Abstract
Context:
Surgical correction of scars may not be an ideal solution in all cases and hence it is desirable to have a nonsurgical option available. Autologous platelet-rich plasma (PRP) and fractional carbon dioxide laser (FCL) offer an alternative treatment modality.
Aims:
To compare the efficacy and safety of FCL and intradermal PRP with FCL in the management of postburn and posttraumatic scars.
Settings and Design:
A prospective, randomized, observer-blinded, comparative study was conducted at a hospital skin centre from Oct 2016 to Sep 2018.
Subjects and Methods:
A total of 67 patients with scars were randomly divided into two groups; Group I was treated with four sessions of monthly FCL and Group II was treated with four sessions of PRP and FCL. The patients were assessed using the Patient and Observer Scar Assessment Scale (POSAS) at baseline and 4 weeks after each session.
Statistical Analysis Used:
For continuous variables, the summary statistics of mean ± standard deviation was used; for categorical data, number and percentage were used. Chi-square (χ2) test was used for association between two categorical variables. P value <0.05 was considered to be statistically significant.
Results:
Thirty cases in each group completed the study. There was a significant improvement in the total score of POSAS (p < 0.001) in both groups, but the final difference between the two groups was not statistically significant (p = 0.793 and P = 0.278, respectively).
Conclusions:
Fractional CO2 laser causes significant improvement in scar appearance. PRP in combination with FCL offers no additional advantage.
Keywords: Fractional CO2 laser, platelet-rich plasma, POSAS, scars
Introduction
Scars are a common problem as they inevitably develop after cutaneous dermal injury.[1] Superficially, a scar may appear to be only a cosmetic problem; however, they can remarkably impact the patients on many different physical and psychological levels. Physically, scars can impede the patients’ range of movements and can cause pain, dysesthesia, and pruritus.[2] Psychologically, low self-esteem and feelings of psychosocial alienation are felt.[3]
Various methods to improve the appearance of scars include pressure garments, intralesional corticosteroid therapy, dermabrasion, surgical corrections, chemical peels, laser treatment, and autologous platelet-rich plasma.[4]
Autologous platelet-rich plasma (PRP) is popular for posttraumatic, postburns, and acne scar treatment.[5,6,7,8] Platelet-rich plasma with platelet derived and other growth factors helps in regenerating damaged soft tissue.[9]
Fractional CO2 laser (FCL) is now well established in scar management as it provides superior results and lower side effects compared to conventional ablative lasers.[1,2,10]
As FCL creates microthermal wounding of skin, PRP is added to aid in wound healing and promote scar resolution.[11] Discordant reports in literature about efficacy of PRP exist and hence we conducted this study to compare the use of FCL monotherapy and addition of PRP in postburn and posttraumatic scar treatment.
Subjects and Methods
The study was conducted over a period of two years from Oct 2016 to Sep 2018 at a skin center of a referral hospital after obtaining ethical clearance from the institutional ethics committee. Patients aged 18–60 years reporting to the dermatology department with postburns or posttrauma scars were enrolled in the study [Figure 1]. Those with scars less than 6 months duration, concurrent infections or inflammatory skin disorders, known connective tissue disorders or hypersensitivity to lidocaine, history of laser or any other procedure for scars in last 06 months, keloidal/bleeding tendencies, unrealistic expectations, history of malignancy, and pregnancy/lactation were excluded.
Figure 1.
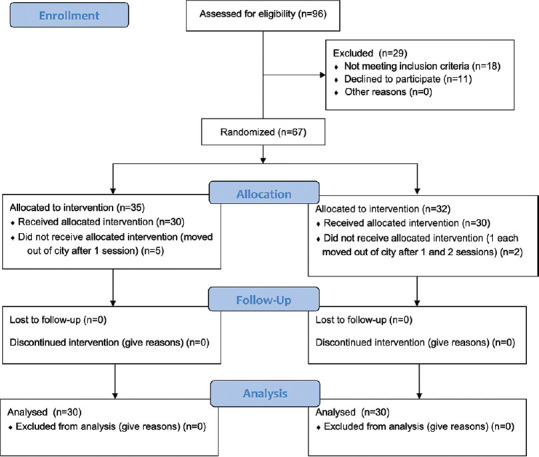
Study consort flow diagram
A written informed consent was obtained from each patient before recruitment. Patients who met the eligibility criteria were randomized by draw of cards into two groups, Group I and II by a dermatologist not engaged in this study.
Prior to treatment, a topical anesthetic cream containing a combination of topical lidocaine and prilocaine (EMLA) in a cream base was applied for 1 hour on and 1 cm around the scar area. Under aseptic precautions, Group I was treated with a single pass of FCL (Cis F1-Fractional CO2 Laser, Sellas, Korea) using a pulse energy of 25 mJ, spot density of 144/cm2, pulse interval of 0.5 mm, and pulse duration of 0.1 milliseconds. The second group was treated with FCL using the Group I settings and, in addition, intradermal injections at 1cm intervals of 0.1 ml PRP were given.[8] A two-stage centrifuge process was performed using an R8C centrifuge device (REMI Sales & Engineering Ltd. Goregaon (East), Mumbai, India) to obtain PRP. The spin speed determined using the device radius was 2316 RPM for 5 minutes-1st spin and 3538 RPM for 17 minutes-2nd spin.[12]
Four sessions of treatment were administered to each group at 4-week intervals and patients were assessed at baseline and after 4 weeks of each session by a third observer (blinded) using the Patient and Observer Scar Assessment Scale (POSAS) into the observer scale and patient scale to obtain the total POSAS score.[13] Requisite permission was obtained from POSAS group to use and quote the scale.
POSAS consists of an observer scale [Figure 2] and a patient scale [Figure 3] which includes a comprehensive list of items, based on the clinically relevant scar characteristics. Each item has a 10-point scoring ranging from “1” corresponding to normal skin to “10” implying the worst imaginable scar. The total score is calculated by adding up the scores of six items for both scales, the final score ranging from 6 to 60. An “Overall Opinion” of the scar quality is scored separately although it is not part of the total score.
Figure 2.
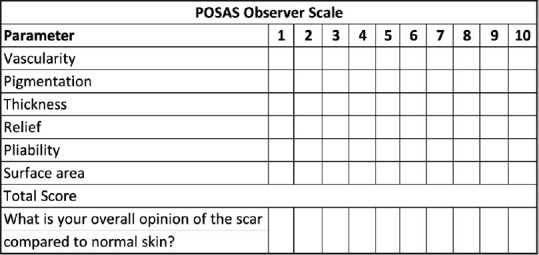
Observer-scale POSAS
Figure 3.
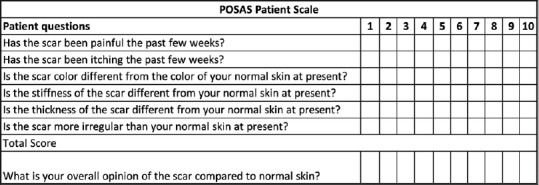
Patient-scale POSAS
Statistical analysis
All characteristics were summarized descriptively. For continuous variables, the summary statistics of mean ± standard deviation (SD) were used. For categorical data, the number and percentage were used in the data summaries and diagrammatic presentation. Chi-square (χ2) test was used to find the association between two categorical variables. If the P value was <0.05, then the results were considered to be statistically significant; otherwise, it was considered as not statistically significant. Data were analyzed using the Statistical Package for the Social Sciences (SPSS) software v. 23.0 and Microsoft Office 2007.
Results
A total of 96 patients were screened and 67 were randomized into the two groups. A total of 60 completed the study [Figure 1]. Both groups were age and gender matched with no statistical difference in number, location, and duration of scars between them [Table 1]. The commonest location of scars in both groups was the face. The mean duration of scars in Group I was 3 years and in Group II, 2.4 years.
Table 1.
Profile of patients
| Group I | Group II | |
|---|---|---|
| Age (Years)* | ||
| ≤20 | 8 | 7 |
| 21-25 | 14 | 14 |
| 26-30 | 7 | 7 |
| >30 | 1 | 2 |
| Number of scars* | ||
| 1 | 23 | 21 |
| 2 | 4 | 7 |
| 3 | 2 | 1 |
| >3 | 1 | 1 |
| Location of scars* | ||
| Face | 21 | 21 |
| Lower limb | 3 | 2 |
| Trunk | 2 | 0 |
| Upper limb | 4 | 7 |
| Cause of scars* | ||
| Post burn | 4 | 4 |
| Post traumatic | 26 | 26 |
*Difference between group I and II not significant (P>0.05)
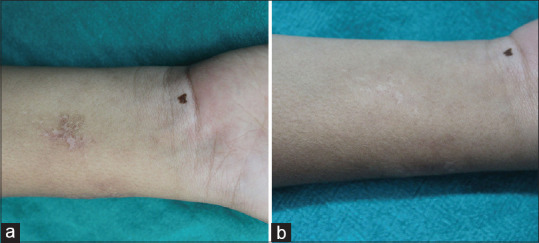
Statistically significant difference in the quality of scars was seen when the baseline individual parameters and total scores of observer part of POSAS were compared with the final scores in each group. Before and after scores were statistically significant (P < 0.001) in Group I [Figures 4a, b, 5a, b] and similar results (P < 0.001) were seen in Group II Table 2 and Table 3 indicating improvement in the quality of scars [Figures 6a, b and 7a, b].
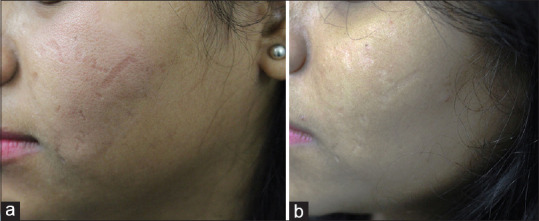
Figure 4.
(a) Baseline (POSAS Observer scale 28 and Patient scale 26); (b) at 16 weeks (POSAS Observer scale 20 and Patient scale 17) in a patient of Group I
Figure 5.

(a) Baseline picture (POSAS Observer scale 26 and Patient scale 20); (b) at 16 weeks (POSAS Observer scale 18 and Patient scale 16) in a patient of Group I
Table 2.
Mean POSAS observer scale parameters at baseline and week 16
| POSAS observer scale parameters Group I | Baseline | Week 16 | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Vascularity | 3.57 | 1.07 | 2.40* | 0.67 |
| Pigmentation | 4.57 | 1.33 | 3.37* | 0.72 |
| Thickness | 4.87 | 1.17 | 3.27* | 0.94 |
| Relief | 5.23 | 1.01 | 3.47* | 0.78 |
| Pliability | 4.63 | 1.25 | 3.57* | 0.90 |
| Surface area | 4.97 | 0.61 | 4.47* | 0.78 |
| Overall opinion | 5.50 | 0.73 | 3.77* | 0.90 |
| Total score | 27.83 | 4.36 | 20.53* | 3.42 |
| POSAS observer scale parameters Group II | ||||
| Vascularity | 3.52 | 0.96 | 2.29* | 0.86 |
| Pigmentation | 4.32 | 1.25 | 3.26* | 0.73 |
| Thickness | 5.19 | 1.05 | 3.45* | 0.81 |
| Relief | 5.26 | 0.68 | 3.35* | 0.80 |
| Pliability | 4.84 | 1.10 | 3.55* | 0.89 |
| Surface area | 4.97 | 0.55 | 4.39* | 0.84 |
| Overall opinion | 5.48 | 0.72 | 3.71* | 1.04 |
| Total score | 28.10 | 3.91 | 20.29* | 3.77 |
*Significant with level of significance (P<0.001). SD: Standard deviation
Table 3.
Mean POSAS patient scale parameters at baseline and week 16
| POSAS Patients scale parameters Group I | BASELINE | WEEK 16 | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Painful scar | 1.37 | 0.85 | 1.10** | 0.31 |
| Scar itching | 2.03 | 0.93 | 1.50* | 0.73 |
| Scar color different from normal skin | 4.63 | 1.30 | 3.37* | 0.93 |
| Stiffness of the scar different from normal skin | 4.80 | 1.03 | 3.63* | 0.85 |
| Thickness of the scar different from normal skin | 4.93 | 1.01 | 3.57* | 0.86 |
| Irregular scar | 5.33 | 1.06 | 3.73* | 0.58 |
| Overall opinion | 5.27 | 0.87 | 3.70* | 0.79 |
| Total score | 23.10 | 4.12 | 16.90* | 2.77 |
| POSAS Patients scale parameters Group II | ||||
| Painful scar | 1.07 | 0.25 | 1.00** | 0.00 |
| Scar itching | 1.67 | 0.66 | 1.13* | 0.35 |
| Scar color different from normal skin | 4.30 | 1.47 | 3.17* | 0.83 |
| Stiffness of the scar different from normal skin | 4.90 | 0.84 | 3.60* | 0.93 |
| Thickness of the scar different from normal skin | 5.07 | 0.98 | 3.53* | 0.86 |
| Irregular scar | 5.07 | 0.74 | 3.67* | 0.76 |
| Overall opinion | 5.27 | 0.78 | 3.57* | 0.82 |
| Total score | 22.07 | 3.26 | 16.10* | 2.88 |
**Not significant with level of significance (P>0.05). *Significant with level of significance (P<0.05). SD: Standard deviation
Figure 6.
(a) Baseline (POSAS Observer scale 22 and Patient scale 22); (b) at 16 weeks (POSAS Observer scale 19 and Patient scale 17) in a patient of Group II
Figure 7.
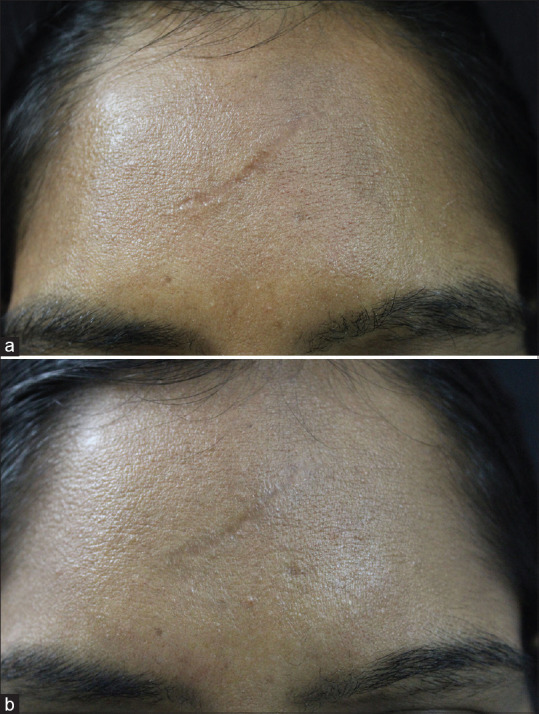
(a) Baseline picture (POSAS Observer scale 23 and Patient scale 19); (b) at 16 weeks (POSAS Observer scale 19 and Patient scale 15) in a patient of Group II
Similarly, a statistically significant difference in the quality of scars was noted when the baseline individual parameters and total scores of patient part of POSAS were compared with the final scores of each group, except for the parameter “painful scar.”
The baseline total scores of the observer and patient part of POSAS for Groups I and II indicated that the severity of scars was similar in both the groups and that they were comparable at the initiation of treatment. However, the final scores also indicated no significant difference in the quality of scars between the two groups. This indicated that although there was a significant improvement in both the groups, the addition of PRP to FCL in Group II did not result in superior scar improvement posttreatment as compared to Group I that was treated with FCL only [Tables 4 and 5].
Table 4.
Mean total score of the observer part of POSAS between study groups on follow up
| Total score | Group I | Group II | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| BASELINE | 27.83 | 4.36 | 28.10* | 3.91 |
| WEEK 4 | 26.77 | 4.23 | 26.94* | 4.08 |
| WEEK 8 | 24.13 | 3.89 | 24.16* | 4.07 |
| WEEK 12 | 22.70 | 3.69 | 22.81* | 3.29 |
| WEEK 16 | 20.53 | 3.42 | 20.29* | 3.77 |
*Not significant with level of significance (P>0.05). SD: Standard deviation
Table 5.
Mean total score of the patient part of POSAS between study groups at different weeks
| Total score | Group I | Group II | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| BASELINE | 23.10 | 4.12 | 22.07* | 3.26 |
| WEEK 4 | 22.37 | 3.58 | 21.67* | 3.11 |
| WEEK 8 | 20.43 | 3.62 | 19.33* | 3.10 |
| WEEK 12 | 18.73 | 3.12 | 18.10* | 2.90 |
| WEEK 16 | 16.90 | 2.77 | 16.10* | 2.88 |
*Not significant with level of significance (P>0.05). SD: Standard deviation
Pain and erythema were the commonest side effects observed in both groups with 11 affected in Group I and all 30 in Group II.
Discussion
Scar treatment is a challenge and a number of therapeutic options exist for the treating dermatologist. Among the treatment options available, literature reports successful use of lasers and nonablative devices in the management of acne scars, traumatic scars, and atrophic and hypertrophic burn scars with or without the use of PRP as an alternative to surgical correction.[7,14,15] The use of FCL in improving traumatic and burn scars is reportedly useful.[16,17] The rational for the clinical use of PRP is based on its ability to stimulate the production and subsequently, increase the concentration of growth factors and secretion of proteins which are able to improve the healing process at cellular level.[14]
We reviewed studies [Table 6] using FCL and PRP in traumatic and burn scars and also included postacne scars as fewer studies exist in the former. Acne scars are usually atrophic and thinner while posttraumatic and postburn scars are usually thicker.[16] While studies report FCL improves scars, discordance exists when PRP and FCL combination is compared to FCL alone. In studies, acne scars were noted to improve better when treated with FCL and topical PRP[6,7] or when PRP was injected.[5,7,8] Another comparative split face study done in acne scars comparing FCL and FCL with PRP did not reveal any additional PRP benefit.[18] A study conducted on posttraumatic scars showed that more than 50% treated showed moderate to excellent response,[11,19] while Faghihi et al. noted better scar correction on the PRP side but no statistical difference compared to FCL monotherapy.[20]
Table 6.
Review of studies on use of fractional CO2 laser and autologous platelet rich plasma in post acne, post traumatic and post burn scars
| Study | Type of study | Indication | Treatment modality | Number of patients | Duration of treatment/sessions | Scoring system used | Results |
|---|---|---|---|---|---|---|---|
| Lee JW et al. 2011[5] | Split-face randomized comparative study | Acne scars | Autologous PRP with Ablative CO2 Fractional resurfacing vs Fractional CO2 laser only | 14 | 01 session | Chromometer Quartile grading scale | PRP and FCL: enhanced recovery of laser-damaged skin, better clinical outcomes |
| Gawdat H I et al. 2014[6] | Split-face randomized study | Atrophic acne scars | FCL and (Intradermal or topical) PRP vs FCL monotherapy | 30 | 3 monthly sessions | GBQS | Combined PRP and FCL- significantly better response - no significant differences between intradermal and topical PRP |
| Arsiwala et al. 2019[7] | Randomized comparative study | Atrophic acne scars | FCL monotherapy versus FCL plus topical PRP | 25 | 03 monthly sessions | GBQS VAS | FCL plus topical PRP more effective |
| Majid et al. 2015[10] | Observational study | Nonhypertrophic traumatic and burn scar | FCL | 25 | 04 sessions at 06 weekly interval | Quartile grading scale | Excellent results with minimal adverse effects |
| Elsaie ML et al. 2018[14] | Randomized controlled trial | Postacne atrophic scars | Nonablative fractional erbium-doped glass 1540 nm and fractional ablative 10600 nm CO2 laser | 58 | 4 treatment sessions at 3 weeks interval | 4-grade satisfaction scale | Fractional ablative laser showed higher efficacy while nonablative laser offered less pain and shorter downtime |
| El-Hoshy K et al. 2017[15] | Uncontrolled, open-label clinical trial | Mature burn scars | FCL monotherapy | 20 | 03 sessions, at 4 to 8 weeks interval | VSS, POSAS | Effective and safe treatment method |
| Tawfic S et al. 2019[16] | Randomized study | Hypertrophic burn scars | Low, medium, and high-density FCL | 25 | 03 monthly sessions | VSS, POSAS | High-density fractional CO2: provides more improvement in burn scars both clinically and histopathologically |
| Kar BR, Raj C 2018[17] | Split-face comparative study | Acne scars | FCL and topical PRP vs FCL monotherapy | 30 | 03,monthly sessions | GBQS | Addition of PRP - better clinical outcome (but not statistically significant) |
| Faghihi G et al. 2015[19] | Split-face randomized controlled trial | Acne scars | FCL and PRP vs FCL monotherapy | 16 | 02 monthly session | VAS | FCL and PRP: no statistically significant synergistic effects |
| Present study | Randomized controlled study | Posttraumatic and postburn scars | FCL monotherapy vs FCL and PRP | 67 | 04 monthly sessions | POSAS | Statistically significant results in both groups; difference between both groups not statistically significant |
GBQS: Goodman and Baron qualitative scarring grading system, VAS: Visual Analogue Scale, VSS: Vancouver Scar Scale, POSAS: Patient and Observer Scar Assessment Scale, FCL: Fractional CO2 laser, PRP: Autologous Platelet rich plasma
We used POSAS, a validated tool which includes both the patients’ and physician's perspective, for outcome assessment, by a blinded observer and demonstrated that FCL is an effective modality in posttraumatic and postburn scar treatment. The addition of PRP to FCL offered no additional benefit and was accompanied with greater side effects in the form of pain and erythema in all cases. This worsening of erythema and pain could be attributed to the accumulating evidence that demonstrates that platelets contribute to the initiation and propagation of the inflammatory process.[21] Dermal scar pain is a complex issue and it is hypothesized that nerve growth factors which stimulate C-fibers not only play an important role in wound healing but also promote inflammation.[22] PRP despite its initial proinflammatory property is reported to help reduce this pain in the long run.[23] However, central sensitization results in long lasting pain despite adequate healing.[22] This may be the cause why our patients had persisting pain despite scar improvement on treatment. Patients in both groups observed stiffness of scar responded earliest followed by itching, thickness, and color response. The observer felt pliability and vascularity responded earlier than other parameters. We did not observe any long-term side effects.[7,10]
Thus, from this study, we concluded that the fractional CO2 laser alone was as effective as the combination of fractional CO2 laser with PRP. Avoiding PRP shall help reduce side effects, additional interventional procedures, and the overall cost.
Our study was limited due to the small sample size. The laser parameters were kept fixed for all scars to maintain consistency and avoid bias. This may have affected the end result as some scars may have been under or overtreated. An ideal assessment would include an ultrasonographic assessment of scar thickness to decide the laser type and its parameters.[24] Larger numbers of patient cohort, especially, for postburn scars, shall be needed to derive a final conclusion about the discordance in PRP effect and its usage.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Alster TS, Handrick C. Laser treatment of hypertrophic scars, keloids, and striae. Semin Cutan Med Surg. 2000;19:287–92. doi: 10.1053/sder.2000.18369. [DOI] [PubMed] [Google Scholar]
- 2.Lupton JR, Alster TS. Laser scar revision. Dermatol Clin. 2002;20:55–65. doi: 10.1016/s0733-8635(03)00045-7. [DOI] [PubMed] [Google Scholar]
- 3.Van Loey NEE, Van Son MJM. Psychopathology and psychological problems in patients with burn scars: Epidemiology and management. Am J Clin Dermatol. 2003;4:245–72. doi: 10.2165/00128071-200304040-00004. [DOI] [PubMed] [Google Scholar]
- 4.Gold MH, McGuire M, Mustoe TA, Pusic A, Sachdev M, Waibel J, et al. Updated international clinical recommendations on scar management: Part 2--algorithms for scar prevention and treatment. Dermatol Surg. 2014;40:825–31. doi: 10.1111/dsu.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 5.Lee JW, Kim BJ, Kim MN, Mun SK. The efficacy of autologous platelet rich plasma combined with ablative carbon dioxide fractional resurfacing for acne scars: A simultaneous split-face trial. Dermatol Surg. 2011;37:931–8. doi: 10.1111/j.1524-4725.2011.01999.x. [DOI] [PubMed] [Google Scholar]
- 6.Gawdat HI, Hegazy RA, Fawzy MM, Fathy M. Autologous platelet rich plasma: Topical versus intradermal after fractional ablative carbon dioxide laser treatment of atrophic acne scars. Dermatol Surg. 2014;40:152–61. doi: 10.1111/dsu.12392. [DOI] [PubMed] [Google Scholar]
- 7.Arsiwala NZ, Inamadar AC, Adya KA. A comparative study to assess the efficacy of fractional carbon dioxide laser and combination of fractional carbon dioxide laser with topical autologous platelet-rich plasma in post-acne atrophic scars. J Cutan Aesthet Surg. 2020;13:11–7. doi: 10.4103/JCAS.JCAS_142_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abdel Aal AM, Ibrahim IM, Sami NA, Abdel Kareem IM. Evaluation of autologous platelet-rich plasma plus ablative carbon dioxide fractional laser in the treatment of acne scars. J Cosmet Laser Ther. 2018;20:106–13. doi: 10.1080/14764172.2017.1368667. [DOI] [PubMed] [Google Scholar]
- 9.Boswell SG, Cole BJ, Sundman EA, Karas V, Fortier LA. Platelet-rich plasma: A milieu of bioactive factors. Arthrosc J Arthrosc Relat Surg. 2012;28:429–39. doi: 10.1016/j.arthro.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 10.Hsiao PF, Lin YC, Huang CC, Wu YH. Efficacy and safety of a single treatment using a 10,600-nm carbon dioxide fractional laser for mild-to-moderate atrophic acne scars in Asian skin. Dermatol Sin. 2013;31:59–63. [Google Scholar]
- 11.Makki M, Younes AEKH, Fathy A, Abd ElDayem OY, Morsy H. Efficacy of platelet-rich plasma plus fractional carbon dioxide laser in treating posttraumatic scars. Dermatol Ther. 2019;32:e13031. doi: 10.1111/dth.13031. [DOI] [PubMed] [Google Scholar]
- 12.Dhurat R, Sukesh M. Principles and methods of preparation of platelet-rich plasma: A review and author′s perspective. J Cutan Aesthetic Surg. 2014;7:189–97. doi: 10.4103/0974-2077.150734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Draaijers LJ, Tempelman FRH, Botman YAM, Tuinebreijer WE, Middelkoop E, Kreis RW, et al. The patient and observer scar assessment scale: A reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004;113:1960–5. doi: 10.1097/01.prs.0000122207.28773.56. [DOI] [PubMed] [Google Scholar]
- 14.Alser OH, Goutos I. The evidence behind the use of platelet-rich plasma (PRP) in scar management: a literature review Scars. Burns Heal [Internet] 2018. p. 4. cited 2020 Jun 8. Available from: https://wwwncbinlmnihgov/pmc/articles/PMC6243404/2 . [DOI] [PMC free article] [PubMed]
- 15.Elsaie ML, Ibrahim SM, Saudi W. Ablative fractional 10 600 nm carbon dioxide laser versus non-ablative fractional 1540 nm erbium-glass laser in Egyptian post-acne scar patients. J Lasers Med Sci. 2018;9:32–5. doi: 10.15171/jlms.2018.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El-Hoshy K, Abdel-Halim MRE, Dorgham D, El-Din Sayed SS, El-Kalioby M. Efficacy of fractional carbon dioxide laser in the treatment of mature burn scars: A clinical, histopathological, and histochemical study. J Clin Aesthetic Dermatol. 2017;10:36–43. [PMC free article] [PubMed] [Google Scholar]
- 17.Tawfic S, Sayed S, Nada A, Manaa D, Shalaby S. High- versus low-density fractional laser in the treatment of hypertrophic postburn scars: A randomized clinical trial. Dermatol Surg. 2019 doi: 10.1097/DSS.0000000000002293. doi: 101097/DSS0000000000002293. [DOI] [PubMed] [Google Scholar]
- 18.Kar BR, Raj C. Fractional CO2 laser vs fractional CO2 with topical platelet-rich plasma in the treatment of acne scars: A split-face comparison trial. J Cutan Aesthetic Surg. 2017;10:136–44. doi: 10.4103/JCAS.JCAS_99_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Majid I, Imran S. Efficacy and safety of fractional CO2 laser resurfacing in non-hypertrophic traumatic and burn scars. J Cutan Aesthetic Surg. 2015;8:159–64. doi: 10.4103/0974-2077.167276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Faghihi G, Fatemi-Tabaei S, Abtahi-Naeini B, Siadat AH, Sadeghian G, Ali Nilforoushzadeh M, et al. The effectiveness of a 5% retinoic acid peel combined with microdermabrasion for facial photoaging: A randomized, double-blind, placebo-controlled clinical trial? Dermatol Res Pract. 2017;2017:8516527. doi: 10.1155/2017/8516527. doi: 10.1155/2017/8516527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.May AE, Seizer P, Gawaz M. Platelets: Inflammatory firebugs of vascular walls. Arterioscler Thromb Vasc Biol. 2008;28:s5–10. doi: 10.1161/ATVBAHA.107.158915. [DOI] [PubMed] [Google Scholar]
- 22.Bijlard E, Uiterwaal L, Kouwenberg CAE, Mureau MAM, Hovius SER, Huygen FJPM. A systematic review on the prevalence, etiology, and pathophysiology of intrinsic pain in dermal scar tissue. Pain Physician. 2017;20:1–13. [PubMed] [Google Scholar]
- 23.Huang SH, Wu SH, Lee SS, Lin YN, Chai CY, Lai CS, et al. Platelet-rich plasma injection in burn scar areas alleviates neuropathic scar pain. Int J Med Sci. 2018;15:238–47. doi: 10.7150/ijms.22563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anderson RR, Donelan MB, Hivnor C, Greeson E, Ross EV, Shumaker PR, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: Consensus report. JAMA Dermatol. 2014;150:187–93. doi: 10.1001/jamadermatol.2013.7761. [DOI] [PubMed] [Google Scholar]


