Abstract
Study Design:
Break-even cost analysis.
Objective:
The goal of this study is to examine the cost-effectiveness of vancomycin powder for preventing infection following lumbar laminectomy.
Methods:
The product cost of vancomycin powder was obtained from our institution’s purchasing records. Infection rates and revision costs for lumbar laminectomy and lumbar laminectomy with fusion were obtained from the literature. A break-even analysis was then performed to determine the absolute risk reduction (ARR) in infection rate to make prophylactic application of vancomycin powder cost-effective. Analysis of lumbar laminectomy with fusion was performed for comparison.
Results:
Costing $3.06 per gram at our institution, vancomycin powder was determined to be cost-effective in lumbar laminectomy if the infection rate of 4.2% decreased by an ARR of 0.015%. Laminectomy with fusion was also determined to be cost-effective at the same cost of vancomycin powder if the infection rate of 8.5% decreased by an ARR of 0.0034%. The current highest cost reported in the literature, $44.00 per gram of vancomycin powder, remained cost-effective with ARRs of 0.21% and 0.048% for laminectomy and laminectomy with fusion, respectively. Varying the baseline infection rate did not influence the ARR for either procedure when the analysis was performed using the product cost of vancomycin at our institution.
Conclusions:
This break-even analysis demonstrates that prophylactic vancomycin powder can be highly cost-effective for lumbar laminectomy. At our institution, vancomycin powder is economically justified if it prevents at least one infection out of 6700 lumbar laminectomy surgeries.
Keywords: cost-benefit analysis, economic models, laminectomy, lumbar, vancomycin
Introduction
Infection following lumbar laminectomy with fusion is both devastating and costly.1 The average cost of revision following an infected lumbar laminectomy with fusion has recently been reported as $90 938.2 The rates of infection with different organisms following spine surgery vary by study; however, some of the most frequent organisms identified are gram-positive cocci including methicillin-resistant Staphylococcus aureus (MRSA) and Staphylococcus epidermidis.3 Increasing methicillin resistance has decreased the efficacy of intravenous cephalosporins as the standard preoperative antibiotic prophylaxis used in orthopedic procedures in general, and spine surgery in particular.3-5
Studies have reported that more than 60% of wound infection isolates in the United States are cephalosporin-resistant, including MRSA and coagulase-negative Staphylococcus. 6,7 Among orthopedic patients in the United States, 20% to 30% have anterior nares colonized by methicillin-sensitive S aureus (MSSA), and 2% to 6% are colonized by MRSA.8 Patients colonized preoperatively with MSSA face an added risk of surgical site infection 9 to 10 times greater than those who are not colonized, whereas patients preoperatively colonized with MRSA face an added risk of up to 4 times greater than those colonized with MSSA.8 The incidence of MRSA colonization among orthopedic patients is particularly concerning due to the virulent nature of the microbe. It not only poses a greater risk but is also more difficult to treat and, as a result, more expensive to the health care system.9 Rising prevalence of methicillin resistance and recognition of S aureus colonization as a modifiable risk factor for wound infection has resulted in a growing adoption of prophylactic antibiotic usage in spine surgery to prevent infection with S aureus and other gram-positive microbes.10,11
In particular, vancomycin powder has been added as a local application in wound beds for cardiac, vascular, spine, and a variety of other orthopedic procedures.10,11 The effect has been a demonstrable decrease in infection without any appreciable complications.12,13 Sweet et al found that the addition of vancomycin powder to traditional intravenous antibiotics reduced the deep infection rate after thoracic and lumbar instrumented spinal fusions from 2.6% to 0.2%, with no adverse clinical or wound complications.13 Other studies have found a decrease in infection from 15% to 0% with the addition of vancomycin powder in instrumented posterior cervical spine fusions and a decrease from 13% to 0% when vancomycin was added to posterior spinal fusions for trauma.14,15
The cost-effectiveness of vancomycin powder as a means of infection prophylaxis in lumbar laminectomy with fusion has been assessed in prior studies. In a retrospective review of 110 patients with traumatic spine injuries treated with instrumented posterior spine fusions over a 2-year period at a single institution, Godil et al16 found that vancomycin powder led to cost-savings of $438 165 per 100 spinal fusions performed, while Emohare et al17 found that their use of vancomycin powder in posterior instrumented spine surgery saved their hospital more than $500 000 over a 2-year span.
However, to our knowledge, no prior studies have examined the cost-effectiveness of vancomycin powder when utilized specifically for simple laminectomy without concomitant fusion. The goal of this study was to examine the cost-effectiveness of vancomycin powder in lumbar laminectomy without fusion using a simple break-even cost analysis that any spine surgeon can utilize to determine the exact economic viability of intraoperative vancomycin powder for their specific practice. This study also compared the cost-effectiveness of vancomycin powder for lumbar laminectomy in comparison to lumbar laminectomy with fusion to determine the degree to which the added fusion procedure changes the overall break-even economic calculations.
Materials and Methods
As an economic model for determining cost-effectiveness, we utilized a break-even analysis originally described by Hatch et al (Figure 1).18 This equation produces the final break-even infection rate necessary to make a protocol cost-effective, given the initial infection rate, the total cost of treating an infection, and the cost of a treatment or prevention protocol. These values were determined from the literature and our institution’s purchasing records. Calculating the difference between the initial and final infection rates yields the absolute risk reduction (ARR), which is the percent by which a protocol must reduce the infection rate to economically justify its use as a prophylactic measure. Clinicians can tailor this equation to their practice, by using their preferred method and institutional product costs, to determine the ARR of their given protocol.
Figure 1.
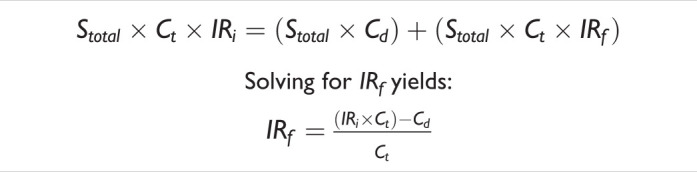
Equation used to calculate the break-even infection rate.
Where: Stotal = total annual surgeries; Ct = total cost of treating an infection; Cd = cost of drug; IRi = initial infection rate; IRf = breakeven infection rate. Adapted from Hatch et al.18
Prior studies have shown drastically different rates of both infection and cost of revision when comparing lumbar laminectomy with fusion to simple laminectomy alone. Reported literature values for baseline infection rates after lumbar laminectomy with fusion are 8.50%, while infection rates from lumbar laminectomy alone are 4.20%.2,19 The average total hospital cost of revision following infection after lumbar laminectomy with fusion has been reported as $90 938, while the total hospital cost of revision for infected lumbar laminectomy alone is much lower at $21 060.20,21 The product cost of vancomycin powder was obtained from our institution’s purchasing records and was found to be $3.06 per gram. Within the literature, the cost of vancomycin powder was found to range from $2.50 to $44.13,16-18,22,23
Results
Costing $3.06 per gram at our institution, vancomycin powder was determined to be cost-effective in lumbar laminectomy if the infection rate of 4.2% decreased by an ARR of 0.015% (Table 1). Laminectomy with fusion was determined to be cost-effective at the same cost of vancomycin powder if the infection rate of 8.5% decreased by an ARR of 0.0034%. The current highest cost of vancomycin reported in the literature, $44.00 per gram, was cost-effective with ARRs of 0.21% and 0.048% for laminectomy alone and laminectomy with fusion, respectively.
Table 1.
Cost-Effectiveness of Prophylactic Vancomycin Powder for Lumbar Laminectomy.
| Vancomycin Powder (1 g) Cost (US$) | Laminectomy | Laminectomy and Fusion | ||
|---|---|---|---|---|
| Break-Even Infection Rate (%) | Break-Even ARR (%) | Break-Even Infection Rate (%) | Break-Even ARR (%) | |
| 2.50 | 4.19 | 0.01 | 8.50 | 0.003 |
| 3.06a | 4.19 | 0.01 | 8.50 | 0.003 |
| 10.00 | 4.15 | 0.05 | 8.49 | 0.01 |
| 17.00 | 4.12 | 0.08 | 8.48 | 0.02 |
| 34.00 | 4.04 | 0.16 | 8.46 | 0.04 |
| 44.00 | 3.99 | 0.21 | 8.45 | 0.05 |
| 50.00 | 3.96 | 0.24 | 8.45 | 0.05 |
| 75.00 | 3.84 | 0.36 | 8.42 | 0.08 |
| 100.00 | 3.73 | 0.47 | 8.39 | 0.11 |
Abbreviation: ARR, absolute risk reduction.
a Value at our institution.
Additional calculations were performed using a wide range of infection rates, taking into consideration the fact that infection rates after lumbar procedures vary in the literature and are also presumed to vary by institution and surgeon. For these analyses, the costs of revision following infection after both procedures were held constant. These calculations demonstrated that even at initial infection rates as high as 10%, the cost-effectiveness of vancomycin powder in both procedures remained unchanged with an ARR of 0.015% for lumbar laminectomy alone and 0.0034% for laminectomy with fusion (Table 2).
Table 2.
Maintaining Cost of Vancomycina and the Cost of Treating Infection Constant Does Not Change Cost-Effectiveness.
| Initial Infection Rateb (%) | Laminectomy | Laminectomy and Fusion | ||
|---|---|---|---|---|
| Final Infection Rate (%) | ARR (%) | Final Infection Rate (%) | ARR (%) | |
| 0.50 | 0.49 | 0.0145 | 0.50 | 0.0034 |
| 1 | 0.99 | 0.0145 | 1.00 | 0.0034 |
| 2 | 1.99 | 0.0145 | 2.00 | 0.0034 |
| 3 | 2.99 | 0.0145 | 3.00 | 0.0034 |
| 4 | 3.99 | 0.0145 | 4.00 | 0.0034 |
| 5 | 4.99 | 0.0145 | 5.00 | 0.0034 |
| 6 | 5.99 | 0.0145 | 6.00 | 0.0034 |
| 7 | 6.99 | 0.0145 | 7.00 | 0.0034 |
| 8 | 7.99 | 0.0145 | 8.00 | 0.0034 |
| 9 | 8.99 | 0.0145 | 9.00 | 0.0034 |
| 10 | 9.99 | 0.0145 | 1.00 | 0.0034 |
Abbreviation: ARR, absolute risk reduction.
a Cost of vancomycin $3.06 per gram at our institution.
b Presumes cost of treating infection is $21 060 for laminectomy and $90 938 for laminectomy and fusion.
To determine how much impact the cost of revision had on the break-even analysis, the ARR was calculated when the initial rate of infection and the cost of vancomycin powder was held constant across various costs of revision. The results showed that the ARR does vary based on the revision rate, but most of the variation is at extremes of cost and is not clinically relevant (Table 3).
Table 3.
Maintaining Cost of Vancomycina and Initial Rate of Infectionb Constant Changes Cost-Effectiveness.
| Cost of Treating Infection (US$) | Laminectomy | Laminectomy and Fusion | ||
|---|---|---|---|---|
| Final Infection Rate (%) | ARR (%) | Final Infection Rate (%) | ARR (%) | |
| 500 | 3.59 | 0.6120 | 7.89 | 0.6120 |
| 1000 | 3.89 | 0.3060 | 8.19 | 0.3060 |
| 5000 | 4.14 | 0.0612 | 8.44 | 0.0612 |
| 10 000 | 4.17 | 0.0306 | 8.47 | 0.0306 |
| 21 060c | 4.19 | 0.0145 | 8.49 | 0.0145 |
| 30 000 | 4.19 | 0.0102 | 8.49 | 0.0102 |
| 40 000 | 4.19 | 0.0077 | 8.49 | 0.0076 |
| 50 000 | 4.19 | 0.0061 | 8.49 | 0.0061 |
| 75 000 | 4.20 | 0.0041 | 8.50 | 0.0041 |
| 90 938d | 4.20 | 0.0034 | 8.50 | 0.0034 |
| 100 000 | 4.20 | 0.0031 | 8.50 | 0.0031 |
| 120 000 | 4.20 | 0.0025 | 8.50 | 0.0025 |
Abbreviation: ARR, absolute risk reduction.
a Cost of vancomycin $3.06 per gram at our institution.
b Presumes initial rate of infection is 4.20% for laminectomy and 8.50% for laminectomy and fusion.
c Denotes literature value of treating infected laminectomy.
d Denotes literature value of treating infected laminectomy and fusion.
Discussion
The intra-wound application of vancomycin powder has been utilized for infection prophylaxis across a variety of surgical specialties, including multiple subspecialties of orthopedic surgery.10,11 The effect has been a demonstrable decrease in infection without any appreciable complications.12,13 With regard to spine surgery, Sweet et al demonstrated that vancomycin powder reduced the deep infection rate after thoracic and lumbar instrumented spinal fusions from 2.6% to 0.2% compared to traditional intravenous antibiotics, with no adverse clinical or wound complications.13 Additional studies have reported precipitous decreases in infection rates with vancomycin powder prophylaxis in spine surgeries, such as instrumented posterior cervical spine fusions (15% to 0%), posterior spinal fusions for trauma (13% to 0%), and complex posterior instrumented spine surgery (10% to 5%).14,15,24
Given the recent economic changes in orthopedic reimbursement, including the trend toward bundle payments, minimizing costs while improving efficacy and patient outcomes is more important than ever before.25-27 There is a dearth of published data on the economic burden of infection after lumbar laminectomy with fusion, but the limited studies that have described these costs have uniformly shown the tremendous economic burden of an infected spinal surgery, particularly with implants.1 A recent study by Patel et al identified postoperative spinal infection as one of the most expensive causes of readmission and concluded that patients with spine surgery incur approximately double the health care costs when they develop a surgical site infection.28
The most common organism causing infection after lumbar laminectomy with fusion is S aureus, estimated to account for up to 90% of all infection following these operations.28 The incidence of MRSA in spinal surgery has been found to account for an estimated 25% to 52% of all S aureus isolates from infected spine procedures.28 Infection with this microorganism is particularly worrisome, as prior studies have shown that treatment outcomes are less successful and more costly for patients.9,29 Thus, there has been an increased focus on preventing MRSA infections after lumbar laminectomy with fusion by utilizing local vancomycin powder intraoperatively.12,22,30
In addition to its advantageous antimicrobial properties, vancomycin powder has also gained popularity due to its cost-effectiveness.16,17 However, prior cost-effectiveness studies have looked at cost-effectiveness either from a macroeconomic standpoint or utilizing institution-specific values that may not apply to other practices.16,17 In addition, prior studies have looked at the cost-effectiveness of vancomycin powder for laminectomy with instrumented fusion but have failed to examine the cost-effectiveness in laminectomy alone or to provide a cost-effectiveness comparison between the 2 procedures.
Despite the growing body of evidence supporting the efficacy of vancomycin powder for infection prophylaxis in orthopedic surgery, many researchers remain concerned regarding the routine prophylactic use of a potent antimicrobial agent. In a recent investigation of patients who underwent irrigation and debridement of wound infections following elective thoracic or lumbar surgery, Grabel et al found that polymicrobial infections and infection with gram-negative organisms was significantly more common among patients who had received vancomycin powder prophylaxis during the index procedure.31 Nevertheless, Grabel et al did not appreciate any differences between infected spine patients who received vancomycin powder and those who did not regarding rate of requiring greater than one antibiotic to treat the infection. However, the rate of repeated irrigation and debridement was significantly less in the vancomycin-treated group.31
There are a few important considerations derived from this break-even equation. First, the major determinant of cost-effectiveness is the cost of the vancomycin powder itself. At our institution, the cost of the powder was low at $3.06; however, even at inflated values as high as $44.00, it remained cost-effective for both procedures. Second, the baseline infection rate does not affect the ARR obtained at any specific cost of vancomycin powder. When both the cost of treating an infection and the cost of the powder were kept constant, the final break-even ARR remained unchanged for both procedures, regardless of initial infection rate. Finally, the cost of treating an infection does make a difference, but the difference is probably subclinical at the current cost levels estimated in the literature. When the cost of vancomycin powder and the initial infection rates were kept constant, the ARR for vancomycin powder varied very little when calculated within the cost ranges of treating an infection cited in the literature.
The utility of this break-even equation is that it provides a straightforward method to determine the economic viability of vancomycin powder for lumbar laminectomy with and without fusion, even though the incidence of infection is low enough to preclude a randomized controlled trial. For instance, assuming that vancomycin powder has a hypothetical ARR of 0.02%, the number needed to treat to prevent an infection would be 1 in 5000. To determine this same result in a clinical trial using a power analysis, the sample size, assuming P < .05 and power = 80%, would need to be extremely high (15 366 400). In our case, even with the most expensive vancomycin powder cost, which requires the largest ARR of 0.21% for laminectomy without fusion, the sample size remains prohibitively large at 139 378. Likewise, laminectomy with fusion, which requires an ARR of 0.048% at the most expensive cost of vancomycin, would require an even larger sample size of 2 667 778, which is an impossible number of patients to follow in a clinical study. Thus, this equation serves as an extremely useful tool for any clinician to determine the cost-effectiveness of intraoperative vancomycin powder utilization, both in simple lumbar laminectomy and in any other spine procedure. All the clinician requires is their initial infection rate, the costs of surgical revision for a given procedure at their institution, and their purchasing costs for vancomycin powder, and they can calculate the cost-effectiveness of vancomycin powder for any procedure used in their own practice.
Based on our results, we believe that vancomycin powder is a cost-effective measure for the prevention of infection in both lumbar laminectomy with fusion and lumbar laminectomy alone, although it is more cost-effective when used for laminectomy with fusion. Despite the fact that the efficacy of vancomycin powder has not been directly examined in simple lumbar laminectomy, its efficacy has been documented in noninstrumented lumbar procedures.22 The choice to utilize this modality intraoperatively should be a multifactorial decision that includes individualized patient and physician decision making, as well as institutional infection rates and protocols. It is important to note that we are not recommending that all institutions utilize vancomycin powder in all their laminectomy procedures. This article simply aims to serve as an objective cost-analysis model for physicians to use when considering the financial aspects of their spine surgery infection prevention algorithm.
While this study provides a useful framework for any clinician to improve the cost-effectiveness of their practice, it contains several flaws. First, the cost and infection data are not exact and are liable to fluctuate between different institutions. Our infection data was based on national estimates provided in the literature, which may vary greatly by practice and patient population. Second, this study only considers a single type of spine surgery and may not be generalizable to other spinal procedures or differing techniques, such as minimally invasive versus open. Third, modelling can only account for averages and does not include individualized patient and regional demographics. We believe, however, that this model still provides a useful conceptual framework for overall practice management that can be deviated from for anomalous or complex patients. Finally, our study does not consider the noneconomic aspects of these protocols, such as antibiotic resistance and the wider public health implications of using vancomycin powder in all patients. We deliberately chose to focus this article solely on the economic implications of this treatment protocol.
This break-even analysis demonstrates that prophylactic intra-wound application of vancomycin powder can be highly cost-effective not only for lumbar laminectomy with fusion but also for laminectomy alone. At our institution’s price point, the use of vancomycin powder is economically justified if it prevents at least one infection out of 6667 lumbar laminectomy surgeries. By comparison, the use of vancomycin powder in lumbar laminectomy with fusion would be cost-effective if it prevented at least one infection out of 29 411 surgeries. Additionally, the baseline infection rate did not affect the ARR of the protocols studied, with the ARR of vancomycin powder remaining constant at both extremely low and high initial infection rates. Finally, the cost of treating an infection did affect the ARR of the protocols studied when extreme values were used but had no clinical significance at the average cost ranges cited in the literature. This break-even analysis is easily adaptable to the individual practices of academic institutions or private practice surgeons, providing a useful economic analysis tool for the practicing spine surgeon.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Gregory J. Kirchner, MPH  https://orcid.org/0000-0003-0959-0222
https://orcid.org/0000-0003-0959-0222
Alexander M. Lieber, BA  https://orcid.org/0000-0001-6517-4472
https://orcid.org/0000-0001-6517-4472
References
- 1. Calderone RR, Garland DE, Capen DA, Oster H. Cost of medical care for postoperative spinal infections. Orthop Clin North Am. 1996;27:171–182. [PubMed] [Google Scholar]
- 2. Kalakoti P, Missios S, Maiti T, et al. Inpatient outcomes and postoperative complications after primary versus revision lumbar spinal fusion surgeries for degenerative lumbar disc disease: a national (nationwide) inpatient sample analysis, 2002-2011. World Neurosurg. 2016;85:114–124. [DOI] [PubMed] [Google Scholar]
- 3. Adogwa O, Elsamadicy AA, Sergesketter A, et al. Prophylactic use of intraoperative vancomycin powder and postoperative infection: an analysis of microbiological patterns in 1200 consecutive surgical cases. J Neurosurg Spine. 2017;27:328–334. [DOI] [PubMed] [Google Scholar]
- 4. Nakamura M, Shimakawa T, Nakano S, et al. Screening for nasal carriage of Staphylococcus aureus among patients scheduled to undergo orthopedic surgery: incidence of surgical site infection by nasal carriage. J Orthop Sci. 2017;22:778–782. [DOI] [PubMed] [Google Scholar]
- 5. Adogwa O, Vuong VD, Elsamadicy AA, et al. Does nasal carriage of Staphylococcus aureus increase the risk of post-operative infections after elective spine surgery: do most infections occur in carriers? World Neurosurg. 2018;116:e519–e524. [DOI] [PubMed] [Google Scholar]
- 6. Klevens RM, Edwards JR, Richards CL, Jr, et al. Estimating health care-associated infections and deaths in US hospitals, 2002. Public Health Rep. 2007;122:160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Klevens RM, Morrison MA, Nadle J, et al. ; Active Bacterial Core surveillance (ABCs) MRSA Investigators. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–1771. [DOI] [PubMed] [Google Scholar]
- 8. Malcolm TL, Robinson le D, Klika AK, Ramanathan D, Higuera CA, Murray TG. Predictors of Staphylococcus aureus colonization and results after decolonization. Interdiscip Perspect Infect Dis. 2016;2016:4367156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Parvizi J, Pawasarat IM, Azzam KA, Joshi A, Hansen EN, Bozic KJ. Periprosthetic joint infection: the economic impact of methicillin-resistant infections. J Arthroplasty. 2010;25(6 suppl):103–107. [DOI] [PubMed] [Google Scholar]
- 10. Horii C, Yamazaki T, Oka H, et al. Does intrawound vancomycin powder reduce surgical site infection after posterior instrumented spinal surgery? A propensity score-matched analysis. Spine J. 2018;18:2205–2212. [DOI] [PubMed] [Google Scholar]
- 11. Yao R, Tan T, Tee JW, Street J. Prophylaxis of surgical site infection in adult spine surgery: a systematic review. J Clin Neurosci. 2018;52:5–25. [DOI] [PubMed] [Google Scholar]
- 12. Evaniew N, Khan M, Drew B, Peterson D, Bhandari M, Ghert M. Intrawound vancomycin to prevent infections after spine surgery: a systematic review and meta-analysis. Eur Spine J. 2015;24:533–542. [DOI] [PubMed] [Google Scholar]
- 13. Sweet FA, Roh M, Sliva C. Intrawound application of vancomycin for prophylaxis in instrumented thoracolumbar fusions: efficacy, drug levels, and patient outcomes. Spine (Phila Pa 1976). 2011;36:2084–2088. [DOI] [PubMed] [Google Scholar]
- 14. Caroom C, Tullar JM, Benton EG, Jr, Jones JR, Chaput CD. Intrawound vancomycin powder reduces surgical site infections in posterior cervical fusion. Spine (Phila Pa 1976). 2013;38:1183–1187. [DOI] [PubMed] [Google Scholar]
- 15. O’Neill KR, Smith JG, Abtahi AM, et al. Reduced surgical site infections in patients undergoing posterior spinal stabilization of traumatic injuries using vancomycin powder. Spine J. 2011;11:641–646. [DOI] [PubMed] [Google Scholar]
- 16. Godil SS, Parker SL, O’Neill KR, Devin CJ, McGirt MJ. Comparative effectiveness and cost-benefit analysis of local application of vancomycin powder in posterior spinal fusion for spine trauma: clinical article. J Neurosurg Spine. 2013;19:331–335. [DOI] [PubMed] [Google Scholar]
- 17. Emohare O, Ledonio CG, Hill BW, Davis RA, Polly DW, Jr, Kang MM. Cost savings analysis of intrawound vancomycin powder in posterior spinal surgery. Spine J. 2014;14:2710–2715. [DOI] [PubMed] [Google Scholar]
- 18. Hatch MD, Daniels SD, Glerum KM, Higgins LD. The cost effectiveness of vancomycin for preventing infections after shoulder arthroplasty: a break-even analysis. J Shoulder Elbow Surg. 2017;26:472–477. [DOI] [PubMed] [Google Scholar]
- 19. Sclafani JA, Raiszadeh K, Raiszadeh R, et al. Validation and analysis of a multi-site MIS prospective registry through sub-analysis of an MIS TLIF Subgroup. Int J Spine Surg. 2014;8 doi:10.14444/1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kurtz SM, Lau E, Ong KL, et al. Infection risk for primary and revision instrumented lumbar spine fusion in the Medicare population. J Neurosurg Spine. 2012;17:342–347. [DOI] [PubMed] [Google Scholar]
- 21. Adogwa O, Parker SL, Shau DN, et al. Cost per quality-adjusted life year gained of revision neural decompression and instrumented fusion for same-level recurrent lumbar stenosis: defining the value of surgical intervention. J Neurosurg Spine. 2012;16:135–140. [DOI] [PubMed] [Google Scholar]
- 22. Strom RG, Pacione D, Kalhorn SP, Frempong-Boadu AK. Lumbar laminectomy and fusion with routine local application of vancomycin powder: decreased infection rate in instrumented and non-instrumented cases. Clin Neurol Neurosurg. 2013;115:1766–1769. [DOI] [PubMed] [Google Scholar]
- 23. Kanj WW, Flynn JM, Spiegel DA, Dormans JP, Baldwin KD. Vancomycin prophylaxis of surgical site infection in clean orthopedic surgery. Orthopedics. 2013;36:138–146. [DOI] [PubMed] [Google Scholar]
- 24. Lemans JVC, Öner FC, Wijdicks SPJ, Ekkelenkamp MB, Vogely HC, Kruyt MC. The efficacy of intrawound vancomycin powder and povidone-iodine irrigation to prevent surgical site infections in complex instrumented spine surgery. Spine J. 2019;19:1648–1656. [DOI] [PubMed] [Google Scholar]
- 25. Siddiqi A, White PB, Mistry JB, et al. Effect of bundled payments and health care reform as alternative payment models in total joint arthroplasty: a clinical review. J Arthroplasty. 2017;32:2590–2597. [DOI] [PubMed] [Google Scholar]
- 26. Elbuluk AM, O’Neill OR. Private Bundles: The nuances of contracting and managing total joint arthroplasty episodes. J Arthroplasty. 2017;32:1720–1722. [DOI] [PubMed] [Google Scholar]
- 27. Whitcomb WF, Lagu T, Krushell RJ, et al. Experience with designing and implementing a bundled payment program for total hip replacement. Jt Comm J Qual Patient Saf. 2015;41:406–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Patel H, Khoury H, Girgenti D, Welner S, Yu H. Burden of Surgical Site Infections Associated with Select Spine Operations and Involvement of Staphylococcus aureus. Surg Infect (Larchmt). 2017;18:461–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014;27:302–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bakhsheshian J, Dahdaleh NS, Lam SK, Savage JW, Smith ZA. The use of vancomycin powder in modern spine surgery: systematic review and meta-analysis of the clinical evidence. World Neurosurg. 2015;83:816–823. [DOI] [PubMed] [Google Scholar]
- 31. Grabel ZJ, Boden A, Segal DN, Boden S, Milby AH, Heller JG. The impact of prophylactic intraoperative vancomycin powder on microbial profile, antibiotic regimen, length of stay, and reoperation rate in elective spine surgery. Spine J. 2019;19:261–266. [DOI] [PubMed] [Google Scholar]


