Abstract
Background
Singapore saw an escalation of coronavirus disease 2019 (COVID-19) cases from under 4,000 in April 2020 to over 40,000 in June 2020 largely attributed to spread within shared facilities housing foreign workers. Appropriate triage and escalation of clinical care are critical for this patient group managed in community care facilities (CCFs).
Purpose
To evaluate the imaging guideline recommendations for COVID-19 from the Fleischner Society and analyze the clinical utility of chest radiograph screening for asymptomatic or minimally symptomatic patients with COVID-19.
Materials and Methods
In this retrospective study, patients with COVID-19 confirmed by reverse transcriptase polymerase chain reaction (RT-PCR) who were admitted to Singapore Expo, a designated CCF, for continuation of their management during May 3-31, 2020 were identified. Upon admission, patients aged 36 and older without any baseline chest imaging received a chest radiograph. All chest radiographs and clinical outcomes of patients including those who were subsequently transferred to acute hospitals for escalation of care were reviewed. Key proportions of patients with findings of pulmonary infection and those requiring further inpatient treatment were calculated, and 95% binomial proportion confidence intervals obtained using the Clopper-Pearson method.
Results
The study included 5,621 patients: all men 100% (5,621/5,621), mean age 37 ± 8 years (range 17-60). A total of 1,964 chest radiographs were performed of which normal accounted for 98.0% (1,925/1,964) and findings of pulmonary infection represented 2.0% (39/1,964). Only 0.2% (4/1,964) with chest radiograph findings of pulmonary infection (all of whom were symptomatic) required supplemental oxygenation and inpatient treatment. None of the asymptomatic patients with findings of pulmonary infection required supplemental oxygenation, and they received only symptomatic treatment.
Conclusion
In accordance with Fleischner Society recommendations, chest radiograph screening for patients with COVID-19 aged 17-60 with mild or no symptoms is not indicated unless there is risk of clinical deterioration.
See also the editorial by Schaefer-Prokop and Prokop.
Summary
In accordance with Fleischner Society recommendations, chest radiograph screening in young and middle-aged adults with asymptomatic or minimally symptomatic COVID-19 is not indicated unless there is risk of deterioration.
Key Results
■ In 1,964 asymptomatic or minimally symptomatic patients with COVID-19, more than 98% had normal chest radiographs.
■ Among 39 chest radiographs with findings of pulmonary infection, only 4 were of patients who subsequently required inpatient treatment for oxygen support and IV medication.
■ All 14 asymptomatic patients with findings of pulmonary infection admitted to hospital remained well without supplemental oxygen.
Introduction
The outbreak of the coronavirus disease 2019 (COVID-19) that started in December 2019 in Wuhan China was characterized as a worldwide pandemic by the World Health Organization (WHO) in March of 2020 (1,2). Cases have since increased exponentially around the world with many countries facing an unprecedented healthcare crisis with broad socioeconomic ramifications (3). Worldwide, there were 34 million cases, 1 million deaths, and 188 countries affected as of October 2020 (4).
Singapore received global recognition with its comprehensive policy to contain the epidemic early on (5,6). But a second wave of rapid spread among its foreign workers housed in shared facilities resulted in a surge of cases from 4,000 in April to over 40,000 in June 2020 (7). This was due in part to aggressive testing to assess the extent of infections in foreign worker dormitories (8). The majority of these patients were young and asymptomatic or minimally symptomatic. To contain the spread within dormitories without overwhelming hospital systems, several convention centers, hotels, and temporary facilities were converted into community care facilities (CCF) designed to provide clinical care for these patients (9–11). The largest was the CCF at Singapore Expo, a convention center with 10 halls, fitted with a capacity to accommodate 7,873 residents (12). Our institution, SingHealth, was tasked to operationalize four halls, with a capacity of 3,200 residents, beginning on May 3, 2020.
CT is more sensitive than chest radiography in diagnosing and prognosticating COVID-19 pneumonia early in the disease course (13,14), but its application as a screening modality is hindered by readiness to cope with the volume and the necessary safety precautions required (15). While chest radiography has the logistical advantage compared to CT, its clinical utility is dependent on the temporal relationship to symptom onset and largely studied in the context of patients presenting to emergency departments and hospitalized patients (16,17).
The Fleischner Society has put forth a consensus statement on imaging recommendations for three COVID-19 scenarios stratified by clinical risk of disease progression (18). For patients with mild features of COVID-19 without risk of disease progression, imaging is not advised. Similarly, the American College of Radiology has also recommended that the use of chest radiography in ambulatory settings be considered when medically necessary (19). The purpose of this study was to evaluate the Fleischner Society recommendations with clinical data collected from a large sample of patients with asymptomatic or minimally symptomatic COVID-19.
Methods and Materials
This was an Institutional Review Board approved retrospective study where informed patient consent was waived as the process of obtaining consent was deemed impracticable due to the large patient volume and complex Singapore Expo CCF workflow.
Patients
All patients admitted to Singapore Expo under the care of SingHealth during May 3 – 31st 2020 were included in the study. The majority of patients were transferred from dormitories and hotels where the initial clinical assessment and COVID-19 RT-PCR testing (using test kits approved by the Health Sciences Authority, Singapore) (19) were carried out. Across Singapore there are more than 300,000 foreign workers housed in 43 mega-dormitories with capacities ranging from 1,500 to 25,000 and many smaller sized factory converted dormitories (22,23). Patients with COVID-19, mild respiratory disease as defined previously (18), and who fulfill CCF admission criteria were transferred to Singapore Expo (12). CCF admission criteria included COVID-19 confirmation by RT-PCR, no fever or supplemental oxygen required for three days or more, activities of daily living independent, and with no medical indications or comorbidities requiring inpatient care. Exclusion criteria were patients who were 36 years or less in age and for whom the clinical team deemed chest radiography not indicated, and those above 36 years of age who already had baseline chest radiography prior to transfer to CCF.
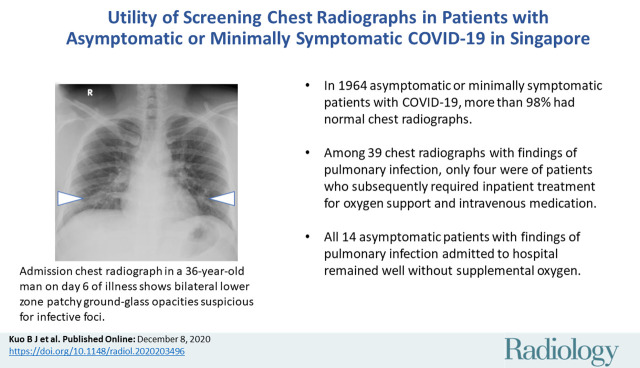
Singapore Expo Operational Workflow
The admission workflow operated sequentially through several stations involving security check, registration, medical assessment, chest radiograph screening, and on-boarding (Fig 1). Patients were required to submit vital parameters daily including heart rate, blood pressure, and oxygen saturation at self-monitoring stations throughout the CCF (24). There were sickbay centers within each hall that operated like primary care clinics in the daytime. They were staffed by doctors and nurses to manage both acute and chronic illnesses. There were also virtual telecommunication medical stations that were monitored by doctors twenty-four hours a day. Furthermore, a review process was in place for patients that needed to be transferred to acute hospitals for further escalation of care. The remaining patients were subsequently discharged to community or step-down community recovery facilities (CRF), which included government contracted hotels, cruise ships, and temporary facilities after remaining stable for 14-21 days from symptom onset.
Figure 1:
Workflow diagram illustrating the sequential stations of the admission process for patients with COVID-19 admitted into a community care facility, Singapore Expo, during May 3-31 for continuation of their management.
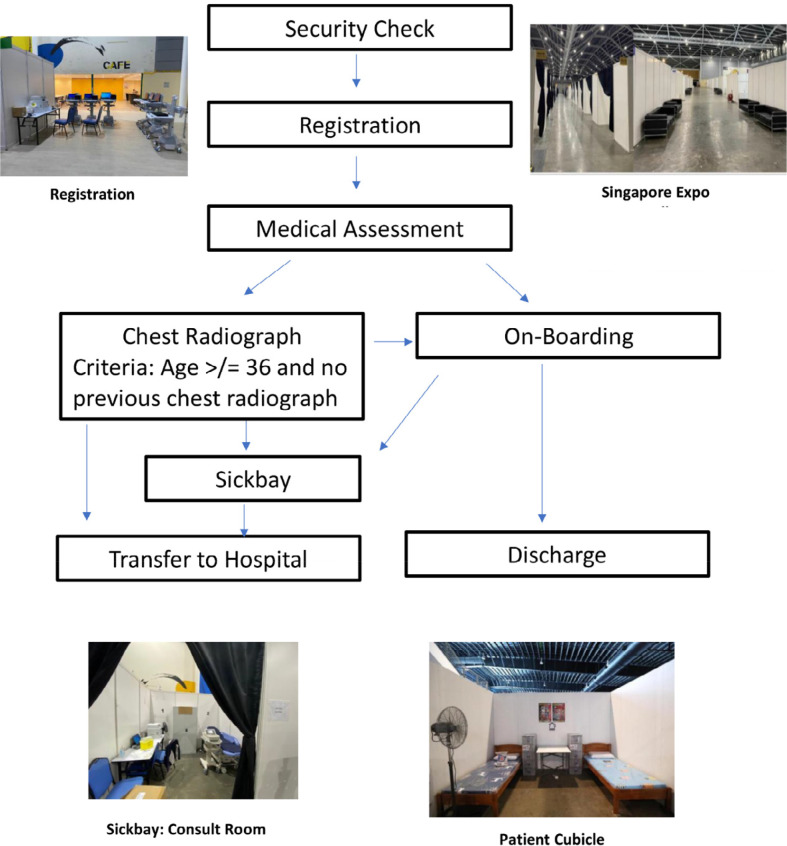
Chest Radiograph Workflow and Image Analysis
All patients aged 36 and older who had no baseline chest imaging received a chest radiograph upon admission (Fig 2). Additionally, patients with abnormal respiratory exam findings or other medical indications also received a chest radiograph regardless of age. All chest radiographs were acquired as digital radiographs as per local protocols by SATA CommHealth, a private company that specializes in community health screening. Chest radiographs were acquired in the posteroanterior projection from two portable X-ray systems (Fujifilm Velocity, Fujifilm, Tokyo, Japan) and images were read by one radiologist (Tan ML with ten years of experience post board certification). Radiographic features of consolidation or ground-glass opacities (GGOs) were flagged as abnormal, categorized as findings of pulmonary infection, and the results conveyed to the clinical team. The final decision for transfer to hospital was left to the managing clinical team. Guidance was given by facility leadership, however, to err on the side of caution for patients who had chest radiographic features of pulmonary infection and who were within seven days of symptom onset as they were deemed at higher risk of deterioration, regardless of symptom status. Non-pneumonic abnormalities which included pulmonary scarring, granuloma, pulmonary nodule, scoliosis, old fractures were categorized as normal for the purposes of analysis.
Figure 2:
Diagram illustrating the screening chest radiograph workflow for patients with COVID-19 admitted to a community care facility, Singapore Expo, during May 3-31. Patients aged 36 and older who had no baseline chest imaging received a screening chest radiograph. Additionally, patients who reported ill with respiratory symptoms during admission or subsequently to sick bay also received a chest radiograph regardless of age. Those with pulmonic changes on chest radiographs are either transferred to hospital if they are within 7 days of illness or deemed at risk of clinical deterioration.
Clinical Data Collection
Demographic variables collected included age and ethnicity. Clinical variables were obtained from an electronic health record platform, GPConnect (Integrated Health Information Systems, Singapore, Singapore). Data obtained included symptom onset date, symptoms, underlying chronic illnesses when available, and vitals. Clinical outcomes of patients transferred to hospital for respiratory indications, which include both clinical and radiographic indication of respiratory infection, were tracked up to one month beyond the study period (June 30, 2020). These included mortality, requiring inpatient care as defined by patients on supplemental oxygen, intravenous (IV) medications, invasive procedures such as bronchoscopy, chest drains, high-dependency (HD), or intensive care unit (ICU) support. Outcomes of patients who remained stable in Singapore Expo until discharge to CRFs were also collected. Additionally, the mortality and number of patients transferred for non-respiratory reasons were evaluated.
Statistical Analysis
Proportion of normal radiographs and chest radiographs with findings of pulmonary infection were calculated and trended by days from symptom onset. The proportion of patients requiring inpatient care, chronic illness and incidental issue treatment were determined. Additionally, proportion of patients who did not receive chest radiographs and were transferred to hospitals for respiratory symptoms were calculated.
Two-sided 95% Clopper-Pearson (exact) confidence interval (CI) uncertainty measures on estimated binomial proportions were obtained using SAS v9.4 statistical software (SAS Institute Inc., Cary, NC, USA).
Results
Patient Characteristic and Screening Chest Radiograph Findings
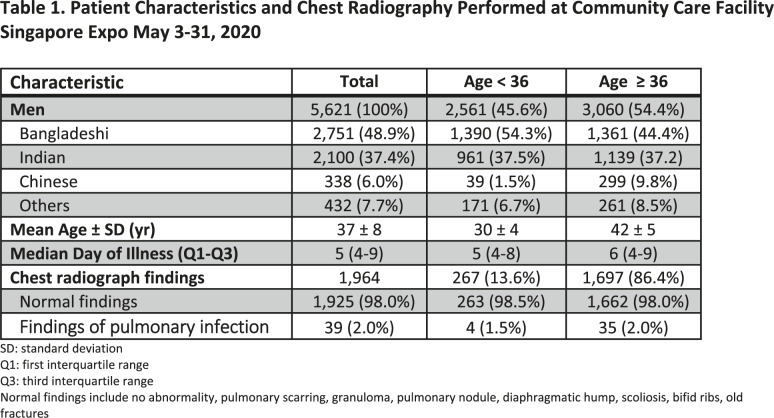
A total of 5,621 patients with COVID-19 were admitted to CCF Singapore Expo during May 3-31, 2020. All were men with an average age of 37 years and nearly half were under the age of 36 (age range 17-60). The three most common ethnicities were Bangladeshi, Indian, and Chinese, in that order (Table 1). The average day of illness was 7 ± 5.3 days while the median day of illness was 5 with an interquartile range of 4-9. We excluded 2,561 patients who were under the age of 36 and did not receive a chest radiograph at Singapore Expo and 1,363 patients who were aged 36 and older and had baseline chest imaging prior to Singapore Expo admission. This resulted in a study sample of 1,964 patients with chest radiographs.
Table 1:
Patient Characteristics and Chest Radiography Performed at Community Care FacilitySingapore Expo May 3-31, 2020
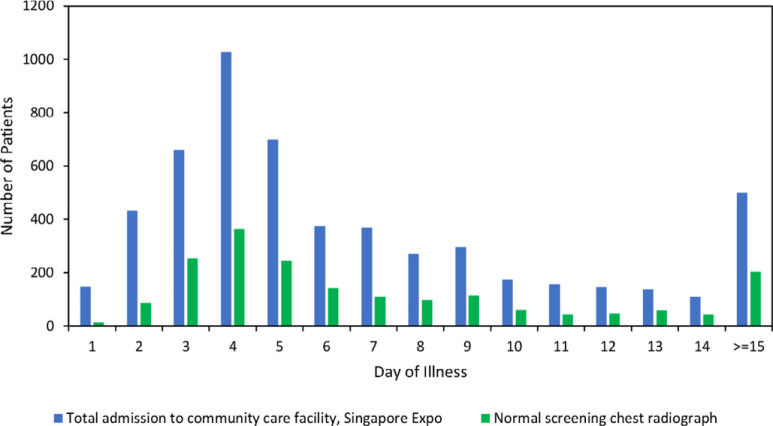
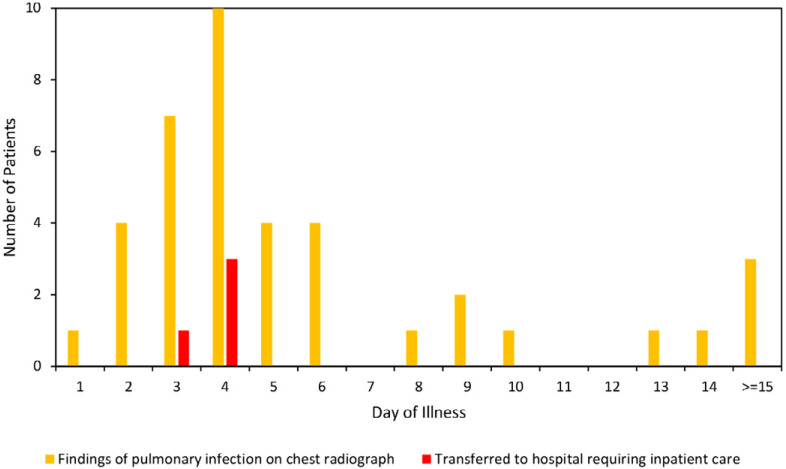
Chest Radiograph Findings by Day of Illness Trend
A total of 5,050 (90%, 5,050/5,621) patients admitted to CCF Singapore Expo were within the first two weeks of illness and 68% (3,820/5,621) were within the first week of illness (Fig 3a). Normal chest radiographs were most common throughout the disease course. Findings of pulmonary infection followed a similar frequency trend in relation to symptom onset compared to normal chest radiographs. However, patients who subsequently required inpatient care occurred more commonly in the first week than later in the disease course (Fig 3b).
Figure 3a:
Screening chest radiograph findings of all patients with COVID-19 admitted to community care facility, Singapore Expo, by day of illness during May 3-31, 2020. Majority of patients (a) admitted to Singapore Expo were in the early phases of disease. Of the patients with screening chest radiograph, normal chest radiograph findings were most common throughout the disease course. Chest radiograph showing findings of pulmonary infection (b) showed a similar frequency trend in relation to symptom onset date. However, all hospitalizations requiring supplemental oxygenation or IV medication occurred in the first 4 days after symptom onset.
Figure 3b:
Screening chest radiograph findings of all patients with COVID-19 admitted to community care facility, Singapore Expo, by day of illness during May 3-31, 2020. Majority of patients (a) admitted to Singapore Expo were in the early phases of disease. Of the patients with screening chest radiograph, normal chest radiograph findings were most common throughout the disease course. Chest radiograph showing findings of pulmonary infection (b) showed a similar frequency trend in relation to symptom onset date. However, all hospitalizations requiring supplemental oxygenation or IV medication occurred in the first 4 days after symptom onset.
Outcomes of Asymptomatic Patients with Findings of Pulmonary Infection on Chest Radiographs
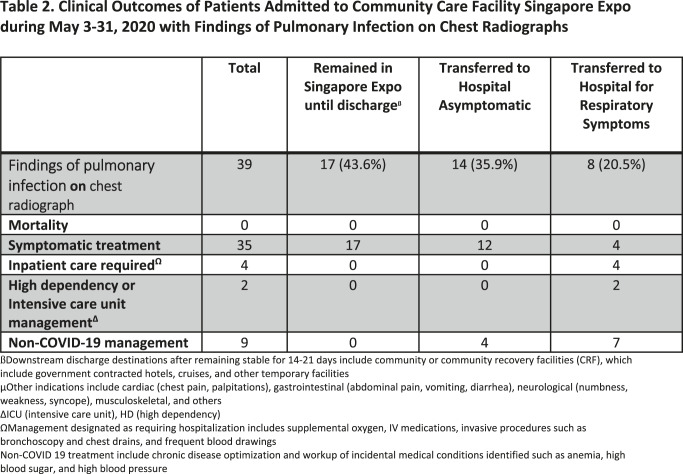
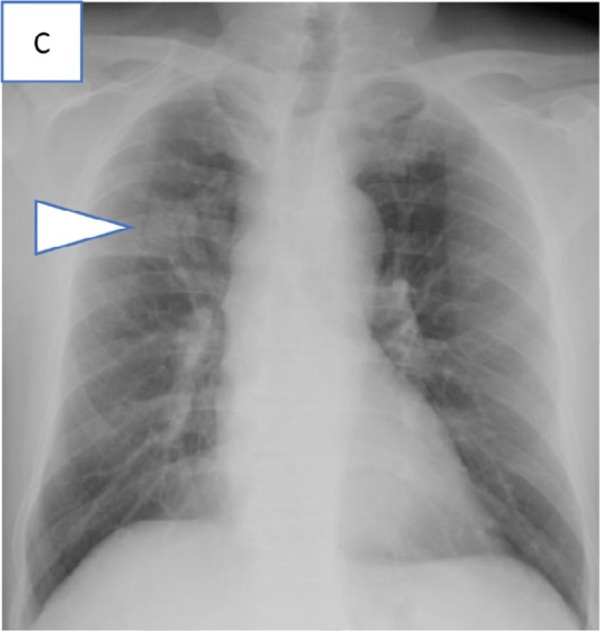
There were 39/1,964 (2.0%, 95% CI: 1.4%-2.7%) patients with chest radiographic findings of pulmonary infection, of which 17/39 (43.6%) were more than seven days from symptom onset, had no underlying chronic medical condition, clinically assessed to be low risk for deterioration and were not transferred to hospitals. They all remained well in Singapore Expo or were discharged by the end of the study period (Table 2). There were 14/39 (35.9%) asymptomatic patients with chest radiograph findings of pulmonary infection who were transferred to hospitals for closer monitoring as these patients were deemed at higher risk of deterioration based on symptom onset date or chronic medical conditions. 11 of the patients were still within seven days of symptom onset and the other 3 patients had chronic medical conditions (previous pulmonary tuberculosis, hypertension, and diabetes mellitus) (Fig 2). None of these patients required supplemental oxygenation, IV medication, HD, or ICU support. Twelve of these fourteen patients received symptomatic treatment with one patient’s chest radiograph depicted in (Fig 4, A). One patient received prophylactic oral antibiotics and his chest radiograph showed consolidation in the right mid-lower zone (Fig 4, B). Another patient received treatment for latent tuberculosis after confirmation on subsequent elective bronchoscopic alveolar lavage (Fig 4, C). Two received treatment for known underlying chronic diseases.
Table 2:
Clinical Outcomes of Patients Admitted to Community Care Facility Singapore Expo during May 3-31, 2020 with Findings of Pulmonary Infection on Chest Radiographs
Figure 4a:
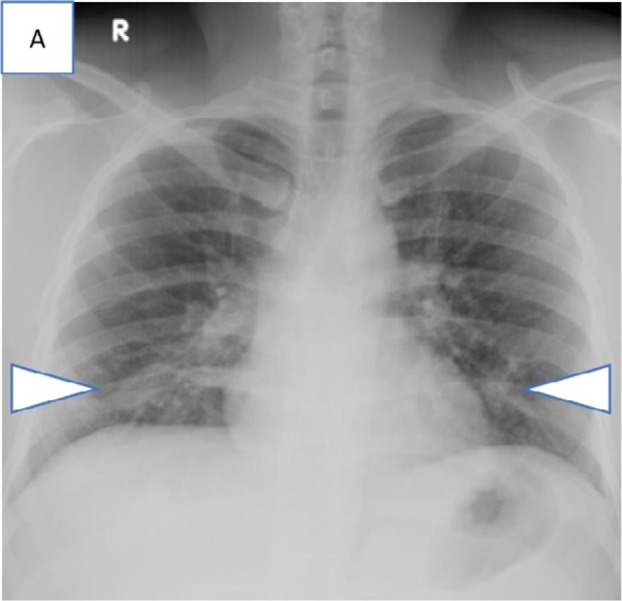
Series of chest radiograph in patients with COVID-19 pneumonia who were clinically asymptomatic and transferred out of the community care facility, Singapore Expo, to acute hospitals in view of findings of pulmonary infection on chest radiographs. Admission chest radiographs, A, in 36-year-old man on day 6 of illness showing bilateral lower zone patchy GGOs suspicious for infective foci (arrowheads), B, in 28-year-old man on day 2 of illness showing extensive consolidation (arrowheads) in the right mid and lower zone, and, C, in 55-year-old man on day 24 of illness with consolidation in the right upper zone (arrowhead).
Figure 4b:
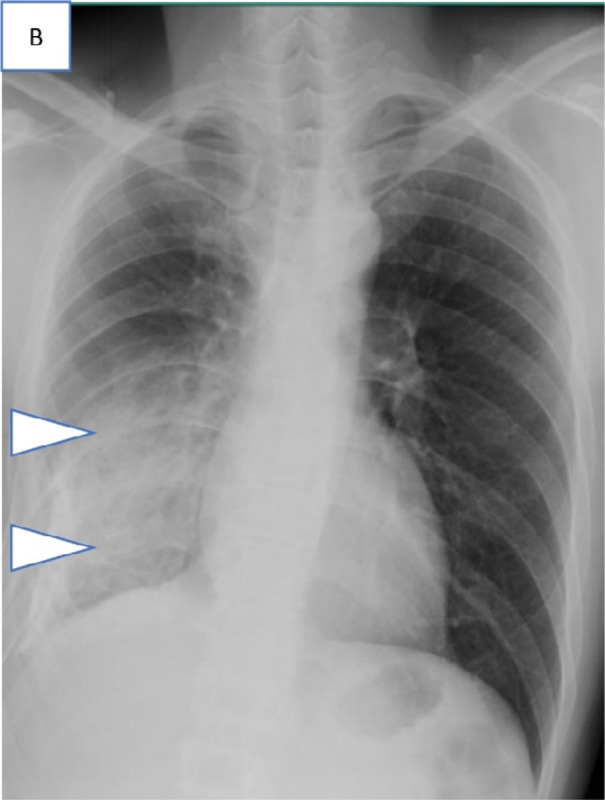
Series of chest radiograph in patients with COVID-19 pneumonia who were clinically asymptomatic and transferred out of the community care facility, Singapore Expo, to acute hospitals in view of findings of pulmonary infection on chest radiographs. Admission chest radiographs, A, in 36-year-old man on day 6 of illness showing bilateral lower zone patchy GGOs suspicious for infective foci (arrowheads), B, in 28-year-old man on day 2 of illness showing extensive consolidation (arrowheads) in the right mid and lower zone, and, C, in 55-year-old man on day 24 of illness with consolidation in the right upper zone (arrowhead).
Figure 4c:
Series of chest radiograph in patients with COVID-19 pneumonia who were clinically asymptomatic and transferred out of the community care facility, Singapore Expo, to acute hospitals in view of findings of pulmonary infection on chest radiographs. Admission chest radiographs, A, in 36-year-old man on day 6 of illness showing bilateral lower zone patchy GGOs suspicious for infective foci (arrowheads), B, in 28-year-old man on day 2 of illness showing extensive consolidation (arrowheads) in the right mid and lower zone, and, C, in 55-year-old man on day 24 of illness with consolidation in the right upper zone (arrowhead).
Outcomes of Symptomatic Patients with Findings of Pulmonary infection on Chest Radiographs
The remaining 8/39 patients with chest radiograph findings of pulmonary infection were transferred to hospitals for respiratory symptoms or deranged vital parameters such as tachycardia and fever (Table 2). From this subset, 4/1,964 (0.2%, 95% CI: 0.1%-0.5%) required inpatient care. One patient received IV antibiotics for superimposed pneumonia. Three patients required supplemental oxygenation (Fig 5, A-C) of which one needed HD (Fig 5, A) and another needed ICU (Fig 5, B) support. Figure 5, A depicts the chest radiograph of a 41-year-old man on day 3 of illness who presented with shortness of breath and general malaise. His chest radiograph showed a large left sided pleural effusion for which he was subsequently treated for concomitant pleural tuberculosis. The second patient needing supplemental oxygen was a 40-year-old man on day 4 of illness who presented with shortness of breath and low oxygen saturation and was febrile. His chest radiograph showed consolidation across the left mid and upper zone (Fig 5, B). He subsequently received supplemental oxygen by high flow nasal cannula, ICU monitoring, and Remdesivir trial therapy. The third patient was a 42-year-old man on day 4 of illness who had no respiratory symptom but flagged for persistent tachycardia and noted to have left lung crepitations during evaluation. His chest radiograph showed patchy GGOs in the peripheral aspects of both the mid zone and left lower zone (Fig 5, C) for which he was transferred to the hospital and received oxygen support and prophylactic IV antibiotics. All 39 patients with infective chest radiograph findings recovered well with no mortality recorded within the study period.
Figure 5a:
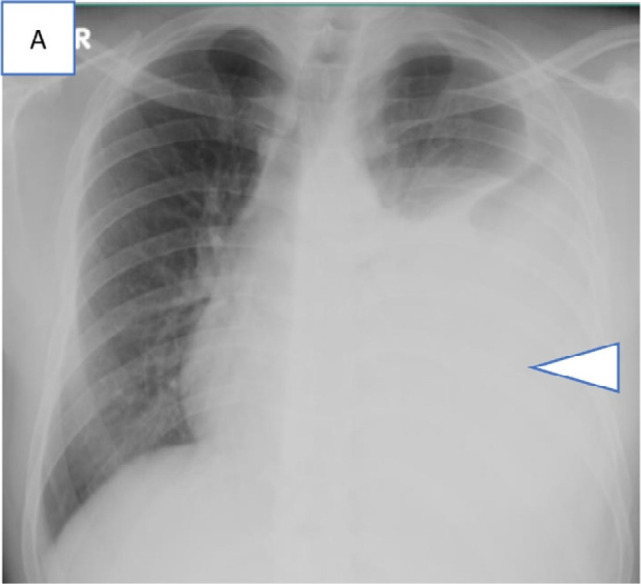
Series of chest radiograph in patients with COVID-19 pneumonia who were transferred out of community care facility, Singapore Expo, to acute hospitals in view of respiratory symptoms or deranged vitals and subsequently required supplemental oxygen. Admission chest radiographs, A, in a 41-year-old man on day 3 of illness with a large left pleural effusion and adjacent consolidation (arrowhead) treated for concomitant pleural tuberculosis, B, in a 40-year-old man on day 4 of illness with consolidation across the left mid and upper zones (arrowheads), and, C, in a 42-year-old man on day 4 of illness with patchy GGOs in the peripheral aspects of both the mid zone and the left lower zone (arrowheads).
Figure 5b:
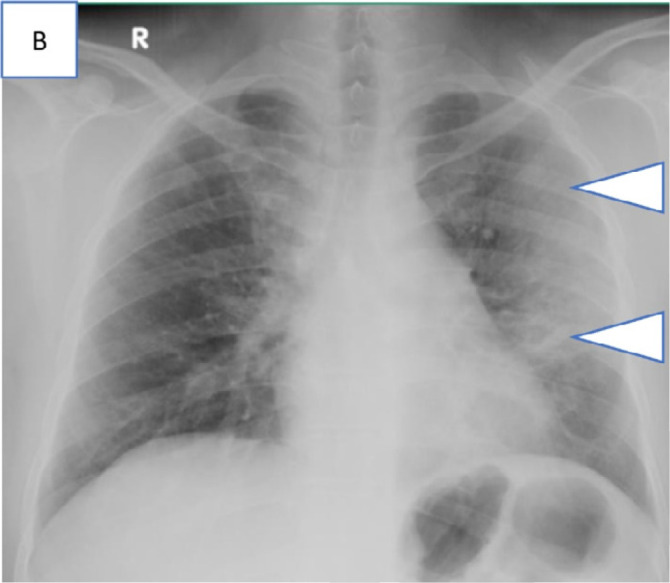
Series of chest radiograph in patients with COVID-19 pneumonia who were transferred out of community care facility, Singapore Expo, to acute hospitals in view of respiratory symptoms or deranged vitals and subsequently required supplemental oxygen. Admission chest radiographs, A, in a 41-year-old man on day 3 of illness with a large left pleural effusion and adjacent consolidation (arrowhead) treated for concomitant pleural tuberculosis, B, in a 40-year-old man on day 4 of illness with consolidation across the left mid and upper zones (arrowheads), and, C, in a 42-year-old man on day 4 of illness with patchy GGOs in the peripheral aspects of both the mid zone and the left lower zone (arrowheads).
Figure 5c:
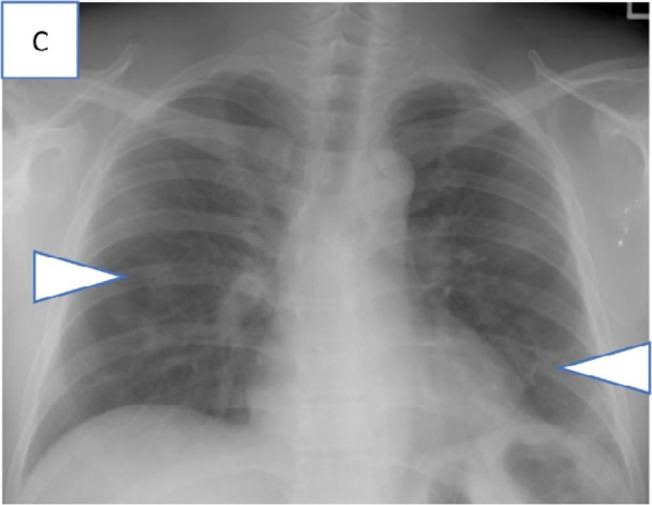
Series of chest radiograph in patients with COVID-19 pneumonia who were transferred out of community care facility, Singapore Expo, to acute hospitals in view of respiratory symptoms or deranged vitals and subsequently required supplemental oxygen. Admission chest radiographs, A, in a 41-year-old man on day 3 of illness with a large left pleural effusion and adjacent consolidation (arrowhead) treated for concomitant pleural tuberculosis, B, in a 40-year-old man on day 4 of illness with consolidation across the left mid and upper zones (arrowheads), and, C, in a 42-year-old man on day 4 of illness with patchy GGOs in the peripheral aspects of both the mid zone and the left lower zone (arrowheads).
Outcomes of Patients with Normal Chest Radiographs
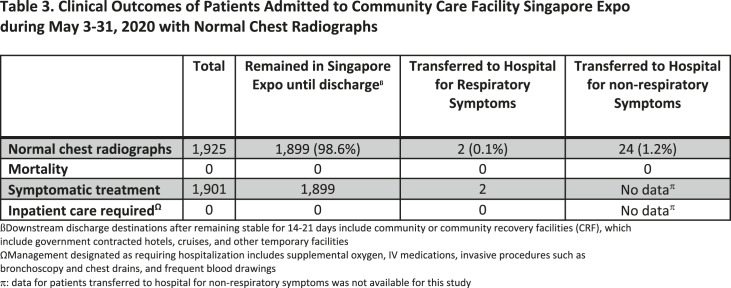
Out of 1,964 chest radiographs performed, 98.0% (1,925/1,964, 95% CI: 97.3%-98.6%) were normal. Within this group, 98.6% (1,899/1,925) remained stable in Singapore Expo until discharge (Table 3), while 1.4% (26/1,925) were transferred to hospitals for further management. Two patients (0.1%, 2/1,925) were transferred to hospitals for respiratory symptoms, received symptomatic management and recovered well without supplemental oxygen or IV medication. The remaining 24/1,925 patients (1.2%) were transferred to hospitals for evaluation of non-respiratory symptoms. The complaints were broad and included cardiac (chest pain, palpitations), gastrointestinal (abdominal pain, vomiting, diarrhea), neurological (numbness, weakness, syncope), musculoskeletal, and other symptoms. No mortality was recorded for this group of patients within the study period while the patients were managed in the hospital or in Singapore Expo.
Table 3:
Clinical Outcomes of Patients Admitted to Community Care Facility Singapore Expo during May 3-31, 2020 with Normal Chest Radiographs
Outcomes of Patients Excluded from Chest Radiography at Singapore Expo
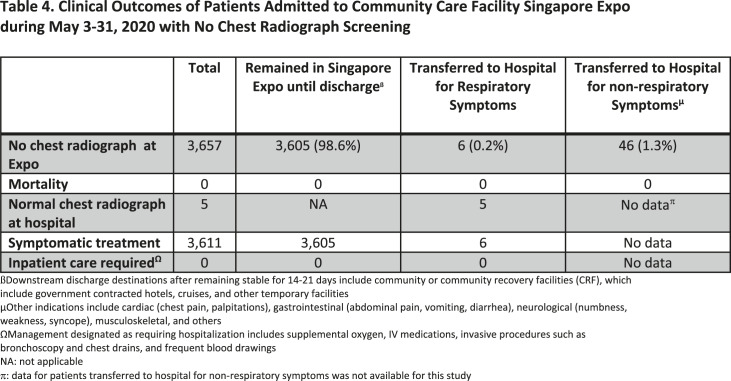
A total of 3,657/5,621 patients (65%) were excluded from chest radiography screening. Within this group, 98.6% (3,605/3,657) remained stable in Singapore Expo until discharge (Table 4). 6/3,657 patients (0.2%, 95% CI: 0.1%-0.4%) were transferred to hospitals for respiratory symptoms and only one patient showed findings of pulmonary infection on chest radiography from the hospital. No patient (0/3,657) received supplemental oxygen support or IV medication treatment (0%, 95% CI: 0%-0.1%), and all recovered well. A further 46/3,657 (1.3%) patients were transferred to hospitals for evaluation of non-respiratory symptoms. No mortality was recorded for this group of patients within the study period while the patients were managed in the hospital or in Singapore Expo.
Table 4:
Clinical Outcomes of Patients Admitted to Community Care Facility Singapore Expo during May 3-31, 2020 with No Chest Radiograph Screening
Discussion
The COVID-19 pandemic has overwhelmed hospitals globally and placed an unprecedented burden at the ambulatory setting with large numbers of relatively healthy patients with COVID-19. This highlights the need to evaluate the role of chest radiograph screening for this patient population when resource capacity is critically limited. We report our findings from a large sample of young asymptomatic or minimally symptomatic patients with COVID-19 admitted to Singapore Expo. A total of 1,964 chest radiographs were performed, of which 98.0% (1,925/1,964) were normal and only 2.0% (39/1,964) showed findings of pulmonary infection. Of these 39 patients with pneumonic changes on chest radiograph, 8 were transferred for respiratory symptoms representing just 0.4% (8/1964) with 4 requiring supplemental oxygen and inpatient care. None of the 14 asymptomatic patients with findings of pulmonary infection transferred to hospitals required supplemental oxygen or inpatient care related to COVID-19 pneumonia. Furthermore, there were 17 asymptomatic patients with findings of pulmonary infection who remained stable until discharge. While older age and comorbidities are associated with poorer COVID-19 outcomes (25), none of the 281 asymptomatic patients aged 50 and older (5.0%, 281/5,621) required transfer to hospitals. Finally, nearly two-thirds of all admitted patients, 3,657/5,621 (65%) were excluded from chest radiograph screening because of young age or prior baseline chest radiograph. The mortality rate was zero throughout their admission and no patient transferred to the hospital for respiratory symptoms required oxygen support or inpatient care. Our findings support the Fleischner Society recommendations that chest imaging in patients with mild features of COVID-19 is not indicated unless there is risk of clinical deterioration.
Studies on the role of chest radiographs during the severe acute respiratory syndrome outbreak in 2003 have suggested its value in predicting poor clinical outcomes in hospitalized patients (26,27). Similarly for COVID-19, chest radiograph severity can be predictive of hospital admission and intubation for patients presenting to emergency departments (17). But its clinical value in patients with mild disease and in ambulatory settings is less well known.
The proportion of normal chest radiographs in our patient sample was higher than the 25% and 31% found previously in hospitalized patients with moderate to severe COVID-19 disease (16,28). The differences observed reflect the expected association between symptom severity and radiographic features (17), highlighting the detection limits of chest radiography for patients with mild COVID-19 disease.
The risk of clinical deterioration was high for the 8 patients transferred to hospitals with findings of pulmonary infection and respiratory symptoms (29), and the availability of chest radiography allowed for the swift downstream arrangement of clinical care. The chest radiographs from these patients were taken on days 3-4 of disease in alignment with published findings of chest radiograph severity peaking earlier in the disease course (16,28).
Several limitations exist in our study. First, not all patients fulfilling the age criteria received a screening chest radiograph upon admission thereby underestimating the true number of patients with normal chest radiographs. Second, information on underlying chronic illnesses were not available for most patients who remained well. This limited correlational studies of underlying risk factors (25) with radiographic features and clinical outcomes. Third, outcomes of patients discharged were not tracked. While infrequent, this may not capture late complications that may correlate with early clinical and radiological findings. Fourth, outcomes of patients transferred to hospitals for non-respiratory indications were not followed. While this may fail to capture additional patients requiring supplemental oxygen and inpatient care, the role of chest radiograph screening is limited in this context as the decision for care escalation was largely clinical. Furthermore, despite its wide-ranging manifestations (30), COVID-19 remains primarily a respiratory illness with characteristic symptoms and radiological features. Fifth, our patient sample was all men. While this may limit the broader interpretation of our findings, it is unlikely to differ significantly for women with similar risk profiles as studies have shown that men tend to have poorer outcomes and more severe radiographic features (31,32). Finally, the small number of patients requiring inpatient treatment limits our ability to interpret prognostic factors for clinical deterioration.
In conclusion, our findings support Fleischner Society’s recommendation against the use of chest imaging in patients with mild COVID-19 disease without clinical risk of deterioration. Our results demonstrate that the overwhelming majority of asymptomatic and minimally symptomatic patients with COVID-19 had normal chest radiographs. Furthermore, all asymptomatic patients with findings of pulmonary infection recovered well without supplemental oxygen or IV medication treatment. While our findings recommended against the use of chest radiograph screening in asymptomatic patients with COVID-19, we also offered clinical data to suggest the potential role of targeted chest radiograph in ambulatory settings for patients with risk of clinical deterioration. Future research is needed in this area for better prognostication and distribution of imaging diagnostics in ambulatory settings.
Acknowledgments
Acknowledgements
The authors would like to thank the multidisciplinary Singapore Expo management team in particular Clinical Associate Professor Tan Hiang Khoon, Dr. Chow Weien, Associate Professor Henry Ho Sun Sien and Dr. Tan Kian Hian for their leadership and support. Additionally, we are grateful to the SGH clinical staff deployed to support the Expo operation for their commitment and selfless sacrifice. The authors would also like to acknowledge Dr. Xu Shuxiang for his diligence in maintaining our CXR database, Dr. John Carson Allen Jr. for his input on statistical analysis, and the diagnostic radiology department from our institution for its support of this research.
Institutional Address: Division of Radiological Sciences, Singapore General Hospital, 20 College Road, Singapore 169608, Republic of Singapore
Abbreviations:
- (COVID-19)
- coronavirus disease 2019
- (CCF)
- community care facility
- (SGH)
- Singapore General Hospital
- (CRF)
- community recovery facility
- (HD)
- high-dependency
- (ICU)
- intensive care unit
- (IV)
- intravenous
- (GGO)
- ground-glass opacity
References
- 1.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus Disease (COVID-19) [Internet]. 2020 [cited 2020 Jun 17]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 3.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review [Internet]. Vol. 78, International Journal of Surgery. IJS Publishing Group Ltd; 2020. 185–193 p. Available from: 10.1016/j.ijsu.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis [Internet]. 2020;20(5):533–4. Available from: 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee VJ, Chiew CJ, Khong WX. Interrupting transmission of COVID-19: lessons from containment efforts in Singapore. J Travel Med. 2020 May;27(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee Kuan Yew School of Public Policy NU of S . Singapore earns high praise for COVID-19 response [Internet]. Global is Asian. 2020 [cited 2020 Jun 17]. Available from: https://lkyspp.nus.edu.sg/gia/article/singapore-earns-high-praise-for-covid-19-response
- 7.Singapore Ministry of Health . UPDATES ON COVID-19 (CORONAVIRUS DISEASE 2019) LOCAL SITUATION [Internet]. [cited 2020 Jun 17]. Available from: https://www.moh.gov.sg/covid-19 [Google Scholar]
- 8.Singapore Ministry of Health . Scaling up of COVID-19 testing [Internet]. [cited 2020 Aug 17]. Available from: https://www.moh.gov.sg/news-highlights/details/scaling-up-of-covid-19-testing
- 9.Lim MZ, Goh T. Community care facilities for Covid-19 patients with mild symptoms will double bed capacity to 20,000 by end-June [Internet]. Straits Times. 2020 [cited 2020 Jun 17]. Available from: https://www.straitstimes.com/singapore/coronavirus-community-care-facilities-for-patients-with-mild-symptoms-will-have-bed [Google Scholar]
- 10.Menon M. Covid-19 facility at Tanjong Pagar Terminal begins receiving workers [Internet]. The Straits Times. [cited 2020 Jun 17]. Available from: https://www.straitstimes.com/singapore/facility-at-tanjong-pagar-terminal-begins-receiving-workers
- 11.Singapore Ministry of Health . Comprehensive Medical Strategy for Covid-19 - 28th April 2020 [Internet]. Ministry of Health (MOH), Singapore. 2020 [cited 2020 Jun 19]. Available from: https://www.moh.gov.sg/news-highlights/details/comprehensive-medical-strategy-for-covid-19 [Google Scholar]
- 12.Chia ML, Him Chau DH, Lim KS, Yang Liu CW, Tan HK, Tan YR. Managing COVID-19 in a Novel, Rapidly Deployable Community Isolation Quarantine Facility. Ann Intern Med [Internet]. 2020 Sep 17;M20-4746. Available from: https://pubmed.ncbi.nlm.nih.gov/32941059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, et al. Temporal Changes of CT Findings in 90 Patients with COVID-19 Pneumonia: A Longitudinal Study. Radiology. 2020;2020:200843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zu ZY, Jiang M Di, Xu PP, Chen W, Ni QQ, Lu GM, et al. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology. 2020;2019:200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mossa-Basha M, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology Department Preparedness for COVID-19: Radiology Scientific Expert Panel. Radiology. 2020;1064:200988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wong HYF, Lam HYS, Fong AHT, Leung ST, Chin TWY, Lo CSY, et al. Frequency and Distribution of Chest Radiographic Findings in COVID-19 Positive Patients. Radiology. 2019;201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Toussie D, Voutsinas N, Finkelstein M, Cedillo MA, Manna S, Maron SZ, et al. Clinical and Chest Radiography Features Determine Patient Outcomes In Young and Middle Age Adults with COVID-19. Radiology. 2020;201754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rubin GD, Haramati LB, Kanne JP, Schluger NW, Yim J-J, Anderson DJ, et al. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology. 2020;201365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American College of Radiology . ACR recommendations for the use of chest radiographyand computed tomography (CT) for suspected COVID-19 infection [Internet]. 2020. [cited 2020 Jun 25]. Available from: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection [Google Scholar]
- 20.The Health Sciences Authority . HSA Expedites Approval of COVID-19 Diagnostic Tests in Singapore via Provisional Authorisation [Internet]. 2020 [cited 2020 Oct 1]. Available from: https://www.hsa.gov.sg/announcements/regulatory-updates/hsa-expedites-approval-of-covid-19-diagnostic-tests-in-singapore-via-provisional-authorisation
- 21.et al. FIGHTING COVID-19 WITH FORTITUDE [Internet]. 2020 cited 2020 Oct 1]. Available from: https://www.a-star.edu.sg/News-and-Events/a-star-news/news/covid-19/fighting-covid-19-with-fortitude [Google Scholar]
- 22.Singapore Ministry of Manpower . Foreign workforce numbers [Internet]. [cited 2020 Aug 17]. Available from: https://www.mom.gov.sg/documents-and-publications/foreign-workforce-numbers
- 23.Singapore Ministry of Manpower . List of foreign worker dormitories [Internet]. [cited 2020 Aug 17]. Available from: https://www.mom.gov.sg/passes-and-permits/work-permit-for-foreign-worker/housing/foreign-worker-dormitories#/
- 24.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet [Internet]. 2020;395(10229):1054–62. Available from: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in coronavirus disease 2019 patients: A systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hui DSC, Wong KT, Antonio GE, Lee N, Wu A, Wong V, et al. Severe acute respiratory syndrome: Correlation between clinical outcome and radiologic features. Radiology. 2004;233(2):579–85. [DOI] [PubMed] [Google Scholar]
- 27.Chau TN, Lee PO, Choi KW, Lee CM, Ma KF, Tsang TY, et al. Value of initial chest radiographs for predicting clinical outcomes in patients with severe acute respiratory syndrome. Am J Med. 2004;117(4):249–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vancheri SG, Savietto G, Ballati F, Maggi A, Canino C, Bortolotto C, et al. Radiographic findings in 240 patients with COVID-19 pneumonia: time-dependence after the onset of symptoms. Eur Radiol. 2020;1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li L, Yang L, Gui S, Pan F, Ye T, Liang B, et al. Association of clinical and radiographic findings with the outcomes of 93 patients with COVID-19 in Wuhan, China. Theranostics. 2020;10(14):6113–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gulati A, Pomeranz C, Qamar Z, Thomas S, Frisch D, George G, et al. A Comprehensive Review of Manifestations of Novel Coronaviruses in the Context of Deadly COVID-19 Global Pandemic. Am J Med Sci [Internet; ]. 2020; Available from: 10.1016/j.amjms.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jin J-M, Bai P, He W, Wu F, Liu X-F, Han D-M, et al. Gender Differences in Patients With COVID-19: Focus on Severity and Mortality [Internet]. Vol. 8, Frontiers in Public Health. 2020. p. 152. Available from: https://www.frontiersin.org/article/10.3389/fpubh.2020.00152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cozzi D, Albanesi M, Cavigli E, Moroni C, Bindi A, Luvarà S, et al. Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: findings and correlation with clinical outcome. Radiol Medica; [Internet]. 2020;125(8):730–7. Available from: 10.1007/s11547-020-01232-9 [DOI] [PMC free article] [PubMed] [Google Scholar]