Abstract
Purpose:
Alemtuzumab is a humanized monoclonal antibody against CD52 which is predominantly present on T- and B-lymphocytes. Alemtuzumab has been used as part of conditioning regimens for prophylaxis against rejection and GVHD. While the mechanism of action is well-understood, the pharmacokinetics of this drug in children needed to be studied in more detail especially in the setting of ex vivo T-cell depleted hematopoietic cell transplantation (HCT).
Methods:
Serum alemtuzumab levels were measured at various time points in 13 patients who underwent haploidentical HCT utilizing ex vivo donor T-cell depletion. Alemtuzumab was administered subcutaneously at a cumulative dose of 45 mg/m2 from days −13 to −11. A one-compartmental model was used to fit the data using non-linear mixed effects modeling.
Results:
We determined the median half-life to be 11 days. Alemtuzumab clearance increased with increasing baseline lymphocyte count (p = 0.008). Additionally, clearance increased with weight and age (p ≤ 0.035). AUC of alemtuzumab did not have any significant relationship with type of leukemia, overall survival, engraftment, immune reconstitution, mixed chimerism or GVHD, although the number of subjects in this pilot study was limited.
Conclusion:
Absolute lymphocyte count and body weight affect alemtuzumab clearance. We also demonstrate feasibility of body surface area-based dosing of alemtuzumab in pediatric HCT patients. Further studies are needed to evaluate the role of monitoring alemtuzumab serum concentrations to balance the prevention of graft rejection and GVHD with the promotion of rapid donor immune reconstitution.
Keywords: Alemtuzumab, pharmacokinetics, Haploidentical bone marrow transplantation, T-cell depleted transplantation, pediatric bone marrow transplantation, campath, bone marrow, peripheral blood stem cell
Introduction
Outcomes for children with acute leukemia have improved in recent decades, aided by advances in understanding the biology of leukemia, improved risk-stratification, use of multiagent chemotherapy and superior supportive care [1,2]. Despite these advances, many patients continue to have high rates of relapse and correspondingly poor survival. These patients are ideal candidates for allogeneic hematopoietic cell transplantation (HCT). While HLA-matched donor transplantation has been a well-established and well-studied standard of care, many patients do not have an appropriate sibling donor and often also lack a matched unrelated donor. Haploidentical donor HCT is a viable option for these patients [3]. However, the presence of HLA-mismatch can be associated with increased risk of donor graft rejection, graft versus host disease (GVHD), infections due to delayed immune reconstitution and regimen-related toxicity [3]. Various conditioning regimens and graft manipulation techniques are being utilized to improve outcomes after haploidentical HCT [4,5].
Alemtuzumab is a humanized monoclonal antibody targeted against human CD52, which is predominantly expressed on T- and B- cells with negligible expression in hematopoietic stem and progenitor cells [6]. Alemtuzumab has been used as part of conditioning regimen for HCT to prevent GVHD and graft rejection by depletion of T-lymphocytes in vivo [7]. Increased exposure to alemtuzumab can result in prolonged T-cell suppression, reduced graft-versus-leukemia (GVL) effect, delayed immune reconstitution and increased risk of infections such as CMV [8], whereas decreased exposure to alemtuzumab is associated with increased risk of acute GVHD and graft rejection. Considering this, dosing alemtuzumab appropriately is of critical importance in achieving a balance between graft rejection, GVHD, and immune reconstitution.
Previous pharmacokinetic studies of alemtuzumab in adult CLL patients receiving fixed dose alemtuzumab showed variability between patients believed to be related to tumor burden and baseline absolute lymphocyte count (ALC) [9]. Studies in children undergoing HCT did not show any effect of ALC on clearance [10]. It is suggested that higher dosing used in HCT rapidly saturates all the available CD52 sites resulting in ALC not having a substantial effect on clearance. Additionally, the study population was very heterogenous in terms of their diagnosis and type of HCT employed. In this work we describe the pharmacokinetics of body surface area (BSA)-dosed alemtuzumab in children with leukemia undergoing ex vivo T-cell depleted haploidentical hematopoietic transplantation in a single-center study.
Patients and Methods
Study Design
Patients, younger than 21 years of age, with hematological malignancy and undergoing haploidentical HCT using a reduced intensity conditioning (RIC) regimen with CD3-depleted hematopoietic progenitor cell grafts between March 2011 and November 2012 were included in this study (NCT00566696). Patients were excluded if they had received a previous HCT. Patients received alemtuzumab as part of the conditioning regimen from days −14 to −11 using a body-surface area (BSA)-based dosing. Patients received a test dose of 2 mg on day −14 followed by escalating doses of 10 mg/m2, 15 mg/m2 and 20 mg/m2 on days −13, −12 and −11 respectively. A total dosage of 45 mg/m2 was administered and eight post-regimen serum pharmacokinetic samples were obtained over the following 16 weeks as described in Figure 1. Recipients received haploidentical donor grafts that underwent ex vivo T-cell depletion via immunomagnetic depletion of CD3+ cells using CliniMACS (Miltenyi Biotec, Germany) following conditioning with fludarabine (40 mg/m2/day; day −9 to −5), thiotepa (10 mg/kg divided into two doses; day −4), melphalan (60 mg/m2/day; day −3 and −2) and rituximab (375 mg/m2; day −1) [11]. Mycophenolate mofetil (MMF) was given for 60 days for post-HCT GVHD prophylaxis. The study was approved by IRB of St. Jude Children’s Research Hospital in accordance with federal regulations and the principles of the Helsinki Declaration. Patients were enrolled after informed consent was given by parent and/or patient.
Figure 1.
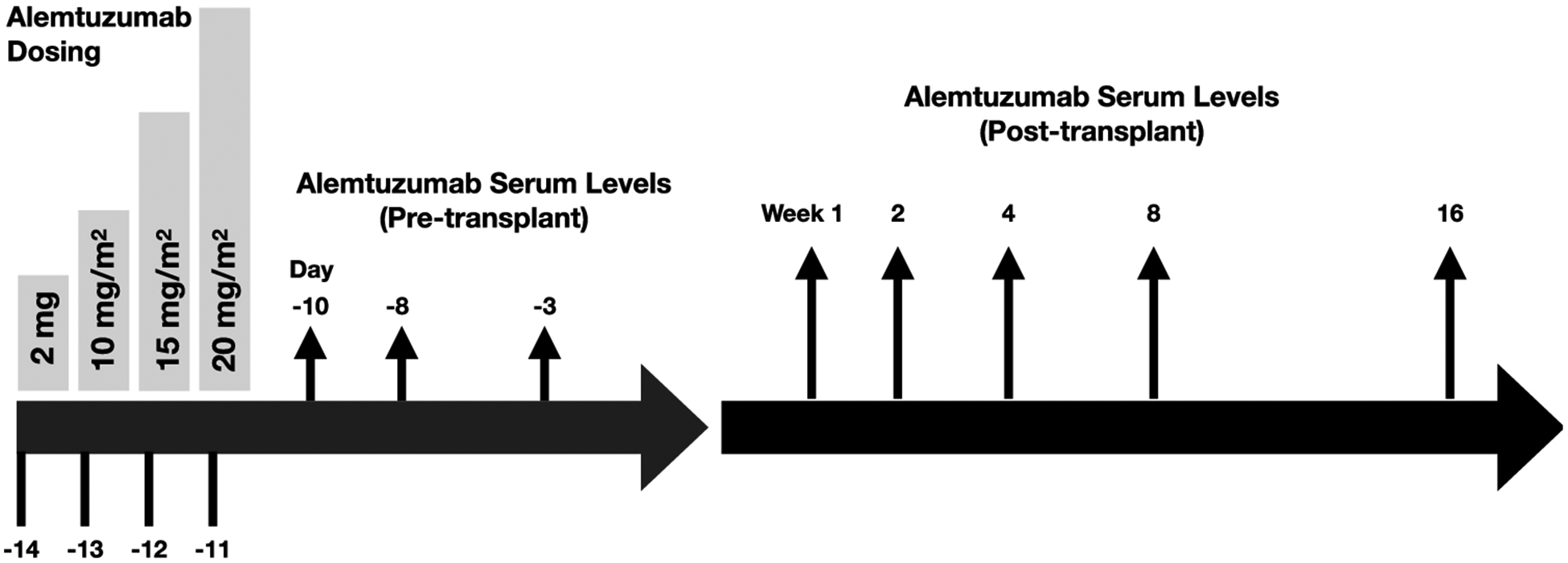
Scheme of alemtuzumab administration as part of conditioning and time points at which serum concentrations were checked to establish pharmacokinetic properties.
Alemtuzumab administration and measurement:
All doses of alemtuzumab were administered subcutaneously except for 5 patients who received intravenous dosing for their third and fourth doses. Serum concentrations were measured by enzyme linked-immunosorbent assay at the following timepoints: day −10, day −8, day −3 before transplant, and then at weeks 1, 2, 4, 8 and 16 post-HCT. The lower limit of detection of alemtuzumab in this assay was 141 ng/mL.
Pharmacokinetic Analysis:
The pharmacokinetics were estimated with non-linear mixed effects modeling (Monolix version 5.1.0; Lixoft, Antony, France) using the Stochastic Approximation Expectation-Maximization (SAEM) method. A one-compartment PK model with first-order subcutaneous absorption was used to describe the data. The PK parameters estimated included clearance (CL; mL/m2/day), volume of distribution (V; mL/m2), the first-order absorption rate constant (ka; 1/day), and bioavailability (f). The inter-individual variability of the parameters was assumed to be log-normally distributed and a proportional residual error model was used with assumed normal distribution of the residuals. Concentrations below the lower limit of quantification (141 ng/mL) were treated as censored and the M3 method of handling these values was used as implemented in Monolix [12]. In addition, the individual posthoc parameter estimates (both the conditional mode and random samples from the conditional distribution (n=10) per individual) were determined and used to estimate the area under the concentration-time curve (AUC; μg*day/mL) and half-life (t1/2; days). The relationships between PK parameters and covariates were described using the following model: θ=θBase*exp(β*covariate).
Statistical analysis:
A covariate in the pharmacokinetic model was considered significant in the univariate analysis, if the addition of the covariate to the model reduced the objective function value at least 3.84 units (p < 0.05, based on the χ2 test for the difference in the −2 log-likelihood between two hierarchical models that differ by 1 degree of freedom). Only univariate analysis was considered due to the small sample size of the population. Continuous variables were expressed as median (range) and categorical variables were expressed as absolute units (percentage). Overall survival was determined by Kaplan-Meier method implemented in R (version 3.5).
Results
Patient characteristics
Thirteen patients with acute leukemia receiving their first HCT were enrolled. All patients received CD3-depleted grafts from haploidentical donors. Table 1 summarizes the characteristics of the 13 patients. All 13 patients received alemtuzumab test dose on day −14 which they tolerated well and proceeded to receive rest of dosing as planned. Graft source was GCSF-mobilized peripheral blood in all cases with a median (range) CD34+ dose of 10.3 × 106 cells/kg (5.6 – 48), and median (range) CD3+ dose of 0.024 × 106 cell/kg (0.01 – 0.085).
Table 1.
Patient characteristics.
| Total number of patients | 13 |
| Median age, years (range) | |
| Median weight, kg (range) | |
| Median BSA, m2 (range) | |
| Sex | |
| Female | |
| Male | |
| Diagnoses | |
| ALL | |
| AML | |
| CML | |
| Therapy-related MDS | |
| Median CD34+ cell dose, 10e6 cells/kg (range) | |
| Median neutrophil engraftment, days (range) | |
| Median platelet engraftment, days (range) | |
| Primary graft failure | |
| Secondary graft failure | |
| Relapse | |
| 1-year OS | |
| aGVHD | |
| Grade I | |
| Grade II | |
| Grade III | |
| Grade IV | |
| cGVHD | |
| DLI administered | |
| Stem cell boost | |
| Median follow-up, years (range) |
Pharmacokinetics
The population pharmacokinetics of alemtuzumab are summarized in Table S1 and quality of the model fit is shown in Figure 2 and Figure S1. BSA-normalized dosing significantly improved the model fit (p=8.7 × 10−7) and explained 15 and 64% of the IIV on CL and V respectively. Weight based dosing was also evaluated and was not significantly different from BSA based dosing. Therefore, all the remaining analysis used BSA normalized pharmacokinetics. The median (range) posthoc estimated clearance and AUC were 255 (211 – 600) mL/m2/day and 117.1 (28.1 – 165.4) ug*day/mL, respectively. The median estimated peritransplant serum concentration on day −3 was 4.0 (10th–90th percentile: 2.1–7.1) μg/mL. Ten of thirteen (77%) patients had detectable concentrations as late as week 4 post-HCT (6 weeks after alemtuzumab infusion) and the median (range) half-life was 11 (4.3 – 12.9) days (Figure 2). Clearance increased with age, weight, and serum creatinine (p ≤ 0.035) (Table S1, Figure 3 a–c). Conversely AUC decreased with age, weight, and serum creatinine (p < 0.05). Since alemtuzumab is not renally excreted, serum creatinine levels should not have any direct effect on the pharmacokinetics of alemtuzumab. This was confirmed by the lack of an association between alemtuzumab clearance or AUC and glomerular filtration rate (GFR) as measured by technetium-99m DTPA radioisotope or 24-hour urine collection. Although we did not notice a statistically significant relationship between AUC and absolute lymphocyte count (ALC), clearance increased with increase in ALC (p = 0.008) (Table S1, Figure 3d). Additionally, there was no statistically significant association between AUC and type of leukemia, immune reconstitution, survival, relapse, graft failure, incidence of mixed chimerism, acute or chronic GVHD.
Figure 2.
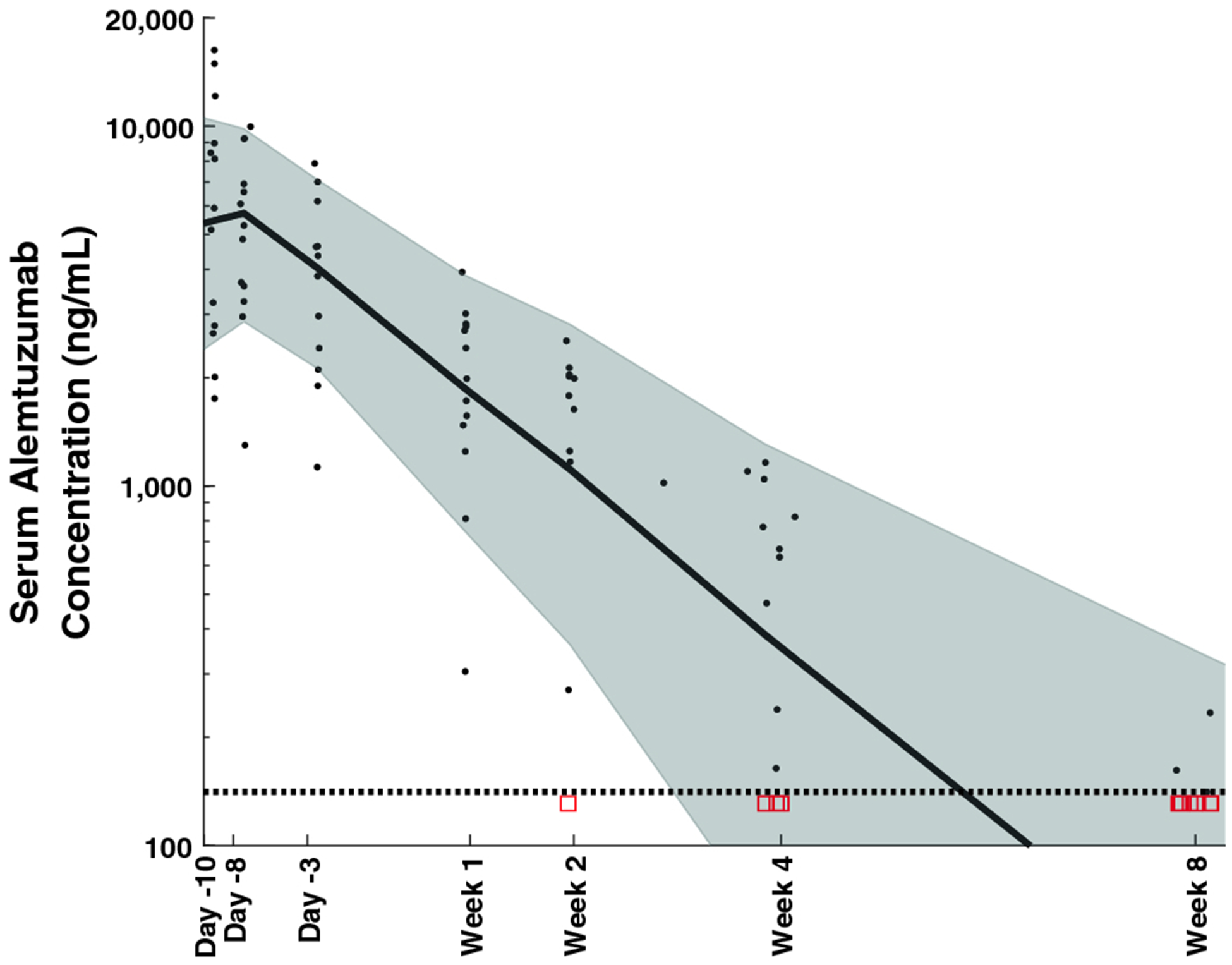
Alemtuzumab concentration versus time and Visual Predictive Check. The black dots represent the measured concentrations and the red squares represent censored data (plotted at the LLOQ). The solid black curve is the population predicted median curve and the grey shaded region represents the population predicted 10th to 90th percentile. The horizontal dotted line represents the lower limit of quantification of the assay (141 ng/mL).
Figure 3.
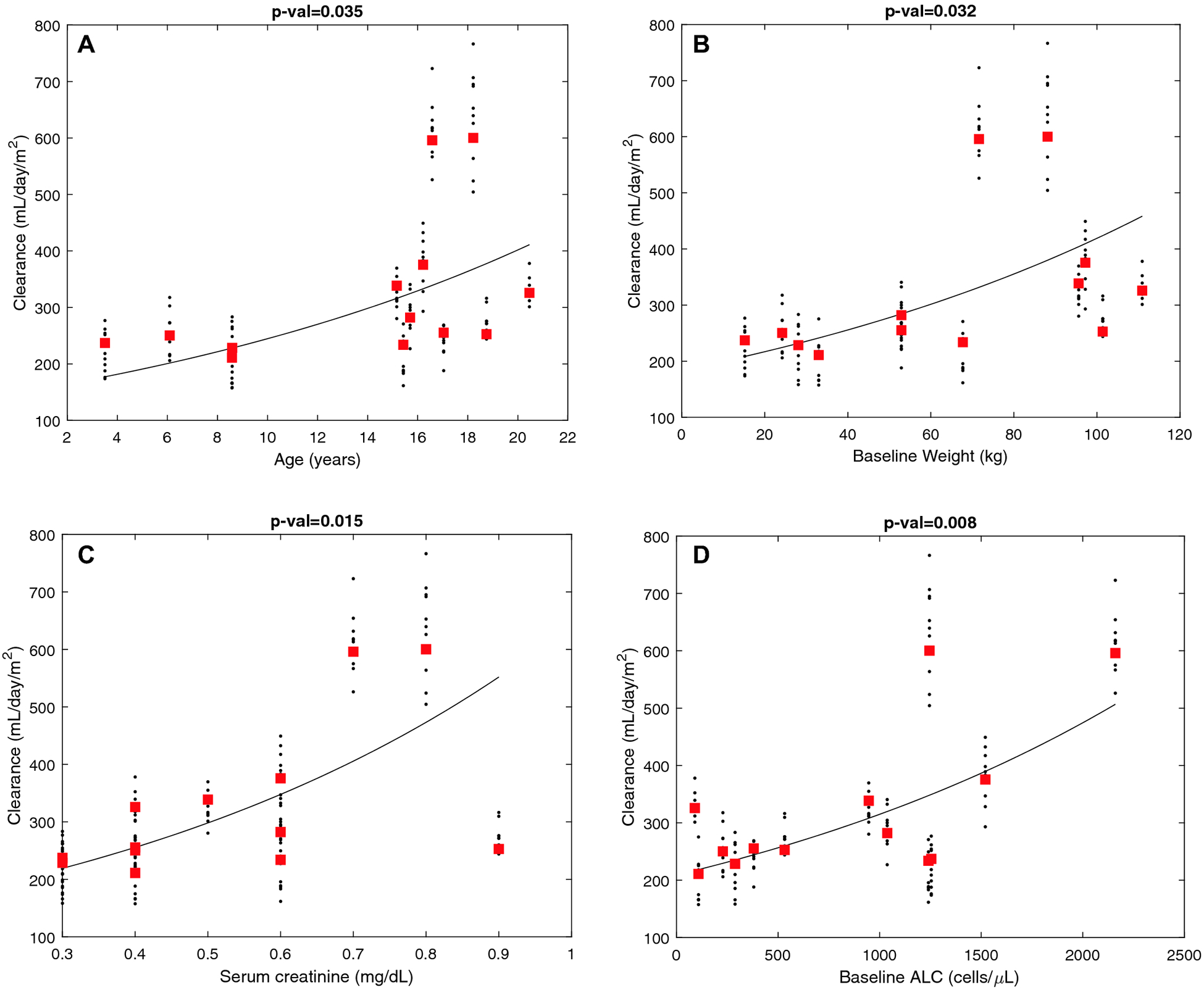
Covariate relationship between alemtuzumab clearance and a) age, b) weight, c) serum creatinine, and d) absolute lymphocyte count. The red squares are the conditional mode and the black dots are random samples (n=10 per individual) from the conditional distribution.The curve represents the covariate model fit to the data.
Engraftment, GVHD, infections and outcomes
Median time for neutrophil engraftment was 11 days (range 8–12) and platelet engraftment was 15 days (range 13–19). Median time for absolute lymphocyte count to reach more than 1000/mm3 was 96 days (range 70–763). We did not find any association between time for ALC recovery and AUC or baseline ALC. One patient had primary graft failure, and another had secondary graft failure. Acute GVHD was observed in 6, out of which 4 had Grade III/IV acute GVHD. Two patients had chronic GVHD, with one each of limited and extensive chronic GVHD. All 7 patients with acute and/or chronic GVHD had received prior donor lymphocyte infusion (DLI). Median (range) follow-up period was 4.9 years (0.1 – 8.9). Seven patients were alive 1 year after transplant. Our cohort included three patients who relapsed in the first year. Overall survival (OS) for 100 days was 84.6% (95% CI, 51.2–95.9) and 1-year OS was 53.8%, (95% CI, 24.8–76) (Figure 4). Twelve out of thirteen patients received DLI for various reasons with the most common indication being mixed chimerism (n=7 patients). DLIs were administered in 2–4 week intervals, with a dose range from 2.5–10 × 104 CD3+ cells/kg. The median duration from the last dose of alemtuzumab to the first DLI administration was 49.5 days (range 31 to 87) raising the possibility that CD52-expressing DLI could affect alemtuzumab pharmacokinetics. However, we did not note any significant relationship between time of DLI infusion and AUC (p=0.47) or CL (p=0.28).
Figure 4.
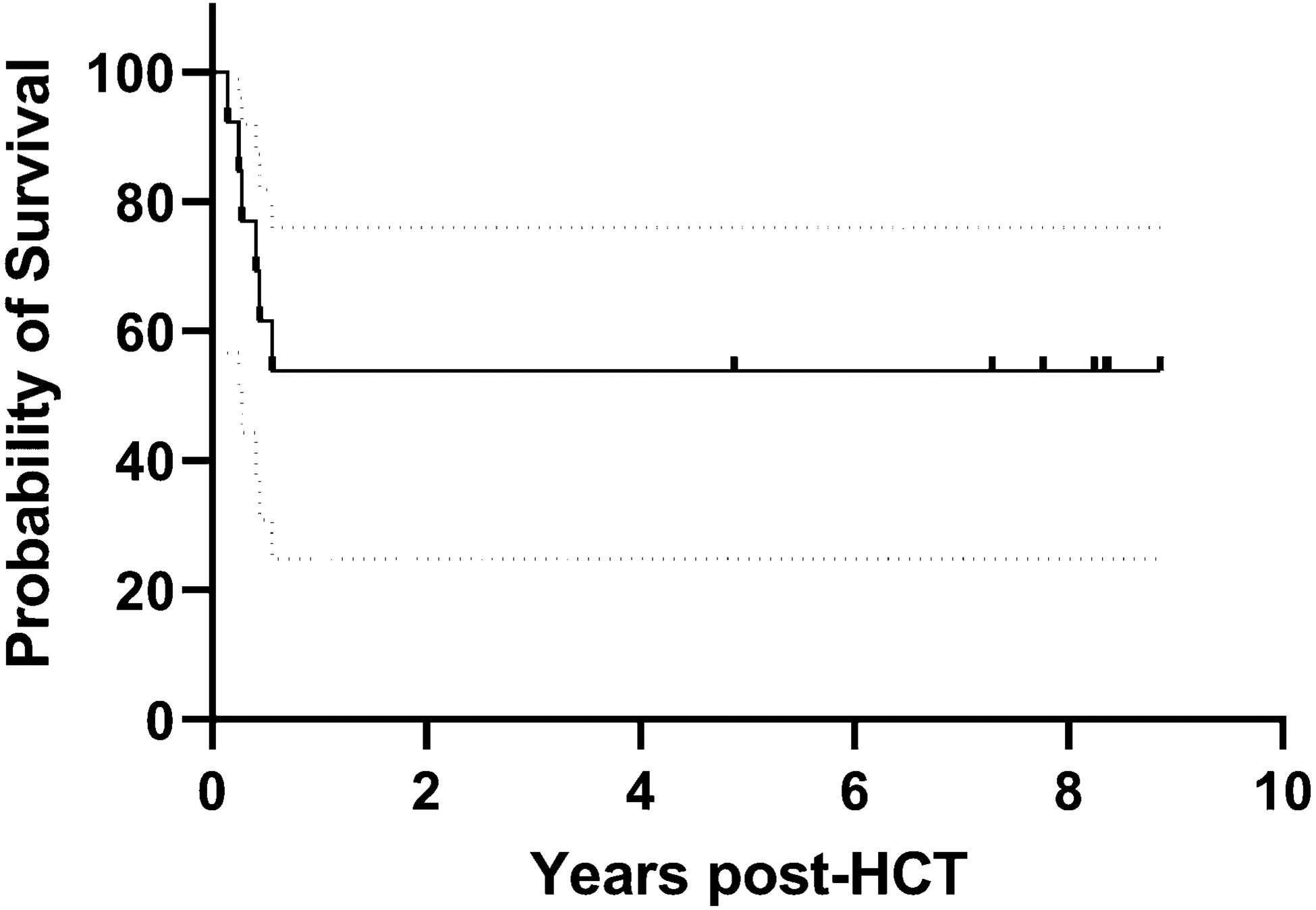
Overall survival curve for our patient cohort with dotted lines representing boundaries of 95% confidence interval (CI).
Discussion
Our study demonstrates that dosing alemtuzumab by body-surface area is a feasible approach resulting in consistent pharmacokinetics (Figure 2). We report a statistically significant relationship between alemtuzumab clearance and age, weight, serum creatinine and ALC. We found no significant effect of sex or GFR on clearance. Although our pilot study is limited by small sample size, to our knowledge this is the first pharmacokinetic study of alemtuzumab in pediatric patients undergoing ex vivo T-cell depleted haploidentical transplantation. In this study, we primarily focused on the terminal pharmacokinetic parameters as we hypothesized that the serum levels after donor cell infusion had a higher clinical impact on HCT outcomes than early serum levels. The clinical importance of post-donor infusion pharmacokinetics has previously been noted with rabbit-derived antithymocyte globulin (rATG) [13].
Monoclonal antibodies, such as alemtuzumab, are cleared by one of two mechanisms: a slower non-specific proteolytic pathway and a more-rapid target antigen-mediated clearance pathway. As suggested by previous studies demonstrating a significant effect of lymphocyte count on the pharmacokinetics of alemtuzumab [9], target antigen-mediated clearance likely plays an important role in alemtuzumab clearance. Since the target antigen for alemtuzumab is present on white blood cells and lymphoid tissue, we hypothesized that a body-surface area would be more representative of lymphoid tissue content than body weight in pediatric patients. A previous study that used BSA-based dosing strategy (cumulative dose of 52 mg/m2) for alemtuzumab in patients undergoing matched unrelated donor HCT for non-malignant genetic diseases demonstrated that elevated clearance (i.e., lower exposure) was associated with graft rejection [14]. The importance of appropriate dosing was further highlighted by Marsh et al. who noted lower alemtuzumab concentrations during peritransplant period is associated with higher incidence of acute GVHD, mixed chimerism and immune reconstitution [15].
Considering that we were depleting T-cells ev vivo we rationalized that using a lower alemtuzumab dose (cumulative dose of 45 mg/m2 plus a 2 mg test dose, as opposed to 52 mg/m2) [14,16] using an intermediate schedule (day −14 to −10), as opposed to a proximal schedule, would be appropriate. We hypothesized that this would result in minimal effect on donor cells. However, our cohort had estimated lympholytic concentrations (> 0.1 μg/mL) as late as 6 weeks after infusion and a conspicuously high frequency of mixed chimerism necessitating DLI. Together, this suggests we likely had a higher than required concentrations of alemtuzumab which, presumably, affected engraftment by killing alloreactive donor lymphocytes. However, we did not notice an association between alemtuzumab AUC and immune reconstitution. Future studies in T-cell depleted HCTs should consider reducing the cumulative dose of alemtuzumab but keeping in mind that WBC count might have a larger impact on the pharmacokinetics as the dose is reduced [9,10].
The median half-life of alemtuzumab in our study is estimated to be 11 days. The longer half-life estimated in this study compared to previously published values in CLL patients is likely because of the lower starting white blood cell count in our patients, the use of an ex vivo T-cell depleted donor graft, and the multiple dosing scheme employed [9]. Additionally, by measuring serum concentrations over days to weeks, instead of hours after infusion, (Figure 1) we are capturing the terminal half-life - a more clinically relevant phase. The half-life determined in our study is more closer to the terminal half-life of 2–3 weeks determined in adult patients undergoing HCT [17].
Previous pharmacokinetics study on alemtuzumab have mostly been reported using adult data where patients received a wide range of dosing. Multiple dosing regimens have been used: 20 mg/day × 5 days, 0.2 mg/kg/day × 5 days, 0.25 mg/kg × 2 days [7,18–20]. One of the largest studies in pediatric population used data from 206 patients who received alemtuzumab in two different centers [10]. Most of these patients received a cumulative dose of 1 mg/kg given as 0.2 mg/kg/day × 5 days with some patients receiving a cumulative dose of 0.5 mg/kg. The study used a two-compartment model and suggested body weight-based doses result in highly variable exposure. However, as demonstrated in our results, BSA-normalization resulted in a better model fit compared to weight-normalization, although the results were similar. This highlights the feasibility of BSA-based dosing for alemtuzumab consistent with general chemotherapy dosing in pediatric cancer patients. Whether and how exposure affects transplant outcomes and survival needs to be investigated further, especially in haploidentical HCTs as the donor graft is invariably manipulated either ex vivo or in vivo. There is likely to be an important role for therapeutic drug monitoring (TDM) especially in patients receiving both T-cell replete as well as T-cell depleted grafts. TDM of rATG has been shown to be a feasible approach to balance graft failure and immune reconstitution [21,22].
To summarize, BSA-based dosing of intermediate-scheduled alemtuzumab is a feasible approach for pediatric patients undergoing ex vivo T-cell depleted haploidentical hematopoietic cell transplantation and results in consistent serum concentration. Further studies are needed to determine if AUC and clearance affect transplant outcomes and if TDM of alemtuzumab can be utilized to achieve individualized drug dosing.
Supplementary Material
Supplemental Figure S1. Goodness-of-Fit plots. Black dots: measured concentrations/residuals; Red dots: simulated concentrations below the LLOQ (141 ng/mL); Panel A: individual predicted vs actual concentration; Panel B: population predicted vs actual concentration; Panel C: individual weighted residuals vs time; Panel D: population weighted residual vs time.
Acknowledgement:
This work is supported, in part, by the National Cancer Institute Cancer Center Support (CORE) grant P30 CA021765 and the American Lebanese Syrian Associated Charities (ALSAC).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest: B.M.T. received travel support for EBMT 2018 Annual Meeting from Miltenyi Biotec Inc to present published data. The remaining authors declare no competing financial interests.
Ethics Approval: This work was approved by IRB and Ethics Committee of our institution.
Availability of data and transplarency: Data is available at request.
Code availability: Not applicable.
References:
- 1.Alexander TB, Wang L, Inaba H, Triplett BM, Pounds S, Ribeiro RC, Pui CH, Rubnitz JE (2017) Decreased relapsed rate and treatment-related mortality contribute to improved outcomes for pediatric acute myeloid leukemia in successive clinical trials. Cancer 123 (19):3791–3798. doi: 10.1002/cncr.30791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campana D, Pui C-H (2017) Minimal residual disease-guided therapy in childhood acute lymphoblastic leukemia. Blood 129 (14):1913–1918. doi: 10.1182/blood-2016-12-725804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu JH, Kanakry CG, Luznik L (2018) Have haploidentical transplants replaced umbilical cord transplants for acute leukemias? Current opinion in hematology 25 (2):103–111 [DOI] [PubMed] [Google Scholar]
- 4.Vadakekolathu J, Rutella S (2017) T-Cell Manipulation Strategies to Prevent Graft-Versus-Host Disease in Haploidentical Stem Cell Transplantation. Biomedicines 5 (2). doi: 10.3390/biomedicines5020033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martelli MF, Di Ianni M, Ruggeri L, Pierini A, Falzetti F, Carotti A, Terenzi A, Reisner Y, Aversa F, Falini B, Velardi A (2014) “Designed” grafts for HLA-haploidentical stem cell transplantation. Blood 123 (7):967–973. doi: 10.1182/blood-2013-10-531764 [DOI] [PubMed] [Google Scholar]
- 6.Gribben JG, Hallek M (2009) Rediscovering alemtuzumab: current and emerging therapeutic roles. Br J Haematol 144 (6):818–831. doi: 10.1111/j.1365-2141.2008.07557.x [DOI] [PubMed] [Google Scholar]
- 7.Kottaridis PD, Milligan DW, Chopra R, Chakraverty RK, Chakrabarti S, Robinson S, Peggs K, Verfuerth S, Pettengell R, Marsh JC, Schey S, Mahendra P, Morgan GJ, Hale G, Waldmann H, de Elvira MC, Williams CD, Devereux S, Linch DC, Goldstone AH, Mackinnon S (2000) In vivo CAMPATH-1H prevents graft-versus-host disease following nonmyeloablative stem cell transplantation. Blood 96 (7):2419–2425 [PubMed] [Google Scholar]
- 8.Marek A, Stern M, Chalandon Y, Ansari M, Ozsahin H, Gungor T, Gerber B, Kuhne T, Passweg JR, Gratwohl A, Tichelli A, Seger R, Schanz U, Halter J, Stussi G, Swiss Blood Stem Cell T (2014) The impact of T-cell depletion techniques on the outcome after haploidentical hematopoietic SCT. Bone Marrow Transplant 49 (1):55–61. doi: 10.1038/bmt.2013.132 [DOI] [PubMed] [Google Scholar]
- 9.Mould DR, Baumann A, Kuhlmann J, Keating MJ, Weitman S, Hillmen P, Brettman LR, Reif S, Bonate PL (2007) Population pharmacokinetics-pharmacodynamics of alemtuzumab (Campath) in patients with chronic lymphocytic leukaemia and its link to treatment response. Br J Clin Pharmacol 64 (3):278–291. doi: 10.1111/j.1365-2125.2007.02914.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Admiraal R, Jol-van der Zijde CM, Furtado Silva JM, Knibbe CAJ, Lankester AC, Boelens JJ, Hale G, Etuk A, Wilson M, Adams S, Veys P, van Kesteren C, Bredius RGM (2019) Population Pharmacokinetics of Alemtuzumab (Campath) in Pediatric Hematopoietic Cell Transplantation: Towards Individualized Dosing to Improve Outcome. Clin Pharmacokinet 58 (12):1609–1620. doi: 10.1007/s40262-019-00782-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aversa F, Pierini A, Ruggeri L, Martelli MF, Velardi A (2019) The Evolution of T Cell Depleted Haploidentical Transplantation. Front Immunol 10:2769. doi: 10.3389/fimmu.2019.02769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beal SL (2001) Ways to fit a PK model with some data below the quantification limit. Journal of pharmacokinetics and pharmacodynamics 28 (5):481–504 [DOI] [PubMed] [Google Scholar]
- 13.Admiraal R, Lindemans CA, van Kesteren C, Bierings MB, Versluijs AB, Nierkens S, Boelens JJ (2016) Excellent T-cell reconstitution and survival depend on low ATG exposure after pediatric cord blood transplantation. Blood 128 (23):2734–2741. doi: 10.1182/blood-2016-06-721936 [DOI] [PubMed] [Google Scholar]
- 14.Abdel-Azim H, Mahadeo KM, Zhao Q, Khazal S, Kohn DB, Crooks GM, Shah AJ, Kapoor N (2015) Unrelated donor hematopoietic stem cell transplantation for the treatment of non-malignant genetic diseases: An alemtuzumab based regimen is associated with cure of clinical disease; earlier clearance of alemtuzumab may be associated with graft rejection. Am J Hematol 90 (11):1021–1026. doi: 10.1002/ajh.24141 [DOI] [PubMed] [Google Scholar]
- 15.Marsh RA, Lane A, Mehta PA, Neumeier L, Jodele S, Davies SM, Filipovich AH (2016) Alemtuzumab levels impact acute GVHD, mixed chimerism, and lymphocyte recovery following alemtuzumab, fludarabine, and melphalan RIC HCT. Blood 127 (4):503–512. doi: 10.1182/blood-2015-07-659672 [DOI] [PubMed] [Google Scholar]
- 16.Mahadeo KM, Weinberg KI, Abdel-Azim H, Miklos DB, Killen R, Kohn D, Crooks GM, Shah AJ, Kharbanda S, Agarwal R, Kapoor N (2015) A reduced-toxicity regimen is associated with durable engraftment and clinical cure of nonmalignant genetic diseases among children undergoing blood and marrow transplantation with an HLA-matched related donor. Biol Blood Marrow Transplant 21 (3):440–444. doi: 10.1016/j.bbmt.2014.11.005 [DOI] [PubMed] [Google Scholar]
- 17.Rebello P, Cwynarski K, Varughese M, Eades A, Apperley JF, Hale G (2001) Pharmacokinetics of CAMPATH-1H in BMT patients. Cytotherapy 3 (4):261–267. doi: 10.1080/146532401317070899 [DOI] [PubMed] [Google Scholar]
- 18.Spyridonidis A, Liga M, Triantafyllou E, Themeli M, Marangos M, Karakantza M, Zoumbos N (2011) Pharmacokinetics and clinical activity of very low-dose alemtuzumab in transplantation for acute leukemia. Bone Marrow Transplant 46 (10):1363–1368. doi: 10.1038/bmt.2010.308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oshima K, Kanda Y, Nakahara F, Shoda E, Suzuki T, Imai Y, Watanabe T, Asai T, Izutsu K, Ogawa S, Motokura T, Chiba S, Kurokawa M (2006) Pharmacokinetics of alemtuzumab after haploidentical HLA-mismatched hematopoietic stem cell transplantation using in vivo alemtuzumab with or without CD52-positive malignancies. American journal of hematology 81 (11):875–879. doi: 10.1002/ajh.20694 [DOI] [PubMed] [Google Scholar]
- 20.Kako S, Gomyo A, Akahoshi Y, Harada N, Kameda K, Ugai T, Wada H, Ishihara Y, Kawamura K, Sakamoto K, Sato M, Terasako-Saito K, Kimura S-I, Kikuchi M, Nakasone H, Kanda J, Kanda Y (2019) Haploidentical transplantation using low-dose alemtuzumab: Comparison with haploidentical transplantation using low-dose thymoglobulin. European journal of haematology 102 (3):256–264. doi: 10.1111/ejh.13204 [DOI] [PubMed] [Google Scholar]
- 21.Admiraal R, van Kesteren C, Nierkens S, Boelens J-J, Lacna AM, Ebskamp-van Raaij L (2016) Individualized dosing and therapeutic drug monitoring for anti-thymocyte globulin to improve outcome following cord blood transplantation: proof of concept. Biology of Blood and Marrow Transplantation 22 (3):S116 [Google Scholar]
- 22.Lindemans CA, Admiraal R, Haar CG, van Raaij LEE, Lacna AM, Bierings M, Nierkens S, Boelens J-J (2017) Individualized Dosing and Therapeutic Drug Monitoring (TDM) of ATG is Feasible, Safe, Effective, and Associated with Excellent Immune Reconstitution. Biology of Blood and Marrow Transplantation 23 (3):S124–S125 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure S1. Goodness-of-Fit plots. Black dots: measured concentrations/residuals; Red dots: simulated concentrations below the LLOQ (141 ng/mL); Panel A: individual predicted vs actual concentration; Panel B: population predicted vs actual concentration; Panel C: individual weighted residuals vs time; Panel D: population weighted residual vs time.


