Abstract
Introduction:
Lupus Vulgaris (LV) is the chronic, progressive, tissue destructive form of cutaneous tuberculosis. LV should be diagnosed and treated to prevent scaring and deformities. Histopathology is the gold standard for the diagnosis. Dermoscopy is helpful tool in diagnosing different dermatological condition. Here, dermoscopic and histopathogical correlation in LV was attempted.
Materials and Methods:
It was a cross sectional, observational study done from February 2019 to October 2019. Nineteen patients of LV were included. Dermlite 4 with attached smart phone (iphone) was employed. LV lesions were subjected to skin biopsy to confirm the diagnosis.
Results:
Study enrolled 19 patients, with 8males, 5 female and 6 children. Dermoscopy showed yellowish-white globules, white structureless areas and white scales were noted in 19 (100%) patients. Telangiectasias were seen in 16 (84.21%) patients as long linear, branching and short linear vessels. Pinkish-red background was noted in all patients (100% n=19). Newer observations included white shiny streaks, white rosettes and bluish hue. Age, sex, duration of lesions had no influence in the dermoscopic patterns. Discrepancy in dermoscopic-histopathologic correlation was noted. Facial lesions showed increased frequency of follicular plugs, patulous follicles and white rosettes.
Conclusion:
Dermoscopy is widely gaining importance in the realm of dermatology. In this study, dermoscopy demonstrated characteristic patterns in LV. Thus, dermoscopy a non-invasive procedure can be used as diagnostic tool in many infective dermatoses.
Keywords: Dermoscopy, diagnosis, histopathology, lupus vulgaris, patterns
Introduction
Lupus Vulgaris (LV) is a chronic, progressive, tissue destructive form of cutaneous tuberculosis commonly affecting the head and neck region. Occasionally due to its unusual presentation, it can pose difficulties in diagnosis.[1] LV should be diagnosed and treated as early as possible to prevent deformities. Histopathology is the gold standard for the diagnosis, but is an invasive, cumbersome and time-consuming process. Dermoscopy is an non-invasive, in vivo technique that helps in diagnosing different dermatological conditions by magnifying both surface and sub-surface features that are not appreciated by the unaided eye.[2] It is a link between clinical and histopathological diagnosis thereby may help avoiding the need for biopsy in certain situations.[3] Currently, utility of dermoscopy in LV is limited only to case reports.[4] Hence, we evaluated the dermoscopic patterns in LV and correlated them with histopathogical findings in patients with Fitzpatrick skin types IV-V.
Materials and Methods
This was a cross-sectional and observational study of 19 patients with clinical signs and symptoms of LV attending the Dermatology departments of two tertiary care hospitals in the Southern part of India between February 2019 and October 2019. Detailed history including the age, sex, duration of the disease, family history was documented. Dermlite™ DL4 (3Gen Inc., San Juan Capistrano, CA, USA) with 10× magnification attached to a Smartphone (iPhone 6, Apple Inc., Cupertino, CA, USA) was employed for dermoscopy. The technique was contact dermoscopy with and without ultrasound gel as an interface medium under polarized mode for the clarity of images.[5]
All the lesions were subjected to skin biopsy to confirm the diagnosis. Two of the authors (BSA, KAA) evaluated the dermoscopic patterns. The statistical analysis was performed using SPSS software (version 20; SPSS Inc., Chicago IL, USA). Frequencies were calculated for variables related to clinical and dermoscopic patient characteristics. Continuous variables such as age, duration are described as means ± standard deviations. Discrete variables are shown as percentages. Associations between qualitative variables, such as the presence or absence of specific dermoscopic features, were tested for statistical significance using χ2 test. A P value of <0.05 was considered to be statistically significant.
Results
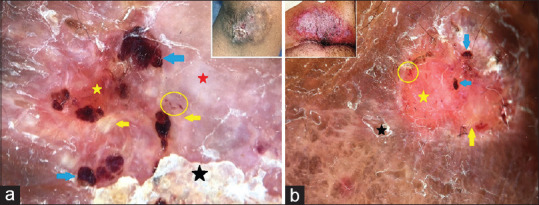
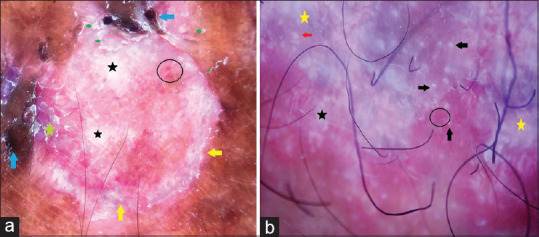
Of the 19 patients studied, 10 were males and 9 were females. The mean age of the patients was 33 years (with the youngest 10 years old and the oldest 56 years old). The mean duration of disease was 14 months (with a minimum of 4 months and maximum of 24 months). Dermoscopy showed yellowish-white globules which were seen scattered throughout the lesions in all the patients [Figure 1a]. Both white structureless areas and white scales were present in 19 (100%) patients [Figures 1a, b and 2a, b]. White shiny streaks [Figure 3a and b] which represent different orientation of collagen bundles in the dermis were observed in 6 (31.5%) patients. Interestingly, four-dot clods (white rosettes), an optical phenomenon on polarized dermoscopy, that correlates to the hyperkeratosis of dilated infundibulum, a form of white shiny streaks, were noted in two of the lesions. Telangiectasias were seen as long linear, branching and short linear vessels in the vicinity of yellowish-white globular structures [Figure 3a and b]. Patulous follicles [Figure 4a and b] and follicular plugging [Figure 2a and b] were seen in 3 (15.7%) and 4 (21.05%) patients, respectively, and were due to dilated infundibulum and keratin-filled follicles in histopathology. Small erosions were seen as ulcerations, whereas dried blood in the lesions appeared as dark red globular structures [Figures 5a, 5b and 6a]. Two patients (10.5%) showed bluish hue [Figure 6b]. which is similar to the bluish hue noted in basal cell carcinoma and melanoma. The pinkish-red background was noted in all the 19 patients (100%). The frequency of dermoscopic patterns is depicted in Table 1.
Figure 1.
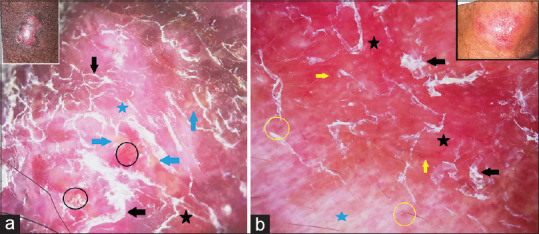
Panels a and b: Dermoscopy of lupus vulgaris shows yellow globules (blue arrows), white scales (black arrows), white structureless areas (blue stars), dotted vessels (black circles) and red globules (yellow circles) on the pinkish background (black stars). Linear vessels (yellow arrows) are well appreciated. Inset: Clinical images. [Polarized Dermoscopy, original magnification ×10]
Figure 2.
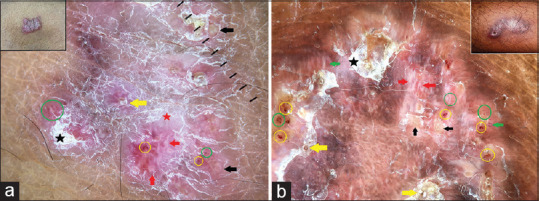
Panels a and b: Dermoscopy of lupus vulgaris shows yellow globules (black arrows), white scales (black stars), white structureless areas (red star), red dots (green circles), red globules (yellow circles) and linear vessels (green arrows). Note the white shiny streaks (red arrows) and pinkish background. Follicular plugs (yellow arrows) are well appreciated. Inset: Clinical images. [Polarized dermoscopy, original magnification ×10]
Figure 3.
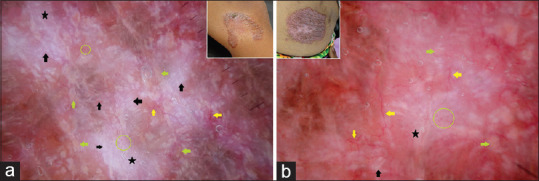
Panels a and b: Dermoscopy of lupus vulgaris shows white shiny streaks (black arrows), white structureless areas (black stars), linear and branching vessels (yellow arrows) and dotted vessels (green circles). Yellow globules (green arrows) and pinkish background are well appreciated. Inset: Clinical images. [Polarized dermoscopy, original magnification ×10]
Figure 4.
Panels a and b: Dermoscopy of lupus vulgaris shows white scales (black arrows), white structureless areas (black stars), linear vessels (yellow arrows) and patulous follicular openings (red arrows) on pinkish background. Note the four-dot clod (black circle) in panel b. Inset: Clinical images. [Polarized dermoscopy, original magnification ×10]
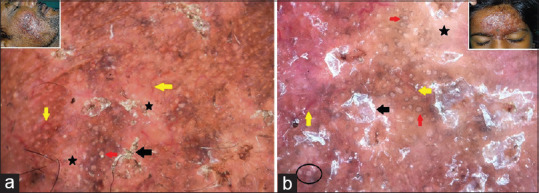
Figure 5.
Panels a and b: Dermoscopy of lupus vulgaris shows yellow globules (yellow arrows), ulceration (yellow stars), white structureless areas (red star), red globules (blue arrows) and red dots (yellow circles). White scales (black stars) and pinkish background are well appreciated. Inset: Clinical images. [Polarized dermoscopy, original magnification ×10]
Figure 6.
Panels a and b: Dermoscopy of lupus vulgaris shows white structureless areas (black stars), ulceration (yellow arrows), dark red globules (blue arrows), red dots and globules (black circles). Note the bluish hue (yellow stars), pinkish background and white rosette (red arrow) and white scales (green arrow). [Polarized dermoscopy, original magnification ×10]
Table 1.
Frequency of dermoscopic patterns in lupus vulgaris
| Dermoscopic patterns | Frequency (n=19) |
|---|---|
| Yellowish-white globules | 100% (19) |
| Pinkish-red background | 100% (19) |
| Reddish globules | 84.21% (16) |
| Dotted vessels | 84.21% (16) |
| Linear vessels | 84.21% (16) |
| Ulceration | 26.3% (5) |
| Whitish structureless areas | 100% (19) |
| Superficial scaling (white or yellow) | 100% (19) |
| White shiny streaks | 31.5% (6) |
| Follicular plugs | 21.05% (4) |
| Patulous follicles | 15.7% (3) |
| Bluish hue | 10.5% (2) |
Histopathology revealed hyperkeratosis, acanthosis, dilated capillaries, granulomas with lymphocytic infiltrate and Langhans giant cells [Figures 7 and 8a, b]. Other histopathological changes observed were dilated follicles with keratotic material and dermal fibrosis. The frequency of histopathological findings is outlined in Table 2. Dermoscopic-histopathologic correlation is described in Table 3. Some discrepancies between histopathological changes and dermoscopic patterns were observed in this study, possibly due to the difference in the site of biopsy and site of dermoscopy. Yellow globules demonstrated the highest diagnostic accuracy with 94.74% and correlated well with dermal granulomas, whereas the follicular plugs showed the lowest accuracy of diagnosis with 15.79%. The diagnostic accuracy of various dermoscopic patterns is depicted in Table 4. Age, sex and duration of lesions had no influence on the dermoscopic patterns. Facial lesions showed increased frequency of follicular plugs, patulous follicles and white rosettes. This can be attributed to the more number of follicles in facial skin and sun exposure may also play a role.
Figure 7.
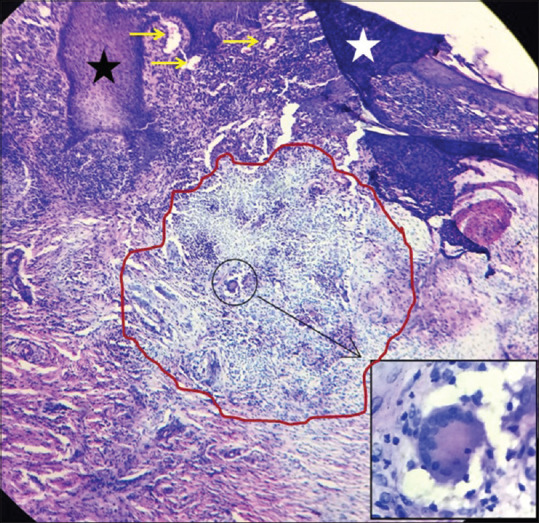
Histopathology of lupus vulgaris shows acanthosis (black star), hyperkeratosis (white star) and dilated capillaries (yellow arrows) and granuloma (red circle). Inset: Langhans giant cell. [H and E, 10×]
Figure 8.
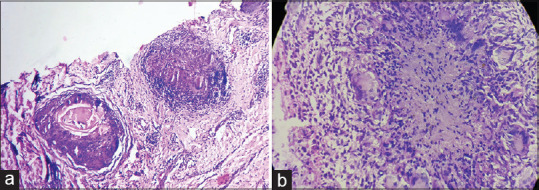
Panels a and b: Histopathology of lupus vulgaris shows well-demarcated granuloma with dilated capillaries and dilated follicles with follicular plug and lymphocytic infiltrate (panel a). Granuloma with multiple Langhans giant cells and lymphocytes are well appreciated (panel b). [H and E, 10×]
Table 2.
Frequency of histopathological changes in lupus vulgaris
| Histopathological Findings | Frequency (n=19) |
|---|---|
| Granuloma | 94.7% (18) |
| Dilated vessels | 84.21% (16) |
| Erosions in the epidermis and dermis | 52.6% (10) |
| Lymphocytic infiltrate | 94.7% (18) |
| Fibrosis | 84.21% (16) |
| Hyperkeratosis | 68.4% (13) |
| Acanthosis | 52.6% (10) |
Table 3.
Correlation of dermoscopic and histopathological changes in lupus vulgaris
| Dermoscopic patterns | Histopathological correlation |
|---|---|
| Yellowish-white globules | Dermal granulomas |
| Pinkish-red background | Widespread vasodilatation |
| Dotted vessels | Tips of normal vertical papillary loops |
| Red globules | Tips of ectatic/elongated papillary loops |
| Linear vessels | Ectatic/elongated subpapillary capillary plexus |
| Ulceration | Erosions in the epidermis and dermis |
| Whitish structureless areas* | Acanthosis and dermal fibrosis |
| Superficial white or yellow scales | Hyperkeratosis and/or parakeratosis |
| White shiny streaks | Orientation of collagen bundles in different angles in the dermis |
| Follicular plugs | Keratotic material in follicular infundibulum |
| Patulous follicles | Dilatation of infundibulum |
| Bluish hue | Orthokeratosis |
*White structureless area correlate with keratin (acanthosis) and collagen (fibrosis)
Table 4.
Diagnostic accuracy of dermoscopy and histopathological changes in lupus vulgaris
| Dermoscopy | Histopathology | Sensitivity % | Specificity % | Positive predictive value (%) | Negative predictive value (%) | Diagnostic accuracy % |
|---|---|---|---|---|---|---|
| Yellowish white globules | Granuloma | 100 | 0.0 | 94.74 | - | 94.74 |
| Pinkish red background | Dilated vessels | 100 | 0.0 | 84.21 | - | 84.21 |
| Linear vessels | 100 | 0.0 | 84.21 | - | 84.21 | |
| Dotted vessels | 100 | 0.0 | 84.21 | - | 84.21 | |
| Red globules | 100 | 0.0 | 84.21 | - | 84.21 | |
| Ulceration | Erosions in the epidermis and dermis | 81.82 | 87.50 | 90 | 77.78 | 84.21 |
| White structureless area* | Dermal fibrosis | 100 | 50 | 81.25 | 100 | 84.21 |
| White shiny streaks | Orientation of collagen in dermis | 100 | 0.0 | 31.58 | - | 31.58 |
| Follicular plugs | Keratotic material in follicular infundibulum | 100 | 0.0 | 15.79 | - | 15.79 |
| Patulous follicles | Dilatation of infundibulum | 100 | 0.00 | 21.05 | - | 21.05 |
| Scaling | Hyperkeratosis | 100 | 0.0 | 68.42 | - | 68.42 |
| Bluish hue | Orthokeratosis | - | 89.47 | 0.0 | 100 | 89.47 |
| White structureless area* | Acanthosis | 50% | 50% | 52.63% | 47.37% | 50% |
*White structureless area correlate with keratin (acanthosis) and collagen (fibrosis)
Discussion
Lupus vulgaris is the most common paucibacillary form of cutaneous tuberculosis (TB). It results from the dissemination of mycobacteria from an underlying focus present elsewhere in the body mainly through direct, hematogenous and lymphatic routes. It can also occur by activation of latent cutaneous focus. Initially, lesions occur as reddish or brownish red macules or papules, with or without verrucosity that typically exhibit ‘apple jelly’ nodules on diascopy. Clinical variants of LV include papular, nodular, plaque, ulcerative, vegetative, hypertrophic, atrophic, tumour like and mutilating types.[1] Dermoscopy assists in the distinction of similar dermatoses by demonstrating characteristic patterns. Its role in the diagnosis in many conditions such as melanocytic nevi and melanoma, basal cell carcinoma and seborrheic keratosis is well established. It is also gaining popularity for its usefulness in inflammatory, infective and parasitic dermatoses.[6,7]
Generally, dermoscopy in granulomatous disease demonstrates yellow globules and telangiectasia. Well-focused telangiectasia on the yellowish background has been described as typical of LV and also correlate with the clinically appreciated “apple jelly sign”.[4] In addition to classical dermoscopic patterns, other findings in LV include erythema, whitish structureless areas, follicular plugs, dilated follicles, and white or yellow scales.[3] Similar findings were noted in this study as well. Nevertheless, orange-yellow structures that correlate with granuloma were seen as yellowish-white globules in the present study. This is possibly due to difference in colour contrast and presence of acanthosis as well.
Furthermore, white shiny streaks, four-dot clods (white rosettes), red globules and ulcerations were the new observations made in this study. White shiny streaks are white short linear structures that run obliquely and correlate with collagen in the dermis. They are described in histoid and other types of leprosy but not in other granulomas.[8,9] White rosettes are special structures that appear as four shiny globular structures coming to a central point [Figure 4b]. They correlate with infundibular hyperkeratosis and are attributable to the optical phenomenon by the polarized light.[10] This is related to follicular abnormalities that ensue in LV as described in earlier studies and are largely seen in facial lesions. It is noteworthy that both these structures are visible only with polarized lights and they are not mentioned in previous reports of dermoscopy in LV. However, this is a preliminary observation that requires further studies to affirm these findings.
All granulomatous conditions show yellowish areas and telangiectasia irrespective of etiology and hence recognition of individual granulomatous condition is a difficult task. Despite this factor, discrimination can be made by the presence of some additional features. Leishmaniasis demonstrates white star burst pattern, hair-pin or corkscrew vessels, and milia-like cysts,[11] whereas sarcoidosis shows scar-like depigmentation and translucent orange globules.[12] Granuloma annulare illustrates pinkish-white and yellow background and arborizing vessels. Hair-pin-like vasculature is viewed in necrobiosis lipoidica.[13] In this study, the most common dermoscopic findings in all the patients were pinkish-red background representing inflammation, superficial scaling representing hyperkeratosis and yellowish-white globules representing granuloma.
Dermoscopy also showed reddish globules, dotted and linear vessels, haemorrhage, whitish structureless areas and bluish hue in variable frequency. Importantly, bluish hue which was noted in two patients looks like a veil that covers some part of the lesion in dermoscopy and is a recognised entity in tumorous conditions. Blue areas correspond to a large amount of melanin in dermis and acanthosis whereas blue-white veil corroborates with compact orthokeratosis with large amount of melanin in dermis.[14] Surprisingly, none of these features were observed in this study except acanthosis. Hence, we propose that blue hue may be an artefact that warrants elaborate analysis for its presence in LV.
Discrepancy in histopathological and dermoscopic features was striking. Granuloma, acanthosis and hyperkeratosis were not present in all the patients. White structureless areas were seen in 19 patients, whereas fibrosis was present only in 16 patients. Reason for such discrepancy could be the difference in sites of dermoscopy and biopsy. Also the tissue processing and sectioning done during histopathological examination can add to this discrepancy, explaining the presence of hyperkeratosis on dermoscopy but not in histopathology. Variation in the depth of the biopsy can explain the dermoscopic and histopathological discrepancy relating to fibrosis. Thus a ‘dermoscopy-guided biopsy’ can be useful in alleviating such issues.
Conclusion
Dermoscopy is practical and rapid adjunctive method for accurate diagnosis. It demonstrated characteristic patterns in LV that included a few new observations such as white shiny streaks and white rosettes. Authors perceived a negligible variation of pattern in darker skin types as compared to fairer skin type. Inconsistency in dermoscopic-histopathology correlation demands dermoscopy guided biopsy for the appropriate yield of histopathological changes. Thus, dermoscopy, although not a replacement for histopathology, is a non-invasive procedure that can be used as diagnostic tool or at least as an assertion to clinical diagnosis in many infective dermatoses as well.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pai VV, Naveen KN, Athanikar SB, Dinesh US, Divyashree A, Gupta G. A clinico-histological study of Lupus vulgaris: A 3 year experience at a tertiary care centre. Indian Dermatol Online J. 2014;5:461–5. doi: 10.4103/2229-5178.142497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kittler H, Pehamberger H, Wolff K, Binder M. Diagnostic accuracy of dermoscopy. Lancet Oncol. 2002;3:159–65. doi: 10.1016/s1470-2045(02)00679-4. [DOI] [PubMed] [Google Scholar]
- 3.Errichetti E, Stinco G. Dermoscopy in general dermatology: A practical overview. Dermatol Ther (Heidelb) 2016;6:471–507. doi: 10.1007/s13555-016-0141-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brasiello M, Zalaudek I, Ferrara G, Gourhant JY, Capoluongo P, Roma P, et al. Lupus vulgaris: A new look at an old symptom-The lupoma observed with dermoscopy. Dermatology. 2009;218:172–4. doi: 10.1159/000182255. [DOI] [PubMed] [Google Scholar]
- 5.Kreusch J. How to perform dermoscopy of non-pigmented skin lesions. In: Zalaudek I, Argenziano G, Giacomel J, editors. Dermatoscopy of Non-Pigmented Skin Tumors. London: CRC Press; 2016. pp. 17–8. [Google Scholar]
- 6.Errichetti E. Dermoscopy of inflammatory dermatoses (inflammoscopy): An up-to-date overview. Dermatol Pract Concept. 2019;9:169–80. doi: 10.5826/dpc.0903a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ankad BS, Beergouder SL. Dermoscopy of inflammatory conditions: The journey so far. EMJ Dermatol. 2017;5:98–105. [Google Scholar]
- 8.Acharya P, Mathur MC. Clinicodermoscopic study of histoid leprosy: A case series. Int J Dermatol. 2020;59:365–8. doi: 10.1111/ijd.14731. [DOI] [PubMed] [Google Scholar]
- 9.Vinay K, Kamat D, Chatterjee D, Narang T, Dogra S. Dermatoscopy in leprosy and its correlation with clinical spectrum and histopathology: A prospective observational study. J Eur Acad Dermatol Venereol. 2019;33:1947–51. doi: 10.1111/jdv.15635. [DOI] [PubMed] [Google Scholar]
- 10.Haspeslagh M, Noe M, De Wispelaere I, Degryse N, Vossaert K, Lanssens S, et al. Rosettes and other white shiny structures in polarized dermoscopy: Histological correlate and optical explanation. J Eur Acad Dermatol Venereol. 2016;30:311–3. doi: 10.1111/jdv.13080. [DOI] [PubMed] [Google Scholar]
- 11.Llambrich A, Zaballos P, Terrasa F, Torne I, Puig S, Malvehy J. Dermoscopy of cutaneous leishmaniasis. Br J Dermatol. 2009;160:756–61. doi: 10.1111/j.1365-2133.2008.08986.x. [DOI] [PubMed] [Google Scholar]
- 12.Chauhan P, Meena D, Hazarika N. Dermoscopy of Sarcoidosis: A useful clue to diagnosis. Indian Dermatol Online J. 2018;9:80–1. doi: 10.4103/idoj.IDOJ_84_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lallas A, Zaballos P, Zalaudek I, Apalla Z, Gourhant JY, Longo C, et al. Dermoscopic pattern of granuloma annulare and necrobiosis lipoidica. Clin Exp Dermatol. 2013;38:425–7. doi: 10.1111/ced.12126. [DOI] [PubMed] [Google Scholar]
- 14.Massi D, De Giorgi V, Carli P, Santucci M. Diagnostic significance of the blue hue in dermoscopy of melanocytic lesions: A dermoscopic-pathologic study. Am J Dermatopathol. 2001;23:463–9. doi: 10.1097/00000372-200110000-00013. [DOI] [PubMed] [Google Scholar]


