Introduction
Heart rate variability (HRV), the variation in time intervals between consecutive heart beats, is commonly used to index the functionality of the cardiac autonomic nervous system in healthy individuals and patients suffering from various cardiovascular and non-cardiovascular disorders.1 However, there are currently no population-based HRV reference values for men and women separately covering a wide age range, with the notable exception of the recent work of van den Berg and colleagues who described this for 10-second (ultra-short) electrocardiogram recordings.2 While highly valued, in their study HRV data were derived from multiple cohorts using different electrocardiogram recording techniques, and a sample-dependent, exponential correction formula was used to correct for the influence of mean heart rate on HRV. We therefore aim to estimate HRV reference values derived from 10-second electrocardiogram, both uncorrected and generically corrected for heart rate,3 from a single population sample with a wide age range.
Methods
Data from a large population-based study in the north of The Netherlands aiming to investigate risk factors for multifactorial diseases4 (Lifelines Cohort Study and Biobank) were used. From 10-second resting electrocardiogram recordings, inter-beat intervals (IBIs, in ms) were obtained from 153,793 participants. Participants with cardiovascular disease, hypertension, type 2 diabetes, obesity and the use of anti-depressants, beta-blockers and vagal modulating agents were excluded (n = 64,433) as were electrocardiogram recordings with excessive noise and ectopic (non-sinus node) beats (n = 4586). HRV values were estimated from the remaining 84,772 participants (59.5% women; mean age 40.8 (range 13–91) years). Details on HRV calculation have been published elsewhere.5 In short, the root mean square of successive differences (RMSSD, in ms) between IBIs were calculated as HRV index. In addition, taking into account the effect of mean IBI, corrected RMSSD (cRMSSD) was calculated.3 We categorised participants into 12 5-year age bins. Centile curves, as a function of age, were estimated using the Box–Cox T-distribution of the gamlss function in R. Comparable with the recent paper by van den Berg et al.,2 we chose to report the 2nd and 98th percentiles as lower and upper limits, respectively. The study was approved by the medical ethical committee of the University Medical Center Groningen. All participants were fully informed and gave consent prior to participation.
Results and discussion
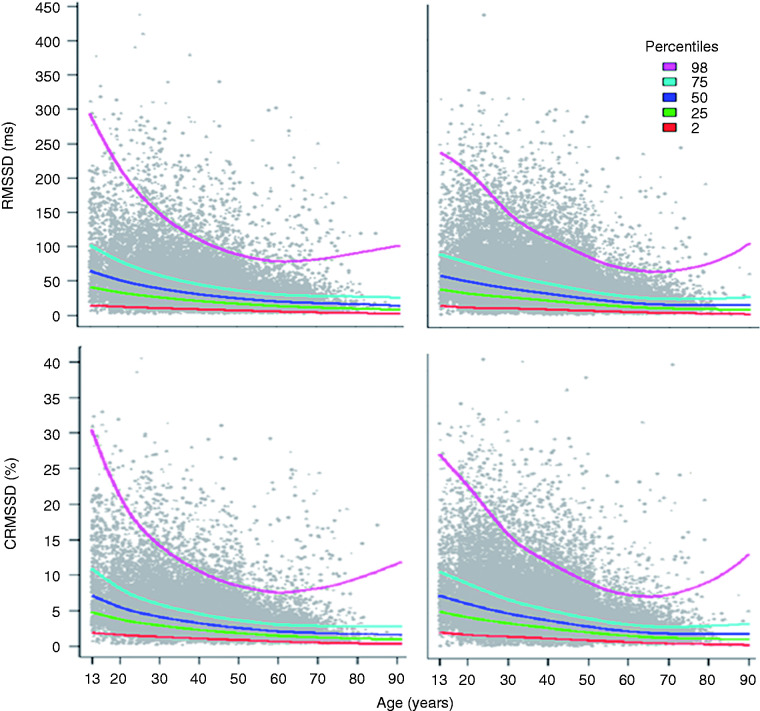
The mean of IBI, median, 2nd and 98th percentiles of RMSSD and cRMSSD per age bin, for women and men separately, are given (Table 1). Men had higher IBIs at all ages. For women the highest median RMSSD of 66.5 ms was observed in the youngest age category (13–14 years) and lowest value of 16.1 ms in the oldest age category (75 + years). This was comparable for men with values of 67.4 and 14.9 ms, respectively. Figure 1 illustrates the centile curves as a function of age. In both sexes, the 25th percentile, median and 75th percentile of RMSSD steadily became lower from a young age until age 60 years, and then remained stable. There is also a sharp drop of the 98th percentile from the younger to the older age bins until age 60 years, after which it shows a rise resulting in a wider range of RMSSD values in individuals from age 60 years onwards. The lower normal limit is, however, remarkably stable throughout the lifespan of both sexes. Women aged 20–45 years had on average 5.02 ms significantly higher median RMSSD values than men, and the difference was smaller (2.53 ms) in the age bin 45–59 years but was still significant. There were no sex differences in RMSSD values in the age bins below age 20 years and above age 60 years. Similar results were found for cRMSSD, including the pattern of centile curves as a function of age. With the notable exception for the median sex differences in cRMSSD which were more pronounced and applicable in a wider age range (15–75 years).
Table 1.
Reference values of RMSSD and cRMSSD per age bin for women and men separately.
| Age bins (years) | Sex | N | Mean IBI (ms) |
RMSSD (ms) |
cRMSSD (%) |
||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Median (2nd, 98th percentile) | P valuea | Mean (SD) | Median (2nd, 98th percentile) | P valuea | |||
| 13–14 | Women | 275 | 862.2 (134.6) | 77.7 (51.3) | 66.5 (17.4; 232.2) | 0.865 | 8.8 (5.3) | 7.6 (2.4; 26.6) | 0.865 |
| Men | 278 | 896.9 (128.2) | 80.3 (53.6) | 67.4 (12.8; 213.0) | 8.7 (5.3) | 7.5 (1.7; 22.0) | |||
| 15–19 | Women | 1787 | 890.7 (146.8) | 73.8 (50.5) | 60.7 (12.4; 225.9) | 0.526 | 8.0 (4.9) | 6.9 (1.7; 22.8) | 0.001 |
| Men | 1089 | 948.4 (163.9) | 70.8 (48.8) | 59.9 (9.8; 213.2) | 7.3 (4.7) | 6.3 (1.3; 20.9) | |||
| 20–24 | Women | 3478 | 886.7 (144.7) | 64.7 (47.3) | 52.1 (11.3; 205.5) | ≤0.001 | 7.0 (4.5) | 5.9 (1.6; 20.6) | ≤0.001 |
| Men | 1653 | 941.7 (159.6) | 57.3 (40.1) | 47.6 (9.6; 174.0) | 5.9 (3.7) | 5.0 (1.4; 17.1) | |||
| 25–29 | Women | 5262 | 902.8 (144.9) | 58.0 (40.0) | 47.5 (11.5; 180.7) | ≤0.001 | 6.2 (3.7) | 5.3 (1.6; 17.4) | ≤0.001 |
| Men | 3454 | 951.9 (162.7) | 52.1 (38.8) | 42.3 (10.1; 172.7) | 5.3 (3.5) | 4.4 (1.3; 16.5) | |||
| 30–34 | Women | 5307 | 917.2 (138.9) | 51.6 (35.4) | 42.3 (11.5; 161.0) | ≤0.001 | 5.4 (3.3) | 4.7 (1.5; 15.4) | ≤0.001 |
| Men | 4058 | 959.9 (158.7) | 45.4 (32.4) | 36.9 (10.2; 140.8) | 4.6 (2.9) | 3.9 (1.3; 13.2) | |||
| 35–39 | Women | 6437 | 921.6 (137.0) | 46.0 (31.9) | 37.9 (10.8; 141.9) | ≤0.001 | 4.8 (2.9) | 4.1 (1.4; 13.9) | ≤0.001 |
| Men | 4456 | 957.0 (155.3) | 39.9 (28.1) | 32.8 (8.6; 123.8) | 4.0 (2.5) | 3.5 (1.1; 11.4) | |||
| 40–44 | Women | 8315 | 922.8 (138.7) | 41.0 (28.6) | 33.9 (9.7; 123.7) | ≤0.001 | 4.3 (2.7) | 3.7 (1.2; 12.0) | ≤0.001 |
| Men | 5507 | 959.5 (155.2) | 35.2 (24.7) | 29.0 (8.1; 105.5) | 3.5 (2.2) | 3.0 (1.0; 10.3) | |||
| 45–49 | Women | 8643 | 916.6 (137.4) | 35.6 (25.5) | 29.2 (8.3; 109.5) | ≤0.001 | 3.7 (2.4) | 3.2 (1.1; 10.8) | ≤0.001 |
| Men | 5947 | 962.5 (157.7) | 31.6 (22.9) | 26.0 (7.1; 95.5) | 3.2 (2.1) | 2.7 (0.9; 9.3) | |||
| 50–54 | Women | 4907 | 916.9 (135.8) | 31.8 (22.0) | 26.6 (7.5; 96.3) | ≤0.001 | 3.3 (2.1) | 2.9 (1.0; 9.5) | ≤0.001 |
| Men | 3396 | 960.1 (150.1) | 28.7 (20.2) | 23.7 (6.7; 87.5) | 2.9 (1.8) | 2.5 (0.9; 8.5) | |||
| 55–59 | Women | 2422 | 909.0 (132.1) | 27.2 (19.4) | 22.5 (6.7; 83.6) | 0.003 | 2.9 (1.9) | 2.5 (0.9; 8.5) | ≤0.001 |
| Men | 1650 | 961.6 (150.0) | 26.2 (21.9) | 21.0 (5.5; 89.5) | 2.6 (2.0) | 2.2 (0.7; 8.4) | |||
| 60–64 | Women | 1968 | 898.0 (131.1) | 25.2 (20.0) | 20.5 (5.5; 79.3) | 0.025 | 2.7 (2.0) | 2.3 (0.7; 8.5) | ≤0.001 |
| Men | 1342 | 957.9 (150.1) | 24.8 (25.0) | 19.1 (4.8; 86.6) | 2.5 (2.4) | 2.0 (0.6; 9.1) | |||
| 65–69 | Women | 1036 | 888.9 (127.7) | 22.9 (20.6) | 17.8 (5.0; 83.0) | 0.632 | 2.5 (2.2) | 2.0 (0.6; 8.8) | 0.008 |
| Men | 834 | 945.9 (145.7) | 24.4 (24.9) | 17.7 (4.87; 110.5) | 2.5 (2.5) | 1.9 (0.6; 11.4) | |||
| 70–74 | Women | 403 | 890.2 (121.2) | 25.2 (31.3) | 18.3 (5.0; 115.8) | 0.024 | 2.7 (3.2) | 2.0 (0.6; 12.9) | ≤0.001 |
| Men | 355 | 936.3 (139.3) | 27.2 (37.6) | 16.0 (4.7; 161.9) | 2.8 (3.8) | 1.6 (0.5; 16.6) | |||
| 75+ | Women | 172 | 860.5 (131.9) | 24.0 (25.0) | 16.1 (3.5; 106.2) | 0.295 | 2.7 (2.8) | 1.9 (0.5; 14.4) | 0.053 |
| Men | 140 | 931.2 (128.7) | 25.4 (31.8) | 14.9 (3.7; 130.3) | 2.7 (3.3) | 1.6 (0.5; 17.4) | |||
Values are given as mean (SD) and as median (2nd and 98th percentiles).
IBI: inter-beat interval; RMSSD: root mean square of successive differences; cRMSSD: corrected root mean square of successive differences.
Differences in RMSSD median values between women and men.
Figure 1.
Centile curves of RMSSD (top) and cRMSSD (bottom) as a function of age for men (left) and women (right). RMSSD: root mean square of successive differences; cRMSSD: corrected root mean square of successive differences.
In conclusion, we provide population-based RMSSD and cRMSSD reference values using 10-second resting electrocardiogram recordings, from a single cohort with a wide age range. These reference values were derived from a sample at least six times larger than previous studies. These age and sex-specific RMSSD values constitute benchmarks for application in both research and clinical settings in which indications on physiologically plausible ranges are highly valuable.
Footnotes
Author contribution: BST, HS and HR contributed to the conception or design of the work. BST, TM, AMR, HS and HR contributed to the acquisition, analysis, or interpretation of data for the work. BST drafted the manuscript. All authors critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work ensuring integrity and accuracy.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: the Lifelines Cohort Study and Biobank is supported by the Netherlands Organization of Scientific Research grant 175.010.2007.006, the Economic Structure Enhancing Fund of the Dutch government, the Ministry of Economic Affairs, the Ministry of Education, Culture and Science, the Ministry for Health, Welfare and Sports, the Northern Netherlands Collaboration of Provinces, the Province of Groningen, University Medical Center Groningen, the University of Groningen, Dutch Kidney Foundation and Dutch Diabetes Research Foundation.
References
- 1.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Eur Heart J 1996; 17: 354–381. [PubMed] [Google Scholar]
- 2.van den Berg ME, Rijnbeek PR, Niemeijer MN, et al. Normal values of corrected heart-rate variability in 10-second electrocardiograms for all ages. Front Physiol 2018; 9: 424–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Roon AM, Snieder H, Lefrandt JD, et al. Parsimonious correction of heart rate variability for its dependency on heart rate. Hypertension 2016; 68: e63–e65. [DOI] [PubMed] [Google Scholar]
- 4.Scholtens S, Smidt N, Swertz MA, et al. Cohort Profile: LifeLines, a three-generation cohort study and biobank. Int J Epidemiol 2015; 44: 1172–1180. [DOI] [PubMed] [Google Scholar]
- 5.Tegegne BS, Man T, van Roon AM, et al. Determinants of heart rate variability in the general population: the Lifelines Cohort Study. Heart Rhythm 2018; 15: 1552–1558. [DOI] [PubMed] [Google Scholar]