Abstract
Prostate cancer is the most common malignancy diagnosed in North American men. Although medical advances have improved survival rates, men treated for prostate cancer experience side-effects that can reduce their work capacity, increase financial stress, and affect their career and/or retirement plans. Working-age males comprise a significant proportion of new prostate cancer diagnoses. It is important, therefore, to understand the connections between prostate cancer and men’s work lives. This scoping review aimed to summarize and disseminate current research evidence about the impact of prostate cancer treatment on men’s work lives. Electronic databases were searched to identify peer-reviewed articles published between 2006 and 2020 that reported on the impact of prostate cancer treatment on men’s work. Following scoping review guidelines, 21 articles that met inclusion criteria were identified and analyzed. Evidence related to the impact of prostate cancer on work was grouped under three themes: (1) work outcomes after prostate cancer treatment; (2) return to work considerations, and (3) impact of prostate cancer treatment on men’s finances. Findings indicate that men’s return to work may be more gradual than expected after prostate cancer treatment. Some men may feel pressured by financial stressors and masculine ideals to resume work. Diverse factors including older age and social benefits appear to play a role in shaping men’s work-related plans after prostate cancer treatment. The findings provide direction for future research and offer clinicians a synthesis of current knowledge about the challenges men face in resuming work in the aftermath of prostate cancer treatment.
Keywords: Prostate cancer, return to work, working men, financial worries, career, retirement
Background
Prostate cancer is the most common malignancy diagnosed in North American men. It is expected that 23,300 new cases will be reported in Canada and 191,930 new cases are expected in the United States in 2020 (American Cancer Society, 2020; Canadian Cancer Society, 2020a). Men of working age make up a significant proportion of new cases: 19% of all diagnoses are males under the age of 59, and 40% of diagnoses occur in men between the ages of 60 and 69 years (Canadian Cancer Society’s Steering Committee on Cancer Statistics, 2012). Although work is recognized as an essential activity affording men income to satisfy material needs (Emslie & Hunt, 2009), prostate cancer diagnosis and treatment side-effects can result in reduced work capacity, threatening men’s financial security and triggering changes to career and/or retirement plans (Grunfeld et al., 2013; Yu Ko et al., 2020).
With regard to the connections between work and prostate cancer, it is known that early prostate cancer diagnosis, coupled with advances in treatment, have resulted in high 5-year relative survival rates of over 93% (American Cancer Society, 2020; Canadian Cancer Society, 2020b). Given these statistics, a significant number of men experience prostate cancer as a chronic illness. There is an increasing number of men in North America who plan to work past age 65 or return to work after retirement (MacEwen, 2012; Sun Life Canadian Unretirement Index, 2015; United States Department of Labor, 2017). This trend for larger numbers of men to continue working until later in life may reflect concerns about financial uncertainties after retirement (Sun Life Canadian Unretirement Index, 2015). While labor force participation for Canadian men aged 65–69 has more than doubled (7%–18%) between 2000 and 2010 (MacEwen, 2012), the American male workforce of the same age group is expected to increase by 4.4% by 2026 (United States Department of Labor, 2017).
Given the expected rise of new prostate cancer diagnoses due to an aging population (Quon et al., 2011) and the trend for more men to work past age 65 (Sun Life Canadian Unretirement Index, 2015; United States Department of Labor, 2017), it is important to review current evidence regarding the connections between prostate cancer treatment and its impact on men’s work lives to provide direction for approaches to support working men diagnosed with prostate cancer and to identify directions for future research. The purpose of this scoping review is to summarize and disseminate current research evidence about the impact of prostate cancer treatment on men’s work lives.
Methods
Search strategy
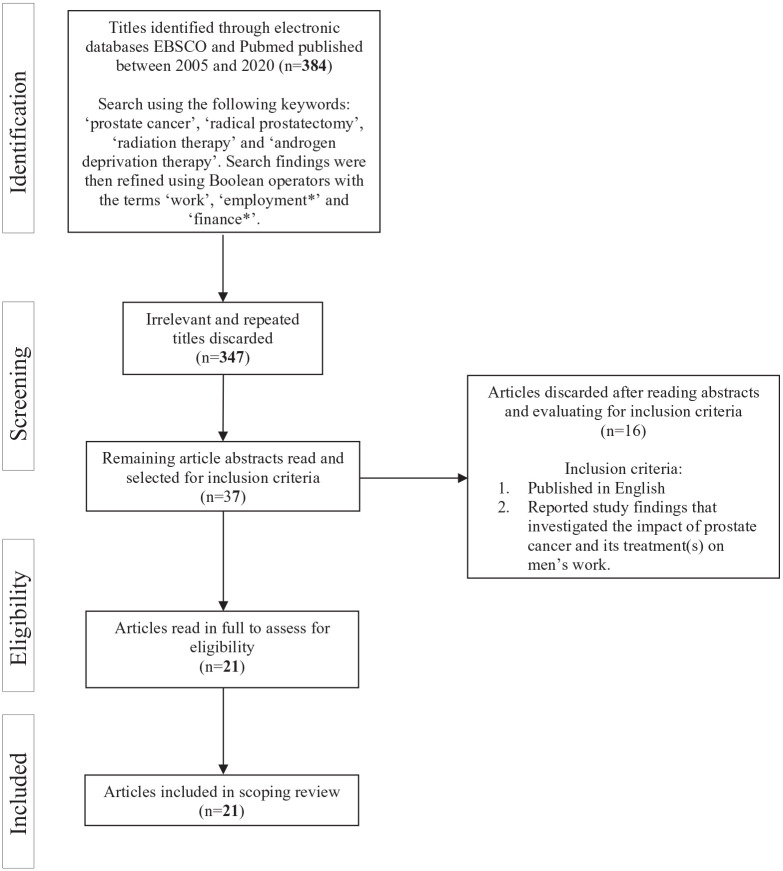
The search for a comprehensive range of relevant research publications was guided by Arksey and O’Malley’s (2005) scoping review methodology. Titles in the Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL, EBSCO, EMBASE, MEDLINE, PsychINFO, and PubMed were searched using the following keywords: “prostate cancer,” “radical prostatectomy,” “radiation therapy,” and “androgen deprivation therapy” (see Figure 1). Search findings were then refined using Boolean operators with the terms “work,” “employment*,” and “finance*.” The search strategy produced 384 results. The search was conducted in October 2020.
Figure 1.
Flow diagram of article inclusion/exclusion process.
Irrelevant and repeated titles were discarded (n = 347). Abstracts were screened for the following inclusion criteria: (1) published in English between 2006 and 2020 and (2) reported study findings that investigated the impact of prostate cancer and its treatment(s) on men’s work. All study designs were considered. The screening yielded 37 article abstracts that were read to inspect for relevance. This resulted in the inclusion of 21 articles for the current scoping review.
Six articles reported findings from studies with samples that included participants with prostate cancer in addition to individuals with other cancer types (Arndt et al., 2019; Bradley et al., 2006; Gunnarsdottir et al., 2013; Oberst et al., 2010; Sharp & Timmons, 2011, 2016); however, only findings pertaining to participants with prostate cancer were considered in the current analysis. Key findings were extracted from each article and transcribed in a table (Table 1) to map the current state of knowledge about the linkages between prostate cancer, its treatment(s), and work. Analysis consisted of (1) comparing and contrasting the findings among the articles, (2) identifying categories across the findings, and (3) condensing the categories into overarching themes.
Table 1.
Summary of Scoping Review Articles.
| Study | Aims/objectives | Design/methodology | Data collection/sample | Sample characteristics | Key findings |
|---|---|---|---|---|---|
| Arndt et al. (2019), Germany | 1. Find how many cancer survivors below age 60 at diagnosis return to work and how long does it take. 2. Find how many survivors take up a new job, reduce working hours, or quit their jobs after resuming work. 3. Find how does the proportion of return to work varies with specific sociodemographical and clinical characteristics. |
Quantitative, retrospective | Survey questionnaire 1070 women with breast cancer 111 women with colorectal cancer 170 men with colorectal cancer 207 men with prostate cancer |
Men with prostate cancer only Mean age: 55.4 62.3% returned to same job 63.8% nonphysically demanding job. 84.5% surgery 69.9% received rehabilitation 21.3% on disability pension |
17% of all respondents reduced working hours and 6% quit their jobs within 5 years of returning to work. Individuals who changed jobs experienced greater financial difficulties than those who did not. Younger age, non-manual labor, self-employment, earlier cancer stage, and higher education were strong predictors of return to the same job in men with prostate cancer. 90% of all returnees to work resumed activities within the first 2 years of diagnosis. Rehabilitation therapy after cancer treatment is inversely associated with return to work. |
| Bennett et al. (2018), United Kingdom | Identify factors associated with movement from employment to unemployment or early retirement in working-age men diagnosed with prostate cancer. | Quantitative, retrospective | Survey questionnaire Population-based cancer databases 35,823 men under the age of 60 at the time of prostate cancer diagnosis |
Mean age of those who remained employed: 55.4; mild side-effects: 89.4% full time: 72.3% Mean age of those who became unemployed: 55.9; moderate/severe side-effects: 31% Mean age of those who became retired: 57.7; moderate/severe side-effects: 10.1% |
Late-stage cancer, bowel, and urinary problems, symptoms at diagnosis, and comorbidities increased the odds of job loss. Older age, more severe urinary side-effects, caregiving sick family member, white ethnicity, full-time employment, and advanced disease increased odds of early retirement. Men living in the poorest areas had over twice the odds of becoming unemployed. Physically demanding jobs associated with greater difficulties returning to work. |
| Bradley et al. (2005), United States | Investigate the influence of prostate cancer treatment on participants’ work activities. | Quantitative, prospective, 6 and 12 month postdiagnosis follow-up | Survey Medical records database 267 men diagnosed with prostate cancer and two control groups of 283 and 265 men without cancer |
Men with prostate cancer only Mean age: 55.5 76.8% had surgery 43.8% had college degree 63.7% white collar job Employed at 6 months: 72.4%; at 12th month: 80.5% |
Men diagnosed with prostate cancer were 10% less likely to be working 6 months after diagnosis than men in the control groups. 80.5% of men were working by the 12th month after prostate cancer diagnosis; however, 30% of the men were unable to fully restore/perform work tasks. |
| Bradley et al. (2006), United States | Examine the length of work absenteeism due to either breast or prostate cancer treatment. | Quantitative, prospective, 6 and 12 month postdiagnosis follow-up | Phone interviews 206 employed men with prostate cancer 239 employed women diagnosed with breast cancer |
Men with prostate cancer only Mean age: 55 75.3% had surgery 52.4% had college degree 60.7% earned more than $75,000 82% had paid sick leave 42.7% had physical job 75% diagnosed with early disease |
Employed men newly diagnosed with prostate cancer missed an average of 27 days from work. Radical prostatectomy and radiation therapy for prostate cancer result in work absenteeism and substantial loss of income. |
| Dahl et al (2014), Norway | Identify factors associated with declined work status 3 months after radical prostatectomy. | Quantitative, prospective | Self-administered, mailed questionnaire 264 employed men at the time of prostate cancer diagnosis and who were under age 65 at the time of radical prostatectomy |
Mean age: 59.2 70% no urinary leakage by weeks 69% no comorbidities |
73% of participants “had regained or improved their preoperative work status” by the third month after radical prostatectomy. 15% of participants experienced medical complications that might be associated with “declined 3-months work status”. Strenuous physical work and lower age predicted prolonged sick leave. |
| Dahl et al (2015), Norway | To study the influence of radical prostatectomy on work status and work-life 3 years after surgery. | Quantitative, prospective | Self-administered, mailed questionnaires 330 men who were working, on sick leave/rehab, or were seeking work at the time of prostate cancer diagnosis and who underwent radical prostatectomy |
Mean age: 60.7 Return to work at 3 year postsurgery: no change Full-time: decreased from 75% to 66% Part-time: increased from 9% to 21% |
80% of participants who returned to work worked the same or more than before surgery. The number of men working part-time almost doubled by the third year after radical prostatectomy. One-third of the participants reported prostate cancer and treatment side-effects affected their work. |
| Dahl et al. (2016), Norway | Evaluate work ability after radical prostatectomy in relation to postsurgical urinary leakage, and adjuvant or salvage radiation therapy and androgen deprivation therapy | Quantitative, prospective | Survey questionnaire 563 men employed men with prostate cancer who received radical prostatectomy |
Mean age: 62.6 Return to work rate: full-time: 74%; part-time: 19% |
24.5% of participants rated their work ability as being moderate to poor up to 1 year postradical prostatectomy. Comorbidities were found to be the strongest independent factor associated with lower work ability after radical prostatectomy. 30% of participants reported urinary leakage, which is independently associated with poorer work ability. Time since radical prostatectomy was independently associated with improved work ability. |
| Dahl et al. (2020), Norway | Examine the prevalence of men who had high versus moderate/poor current work ability compared with their lifetime best work ability at a mean of 3 years after robot-assisted laparoscopic prostatectomy | Quantitative, cross-sectional | Survey questionnaire 777 men who underwent robot-assisted radical prostatectomy |
Mean age at diagnosis: 62.5 28% with positive margins at postsurgical biopsy 21% recurrence by third year postsurgery |
Age, comorbidities, lower education, and urinary leakage are significantly associated with reduced work ability. By the third year after surgery, only 38% of men were working full-time, while 40% had retired. Men who were working full-time had higher work ability than men who worked part-time. |
| Gordon et al. (2017), Australia | To understand the economic burden of prostate cancer among Australian men | Quantitative, retrospective | Online survey 289 men who reported having a prostate cancer diagnosis |
Mean age: 65.1 69% surgery 31% radiotherapy 18% metastases Work status: 55% retired; 38% employed; 7% unemployed; 44% university educated; 35% higher education diploma Income: $18k–37k: 18%; $37k–80k: 38%; $80k–180k: 25% 202 men with comorbidities |
Almost a quarter of men who were employed at the time of prostate cancer diagnosis reported retiring earlier than expected as a result of their diagnosis. 17% of the participants reduced their work hours, while another 17% stopped work prior to the survey. A few men noted they were passed over for promotion (2%) or had been made redundant at work (3%) due to their prostate cancer diagnosis. Men who were diagnosed with prostate cancer in 2012 reported a mean out-of-pocket expenses of AU$ 11,077 for specialist fees, hospital services, medical equipment, supplies, and medicines. 70% of participants reported spending more on their cancer treatment than they expected to. 34% reported financial struggles, while 38% drew on savings. Although 71% of participants had private health insurance, deductible fees/co-payments for health services add up and can become a financial burden to patients. |
| Grunfeld et al. (2013), United Kingdom | Investigate the meaning of work and describe the connections between masculinity and work after prostate cancer treatment. | Qualitative, retrospective, “framework” analysis, cross-sectional | Face-to-face and/or phone interviews 50 men treated for prostate cancer. Of these, 41 men participated in a 12-month follow-up interview |
Mean age: 59 66% surgery 49 men returned to work by the 12th month posttreatment 85% worked at same employer 78% no change in work duties 38% college/university education 56% white collar 30% blue collar |
Men worry about prostate cancer recurrence and prioritize pursuing health and quality of life, often by reducing work and/or work-exertion. Men’s narratives indicate that urinary side-effects have a profound effect on decisions around return to work. Prostate cancer treatment side-effects threaten men’s ability to work. This, in turn, affects their self-perceived sense of masculinity. |
| Gunnarsdottir et al. (2013), Denmark, Finland, Iceland, Norway | Investigate whether employment status and work experiences differ among male cancer survivors with prostate, testicular, lymphoma, and cancer-free men. | Quantitative, retrospective | Self-administered, mailed questionnaires 233 men with prostate cancer 101 men with lymphoma 462 men with testicular cancer 1208 men in a reference group (without a cancer diagnosis) |
Men with prostate cancer only Mean age: 58.4 Employed: 58% |
Men treated for prostate cancer had the highest cancer recurrence rate (13%). Men with prostate cancer were more likely than participants in other groups to experience greater competitiveness, distrust, and discrimination at work and were less likely to remain employed than men in the reference group. Men in the prostate cancer group were less committed to their work than men in the reference group. Career and life priorities may have been reevaluated by men with prostate cancer. |
| von Mechow et al. (2018), Germany | Compare the duration of sick leave in patients with localized prostate cancer after robot-assisted radical prostatectomy and open retropubic radical prostatectomy | Quantitative, cohort study |
Online questionnaires 1415 men under the age of 65 who underwent radical prostatectomy |
Median age: 58 (range 54–62) 87.3% negative cancer margins 52.3% received rehabilitation Full-time work: 93% Light physical workload: 67.6% Self-employed: 27.9% |
No difference was noted in the length of men’s sick leave after radical prostatectomy, regardless of surgical technique. Laws protecting workers who need medical treatment and social welfare benefits (i.e., sick leave, income replacement) may influence when men decide to return to work after radical prostatectomy. |
| Nilsson et al. (2020), Norway |
To describe the changes in work status and work ability from diagnosis of prostate cancer to median 4 years after diagnosis. To compare characteristics of patients with reduced versus unchanged work ability. To explore factors associated with reduced work ability. |
Quantitative, retrospective, cross-sectional | Questionnaire survey 440 men who received either radical prostatectomy or active surveillance |
Mean age at diagnosis: 61.1 Median time from diagnosis to survey: 4.1 years. 82% employed at the time of prostate cancer diagnosis and 49% working at the time of the survey |
Reduced work ability associated with age, poorer health, incontinence, chronic fatigue, and mental health issues were associated with reduced work ability. Compared with active surveillance, work ability is affected by radical prostatectomy in the long term. Men on active surveillance who reported reduced work ability had greater incontinence than those who did not. Comorbidities associated with poorer work ability in bivariate analysis, but not in multivariate analysis. |
| Oberst et al. (2010), United States | Describe work-related physical and cognitive disability estimates 12 and 18 months after diagnosis and treatment for breast and prostate cancer. | Quantitative, prospective, longitudinal | Phone interviews 267 men who were employed at the time of prostate cancer diagnosis 447 women newly diagnosed with breast cancer |
Men with prostate cancer only Mean age: 55 64% had surgery Return to work rate posttreatment at: 12 months: 91%; 18 months: 85%; 30.4% did heavy lifting by 12th month posttreatment |
Treatment side-effects lead to reduced work capacity after prostate cancer treatment. Financial need may represent a significant barrier to leaving the workforce. |
| Plym et al. (2016), Sweden | Investigate short-term and long-term rates of work disability following robot-assisted radical prostatectomy and open radical prostatectomy. | Quantitative, cohort study |
Medical records database 2571 men who underwent radical prostatectomy |
Mean age at surgery: 58 (robot assisted); 59 (open) Employment rate: 78% (robot assisted); 80% (open) Cancer risk: 54% low (robot assisted); 46% (open) |
Men who undergo robot-assisted radical prostatectomy returned to work 13 days earlier than men who received open radical prostatectomy. Surgery type did not have an impact on long-term rates of work disability. Social welfare benefits (i.e., sick leave, income replacement) may influence when men decide to return to work after radical prostatectomy. |
| Sharp and Timmons, (2011), Ireland | Investigate employment outcomes among breast and prostate cancer survivors. | Quantitative, retrospective, cross-sectional | Self-administered, mailed questionnaires 100 men with prostate cancer 246 women with breast cancer |
Men with prostate cancer only Median age: 58 58% had surgery 21.4% had postsecondary education 57% employees 43% self-employed 15% reported financial difficulties |
Men with prostate cancer tended to work longer hours than women before diagnosis and were more likely to be self-employed (43% vs. 13%). Men were more than three times as likely to return and remain employed than women. Household income, debt, and welfare status were correlated with men’s length of sick leave and return to work. Hours worked fell significantly postcancer treatment. |
| Sharp and Timmons, (2016), Ireland | Investigate factors associated with cancer-related financial stress and strain in breast and prostate cancer survivors. | Quantitative, cross-sectional | Self-administered, mailed questionnaires 212 men with prostate cancer 486 women with breast cancer |
Men with prostate cancer and women with breast cancer 60.4% had dependents 65.3% had a mortgage 63.8% had increased household bills since diagnosis 43.1% working for employer |
Despite publicly funded health care, prostate cancer treatment is associated with financial stress. Men who were working at the time of diagnosis were more likely to experience prostate cancer treatment-related financial stress than men who were retired. Prostate cancer diagnosis is positively associated with an exacerbation of preexisting financial hardships. |
| Sveistrup, et al. (2016), Denmark | Determine employment outcomes after prostate cancer treatment with radiotherapy. | Quantitative, retrospective | Medical records database 120 men of working age treated with external beam radiotherapy |
Mean age: 65 At 1 year postradiation: 75% of working-age men returned to work 27% chose early retirement 13% were on disability pension |
75% of men were working 1 year after radiation therapy. Good prostate cancer prognosis and lack of chronic comorbidities favored men’s return to work. Age was found to be single factor that may influence employment outcome after radiation therapy. |
| Ullrich, et al. (2017), Germany | Investigate return to work outcomes among prostate cancer survivors attending a cancer rehabilitation intervention. | Quantitative, prospective | Self-administered questionnaires, medical records, physicians’ assessments of functional outcomes 837 employed men treated with radical prostatectomy who started rehabilitation within 14 days of surgery |
Mean age: 56.8 87% returned to work by 12th month postsurgery 90% reported stable working conditions postreturn to work 49% white collar 52.5% middle class 51.8% open radical prostatectomy |
Men over 60 were more likely to reduce work hours and to report intention to apply for disability pension. Men under 60 often experienced changes in their relationship with employers. Men of the lowest socioeconomic status had the longest sick leave following the rehabilitation intervention and the lowest level of perceived work ability. |
| Ullrich et al. (2020), Germany | Investigate personal, health-related, psychosocial, and work-related factors associated with expectations of delayed return to work. | Quantitative, prospective, longitudinal | Survey questionnaire 822 men who had radical prostatectomy and attended a rehabilitation program |
Mean age: 56.8 81.9% married 34.4% manual worker 50% white collar job Mean time since diagnosis: 2.8 months |
21% of participants expected delayed return to work (>3 months) Higher tumor stage, low self-perception of work ability/ability to return to former job associated with delayed return to work. Quality of life and mental health not associated with delayed return to work. |
| Yu Ko et al. (2020), Canada | Explore the processes involved in men’s return to work postradical prostatectomy and understand how these events are connected to masculinities | Qualitative, retrospective, cross-sectional | One-to-one interviews, demographics data questionnaire 23 men who were employed at the time of prostate cancer diagnosis and who received radical prostatectomy |
Age range: ≤54: 3 men 55–60: 4 men 61–64: 7 men ≥65:10 men 9 self-employed 20 married |
The decision to return to work after radical prostatectomy is premised on men’s evaluation of career goals, retirement plans, and family needs. For many men, returning to work competes against their need to restore health and strengthening family relationships. Full resumption of work activities was found to be a process that was achieved gradually and over time. |
Results
Characteristics of the Review Articles
Nineteen articles reported findings from quantitative research studies. Study sample sizes ranged from 100 to 35,823 participants and were conducted in: Australia (n = 1), Denmark (n = 1), Germany (n = 4), Ireland (n = 2), Norway (n = 5), Sweden (n = 1), United Kingdom (n = 2), and the United States (n = 3). One multinational study was conducted with participants from Denmark, Finland, Iceland, and Norway. Data collection methods included medical records database information, survey questionnaires, and/or a combination of both. Results are reported herein with percentages and total number of occurrences when available. The set of articles reviewed included two qualitative studies that relied on individual interviews: a Canadian study involving 23 men and a study conducted in the United Kingdom with 50 participants. Results from qualitative studies offered rich descriptions that complemented the quantitative research findings. Within the literature reviewed, three overarching themes were assembled: (1) work outcomes after prostate cancer treatment, (2) return to work considerations, and (3) impact of prostate cancer treatment on men’s finances.
Work Outcomes After Prostate Cancer Treatment
Overall, work absenteeism was common for men who received prostate cancer treatment due to a period of recovery and the experience of side-effects that restricted men’s work capacity (Bradley et al., 2005, 2006; Dahl, et al., 2014, 2015, 2016, 2020; Nilsson et al., 2020; Oberst et al., 2010; Plym et al., 2016; Ullrich et al., 2017, 2020; Yu Ko et al., 2020). Bradley et al. (2006) reported that men missed an average of 27 days of work due to prostate cancer treatment (with either one treatment or a combination of radical prostatectomy, radiation therapy, and androgen deprivation therapy). Although the findings of several studies indicated that return to work rates were over 70% within the first year of treatment (Dahl et al., 2014, 2015, 2016; Plym et al., 2016; Sveitstrup et al., 2016), in eight studies the resumption of work responsibilities was reported to be shaped by a range of issues including the type of treatment and experience of side-effects (Arndt et al., 2019; Bennett et al., 2018; Dahl et al., 2014, 2016, 2020; Plym et al., 2016; Sveitstrup et al., 2016; Yu Ko et al., 2020).
The connections between radical prostatectomy and men’s ability to return to work were explicitly explored. Radical prostatectomy is known to have a period of postsurgical recovery lasting 4–5 weeks (Dahl et al., 2014; Plym et al., 2016; von Mechow et al., 2018; Yu Ko et al., 2020). In a German study that explored a return to work outcomes in 837 men (mean age = 56.8) who received radical prostatectomy, Ullrich et al. (2017) reported that the men were generally optimistic about their ability to return to work during postsurgical recovery. Common side-effects of radical prostatectomy such as urinary incontinence and reductions in physical functioning restrict men’s capacity to perform various work tasks (Dahl et al., 2014, 2016; Grunfeld et al., 2013; Nilsson et al., 2020; Yu Ko et al., 2020). Work capacity is reported to be most severely affected in the first 3 months after radical prostatectomy in two studies (Dahl et al., 2014; Yu Ko et al., 2020). In a study that followed 563 Norwegian men (mean age = 62.5) 1 year after radical prostatectomy, time lapsed after surgery was independently associated with improved capacity to do work (Dahl et al., 2016). This is an important finding because it suggests that postprostatectomy recovery is an ongoing process and that men may not have fully recovered their strength or endurance by the time they return to work.
Other factors affecting men’s work capacity after radical prostatectomy have been identified. For example, in a Swedish study involving 2571 men who underwent radical prostatectomy, researchers reported that men with “high” risk prostate cancer tended to have longer periods of sick leave postprostatectomy than men with “low” or “intermediate” risk prostate cancer (Plym et al., 2016). In a Norwegian study involving 264 employed men, Dahl et al. (2014) reported that medical complications related to radical prostatectomy occurred in up to 15% (n = 32) of men and resulted in unexpected delays for returning to work. With regard to comorbidities, preexisting illnesses have been reported to be associated with reduced work capacity after radical prostatectomy (Dahl et al., 2016, 2020; Nilsson et al., 2020; Sveitstrup et al., 2016). In this respect, postsurgical recovery may be complex, especially when comorbidities are present.
In terms of prostatectomy techniques, robot-assisted radical prostatectomy is associated with less intraoperative blood loss and a shorter postsurgical recovery period than an open radical prostatectomy. In addition, by examining outcomes between prostatectomy techniques, Plym et al. (2016) reported that Swedish men who received robot-assisted radical prostatectomy (n = 1062) returned to work 13 days earlier (median = 35 days) than those who underwent open radical prostatectomy (n = 1509). In a German study involving 1415 men who underwent radical prostatectomy and who completed online questionnaires, von Mechow et al. (2018) reported no differences in the length of sick leave between men who had a robot-assisted radical prostatectomy (n = 535) and men who underwent open radical prostatectomy (n = 880); men in both groups reported returning to work after a median of 42 days. It is important to note that return to work may be influenced by a number of system, family, or individual factors (i.e., lack of sick leave benefits, medical complications) (Dahl et al., 2015; Oberst et al., 2010; Sharp & Timmons, 2011; Yu Ko et al., 2020) and men’s actual return to work may not necessarily mean that they are fit and/or ready to resume work.
Little is known about the long-term implications of radical prostatectomy on men’s performance at work or career and retirement aspirations. Addressing this knowledge gap, Dahl et al. (2015) conducted a questionnaire-based study that explored the influence of radical prostatectomy on work status and work-life 3 years after surgery. The study included 330 men (mean age = 60.7) who were employed at the time of radical prostatectomy. Although 25% (n = 83) of the participants had age-retired by the third year after surgery, 80% (n = 192) of the remaining men in the workforce reported their employment status as increased or unchanged compared with the period leading up to radical prostatectomy. At 3 years postradical prostatectomy, 34% (n = 103) of the men considered that prostate cancer had influenced their work to some or great extent (Dahl, 2015). These findings suggest that the work capacity of aging men with prostate cancer may be impacted even after fully recovering from radical prostatectomy, and should be considered when evaluating prostate cancer treatment(s).
Only one study explored the impact of radiation therapy on men’s work. In a Danish study involving an analysis of medical records for 120 men of working age who received external beam radiation therapy, Sveistrup et al. (2016) reported that the proportion of men on sick leave peaked at 56% (n = 47) during the sixth and 10th week after the start of treatment. Further, Sveistrup et al. (2016) also noted that the men missed an average of 13.2 weeks of work during the year following radiation therapy, which is longer than the average sick leave reported for men who undergo radical prostatectomy (Dahl et al., 2014; Plym et al., 2016). Although 75% (n = 71) of the men in the Sveitsrup et al.’s (2016) study had returned to work by the 12th month after radiation therapy, the report does not provide details on whether men returned to the same work conditions. In this regard, there is a need to address this knowledge gap to better inform employed men about the potential work-related outcomes of the various treatment options available to them.
Return to Work Considerations
Six studies report factors that influence men’s decisions about postprostate cancer treatment return to work (Dahl et al., 2015; Grunfeld et al., 2013; Gunnarsdottir et al., 2013; von Mechow et al., 2018; Ullrich et al., 2020; Yu Ko et al., 2020). In two qualitative studies, prostate cancer diagnosis was viewed as a major life event that precipitated the reevaluation of men’s priorities, wherein the pursuit of career plans were experienced as competing with their efforts at maintaining health and strengthening family relationships, and work was perceived as potentially detrimental to their ongoing recovery from prostate cancer treatment (Grunfeld et al., 2013; Yu Ko et al., 2020). Yu Ko et al. (2020) reported that concerns around death and/or health complications underpinned men’s lifestyle decisions to decrease work-hours and spend more time with family after prostatectomy; and argued that the fear of cancer recurrence provided men with strong incentives to reduce work commitments and improve their quality of life.
Age was identified in nine studies as an influencing factor in men’s work decisions after prostate cancer treatment (Arndt et al., 2018; Bennett et al., 2018; Dahl et al., 2015, 2016, 2020; Nilsson et al., 2020; Sveitrup et al., 2016; Ullrich et al., 2017; Yu Ko et al., 2020). For example, in a study involving 837 German men who underwent radical prostatectomy and who subsequently received rehabilitation therapy, Ullrich et al. (2017) reported that men over the age of 60 were more likely to withdraw permanently from work and apply for disability pension than men in their 50s. The availability of early retirement benefits (Sveistrup et al., 2016; Ullrich et al., 2017), age-related decline in work capacity and concurrent or chronic illnesses (Dahl et al., 2015, 2016, 2020; Yu Ko et al., 2020) were also issues that were associated with older men’s work-related decisions postprostate cancer treatment.
Higher prostate cancer stage is linked with expected delays in return to work regardless of the type of occupation, level of income, or perceived quality of life (Ullrich et al., 2020). Ullrich et al. (2020) suggested that higher prostate cancer stage may be associated with a more aggressive cancer treatment regime resulting in greater or more intense side-effects and longer posttreatment recovery times. Regarding the impact of prostate cancer treatment side-effects, urinary incontinence has been reported to be a major factor influencing men’s decisions related to the resumption of work activities in eight studies (Arndt et al., 2018; Bennett et al., 2018; Dahl, et al., 2015, 2016, 2020; Grunfeld et al., 2013; Nilsson et al., 2020; Yu Ko et al., 2020). In a British qualitative study, Grunfeld et al. (2013) reported that treatment-induced urinary incontinence challenged men’s opportunities to socialize with co-workers and severely affected their masculine identities, despite efforts to manage urinary incontinence by hiding leakage to present a self-image of control at work. This finding suggests that men view bladder control as deeply tied to professionalism and that the management of incontinence is central to men’s ability to fulfill worker roles.
Decisions about readiness to return to work after prostate cancer treatment is influenced, at least in part, by the type of work men perform (Arndt et al., 2018; Dahl et al., 2015; Oberst et al., 2010; Ullrich et al., 2020; von Mechow et al., 2018; Yu Ko et al., 2020). von Mechow et al. (2018) reported that men in physically demanding jobs took longer to return to work than men in physically nondemanding occupations (median = 84 days vs. 49 days), while Dahl et al. (2015) reported that a physically demanding workload was negatively associated with work capacity and hours worked after men’s return to work following prostate cancer treatment. There were other factors that also influenced men’s decisions to return to work. Dahl et al. (2020) reported that more men under the age of 65 who did not have comorbidities (58%; n = 450) fully resumed work activities earlier than older men with multiple chronic illnesses (42%; n = 327), suggesting that age and concurrent health issues may exacerbate or lengthen reductions in work capacity. In a study involving 267 American workers (mean age = 55) who were treated for prostate cancer, Oberst et al. (2010) found that 28.6% (n = 76) of the men experienced iatrogenic physical disabilities reducing their work capacity at 12 months after diagnosis. At 18 months, the proportion of men affected by such disabilities was reduced to 17.2% (n = 46), suggesting that improvements occurred over time.
The experience of prostate cancer treatment side-effects determines men’s readiness to return to work (Grunfeld et al., 2013; Yu Ko et al., 2020). Yu Ko et al. (2020) indicated that the range and severity of postprostatectomy side-effects limited the types of tasks and roles men could fulfill at work. For example, men who experienced fatigue were unable to operate heavy equipment, while those with postsurgical abdominal pain could not move machinery unassisted. There is emerging evidence that some men are able to manage these limitations with workplace support. For example, Ullrich et al. (2017) reported that 35.8% (n = 220) of the participants made return to work arrangements that allowed them to gradually resume work, whereas Yu Ko et al. (2020) noted that men negotiated for favorable working conditions to ensure safety and ongoing postprostatectomy recovery upon returning to work.
Socioeconomic status is associated with the timing of men’s to return to work after prostate cancer treatment (Sharp & Timmons, 2011; Ullrich et al., 2017; von Mechow et al., 2018). Ullrich et al. (2017) reported that 69% (n = 80) of men from the lowest socioeconomic status had returned to work by the third month posttreatment compared with 29.2% (n = 50) of those in the highest socioeconomic bracket. However, divergent evidence was detailed by von Mechow et al. (2018) who reported median return to work time was 63 days for men who earned less than €2000 monthly (n = 74) versus 42 days for those who made over €4000 (n = 689). Regarding this, von Mechow et al. (2018) and Sharp and Timmons (2011) argued that men in the lowest income brackets were more likely to work in physically demanding jobs and that they required longer recovery times before resuming work activities than the men who were in the highest income brackets.
Self-employment and the lack of sick leave entitlements can determine the timing of men’s return to work after prostate cancer treatment (Gunnarsdottir et al., 2013; Sharp & Timmons, 2011; von Mechow et al., 2018). In an Irish study involving 100 working men treated for prostate cancer, Sharp and Timmons (2011) reported that self-employed participants were less likely to have work-sponsored benefits and resumed work earlier than employees (median = 17.2 weeks vs. 34.4 weeks). Similarly, von Mechow et al. (2018) noted that more self-employed men (24%; n = 339) reported that their return to work was premature than men who were employees (17%; n = 241). Related, the availability of workplace accommodations also influenced men’s return to work decisions in seven studies (Dahl et al., 2015; Grunfeld et al., 2013; Gunnarsdottir et al., 2013; von Mechow et al., 2018; Sharp & Timmons, 2011; Ullrich et al., 2017). For example, Sharp and Timmons (2011) noted that concern about the negative impact of work strain on posttreatment recovery was a factor that delayed men’s readiness to resume work. In this respect, Dahl et al. (2015) and Yu Ko et al. (2020) reported that work-role flexibility and employer support influenced men’s return to work. The fear of being seen as inferior workers was a barrier for men to fully disclose the impact of treatment side-effects on work capacity (Grunfeld et al., 2013; Yu Ko et al., 2020). Grunfeld et al. (2013) indicated that men worried about “appearing to be seeking sympathy” in the workplace and were reluctant to request posttreatment work accommodations. Yu Ko et al. (2020) reported that a competitive workplace fueled men’s fears about job security postradical prostatectomy. As a result, some men felt pressure to match their co-workers’ productivity levels amid their ongoing recovery and experience of surgery-related discomfort. Thus, suggesting that work-demands, competitiveness, and support in the workplace can influence men’s return to work in the aftermath of prostate cancer treatment.
Impact of Prostate Cancer Treatment on Men’s Finances
Time away from work to treat prostate cancer and its influence on income and financial stress was investigated in four studies (Arndt et al., 2019; Gordon et al., 2017; Sharp & Timmons, 2011; Ullrich et al., 2017). Sharp and Timmons (2011) reported that men who experienced reduced income and increased financial worries tended to prioritize return to work and that out-of-pocket expenses related to prostate cancer treatment (e.g., therapies not covered under health insurance, transportation to medical appointments) could exacerbate men’s vulnerability to financial uncertainty. Similarly, in a study involving 289 Australian men with prostate cancer (mean age=65.1; 71%; n = 205 of whom had private health insurance), Gordon et al. (2017) reported 70% (n = 202) of the participants spent more than they expected on out-of-pocket expenses related to their cancer treatment. Furthermore, 34% (n = 98) of the men described themselves as “just getting on” or “struggling” financially (Gordon et al., 2017). Recognizing that patient-borne expenses vary in different contexts and countries, these results indicate that out-of-pocket expenses related to prostate cancer can become a burden for men and their families.
The degree of financial support received by men treated for prostate cancer varies across socioeconomic status (Sharp & Timmons, 2011; Ullrich et al., 2017; von Mechow et al., 2018). Sharp and Timmons (2011) reported that more high-income individuals (59%; n = 59) received government and/or work-sponsored income-replacement benefits during their sick leave than those in the lowest income brackets (44%; n = 49). Men’s ability to generate income could also be affected by the physicality of their work. von Mechow et al. (2018) reported that German men who worked in physically straining occupations stayed off work longer, with potential financial implications. Premature retirement after prostate cancer treatment can also accentuate men’s financial difficulties. In a study that included 207 German men who were on average 55.4 years old and employed at the time of prostate cancer diagnosis, Arndt et al. (2019) reported that 9.7% (n = 20) of men had quit their jobs within 5 years of treatment because they were unable to meet work demands. Despite the availability of direct welfare payments for low-income individuals and people with disabilities (von Mechow et al., 2018), such benefits may not be available to all men with cancer and/or the amounts paid may not be sufficient to cover costs of living.
Discussion and Recommendations
The scoping review results indicate that prostate cancer treatment often impacts men’s return to work and work capacity. Studies indicate that men’s return to work may be more gradual than expected after prostate cancer treatment. Some men may feel pressured due to financial stressors to resume work. Diverse factors including older age and social benefits appear to play a significant role in shaping men’s work-related plans after prostate cancer treatment.
Absent in the selected literature were insights about the effectiveness of return to work accommodations in facilitating men’s full resumption of work activities, creating challenges for making evidence-based recommendations about how best to support men returning to work. There is an extensive body of research on the significance and impact of prostate cancer on men’s masculine identities (Kelly, 2009; Klaeson et al., 2012; Maliski et al., 2008; Oliffe, 2009) that could help guide future research about how men’s work-related decisions relate to workplace accommodations.
While evidence suggests that multidisciplinary interventions integrating physical exercise and occupational counseling improve return to work outcomes in breast, colorectal, and non-Hodgkin’s lymphoma (Leensen et al., 2017), none of the articles reviewed offered descriptions about the effectiveness of urinary continence interventions on work resumption. Future studies must explore the effectiveness of improving bladder control and work-fitness within the context of return to work. Further, interventions must consider the impact of masculinities in social and workplace contexts to enhance the uptake and effectiveness of interventions.
Though none of the studies reviewed explored the impact of aging on work capacity in the years following prostate cancer treatment, evidence suggests that work continuity results from the intertwined effects of men’s age, prostate cancer management, and changes in work demands (Yu Ko et al., 2020). Related, older men’s participation in the workforce (Mather et al., 2015) and rises in the prevalence of prostate cancer cases (Wong et al., 2016) suggest that an increasing number of males will be managing prostate cancer within the context of their working lives. Thus, a prostate cancer diagnosis might be understood as a health issue that can severely affect men’s work, career goals, and finances. Grunfeld et al. (2013) and Yu Ko et al. (2020) assertion that work retains central importance in men’s daily lives supports the need for future work to explore the ways men reposition work in relation to their health concerns and family relationships. This is important to understand the specific needs and unique challenges working men face when making prostate cancer treatment and work-related decisions posttreatment.
Reports that men are reluctant to disclose their health status or request assistance from co-workers after prostate cancer treatment (Grunfeld et al., 2013; Yu Ko et al., 2020) highlight two clinical practice issues. First, clinicians must advocate for patients’ recovery needs by gaining a better understanding of men’s work responsibilities and including ongoing work-capacity assessments as part of a comprehensive prostate cancer management plan. Further, clinicians can partner with employers to help retain skilled labor by offering individualized interventions (e.g., introducing breaks) within the context of work to reduce work-related injuries, improve productivity, and work longevity.
The second issue is related to expectations of productivity and competitiveness in the workplace (Grunfeld et al., 2013; Yu Ko et al., 2020). In this regard, men’s fears about being perceived as weak workers were linked, in part, to their concerns about reduced work output and job insecurity after prostate cancer treatment (Yu Ko et al., 2020). In this context, men treated for prostate cancer represent a population at risk for resuming work without having fully recovered from treatment and are at an increased risk for work-related injury or posttreatment complications. Recognizing that work capacity after prostate cancer treatment improves over time (Dahl, et al., 2015; Ullrich et al., 2017, 2020), clinical interventions should include tailored and incremental milestones toward graduated return to work.
Though legislation against discrimination at work is available in the countries of all reviewed articles (Australian Government, 2020; European Commission, 2020; Government of Canada, 2020; Government of Iceland, 2020; Government of Norway, 2020; Government of the United Kingdom, 2020; United States Department of Labor, 2020), little is known about their effectiveness on ensuring equal opportunities for men resuming work. Related, men fear work opportunity reductions (e.g., training, promotion) upon return to work postprostate cancer treatment (Grunfeld et al., 2013) and often overexert at work to make up for lost productivity (Yu Ko et al., 2020). This has two implications for industry. First, employers must establish a workplace culture wherein stigma against workers with prostate cancer and/or other health issues is eliminated. Further, employers must ensure equal opportunities for workers and making provisions to maintain a safe work environment; improving worker loyalty, teamwork, and productivity. Second, employers must proactively prevent overexertion and/or injury by workers who are recovering from prostate cancer treatment. This can be achieved through periodic evaluations on the appropriateness of return to work arrangements that include an assessment of men’s concerns about workloads/tasks and offer flexibility to change men’s work responsibilities in a way that fosters their ongoing recovery.
While various factors such as older age and chronic illnesses are known to be independently associated with reduced work capacity postprostate cancer treatment (Arndt et al., 2019; Bennett et al., 2018; Dahl et al., 2015, 2020; Sveistrup et al., 2016; Ullrich et al., 2017), missing in the reviewed articles are descriptions of the compounding effect of concomitant factors (e.g., cancer aggressiveness, financial need) on men’s decisions around return to work, career, and/or retirement. Further, despite the known factors that affect men’s return to work, patients are rarely aware of the impact of prostate cancer treatment on work capacity (Yu Ko et al., 2020). This gap in clinical practice should be addressed shortly after diagnosis and/or during the treatment decision-making process. In this regard, clinicians must discuss the potential impact of prostate cancer treatment side-effects and recovery on work, exploring options for rehabilitation, and/or plans for graduated return to work.
Reduced work capacity can be especially problematic for men of lower socioeconomic status (Gordon et al., 2017; Timmons & Sharp, 2011). While self-employment and the lack of sick leave benefits were found to shorten men’s time off work (Bennett et al., 2018; Gunnarsdottir et al., 2013; von Mechow et al., 2018; Yu Ko et al., 2020), there is a knowledge gap regarding the facilitators and barriers for men of lower socioeconomic status to transition to less demanding work roles. In this regard, future research might explore how physical rehabilitation and occupational re-training after prostate cancer treatment can be used to restore men’s work capacity and improve their employability.
Limitations
Several limitations are acknowledged. The inclusion of studies conducted in diverse countries with unique health service delivery, employment regulations, and social programs limits the generalizability of the findings. Indeed, findings on the facilitators and barriers for men’s return to work (e.g., laws protecting workers from layoff due to illness) cannot be standardized across studies for meaningful comparisons. Second, although the return to work rates were reported in most articles, the impact of prostate cancer treatment side-effects on work capacity in different types of occupations (i.e., desk vs. physically demanding jobs) have not been fully explored. This limitation can be addressed in future work to help design evidence-based interventions aimed at facilitating men’s return to work in different industries. Third, several studies measured return to work as an endpoint in men’s post-prostate cancer treatment and recovery (Arndt et al., 2019; Plym et al., 2016; von Mechow et al. 2018). However, Dahl et al. (2016), Sharp and Timmons (2011), Ullrich et al. (2017), and Yu Ko et al. (2020) argued that men’s return to work is also shaped by various factors including age, financial need, and retirement plans. Thus, return to work rates should be seen as only one event amid many with which to gauge the state of men’s postprostatectomy recovery.
Conclusion
Prostate cancer treatment affects men’s work capacity and shapes their career and retirement plans. Clinicians play an important role in men’s prostate cancer treatment decisions which, in turn, impact men’s work capacity. Further research is needed to identify the facilitators, barriers, and processes involved in men’s decisions to resume, or not, work activities and effectively support men’s prostate cancer treatment and work-related decisions.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Canadian Institutes of Health Research (CIHR: Grant#: 1R06913), the Men’s Health Research Program at the University of British Columbia (www.menshealthresearch.ubc.ca), and the School of Nursing at the University of British Columbia (www.nursing.ubc.ca).
ORCID iDs: Wellam F. Yu Ko  https://orcid.org/0000-0001-5504-9707
https://orcid.org/0000-0001-5504-9707
John L. Oliffe  https://orcid.org/0000-0001-9029-4003
https://orcid.org/0000-0001-9029-4003
Joan L. Bottorff  https://orcid.org/0000-0001-9724-5351
https://orcid.org/0000-0001-9724-5351
References
- American Cancer Society. (2020). Survival rates for prostate cancer. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/survival-rates.html
- Arksey H., O’Malley L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Arndt V., Koch-Gallenkamp L., Bertram H., Eberle A., Holleczek B., Pritzkuleit R., Brenner H. (2019). Return to work after cancer. A multi regional population-based study from Germany. Acta Oncologica, 58(5). doi: 10.1080/0284186X.2018.1557341 [DOI] [PubMed] [Google Scholar]
- Australian Government. (2020). Fair Work Ombudsman – Protection from discrimination at work. https://www.fairwork.gov.au/employee-entitlements/protections-at-work/protection-from-discrimination-at-work
- Bennett D., Kearney T., Donnelly D. W., Downing A., Wright P., Wilding S., Gavin A. (2018). Factors influencing job loss and early retirement in working men with prostate cancer: Findings from the population-based Life After Prostate Cancer Diagnosis (LAPCD) study. Journal of Cancer Survivorship, 12(5), 669–678. doi: 10.1007/s11764-018-0704-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley C. J., Neumark D., Lou Z., Bednareck H., Schenk M. (2005). Employment outcomes of men treated for prostate cancer. Journal of the National Cancer Institute, 97(13), 958–965. [DOI] [PubMed] [Google Scholar]
- Bradley C. J., Oberst K., Schenk M. (2006). Absenteeism from work: The experience of employed breast and prostate cancer patients in the months following diagnosis. Psycho-Oncology, 15(8), 739–747. doi: 10.1002/pon.1016 [DOI] [PubMed] [Google Scholar]
- Canadian Cancer Society. (2020. a). Prostate cancer statistics. https://www.cancer.ca/en/cancer-information/cancer-type/prostate/statistics/?region=ab
- Canadian Cancer Society. (2020. b). Survival statistics for prostate cancer. https://www.cancer.ca/en/cancer-information/cancer-type/prostate/prognosis-and-survival/survival-statistics/?region=ab
- Canadian Cancer Society’s Steering Committee on Cancer Statistics. (2012). Canadian cancer statistics 2012. Canadian Cancer Society. [Google Scholar]
- Emslie C., Hunt K. (2009). ‘Live to work’ or ‘Work to live’? A qualitative study of gender and work-life balance among men and women in mid-life. Gender, Work & Organization, 16(1), 151–172. doi: 10.1111/j.1468-0432.2008.00434.x [DOI] [Google Scholar]
- European Commission. (2020). Employment, social affairs & Inclusion: Tackling discrimination at work. https://ec.europa.eu/social/main.jsp?catId=158&langId=en
- Dahl A. A., Brennhovd B., Fosså S. D., Axcrona K. (2020). A cross-sectional study of current work ability after radical prostatectomy. BMC Urology, 20(9), 1–7. doi: 10.1186/s12894-020-0579-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl S., Cvancarova M., Dahl A. A., Fosså S. D. (2016). Work ability in prostate cancer survivors after radical prostatectomy. Scandinavia Journal of Urology, 50(2), 116–122. doi: 10.3109/21681805.2015.1100674. [DOI] [PubMed] [Google Scholar]
- Dahl S., Loge H. J., Berge V., Dahl A. A., Cvancarova M., Fosså S. D. (2015). Influence of radical prostatectomy for prostate cancer on work status and working life 3 years after surgery. Journal of Cancer Survivorship, 9(2), 172–179. doi: 10.1007/s11764-014-0399-6 [DOI] [PubMed] [Google Scholar]
- Dahl S., Steinsvik E. A. S., Dahl A. A., Loge J. H., Cvancarova M., Fosså S. D. (2014). Return to work and sick leave after radical prostatectomy: A prospective clinical study. ActaOncologica, 53(6), 744–751. doi: 10.3109/0284186X.2013.844357 [DOI] [PubMed] [Google Scholar]
- Gordon L. G., Walker S. M., Mervin M. C., Lowe A., Smith D. P., Gardiner R. A., Chambers S. K. (2017). Financial toxicity: A potential side effect of prostate cancer treatment among Australian men. European Journal of Cancer Care, 26(1), e12392. doi: 10.1111/ecc.12392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Canada. (2020). Rights in the workplace. https://www.canada.ca/en/canadian-heritage/services/rights-workplace.html
- Government of Iceland. (2020). Labour market and employment. https://www.government.is/topics/labour-market-and-employment/
- Government of Norway. (2020). Anti-Discrimination-Act. https://www.regjeringen.no/en/dokumenter/the-anti-discrimination-act/id420606/
- Government of the United Kingdom. (2020). Discrimination: Your rights – Discrimination at work. https://www.gov.uk/discrimination-your-rights/discrimination-at-work
- Grunfeld E. A., Drudge-Coates L., Rixon L., Eaton E., Cooper A. F. (2013). “The only way I know how to live is to work”: A qualitative study of work following treatment for prostate cancer. Health Psychology, 32(1), 75–82. doi: 10.1037/a0030387 [DOI] [PubMed] [Google Scholar]
- Gunnarsdottir H. K., Vadarsdottir H., Rafnsdottir G. L., Tryggvadottir L., Ofafsdottir E. J., Lindbohm M-L. (2013). Employment participation and work experience of male cancer survivors: A NOCWO study. Work, 46(4), 385–394. doi: 10.3233/WOR-131674 [DOI] [PubMed] [Google Scholar]
- Kelly D. (2009). Changed men: The embodied impact of prostate cancer. Qualitative Health Research, 19(2), 151–163. doi: 10.1177/1049732308328067 [DOI] [PubMed] [Google Scholar]
- Klaeson K., Sandell K., Berterö C. M. (2012). Sexuality in the context of prostate cancer narratives. Qualitative Health Research, 22(9), 1184–1194. doi: 10.1177/1049732312449208 [DOI] [PubMed] [Google Scholar]
- Leensen M. C. J., Groeneveld I. F., Heide I. V. D., Rejda T., van Veldhoven P. L. J., van Berkel, de Boer A. G. E. M. (2017). Return to work of cancer patients after a multidisciplinary intervention including occupational counselling and physical exercise in cancer patients: A prospective study in the Netherlands. Occupational and Environmental Medicine, 7(6), e014746. doi: 10.1136/bmjopen-2016-014746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacEwen A. (2012). Working after age 65: What is at stake? Alternative federal budget 2012 technical paper. Canadian Centre for Policy Alternatives; https://www.policyalternatives.ca/publications/reports/working-after-age-65 [Google Scholar]
- Maliski S. L., Rivera S., Connor S., Lopez G., Litwin M. S. (2008). Renegotiating masculine identity after prostate cancer treatment. Qualitative Health Research, 18(12), 1609–1620. doi: 10.1177/1049732308326813. [DOI] [PubMed] [Google Scholar]
- Mather M., Jacobsen L., Pollard K. (2015). Aging in the United States. Population Bulletin, 70(2). https://www.prb.org/wp-content/uploads/2016/01/aging-us-population-bulletin-1.pdf [Google Scholar]
- von Mechow S., Graefen M., Haese A., Tennstedt P., Pehrke M., Friedersdorff F., Beyer B. (2018). Return to work following robot-assisted laparoscopic and open retropubic radical prostatectomy: A single-center cohort study to compare duration of sick leave. Urologic Oncology, 36(6), 309.e1-309.e6. doi: 10.1016/j.urolonc.2018.02.006 [DOI] [PubMed] [Google Scholar]
- Nilsson R., Dahl A. A., Bernklev T., Kersten H., Haug E. S. (2020). Work status and work ability after radical prostatectomy or active surveillance for prostate cancer. Scandinavian Journal of Urology, 54(3), 194–200. doi: 10.1080/21681805.2020.1750473 [DOI] [PubMed] [Google Scholar]
- Oberst K., Bradley C. J., Gardiner J. C., Shenck M., Given C. W. (2010). Work task disability in employed breast and prostate cancer patients. Journal of Cancer Survivorship. 4(4), 322–330. doi: 10.1007/s11764-010-0128-8 [DOI] [PubMed] [Google Scholar]
- Oliffe J. (2009). Positioning prostate cancer as the problematic third testicle. In Broom A., Torvey P. (Eds.) Men’s health: Body identity and social context (pp. 33–62). Wiley-Blackwell. [Google Scholar]
- Plym A., Chiesa F., Voss M., Holmberg L., Johansson E., Stattin P., Lambe M. (2016). Work disability after robot-assisted or open radical prostatectomy: A nationwide, population-based study. European Urology, 70(1), 64–71. doi: 10.1016/j.eururo.2015.12.049 [DOI] [PubMed] [Google Scholar]
- Quon H., Loblaw A., Nam R. (2011). Dramatic increase in prostate cancer cases by 2021. British Journal of Urology International, 108(11), 1734–1738. doi: 10.1111/j.1464-410X.2011.10197.x [DOI] [PubMed] [Google Scholar]
- Sharp L., Timmons A. (2011). Social welfare and legal constraints associated with work among breast and prostate cancer survivors: Experiences from Ireland. Journal of Cancer Survivorship, 5(4), 382–394. doi: 10.1007/s11764-011-0183-9 [DOI] [PubMed] [Google Scholar]
- Sharp L., Timmons A. (2016). Pre-diagnosis employment status and financial circumstances predict cancer-related financial stress and strain among breast and prostate cancer survivors. Supportive Cancer Care, 24(2), 699–709. doi: 10.1007/s00520-015-2832-4 [DOI] [PubMed] [Google Scholar]
- Sun Life Canadian Unretirement Index.(2015). 2015Canadian unretirement index report. Sun Life Assurance Company of Canada. [Google Scholar]
- Sveistrup J., Mortensen O. S., Rosenchöld P. M., Engelholm S. A., Pertersen P. M. (2016). Employment and sick leave in patients with prostate cancer before, during and after radiotherapy. Scandinavian Journal of Urology, 50(3), 164–169. doi: 10.3109/21681805.2015.1119190 [DOI] [PubMed] [Google Scholar]
- Ullrich A., Rath H. M., Otto U., Kerschgens C., Ralda M., Hagen-Aukamp C., Bergelt C. (2017). Outcomes across the return-to-work process in PC survivors attending a rehabilitation measure - Results from a prospective study. Supportive Cancer Care, 25(10), 3007–3015. doi: 10.1007/s00520-017-3790-9 [DOI] [PubMed] [Google Scholar]
- Ullrich A., Rath H. M., Otto U., Kerschgens C., Ralda M., Hagen-Aukamp C., Bergelt C. (2020). Identifying expectations of delayed return to work in patients with prostate cancer at the beginning of a cancer rehabilitation program. Journal of Occupational Rehabilitation, 30(2), 183–193. doi: 10.1007/s10926-019-09860-3 [DOI] [PubMed] [Google Scholar]
- United States Department of Labor. (2017). Civilian labor force participation rate, by age, sex, race, and ethnicity. https://www.bls.gov/emp/tables/civilian-labor-force-participation-rate.htm
- United States Department of Labor. (2020). Americans with Disabilities Act. https://www.dol.gov/general/topic/disability/ada
- Wong M. C., Goggins W. B., Wang H. H., Fung F. D., Leung C., Wong S. Y., Sung J. J. (2016). Global incidence and mortality for prostate cancer: Analysis of temporal patterns and trends in 36countries. European Urology, 70(5), 862–874. doi: 10.1016/j.eururo.2016.05.043. [DOI] [PubMed] [Google Scholar]
- Yu Ko W. F., Oliffe J. L., Johnson J. L., Bottorff J. L. (2020). Reformulating the worker identity: Men’s experiences after radical prostatectomy. Qualitative Health Research, 30(8), 1225–1236. doi: 10.1177/1049732318825150. [DOI] [PubMed] [Google Scholar]