious complications (6, 7). There is considerable evidence to show that immunopathological changes, including diminished lymphocytes and elevated cytokines, are important drivers of disease progression and death of COVID-19 patients, especially those who are critically ill (8). Early detection and control of cytokine storms may effectively prevent disease progression and reduce the mortality rate. This review will summarize research progress on cytokine storms occurring in COVID-19 as well as potential intervention strategies.
Cytokine Storm and Cytokine Release Syndrome
The cytokine storm, previously reported in rheumatoid arthritis and graft-versus-host disease (GVHD), has been used to describe the overactive immune responses that can be triggered by a variety of factors, such as virus infection, autoimmune disease, and immunotherapies (8–10). Under the normal physiological state, the levels of pro-inflammatory cytokines and anti-inflammatory cytokines in the body are kept in relative balance, which can be broken by abnormal activation of a variety of immune cells (such as dendritic cells, macrophages, and lymphocytes) during viral infections. These abnormally activated immune cells could release large amounts of cytokines, among which the pro-inflammatory cytokines could promote more immune cells in a positive feedback loop. The formation of cytokine storm leads to “suicide attack” that not only contributes the elimination of pathogenic microorganisms but also causes tissue toxicities affecting a wide variety of organs (Table 1) (9). The cytokine release syndrome (CRS), a kind of systemic inflammation syndrome caused by cytokine storm, was previously observed in patients infected with SARS-CoV and MERS-CoV, as well as in leukemia patients receiving engineered T cell therapy (8, 9, 11, 12). Mild cases are characterized by fever, fatigue, headache, rash, arthralgia, and myalgia. Patients with more severe symptoms usually present with high fever, headache, fatigue, diffuse intravascular coagulation (DIC), shock, multiple organ failure (MOF), or even death (9, 11). Common laboratory abnormalities include cytopenia, elevated creatinine and liver enzymes, high levels of C-reactive protein (CRP), and deranged coagulation parameters (9, 11). Lee et al. reported a modified grading system for the severity of CRS regardless of the inciting agent, which defined mild, moderate, severe, life-threatening symptoms, and even death. This grading system is also used to guide clinical decisions in CRS (11). Vigilant supportive care is recommended for every grade; immunosuppression should be used in all patients with grade 3 or 4 CRS and instituted earlier in patients with extensive comorbidities or the elderly (11).
Table 1.
Clinical signs and laboratory findings about cytokine storms.
| Organ | Clinical signs and laboratory findings |
|---|---|
| Constitutional | Fever, rigors, headache, malaise, fatigue, anorexia, myalgias, nausea, vomiting |
| Pulmonary | Tachypnea, hypoxemia |
| Hematologic | Anemia, thrombocytopenia, neutropenia, febrile neutropenia, lymphopenia, B-cell aplasia, hypofibrinogenemia, bleeding, elevated D-dimer, prolonged prothrombin time, prolonged activated partial prothrombin time, disseminated intravascular coagulation |
| Gastrointestinal | Nausea, diarrhea, emesis |
| Cardiovascular | Tachycardia, widened pulse pressure, hypotension, arrhythmias, QT prolongation, increased cardiac output (early), potentially diminished cardiac output (late) |
| Renal | Acute kidney injury, hyponatremia, hypokalemia, hypophosphatemia, tumor lysis syndrome, azotemia |
| Hepatic | Transaminitis, hyperbilirubinemia |
| Neurologic | Headache, mental status changes, confusion, delirium, word finding difficulty or frank aphasia, hallucinations, tremor, dymetria, altered gait, seizures |
| Skin | Rash, edema |
Cytokine Storm Induced in Viral Infection
The virus can promote the activation of immune cells (such as T cells, B cells, macrophages, dendritic cells, neutrophils, monocytes) and resident tissue cells, resulting in the production of large amounts of inflammatory cytokines (13, 14). During the flu virus infection, innate immune responses get started through the cascade amplification reactions of interferon stimulated gene expression, and type | interferon (IFN) is mainly produced by monocytes, macrophages and dendritic cells (15). Serum levels of interleukin 8 (IL-8), IP-10 (interferon-induced protein 10), MCP-1 (monocyte chemoattractant protein-1), MIP-1 (macrophage inflammatory protein-1), MIG (monokine induced by IFN-γ) and CXCL-9 (CXC chemokine ligand-9) were abnormally elevated in H5N1 influenza virus infection, while IL-8, IL-9, IL-17, IL-6, IL-15, TNF-α (tumor necrosis factor-α), IL-10 were increased in H1N1 influenza virus infection (16–18). Earlier researches demonstrated that serum levels of proinflammatory factors IFN-γ, IL1β, IL-6, IL-12, IL-18, IP-10, MCP-1, and CCL2 (CC chemokine ligand-2), CXCL-10 and IL-8 are positively correlated with lung inflammation and extensive lung tissue injury in SARS patients (19–21). Whereas, the levels of serum pro-inflammatory cytokines IL-6, IFN-γ, TNF-α, IL-15, IL-17, and chemokines IL-8, CXCL-10, and CCL5 were significantly increased in severe MERS patients (22, 23). Among numerous molecules that increase in virally-mediated cytokine storms, IL-6, IFN-γ, IL-1β, IL-8, IL-10, and TNF-α are of crucial importance (9, 24, 25). The occurrence of cytokine storm has been reported to be one of the main causes of death in patients with SARS-CoV, MERS-CoV, and influenza virus infections (8, 26). Similarly, cytokine storm is also a common feature of severe cases in COVID-19, and elevated levels of serum IL-6 and CRP correlate with respiratory failure, ARDS, MOF and adverse clinical outcomes (27, 28).
Pathophysiology of Cytokine Storm
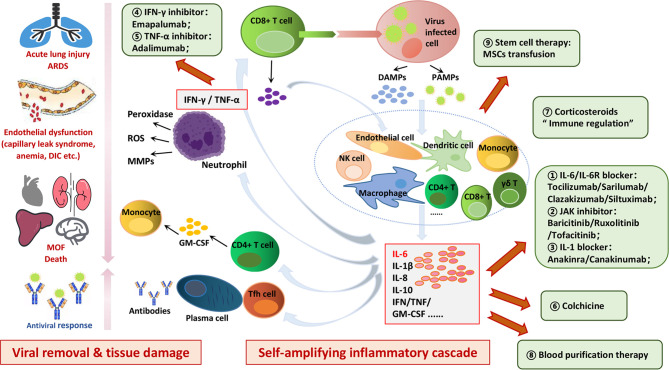
Both damage-associated molecular patterns (DAMPs) and pathogen-associated molecular patterns (PAMPs) are produced upon viral infection, which can activate antiviral responses in neighboring cells as well as recruit innate and adaptive immune cells, such as macrophages, natural killer (NK) cells, and gamma-delta T (γδ T) cells (Figure 1) (24, 29–33). Downstream production of interferons promotes intracellular antiviral defenses in neighboring epithelial cells which may limit viral dissemination, while the release of IL-6 and IL-1β from other immune cells promotes recruitment of neutrophils and T cells (29). Subsequently, the activation of T cells or lysis of immune cells induces secretion of IFN-γ and TNF-α, leading to the activation of immune cells and endothelial cells with further release of pro-inflammatory cytokines in a positive feedback loop manner (9). Although these inflammatory cytokines promote T follicular helper (Tfh) cell differentiation, B cell germinal center formation and antibody production, as well as Th1 (T helper 1) cell differentiation and cytotoxic CD8+ T cell generation to help viral removal, tissue damage caused by them cannot be ignored (34, 35). Activated neutrophils release leukotrienes and reactive oxygen species (ROS) that induce local pneumocyte and endothelial injury, directly leading to acute lung injury (29). Inflammatory mediators promote neutrophil release of nuclear deoxyribonucleic acid (DNA) to form neutrophil extracellular traps (NETs) which can snare pathogens as well as contribute to thrombi formation (33). This process, termed immuno-thrombosis, can also amplify the production of cytokines and is exemplified by links of thrombin with inflammasome activation and production of IL-1 (36). As vascular endothelial cells would be exposed to circulating cytokines and other immune mediators, coagulation disorders (such as capillary leak syndrome, thrombus formation, and even DIC) can also be caused by endothelial cell dysfunction in cytokine storms, indicating the crosstalk between hemostasis and cytokines (24, 33). High levels of circulating inflammatory cytokines can cause cell death as well as tissue damage, whereas their promotion of macrophages activation can lead to erythro-phagocytosis and anemia (24, 33). The successive occurrences of acute lung injury, abnormal alterations in vascular hemostasis, and cytokine-mediated tissue damage can eventually result in MOF (24, 33, 37).
Figure 1.
Mechanisms and hazards of cytokine storms induced in COVID-19 and potential therapeutic targets. Viral infection can induce antiviral responses in neighboring cells as well as recruit innate and adaptive immune cells, such as macrophages, dendritic cells, T cells, B cells and NK cells, leading to self-amplifying inflammatory cascade in a positive feedback loop manner. Cytokine storm not only limits further spread of virus in the body but also induces secondary tissue damage through the secretion of a large number of active mediators and inflammatory factors. The successive occurrences of acute lung injury, abnormal alterations in vascular hemostasis, and cytokine-mediated tissue damage can eventually result in MOF. Potential therapeutic targets to control cytokines storms in COVID-19 are as follows: IL-6/IL-6R blocker; JAK inhibitor; IL-1 blocker; IFN-γ inhibitor; TNF-α inhibitor; colchicine; corticosteroids; blood purification therapy; stem cell therapy.
As discussed above, cytokine storm not only limits further spread of virus but also induces secondary tissue damage through the secretion of large amounts of active mediators and inflammatory factors (Figure 1) (24, 29–33, 35, 38, 39). Thus, it can be seen that inhibition of this self-amplifying inflammatory cascade may not only control tissue damage, but also impair viral clearance. Unlike that in viral infection, the occurrence of cytokine storm in CAR-T therapy is secondary to T cell-mediated killing of tumor cells, and inhibition of this self-amplifying inflammatory cascade has no influence on therapeutic efficacy (9, 29). Nevertheless, it has been proved that antiviral immune responses and tissue toxicity could be at least partially uncoupled; therefore, inhibition of select arms of innate immune responses could limit tissue toxicity while not greatly suppressing ongoing antiviral immunity (29).
Clinical, Pathological, and Serological Manifestations in COVID-19
The incubation period of COVID-19 patients ranged from 1 to 14 days, and mostly from 3 to 7 days (8, 40). Common symptoms at onset of illness were fever, dry cough, myalgia, fatigue, dyspnea, and anorexia; however, a few patients presented initially with atypical symptoms, such as diarrhea and nausea (6, 40). Most patients had good results with treatment, while the elderly patients and those with chronic diseases usually had poor prognoses. Although most patients with COVID-19 had mild and moderate symptoms, severe and critically ill patients progressed rapidly to acute respiratory failure, ARDS, metabolic acidosis, coagulopathy, septic shock, and MOF (7, 40–42). The autopsy report in the journal The Lancet Respiratory Medicine showed typical ARDS-like lung injury with lymphocyte infiltration, liver injury with moderate micro-vesicular steatosis, mild lobular and portal activity (43). COVID-19 patients usually revealed significantly reduced lymphocyte counts and increased inflammatory factors, especially those with severe illnesses (6, 40, 44). Wang et al. reported that the neutrophil count and D-dimer continued to increase in non-survivors, whereas lymphocyte counts continued to decrease until death occurred (40). Neutrophilia may be related to cytokine storms induced by virus invasion, and coagulation activation may be related to sustained inflammatory responses (40).
Cytokine Storm Is a Key Determiner in the Fate of COVID-19
Huang et al. observed that patients in intensive care unit (ICU) showed higher levels of plasma inflammatory cytokines IL-2, IL-7, IL-10, G-CSF (granulocyte colony-stimulating factor), IFN-γ and MCP and TNF-α than non-ICU patients (6), indicating the positive correlation between the cytokine storm and the severity of illness. These cytokines suggested not only Th1 responses but also Th2 responses in COVID-19, which differed from SARS-CoV infections (6). After being infected with the SARS-CoV-2, CD4+ T cells were activated and differentiated into Th1 cells to secrete pro-inflammatory cytokines, such as IL-6, IFN-γ, and GM-CSF (granulocyte-macrophage colony stimulating factor) (6, 45). GM-CSF could activate mononuclear cells to promote further release of IL-6 and other pro-inflammatory cytokines, leading to the generation of cytokine storms (45). Therefore, IL-6 and GM-CSF released by T lymphocytes and mononuclear cells may be the key link of cytokine storm in COVID-19 (45). Moreover, the activation of monocytes may suggest that the cytokine storm in COVID-19 is closely related to the destruction of the balance between innate and adaptive immunity.
Recent studies also showed that the level of IL-6 in severe cases was significantly higher than that in mild and moderate cases, but the levels of CD4+ T cells, CD8+ T cells and NK cells were decreased, indicating the immunosuppression in severe COVID-19 patients (44). Although peripheral CD4+ T cells and CD8+ T cells were significantly reduced, the number of Th17 cells increased and CD8+ T cells were highly cytotoxic, which further suggested that cytokine storms may aggravate tissue damage (43). Meanwhile, T lymphocyte cells were excessively activated during the cytokine storm in COVID-19 patients, which may be accompanied by severe immune dysfunctions (43). The cytokine storm can directly damage the pulmonary capillary mucosa, promote alveolar edema, and further induce the diffusion of inflammatory cytokines, thus resulting in the damage of alveolar structure and pulmonary ventilation dysfunction (25, 46). In addition, the cytokine storm is associated with the sequence and severity of organ dysfunction in multiple organ dysfunction syndrome (MODS) (37). Therefore, the cytokine storm may be an important factor that affects the fate of patients with COVID-19 pneumonia.
Possible Mechanisms of Cytokine Storm in COVID-19
Hyperactivated Innate Immune Responses
During the process of antiviral immune responses, innate and adaptive immune responses interact with each other and cooperate closely to produce immune protection (47). There is a time limit for adaptive immune responses, which usually gets initiated 4 to 7 days after infection. Unlike adaptive immune responses, innate immune responses occur immediately after infection and are fully involved in virus clearance. However, the innate immunity is relatively weak in virus clearance, and adaptive immunity is the key factor in complete elimination of the virus (47). If the body does not generate effective adaptive antiviral responses in time to clear the virus, the innate immune responses will be strengthened, which cannot eliminate the virus effectively and even lead to systematic inflammation responses with uncontrolled release of inflammatory cytokines (48, 49). The latest studies have shown that the average age of severe and critically ill patients is higher than that of mild cases (66-years old vs. 51-years old), and severe cases are more likely to have other chronic diseases (72.2% vs. 37.3%) (40, 50). As for the elderly patients and those with chronic diseases, it takes a longer period of time to generate effective adaptive immune responses due to the deterioration of immune functions. These patients only rely on strengthening the innate antiviral immune responses in the early stages of infection, leading to a higher risk of cytokine storms, earlier onset of severe illness, and a higher mortality rate. Although the kinetics of the responses to SARS-CoV-2 fit with models of the induction of conventional antiviral immunity, it is still unclear whether immune hyperactivity is due to ongoing viral replication or immune dysregulation (33). Pyroptosis is a highly inflammatory and caspase-1-dependent form of programmed cell death that occurs most frequently upon infection with intracellular pathogens and is a part of the antimicrobial responses, which may also play a role in COVID-19 pathogenesis (51, 52). Rapid viral replication that causes increased pyroptosis may lead to a massive release of inflammatory mediators (51). Taken together, viral escape to avoid anti-viral immunity, together with genetic or acquired defects in host defense, may impair viral clearance, resulting in inappropriate immune activation and consequently causing cytokine storms (52). In a word, the exaggerated activation of innate immunity may be an important factor in the formation of cytokine storms in COVID-19 (29).
Dysregulation of ACE2 and Its Downstream Pathway
Angiotensin converting enzyme 2 (ACE2) primarily catalyzes the breakdown of angiotensin II (AngII) to maintain the homeostasis of renin-angiotensin-aldosterone system (RAAS) as a pivotal counter-regulator, which is crucial for the physiology and pathology of most human organs (53, 54). Significant to COVID-19, ACE2 has been established as the functional host receptor for SARS-CoV-2, and many factors have proved to be associated with both altered ACE2 expression and disease severity and progression, including age, sex, ethnicity, medication, and several co-morbidities (such as cardiovascular disease, metabolic syndrome, and lung cancer) (53–57). Recent studies have also revealed potential roles of ACE2 in regulating immune responses rather than merely being a viral-binding receptor in COVID-19 (53–55, 58–61). Chen’s team found the expression axis “mir-125b-5p-ACE2-IL-6” existed in lung adenocarcinoma, in which mir-125b-5p inhibited the expression of IL-6 through promoting the up-regulation of ACE2 (58). Once bound by SARS-CoV-2, the ACE2 expression (including mRNA level and enzyme activity) on the surface of host cells were significantly decreased, and then IL-6 in the toll-like receptor signaling pathway might influence the immune system as the downstream effector (53, 54, 58). Therefore, the dysregulation of ACE2 induced by SARS-CoV-2 infection may further cause cytokine storms and pneumonia, and targeting to the upstream regulator mir-125b-5p may provide a new way for the control of COVID-19 (58, 60). More interestingly, the spike protein of SARS-CoV has been previously demonstrated to downregulate ACE2 expression, thus resulting in over-production of AngII (the downstream of ACE2) by the related enzyme ACE (62, 63). Similarly, it could be hypothesized that SARS-CoV-2 may downregulate ACE2 receptors and thereby leading to an over-production of AngII, which may be another possible explanation of cytokine storm in COVID-19 (59, 61). ACE2 molecules on the cell surface are occupied by SARS-CoV-2, and then AngII increases due to a reduction of ACE2-mediated degradation (59, 61). SARS-CoV-2 itself activates nuclear factor kappa B (NF-κB) via pattern recognition receptors (PPRs), and the accumulated AngII in turn induces the activation of the IL-6 amplifier through enhanced activation of NF-κB pathway and IL-6-STAT3 (signal transducers and activators of transcription family 3) axis (61). IL-6 is a key factor in this positive feedback loop, ultimately leading to the release of cytokines out of control (64). More importantly, IL-6 is a major functional marker of cellular senescence, and the age-dependent enhancement of the IL-6 amplifier may correspond to the age-dependent increase of COVID-19 mortality (61, 64).
Controlling Cytokine Storm is Vital in COVID-19
Lessons should be learned from the outbreak of SARS-CoV and MERS-CoV to accumulate valuable experience and insights on how to effectively treat COVID-19 pneumonia patients. There are three progressive stages upon SARS-CoV-2 infection: early infection, pulmonary phase, and hyper-inflammation phase (65). Targeted treatments are urgently needed to prevent the occurrence of cytokine storms, and the early infection stage with no or mild symptoms is the key period for active treatment to control further deterioration (65). Antiviral drugs that inhibit virus transmission and destroy virus replication can reduce direct cell damage caused by COVID-19, and appropriate combinations with immunoregulatory therapies that inhibit hyper-activated inflammatory responses can resist cytokine storms triggered by the virus (Figure 1 and Table 2) (72, 73). Multiple clinical trials have been initiated to investigate potential interventions to control cytokine storms in patients with COVID-19, mainly including direct inhibition of cytokines and immunomodulatory therapies (Figure 1 and Table 2).
Table 2.
Ongoing clinical trials of strategies to control cytokine storms in COVID-19.
| Trial identifier | Participants | Trial design | Therapy | Mechanism | Adverse effects |
|---|---|---|---|---|---|
| ChiCTR2000029765 | Adult (18–85 years), moderate/severe/critically ill patients | A multicenter, randomized controlled trial | Tocilizumab vs. Standard medical care |
IL-6 receptor blocker | Infections; skin rash; anemia; neutropenia; lymphopenia; liver enzyme elevations etc. |
| ChiCTR2000030796 | Diagnosed cases | A retrospective study | Tocilizumab | ||
| ChiCTR2000030894 | Adult (18 Years to 65 Years), moderate/severe patients | A multicenter, randomized, controlled trial | Tocilizumab combined with Favipiravir vs. Standard medical care |
||
| NCT04332913 | Adult, severe/critically ill patients | A prospective, observational study | Tocilizumab | ||
| NCT04322773 | Adult, severe/critically ill patients | An open-Label, multicenter sequential, cluster randomized trial | Tocilizumab vs. Sarilumab vs. Standard medical care |
||
| NCT04317092 | Adult, severe/critically ill patients | A multicenter, single-arm, open-label, phase 2 study | Tocilizumab | ||
| NCT04320615 | Adult, severe/critically ill patients | A randomized, double-blind, placebo-controlled, multicenter, phase 3 trial | Tocilizumab vs. Placebo |
||
| NCT04306705 | Adult, severe/critically ill patients | A retrospective study | Tocilizumab vs. Standard medical care vs. Continuous renal replacement therapy |
||
| NCT04315480 | Adult, severe/critically ill patients | A phase 2 Simon’s optimal two-stages trial | Tocilizumab | ||
| NCT04335071 | Adult, severe/critically ill patients | A multicenter, double-blind, randomized controlled phase II trial | Tocilizumab vs. Placebo |
||
| NCT04324073 | Adult, moderate/severe/critically ill patients | A multiple, open-label, randomized controlled trial | Sarilumab vs. Standard medical care |
||
| NCT04315298 | Adult, severe/critically ill patients | An adaptive phase 2/3, randomized, double-blind, placebo-controlled Study | Sarilumab vs. Placebo |
||
| NCT04327388 | Adult, severe/critically ill patients | An adaptive phase 3, randomized, double-blind, placebo-controlled trial | Sarilumab vs. Placebo |
||
| NCT04341870 | Adult (18–80 years), moderate/severe/critically ill patients | a multicenter open-label 1:1 randomized controlled trial | Sarilumab vs. Azithromycin vs. Hydroxychloroquine |
||
| NCT04348500 | Adult patients with pulmonary involvement who have not yet required mechanical ventilation and/or ECMO | A single center, randomized, double-blind, placebo-controlled, exploratory phase II study | Clazakizumab vs. Placebo |
IL- 6 monoclonal antibody | |
| NCT04322188 (66) | Adult, severe/critically ill patients | A single-center observational cohort study | Siltuximab vs. Standard medical care |
||
| NCT04329650 | Adult, severe/critically ill patients | A phase 2, randomized, open-label study | Siltuximab vs. methylprednisolone |
||
| NCT04318366 (67) | Adult, moderate to severe patients | A retrospective cohort study | Anakinra vs. Standard medical care |
IL-1 receptor antagonist blocking IL-1α and IL-1β | Infections; skin rash; anemia; neutropenia; lymphopenia; liver enzyme elevations etc. |
| NCT04330638 | Adult, severe/critically ill patients | A prospective, randomized, factorial design, interventional Study | Anakinra vs. Tocilizumab vs. Siltuximab vs. Usual Care |
||
| NCT04341584 | Adult, severe/critically ill patients | A multiple randomized controlled trial | Anakinra vs. Standard medical care |
||
| NCT04339712 | Adult, severe/critically ill patients | A non-randomized, open-label trial | Anakinra vs. Tocilizumab |
||
| NCT04365153 (68) | Adult, severe/critically ill patients with cardiac injury | A double-blind, randomized controlled trial | Canakinumab vs. Placebo |
IL-1β monoclonal antibody | |
| NCT04348448 (69) | Adult (18–100 years), severe/critically ill patients | A prospective, observational study | Canakinumab | ||
| ChiCTR2000030089 | Adult, severe/critically ill patients | A randomized, open-label, controlled trial | Adalimumab vs. Standard medical care |
TNF-α inhibitor | Infections; fever; anemia, neutropenia, lymphopenia etc. |
| NCT04324021 (70) | Adult (30–79 years), severe/critically ill patients | An open label, controlled, parallel group, 3-arm, multicenter study | Emapalumab vs. Anakinra vs. Standard medical care |
IFN-γ inhibitor | Serious infections; skin rash; fever; anemia; coagulopathy etc. |
| NCT04358614 | Adult, moderate patients | A phase 2/3, open label, clinical trial | Baricitinib vs. Standard medical care |
JAK1/JAK2 inhibitor | Infections; malignancy; thrombosis: DVT, PE; bleeding; myelofibrosis; anemia, neutropenia, lymphopenia, thrombocytosis, liver enzyme elevations etc. |
| NCT04321993 | Adult, severe/critically ill patients | An open label, non-randomized, parallel group study | Baricitinib vs. Standard medical care |
||
| NCT04320277 | Adult (18–85 years), mild/moderate patients | An open label, non-randomized, crossover assignment study | Baricitinib vs. Standard medical care |
||
| NCT04346147 | Adult, non-severe patients | A prospective, phase II, randomized, open-label, parallel group study | Baricitinib vs. Hidroxicloroquine vs. Lopinavir/ritonavir vs. Imatinib |
||
| NCT04340232 | Adult (18–89 years), without invasive oxygen supplementation | A single arm, open label study | Baricitinib | ||
| NCT04321993 | Adult, severe/critically ill patients | A parallel, open-label, non-randomized intervention trial | Baricitinib vs. Standard medical care |
||
| NCT04348695 | Adult, severe patients | A randomized, open label, phase II trial | Ruxolitinib plus simvastatin vs. Standard medical care | ||
| NCT04331665 | 12 Years and older, require supplemental oxygen | A single arm open-label clinical study | Ruxolitinib | ||
| NCT04337359 | 6–90 years, severe/critically ill patients | A single arm open-label, intermediate-size population | Ruxolitinib | ||
| NCT04338958 | Adult, severe/critically ill patients | A single arm, non-randomized open phase II trial | Ruxolitinib | ||
| NCT04348071 | Adult (18–89 years), requires supportive care | An adaptive phase 2/3 clinical trial | Ruxolitinib vs. Standard medical care |
||
| NCT04332042 | Adult (18–65 years), hospital admission from less than 24 h | A prospective, single cohort, open study | Tofacitinib | JAK1/JAK3 inhibitor | |
| NCT04322682 | 40 Years and older, possess at least one high-risk criteria | A randomized, double-blind, placebo-controlled, multi-center study | Colchicine vs. Placebo oral tablet |
Inhibition of pyrin and NLRP3 inflammasome activation | Diarrhea; pancytopenia nausea; abdominal pain etc. |
| NCT04322565 | Adult (18–100 years), severe patients | A prospective, phase II, randomized, open-label, Parallel Group Study | Colchicine vs. Standard of care |
||
| NCT04328480 | Adult, severe/critically ill patients | A simple pragmatic randomized open controlled trial | Colchicine vs. Local standard of care |
||
| NCT04326790 (71) | Adult, severe/critically ill patients | An open label, randomized, parallel group study | Colchicine vs. Standard of care |
||
| NCT04350320 | Adult, admitted in the hospital in the previous 48 hours, with clinical status 3, 4, or 5 of WHO classification. | A phase III, prospective, pragmatic, randomized, controlled and open-label trial | Colchicine vs. Standard of care |
||
| ChiCTR2000029386 | Adult, severe/critically ill patients | A prospective, phase II, randomized, open-label, Parallel Group Study | Methylprednisolone vs. Standard of care |
Promote the inhibition of HAT and recruitment of HDAC2 activity to downregulate inflammatory genes | Serious Infections: pneumonia, herpes zoster, urinary tract infection; fever; allergy; thrombosis; abnormal blood glucose and pressure; arrhythmia etc. |
| ChiCTR2000029656 | Adult, severe/critically ill patients | A randomized, open-label study | Methylprednisolone vs. Standard of care |
||
| NCT04263402 | Adult, severe/critically ill patients | An open, prospective/retrospective, randomized controlled Cohort Study | Methylprednisolone vs. Standard of care |
||
| ChiCTR2000030503 | Adult, severe/critically ill patients in ICU | A prospective cohort stud | Blood purification therapy | Remove elevated inflammatory mediators and cytokines | Allergies; fever, thrombosis; hypotension; thrombocytosis; bleeding; air embolism etc. |
| ChiCTR2000029606 | Adult, critically ill patients | An open, randomized controlled trial | Menstrual Blood-derived Stem Cells | Inhibit abnormal activation of T cells and macrophages and induce their differentiation into regulatory T cells and anti-inflammatory macrophages; obstruct the secretion of pro-inflammatory cytokines. | Allergies; fever; arrhythmia etc. |
| ChiCTR2000031139 | Adult (18–80 years), severe/critically ill patients | An open label, single arm study | Embryonic MSCs | ||
| ChiCTR2000030088 | Adult (18–80 years), severe/critically ill patients | An open label, randomized, parallel group study | Wharton’s Jelly MSCs | ||
| NCT04269525 | Adult (18–80 years), severe/critically ill patients | An open label, single arm study | Umbilical cord-derived MSCs | ||
| NCT04252118 | Adult (18–70 years), severe/critically ill patients | An open label, non-randomized, parallel group study | MSCs vs. Standard of care |
||
| NCT04288102 | Adult (18–75 years), severe/critically ill patients | A phase II, multicenter, randomized, double-blind, placebo-controlled Trial | MSCs vs. Standard of care |
||
| NCT04276987 | Adult (18–75 years), severe/critically ill patients | An open label, single arm, pilot clinical study | Allogenic adipose MSCs | ||
| NCT04273646 | Adult (18–65 years), severe/critically ill patients | An open label, randomized, parallel group study | Umbilical cord-derived MSCs vs. Standard of care |
Inhibition of Cytokines
Blocking of IL-6/IL-6R
One meta-analysis of mean IL-6 concentrations demonstrated 2.9-fold higher levels in patients with complicated COVID-19 compared with those with non-complicated disease (74), and another meta-analysis also reported the relation between IL-6 levels and severe condition (75), indicating that IL-6 was a good indicator of poor prognosis in COVID-19 (74). At present, blockers of IL-6/IL-6R have been preliminarily applied in a series of ongoing clinical trials of COVID-19 and further multi-center clinical trials are being carried out (Table 2). Tocilizumab (a kind of IL-6 receptor blocker, IL-6R), first approved for rheumatic conditions, can effectively reverse iatrogenic cytokine storms which are caused by CAR-T therapy in patients with hematological malignancies (11, 76). One clinical trial from China (ChiCTR2000029765) reported that tocilizumab made rapid improvements in fever control and respiratory functions in 21 severe patients with COVID-19, and all participants including two seriously ill patients recovered and were discharged from the hospital (77, 78). Roumier et al. reported their experience regarding tocilizumab in 30 COVID-19 patients, suggesting that tocilizumab significantly reduced mechanical ventilation requirements (odd ratio, OR=0.42) and risk of subsequent ICU admissions (OR=0.17) (79). Toniati’s group published a single center study of 100 COVID-19 patients in Italy and also demonstrated that the response to tocilizumab was rapid, sustained, and associated with significant clinical improvements (80). A systematic review and meta-analysis of observational studies found decreased mortality in COVID-19 patients treated with tocilizumab (81). In addition, IL-6 blockade with tocilizumab does not impair the viral specific antibody responses despite of a delayed viral clearance driven by a higher initial viral load, indicating the safety of tocilizumab in patients with COVID-19 (82). Sarilumab is another kind of IL-6R blocker that is being investigated in SARS-CoV-2 infection (83, 84), which may reflect a possible clinical benefit regarding early intervention with IL-6-modulatory therapies for COVID-19 (85). Although not yet approved by Food and Drug Administration (FDA), clazakizumab (a monoclonal antibody against human IL-6) may be helpful in inhibiting the cytokine storms, and related clinical trials are underway worldwide (86). It is also reported that patients with rapidly progressing COVID-19 respiratory failure requiring ventilatory support may benefit from treatment with siltuximab (IL-6 monoclonal antibody) because of reduced mortality and cytokine-driven hyperinflammation (NCT04322188) (66).
Blocking of IL-1 Family
There are three important cytokines of IL-1 family in cytokine storms: IL-1β, IL-18, and IL-33, among which the block of IL-1β to counteract the cytokine storms is of great concern (9, 29). Anakinra, a kind of IL-1 receptor antagonist that blocks activity of both IL-1α and IL-1β, has been approved by the FDA and the EDA (European Drug Administration) for the treatment of rheumatoid arthritis, systemic-onset juvenile idiopathic arthritis, and familial Mediterranean fever (67, 87, 88). Anakinra can also be used in the treatment of cytokine storms caused by infection, significantly improving the survival rate of severe sepsis (89). Compared with other cytokine blockers, anakinra has shorter half-life; thus, it is safer and more suitable for severe and critically ill patients. A retrospective cohort study (NCT04324021) reported that high doses of intravenous anakinra inhibit systemic inflammation and were associated with progressive improvement in respiratory function in severe patients with COVID-19 (70). Other clinical trials are also under way to evaluate the use of anakinra in COVID-19 (NCT04330638, NCT04341584, NCT04339712 etc.). Canakinumab, a monoclonal antibody selectively targeting IL-1β, is also being investigated in the treatment for COVID-19. It was proved that canakinumab was safe, well tolerated, and associated with a rapid reduction in the systemic inflammatory response and an improvement in cardiac and respiratory function (68, 69). Nevertheless, strengthened evidence for the application of anakinra and canakinumab in COVID-19 are required in further random controlled trials.
Other Blockers
There is no clinical evidence nor any registered clinical trials assessing the possibility of IL-18 blockers and IL-33 blockers in COVID-19. TNF-α and IFN-γ are also key inflammatory cytokines and attractive targets in the control of cytokine storms (6, 90, 91), and clinical trials are ongoing to test these blockers in COVID-19 (ChiCTR2000030089, NCT04324021) (70, 92). JAK/STAT (janus kinase/signal transducers and activators of transcription) signal transduction pathway, a common downstream signaling pathway of various cytokines, can block multiple targeted cytokines at the same time if inhibited (93, 94). However, its possible side effects cannot be ignored, such as increased risk for pulmonary embolism (PE), liver enzyme elevations, hematological abnormalities and suppression of antiviral immunity (94–96). Several representative JAK inhibitors, such as tofacitinib, baricitinib, and ruxolitinib, are currently being investigated to determine whether they can be applied to the treatment of COVID-19 (NCT04332042, NCT04348695, NCT04321993, NCT04348695, etc.) (94). Baricitinib and ruxolitinib are selective inhibitors of JAK1/JAK2 which is responsible for multiple cellular signals including the proinflammatory IL-6 and works as immunomodulator decreasing the cytotoxic T lymphocytes and increasing the regulatory T cells (97, 98). A phase 2/3 clinical trial (NCT04358614) showed that all clinical characteristics and respiratory function parameters significantly improved in the baricitinib-treated group compared to the baseline, and no serious infections, cardiovascular and hematologic adverse effects occurred after treatment (29). Although tofacitinib is a selective inhibitor of JAK1/JAK3, it is suggested that for patients not on tofacitinib that this be initiated, but rather for those already on it that it can potentially be continued during a pandemic (99). Colchicine can inhibit the inflammasome activation of pyrin and NLRP3 (NLR Family Pyrin Domain Containing 3), and are also currently under way to be evaluated in the treatment of COVID-19 (71, 100, 101). A single-center cohort study showed that patients treated with colchicine had a better survival rate as compared with standard care at 21 days of follow-up, and the adverse effects were similar for two groups, which may support the rationale of use of colchicine for the treatment of COVID-19 (100). Another randomized clinical trial of 105 COVID-19 patients also suggested that low-dose of colchicine combined anti-inflammatory action with a favorable safety profile (71). Moreover, it is also recommended as a therapeutic option in patients who have contraindications to other drugs or in the context of shortage/unavailability of anti-viral drugs (such as in underdeveloped countries) due to high availability (101).
Corticosteroids
Corticosteroids, a type of steroid hormones, exhibit anti-inflammatory activity via binding to the cytoplasmic corticosteroid receptor, which leads to inhibitions of HAT (histone acetyltransferase) and recruitment of HDAC2 (histone deacetylases 2) activity to downregulate inflammatory genes (102). Thus, corticosteroids have been widely used to control cytokine storms. Data from a limited-size trial showed that the early use of low or medium doses of methylprednisolone had a positive effect for patients with severe COVID-19 (103). A single-blind, randomized, controlled trial in Iran (trial identifier: IRCT20200404046947N1) suggested that methylprednisolone pulse could be an efficient therapeutic agent for hospitalized severe COVID-19 patients at the pulmonary phase (104). Although there was no significant difference in mortality, patients receiving methylprednisolone treatment seemed to be with a faster improvement of oxygen saturation, decrease in CRP and IL-6 level, and less demand for invasive ventilation (104, 105). However, adverse effects (including serious infection and edema etc.) were also observed in several patients after the methylprednisolone treatment (103–105). In addition, there are heated debates as to whether corticosteroid therapy will delay viral clearance in COVID-19 (106, 107). Therefore, the pros and cons should be carefully weighed before using glucocorticoids in the treatment of COVID-19 patients. It is very important for clinicians to master the time and dose of corticosteroids for the treatment of severe patients, especially before the infection occurs. In addition, great caution should be exercised for patients who already have hypoxemia for various reasons or those who take glucocorticoids regularly due to other chronic diseases.
Blood Purification Therapy
It has been demonstrated that the blood purification system, such as plasma exchange, adsorption, perfusion, blood/plasma filtration, can remove inflammatory factors and then reduce tissue damage of hyper-activated inflammatory responses (108). Li et al. demonstrated that the artificial liver blood purification system could rapidly remove inflammatory mediators, block cytokine storms, favor the balance of fluid, electrolytes and acid-base, and thus improve treatment efficacy in critical illnesses (109, 110). Ma et al. reported that three COVID-19 patients who received blood purification therapy were tolerable and effective in limited experiences (111). Successful recovery of a severe patient was also presented in one case report (112). Yang’s group developed a blood purification protocol for patients with severe COVID-19 based on previous experience in SARS and MERS, including four major steps: (i) to assess whether patients with severe COVID-19 require blood purification; (ii) to prescribe a blood purification treatment for patients with COVID-19; (iii) to monitor and adjust parameters of blood purification; (iv) to evaluate the timing of discontinuation of blood purification (113). Last but not least, possible adverse effects in blood purification therapy (such as allergies, thrombocytosis, bleeding, air embolism etc.) should be timely identified and controlled to ensure safe and effective treatment (109–113).
Stem Cell Therapy
As an important member of the stem cell family, mesenchymal stem cells (MSCs) not only have potentials for self-renewal and multidirectional differentiation but also have strong anti-inflammatory and immune regulatory functions (114–117). In addition, MSCs inhibit abnormal activation of T lymphocyte cells and macrophages and induce their differentiation into regulatory T cells and anti-inflammatory macrophages (117). MSCs also obstruct the secretion of pro-inflammatory cytokines, thereby reducing the occurrence of cytokine storms (114, 115, 117, 118). Currently, over thirty clinical trials about intravenous administration of MSCs in COVID-19 patients have been officially registered (www.clinicaltrials.gov), but most of them are under the recruitment phase. Recently, Zhao et al. reported the results of seven severe and critically ill patients with COVID-19 receiving MSCs transplantation therapy, which showed improved prognosis and effective avoidance of cytokine storms with no obvious side effects (119). Furthermore, other stem cell therapies have been initiated in clinical trials, such as human menstrual blood-derived stem cells (ChiCTR2000029606) and embryonic stem cells (ChiCTR2000031139).
Concluding Remarks
COVID-19 has been listed as an international public health emergency by WHO and the treatment of severe and critically ill patients is the burning issue in current prevention and control. As cytokine storm is one of the most common causes of mortality in COVID-19, therapeutic approaches to manage cytokine storm may provide a novel avenue to decrease the COVID-19 associated morbidity and mortality. Hyperactivated innate immune responses, dysregulation of ACE2 expression and its downstream pathway may be possible mechanisms. In the treatment of COVID-19, high levels of attention must be paid to the identification of the occurrence cytokine storm. Tailored immunoregulatory therapies to control and resist the progress of cytokine storms in early stages of COVID-19 can greatly improve prognosis and reduce mortality rates. Although several therapies used to control cytokine storm have entered the stage of clinical trials for the treatment of COVID-19, the limited source and potential adverse effects have delayed widespread application in clinical treatment. Moreover, the best timing of anti-cytokine storm therapies remains to be explored, as well as novel therapeutic methods which are more effective and tolerated.
Author Contributions
LT, YH, and HM: writing, original draft preparation. LT: table and figure preparation and editing. ZY, YH, and HM: review and editing. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by funds from the Key Special Project of Ministry of Science and Technology of China (no. 2020YFC0845700), Scientific Research Projects of Chinese Academy of Engineering of China no. 2020-XY-70 (2020-KYGG-01-07), and Fundamental Research Funds for the Central Universities of China (no. 2020kfyXGYJ029).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1. Ren LL, Wang YM, Wu ZQ, Xiang ZC, Guo L, Xu T, et al. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin Med J (Engl) (2020) 133(9):1015–24. 10.1097/cm9.0000000000000722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus ADME, Fouchier RAM. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. New Engl J Med (2012) 367(19):1814–20. 10.1056/NEJMoa1211721 [DOI] [PubMed] [Google Scholar]
- 3. Drosten C, Günther S, Preiser W, van der Werf S, Brodt H-R, Becker S, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. New Engl J Med (2003) 348(20):1967–76. 10.1056/NEJMoa030747 [DOI] [PubMed] [Google Scholar]
- 4. Bogoch II, Watts A, Thomas-Bachli A, Huber C, Kraemer MUG, Khan K. Potential for global spread of a novel coronavirus from China. J Travel Med (2020) 27(2):taaa011. 10.1093/jtm/taaa011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet (2020) 395(10223):470–3. 10.1016/S0140-6736(20)30185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London England) (2020) 395(10223):497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. New Engl J Med (2020) 382(18):1708–20. 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol (2017) 39(5):529–39. 10.1007/s00281-017-0629-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shimabukuro-Vornhagen A, Gödel P, Subklewe M, Stemmler HJ, Schlößer HA, Schlaak M, et al. Cytokine release syndrome. J Immunother Cancer (2018) 6(1):56. 10.1186/s40425-018-0343-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ferrara JL, Abhyankar S, Gilliland DG. Cytokine storm of graft-versus-host disease: a critical effector role for interleukin-1. Transplant Proc (1993) 25(1 Pt 2):1216–7. [PubMed] [Google Scholar]
- 11. Lee DW, Gardner R, Porter DL, Louis CU, Ahmed N, Jensen M, et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood (2014) 124(2):188–95. 10.1182/blood-2014-05-552729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fehr AR, Channappanavar R, Perlman S. Middle East Respiratory Syndrome: Emergence of a Pathogenic Human Coronavirus. Annu Rev Med (2017) 68:387–99. 10.1146/annurev-med-051215-031152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Krischuns T, Günl F, Henschel L, Binder M, Willemsen J, Schloer S, et al. Phosphorylation of TRIM28 Enhances the Expression of IFN-β and Proinflammatory Cytokines During HPAIV Infection of Human Lung Epithelial Cells. Front Immunol (2018) 9:2229. 10.3389/fimmu.2018.02229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Behrens EM, Koretzky GA. Review: Cytokine Storm Syndrome: Looking Toward the Precision Medicine Era. Arthritis Rheumatol (2017) 69(6):1135–43. 10.1002/art.40071 [DOI] [PubMed] [Google Scholar]
- 15. Klinkhammer J, Schnepf D, Ye L, Schwaderlapp M, Gad HH, Hartmann R, et al. IFN-λ prevents influenza virus spread from the upper airways to the lungs and limits virus transmission. Elife (2018) 7:e33354. 10.7554/eLife.33354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Liu Q, Zhou YH, Yang ZQ. The cytokine storm of severe influenza and development of immunomodulatory therapy. Cell Mol Immunol (2016) 13(1):3–10. 10.1038/cmi.2015.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Us D. Cytokine storm in avian influenza. Mikrobiyol Bul (2008) 42(2):365–80. [PubMed] [Google Scholar]
- 18. Thomas M, Mani RS, Philip M, Adhikary R, Joshi S, Revadi SS, et al. Proinflammatory chemokines are major mediators of exuberant immune response associated with Influenza A (H1N1) pdm09 virus infection. J Med Virol (2017) 89(8):1373–81. 10.1002/jmv.24781 [DOI] [PubMed] [Google Scholar]
- 19. Wong CK, LAM CWK, WU AKL, IP WK, LEE NLS, CHAN IHS, et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol (2004) 136(1):95–103. 10.1111/j.1365-2249.2004.02415.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhang Y, Li J, Zhan Y, Wu L, Yu X, Zhang W, et al. Analysis of serum cytokines in patients with severe acute respiratory syndrome. Infect Immun (2004) 72(8):4410–5. 10.1128/iai.72.8.4410-4415.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chien JY, Hsueh PR, Cheng WC, Yu CJ, Yang PC. Temporal changes in cytokine/chemokine profiles and pulmonary involvement in severe acute respiratory syndrome. Respirology (2006) 11(6):715–22. 10.1111/j.1440-1843.2006.00942.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mahallawi WH, Khabour OF, Zhang Q, Makhdoum HM, Suliman BAJC. MERS-CoV infection in humans is associated with a pro-inflammatory Th1 and Th17 cytokine profile. Cytokine (2018) 104:8–13. 10.1016/j.cyto.2018.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kim ES, Choe PG, Park WB, Oh HS, Kim EJ, Nam EY, et al. Clinical Progression and Cytokine Profiles of Middle East Respiratory Syndrome Coronavirus Infection. J Korean Med Sci (2016) 31(11):1717–25. 10.3346/jkms.2016.31.11.1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chousterman BG, Swirski FK, Weber GF. Cytokine storm and sepsis disease pathogenesis. Semin Immunopathol (2017) 39(5):517–28. 10.1007/s00281-017-0639-8 [DOI] [PubMed] [Google Scholar]
- 25. Tisoncik JR, Korth MJ, Simmons CP, Farrar J, Martin TR, Katze MG. Into the eye of the cytokine storm. Microbiol Mol Biol Rev MMBR (2012) 76(1):16–32. 10.1128/MMBR.05015-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dawood FS, Iuliano AD, Reed C, Meltzer MI, Shay DK, Cheng PY, et al. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study. Lancet Infect Dis (2012) 12(9):687–95. 10.1016/s1473-3099(12)70121-4 [DOI] [PubMed] [Google Scholar]
- 27. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest (2020) 130(5):2620–9. 10.1172/jci137244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med (2020) 46(5):846–8. 10.1007/s00134-020-05991-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vardhana SA, Wolchok JD. The many faces of the anti-COVID immune response. J Exp Med (6) (2020) 217(216):e20200678. 10.1084/jem.20200678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell (2006) 124(4):783–801. 10.1016/j.cell.2006.02.015 [DOI] [PubMed] [Google Scholar]
- 31. Kawai T, Akira S. Innate immune recognition of viral infection. Nat Immunol (2006) 7(2):131–7. 10.1038/ni1303 [DOI] [PubMed] [Google Scholar]
- 32. Medzhitov R. Recognition of microorganisms and activation of the immune response. Nature (2007) 449(7164):819–26. 10.1038/nature06246 [DOI] [PubMed] [Google Scholar]
- 33. Mangalmurti N, Hunter CA. Cytokine Storms: Understanding COVID-19. Immunity (2020) 53(1):19–25. 10.1016/j.immuni.2020.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Harker JA, Lewis GM, Mack L, Zuniga EI. Late interleukin-6 escalates T follicular helper cell responses and controls a chronic viral infection. Science (2011) 334(6057):825–9. 10.1126/science.1208421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Azkur AK, Akdis M, Azkur D, Sokolowska M, van de Veen W, Brüggen MC, et al. Immune response to SARS-CoV-2 and mechanisms of immunopathological changes in COVID-19. Allergy (2020) 75(7):1564–81. 10.1111/all.14364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol (2013) 13(1):34–45. 10.1038/nri3345 [DOI] [PubMed] [Google Scholar]
- 37. Wang H, Ma S. The cytokine storm and factors determining the sequence and severity of organ dysfunction in multiple organ dysfunction syndrome. Am J Emergency Med (2008) 26(6):711–5. 10.1016/j.ajem.2007.10.031 [DOI] [PubMed] [Google Scholar]
- 38. Iwasaki A, Pillai PS. Innate immunity to influenza virus infection. Nat Rev Immunol (2014) 14(5):315–28. 10.1038/nri3665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Betakova T, Kostrabova A, Lachova V, Turianova L. Cytokines Induced During Influenza Virus Infection. Curr Pharm Des (2017) 23(18):2616–22. 10.2174/1381612823666170316123736 [DOI] [PubMed] [Google Scholar]
- 40. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA (2020) 323(11):1061–9. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost (2020) 18(4):844–7. 10.1111/jth.14768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Liao D, Zhou F, Luo L, Xu M, Wang H, Xia J, et al. Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study. Lancet Haematol (2020) 7(9):e671–8. 10.1016/s2352-3026(20)30217-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med (2020) 8(4):420–2. 10.1016/S2213-2600(20)30076-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, et al. Characteristics of lymphocyte subsets and cytokines in peripheral blood of 123 hospitalized patients with 2019 novel coronavirus pneumonia (NCP). medRxiv (2020) 2020.02.10.20021832. 10.1101/2020.02.10.20021832. [DOI]
- 45. Zhou Y, Fu B, Zheng X, Wang D, Zhao C, Qi Y, et al. Pathogenic T-cells and inflammatory monocytes incite inflammatory storms in severe COVID-19 patients. Natl Sci Rev (2020) 7(6):998–1002. 10.1093/nsr/nwaa041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zhang B, Swamy S, Balijepalli S, Panicker S, Mooliyil J, Sherman MA, et al. Direct pulmonary delivery of solubilized curcumin reduces severity of lethal pneumonia. FASEB J (2019) 33(12):13294–309. 10.1096/fj.201901047RR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Iwasaki A, Medzhitov R. Regulation of adaptive immunity by the innate immune system. Science (2010) 327(5963):291–5. 10.1126/science.1183021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Braciale TJ, Sun J, Kim TS. Regulating the adaptive immune response to respiratory virus infection. Nat Rev Immunol (2012) 12(4):295–305. 10.1038/nri3166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Newton AH, Cardani A, Braciale TJ. The host immune response in respiratory virus infection: balancing virus clearance and immunopathology. Semin Immunopathol (2016) 38(4):471–82. 10.1007/s00281-016-0558-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet (2020) 395(10223):507–13. 10.1016/s0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bergsbaken T, Fink SL, Cookson BT. Pyroptosis: host cell death and inflammation. Nat Rev Microbiol (2009) 7(2):99–109. 10.1038/nrmicro2070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Soy M, Keser G, Atagündüz P, Tabak F, Atagündüz I, Kayhan S. Cytokine storm in COVID-19: pathogenesis and overview of anti-inflammatory agents used in treatment. Clin Rheumatol (2020) 39(7):2085–94. 10.1007/s10067-020-05190-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Datta PK, Liu F, Fischer T, Rappaport J, Qin X. SARS-CoV-2 pandemic and research gaps: Understanding SARS-CoV-2 interaction with the ACE2 receptor and implications for therapy. Theranostics (2020) 10(16):7448–64. 10.7150/thno.48076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Li Y, Zhou W, Yang L, You R. Physiological and pathological regulation of ACE2, the SARS-CoV-2 receptor. Pharmacol Res (2020) 157:104833. 10.1016/j.phrs.2020.104833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol (2020) 251(3):228–48. 10.1002/path.5471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol (2020) 21(3):335–7. 10.1016/s1470-2045(20)30096-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Jia X, Yin C, Lu S, Chen Y, Liu Q, Bai J, et al. Two Things about COVID-19 Might Need Attention. Preprints (2020) 2020020315. 10.20944/preprints202002.0315.v1 [DOI]
- 58. Chen L, Zhong L. Lung Adenocarcinoma Patients Own Higher Risk of SARS-CoV-2 Infection. Preprints (2020) 2020020386. [DOI] [PMC free article] [PubMed]
- 59. Catanzaro M, Fagiani F, Racchi M, Corsini E, Govoni S, Lanni C. Immune response in COVID-19: addressing a pharmacological challenge by targeting pathways triggered by SARS-CoV-2. Signal Transduct Target Ther (2020) 5(1):84. 10.1038/s41392-020-0191-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature (2005) 436(7047):112–6. 10.1038/nature03712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Hirano T, Murakami M. COVID-19: A New Virus, but a Familiar Receptor and Cytokine Release Syndrome. Immunity (2020) 52(5):731–3. 10.1016/j.immuni.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med (2005) 11(8):875–9. 10.1038/nm1267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Glowacka I, Bertram S, Herzog P, Pfefferle S, Steffen I, Muench MO, et al. Differential downregulation of ACE2 by the spike proteins of severe acute respiratory syndrome coronavirus and human coronavirus NL63. J Virol (2010) 84(2):1198–205. 10.1128/jvi.01248-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Murakami M, Kamimura D, Hirano T. Pleiotropy and Specificity: Insights from the Interleukin 6 Family of Cytokines. Immunity (2019) 50(4):812–31. 10.1016/j.immuni.2019.03.027 [DOI] [PubMed] [Google Scholar]
- 65. Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal. J Heart Lung Transplant (2020) 39(5):405–7. 10.1016/j.healun.2020.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Gritti G, Raimondi F, Ripamonti D, Riva I, Landi F, Alborghetti L, et al. IL-6 signalling pathway inactivation with siltuximab in patients with COVID-19 respiratory failure: an observational cohort study. medRxiv (2020) 2020.2004.2001.20048561. 10.1101/2020.04.01.20048561. [DOI]
- 67. Quartier P, Allantaz F, Cimaz R, Pillet P, Messiaen C, Bardin C, et al. A multicentre, randomised, double-blind, placebo-controlled trial with the interleukin-1 receptor antagonist anakinra in patients with systemic-onset juvenile idiopathic arthritis (ANAJIS trial). Ann Rheum Dis (2011) 70(5):747–54. 10.1136/ard.2010.134254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Sheng CC, Sahoo D, Dugar S, Prada RA, Wang TKM, Abou Hassan OK, et al. Canakinumab to reduce deterioration of cardiac and respiratory function in SARS-CoV-2 associated myocardial injury with heightened inflammation (canakinumab in Covid-19 cardiac injury: The three C study). Clin Cardiol (2020) 43(10):1055–63. 10.1002/clc.23451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ucciferri C, Auricchio A, Di Nicola M, Potere N, Abbate A, Cipollone F, et al. Canakinumab in a subgroup of patients with COVID-19. Lancet Rheumatol (2020) 2(8):e457–ee458. 10.1016/s2665-9913(20)30167-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Cavalli G, De Luca G, Campochiaro C, Della-Torre E, Ripa M, Canetti D, et al. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol (2020) 2(6):e325–31. 10.1016/S2665-9913(20)30127-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Deftereos SG, Giannopoulos G, Vrachatis DA, Siasos GD, Giotaki SG, Gargalianos P, et al. Effect of Colchicine vs Standard Care on Cardiac and Inflammatory Biomarkers and Clinical Outcomes in Patients Hospitalized With Coronavirus Disease 2019: The GRECCO-19 Randomized Clinical Trial. JAMA Netw Open (2020) 3(6):e2013136. 10.1001/jamanetworkopen.2020.13136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Li JY, You Z, Wang Q, Zhou ZJ, Qiu Y, Luo R, et al. The epidemic of 2019-novel-coronavirus (2019-nCoV) pneumonia and insights for emerging infectious diseases in the future. Microbes Infect (2020) 22(2):80–5. 10.1016/j.micinf.2020.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Liu J, Zheng X, Tong Q, Li W, Wang B, Sutter K, et al. Overlapping and discrete aspects of the pathology and pathogenesis of the emerging human pathogenic coronaviruses SARS-CoV, MERS-CoV, and 2019-nCoV. J Med Virol (2020) 92(5):491–4. 10.1002/jmv.25709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Coomes EA, Haghbayan H. Interleukin-6 in COVID-19: A Systematic Review and Meta-Analysis. medRxiv (2020) 2020.2003.2030.20048058. 10.1101/2020.03.30.20048058. [DOI] [PMC free article] [PubMed]
- 75. Ulhaq ZS, Soraya GV. Interleukin-6 as a potential biomarker of COVID-19 progression. Méd Maladies Infectieuses (2020) 50(4):382–3. 10.1016/j.medmal.2020.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Grupp SA, Kalos M, Barrett D, Aplenc R, Porter DL, Rheingold SR, et al. Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. N Engl J Med (2013) 368(16):1509–18. 10.1056/NEJMoa1215134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Xu X, Han M, Li T, Sun W, Wang D, Fu B, et al. Effective Treatment of Severe COVID-19 Patients with Tocilizumab. ChinaXiv (2020) 117(20):10970–5. 10.1073/pnas.2005615117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Xu X, Han M, Li T, Sun W, Wang D, Fu B, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci USA (2020) 117(20):10970–5. 10.1073/pnas.2005615117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Roumier M, Paule R, Groh M, Vallee A, Ackermann F. Interleukin-6 blockade for severe COVID-19. MedRxiv (2020) 2020.2004.2040.20061861. 10.1101/2020.04.20.20061861 [DOI]
- 80. Toniati P, Piva S, Cattalini M, Garrafa E, Regola F, Castelli F, et al. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: A single center study of 100 patients in Brescia, Italy. Autoimmun Rev (2020) 19(7):102568. 10.1016/j.autrev.2020.102568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Malgie J, Schoones JW, Pijls BG. Decreased mortality in COVID-19 patients treated with Tocilizumab: a rapid systematic review and meta-analysis of observational studies. Clin Infect Dis (2020) ciaa1445. 10.1093/cid/ciaa1445 [DOI] [PMC free article] [PubMed]
- 82. Masiá M, Fernández-González M, Padilla S, Ortega P, García JA, Agulló V, et al. Impact of interleukin-6 blockade with tocilizumab on SARS-CoV-2 viral kinetics and antibody responses in patients with COVID-19: A prospective cohort study. EBioMedicine (2020) 60:102999. 10.1016/j.ebiom.2020.102999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Caballero Bermejo AF, Ruiz-Antorán B, Fernández Cruz A, Diago Sempere E, Callejas Díaz A, Múñez Rubio E, et al. Sarilumab versus standard of care for the early treatment of COVID-19 pneumonia in hospitalized patients: SARTRE: a structured summary of a study protocol for a randomised controlled trial. Trials (2020) 21(1):794. 10.1186/s13063-020-04633-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Garcia-Vicuña R, Abad-Santos F, González-Alvaro I, Ramos-Lima F, Sanz JS. Subcutaneous Sarilumab in hospitalised patients with moderate-severe COVID-19 infection compared to the standard of care (SARCOVID): a structured summary of a study protocol for a randomised controlled trial. Trials (2020) 21(1):772. 10.1186/s13063-020-04588-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Montesarchio V, Parrela R, Iommelli C, Bianco A, Manzillo E, Fraganza F, et al. Outcomes and biomarker analyses among patients with COVID-19 treated with interleukin 6 (IL-6) receptor antagonist sarilumab at a single institution in Italy. J Immunother Cancer (2020) 8(2):e001089. 10.1136/jitc-2020-001089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Vaidya G, Czer LSC, Kobashigawa J, Kittleson M, Patel J, Chang D, et al. Successful Treatment of Severe COVID-19 Pneumonia With Clazakizumab in a Heart Transplant Recipient: A Case Report. Transplant Proc (2020) 52(9):2711–4. 10.1016/j.transproceed.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Cavalli G, Dinarello CA. Treating rheumatological diseases and co-morbidities with interleukin-1 blocking therapies. Rheumatol (Oxford) (2015) 54(12):2134–44. 10.1093/rheumatology/kev269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Ben-Zvi I, Kukuy O, Giat E, Pras E, Feld O, Kivity S, et al. Anakinra for Colchicine-Resistant Familial Mediterranean Fever: A Randomized, Double-Blind, Placebo-Controlled Trial. Arthritis Rheumatol (2017) 69(4):854–62. 10.1002/art.39995 [DOI] [PubMed] [Google Scholar]
- 89. Shakoory B, Carcillo JA, Chatham WW, Amdur RL, Zhao H, Dinarello CA, et al. Interleukin-1 Receptor Blockade Is Associated With Reduced Mortality in Sepsis Patients With Features of Macrophage Activation Syndrome: Reanalysis of a Prior Phase III Trial. Crit Care Med (2016) 44(2):275–81. 10.1097/ccm.0000000000001402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Feldmann M, Maini RN, Woody JN, Holgate ST, Winter G, Rowland M, et al. Trials of anti-tumour necrosis factor therapy for COVID-19 are urgently needed. Lancet (2020) 395(10234):1407–9. 10.1016/S0140-6736(20)30858-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis (2020) 71(15):762–8. 10.1093/cid/ciaa248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Blaszczak A, Trinidad JCL, Cartron AM. Adalimumab for treatment of hidradenitis suppurativa during the COVID-19 pandemic: Safety considerations. J Am Acad Dermatol (2020) 83(1):e31. 10.1016/j.jaad.2020.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Maschalidi S, Sepulveda FE, Garrigue A, Fischer A, de Saint Basile G. Therapeutic effect of JAK1/2 blockade on the manifestations of hemophagocytic lymphohistiocytosis in mice. Blood (2016) 128(1):60–71. 10.1182/blood-2016-02-700013 [DOI] [PubMed] [Google Scholar]
- 94. Peterson D, Damsky W, King B. The use of Janus kinase inhibitors in the time of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). J Am Acad Dermatol (2020) 82(6):e223–6. 10.1016/j.jaad.2020.03.099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. El Jammal T, Gerfaud-Valentin M, Sève P, Jamilloux Y. JAK inhibitors: Perspectives in internal medicine. Rev Med Interne (2019) 40(12):816–25. 10.1016/j.revmed.2019.07.016 [DOI] [PubMed] [Google Scholar]
- 96. Claire B. FDA issues tofacitinib safety alert. RheumatologyMedicinemattersCom (2019). Available at: https://rheumatology.medicinematters.com/rheumatoid-arthritis-/tofacitinib/fda-issues-tofacitinib-safety-alert/16527134.
- 97. Zhang X, Zhang Y, Qiao W, Zhang J, Qi Z. Baricitinib, a drug with potential effect to prevent SARS-COV-2 from entering target cells and control cytokine storm induced by COVID-19. Int Immunopharmacol (2020) 86:106749. 10.1016/j.intimp.2020.106749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Modi B, Hernandez-Henderson M, Yang D, Klein J, Dadwal S, Kopp E, et al. Ruxolitinib as Salvage Therapy for Chronic Graft-versus-Host Disease. Biol Blood Marrow Transplant (2019) 25(2):265–9. 10.1016/j.bbmt.2018.09.003 [DOI] [PubMed] [Google Scholar]
- 99. Jacobs J, Clark-Snustad K, Lee S. Case Report of a SARS-CoV-2 Infection in a Patient With Ulcerative Colitis on Tofacitinib. Inflammation Bowel Dis (2020) 26(7):e64. 10.1093/ibd/izaa093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Scarsi M, Piantoni S, Colombo E, Airó P, Richini D, Miclini M, et al. Association between treatment with colchicine and improved survival in a single-centre cohort of adult hospitalised patients with COVID-19 pneumonia and acute respiratory distress syndrome. Ann Rheum Dis (2020) 79(10):1286–9. 10.1136/annrheumdis-2020-217712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Piantoni S, Patroni A, Toniati P, Furloni R, Franceschini F, Andreoli L, et al. Why not to use colchicine in COVID-19? An oldanti-inflammatory drug for a novel auto-inflammatory disease. Rheumatol (Oxford) (2020) 59(7):1769–70. 10.1093/rheumatology/keaa217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Darwish I, Mubareka S, Liles WC. Immunomodulatory therapy for severe influenza. Expert Rev Anti Infect Ther (2011) 9(7):807–22. 10.1586/eri.11.56 [DOI] [PubMed] [Google Scholar]
- 103. Yang R, Xiong Y, Ke H, Chen T, Gao S. The Role of Methylprednisolone on Preventing Disease Progression for Hospitalized Patients with Severe COVID-19. Eur J Clin Invest (2020) 50(11):e13412. 10.1111/eci.13412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Edalatifard M, Akhtari M, Salehi M, Naderi Z, Jamshidi A, Mostafaei S, et al. Intravenous methylprednisolone pulse as a treatment for hospitalised severe COVID-19 patients: results from a randomised controlled clinical trial. Eur Respir J (2020) 2002808. 10.1183/13993003.02808-2020 [DOI] [PMC free article] [PubMed]
- 105. Nelson BC, Laracy J, Shoucri S, Dietz D, Zucker J, Patel N, et al. Clinical Outcomes Associated with Methylprednisolone in Mechanically Ventilated Patients with COVID-19. Clin Infect Dis (2020) ciaa1163. 10.1093/cid/ciaa1163 [DOI] [PMC free article] [PubMed]
- 106. Ji J, Zhang J, Shao Z, Xie Q, Zhong L, Liu Z. Glucocorticoid therapy does not delay viral clearance in COVID-19 patients. Crit Care (2020) 24(1):565. 10.1186/s13054-020-03287-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Huang R, Zhu C, Jian W, Xue L, Li C, Yan X, et al. Corticosteroid therapy is associated with the delay of SARS-CoV-2 clearance in COVID-19 patients. Eur J Pharmacol (2020) 889:173556. 10.1016/j.ejphar.2020.173556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Ye Q, Wang B, Mao J. The pathogenesis and treatment of the `Cytokine Storm’ in COVID-19. J Infect (2020) 80(6):607–13. 10.1016/j.jinf.2020.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Xu K, Cai H, Shen Y, Ni Q, Chen Y, Hu S, et al. Management of corona virus disease-19 (COVID-19): the Zhejiang experience. Zhejiang Da Xue Xue Bao (2020) 49(41):40. 10.3785/j.issn.1008-9292.2020.02.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Zhang Y, Yu L, Tang L, Zhu M, Jin Y, Wang Z, et al. A Promising Anti-Cytokine-Storm Targeted Therapy for COVID-19: The Artificial-Liver Blood-Purification System. Eng (Beijing) (2020). 10.1016/j.eng.2020.03.006 [DOI] [PMC free article] [PubMed]
- 111. Ma J, Xia P, Zhou Y, Liu Z, Zhou X, Wang J, et al. Potential effect of blood purification therapy in reducing cytokine storm as a late complication of critically ill COVID-19. Clin Immunol (2020) 214:108408. 10.1016/j.clim.2020.108408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Wang Q, Hu Z. Successful recovery of severe COVID-19 with cytokine storm treating with extracorporeal blood purification. Int J Infect Dis (2020) 96:618–20. 10.1016/j.ijid.2020.05.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Yang XH, Sun RH, Zhao MY, Chen EZ, Liu J, Wang HL, et al. Expert recommendations on blood purification treatment protocol for patients with severe COVID-19: Recommendation and consensus. Chronic Dis Transl Med (2020) 6(2):106–14. 10.1016/j.cdtm.2020.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Li N, Hua J. Interactions between mesenchymal stem cells and the immune system. Cell Mol Life Sci (2017) 74(13):2345–60. 10.1007/s00018-017-2473-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Galipeau J, Sensébé L. Mesenchymal Stromal Cells: Clinical Challenges and Therapeutic Opportunities. Cell Stem Cell (2018) 22(6):824–33. 10.1016/j.stem.2018.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Atluri S, Manchikanti L, Hirsch JA. Expanded Umbilical Cord Mesenchymal Stem Cells (UC-MSCs) as a Therapeutic Strategy in Managing Critically Ill COVID-19 Patients: The Case for Compassionate Use. Pain Physician (2020) 23(2):E71–e83. [PubMed] [Google Scholar]
- 117. Yagi H, Soto-Gutierrez A, Parekkadan B, Kitagawa Y, Tompkins RG, Kobayashi N, et al. Mesenchymal stem cells: Mechanisms of immunomodulation and homing. Cell Transplant (2010) 19(6):667–79. 10.3727/096368910x508762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Uccelli A, de Rosbo NK. The immunomodulatory function of mesenchymal stem cells: mode of action and pathways. Ann N Y Acad Sci (2015) 1351:114–26. 10.1111/nyas.12815 [DOI] [PubMed] [Google Scholar]
- 119. Leng Z, Zhu R, Hou W, Feng Y, Yang Y, Han Q, et al. Transplantation of ACE2(-) Mesenchymal Stem Cells Improves the Outcome of Patients with COVID-19 Pneumonia. Aging Dis (2020) 11(2):216–28. 10.14336/ad.2020.0228 [DOI] [PMC free article] [PubMed] [Google Scholar]