Abstract
Background
To investigate the effect of the corona virus disease 2019 (COVID-19) pandemic on the acute treatment of patients with ST-segment elevation (STEMI) and Non-ST-segment elevation acute coronary syndrome (NSTE-ACS).
Methods
We retrospectively identified patients presenting to the emergency department (ED) with suspected ACS. We evaluated the number of percutaneous coronary interventions (PCIs) for STEMI, NSTE-ACS, and elective PCI cases. In STEMI patients, we assessed the time from chest pain onset (cpo) to ED presentation, post-infarction left ventricular ejection fraction (LVEF), and time from ED presentation to PCI. We directly compared cases from two time intervals: January/February 2020 versus March/April 2020 (defined as 2 months before and after the COVID-19 outbreak). In a secondary analysis, we directly compared cases from March/April 2020 with patients from the same time interval in 2019.
Results
From January to April 2020, 765 patients presented with acute chest pain to the ED. A dramatic reduction of ED presentations after compared to before the COVID-19 outbreak (31% relative reduction) was observed. Overall, 398 PCIs were performed, 220/398 PCIs (55.3%) before versus 178/398 PCIs (44.7%) after the outbreak. While numbers for NSTE-ACS and elective interventions declined by 21% and 31%, respectively, the number of STEMI cases remained stable. Time from cpo to ED presentation, post-infarction LVEF, and median door-to-balloon time remained unchanged.
Conclusions
In contrast to previous reports, our findings do not confirm the dramatic drop in STEMI cases and interventions in northwestern Switzerland as observed in other regions and hospitals around the world.
Keywords: COVID-19, Acute coronary syndromes, ST-segment elevation myocardial infarction, Non-ST-segment myocardial infarction, Non-ST-segment acute coronary syndrome (NSTE-ACS), Percutaneous coronary intervention, Switzerland, Health care system, Regulatory Authorities
1. Introduction
Acute chest pain as the main symptom of acute coronary syndrome (ACS) is still the leading cause for emergency department (ED) presentations worldwide [1]. Several advantages in early diagnosis and accurate treatment of ST-elevation myocardial infarction (STEMI) and non ST-elevation acute coronary syndrome (NSTE-ACS) have led to a decrease in short and long-term mortality, e.g. by a more frequent use of reperfusion therapy, primary percutaneous coronary intervention (PCI), modern antithrombotic therapy, and secondary prevention. Furthermore, increased public awareness of how to recognize symptoms of ACS and the importance of timely activation of emergency services contributed to a reduction of delay from first medical contact to rapid STEMI and NSTE-ACS diagnosis and early transfer to the catheter laboratory for potential revascularization.
Since December 2019, the emergence of the coronavirus disease 2019 (COVID-19) has evolved into a global pandemic with a massive impact on health care systems worldwide. Several reports from Italy, Spain, Hong Kong, Austria, France, Germany, and the United States [2], [3], [4], [5], [6], [7] revealed a relevant increase in delay from symptom onset to first medical contact [4] and a decline in cardiac catheterization laboratory activation for patients with ACS [2], [3], [5], [6]. Most of these regions and countries are moderately affected by COVID-19 with incidence rates of positive confirmed cases from 77 to 450 per 100.000 inhabitants as provided in online resources on April 30th, as compared to Lombardy or New York with 771 and 1.868 confirmed cases per 100.000 inhabitants, respectively. The University Hospital Basel is located in the northwestern part of Switzerland at the border triangle with France and Germany and serves a population of approximately 500.000 inhabitants. The Cardiology Department is providing 24/7 service for PCI capacities for urgent cases. On April 30th, this region reported 361 confirmed COVID-19 cases per 100.000 inhabitants.
The aim of this report was to investigate the absolute number of PCIs for STEMI, NSTE-ACS, and elective PCI cases and to assess the time from ED presentation to PCI in STEMI patients as a marker of workflow efficiency before and after the COVID-19 outbreak. Furthermore, we analyzed time from chest pain onset to emergency department presentation and post-infarction left ventricular ejection fraction in STEMI patients. In addition, we compared overall numbers to those observed in 2019.
2. Materials and methods
2.1. Study design and population
This was a retrospective single-center study performed at a tertiary University Hospital in northwestern Switzerland. The aim of this study was to investigate the effect of the COVID-19 pandemic on the patient flow of patients with suspected ACS and the number of performed PCIs before and after the COVID-19 outbreak.
We retrospectively identified all consecutive patients presenting to the ED of the University Hospital Basel with symptoms suggestive of ACS between January and April 2020 (primary analysis) as well as during March/April 2019 (secondary analysis). Patients were included irrespective of age, sex, ethnicity, time since chest pain onset or peak, or renal function. The study was carried out according to the principles of the Declaration of Helsinki. As this was a retrospective study solely using clinical demographic and no study-specific data, no approval by the local ethics committee was needed. All patients were asked to sign the general consent of the University Hospital Basel and, therefore, no study-specific written informed consent was obtained. For this analysis, we excluded patients who explicitly declined to sign the general consent. The authors designed the study, gathered, analyzed the data, and decided to submit the manuscript for possible publication.
2.2. Statistical analysis
Normally distributed continuous variables are described as mean with standard deviation (SD) and non-normally distributed variables as median with interquartile range (IQR), while categorical variables are expressed as numbers and percentages. Differences between groups were assessed using the Mann-Whitney U test for continuous variables and the Pearson Chi-square or Fishers s exact test for categorical variables, as appropriate. All hypothesis testing was two-tailed and p-values < 0.05 were considered statistically significant. Statistical analyses were performed using IBM SPSS Statistics for Windows, version 26.0 (SPSS Inc, Chicago, IL).
3. Results
3.1. Emergency department presentations
Starting March 1st 2020, social life was significantly affected, and social distancing was recommended by the Swiss Federal Government. A national lockdown, however, without requirement to carry an exemption form to leave home and without fines, followed on March 16th. Medical facilities were also increasingly affected from this time point on until April 27th, when procedures for purely elective cases were allowed to resume.
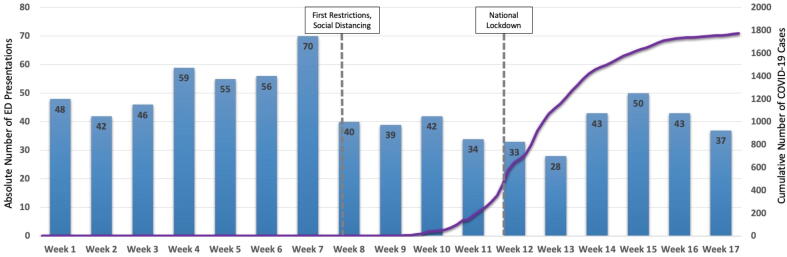
From January 2020 to April 2020, 765 patients presented to the ED with acute chest pain, a mean of 45 patients per week. Compared to January/February 2020, we observed a dramatic reduction of ED presentations after the COVID-19 outbreak on March 1st (31% relative reduction; Fig. 1). Furthermore, from January to April 2019, 1137 patients presented to the ED (absolute change of +372 patients and relative change of +32.7% compared to 2020). In the months March/April 2019 versus March/April 2020, 550 and 337 patients presented to the ED, respectively (absolute change of −213 patients and relative change of −38.7%).
Fig. 1.
Absolute number of patients with acute chest pain presenting to the emergency department. Absolute numbers of patients with acute chest pain presenting to the ED in 2020 per calendar week are displayed on the left y-axis as blue boxes and cumulative numbers of confirmed COVID-19 cases per day are displayed on the right y-axis as purple line. The first gray vertical line indicates the begin of social distancing regulations and other restrictions, the second line indicates the national lockdown. COVID-19 denotes corona virus disease 2019. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.2. Overall number of performed percutaneous coronary interventions
From January 2020 to April 2020, a total of 398 PCIs were performed. Baseline characteristics of the patients who underwent PCI before and after the COVID-19 outbreak are shown in Table 1. Overall, 220/398 PCIs (55.3%) were performed before the COVID-19 outbreak and 178/398 PCIs (44.7%) during the following 2 months. The number of cases were similar in the same period in 2019, when 405 PCIs had been performed (Fig. 2A + B).
Table 1.
Baseline characteristics of the patients.
| All patients with PCI between January and April 2020 |
Patients with PCI January/February 2020 |
Patients with PCI March/April 2020 |
p-value | |
|---|---|---|---|---|
| (n = 398) | (n = 220) | (n = 178) | ||
| Age – years (IQR) | 68 (59–76) | 68 (59–76) | 66 (56–76) | 0.138 |
| Female gender – no. (%) | 91 (22.9) | 51 (23.2) | 40 (22.5) | 0.867 |
| Risk factors – no. (%) | ||||
| Hypertension | 226 (56.8) | 139 (63.2) | 87 (48.9) | 0.004 |
| Hypercholesterolemia | 286 (71.9) | 160 (72.7) | 126 (70.8) | 0.669 |
| Diabetes | 116 (29.1) | 67 (30.5) | 49 (27.5) | 0.523 |
| Smoking | 217 (54.5) | 126 (57.3) | 91 (51.1) | 0.221 |
| History – no. (%) | ||||
| Coronary artery disease | 0.640 | |||
| 1-vessel disease | 115 (28.9) | 64 (29.1) | 51 (28.7) | – |
| 2-vessel disease | 145 (36.4) | 76 (34.5) | 69 (38.8) | – |
| 3-vessel disease | 138 (34.7) | 80 (36.4) | 58 (32.6) | – |
| Body mass index (kg/m2) | 26.8 (24.5–29.8) | 26.7 (24.2–29.9) | 27.0 (24.8–29.4) | 0.719 |
| Laboratory findings | ||||
| Creatinine clearance (mL/min/m2) | 84.0 (65.0–94.0) | 84.0 (66.0–93.0) | 85.0 (63.0–95.0) | 0.623 |
| White Blood Count (×109/L) | 9.0 (6.9–11.8) | 8.9 (6.5–11.7) | 9.3 (7.4–11.9) | 0.079 |
| CRP (mg/L) | 2.1 (0.8–5.4) | 1.9 (0.8–5.1) | 2.3 (0.8–5.6) | 0.681 |
| Troponin T Baseline (ng/L) | 60.0 (16.0–435) | 48.0 (15.0–380) | 82.5 (18.0–820) | 0.149 |
| Troponin T Peak (ng/L) | 515.5 (33.0–3411) | 310 (27.0–2862) | 851 (50–4915) | 0.024 |
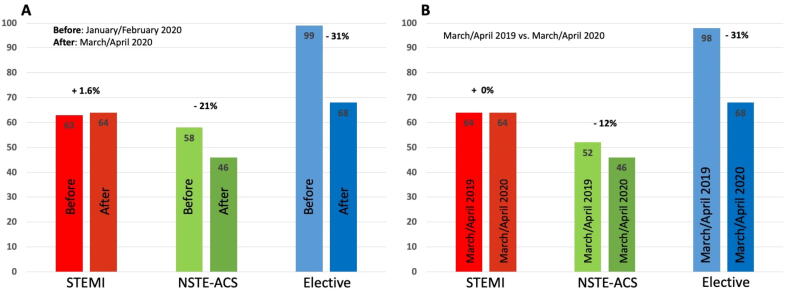
Fig. 2.
A + B. Absolute numbers of percutaneous coronary interventions before and after the COVID-19 outbreak. (A) Absolute numbers of PCI’s for STEMI (red), NSTE-ACS (green) and elective cases (blue) before and after the COVID-19 outbreak and (B) during March/April 2019 versus March/April 2020. PCI denotes percutaneous coronary intervention; STEMI denotes ST-segment elevation myocardial infarction; NSTE-ACS denotes non-ST-segment elevation acute coronary syndrome; COVID-19 denotes corona virus disease 2019. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.3. Number of percutaneous coronary interventions in NSTE-ACS and elective patients
The absolute number of PCIs in NSTE-ACS patients and elective interventions declined from 58 to 46 (reduction of 21%) and from 99 to 68 (reduction of 31%) before and after the COVID-19 outbreak, respectively (Fig. 2A). In the secondary analysis, nearly identical findings occurred. NSTE-ACS and elective cases dropped from 52 to 46 (reduction of −12%) and from 98 to 68 (reduction of −31%), respectively (Fig. 2B).
3.4. Number of percutaneous coronary interventions in STEMI patients
We did not observe an impact of the COVID-19 outbreak on the absolute numbers of PCIs in STEMI cases. The number remained stable with 63 cases before the COVID-19 outbreak versus 64 cases in the following two months (Fig. 2A). In the secondary analysis, we found an identical number of performed PCIs in STEMI patients in the corresponding months in 2019 (64 cases; Fig. 2B).
3.5. Time from chest pain onset to emergency department presentation in STEMI patients
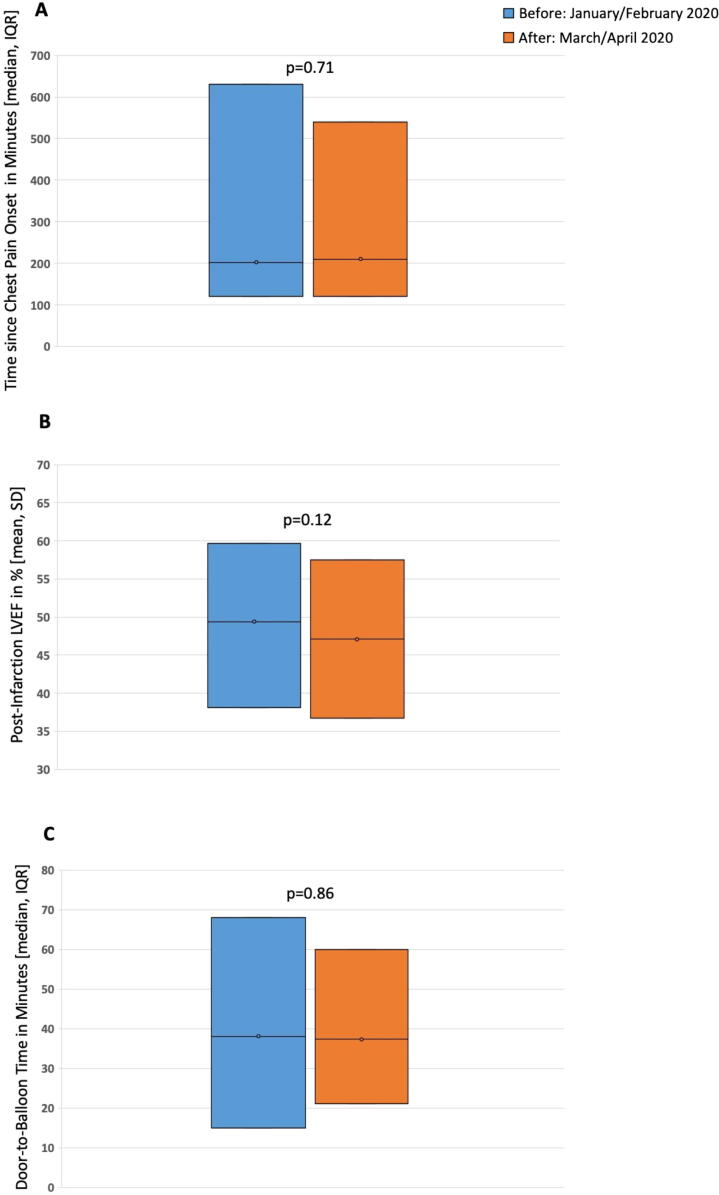
Time from chest pain onset to ED presentation in STEMI patients was nearly similar before versus after the outbreak (202 min [IQR 120–630] vs. 210 [IQR 120–540]; p = 0.71; Fig. 3A). Comparable findings emerged in the secondary analysis with a median time of 180 min (IQR 120–360) in March/June 2019 compared to 210 min (IQR 120–540; p = 0.19) in the after COVID-19 outbreak period in 2020.
Fig. 3.
Time from chest pain onset to emergency department presentation, post-infarction left ventricular ejection fraction, and median door-to-balloon time in STEMI patients before and after the COVID-19 outbreak. (A) Time from chest pain onset to emergency department presentation, (B) post-infarction left ventricular ejection fraction, and (C) median door-to-balloon time in STEMI patients before (blue) and after (orange) the COVID-19 outbreak. Boxes represent either median times and interquartile range (IQR) or mean and standard deviation (SD). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.6. Post-infarction left ventricular ejection fraction in STEMI patients
Before and after the COVID-19 outbreak, STEMI patients had similar post-infarction LVEF (49.4% [SD 11.3] vs. 47.1% [SD 10.4]; p = 0.12; Fig. 3B). Again, similar findings were observed in the secondary analysis (50.7% [9.62] vs. 47.1% [SD 10.4]; p = 0.05).
3.7. Door-to-balloon time in STEMI patients
Median door-to-balloon time in STEMI patients remained stable with a median time of 38 min (IQR 15–68) versus 37 min (IQR 21–60, p = 0.856) before and after the COVID-19 outbreak (Fig. 3C).
4. Discussion
In this retrospective single-center study, we investigated the effect of the COVID-19 pandemic on patient flow and the acute treatment of patients with STEMI, NSTE-ACS and elective PCIs at a tertiary University Hospital in northwestern Switzerland.
We report four major findings: First, we observed a 31% relative reduction of patients presenting to the ED with chest pain after the COVID-19 outbreak on March 1st. Second, we found a decrease in the number of overall performed PCIs before versus after the COVID-19 outbreak (55.3% versus 44.7%). However, the overall number of performed PCIs was similar as compared to the same time period in 2019. Third, the absolute number of PCIs in NSTE-ACS patients and elective interventions declined from 58 to 46 (reduction of 21%) and from 99 to 68 (reduction of 31%) before and after the COVID-19 outbreak, respectively. This finding was consistent when comparing the numbers of the post outbreak months to the same time period in 2019. Fourth, and of most importance, we did not observe an impact of the COVID-19 outbreak on the absolute numbers of PCIs in STEMI cases. Additionally, time from chest pain onset to ED presentation, post-infarction LVEF, and median door-to-balloon remained unchanged after the COVID-19 outbreak.
While our findings regarding the number of NSTE-ACS and elective cases are well in line with previous reports[2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], this is the first detailed report on chest pain patients referred to a large tertiary University Hospital in Europe, which is not in line with prior reports regarding STEMI cases. Most other regions reported a relative decline of PCIs, STEMI or ACS presentations ranging from 18% to 40% (e.g., western part of France 18%, Campania, Italy 32%, northeastern part of the United States 38%, Austria 39% and Spain 40%) [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12]. It was hypothesized that patients may be reluctant to seek medical care during the COVID-19 pandemic because they were concerned of becoming infected, violating social distancing regulations, or believing that medical care is not available. One Chinese study suggested that STEMI patients are delaying seeking medical care during the pandemic by waiting nearly 6 h compared to 1.5 h [4].
Beyond this, our findings provide additional insights in this important field. While we found a relevant decline of 31% and 21% for elective and NSTE-ACS PCIs and a 31% decrease in acute chest pain presentations to our ED, the numbers of PCIs for STEMI remained stable before and after the COVID-19 outbreak. Furthermore, in contrast to previous reports that found a longer average door-to-balloon time (88 versus 53 min, p = 0.03) in post COVID-19 patients [14], median door-to-balloon time was short and remained stable in our study. These findings can at least in part be explained by well-prepared standard operating procedures, including an immediate preparation of the catheter laboratory according to internal safety guidelines in cases of suspected COVID-19 in ACS patients, and a predefined patient pathway from the ED to the catheter laboratory. Additionally, it seems that our well-established ED workflow with, for example, a designated COVID-19 ward in the ED with specialized personnel, were still able to allocate sufficient resources to STEMI patients.
Recently, the European Society of Cardiology (ESC) administered an online questionnaire to cardiovascular specialists (cardiologists and cardiovascular nurses) across 6 continents [15]. Nearly 80% responded that the number of STEMI patients was reduced since the COVID-19 outbreak and 65.2% indicated that the reduction in STEMI presentations was > 40%. Additionally, about 60% of all respondents reported a delay in ED presentation among STEMI patients and that > 40% presented beyond the optimal window for PCI or thrombolysis [15]. In contrast, we did not observe a significantly later presentation of STEMI patients after the COVID-19 outbreak as compared to the time until ED presentation before the outbreak.
Our data suggest, however, that primarily patients with non-cardiac causes of chest pain and NSTE-ACS avoided presentation to the ED, whereas patients with STEMI continued presenting to the hospital. Furthermore, in contrast to previous trials, we found that the time from chest pain onset to ED presentation remained stable after the COVID-19 outbreak. The reasons for this different behavior of patients as compared to several other countries and regions similarly affected by COVID-19, where a relevant decline in STEMI cases and delayed presentation has been reported, is unclear. Explanations might be a high level of confidence in the healthcare system and high awareness of the public regarding acute and severe chest pain symptoms due to proactive information by official authorities, professional societies, and media campaigns, but this remains hypothetical.
Besides the impact of COVID-19 on ED presentations and performed PCIs, previous trials have shown that patients with COVID-19 are at higher risk for thrombotic and thromboembolic disease as well as bleeding complications [16], [17]. Both direct and indirect effects of COVID-19, such as severe inflammatory response, critical illness, and the presence of traditional risk factors may predispose to thrombotic and thromboembolic events [17]. In COVID-19 patients undergoing PCI, the well-validated high bleeding risk criteria, as proposed by consensus by the Academic Research Consortium, might also be of benefit to identify patients at high bleeding risk [18], [19].
The main limitation of our study is its retrospective design and the fact that we report data from a single center. However, previous studies investigating the impact of COVID-19 on ACS cases and treatments were also retrospective reports.
5. Conclusion
In conclusion, the decrease in use of emergency services in life-threatening situations such as STEMI that was observed in several regions and hospitals around the world did not occur in northwestern Switzerland. This may be due to the high standard of the healthcare system and proactive information with regards to availability of hospital beds and intensive care capacities and thus encouragement to seek medical assistance in life-threatening situations such as STEMI.
6. Statement on funding sources and conflicts of interest
We disclose that Dr. Boeddinghaus received research grants from the University of Basel, the University Hospital of Basel and the Division of Internal Medicine, the Swiss Academy of Medical Sciences, the Gottfried and Julia Bangerter-Rhyner-Foundation, and speaker honoraria/consulting honoraria from Siemens, Roche Diagnostics, Ortho Clinical Diagnostics, and Quidel Corporation, all outside of the submitted work.
Dr. Nestelberger has received research support from the Swiss National Science Foundation (P400PM_191037/1), the Prof. Dr. Max Cloëtta Foundation, the Margarete und Walter Lichtenstein-Stiftung (3MS1038), the University Hospital Basel, and the University of Basel, as well as speaker honoraria/consulting honoraria from B. Braun Melsungen AG, Siemens, Beckman Coulter, Bayer, Ortho Clinical Diagnostics and Orion Pharma, all outside the submitted work.
Dr. Twerenbold has received research support from the Swiss National Science Foundation (P300PB_167803), the Swiss Heart Foundation, the Swiss Society of Cardiology, the Cardiovascular Research Foundation Basel, the University of Basel and the University Hospital Basel and speaker honoraria/consulting honoraria from Abbott, Amgen, Astra Zeneca, Roche, Siemens, Singulex and Thermo Scientific BRAHMS, all outside the submitted work.
Dr. Jeger has received research support from the Swiss National Science Foundation, the Basel Cardiovascular Research Foundation, and B Braun Medical AG Switzerland, and speaker honoraria from B. Braun Melsungen AG and Cardionovum, all outside the submitted work.
Dr. Kaufmann reports research grants from the Swiss National Science Foundation (310030_169905), the Cardiovascular Research Foundation Basel and from Eli Lilly outside of the submitted work.
Dr. Mueller has received research support from the Swiss National Science Foundation, the Swiss Heart Foundation, the KTI, the Stiftung für kardiovaskuläre Forschung Basel; Abbott, Alere, Astra Zeneca, Beckman Coulter, Biomerieux, Brahms, Roche, Siemens, Singulex, Sphingotec, and the Department of Internal Medicine, University Hospital Basel, as well as speaker honoraria/consulting honoraria from Abbott, Alere, Astra Zeneca, Biomerieux, Boehringer Ingelheim, BMS, Brahms, Cardiorentis, Novartis, Roche, Siemens, and Singulex, all outside the submitted work.
Dr. Sticherling reports research grants from Biosense-Webster and lecture fees from Abbott, Medtronic, Biosense-Webster, Boston Scientific, Microport, and Biotronik, all outside of the submitted work.
Dr. Kühne has received grants from the Swiss National Science Foundation (Grant numbers 33CS30_148474, 33CS30_177520, 32473B_176178), the Swiss Heart Foundation, personal fees from Bayer, personal fees from Böhringer Ingelheim, personal fees from Pfizer BMS, personal fees from Daiichi Sankyo, personal fees from Medtronic, personal fees from Biotronik, personal fees from Boston Scientific, personal fees from Johnson&Johnson, grants from Bayer, grants from Pfizer BMS, grants from Boston Scientific, all outside the submitted work.
All other authors declare that they have no conflict of interest with this study. The authors designed the study, analyzed the data, prepared the manuscript, and decided to submit the manuscript for publication. All authors have read and approved the manuscript. The manuscript and its contents have not been published previously and are not being considered for publications elsewhere in whole or in part in any language, including publicly accessible web sites or e-print servers.
Acknowledgements
None.
References
- 1.Bingisser R., Dietrich M., Nieves Ortega R., Malinovska A., Bosia T., Nickel C.H. Systematically assessed symptoms as outcome predictors in emergency patients. Eur. J. Intern. Med. 2017;45:8–12. doi: 10.1016/j.ejim.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 2.Garcia S., Albaghdadi M.S., Meraj P.M., Schmidt C., Garberich R., Jaffer F.A. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J. Am. Coll. Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur. Heart J. 2020;41(19):1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tam C.-C.F., Cheung K.-S., Lam S., Wong A., Yung A., Sze M. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ. Cardiovasc. Qual. Outcomes. 2020;13(4) doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piccolo R., Bruzzese D., Mauro C., Aloia A., Baldi C., Boccalatte M. Population trends in rates of percutaneous coronary revascularization for acute coronary syndromes associated with the COVID-19 outbreak. Circulation. 2020 Jun 16;141(24):2035–2037. doi: 10.1161/CIRCULATIONAHA.120.047457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rangé G., Hakim R., Motreff P. Where have the ST-segment elevation myocardial infarctions gone during COVID-19 lockdown? Eur. Hear J. – Qual. Care Clin. Outcomes. 2020 doi: 10.1093/ehjqcco/qcaa034. 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scholz K.H., Lengenfelder B., Thilo C., Jeron A., Stefanow S., Janssens U. Impact of COVID-19 outbreak on regional STEMI care in Germany. Clin. Res. Cardiol. 2020 doi: 10.1007/s00392-020-01703-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.R. Moreno, J.J. Alonso, R. Caballero, E. del Corral, J. Elízaga, R.M. Asenjo, et al., Influence of age and gender on arrival of patients with ST-segment elevation acute myocardial infarction to tertiary centers during COVID-19 pandemic. Experience of Madrid, Spain, STEMI network (Codigo Infarto Madrid). Am. J. Emerg. Med. 2020 Jun 6.
- 9.Vecchio S., Fileti L., Reggi A., Moschini C., Lorenzetti S., Rubboli A. Impact of the COVID-19 pandemic on admissions for acute coronary syndrome: review of the literature and single-center experience. G Ital Cardiol (Rome). 2020;21(7):502–508. doi: 10.1714/3386.33635. [DOI] [PubMed] [Google Scholar]
- 10.De Rosa S., Spaccarotella C., Basso C., Calabrò M.P., Curcio A., Filardi P.P. OUP accepted manuscript. Eur. Heart J. 2020;41(22):2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abdelaziz H.K., Abdelrahman A., Nabi A., Debski M., Mentias A., Choudhury T. Impact of COVID-19 pandemic on patients with ST-segment elevation myocardial infarction: Insights from a British cardiac center. Am Heart J. 2020;11(226):45–48. doi: 10.1016/j.ahj.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.P. Kulkarni, M. Mahadevappa, COVID-19 pandemic and the reduction in ST-elevation myocardial infarction admissions. Postgrad Med J. 2020 Jun 10;postgradmedj-2020-137895. [DOI] [PMC free article] [PubMed]
- 13.U.N. Khot, A.P. Reimer, A. Brown, F.M. Hustey, M.S. Hussain, S.R. Kapadia, et al. Impact of COVID-19 Pandemic on Critical Care Transfers for ST-Elevation Myocardial Infarction, Stroke, and Aortic Emergencies. Circ Cardiovasc Qual Outcomes. 2020 Jun 11;CIRCOUTCOMES.120.006938. [DOI] [PubMed]
- 14.T.A. Hammad, M. Parikh, N. Tashtish, C.M. Lowry, D. Gorbey, F. Forouzandeh, et al., Impact of COVID‐19 pandemic on ST elevation myocardial infarction in a non‐COVID‐19 epicenter. Catheter Cardiovasc Interv. 2020;ccd.28997. [DOI] [PMC free article] [PubMed]
- 15.G. Pessoa-Amorim, C.F. Camm, P. Gajendragadkar, G.L. De Maria, C. Arsac, C. Laroche, et al., Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Hear J - Qual Care Clin Outcomes. 2020 May 28. [DOI] [PMC free article] [PubMed]
- 16.Al-Samkari H., Karp Leaf R.S., Dzik W.H., Carlson J.C.T., Fogerty A.E., Waheed A. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 2020;136(4):489–500. doi: 10.1182/blood.2020006520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bikdeli B., Madhavan M.V., Jimenez D., Chuich T., Dreyfus I., Driggin E. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2020;75(23):2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ueki Y., Bär S., Losdat S., Otsuka T., Zanchin C., Zanchin T. Validation of the Academic Research Consortium for High Bleeding Risk (ARC-HBR) criteria in patients undergoing percutaneous coronary intervention and comparison with contemporary bleeding risk scores. EuroIntervention. 2020 Aug 28;16(5):371–379. doi: 10.4244/EIJ-D-20-00052. [DOI] [PubMed] [Google Scholar]
- 19.Corpataux N., Spirito A., Gragnano F., Vaisnora L., Galea R., Svab S. Validation of high bleeding risk criteria and definition as proposed by the academic research consortium for high bleeding risk. Eur. Heart J. 2020;41(38):3743–3749. doi: 10.1093/eurheartj/ehaa671. [DOI] [PubMed] [Google Scholar]