Abstract
The COVID-19 pandemic has challenged and changed our healthcare systems around the world. There has been a heterogeneity of disease burden, healthcare resources, and non-imaging testing availability, both geographically and over time. In parallel, there has been a continued increase in understanding of how the disease affects patients, effectiveness of therapeutic options, and factors that modulate transmission risk. Here we detail experiences from radiology experts in representative countries from around the world, to share insights gained from local experience. These insights provide a guidepost to help address management challenges as cases continue to rise in many parts of the world and suggest modifications in workflow that are likely to continue after this pandemic subsides.
Summary
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread rapidly around the globe and radiology responses were innovative and varied depending upon the number of patients infected and the resources available to them.
Key Results
■ Early in the pandemic when PCR testing was quite limited, there was a diversity across countries in the use of imaging as first line diagnostic confirmation in high prevalence areas. The variability in approach has decreased with increasing availability of PCR testing and adoption of imaging use guidelines.
■ Rapid changes in radiology workflows were required, as COVID-positive patients’ need for acute care overwhelmed many healthcare systems, and infection control became paramount to decrease in hospital spread of the virus from patient to patient and patient to healthcare worker.
■ Adoption of technological innovations accelerated with COVID-related constraints, resulting in increases in remote image interpretation, the use of AI for image analysis, and the use of automated tools for patient guidance.
Introduction
Our lives have been fundamentally altered this year by the Coronavirus disease 2019 (COVID-19) pandemic. From a medical imaging and healthcare perspective, we have learned a tremendous amount over the last eleven months about how the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) affects the body, and the major routes of transmission. Best practices have been rapidly implemented to address both aspects; however, with a rising number of cases in many regions of the world (Figure 1) we have reached new high case incidences in the fourth quarter of 2020. We will need to continue to innovate in our approaches to help manage this crisis.
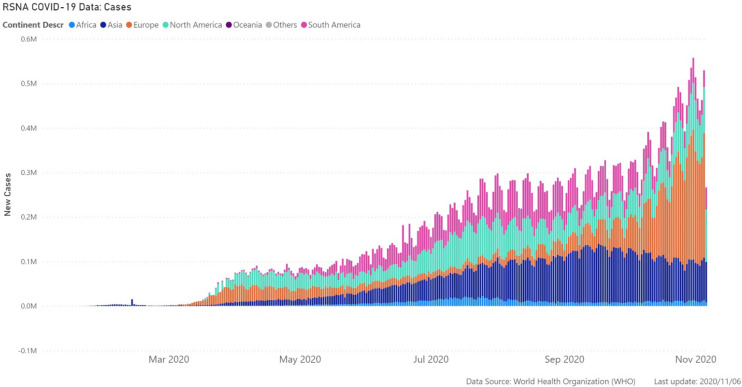
Figure 1.
COVID-19 cases over time by continent. The world’s population is severely affected by this pandemic, with many regions showing increasing cases in the later part of 2020. While healthcare systems and radiology practice have rapidly adapted best practices learned from initial experiences, the growth in COVID-19 incidence will continue to test how best to manage the needs of patients. Data from World Health Organization (WHO), https://covid19.who.int/table, 2020/11/06.
In this perspective piece, radiology experts from around the world share their insights. The tradition of gathering key international thought leaders at the RSNA annual meeting “International Trends Session” has resulted in shared understanding of topics such as the impact of artificial intelligence (AI) on radiology; radiologist shortages; and medical student education. No topic has necessitated convocation and collaboration as compellingly as the COVID-19 pandemic, and we hope radiologists can use these perspectives from around the world to optimize the care of COVID-19 patients and help plan for a near-term increase in the number of cases (Figure 2).
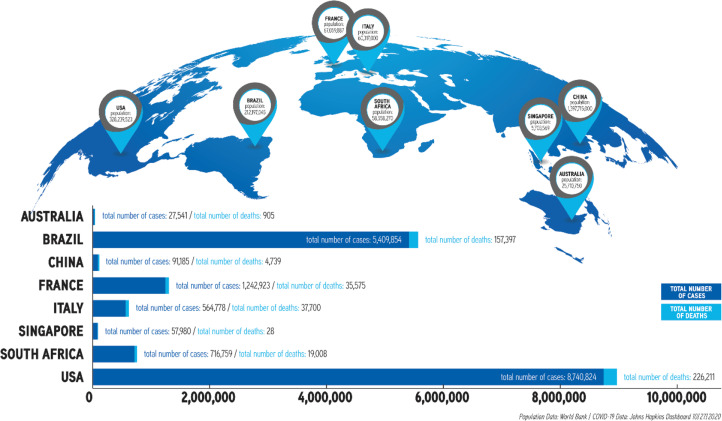
Figure 2.
Total COVID-19 cases to date in representative countries. The heterogeneity of disease burden is in part determined by national or regional mitigation strategies. These case incidences determine the COVID-related need and utilization of overall health care and radiology resources in different countries. Data from World Bank, https://data.worldbank.org/indicator/SP.POP.TOTL, 2019 data and Johns Hopkins Dashboard, https://coronavirus.jhu.edu/map.html, 10/27/2020.
These insights reflect some of the chaos initially experienced as a new infection spread rapidly throughout the world, as well as the rapid adjustments made to address our new reality. Healthcare systems optimized for workflows in one setting were quickly adapted to one in which patients were highly infectious to other patients and healthcare workers. Appropriate personal protective equipment (PPE) was extremely limited; there was a severe shortage of polymerase chain reaction (PCR) test kits and other non-imaging diagnostics; and critically ill COVID-19 patients overwhelmed hospital capacities.
The diversity of approaches in different regions highlight the local choices made based on CT scanner availability, PCR testing availability and turnaround time, PPE availability, and effectiveness of public health measures. The decisions implemented reflect the need to balance supply and demand of these constraints to optimize patient management and resource utilization.
Driven by innumerable advances, radiology has helped to greatly improve patient care in this new environment. As cases surged in different regions, RSNA served as a central point for radiologists to share findings and seek guidance from colleagues from more affected areas. Through journals, news, webinars and communities, radiologists were able to quickly access the latest research, learn practical applications, and improve COVID patient care in their communities (Figure 3). RSNA has published over 130 articles related to COVID-19, with over 5 million page views. The international community came together to build the RSNA International COVID Open Radiology Database (RICORD) (1), which will be accessible to all investigators to further scientific knowledge and facilitate the development of rapid quantitative assessment tools.
Figure 3.
Highlights of RSNA’s efforts. The rapid dissemination of the latest COVID-19 research, education on imaging interpretation, and workflow best practices is vital to the health of patients, both for diagnosis and treatment assessment. The insights allow improved workflows to increase the safety of patients and healthcare workers. The broad RSNA connectivity throughout the imaging community ensures radiologists globally remain fully up to date.
Data source: RSNA internal data/www.rsna.org
This is not a compendium of advancements in all regions, rather we have sought to detail some of the heterogeneity of approaches by highlighting challenges and solutions in representative countries. A snapshot in late 2020 provides a guidepost as we continue to battle this pandemic. We have focused on where we have been as a specialty in the initial response to the first wave, how we have planned for subsequent waves of COVID-19 infections, and what insights we have gained so that we are better prepared for unknown future pandemics.
Section 1: Radiology’s Response to the First Wave
Perspective from China: Initial imaging protocols and early developed guidelines
At the outbreak of the pandemic at the end of 2019, chest radiography (CXR) was used to screen patients for COVID-19 pneumonia. However, CXR has a reported sensitivity of only 69% for the detection of COVID-19 lung disease (2). With chest computed tomography (CT), subtle imaging findings are identified, including areas of ground glass opacities (GGO), rounded opacities with intralobular interstitial thickening and consolidation with a subpleural, peripleural or peribronchovascular distribution (3, 4, 5, 6). Although CT can be negative at the very early stage of the disease, the reported sensitivity of chest CT is over 95% (7,8). Since the PCR testing capacity was limited at the beginning of the first wave, typical findings on chest CT were recognized as primary evidence of COVID-19 infection in the epicenter of the COVID-19 outbreak (Hubei Province) by the National Health and Health Commission of China (5th edition) on February 5, 2020 (9). China's COVID-19 PCR testing capacity was 1.26 million per day in early March, it reached 3.78 million per day in late June, at which time the total number of PCR tests conducted by medical and health institutions nationwide reached 90.41 million (10).
Recommendations from the Chinese Society of Radiology provided details of CT imaging manifestations, including the typical features, staging, and criteria for hospital discharge (11). Regional/national guidelines globally have differed from one another and may depend in part on the availability of imaging and the in vitro testing infrastructure; for example, the American College of Radiology (ACR) recommended that CT be used sparingly and reserved for symptomatic or hospitalized patients with specific clinical indications, such as assessment of complications (12, 13).
CT was shown to be useful for follow-up evaluations and for prognosis (14,15). Although low-dose CT was recommended as the standard scanning protocol to minimize the radiation dose, studies showed that ultra-low-dose CT would make it more difficult to detect subtle GGOs (16). Full radiation dose scanning was therefore established as the technological society consensus (17). However, low dose CT may be useful in areas where there is a high prevalence of disease (18,19) or where there is limited availability of PCR testing (20). CXR is no longer recommended for COVID-19 screening, due to the high false negative rate, but it can help to assess disease severity (21, 22). Given the association of thrombotic complications, including pulmonary embolism (PE), chest CT is recommended whenever there is suspicion of pulmonary embolism (23, 24).
Cardiac complications including arrhythmias, acute myocarditis, cardiomyopathy, and shock are also associated with COVID-19 infection (23, 25). Cardiac magnetic resonance imaging (MRI) is used for differentiating types of myocardial injury and assessing the extent and severity of the injury (26). Abdominal and/or pelvic organ injury is also commonly seen, and abdominal/pelvic CT is indicated when bowel complications, cholecystitis, solid organ infarctions or vascular thromboses are suspected (27, 28, 29). Acute stroke (seen in patients older than 50 years without risk factors) have also been reported (30). Brain MRI may help to diagnose COVID-19 related acute or subacute infarction, as well as diagnose parenchymal abnormalities unrelated to ischemic infarcts (31, 32).
Perspective from France: CT use for diagnosis, the role of ultrasound, interventional radiology and the shift in workforce
In France, the COVID-19 pandemic began in the east and soon spread throughout the country. General lockdowns and social distancing from March 17-May 11, 2020 resulted in major disruptions to radiology services. During this period, daily routines were adjusted to take care of COVID-19 patients while implementing safety measures to keep the virus from spreading. Normal care was maintained for critical interventional procedures and emergency patients.
To prevent the spread of the disease within the hospital, the emergency department was divided into areas for patients suspected of having COVID-19 and non-COVID-19 patients. A triage station for all outpatients and staff was placed at the entrance of the emergency department. The CT scanner in the emergency department, which had a negative pressure environment and an air filtration system, was dedicated to COVID-19 patients. Because an insufficient number of PCR tests were available, all patients suspected of COVID-19 had a chest CT scan. At the peak of infection, two to four CT scanners were utilized for screening, and as many as 240 chest CT scans were completed in a day. The patients were masked and only the CT couch and gantry were cleaned between examinations. The diagnosis was based on the typical findings of bilateral, peripheral and basal ground glass opacities and/or consolidation. If the chest CT were negative and other pathologies were not suspected, the patient was discharged. When the CT was positive, the patient was sent for PCR testing. Those with mild symptoms were discharged and quarantined at their homes. Those with moderate and severe symptoms were admitted for further management. By July, when PCR tests were widely available, they replaced CT as the first line investigation. Ultrasound was used to examine the abdomen, but not the chest.
The COVID-19 pandemic had a profound impact on interventional radiology (IR) services, particularly for elective cases. Due to the scarcity of available hospital beds, IR procedures were limited to medical emergencies and high-priority procedures. The IR capacity was reduced from six operating rooms to three (two angiographic suites and one CT suite). Rooms with a negative pressure environment were decontaminated immediately after each procedure. The most frequent IR procedures performed for COVID-19 patients were central venous catheter insertion, pleural drainage, percutaneous cholecystostomy, nephrostomy, gastrostomy, biopsy, and venous thrombectomy. Most of the IR procedures were performed under ultrasound guidance in the ICU to avoid transportation of these patients.
Radiology technologists contributed to frontline work by rotating to emergency radiology, thus doubling the number of staff handling COVID-19 positive patients. This modification in the rotation was possible because all non-urgent and non-emergent activity within the hospital was postponed. Some of the anesthesiology devices were also transferred to clinical areas that were converted to COVID-19 beds.
Perspective from South Africa: Unique challenges for lower-resource countries and rural hospitals
As the pandemic swept from Asia to Europe, a major challenge in Africa was remaining abreast of the enormous volume of emerging literature, while extracting appropriate and accurate information that could be implemented swiftly in a resource-constrained environment.
The reported pivotal role of CT
At the start of the South African (SA) pandemic in March 2020, the radiological literature was dominated by descriptions of the chest CT findings in patients with COVID-19 pneumonia. It was reported that CT was the preferred imaging examination, with greater sensitivity and specificity than CXR (33, 34) and since the sensitivity of the nasal swab test for PCR was low, a chest CT examination could serve as a substitute in screening patients for COVID-19 infection (35). However, these reports originated in settings with an adequate number of CT scanners, usually between 6 and 11 CT scanners per million people (36). By comparison, countries in sub-Saharan Africa have only 0.08 - 1.7 CT scanners per million people in the public healthcare sector (37,38,39,40). Thus, the greatest initial challenge of the pandemic was managing the expectations of referring physicians that CT was needed for the early diagnosis and management of COVID-19 patients. The situation was addressed by the Radiological Society of South Africa (RSSA) which endorsed the ACR recommendations for patients suspected of COVID-19 infection, limiting the use of CT in the screening or first-line diagnosis setting (41). PCR was relied upon for diagnosis of infection.
Personal Protective Equipment concerns
A major concern was availability of appropriate PPE for imaging staff. Radiology departments with available resources were proactive, funding the manufacture of reusable gowns and purchasing equipment to facilitate daily laundry of PPE. This model has proved sustainable and has served staff well at Tygerberg Hospital in Cape Town, where the infection rate among radiographers and radiologists has been five percent over the past six months, and these infections were likely unrelated to workplace exposure.
The long-term impact of the lockdown on HIV and tuberculosis control
The impact of human immunodeficiency virus (HIV) infection and pulmonary tuberculosis (TB) on the clinical course and radiological features of COVID-19 pneumonia was not known. Research projects commenced, with expedited institutional ethics approval, to address these questions. Preliminary findings show that both HIV and current TB are independently associated with increased COVID-19 mortality (42).
During a 6-month lock-down, March through September, elective out-patient services were reduced by 70%, with a resultant 40% decrease in overall imaging workload. This aggravated already protracted waiting periods for advanced imaging such as MRI and CT.
Modelling data suggests that the interruption of services, with decreased diagnosis and treatment, could trigger an excess of 6 million TB deaths in high-prevalence areas, such as sub-Saharan Africa, in the next 5 years (43). Similarly, a 6-month disruption in antiretroviral therapy delivery for patients with HIV could result in up to 500,000 additional deaths and double the rate of mother-to-child transmission over the next 5 years (44).
Section 2: Radiology’s Response to Multiple Waves and the role of AI
Perspective from Italy: Lessons from the first wave guide preparation for a second wave
The first wave of the pandemic in Europe started in March 2020 in the Lombardy region of Italy and subsequently spread to other regions of northern and central Italy, with less impact on the southern part of the country. In the first wave, the management of COVID-19 patients was difficult due to the shortage of PPE and the scarcity of intensive care unit (ICU) beds, which were already occupied by patients with diseases unrelated to COVID-19. A recent survey conducted by the Italian Society of Medical and Interventional Radiology (SIRM) highlighted that more than two-thirds of institutions had trouble getting PPE for healthcare workers (45).
The national health care system implemented an emergency plan by assigning priority to COVID-19 patients who had flocked to the emergency departments with severe symptoms. In parallel, the Italian radiology departments had to convert their activity to one dedicated completely or partially to COVID-19 patients (46). Entire facilities were adapted with separate pathways for COVID-19 patients, thus reducing radiological activity for non-COVID-19 patients. This created a list of patients waiting for care. Of particular concern were oncology patients who experienced a delay in both radiological diagnosis and follow-up. Many radiologists, even those not expert in thoracic radiology, found themselves at the forefront providing answers to two fundamental clinical questions: the presence of signs of pneumonia and the severity of the radiological findings. To help provide answers, the SIRM activated an initiative called "Coronavisible", publishing a freely accessible radiological case history of patients with COVID-19 pneumonia (47). Further SIRM initiatives included the publication of guidelines on the appropriate use of radiological imaging in these patients and the use of artificial intelligence (AI) (48, 49). In particular, SIRM recommended CXR for initial screening with CT as an additional examination showing the typical features of COVID-19 pneumonia, and the use of AI to predict the need for additional support.
In Italy, in April and May, the number of new patients began to decline and reached a low point of 120 new cases per day in August. Unfortunately, this trend reversed in September and the survey of October 4, 2020 reported the number of new cases in the 30-day period increased to 41,361, of which 23,068 (56%) have recovered (50). A lower severity of symptoms was seen in new cases, due to an earlier diagnosis made possible by increased PCR testing of the Italian population, including health personnel.
To standardize COVID patient evaluation, SIRM has developed a structured CT report model, through a consensus agreement among experts in thoracic radiology, that is accessible on its website (47). The SIRM structured report, in line with the recommendations of the RSNA and other scientific societies, represents a guideline for reporting, and also serves as a system for collecting clinical and radiological data for research purposes.
In anticipation of a second pandemic wave, Italian hospitals are better prepared. PCR testing is widely available and is used as the first line test. Dedicated COVID-19 departments have been created, some of which are equipped with a radiological unit, and ICUs have been upgraded. For example, at the university hospital of the city of Pisa, a small COVID-19 hospital was created, funded by the Italian civil protection, with an ICU, a surgical department, an angiography suite and a dedicated radiological unit with CT, ultrasound and radiography. Radiologists go to the COVID-19 hospital to perform ultrasound examinations. These exams have often been in the setting of PCR-positive disease and severe symptoms of lung involvement. A team of a radiologist, radiographers and a nurse enter the COVID-19 hospital to perform CT examinations. Each access is regulated by security procedures, including donning and doffing of PPE according to a standard procedure to reduce the risk of contagion. To ensure the prompt availability of the radiological team, shifts of radiologists, radiographers and nurses were reorganized within institutions across Italy.
Perspective from Brazil: The use of AI to overcome disparities and shortages
Brazil, the fifth largest country in the world, has marked social inequality, income distribution and access to the healthcare system. COVID-19 infection peaked at different times among Brazil’s 27 states, beginning at the end of February 2020, and starting to show a continuous drop in September, but still reporting 800 deaths daily in the beginning of October. 80% of the Brazilian population uses a public Unified Health System (SUS) (51), which despite limited resources, played a fundamental role in combating the pandemic, by centrally regulating basic health units, emergency rooms and hospitals. The major state capitals of Brazil built field hospitals in soccer stadiums and convention centers, which allowed for a rapid expansion of beds for less complex patients, leaving the most critical cases to be treated in referral hospitals. With respect to imaging, chest CT was always the first choice for initial evaluation when available; however, only chest x-rays were available at many sites in Brazil.
In one of the most affected cities, São Paulo, with approximately 13 million inhabitants, three field hospitals were built totaling 1,339 beds. At the same time, the Hospital das Clinicas of the University of São Paulo (HCFMUSP) (52) which has 6 hospitals and 2,500 beds, dedicated the central hospital with 900 general beds and 300 ICU beds, exclusively for the treatment of severe cases of COVID-19, becoming the largest hospital center in the fight against COVID-19 in Brazil. More than 5,000 patients were hospitalized between March-September 30: 3,000 in ICUs and 80% were on mechanical ventilation. As an intensive care reference center and telemedicine service provider, the knowledge acquired in the management of critically ill patients was shared with 16 affiliated public hospitals.
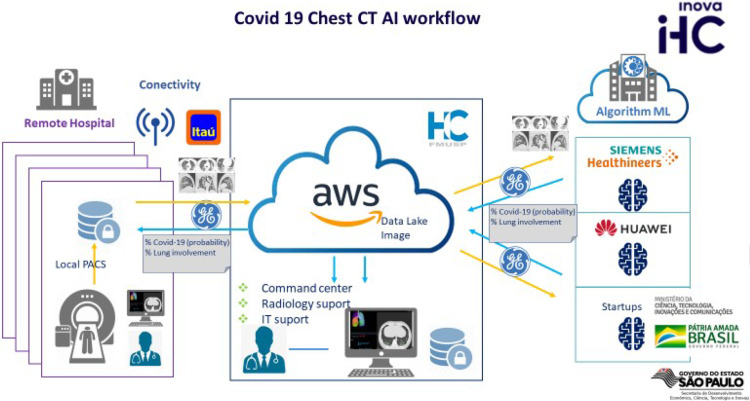
In order to assist hospitals without chest radiologists and to help provide a faster diagnosis, the HCFMUSP innovation center in partnership with private sector and the federal government, created the Radvid-19 project (53). Using this AI platform (Figure 4), any hospital in Brazil can send its chest CT examination to a server, where two AI algorithms (Huawei and Siemens) return a report with a COVID-19 probability analysis and the extent of the affected lung parenchyma. The facility operates 24 hours a day at no cost to the user, and reports are delivered within 10 minutes (Figure 5).
Figure 4:
COVID-19 Chest AI workflow in Radvid19 demonstrates academic, private, and government partnership created in Brazil. This workflow is free to users in Brazil and allowed high level automatic interpretation and quantitative lung involvement results even to remote hospitals in 10 min, helping address the increased demand for COVID-19 related image interpretation in rural parts of the country.
Figure 5:
The Brazilian COVID-19 Chest CT Database. There are 47 hospitals connected from different Brazilian states to the central database. Almost 20,000 chest CT’s have been analyzed to date, with a COVID-19 prevalence of 75%. This high prevalence is in part a reflection of increased cases submitted for analysis from dedicated COVID-19 and reference hospitals. The results screen shows example images, the probability of COVID-19 and the percent of lung parenchyma involvement. Such automated analysis can aid in direct patient management, as well as be potentially utilized for studies evaluating the efficacy of therapeutic interventions.
Several lessons were learned about the pandemic from developing and using Radvid-19. One of the most important was that with technology, innovation and solidarity, it is possible to shorten distances, democratize knowledge, and reduce healthcare costs. Another lesson is that radiologists are accustomed to high technological environments and are quick to adopt digital tools like teleradiology. Our experience in Brazil suggests that radiologists should assume a leadership role in healthcare institutional strategic planning for global pandemic response.
Section 3: Opportunities for Radiology
Perspective from the United States: Balancing and developing new workflows
The United States (U.S.) leads the world in the number of COVID-19 cases and deaths by an extremely large margin. The first case of COVID-19 in the U.S. was reported on January 19, 2020 in a man returning to Seattle, Washington from Wuhan, China (54). The virus hit early hotspots like New York City fast and hard and healthcare systems had to respond rapidly to the increased need for PPE, hospital and ICU beds, ventilators, and viral testing. New workflows were developed to safely deal with a deluge of critically ill patients. Most elective surgeries, procedures, and imaging tests were postponed for months which has delayed critical healthcare for many patients and devastated healthcare systems financially.
As the virus waned in early hotspots, new processes and safety precautions were implemented to address patients whose care was deferred. Hospitals and outpatient centers routinely required safeguards such as universal masking, hand hygiene, and COVID-19 testing prior to specific procedures. New workflows include socially distanced waiting areas, transparent barriers, one-way traffic passageways, and frequent cleaning of equipment and patient areas. Instant messaging allows patients to wait at a distant location with notification when ready for expedited arrival thereby minimizing physical contact and improving distancing.
The clinical impact of COVID-19 with additional waves is expected to be less deadly on a per infection basis because of learned techniques such as placing patients in a prone position and identification of effective chemotherapeutic agents such as dexamethasone and remdesivir (55). With successive waves, many hospitals and outpatient imaging centers hope to continue to safely perform elective imaging and procedures while healthcare systems simultaneously treat COVID-19 patients. Of concern is the anticipation that a second wave of COVID-19 will occur concurrently with the influenza season. Prevention and decreased severity of influenza illness and decreased outpatient visits, hospitalizations, and ICU admissions through influenza vaccination could also help to reduce stress on the U.S. health care system.
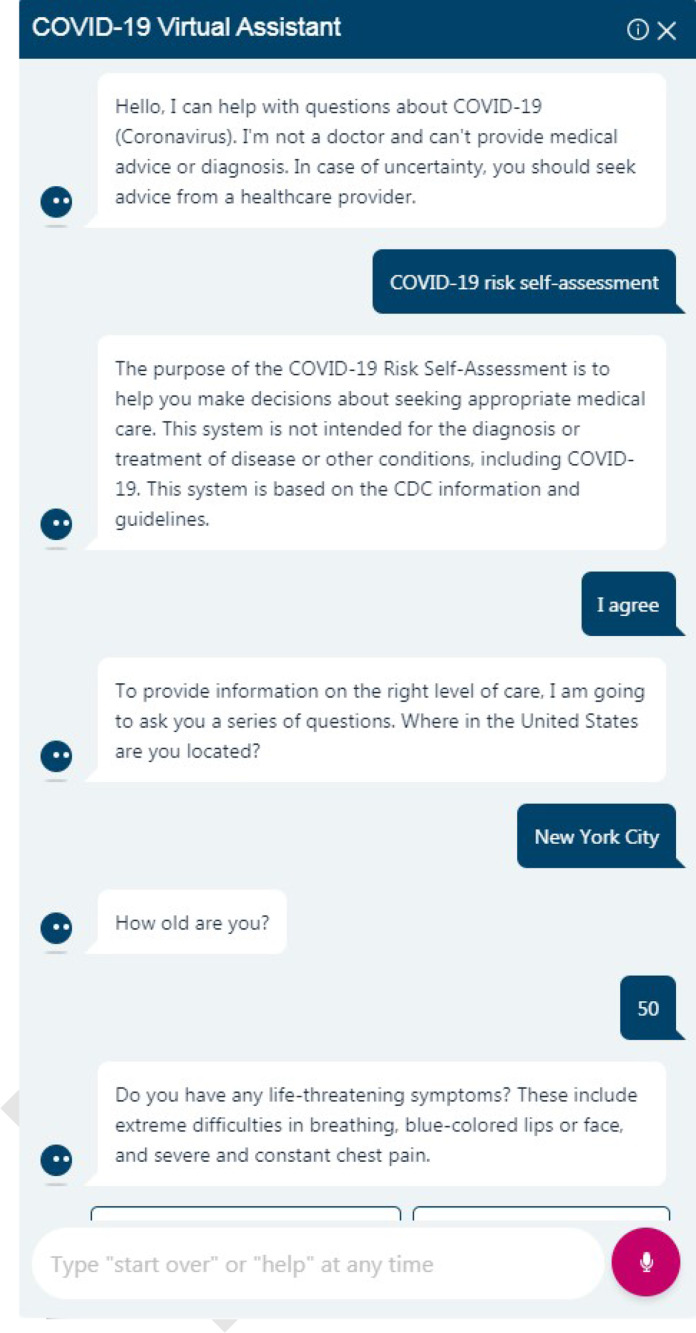
Acceleration of digital innovations is the silver lining of the COVID-19 crisis. Increased integration of AI into new radiology workflows to help with efficient patient communication and scheduling within the constraints of new safety measures include the use of predictive analytics and virtual assistants such as chatbots (Figure 6) (56, 57, 58). A chatbot is a computer application that uses AI to converse with a user typically through text chats or voice commands. Machine learning algorithms are being developed to detect and differentiate COVID-19 pulmonary findings from other etiologies on CT scan and CXR (59, 60).
Figure 6:
COVID-19 Virtual Assistant. Effective integration of AI into new radiology workflows help efficient patient communication and educationwith the use of a chatbot. Virtual assistants can evaluate risk self-assessment including the need for immediate attention, provide access to speak to a provider, help schedule a visit, and provide up-to-date information about COVID-19 testing sites and availability, visitor policies, and other patient care information.
Virtual operations command centers, specifically focused on imaging, enable rapid decision-making and allow radiology departments to effectively manage staffing, resources, image quality and volumes across multiple sites. Thermal temperature-check devices and contactless check-in kiosks allow safe entry into imaging centers. Electronic workflows include symptom reporting, expanded online patient scheduling and preregistration. Patient portal websites allow easy access to imaging test preparation instructions and educational materials.
Digital communications technology has been employed for clinical image interpretation, patient care, conferencing and education. Teleradiology and remote reading have been well-received by radiologists and allow flexible work shifts and reduced stress. Telehealth has rapidly expanded to include remote patient consultation services for IR procedures and lung cancer screening. Teleconferencing and remote readout with screen sharing as well as new electronic teaching tools have been implemented in response to the profound impact of the pandemic on radiology training programs. Digital learning resources for trainees have expanded and are being offered as alternatives to in-person teaching (61). These digital innovations have distinctly transformed the way radiologists work and the changes will continue in the daily practice of radiology after the pandemic ends. The challenge for radiologists will be how to deal with further loss of direct contact and interaction with patients.
Perspective from Australia: The effectiveness of an early concerted response
Australia had a rapid, politically - bipartisan response to the pandemic in March, with implementation of social distancing, work from home orders, closures of non-essential businesses and remote education delivery by universities and schools. These measures were supported by government investment in income support and loan forbearance. International air and sea arrivals from non-Australian citizens and non-permanent residents ceased. Elective surgery was cancelled nationwide to free beds and make PPE more available in both the private and public sectors for anticipated COVID – 19 hospitalizations. Widespread testing, mandatory isolation, intensive contact tracing and 14-day quarantine for international arrivals underpinned a successful national health strategy that saw the first wave end within a few weeks, and the country looking forward to “getting back to normal”. The vast majority of first wave cases were acquired in other countries; community transmission was very low.
Dominating the Australian pandemic story is the heterogeneity of its second wave, a result of widespread community transmission in only one state, Victoria, following breaches of infection control in quarantine facilities. Strict lockdown, school and nonessential business closures, mandatory mask wearing, and police enforced curfews helped daily case numbers in Victoria plummet from over 800 to 21 within 5 weeks. The economic cost to individuals, businesses and government was significant but the number of cases and deaths prevented was also enormous.
Radiology in Australia is not “post pandemic” but is adjusting to a new “COVID normal”. Infrastructure support for remote reporting and provision of PPE has varied widely within each state and around the country and between public and private sectors. For example, radiologists employed in a large multi -campus academic health science center already had access to home reporting workstations for on-call work, and the information technology (IT) systems and staff to support them were in place. This made it far easier to scale work from home. Institution sponsored online videoconferencing platforms were rapidly rolled out to all medical staff allowing supervision of trainees, tutorials and multidisciplinary meetings to be run remotely. Telehealth consultations increased from 20% to nearly 70% of outpatient clinic encounters in a few short months. These sudden, forced innovations transformed the way business is done and have improved care for many patients who no longer need to travel to check in with their specialist or get a prescription. Improved efficiency of uninterrupted home diagnostic reporting and improved attendance at multidisciplinary case conferences have been unexpected side benefits. Paradoxically, increased remote work has made radiologists in Australia more connected to referring physicians, radiology colleagues, trainees and technologists. Increased videoconferencing has not only decreased geographical barriers to participation in international meetings, but has also made radiologists more directly accessible through real-time screen share of workstation images and case discussion, elevating the value of radiologists as consultants, experts, and members of patient care teams. It is likely that after an effective vaccine is developed, SARS-CoV-2 will transition from the virus of the pandemic to the seasonal influenza, just like MERS and the Spanish influenza before it, but it is unlikely radiologists in Australia will go back to previous workflows.
Perspective from Singapore: Long term paradigm shifts based on lessons learned
As we balance ‘business as usual’ with COVID-19 care, it is imperative that radiologists reflect upon long-range permanent changes that radiology services must make in the post-COVID-19 world. We can start by learning from recent experience.
The Severe Acute Respiratory Syndrome (SARS) epidemic had a profound impact on health care systems, resulting in long-term adjustments. In one example (62), transformative changes were instituted in a radiology service that prioritized infection control measures at the individual and system levels. These included scheduling of appointments that consider the infective risks of patients, regular cleaning of facilities undertaken by dedicated staff and including infection control measures in the planning of all future imaging facilities. Separate facilities for inpatients and outpatients were configured and at least one CT and one MRI suite were equipped with negative air pressure for highly infectious cases. Emergency planning also included scenarios for infectious disease outbreaks, coordinated from institutional to national levels. While some of these measures were rapidly implemented, most changes took resources time and resolve to realize. With the COVID-19 pandemic, these measures have stood the test as they were based on strong foundational principles (63).
The scale and duration of the COVID-19 pandemic have, however, highlighted additional issues that radiology services must address in the ‘new normal’ post-COVID-19 world. Patients will demand the highest standard of infection control measures and these must be practiced consistently whether or not there is an infectious disease outbreak (Figure 7). Patients will demand ‘just-in-time’ service. To minimize patient dwell time, detailed preplanning of every patient visit will be required. This can create opportunities for new innovative operational processes, leveraging IT and AI. Radiology can take the lead in deciding on the imaging pathway for each patient rather than delegating this to the clinical teams. Consideration should be made for inpatient general radiography and ultrasound procedures to be performed at the bedside, reducing the need to transport patients to radiology facilities.
Figure 7:
Preparing for a portable interventional radiology procedure in a COVID-19 isolation room. Full PPE with N-95 respirator and face shield. The level of PPE should be concordant with risk of aerosolized particles generated during a procedure.
Organizations must look at sustaining working from home for radiologists and support staff where feasible. Radiology services should also explore how imaging can be delivered in a way that minimizes the need for patient contact and potential disease transmission. When a procedure has to be performed on-site, other processes such as appointment scheduling, counselling and consultation can be delivered virtually.
Facility planning must consider multi-functional facilities with the flexibility to pivot quickly to address different levels of disease outbreaks. In one example, an institution designed a parking garage as an overflow facility that can be converted during civil emergencies (64). In this facility, medical consultation and treatment rooms and a lead lined room for portable x-ray were purpose-built and can be deployed on short notice. These facilities are optimized for providing care unlike make-shift tents and ad-hoc conversion of non-clinical areas. While many solutions will be complex and will take time to implement, radiology must seize the opportunity to transform and thrive in the post-COVID-19 world.
Conclusions
SARS-CoV-2 is easily transmitted among humans and has quickly spread throughout the world. Healthcare professionals responded rapidly to better understand the disease, and developed systems to better diagnose and treat infected patients, protect healthcare workers, and impede spread. However, in the latter part of 2020, infections rose to an all-time high incidence in many parts of the globe. We face new management challenges in radiology departments, and it is imperative that we remain flexible and continue to evolve our approaches to optimize our patients’ care. For example, as healthcare systems mobilized to care for COVID-19 patients, care of patients with other diseases was often delayed. As the initial wave subsided, their care was prioritized based on the severity of disease and risk of further delays.
At the outset of the pandemic, testing kits were not readily available and chest CT examinations were often used to diagnose COVID-19 pneumonia in clinically suspected patients in many regions in the world. Criteria for the appropriate use of imaging examinations have gained consensus, with heterogeneity reflecting local imaging and in vitro testing availability. Improved workflows in radiology departments along with methods for cleaning and extending PPE use have been implemented to decrease the transmission of COVID-19 in the hospital setting.
Radiology has played a crucial role in the assessment of better treatment methods, including measurement of disease changes and predicting prognosis. Moreover, pathophysiology identified by noninvasive imaging has also suggested novel interventions for clinical testing to decrease patient morbidity and mortality. AI approaches have helped make rapid image assessment more available to provide patient management guidance.
Although the responses to the COVID-19 pandemic were variable depending upon the number of infected individuals, effectiveness of governmental leadership and availability of resources, much has been learned and shared through the medical literature. We better understand the transmission of the virus and are more skilled in the treatment of infected patients. Efforts are now underway to prepare for an expected increase in patients as 2020 comes to a close.
Acknowledgments
Acknowledgements
The authors gratefully acknowledge the work of RSNA members around the world in response to the COVID-19 pandemic and in service to their patients. They also thank the Radiological Society of North America (RSNA) staff for its support in coordinating global input and cooperation, as well as technical assistance, in development of this paper.
Footnotes
Funding: $0
References
- 1.RSNA News article: https://www.rsna.org/news/2020/June/COVID-Open-Radiology-Database.
- 2.Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, Lui MM, Lee JCY, Chiu KW, Chung TW, Lee EYP, Wan EYF, Hung IFN, Lam TPW, Kuo MD, Ng MY. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology 2020;296(2):E72-e78. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fang Y, Zhang H, Xu Y, Xie J, Pang P, Ji W. CT Manifestations of Two Cases of 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology 2020;295(1):208-209. doi: 10.1148/radiol.2020200280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, Ling Y, Jiang Y, Shi Y. Emerging 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology 2020;295(1):210-217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li M, Lei P, Zeng H, Li Z, Yu P, Fan B, Wang C, Li Z, Zhou Z, Hu S. and Liu H, Coronavirus Disease (COVID-19): Spectrum of CT Findings and Temporal Progression of the Disease. Acad Radiol 2020; 27:603-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wan S, Li M, Ye Z, Yang C, Cai Q, Duan S. and Song B. CT Manifestations and Clinical Characteristics of 1115 Patients with Coronavirus Disease 2019 (COVID-19): A Systematic Review and Meta-analysis. Acad Radiol 2020; 27:910-921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology 2020;296(2):E32-e40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, Ji W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology 2020;296(2):E115-e117. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.General Office of National Health Committee . Office of state administration of traditional Chinese medicine. Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (trial fifth edition), 2020. http://bgs.satcm.gov.cn/zhengcewenjian/2020-02-06/12847.html. [Google Scholar]
- 10.Zhang Yanling. ”Official: nucleic acid test results for fever outpatients is reported within 6 hours”. http://www.chinanews.com/gn/2020/07-02/9227906.shtml
- 11.Chinese Society of Radiology . Radiological diagnosis of COVID-19: expert recommendation from the Chinese Society of Radiology (First edition). Chinese Journal of Radiology 2020;54(4):279-285. doi: 10.3760/cma.j.cn112149-20200205-00094. [Google Scholar]
- 12.American College of Radiology . ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/ Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Accessed October 06, 2020.
- 13.Stempniak M. CT should not be used as first-line tool against coronavirus, ACR warns following pandemic declaration. Radiology Business. https://www.radiologybusiness.com/topics/care-delivery/ct-scan-coronavirus-chest-x-ray-radiology-covid-19. Accessed October 06, 2020. [Google Scholar]
- 14.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology 2020;295(3):715-721. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Francone M, Iafrate F, Masci GM, Coco S, Cilia F, Manganaro L, Panebianco V, Andreoli C, Colaiacomo MC, Zingaropoli MA, Ciardi MR, Mastroianni CM, Pugliese F, Alessandri F, Turriziani O, Ricci P, Catalano C. Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. European radiology 2020:1-10. doi: 10.1007/s00330-020-07033-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shiri I, Akhavanallaf A, Sanaat A, Salimi Y, Askari D, Mansouri Z, Shayesteh SP, Hasanian M, Rezaei-Kalantari K, Salahshour A, Sandoughdaran S, Abdollahi H, Arabi H, Zaidi H. Ultra-low-dose chest CT imaging of COVID-19 patients using a deep residual neural network. European radiology 2020. doi: 10.1007/s00330-020-07225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chinese Society of Imaging Technology. Expert consensus of radiological examination scheme and infection prevention of coronavirus disease 2019 (Trial version first). Electronic Journal of Emerging Infectious Diseases 2020;5(2):65-73. [Google Scholar]
- 18.Mahdavi A, Haseli S, Mahdavi Arash, Bakhshayeshkaram M, Foroumandi M, Nekooghadam SM, Raoufi M, Taheri MS. The Role of Repeat Chest CT Scan in the COVID-19 Pandemic. Academic Radiology, Vol. 27, Issue 7, p1049–1050. Published online: May 3, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zali A, Sohrabi MR, Mahdavi A, Khalili N, Taheri MS, Maher A, Sadoughi M, Zarghi A, et al. Correlation Between Low-Dose Chest Computed Tomography and RT-PCR Results for the Diagnosis of COVID-19: A Report of 27,824 Cases in Tehran, Iran. Academic Radiology. Publication stage: In Press Corrected Proof. Published online: September 21, 2020. [DOI] [PMC free article] [PubMed]
- 20.Radpour A, Bahrami-Motlagh H, Taaghi MT, Sedaghat A, Karimi MA, Hekmatnia A, Haghighatkhah HR, Sanei-Taheri M, et al. COVID-19 Evaluation by Low-Dose High Resolution CT Scans Protocol. Academic Radiology, Vol. 27, Issue 6, p901. Published online: April 17, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Toussie D, Voutsinas N, Finkelstein M, Cedillo MA, Manna S, Maron SZ, Jacobi A, Chung M, Bernheim A, Eber C, Concepcion J, Fayad ZA, Gupta YS. Clinical and Chest Radiography Features Determine Patient Outcomes in Young and Middle-aged Adults with COVID-19. Radiology 2020;297(1):E197-E206. doi: 10.1148/radiol.2020201754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, Lui MM, Lee JCY, Chiu KW, Chung TW, Lee EYP, Wan EYF, Hung IFN, Lam TPW, Kuo MD, Ng MY. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology 2020;296(2):E72-e78. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Revzin MV, Raza S, Warshawsky R, D'Agostino C, Srivastava NC, Bader AS, Malhotra A, Patel RD, Chen K, Kyriakakos C, Pellerito JS. Multisystem Imaging Manifestations of COVID-19, Part 1: Viral Pathogenesis and Pulmonary and Vascular System Complications. Radiographics 2020;40(6):1574-1599. doi: 10.1148/rg.2020200149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grillet F, Behr J, Calame P, Aubry S, Delabrousse E. Acute Pulmonary Embolism Associated with COVID-19 Pneumonia Detected with Pulmonary CT Angiography. Radiology 2020;296(3):E186-e188. doi: 10.1148/radiol.2020201544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xiao AT, Tong YX, Zhang S. Profile of RT-PCR for SARS-CoV-2: a preliminary study from 56 COVID-19 patients. Clinical infectious diseases : Publication of the Infectious Diseases Society of America 2020. doi: 10.1093/cid/ciaa460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Han Y, Chen T, Bryant J, Bucciarelli-Ducci C, Dyke C, Elliott MD, Ferrari VA, Friedrich MG, Lawton C, Manning WJ, Ordovas K, Plein S, Powell AJ, Raman SV, Carr J. Society for Cardiovascular Magnetic Resonance (SCMR) guidance for the practice of cardiovascular magnetic resonance during the COVID-19 pandemic. J Cardiovasc Magn Reson 2020;22(1):26. doi: 10.1186/s12968-020-00628-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bhayana R, Som A, Li MD, Carey DE, Anderson MA, Blake MA, Catalano O, Gee MS, Hahn PF, Harisinghani M, Kilcoyne A, Lee SI, Mojtahed A, Pandharipande PV, Pierce TT, Rosman DA, Saini S, Samir AE, Simeone JF, Gervais DA, Velmahos G, Misdraji J, Kambadakone A. Abdominal Imaging Findings in COVID-19: Preliminary Observations. Radiology 2020;297(1):E207-E215. doi: 10.1148/radiol.2020201908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldberg-Stein S, Fink A, Paroder V, Kobi M, Yee J, Chernyak V. Abdominopelvic CT findings in patients with novel coronavirus disease 2019 (COVID-19). Abdom Radiol (NY) 2020;45(9):2613-2623. doi: 10.1007/s00261-020-02669-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fan BE. COVID-19-Asspcoated Thromboembolic Events Causing Acute Mesenteric Ischaemia. Acad Radiol In Press September 21, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, De Leacy RA, Shigematsu T, Ladner TR, Yaeger KA, Skliut M, Weinberger J, Dangayach NS, Bederson JB, Tuhrim S, Fifi JT. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. The New England journal of medicine 2020;382(20):e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gulko E, Oleksk ML, Gomes W, Ali S, Mehta H, Overby P, Al-Mufti F, Rozenshtein A. MRI Brain Findings in 126 Patients with COVID-19: Initial Observations from a Descriptive Literature Review. AJNR Am J Neuroradiol 2020. doi: 10.3174/ajnr.A6805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kremer S, Lersy F, de Sèze J, Ferré JC, Maamar A, Carsin-Nicol B, Collange O, Bonneville F, Adam G, Martin-Blondel G, Rafiq M, Geeraerts T, Delamarre L, Grand S, Krainik A, Caillard S, Marc Constans J, Metanbou S, Heintz A, Helms J, Schenck M, Lefèbvre N, Boutet C, Fabre X, Forestier G, de Beaurepaire I, Bornet G, Lacalm A, Oesterlé H, Bolognini F, Messie J, Hmeydia G, Benzakoun J, Oppenheim C, Bapst B, Megdiche I, Henri-Feugeas MC, Khalil A, Gaudemer A, Jager L, Nesser P, Talla Mba Y, Hemmert C, Feuerstein P, Sebag N, Carré S, Alleg M, Lecocq C, Schmitt E, Anxionnat R, Zhu F, Comby PO, Ricolfi F, Thouant P, Desal H, Boulouis G, Berge J, Kazémi A, Pyatigorskaya N, Lecler A, Saleme S, Edjlali-Goujon M, Kerleroux B, Zorn PE, Mathieu M, Baloglu S, Ardellier FD, Willaume T, Brisset JC, Boulay C, Mutschler V, Hansmann Y, Mertes PM, Schneider F, Fafi-Kremer S, Ohana M, Meziani F, David JS, Meyer N, Anheim M, Cotton F. Brain MRI Findings in Severe COVID-19: A Retrospective Observational Study. Radiology 2020:202222. doi: 10.1148/radiol.2020202222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ai T, Yang Z, Hou H, Zhan C, Chen Chong, Lv W, Tao Q, Sun Z, Xia L. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 2020; 296:E32–E40 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu J, Yu H, Zhang S. The indispensable role of chest CT in the detection of coronavirus disease 2019 (COVID-19). Eur J Nucl Med Mol Imaging. 2020 Apr 3 : 1–2. doi: 10.1007/s00259-020-04795-x [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, Ji W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology 2020; 296:E115–E117. doi.org/10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.He L., Yu H., Shi L. et al. Equity assessment of the distribution of CT and MRI scanners in China: a panel data analysis. Int J Equity Health 17, 157 (2018). 10.1186/s12939-018-0869-y Accessed 1 May 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kabongo J, Nel S, Pitcher RD. An analysis of licenced South African diagnostic imaging equipment. Pan Afr Med J. 2015; 22:57 doi:10.11604/pamj.2015.22.57.7016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ngoya P, Muhogora W, Pitcher RD. Defining the diagnostic divide: an analysis of registered radiological equipment resources in a low-income African country. Pan Afr Med J. 2016;25:99. doi:10.11604/pamj.2016.25.99.9736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maboreke T, Banhwa J, Pitcher RD. Licensed radiology equipment resources as a measure of healthcare access and equity: A Zimbabwean study. Pan Afr Med J. 2019;34:60. doi:10.11604/pamj.2019.34.60.18935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mbewe C, Chanda-Kapata P, Sunkutu-Sichizya V, Lambwe N, Yakovlyeva N, Chirwa M, Ayele B, Pitcher RD. An audit of licenced Zambian diagnostic imaging equipment and personnel. Pan Afr Med J. 2020 May 22;36:32. doi: 10.11604/pamj.2020.36.32.21043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.American College of Radiologists . ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Accessed 12 March 2020. [Google Scholar]
- 42.Risk factors for COVID-19 death in a population cohort study from the Western Cape Province, South Africa. Boulle A, Davies MA, Hussey H, et al. Clin Infect Dis. 2020 Aug 29:ciaa1198. doi: 10.1093/cid/ciaa1198. (Online ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stop TB Partnership . The potential impact of the COVID-19 response on tuberculosis in high-burden countries: a modelling analysis. May 20, 2020. http://www.stoptb.org/assets/documents/news/Modeling%20Report_1%20May%202020_FINAL.pdf (accessed September 28, 2020). [Google Scholar]
- 44.Jewell BL, Mudimu E, Stover J, Kelly SL, Phillips A. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models. The Lancet HIV. 10.1016/S2352-3018(20)30211-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Albano D, Bruno A, Bruno F, et al. Impact of coronavirus disease 2019 (COVID-19) emergency on Italian radiologists: a national survey. Eur Radiol. 2020; 10.1007/s00330-020-07046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Politi LS, Balzarini L. The Radiology Department during the COVID-19 pandemic: a challenging, radical change. Eur Radiol. 2020;30(7):3600–3602; 10.1007/s00330-020-06871-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.SIRM. www.sirm.org. Accessed October 4, 2020. [Google Scholar]
- 48.Neri E, Miele V, Coppola F, Grassi R. Use of CT and artificial intelligence in suspected or COVID-19 positive patients: statement of the Italian Society of Medical and Interventional Radiology. Radiol Med. 2020; 10.1007/s11547-020-01197-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Neri E, Coppola F, Larici AR, et al. Structured reporting of chest CT in COVID-19 pneumonia: a consensus proposal. Insights Imaging. 2020;11(1):92 10.1186/s13244-020-00901-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.EpiCentro . Infografica web - Dati della Sorveglianza integrata COVID-19 in Italia. https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard. Accessed October 4, 2020. [Google Scholar]
- 51. Source: https://www.gov.br/saude/pt-br.
- 52. Source: https://www.hc.fm.usp.br/
- 53. Source: https://radvid19.com.br/
- 54.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382:929-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.COVID-19 Treatment Guidelines Panel . Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. Available at https://www.covid19treatmentguidelines.nih.gov/. Accessed September 16, 2020. [PubMed]
- 56.Whitelaw S, Mamas MA, Topol E, et al. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digit Health. 2020 Aug; 2(8):e435-e440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Budd J, Miller BS, Manning EM, et al. Digital technologies in the public-health response to COVID-19. Nat Med. 2020 Aug; 26(8):1183-1192. doi: 10.1038/s41591-020-1011-4. [DOI] [PubMed] [Google Scholar]
- 58.Cai W, Liu T, Xue X, Sheng J, Chen F. and Liang T. CT Quantification and Machine-learning Models for Assessment of Disease Severity and Prognosis of COVID-19 Patients. Acad Radiol In Press September 21, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mei X, Lee HC, Diao KY. et al. Artificial intelligence-enabled rapid diagnosis of patients with COVID-19. Nat Med. 2020 Aug; 26(8):1224-1228. doi: 10.1038/s41591-020-0931-3. Epub 2020 May 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bai HX, Wang R, Xiong Z. et al. AI Augmentation of Radiologist Performance in Distinguishing COVID-19 from Pneumonia of Other Etiology on Chest CT. Radiology. 2020 Sep; 296(3):E156-E165. doi: 10.1148/radiol.2020201491. Epub 2020 Apr 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alvin MD, George E, Deng F, et al. The Impact of COVID-19 on Radiology Trainees. Radiology. 2020 Aug; 296(2):246-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gogna A, Tay KH, Tan BS. Severe acute respiratory syndrome: 11 years later--a radiology perspective. AJR Am J Roentgenol. 2014;203:746–748. doi: 10.2214/AJR.14.13062. [DOI] [PubMed] [Google Scholar]
- 63.Cheng LT, Chan LP, Tan BH, Chen RC, Tay KH, Ling ML. et al. Deja vu or jamais vu? How the severe acute respiratory syndrome experience influenced a Singapore radiology department's response to the coronavirus disease (COVID-19) epidemic. AJR Am J Roentgenol. 2020;214:1206–1210. doi: 10.2214/AJR.20.22927. [DOI] [PubMed] [Google Scholar]
- 64.Quah LJJQ, Tan BKK, FuaT, Wee CPJ, Lim CS, Nadarajan G. et al. Reorganising the emergency department to manage the COVID-19 outbreak. Int J Emerg Med. 2020 Jun 17;13(1):32. doi: 10.1186/s12245-020-00294-w. [DOI] [PMC free article] [PubMed] [Google Scholar]