Abstract
Objective
To contribute objective evidence on health care utilization among migrants to the UK to inform policy and service planning.
Methods
We analysed data from Understanding Society, a household survey with fieldwork from 2015 to 2017, and the European Health Interview Survey with data collected between 2013 and 2014. We explored health service utilization among migrants to the UK across primary care, inpatient admissions and maternity care, outpatient care, mental health, dental care and physiotherapy. We adjusted for age, sex, long-term health conditions and time since moving to the UK.
Results
Health care utilization among migrants to the UK was lower than utilization among the UK-born population for all health care dimensions except inpatient admissions for childbirth; odds ratio (95%CI) range 0.58 (0.50–0.68) for dental care to 0.88 (0.78–0.98) for primary care). After adjusting for differences in age and self-reported health, these differences were no longer observed, except for dental care (odds ratio 0.57, 95%CI 0.49–0.66, P < 0.001). Across primary care, outpatient and inpatient care, utilization was lower among those who had recently migrated, increasing to the levels of the nonmigrant population after 10 years or more since migrating to the UK.
Conclusions
This study finds that newly arrived migrants tend to utilize less health care than the UK population and that this pattern was at least partly explained by better health, and younger age. Our findings contribute nationally representative evidence to inform public debate and decision-making on migration and health.
Keywords: healthcare utilization, migration, primary care, secondary care, survey analysis
Introduction
As in many other countries, the health and care sector in England is facing combined pressures from rising demand against constrained resources. For example, between 2006 and 2016, the number of admissions to hospital rose by 28%,1 alongside increases in primary care clinical workload by 16%,2 requiring growth in funding for the National Health Service (NHS) of 4% per year to keep pace with rising need.3 At the same time, the number of people living in the UK has increased by 5.5 million, of which three million are due to net migration. In 2018, 14% of UK residents were born outside the country, compared with 9% in 2004.4 With public discourse linking immigration to increased demand for health services5,6 and a need to ensure equitable access to care, objective, up-to-date evidence about migrants’ utilization of health care is required to inform policy.
Reasons for increased health care utilization among migrants compared to nonmigrants include greater risk for certain communicable and occupational conditions, poor mental health and maternal health problems7 and unfamiliarity with health care in the new country that may lead to transient rises in utilization in some settings.8 The latter can however also act as barrier to accessing health care, so lowering utilization,9 alongside uncertainty about eligibility for health care among service users and providers.10 Other reasons for lower utilization include the relatively younger ages of migrants,4,11 the ‘salmon-bias effect’ where migrants return to their country of birth when they become ill, or to access health care, and the ‘immigrant health-advantage’ where migrants have better health relative to native-born populations in the host countries.
Existing evidence of health care utilization among migrants tends to be equivocal. For example, analysis of UK household survey data up to 2009 found that migrants used hospital and GP services at broadly the same rate as the UK born populations,12 while during 2000–2008, secondary care use among migrants was about half the rate of the nonmigrant population.13
This study sought to contribute to the evidence base by analysing cross-sectional data, exploring how migrants’ health care utilization compared to that of UK-born population and the factors that may explain utilization patterns among migrants.
Methods
Data
This study used data collected as part of two large national surveys. The first was the Understanding Society (US), a nationally representative longitudinal household panel survey covering approximately 40,000 UK households. It started in 2009 with participants interviewed annually and includes two ‘immigrant and ethnic minority’ boost samples.14 The present analysis focused on wave 7 (January 2015 to June 2017) which included questions on health care utilization for the first time. We used the cross-sectional adult (16+) main interview weight for wave 7, including all households.14
The second survey was the European Health Interview Survey (EHIS), a cross-sectional survey conducted every 5 years of people aged 15 years and older across European countries.15 We used wave 2 (EHIS2), which included the UK, with data collected between March 2013 and September 2014 using nationally representative probability samples of people resident in private households and young people living away from home in a student hall of residence, or similar.15 Twenty per cent of households were interviewed face-to-face; 80% by telephone. Weights were estimated for the final sample to take account of sampling and nonresponse and to adjust to external reference data on the UK population.
Measurement of health care utilization in surveys
In preliminary analyses, we compared the survey measures of utilization to national data (see Online Supplement A and B). We used the survey items from EHIS and US dichotomized to describe health service utilization in the past 12 months across seven domains; US: primary care, inpatient admissions, outpatient care and inpatient admissions for childbirth; EHIS: mental health, dental care and physiotherapy, which are not collected in US. Full question wording is presented in Online Supplement C.
Definition of migrants
There is no formal legal definition of an international migrant but reasonable consensus that ‘an international migrant is someone who changes his or her country of usual residence, irrespective of the reason for migration or legal status.’16 For research, country of birth and nationality are two dimensions that can sometimes define whether someone is considered a migrant.16 We used responses to survey questions in both EHIS and US asking about country of birth to define whether someone is a ‘migrant’ to the UK. In addition, in US, we used responses to a question asking about year of arrival to the UK.
Demographic and health measures
We used self-reported measures of sex (women, men), age (categorized into eight groups 16–24, then 10-year age groups to 75–84, and 85+), grouped household income (using the total household net income without deductions, categorized into five groups), employment status (categorized as in employment, in education, retired and otherwise not working), ethnicity and the presence or absence of a long-term health condition or disability (using responses to the question ‘Do you have any long-standing physical or mental impairment, illness or disability?’). Items were consistent across US and EHIS.
Data analysis
Survey responses with missing data for country of birth, year of arrival in the UK (US only), age, sex and long-term health conditions were excluded. Proxy responses were only included for EHIS, as US proxy responses did not include answers to health care utilization questions. Missing health care utilization responses were excluded on an analysis-by-analysis basis.
After describing the demographic characteristics, we estimated the weighted, unadjusted proportion of people reporting service utilization in the past 12 months over the seven health service domains by migrant status. Inpatient admissions were calculated excluding admissions for childbirth.
Statistical model
In multivariable analysis, we explored the association between utilization in the past 12 months over the seven domains, and whether someone was a migrant, in three separate analyses: (1) unadjusted; (2) adjusting for age and sex and (3) additionally adjusting for whether someone had a long-term health condition. We used weighted logistic regression, accounting for the primary sampling unit (household) in the analysis using clustered standard errors. The analysis of US additionally accounted for sampling strata.
We further explored whether the association between being a migrant and health service utilization varied with time since moving to the UK, after adjusting for age and sex, and then long-term conditions, using only health service utilization outcomes measured in US (primary care, inpatient and outpatient).
Sensitivity analysis
In preliminary analyses, we explored alternative survey items measuring self-rated health. We additionally explored the impact of further adjustment for household income, ethnicity and employment status. Where similar question responses were available from EHIS and US, we compared findings from both surveys. We repeated the analysis of EHIS data excluding proxy responses, and, additionally, repeated our analysis using the 2017 wave of US data.
In further sensitivity analysis, we explored whether results were consistent between EU and non-EU migrants and a further analysis considered England only, as health policy is developed at the level of devolved nations. We used Stata 15.0 for all analyses.17
Results
We included 20,072 people in our sample from EHIS and 38,511 from US (see Online Supplement D for the survey responses flow chart). Among US respondents, 10.2% were migrants to the UK, compared to 11.9% of EHIS respondents. Of these (US respondents), 28.8% had arrived in the UK before 2006. In both samples, migrants were more likely to be aged 25–44 and in employment or studying (Table 1); they were overrepresented in the highest wealth quintile in US (23.9%) but in the lowest quintile in EHIS (23.3%).
Table 1.
Sociodemographic characteristics of respondents to Understanding Society and the European Health Interview Survey.
| Understanding Society |
European Health Interview Survey |
|||
|---|---|---|---|---|
| All included responsesN (weighted %) | Born outside the UKN (weighted %) | All included responsesN (weighted %) | Born outside the UKN (weighted %) | |
| All | 38,511 (100) | 6477 (10.2) | 20,072 (100) | 1825 (11.9) |
| Living in the UK >10 years | ||||
| Yes | 33,198 (92.8) | 1164 (28.8) | ||
| No | 5313 (7.2) | 5313 (71.2) | ||
| Sex | ||||
| Women | 21,407 (52.2) | 3712 (53.4) | 10,935 (51.3) | 1012 (52.5) |
| Men | 17,104 (47.8) | 2765 (46.6) | 9137 (48.7) | 813 (47.5) |
| Age | ||||
| 16–24 | 4766 (12.7) | 525 (11.2) | 1138 (14.2) | 91 (11.2) |
| 25–34 | 5058 (13.6) | 1029 (20.4) | 1693 (16.8) | 311 (26.7) |
| 35–44 | 6568 (15.2) | 1669 (26.2) | 2690 (16.3) | 439 (24.5) |
| 45–54 | 7263 (18.2) | 1310 (18.4) | 3438 (17.5) | 326 (16.6) |
| 55–64 | 6125 (15.9) | 993 (11.5) | 3960 (14.1) | 263 (9.1) |
| 65–74 | 5207 (13.9) | 562 (7.0) | 4298 (11.7) | 224 (6.0) |
| 75–84 | 2759 (7.8) | 317 (4.0) | 2294 (7.5) | 143 (5.1) |
| 85+ | 765 (2.7) | 72 (1.2) | 561 (1.9) | 28 (0.8) |
| Grouped household income (n = 20,064) | ||||
| Lowest | 6630 (20.0) | 1181 (18.4) | 3644 (17.8) | 434 (23.3) |
| Second | 6874 (20.1) | 1172 (18.3) | 4043 (19.3) | 396 (22.6) |
| Third | 6957 (20.0) | 1138 (20.5) | 4024 (18.6) | 299 (15.0) |
| Fourth | 7044 (19.9) | 1089 (19.0) | 4174 (21.2) | 303 (16.7) |
| Highest | 6913 (20.0) | 1272 (23.9) | 4179 (23.2) | 392 (22.4) |
| Employment status (n = 20,061) | ||||
| In employment | 21,214 (55.5) | 3661 (62.7) | 9680 (58.2) | 1037 (61.8) |
| Student | 2599 (6.4) | 378 (8.5) | 548 (5.7) | 83 (8.4) |
| Retired | 9384 (26.0) | 1009 (13.0) | 7599 (23.6) | 399 (12.8) |
| Unemployed/otherwise not working | 5303 (12.0) | 1422 (15.9) | 2234 (12.5) | 305 (17.0) |
| Long-term health condition/disability | ||||
| Yes | 13,062 (35.6) | 1733 (23.1) | 10,673 (45.1) | 746 (33.0) |
| No | 25,449 (64.4) | 4744 (76.9) | 9399 (54.9) | 1079 (67.0) |
In both surveys, migrants were less likely to report a long-term health condition or disability (Table 1). Across all seven domains of health care, except inpatient admissions for childbirth, fewer migrants reported having used services in the 12 months before data collection (Table 2).
Table 2.
Health care utilization in the last 12 months among respondents to Understanding Society and the European Health Interview Survey.
| Survey | All included responsesN (weighted %) | Born outside the UKN (weighted %) | |
|---|---|---|---|
| Primary care (n = 38,477) | Understanding Society | 28,233 (72.4) | 4900 (69.9) |
| Outpatient (n = 38,472) | Understanding Society | 16,605 (43.5) | 2577 (38.5) |
| Inpatient (n = 38,482) | Understanding Society | 3021 (7.9) | 462 (6.3) |
| Inpatient maternity care (n = 9247) | Understanding Society | 521 (5.2) | 133 (6.4) |
| Mental health services (n = 20,055) | European Health Interview Survey | 583 (3.6) | 39 (2.4) |
| Dental care (n = 20,047) | European Health Interview Survey | 14,969 (74.0) | 1226 (64.0) |
| Physiotherapy (n = 20,055) | European Health Interview Survey | 2606 (12.4) | 218 (10.6) |
In unadjusted analysis, the odds ratio (OR) and 95% confidence intervals (CI) of using health care ranged from 0.58 (95% CI 0.50–0.68) for dental care to 0.88 (95% CI 0.78–0.98) for primary care (Table 3). Adjusting for differences in age and sex attenuated the strength of these associations across all domains except for outpatient services (OR 0.90, 95% CI 0.82–0.98; P = 0.022), mental health services (0.57, 0.50–0.67; P = 0.013) and dental care (0.58, 0.50–0.67; P < 0.0001), which remained statistically significant. Additional adjustment for long-term health condition or disability eliminated any evidence of statistical differences in utilization among migrants for all domains except dental care.
Table 3.
Health care utilization in the past 12 months among people born outside the UK (migrants), compared with people born in the UK.
| Unadjusted |
Adjusted for age and sex |
Additionally adjusted for the presence of a long-term health condition or disability |
||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Primary care (n = 38,477) | 0.88 (0.78–0.98) | 0.019 | 0.98 (0.88–1.09) | 0.739 | 1.07 (0.96–1.20) | 0.232 |
| Outpatient (n = 38,472) | 0.79 (0.72–0.87) | <0.001 | 0.90 (0.82–0.98) | 0.022 | 0.99 (0.90–1.09) | 0.801 |
| Inpatient (n = 38,482) | 0.77 (0.65–0.90) | 0.001 | 0.91 (0.78–1.08) | 0.283 | 1.02 (0.86–1.20) | 0.857 |
| Inpatient maternity care (n = 9247) | 1.28 (0.92–1.79) | 0.140 | 1.18 (0.85–1.64) | 0.325 | 1.14 (0.82–1.58) | 0.429 |
| Mental health services (n = 20,055) | 0.63 (0.41–0.97) | 0.036 | 0.57 (0.37–0.89) | 0.013 | 0.71 (0.45–1.10) | 0.121 |
| Dental care (n = 20,047) | 0.58 (0.50–0.68) | <0.001 | 0.58 (0.50–0.67) | <0.001 | 0.57 (0.49–0.66) | <0.001 |
| Physiotherapy (n = 20,055) | 0.82 (0.68–0.99) | 0.040 | 0.83 (0.69–1.00) | 0.053 | 0.88 (0.73–1.06) | 0.183 |
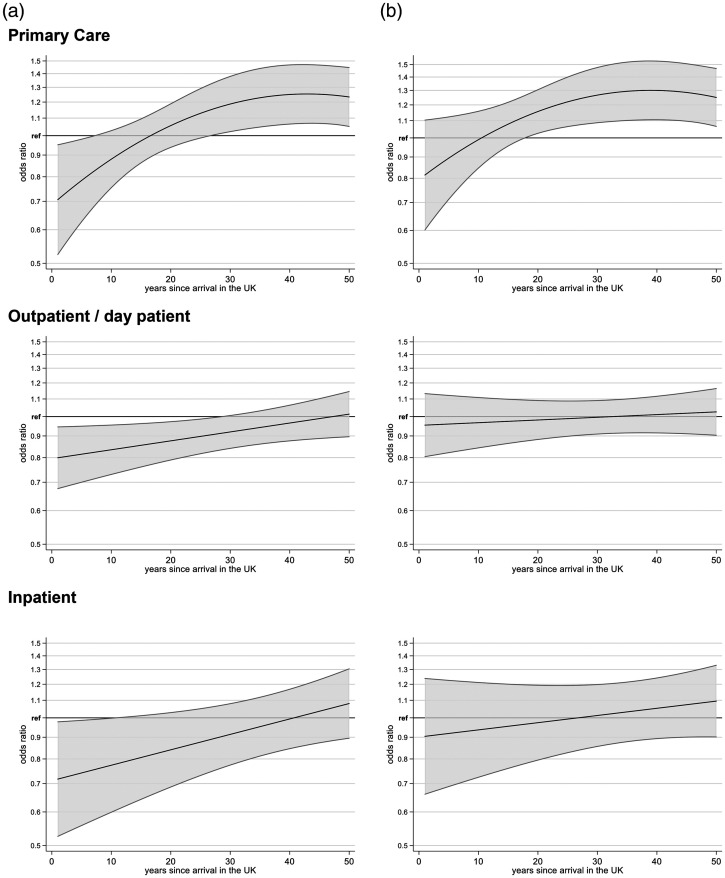
Incorporating time since migration to the UK into the analysis, and adjusting for age and sex, we found that inpatient, outpatient and primary care utilization were lower among migrants who had arrived more recently compared with the UK-born population (Figure 1). Outpatient utilization reached the levels of the nonmigrant population after about 25 years since arrival in the UK, and inpatient utilization after about 10 years. Among migrants who had lived in the UK for more than 10 years, primary care utilization reached the levels of nonmigrants, and after 25 years utilization was higher. After additionally adjusting for long-term health condition or disability, primary care was the only domain where utilization among long-term migrants remained higher compared to nonmigrants (see also Online Supplement E).
Figure 1.
Health care utilization in the last 12 months and time since arrival in the UK. (a) adjusting for age and sex; (b) additionally adjusting for long term health conditions.
Our findings remained stable in a series of sensitivity analyses, which adjusted for household income and employment status, among other items (Online Supplement F–L). Analysis of US 2017 data revealed findings that were broadly consistent with those of 2016 data presented here (Online Supplement J). However, large attrition in recent migrants between waves resulted in wider confidence intervals for the models estimating change in utilization over time, which is why we used 2016 data. Equally, findings remained broadly consistent when restricting the analysis to survey responses from England only (Online Supplement K) and there was no evidence of heterogeneity between EU and non-EU migrants. The only exception was primary care where there was evidence of higher utilization among non-EU migrants compared with EU migrants, and physiotherapy, with lower utilization among non-EU migrants (Online Supplement L).
Discussion
This study finds that, on average, health care utilization among migrants to the UK was lower than utilization among the UK-born population across a range of health service domains. The only exception was inpatient maternity care, where utilization among migrants tended to be higher, but this difference was not statistically significant. Evidence of lower utilization in all domains except dental care was no longer observed once age and self-rated health of migrants were adjusted for.
These findings suggest that lower health care utilization by migrants is driven, mainly, by the younger age of migrants compared to the UK-born population and a better health status with fewer long-term conditions. Having said that, there was heterogeneity in utilization depending on time since individuals had migrated to the UK, with utilization typically lower among recent migrants and increasing to the levels of the nonmigrant population among those who had been living in the UK for 10 years or more.
Findings in context
Our findings are consistent with previous studies reporting lower, or similar, health care utilization among migrants.18 We build on this evidence, suggesting that lower utilization can often be explained by younger age and better health among migrant populations. Previous work from the UK echoes this observation, noting that adjustment for sociodemographic factors explains most differences among migrants to the UK.19
Graetz et al.8 also reported heterogeneity in utilization between types of health services, concluding that utilization of accident and emergency services and hospitalizations were higher among migrants than nonmigrants. However, their systematic review found the opposite to be true for outpatient visits for specialized care, which is consistent with our findings of lower outpatient utilization among migrants. Lower inpatient13 and dental care utilization18 among migrants have also been described previously.
Similarly, variation in health service utilization by length of time in the country among migrants was described previously, although findings are not consistent.7 For example, Steventon and Bardsley found that hospital admission rates among migrants remained low over several years after arrival in the UK13; Jayaweera and Quigley were unable to provide evidence of differences in health care utilization among migrants, even considering changes over time.19 Other work documented evidence regarding changes in health with time since migration, such as an increasing risk of death of migrants from South Asia to the UK over time,20 or, in California, USA, a decline in the rated health advantage of the foreign-born population with increasing duration of residency.21
Strengths and limitations
The strength of our study is that we present findings from two nationally representative data sets. US and EHIS are high-quality national surveys; translators are used when required, responses are weighted to address nonresponse, and there was minimal missing data in the items considered in this analysis. Recent and short-term migrants to the UK may be underrepresented, particularly among US respondents, who are part of a longitudinal study. US recruited an additional immigrant and ethnic minority boost sample in 2016, which was used in this analysis, to address this concern.22
The use of survey responses rather than administrative measures of health service utilization, presents both strengths and limitations; we explored the validity of this approach further in our supplementary analysis. The strength of our study is that the population sample was recruited independent of prior contact with health services. This reduces the risk of underestimating service utilization among migrants when using administrative data, with for example Stagg et al. reporting low-level GP registration among migrant groups.23 In addition, survey measures such as those used in our analysis will capture utilization not routinely recorded in administrative health records (e.g. use of dental services). In the same way, measures of self-reported health may capture unmet health need in the population compared with administrative data, but information reported is subjective and may vary with age, gender, religion and culture.24
A limitation in the scope of this study is that the survey data analysed do not include measures on use of accident and emergency care, with some international evidence indicating there may be higher utilization of such services by migrants than nonmigrants.25
Implications for policy and service planning
Migrants constitute a considerable proportion of the UK population and it is important that appropriate services are available for these populations. Our analysis highlights that recent migrants to the UK are typically working age adults in good health with low health care utilization relative to the nonmigrant UK population, and after accounting for these factors, we find little difference in health service utilization compared with nonmigrants. Health service planning for migrant populations should take into account the lower health care utilization of young, healthy adults; a focus on primary care provision is likely to be most appropriate.
Evidence that the health of migrants to the UK gets worse over time20 and our finding that utilization increases suggests that services should also ensure that migrants are not missing the opportunity for preventive health care that have the potential to prevent onset of conditions and help avoid some later health care use. Our findings that migrants use dental services less than nonmigrants is a second area where future policy should focus on promoting preventive health; addressing barriers to access including cost of dental care in the UK is an additional area for policy development.
US provides a timely snapshot of NHS use by migrants, but the survey is not designed to collect detailed information at the clinical and health service level, such as primary care registration, clinical procedures and diagnoses, or local rather than national impacts, which would be needed to inform those planning services in the NHS. Future research should look at utilizing administrative data from primary and secondary care, with novel linkage techniques likely to provide further insights into service use among and appropriate for migrants.26
Conclusions
This study found that migrants to the UK typically had lower health care utilization than nonmigrant populations. These differences were explained, mainly, by younger age and fewer health conditions and were largest for migrants who had recently moved to the UK. The findings of this work contribute nationally representative evidence to inform public debate and decision-making on migration and health care.
Supplemental Material
Supplemental material, HSR911392 Supplemental Material for Healthcare utilization among migrants to the UK: cross-sectional analysis of two national surveys by Catherine L Saunders, Adam Steventon, Barbara Janta, Mai Stafford, Carol Sinnott, Lucinda Allen and Sarah R Deeny in Journal of Health Services Research & Policy
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed the receipt of the following financial support for the research, authorship, and/or publication of this article: CLS and BJ received payment from The Health Foundation for their work on this project. CS is funded by a National Institute for Health Research (NIHR) Clinical Lectureship in General Practice. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
ORCID iD: Catherine L Saunders https://orcid.org/0000-0002-3127-3218
Supplemental material: Supplemental material is available for this article online.
References
- 1.The Health Foundation. Chart: Trends in the Number of English NHS Hospital Admissions , 2006 to 2016 www.health.org.uk/chart/chart-trends-in-the-number-of-english-nhs-hospital-admissions-2006-to-2016 (2018, accessed 8 February 2020).
- 2.Hobbs FDR, Bankhead C, Mukhtar T, et al. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007-14. Lancet 2016; 387: 2323–2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Health Foundation. Joint letter to the Prime Minister on NHS funding. www.health.org.uk/news-and-comment/news/joint-letter-to-the-prime-minister-on-nhs-funding (2018, accessed 8 February 2020).
- 4.Office for National Statistics. Population of the UK by Country of Birth and Nationality, www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/internationalmigration/datasets/populationoftheunitedkingdombycountryofbirthandnationality (2019, accessed 8 February 2020).
- 5.Hansard. Immigrants (NHS Treatment) House of Commons Hansard. 25 March 2013. http://hansard.parliament.uk/commons/2013-03-25/debates/13032510000004/Immigrants(NHSTreatment) (2013, accessed 8 February 2020).
- 6.Moore M, Ramsay G. UK media coverage of the 2016 EU referendum campaign. London: The Policy Institute at King’s College London, Centre for the Study of Media, Communication and Power, 2017. [Google Scholar]
- 7.Rechel B, Mladovsky P, Devillé W, et al. Migration and health in the European Union: an introduction In: Rechel B, Mladovsky P, Devillé W, et al. (eds) Migration and health in the european union. Maidenhead: Open University Press, 2011, pp. 3–13. [Google Scholar]
- 8.Graetz V, Rechel B, Groot W, et al. Utilization of health care services by migrants in Europe—a systematic literature review. Br Med Bull 2016; 121: 5–18. [DOI] [PubMed] [Google Scholar]
- 9.Agudelo-Suarez AA, Gil-Gonzalez D, Vives-Cases C, et al. A metasynthesis of qualitative studies regarding opinions and perceptions about barriers and determinants of health services’ accessibility in economic migrants. BMC Health Serv Res 2012; 12: 461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rafighi E, Poduval S, Legido-Quigley H, et al. National Health Service principles as experienced by vulnerable London migrants in “Austerity Britain”: a qualitative study of rights, entitlements, and civil-society advocacy. Int J Health Policy Manag 2016; 5: 589–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Health and Social Care. Independent Report : Overseas Visitors and Migrant Use of the NHS : Extent and Costs. www.gov.uk/government/publications/overseas-visitors-and-migrant-use-of-the-nhs-extent-and-costs (2013, accessed 8 February 2020).
- 12.Wadsworth J. Musn’t Grumble. Immigration, health and health service use in the UK and Germany. Fiscal Studies 2013; 34: 55–82. [Google Scholar]
- 13.Steventon A, Bardsley M. Use of secondary care in England by international immigrants. J Health Serv Res Policy 2011; 16: 90–94. [DOI] [PubMed] [Google Scholar]
- 14.University of Essex, Institute for Social and Economic Research. Understanding society: waves 1-8, 2009-2017 and harmonised BHPS: waves 1-18, 1991–2009. [data collection]. 11th ed. UK Data Service SN: 6614, 2018.
- 15.Northern Ireland Statistics and Research Agency, Office for National Statistics. European Health Interview Survey: United Kingdom Data, Wave 2, 2013–2014. [data collection]. UK Data Service SN: 7881, 2016.
- 16.The Migration Observatory at the University of Oxford. Who Counts as a Migrant? Definitions and their Consequences. http://migrationobservatory.ox.ac.uk/resources/briefings/who-counts-as-a-migrant-definitions-and-their-consequences/ (2017, accessed 8 February 2020).
- 17.StataCorp. Stata statistical software: Release 15. College Station: StataCorp LLC, 2017 [Google Scholar]
- 18.Sarria-Santamera A, Hijas-Gomez AI, Carmona R, et al. A systematic review of the use of health services by immigrants and native populations. Public Health Rev 2016; 37: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jayaweera H, Quigley MA. Health status, health behaviour and healthcare use among migrants in the UK: evidence from mothers in the Millennium Cohort Study. Soc Sci Med 2010; 71: 1002–1010. [DOI] [PubMed] [Google Scholar]
- 20.Harding S. Mortality of migrants from the Indian subcontinent to England and Wales: effect of duration of residence. Epidemiology 2003; 14: 287–292. [PubMed] [Google Scholar]
- 21.Uretsky MC, Mathiesen SG. The effects of years lived in the United States on the general health status of California’s foreign-born populations. J Immigr Minor Health 2007; 9: 125–136. [DOI] [PubMed] [Google Scholar]
- 22.Lynn P, Nandi A, Parutis V, et al. Design and implementation of a high-quality probability sample of immigrants and ethnic minorities: lessons learnt. Demres 2018; 38: 513–548. [Google Scholar]
- 23.Stagg HR, Jones J, Bickler G, et al. Poor uptake of primary healthcare registration among recent entrants to the UK: a retrospective cohort study. BMJ Open 2012; 2: e001453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hjelm K, Bard K, Nyberg P, et al. Religious and cultural distance in beliefs about health and illness in women with diabetes mellitus of different origin living in Sweden. Int J Nurs Stud 2003; 40: 627–643. [DOI] [PubMed] [Google Scholar]
- 25.Crede SH, Such E, Mason S. International migrants’ use of emergency departments in Europe compared with non-migrants’ use: a systematic review. Eur J Public Health 2018; 28: 61–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burns R, Pathak N, Campos-Matos I, et al. Million Migrants study of healthcare and mortality outcomes in non-EU migrants and refugees to England: Analysis protocol for a linked population-based cohort study of 1.5 million migrants. Wellcome Open Res 2019; 4: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, HSR911392 Supplemental Material for Healthcare utilization among migrants to the UK: cross-sectional analysis of two national surveys by Catherine L Saunders, Adam Steventon, Barbara Janta, Mai Stafford, Carol Sinnott, Lucinda Allen and Sarah R Deeny in Journal of Health Services Research & Policy