ABSTRACT
The Japanese government suspended proactive recommendation of human papillomavirus (HPV) vaccination due to several reports of adverse events related to it in 2013. After that, the immunization rate of HPV vaccine quickly declined in Japan. Health science teachers (HSTs) are qualified and licensed teachers in charge of health care and health education for students in Japanese schools. HSTs have not recommended HPV vaccination to female students, since active governmental recommendation for HPV vaccination was halted for 5 y. We conducted a primary survey targeting HSTs (N = 39) and university students taking the HST training course (N = 123). In each group, awareness regarding HPV vaccine and disease burden was evaluated and factors related to and barriers to HPV vaccine recommendation were identified. The primary survey found that many HSTs and university students recognized their insufficient knowledge regarding the HPV vaccine. Based on the primary survey’s results, infectious disease specialists, collaborating with Japanese HSTs, developed educational slide sets on HPV vaccine. A secondary survey was conducted before and after the lecture with HSTs (N = 162), where we evaluated their intelligibility and intention to recommend HPV vaccination for female students. In the post-lecture, secondary survey, the number of HSTs who recommended the HPV vaccine to their students had statistically increased from 76 before the lecture, to 103 (p < .05). An educational lecture using appropriate materials improved HSTs’ vaccine confidence and intention to recommend the HPV vaccine to their students, verifying the study’s hypothesis.
KEYWORDS: health science teacher, human papillomavirus, human papillomavirus vaccine, education, Japan
Introduction
During the last several years, six new vaccines have been included in the pediatric immunization program in Japan, and recent progress has partially resolved the “vaccine gap,” a term that has been used in the past decades to emphasize the delayed national immunization program in Japan.1 In Japan, bivalent human papillomavirus (HPV) vaccine was introduced in 2009, and the quadrivalent vaccine was introduced in 2011 as a voluntary vaccine, and it used to be recommended for female students aged 12–16 y. After the governmental subsidization of both vaccines, immunization rates of HPV vaccine quickly increased to more than 70%, and HPV vaccine was included in the routine vaccination program in April 2013.
However, severe adverse events were reported by numerous individuals, which resulted in the Japanese government suspending its proactive recommendation of HPV vaccine. Since then, the immunization rates of HPV have quickly declined in Japan, particularly among adolescents, where it decreased to less than 1%.2 Further, there were studies that proved the effectiveness of HPV vaccination for high-grade cervical lesions, and the causal relationship between the reported severe adverse events and HPV vaccination was not proven in Japan.3–5 However, the Japanese government continues the suspension of proactive recommendation of the HPV vaccine, and immunization rates remain at lower levels. Meanwhile, Japanese people are more sensitive to information about adverse events of vaccine than vaccine efficacy.6 Thus, to improve the situation regarding adolescent HPV vaccination in Japan, it is necessary to introduce an effective educational system on HPV vaccine for children and adolescents.
However, students have no opportunity, at the present time, to learn about the risks and benefits of vaccination or the disease burden of vaccine-preventable diseases in Japanese schools. In that regard, various educational interventions to increase HPV vaccination acceptance among parents and adolescents/young adults have been reported. However, there is no strong evidence for the recommendation of any specific intervention for wide-spread implementation.7
In Japan, there is a unique system that involves “health science teachers” (HSTs),8 who are specially qualified teachers in charge of the health care and health education of children in Japanese schools. This position is similar to a school nurse, except that HSTs have a teacher’s license. Recently, as HSTs have been playing a greater role in coping with students’ modern health problems in schools, their knowledge, beliefs, and behaviors toward HPV vaccination may directly impinge on students’ ways of thinking. Furthermore, because students are more accessible to HSTs than physicians, physicians expect HSTs to respond properly to the uneasiness of children and adolescents regarding the HPV vaccine.9 In addition, there have been reports that students and their parents consider that HSTs play the most important role in their health education, including with regard to the HPV vaccine.10 However, there have been no studies assessing the knowledge, beliefs, and intention to recommend the HPV vaccine among HSTs since the suspension of its active promotion in Japan.
Finally, according to previous studies, HSTs did not strongly recommend HPV vaccination to their students in junior high or high school, even before the suspension of the active governmental recommendation.11,12 Therefore, it is hypothesized that improving their knowledge and understanding regarding the risks and benefits of the HPV vaccine through educational lectures using appropriate materials could improve HSTs’ vaccine confidence, consequently improving recommendation rates for the HPV vaccine to their female students.
Materials and methods
In this study, we initially conducted a primary survey to identify the current status, issues, and barriers regarding HPV vaccination among HSTs. Based on the results of the primary survey, HSTs, and certified infectious disease specialists developed educational materials on HPV and HPV vaccine. Finally, a lecture was delivered to HSTs using our developed materials. Here, we report the effects of health education on HSTs’ intention to recommend adolescent HPV vaccine for their female students, which we examined through a secondary survey assessing the effect of the lecture post-intervention.
Phase 1: primary survey
To identify HSTs’ HPV vaccine awareness, disease burden awareness, and its factors and barriers, we conducted a primary survey among 39 Japanese HSTs in the Chiba prefecture, and 123 students from Chiba University who were taking the HST training course. Primary surveys were conducted during a workshop for HSTs. Before the primary survey, we explained the purpose of the survey. Informed consent was obtained from all participants verbally. The principal investigator collaborated with several HSTs to develop the questionnaire for this survey. First, the questionnaire included demographic information: age (for HSTs only), grade (for university students only), sex, and HPV vaccination history, and attitudes toward general vaccination (a question that was included based on previous studies).11,12 Second, the questionnaire included five questions related to the respondent’s knowledge of cervical cancer, HPV, HPV vaccine, and adverse events of HPV vaccine based on the data published by the Japanese Ministry of Health, Labor and Welfare. The answer was selected as yes, no, or unknown for each question. Third, the respondents’ feelings regarding the HPV vaccine (with two options: uncertain and fearful) and the information source of HPV vaccine were investigated (see supplemental file).
Phase 2: development of educational slide sets on HPV vaccine
Based on the results of the primary survey, certified infectious disease specialists, in collaboration with HSTs, developed educational slide sets about the HPV vaccine. For this purpose, Japanese documents and brochures related to the HPV vaccine were collected.13 We also referred to educational materials from the United States14 and the United Kingdom as the latter was considered as one of the countries with high HPV immunization coverage.15 Further, various textbooks regarding HPV vaccination have been published and utilized for science and/or health education in schools, both by science teachers and school nurses.16 We held regular meetings to develop slide sets promoting reflection for the HSTs regarding their opinions and ideas related to HPV vaccination.
Phase 3: secondary survey
The secondary survey was conducted twice among 162 Japanese HSTs within the Chiba prefecture and used to evaluate their understanding of HPV vaccination and intention to recommend HPV vaccine for their female students before and after the lecture. Secondary surveys were conducted during a workshop for HSTs. Before the survey, we explained the purpose of the survey to all participants. Informed consent was obtained from all participants verbally similar to the primary survey. None of the 162 HSTs had participated in the primary survey. The lecture was delivered by a medical doctor who is an infectious disease specialist, and the session comprised a 15-min survey administered before the lecture, a face-to-face 90-min educational intervention (including discussion), and a 15-min survey after the lecture. The questionnaire covered knowledge, attitudes, and beliefs related to HPV vaccination, and the contents of the questionnaire related to the knowledge and feelings regarding the HPV vaccine were prepared based on the results of the primary survey.
To evaluate the understanding of HPV vaccination, we compared the responses obtained before and after the lecture. Participants’ scores were measured by summing the number of correct answers, and total scores ranged from 0 to 20. To evaluate the intention to recommend the HPV vaccine among HSTs, the survey also included the question, “Do you recommend HPV vaccine if students or their guardians seek advice regarding the HPV vaccine?” This question was rated on a 5-point Likert scale ranging from 1 to 5, where 5 was “recommend,” 4 was “tend to recommend,” 3 was “do not know,” 2 was “tend to not recommend,” and 1 was “not recommend” (see supplemental file).
Statistical analysis was performed using SPSS Statistics version 25 (IBM, Japan). Categorical variables were compared using chi-square tests, and continuous variable analysis was conducted using Wilcoxon signed-rank test. We calculated 95% confidence intervals (CIs) and two-tailed p values, where p < .05 was considered significant. This study was approved by the Ethics Committee of Medical Mycology Research Center, Chiba University (No. 2017–16). The study was carried out in accordance with the code of ethics of the world medical association (Declaration of Helsinki). The privacy rights of participants were respected.
Results
Phase 1: primary survey
Data gathered through the primary survey regarding the 39 HSTs’ sociodemographic information are shown in Table 1. There was only one male student in the university student group, and 122 were female participants. Among 39 HSTs, 7.7% (3/39) had received HPV vaccine. In contrast, among the university students, 78.9% (97/123) had received HPV vaccine. The results of the questionnaire section of the primary survey are presented in Table 2. The results show that, among 20 questions regarding HPV and HPV vaccine, there was no question in which HSTs and university students had similar rates of collected answers. There were some questions that had a correct response rate of less than 50% for both HSTs and university students, which were: “cervical cancer screening starts with 20-year-olds in Japan,” “routine immunization program is still included in HPV vaccine in Japan,” and “rate of severe adverse events of HPV vaccine is less than 10 per 100,000 people.” There were also some questions that had a correct response rate of less than 50% exclusively among the university students, which were “90% of HPV infections clear up,” “HPV infection progresses to cervical cancer over a long period,” and “HPV is a pathogen of a benign tumor.” In terms of the feelings regarding the HPV vaccine among HSTs, 51.3% (20/39) felt uncertain, and 30.8% (12/39) felt fearful; among university students, 60.2% (74/123) felt uncertain, and 19.5% (24/123) felt fearful. Finally, regarding the information sources for HPV vaccine where they obtained their knowledge, 94.9% (37/39) of HSTs and 53.7% (66/123) of university students responded that they learnt through the internet.
Table 1.
Health science teachers’ sociodemographic information from the primary and secondary survey
| Primary survey |
Secondary survey |
|
|---|---|---|
| Number of participants | 39 | 162 |
| Age group | N (%) | N (%) |
| 20s | 12 (30.7%) | 45 (27.8%) |
| 30s | 9 (23.1%) | 33 (20.4%) |
| 40s | 7 (17.9%) | 27 (16.7%) |
| 50s | 11 (28.2%) | 52 (32.1%) |
| 60s | 0 (0.0%) | 5 (3.1%) |
| Sex | ||
| Male | 0 (0.0%) | 0 (0.0%) |
| Female | 39 (100.0%) | 162 (100.0%) |
| History of human papillomavirus vaccination | ||
| Yes | 3 (7.7%) | 14 (8.6%) |
| No | 36 (92.3%) | 148 (91.4%) |
Table 2.
Health science teachers’ and university students’ collected response rate of each subject from the questionnaire of the primary survey
| Topic main subject | Health science teachers (N = 39) | University students (N = 123) |
|---|---|---|
| Knowledge of cervical cancer (CC) | ||
| CC is related to HPV infection. | 38 (97.4%) | 117 (95.1%) |
| CC is mainly a sexually acquired infection. | 37 (94.9%) | 63 (51.2%) |
| CC screening starts with 20-year-olds in Japan. | 19 (48.7%) | 31 (25.2%) |
| HPV infection is initially asymptomatic. | 38 (97.4%) | 120 (97.6%) |
| Highest risk for CC is 20–30 y. | 30 (76.9%) | 72 (58.5%) |
| Knowledge of HPV | ||
| There are many types of HPV. | 38 (97.4%) | 115 (93.5%) |
| 90% of HPV infections clear up. | 25 (64.1%) | 51 (41.5%) |
| HPV infection progresses to CC over a long period. | 33 (84.6%) | 60 (48.8%) |
| HPV is a pathogen of a benign tumor. | 31 (79.5%) | 19 (15.4%) |
| HPV infects men. | 30 (76.9%) | 72 (58.5%) |
| Knowledge of the HPV vaccine | ||
| Japan suspended proactive recommendation of HPV vaccine. | 31 (79.5%) | 88 (71.5%) |
| A routine immunization program is still included in HPV vaccine in Japan. | 15 (38.5%) | 45 (36.6%) |
| Learners in the upper elementary school grades can receive HPV vaccine in Japan. | 27 (69.2%) | 69 (56.1%) |
| HPV vaccine can prevent more than 50% of CC in Japan. | 31 (79.5%) | 97 (78.9%) |
| WHO recommends HPV vaccine. |
33 (84.6%) |
96 (78.0%) |
| Knowledge of adverse events of HPV Vaccine | ||
| Some people complain of muscle pain after injection of the HPV vaccine. | 34 (87.2%) | 111 (90.2%) |
| Syncope occurs after HPV vaccination. | 31 (79.5%) | 106 (86.2%) |
| Motility disturbance and severe pain are observed in unvaccinated young people in Japan. | 20 (51.3%) | 74 (60.2%) |
| Vaccination of an HPV-infected person does not have a negative effect. | 34 (87.2%) | 82 (66.7%) |
| The rate of severe adverse effects of the HPV vaccine is <10/100,000 people. | 15 (38.5%) | 41 (33.3%) |
HPV: human papillomavirus, WHO: World Health Organization.
Phase 2: development of educational slide sets on HPV vaccine
The link for the developed educational slides is as follows: http://www.pf.chiba-u.ac.jp/documents/FY2019/20190507_ishiwada.pdf. The slide sets include general information on the HPV vaccination process, HPV vaccine, and how HSTs should construct their way of thinking about the risks and benefits of HPV vaccination.
Phase 3: secondary survey
Through data analysis, it was found that, among the 162 HSTs, 8.6% (14/162) had received the HPV vaccine. In terms of evaluation of participants’ understanding of HPV vaccination, the average collected scores before and after the lecture were 13.9 points (Median: 14 points, [7.02–19.98]) and 16.2 points (Median: 17 points, [12.30–21.70]), respectively. The scores after the lecture [15.8–16.6] significantly increased compared to the scores before the lecture [13.4–14.4] (p < .0001).
In terms of feelings regarding the HPV vaccine, the number of HSTs who felt uncertain and fearful regarding the HPV vaccine decreased significantly after the lecture compared to that before the lecture (Figure 1). Concerning their intention to recommend HPV vaccination to their female students, the number of HSTs who answered “recommend” and “tend to recommend” HPV vaccine to their students and/or guardians increased significantly after the lecture compared to that before the lecture (Figure 2).
Figure 1.
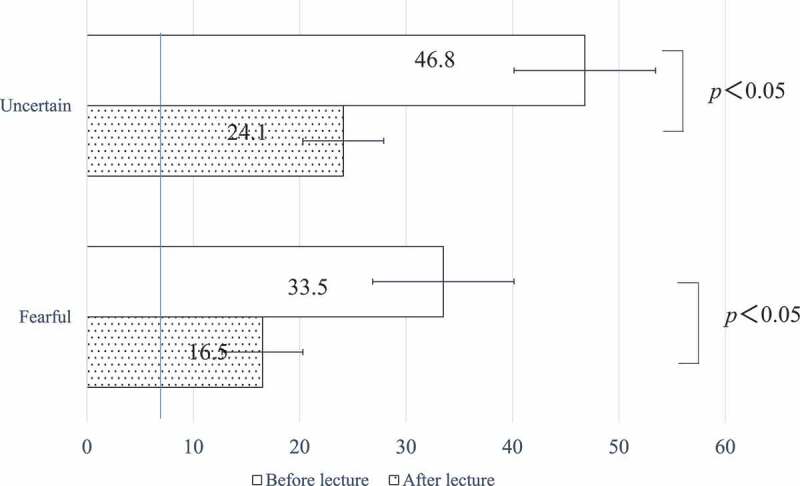
Changes in feelings about HPV vaccination before and after the lecture
The number of HSTs who feel uncertain and fearful about HPV vaccination significantly decreased after the lecture compared to before it.
Figure 2.
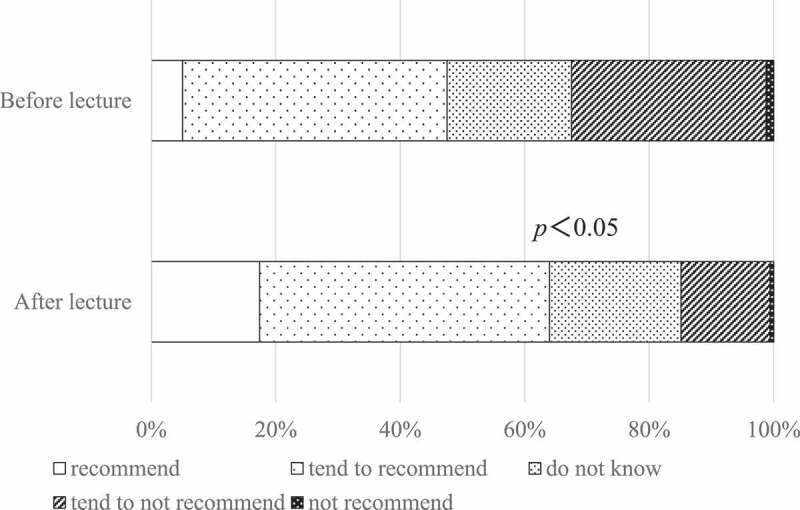
HSTs’ intention to recommend HPV vaccination to their students and/or students’ guardians. The number of HSTs who recommend and tend to recommend HPV vaccine to their students and/or guardians significantly increased after the lecture compared to before it
Discussion
Data analysis discussions and hypothesis confirmation
According to our study, many HSTs acquired information on HPV from the internet. Kamada et al.17 recently conducted a self-administered survey on the perception of Japanese HSTs toward HPV vaccine to determine ways to increase their willingness to encourage its use. Their results showed that most respondents had inadequate knowledge about cervical cancer and HPV vaccine and that they mostly wanted accurate proof of the preventive effects of the vaccine on cervical cancer in Japan. Moreover, it is believed that, after the temporary withdrawal of the active government recommendation for HPV vaccines, media reports strongly influenced confidence in the HPV vaccine among Japanese people.10,18 Therefore, to improve the prevalence of adolescent HPV vaccination in Japan, it is also necessary to introduce an effective educational system for HSTs.19
Regarding the primary survey, the knowledge of HSTs was lacking on some aspects of the HPV vaccine, especially related to the infection route of HPV, appropriate prevention of cervical cancer, and rate of adverse events of HPV vaccine, and they misunderstood the safety and effectiveness of the HPV vaccine. University students were included as a subgroup in the survey used in another recent study.20 We also conducted a primary survey with university students taking the HST training course, and almost all of them wanted to be immediately involved in school health education after graduation. In terms of their knowledge of HPV vaccine, the scores of HSTs were higher than those found among the university students, except for two questions related to adverse events. However, the proportion of university students who felt fearful of HPV vaccination was lower than that of HSTs, and we hypothesized that this might be related to the high HPV immunization rate in university students before the suspension of the active governmental recommendation for the HPV vaccine. Thus, through this primary survey, we could ascertain the awareness of HSTs and identify the current status, issues, and barriers regarding HPV vaccination.
This study hypothesized that improving HSTs’ knowledge and understanding regarding the risks and benefits of the HPV vaccine through educational lectures using appropriate materials could improve HSTs vaccine confidence, consequently improving recommendation rates for the vaccine for their female students. This hypothesis was verified by the secondary survey results. The rates of HSTs’ intention to recommend the HPV vaccine to their female students statistically increased after the lecture compared to before it. However, further relevant discussion regarding this is necessary.
Comparison and discussion between HSTs’ and school nurses’ role related to HPV vaccination
In other countries, school nurses, instead of HSTs, are expected to be the key health-care professionals who provide relevant and instructive information about HPV and HPV vaccination to students and their guardians, ultimately promoting HPV vaccination for youth.21–23 Therefore, to enhance this discussion, we refer to studies that have promoted HPV vaccination in educational programs for school nurses in other countries, as the HSTs profession is unique to Japan.
In Sweden, Grandahl et al.24 conducted a survey to investigate school nurses’ attitudes toward and experiences of HPV vaccination before and after the implementation of the national HPV vaccination program. According to their study, school nurses had a more favorable attitude toward the vaccination program against HPV after the national vaccination program than that before it, and school nurses believed that they needed more education about HPV.
Additionally, an online survey in the United States also revealed that school nurses had relevant knowledge about HPV and its vaccine, and positive attitudes toward the HPV vaccination, though HPV vaccination rates remain low. However, in contrast to our findings, school nurses in the US had unenthusiastic perceptions of their role as leaders promoting the vaccine and implemented few activities related to providing vaccine information. Through this online survey, it was found that, in order to enhance school nurses’ practice related to the HPV vaccine, focus should be placed on increasing positive attitudes toward the vaccine and strengthening perceptions of their role as leaders in promoting the vaccine.25
In terms of the educational method chosen to improve knowledge regarding the HPV vaccine, Rhodes et al. reported the usefulness of short, online educational training for busy school nurses in the US.26 On the other hand, in another study, the same authors pointed out that positive attitudes and adequate knowledge levels were found in school nurses in the US, but the majority of them did not provide information and resources to the students’ parents. Thus, they recommended targeted health promotion programs for school nurses in the US,27 which corroborates the results of their previous study mentioned. With that and our results in mind, we found that knowledge is essential, but was not the strongest predictor of HPV vaccination promotion, as recognizing themselves as opinion leaders (for school nurses and HSTs alike) is the strongest predictor of positive attitudes toward HPV vaccine. Thus, based on the current and other studies, it was found that school nurses need additional professional development to increase their HPV vaccine knowledge and attitudes to encourage parents and adolescents to consider the uptake of HPV vaccination.28
As noted earlier, HSTs’ knowledge and attitudes are important to promote the uptake of HPV vaccination in female students in Japan. However, our study revealed that the knowledge of HPV and HPV vaccine of Japanese HSTs was insufficient, which contrasts other studies in the US with school nurses (mentioned previously in this discussion), as the latter already had strong knowledge on the topic. However, when considering the Japanese situation, despite the very low HPV immunization rates in adolescents, more than 50% of HSTs tended to recommend HPV vaccine before the lecture.
In terms of limitations, this study had a limited sample size in a limited area because it utilized a face-to-face lecture approach and not e-learning lectures. This was the case because face-to-face lectures are easier to conduct and could immediately resolve the participants’ concerns and doubts compared to a lecture conducted over the internet. Further studies should provide a wider sample approach in terms of methodological choices to improve generalizability of the findings.
On the other hand, this study was unique because medical doctors collaborated with HSTs to try and address the important issue of HPV immunization in Japan, which is unprecedented in academic research on this topic as far as we know.
Conclusion
In conclusion, to improve the situation of adolescent HPV vaccination in Japan, it is necessary to introduce an effective educational system for HSTs. However, HSTs did not have access to adequate educational lectures related to the HPV vaccine and specifically crafted for this professional group prior to this study. Thus, we believe that our slide sets on HPV vaccine for HSTs could be widely utilized in Japan to promote awareness among female students through their HSTs in Japanese schools. As the next step, we will plan a subsequent study to evaluate the direct effects of the use of our developed materials by HSTs in their own lectures on female students’ willingness to receive HPV vaccines.
Supplementary Material
Acknowledgments
We thank all participants for taking the time to answer this survey.
Funding Statement
This work was supported by the MSD research fund (V501-IIS-57364).
Disclosure of potential conflicts of interest
This study was funded as an investigator-initiated study program by Merck, Sharp, & Dohme Corp./MSD K.K. The funder had no role in the design or conduct of study, the collection, analysis, or interpretation of data, nor in the preparation, review, or approval of the manuscript. The authors report no personal, political, commercial, financial, or academic conflicts of interest. All authors have approved the final article.
Supplementary material
Supplemental data for this article can be accessed online at http://dx.doi.org/10.1080/21645515.2020.1732163.
References
- 1.Saitoh A, Okabe N.. Progress and challenges for the Japanese immunization program: beyond the “vaccine gap”. Vaccine. 2018;36:4582–88. doi: 10.1016/j.vaccine.2018.01.092. [DOI] [PubMed] [Google Scholar]
- 2.Hanley SJB, Yoshioka E, Ito Y, Kishi R. HPV vaccination crisis in Japan. Lancet. 2015;385:2571. doi: 10.1016/S0140-6736(15)61152-7. [DOI] [PubMed] [Google Scholar]
- 3.Suzuki S, Hosono A. No association between HPV vaccine and reported post-vaccination symptoms in Japanese young women: results of the Nagoya study. Papillomavirus Res. 2018;5:96–103. doi: 10.1016/j.pvr.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Konno R, Konishi H, Sauvaget C, Ohashi Y, Kakizoe T. Effectiveness of HPV vaccination against high grade cervical lesions in Japan. Vaccine. 2018;36:7913–15. doi: 10.1016/j.vaccine.2018.05.048. [DOI] [PubMed] [Google Scholar]
- 5.Kudo R, Yamaguchi M, Sekine M, Adachi S, Ueda Y, Miyagi E, Hara M, Hanley SJB, Enomoto T. Bivalent human papillomavirus vaccine effectiveness in a Japanese population: high vaccine-type-specific effectiveness and evidence of cross-protection. J Infect Dis. 2019;219:382–90. doi: 10.1093/infdis/jiy516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights though a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fu LY, Bonhomme LA, Cooper SC, Joseph JG, Zimet GD. Educational interventions to increase HPV vaccination acceptance: a systematic review. Vaccine. 2014;32:1901–20. doi: 10.1016/j.vaccine.2014.01.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taninami Y, Ujiie Y. Awareness survey of first-year students in the Yogo teacher training program of University A’s School of Education. Saitama Daigak Kiyou. 2015;64:1–5. In Japanese. [Google Scholar]
- 9.Matsumoto A, Nakatsuka M. Knowledge and attitudes of about cervical cancer, HPV infection and HPV vaccination. Adolescentology. 2012;30:143–54. In Japanese. [Google Scholar]
- 10.Ishino S, Kato H. Health education on cervical cancer prevention desired by parents. Boseieisei. 2016;57:115–22. In Japanese. [Google Scholar]
- 11.Ishino S, Kato H, Matsuda H. Research on awareness of HPV vaccine and health education in Japanese Yogo teachers. Hokennokagaku. 2012;54:849–55. In Japanese. [Google Scholar]
- 12.Saito M, Kimura Y. Awareness of HPV vaccination by Yogo teacher of public high-schools and junior high-schools in the metropolitan area. Shishunkigaku. 2015;33:334–39. In Japanese. [Google Scholar]
- 13.Japanese Ministry of Health, Labour and Welfare . HPV infection. [accessed 31October 2019] https://www.mhlw.go.jp/bunya/kenkou/kekkaku-kansenshou28/index.html.
- 14.Coyle E You are the key to HPV cancer prevention. American Cancer Society; 2018. [accessed 26September 2019]. http://healthinfo.montana.edu/health-wellness/YouAreTheKey_5_10_18.pdf
- 15.NHS UK . HPV Vaccine overview. [accessed 31October 2019]. https://www.nhs.uk/conditions/vaccinations/hpv-human-papillomavirus-vaccine/
- 16.ICO Information Centre on HPV and Cancer . 2017. [accessed 31October 2019]. https://www.hpvcentre.net/.
- 17.Kamada M, Inui H, Kagawa T, Mineda A, Tamura T, Fujioka T, Motoki T, Hirai H, Ishii E, Irahara M. What information can change the attitude of teachers toward the human papillomavirus vaccine? J Obstetric Gynaecol Res. 2018;44:778–87. doi: 10.1111/jog.13584. [DOI] [PubMed] [Google Scholar]
- 18.Tsuda K, Yamamoto K, Leppold C, Tanimoto T, Kusumi E, Komatsu T, Kami M. Trends of media coverage on human papillomavirus vaccination in Japanese newspapers. Clin Infect Dis. 2016;63:1634–38. doi: 10.1093/cid/ciw647. [DOI] [PubMed] [Google Scholar]
- 19.Teruya N, Sunagawa Y. Current situation and challenges for junior high and high school nurses in conducting education and raising awareness regarding cervical cancer prevention. Ryukyu Med. 2016;35:21–30. In Japanese. [Google Scholar]
- 20.Suzuki Y, Sukegawa A, Nishikawa A, Kubota K, Motoki Y, Asai-Sato M, Ueda Y, Sekine M, Enomoto T, Hirahara F, et al. Current knowledge of and attitudes toward human papillomavirus-related disease prevention among Japanese: a large-scale questionnaire study. J Obstetric Gynaecol Res. 2019;45:994–1005. doi: 10.1111/jog.13929. [DOI] [PubMed] [Google Scholar]
- 21.Lockwood-Rayermann S, McIntyre SJ. Understanding HPV disease and prevention: a guide for school nurses. J Sch Nurs. 2009;25:261–69. doi: 10.1177/1059840509333787. [DOI] [PubMed] [Google Scholar]
- 22.Boyce T, Holmes A. Addressing health inequalities in the delivery of the human papillomavirus vaccination programme: examining the role of the school nurse. PLoS One. 2012;7:e43416. doi: 10.1371/journal.pone.0043416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosen B, Goodson P. A recommendation to use the diffusion of innovations theory to understand school nurses’ role in HPV vaccine uptake. Int Q Community Health Educ. 2014;34:37–49. doi: 10.2190/IQ.34.1.d. [DOI] [PubMed] [Google Scholar]
- 24.Grandahl M, Larsson M, Tydén T, Stenhammar C. School nurses’ attitudes towards and experiences of the Swedish school-based HPV vaccination programme - A repeated cross sectional study. PLoS One. 2017;12:e0175883. doi: 10.1371/journal.pone.0175883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosen BL, Goodson P, Thompson B, Wilson KL. School nurses’ knowledge, attitudes, perceptions of role as opinion leader, and professional practice regarding human papillomavirus vaccine for youth. J Sch Health. 2015;85:73–81. doi: 10.1111/josh.12229. [DOI] [PubMed] [Google Scholar]
- 26.Rhodes D, Visker JD, Cox C, Sas A, Banez JC. Effects of an online educational module on school nurses’ knowledge of HPV vaccination. J Continuing Educ Nurs. 2017;48:431–36. doi: 10.3928/00220124-20170816-10. [DOI] [PubMed] [Google Scholar]
- 27.Rhodes D, Visker J, Cox C, Forsyth E, Woolman K. Public health and school nurses’ perceptions of barriers to HPV vaccination in Missouri. J Community Health Nurs. 2017;34:180–89. doi: 10.1080/07370016.2017.1369806. [DOI] [PubMed] [Google Scholar]
- 28.Rosen BL, DiClemente R, Shepard AL, Wilson KL, Fehr SK. Factors associated with school nurses’ HPV vaccine attitudes for school-aged youth. Psychol Health Med. 2017;22:535–45. doi: 10.1080/13548506.2016.1173710. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Japanese Ministry of Health, Labour and Welfare . HPV infection. [accessed 31October 2019] https://www.mhlw.go.jp/bunya/kenkou/kekkaku-kansenshou28/index.html.


