Abstract
Objective:
Depression and ADHD are prevalent and highly comorbid. ADHD symptoms are associated with specific dependent (i.e., self-generated) stressors in children, and there is a strong link between dependent stress and depression. Despite continued comorbidity of ADHD and depressive symptoms into adulthood, it is unknown whether stress generation mediates the relation between ADHD and subsequent depressive symptoms in emerging adulthood, a period of heightened stress.
Method:
We tested this mediation model in a semester-long longitudinal study of 224 college students (ages 18–23). We additionally tested whether this model differed between inattentive versus hyperactive/impulsive ADHD symptoms given evidence that they vary in their relations to stress and depression.
Results:
Dependent stress mediated the association between total ADHD symptoms at baseline and later depressive symptoms; these effects were equivalent for inattentive versus hyperactive/impulsive ADHD symptoms.
Conclusion:
These findings suggest stress generation as a mechanism for increased depression in individuals with ADHD symptoms.
Keywords: ADHD, dependent stress, stress generation, depression
Introduction
Depression is a prevalent, debilitating mood disorder with onset typically during adolescence and young adulthood (Mojtabai et al., 2016; Wesselhoft et al., 2013). College years are a high-risk period for depressive symptoms: 26% of college students report experiencing mild or greater depressive symptoms in the past two weeks (Whisman & Richardson, 2015), and 33% of college students report feeling “so depressed it was difficult to function” within the past year (ACHA, 2014). Depressive symptoms in adolescence and emerging adulthood predict many negative outcomes in adulthood, including symptom recurrence and decreased health status (Naicker et al., 2012; Fergusson et al., 2005; Pine et al., 1999), making it crucial to identify risk factors during this developmental period (Meinzer et al., 2016; Mojtabai et al., 2016). One such risk factor may be attention deficit hyperactivity disorder (ADHD) symptoms (Meinzer et al., 2012). ADHD onsets earlier than depression, typically before the age of 12, and has two main symptom dimensions - inattention and/or hyperactivity/impulsivity. Importantly, the rate of major depressive disorder (MDD) in children and adolescents with ADHD is 5.5 times higher than in those without ADHD (Daviss, 2008), and children and adolescents with both disorders display higher levels of psychosocial impairment than those with either disorder alone (Daviss, 2008). Furthermore, subthreshold ADHD and depressive symptoms are associated with significant impairment and predict future symptoms and negative outcomes (Balázs & Keresztény, 2014; Rodríguez et al., 2012) highlighting the necessity of investigating risk pathways between ADHD and depressive symptoms across subthreshold and clinical levels.
There are clear longitudinal links between ADHD and depressive symptoms. Childhood ADHD predicts higher levels of depressive symptoms throughout emerging adulthood (Meinzer et al., 2016; Rabiner et al., 2008), and individuals with comorbid ADHD and MDD have higher rates of depression recurrence (Daviss, 2008). Further, chronic treatment of persistent ADHD symptoms can prevent the development of depressive symptoms (Meinzer & Chronis-Tuscano, 2017), suggesting a potential causal relation between ADHD and depressive symptoms.
The link between ADHD and depressive symptoms is not yet fully understood, but previously demonstrated mechanisms include altered reward responsivity associated with reduced attention capacity leading to anhedonia (Meizner et al., 2012), and emotion regulation difficulties associated with ADHD symptoms leading to heightened depressive symptoms (Seymour et al., 2012, Seymour et al., 2014). Additionally, the dual failure model describes how symptoms of ADHD lead to failures which can cause demoralization and depressive symptoms (Humphreys et al., 2013). This model suggests that stress generation, the creation or exacerbation of stressful situations due to an individual’s behavior, is a potential mechanism connecting ADHD and depression. ADHD hyperactive and inattentive symptoms lead to impulsive, stimulation-seeking behaviors and difficulty concentrating on and completing tasks (Jackson & Farrugia, 1997), respectively, which lead to stressful events due in part to an individual’s characteristics or behaviors, also known as dependent stressors (e.g., difficulty concentrating on studying leading to doing poorly on an exam, impulsively saying something hurtful to a friend leading to an argument; Hammen, 2018). Indeed, in children, academic and peer problems mediate the relation between ADHD and future depressive symptoms and MDD (Humphreys et al., 2013; Herman et al., 2007), although it should be noted that there is some evidence that in boys with comorbid diagnoses of ADHD and MDD, the dual failure model may not be supported (Biedermann et al., 1998). Thus, though inconsistent, there is preliminary evidence supporting stress generation as a mediating mechanism linking ADHD and depression.
Self-generated stressful events play a critical role in the onset of depression (Hankin et al., 2016; Colodro-Conde et al., 2017): life stress strongly predicts increases in depressive symptoms and onset of MDD episodes (Hammen, 2018; Brown & Harris, 1989; Mazure, 1989; Hankin et al., 2016) and dependent stressors are more predictive of depressive symptoms than independent stressors, or fateful events to which an individual does not contribute (e.g., an illness in the family), in adolescents and young adults (Kendler et al., 1999; Technow et al., 2015). This is potentially due to cognitions elicited by self-generated stressors (e.g., self-blame) that increase risk for depression, as well as vulnerability factors that lead to generation of stressors, which in turn lead to increased depressive symptoms, as described by the stress generation hypothesis of depression (Hammen, 2018; Liu, 2013; Liu & Alloy, 2010). ADHD symptoms may be one such vulnerability factor increasing dependent stressors and subsequent depressive symptoms during college, a high-risk time for depression (Ibrahim et al., 2013).
Despite ADHD and depressive symptoms remaining comorbid into adulthood, it is unknown whether dependent stress mediates this relation during the transition to adulthood or beyond. Importantly, links between ADHD symptoms and stress may be especially salient during the college years, a period marked by increased independence and responsibility along with high academic pressure and peer contact, setting the stage for potential stressful situations caused by ADHD symptoms. Cross-sectional studies of adolescents (Overbey et al., 2009) and adults (Combs et al., 2015; Hirvikoski et al., 2009) demonstrate that ADHD behaviors are associated with stressful situations such as academic/occupational struggles and interpersonal rejection (Young, 2000). Furthermore, in college students with ADHD, top sources of concern include academic performance, relationships with friends, and relationships with family (Beiter et al., 2015). It is possible that these dependent stressors are generated or exacerbated by hyperactive, impulsive and inattentive symptoms of ADHD, and subsequently lead to increased depressive symptoms. A recent longitudinal study demonstrated that comorbid ADHD and internalizing symptoms were associated with heightened levels of negative life events during adolescence, suggesting that trajectories of stressors, ADHD symptoms, and internalizing symptoms (including depression) are intertwined across this period (Hartman et al., 2019). Although the directionality of these relations was not determined, this is consistent with the possibility that ADHD symptoms generate life stressors, which confer risk for depressive symptoms. It remains to be tested, however, whether stress generation mediates the relation between ADHD and depressive symptoms in college students.
Importantly, the relation between ADHD symptoms, dependent stress, and depressive symptoms may differ between inattentive and hyperactive/impulsive symptom dimensions in college students. College students more commonly experience inattentive than hyperactive/impulsive symptoms of ADHD (Nugent & Smart, 2014; Combs et al., 2015), and inattentive symptoms are more strongly associated with depressive symptoms and certain types of self-generated stressors (e.g., peer problems; Friedrichs et al., 2012; Humphreys et al., 2013). This suggests that stress generation may be a stronger mediator in the relation between inattentive than hyperactive/impulsive ADHD symptoms and depressive symptoms, but this has not been tested.
In summary, ADHD symptoms and depressive symptoms are tightly linked; ADHD symptoms increase self-generated stressors, and these stressors predict depressive symptoms. However, it is unknown whether stress generation mediates the risk pathway between ADHD symptoms and depressive symptoms during college, a period of high risk for depressive symptoms (ACHA, 2014), and a time when dependent stressors such as academic performance and interpersonal problems are of particular concern for people with ADHD (Beiter et al., 2015). Therefore, the current study longitudinally tested the hypothesis that the frequency of dependent stressors will mediate the association between ADHD symptoms and subsequent depressive symptoms in college students (Figure 1)1. We additionally tested whether stress generation is a stronger mediator in the relation between inattentive than hyperactive/impulsive ADHD symptoms and depressive symptoms due to inattentive symptoms being more prevalent in college students (Nugent & Smart, 2014; Combs et al., 2015) and more strongly associated with depressive symptoms and certain types of self-generated stressful events (e.g., peer problems; Friedrichs et al., 2012; Humphreys et al., 2013; Figure 2). We tested the models over three time points of a college semester, selected to capture the highest-risk periods for experiencing stress and subsequent increases in depressive symptoms across the college semester. Specifically, we tested how baseline ADHD symptoms predict stress in the weeks leading up to final exams, and how this predicts depressive symptoms immediately following final exams (Figure 1). Last, we did not have hypotheses regarding gender moderation, but due to evidence of stronger links between dependent stress and depression (Hankin et al., 2007; Rucklidge, 2008), and ADHD and MDD (Jerrell et al., 2015) in girls and women, we tested whether gender moderated these paths in the mediation models.
Figure 1.
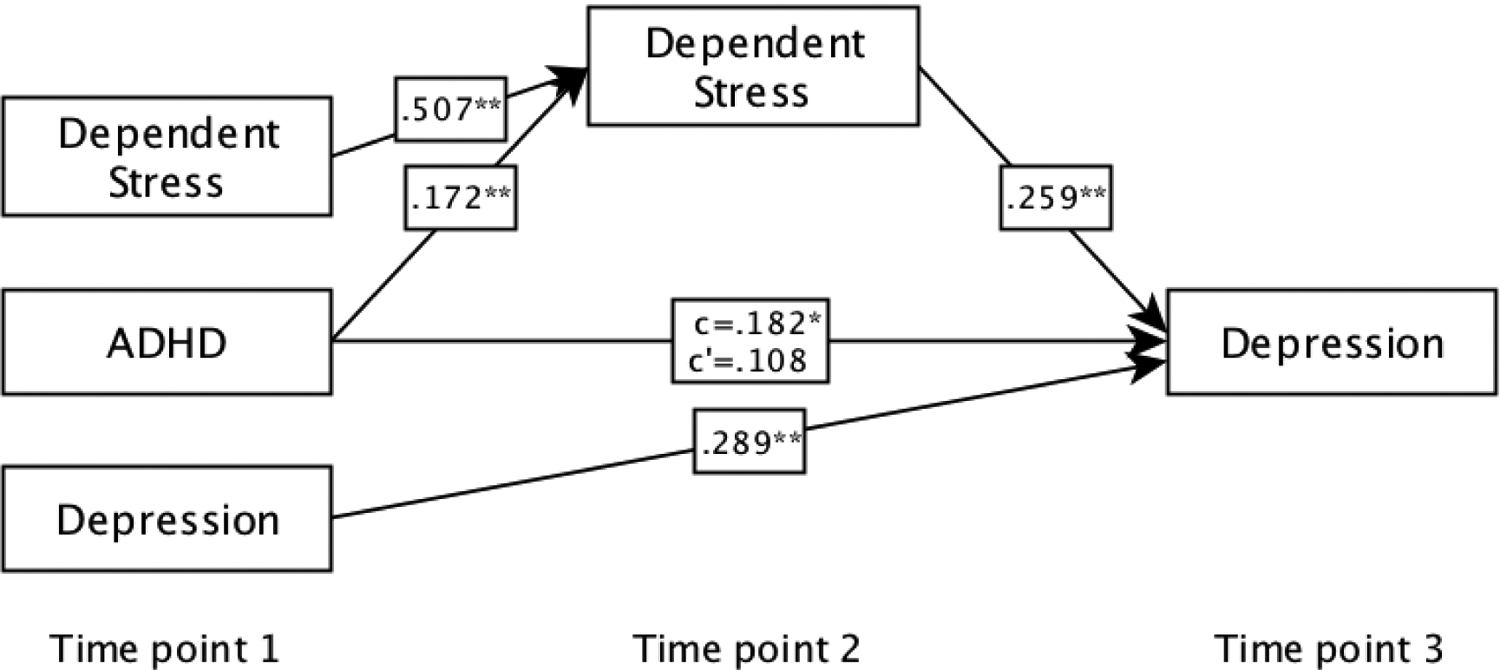
Path models with ADHD at time-point 1, dependent stress at time-point 2, and depression at time-point 3, covarying for time point 1 depressive symptoms and dependent stress. ADHD symptoms significantly prospectively predict increased depressive symptoms over and above concurrent depression via the dependent stress indirect pathway, covarying for age and gender. * p < .05. ** p < .01.
Figure 2.
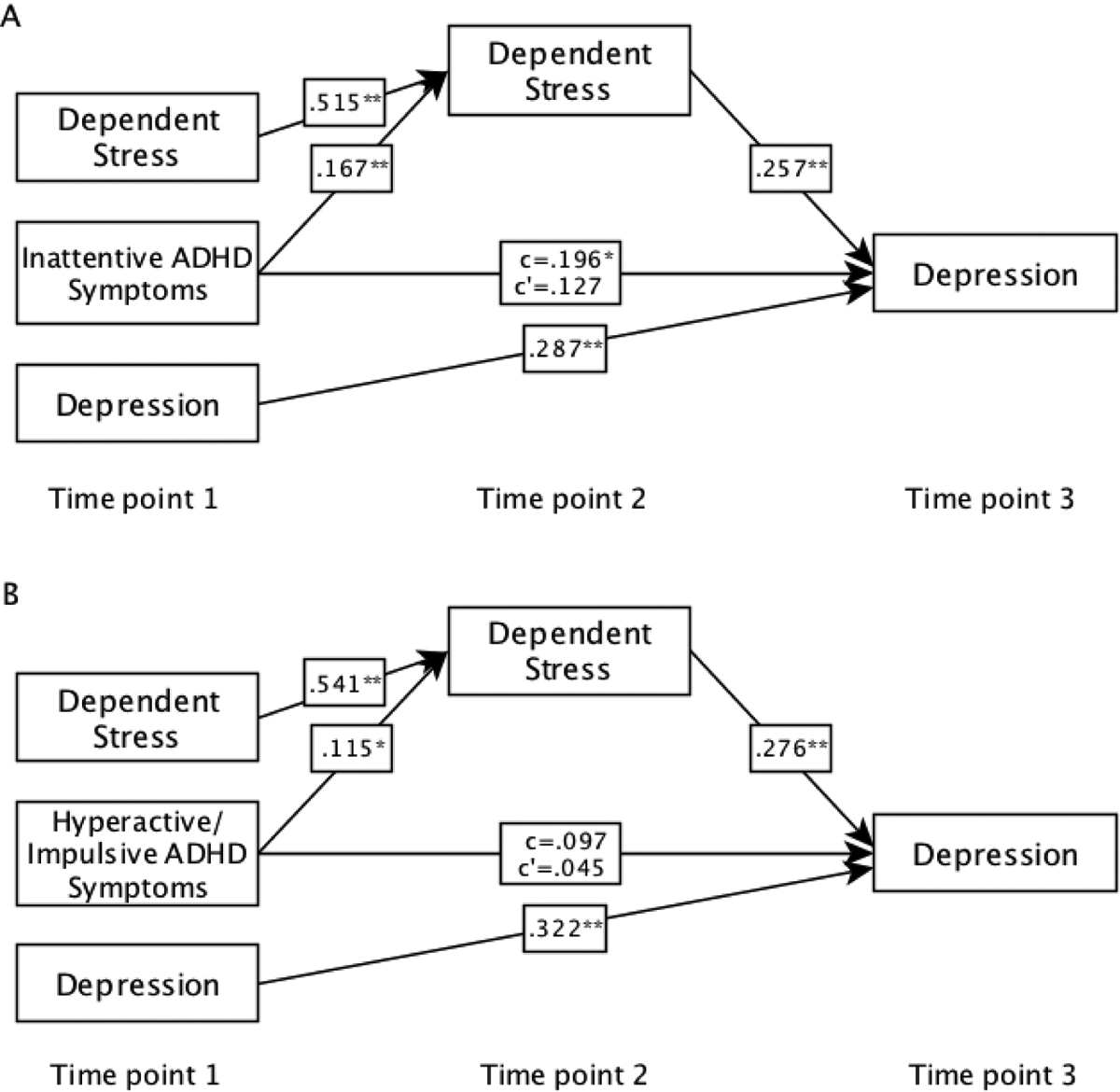
Path models with inattentive ADHD symptoms (A) and hyperactive/impulsive ADHD symptoms (B) at time-point 1, dependent stress at time-point 2, and depression at time-point 3, covarying for time point 1 depressive symptoms and dependent stress. These models covaried for age and gender. The ADHD symptom categories do not significantly differ in their relation to dependent stress or depression. * p < .05. ** p < .01.
Methods
Participants
Participants were 224 undergraduate students (70.1% female) ages 18–23 (M=19.33) and were largely residential students living on or near campus. Self-report indicated that 4.91% had been diagnosed with ADHD, consistent with prevalence estimates for young adults (Willcutt, 2012), and 0.90% took ADHD medication the day of the baseline survey. Participants were recruited via flyers on campus and postings in the university “Class of [year]” Facebook groups and were fluent in English. There were no other exclusion criteria. Participants gave written informed consent and all procedures were approved by the University IRB. Retention in the study was high: 224 participants enrolled, and 208 completed the three study time-points.
Procedure
Data were collected as part of a larger longitudinal study, which included additional measures not relevant to the current hypotheses for other planned publications. Participants were followed over the course of a semester allowing the measurement of ADHD symptoms at baseline (time-point 1, within the first 10 weeks of the semester), stress in the four weeks leading up to final exams (time-point 2), and depressive symptoms immediately following finals (time-point 3). All measures were also collected at time-point 1 to analyze change from baseline. Questionnaires were administered online through the secure Qualtrics system.
Measures
Adult ADHD Self-Report Scale (ASRS; Kessler et al., 2005) is an 18-item measure of the frequency of ADHD symptoms during the last 6 months on a 5-point Likert scale ranging from (0) never to (4) very often. It includes two 9-item subscales measuring inattentive symptoms (e.g., “How often do you have trouble remembering appointments or obligations?”) and hyperactive/impulsive symptoms (e.g., “How often do you feel restless or fidgety?”). The ASRS is reliable and valid for evaluating ADHD in adults (Adler et al., 2006) and internal consistency in the current study was good (α = .823).
The Adolescent/Adult Life Events Questionnaire Revised (ALEQ-R; Fassett-Carman et al., 2019), the revised version of the ALEQ (Abramson & Hankin, 2002), assesses the frequency of 63 independent and dependent stressful life events typical of adolescents and emerging adults over the past six months on a 5-point Likert scale ranging from (0) never to (4) always. Only dependent stressors (e.g., “Problems or arguments with teachers/professors or a boss/supervisor”, for coding see Fassett-Carman et al., 2019), were analyzed in the current study, as the hypotheses tested stress generation models. The full questionnaire, including 23 dependent events, was administered at time-point 1, but a shortened version including 9 dependent stressors frequently experienced by students (Fassett-Carman et al., 2020) was administered in the four weekly time-point 2 questionnaires to decrease participant burden. Dependent stress frequency across the four weeks leading up to finals was averaged to calculate a single time-point 2 score.
Beck Depression Inventory (BDI-II; Beck et al., 1996) includes 21 items assessing depressive symptoms within the past week on a 4-point Likert scale ranging from (0) I do not feel sad to (3) I am so sad and unhappy that I cannot stand it. It is valid and reliable (Beck et al., 1996), and internal consistency in the current study was good (α = .898).
Data Analysis
Mediation analyses were run in Mplus version 8 with FIML estimation to handle missing data and 10,000 bootstrap iterations for robust estimation2. Monte Carlo power analyses with 10,000 repetitions demonstrated adequate power (> 0.8) to detect medium effect sizes (β = 0.3) for each path. Outliers +/− three standard deviations from the mean were excluded from analysis.
First, we tested the total effect of time-point 1 ADHD symptoms on time-point 3 depressive symptoms. Next, we tested the mediation model with an indirect path from time-point 1 ADHD symptoms to time-point 3 depressive symptoms via time-point 2 dependent stress3. All tests covaried for age, gender, and time-point 1 depressive symptoms and dependent stress to assess change over time. We further tested inattentive and hyperactive/impulsive ADHD symptoms in these models separately and conducted Wald tests to determine if they differed in their relation to depressive symptoms or dependent stress.
Results
Descriptive Statistics and Bivariate Correlations (Tables 1 & 2).
Table 1.
Descriptive Statistics
| Measure | n | Mean | SD | Skewness | Kurtosis | ||
|---|---|---|---|---|---|---|---|
| Statistic | SE | Statistic | SE | ||||
| T1 ADHD Overall | 223 | 31.51 | 9.469 | .162 | .163 | −.212 | .324 |
| T1 ADHD-I | 222 | 17.07 | 5.348 | .408 | .163 | −.063 | .325 |
| T1 ADHD-H | 223 | 14.35 | 5.374 | .130 | .163 | −.099 | .324 |
| T1 Dependent Stress | 221 | 14.00 | 8.619 | .808 | .164 | .201 | .326 |
| T1 Dependent Stress (sqrt) | 221 | 3.56 | 1.166 | .132 | .164 | −.547 | .326 |
| T1 Depression | 220 | 8.90 | 7.145 | 1.000 | .164 | .586 | .327 |
| T1 Depression (Sqrt) | 220 | 2.70 | 1.276 | −.026 | .164 | −.401 | .327 |
| T2 Dependent Stress | 217 | 3.19 | 2.54 | .991 | .165 | .302 | .329 |
| T2 Dependent Stress (sqrt) | 217 | 1.63 | .728 | .172 | .165 | −.549 | .329 |
| T3 Depression | 206 | 7.81 | 7.507 | 1.212 | .169 | .958 | .337 |
| T3 Depression (sqrt) | 206 | 2.38 | 1.470 | .036 | .169 | −.615 | .337 |
| Age | 224 | 19.33 | 1.280 | .704 | .163 | −.519 | .324 |
Note: ADHD-I, inattentive ADHD symptoms; ADHD-H, hyperactive/impulsive ADHD symptoms; T1, time-point 1; T2, time-point 2; T3, time-point 3. Sqrt; square-root transform was applied due to high skewness. The square-root transformed versions of the stress and depression variables were used for all subsequent analyses.
Table 2.
Bi-variate Correlations
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. T1 ADHD-I | - | |||||||
| 2. T1 ADHD-H | .536** | - | ||||||
| 3. T1 ADHD Overall | .876** | .869** | - | |||||
| 4. T1 Dependent Stress | .369** | .294** | .396** | - | ||||
| 5. T1 Depression | .490** | .448** | .535** | .579** | - | |||
| 6. T2 Dependent Stress | .369** | .289** | .386** | .578** | .367** | - | ||
| 7. T3 Depression | .330** | .236** | .321** | .319** | .441** | .403** | - | |
| 8. Age | −.039 | −.102 | −.089 | −.063 | −.128 | .030 | .074 | - |
Note. ADHD-I, inattentive ADHD symptoms; ADHD-H, hyperactive/impulsive ADHD symptoms; T1, time-point 1; T2, time-point 2; T3, time-point 3.
p < .05.
p < .01
Descriptive statistics are reported in Table 1. Four participants did not complete time-points 2 and 3, and 11 did not complete time-point 3 (but did complete time-point 2), thus these participants were missing data for these time-points4. Additionally, data were missing from 1 participant on the time-point 1 stress measure due to skipping questions. Outliers (+/− 3SD from the mean) were excluded from analysis (one for time-point 1 ADHD, two for inattentive ADHD symptoms, one for hyperactive/impulsive ADHD symptoms, two for time-point 1 stress, four for time-point 1 depressive symptoms, three for time-point 2 stress, and three for time-point 3 depressive symptoms)5. For depressive symptoms, 10.7 percent of the sample scored in the moderate to severe range (score of 20 or greater; Beck et al., 1996) at baseline. For ADHD symptoms, 22.4% scored in the possible clinical range based on the 6-item continuous ASRS screener (score 14–17; Kessler et al., 2007) and 4.9% scored in the likely clinical range (score 18–24). Gender data for participants that answered ‘Other’ (n= 10) were excluded from analyses. Time-points 1 and 3 stress and depression measures were square-root transformed to correct for high skewness (Table 1). All subsequent analyses used the transformed variables. There were no significant gender differences in ADHD symptoms, dependent stress, or depressive symptoms (Table S1). At time-point 1, there were significant correlations (Table 2) between ADHD and dependent stress, ADHD and depression, and dependent stress and depression. Longitudinally, depression at time-point 1 significantly correlated with depression at time-point 3 and dependent stress at time-point 1 significantly correlated with dependent stress at time-point 2. ADHD at time-point 1 significantly correlated with dependent stress at time-point 2 and dependent stress at time-point 2 significantly correlated with depression at time-point 3.
Total effect model (Figure 1 and Table 3).
Table 3.
ADHD, Dependent Stress, and Depression Mediation Model.
| Outcome Variable | Predictor | β | SE | Est./SE | p | 95% CI | R 2 | |
|---|---|---|---|---|---|---|---|---|
| Longitudinal Total Effect Model | ||||||||
| T3 Depression | T1 ADHD (c)* | .182 | .086 | 2.117 | .034 | [0.011–0.348] | .232 | |
| T1 Depression** | .344 | .082 | 4.206 | <.001 | [0.184–0.506] | |||
| Age | .100 | .062 | 1.621 | .105 | [−0.027–0.217] | |||
| Gender | .098 | .067 | 1.452 | .147 | [−0.037–0.226] | |||
| Longitudinal Mediation Path Model | ||||||||
| T2 Dependent Stress | T1 ADHD (a)** | .172 | .060 | 2.847 | .004 | [0.051–0.289] | .361 | |
| T1 Dependent Stress** | .507 | .059 | 8.549 | <.001 | [0.388–0.618] | |||
| Age | .081 | .058 | 1.388 | .165 | [−0.033–0.195] | |||
| Gender | −.014 | .054 | −0.265 | .791 | [−0.123–0.090] | |||
| T3 Depression | T1 ADHD (direct effect c’) | .108 | .084 | 1.286 | .198 | [−0.062–0.268] | .287 | |
| T1 Depression** | .289 | .083 | 3.484 | <.001 | [0.130–0.452] | |||
| T2 Dependent Stress (b)** | .259 | .067 | 3.875 | <.001 | [0.121–0.387] | |||
| Age | .085 | .059 | 1.452 | .147 | [−0.034–0.197] | |||
| Gender | .074 | .066 | 1.131 | .258 | [−0.054–0.201] | |||
| Longitudinal Mediation Path Model Indirect Effect | ||||||||
| T1 ADHD → T2 Dependent Stress → T3 Depression* | .044 | .020 | 2.245 | .025 | [0.011–0.087] | |||
Note. T1, time-point 1; T2, time-point 2; T3, time-point 3.
p < .05.
p < .01. Gender coded as female=2, male=1.
Higher ADHD scores at time-point 1 significantly predicted increased depression scores at time-point 3, covarying for depression at time-point 1, age, and gender. The variables in this model explained 23.2% of the variance in depressive symptoms at time-point 3.
Mediation path model (Figure 1 and Table 3).
Covarying for age, gender, and dependent stress at time-point 1, higher ADHD scores at time-point 1 significantly predicted higher dependent stress at time-point 2. Higher dependent stress at time-point 2 significantly predicted increased depressive symptoms at time-point 3, covarying for time-point 1 depression, age and gender. There was a significant indirect path from ADHD at time-point 1 to depression at time-point 3 mediated by dependent stress at time-point 2. The variables in this model explained 28.7% of the variance in depressive symptoms at time-point 3.
Exploratory Model by ADHD Symptom Dimensions
ADHD symptom dimension total effect models (Figure 2 and Table 4).
Table 4.
ADHD Inattentive and Hyperactive/Impulsive Symptom Dimension Mediation Models.
| Outcome Variable | Predictor | β | SE | Est./SE | p | 95% CI | R 2 |
|---|---|---|---|---|---|---|---|
| Inattentive Symptom Dimension | |||||||
| Longitudinal Total Effect Model | |||||||
| T3 Depression | T1 ADHD-I (c)* | .196 | .082 | 2.386 | .017 | [0.032–0.356] | .238 |
| T1 Depression** | .347 | .078 | 4.462 | <.001 | [0.193–0.497] | ||
| Age | .092 | .062 | 1.478 | .139 | [−0.036–0.210] | ||
| Gender | .093 | .066 | 1.392 | .164 | [−0.040–0.220] | ||
| Longitudinal Mediation Path Model | |||||||
| T2 Dependent Stress | T1 ADHD-I (a)** | .167 | .060 | 2.764 | .006 | [0.046–0.283] | .361 |
| T1 Dependent Stress** | .515 | .057 | 9.059 | <.001 | [0.399–0.621] | ||
| Age | .074 | .059 | 1.256 | .209 | [−0.042–0.189] | ||
| Gender | −.017 | .053 | −0.322 | .748 | [−0.124–0.086] | ||
| T3 Depression | T1 ADHD- I (direct effect c’) | .127 | .084 | 1.509 | .131 | [−0.042–0.268] | .291 |
| T2 Dependent Stress (b)** | .257 | .066 | 3.898 | <.001 | [0.121–0.383] | ||
| T1 Depression ** | .287 | .080 | 3.581 | <.001 | [0.128–0.442] | ||
| Age | .080 | .059 | 1.346 | .178 | [−0.041–0.192] | ||
| Gender | .073 | .065 | 1.119 | .263 | [−0.055–0.197] | ||
| Longitudinal Mediation Path Model Indirect Effects | |||||||
| T1 ADHD-I → T2 Dependent Stress → T3 Depression | .043 | .020 | 2.196 | .028* | [0.010–0.087] | ||
| Hyperactive/Impulsive Symptom Dimension | |||||||
| Longitudinal Total Effect Model | |||||||
| T3 Depression | T1 ADHD-H (c) | .097 | .080 | 1.205 | .228 | [−0.064–0.252] | .216 |
| T1 Depression** | .397 | .076 | 5.263 | <.001 | [0.246–0.542] | ||
| Age | .107 | .062 | 1.733 | .083 | [−0.019–0.225] | ||
| Gender | .085 | .068 | 1.250 | .211 | [−0.051–0.215] | ||
| Longitudinal Mediation Path Model | |||||||
| T2 Dependent Stress | T1 ADHD-H (a)* | .115 | .058 | 1.973 | .049 | [−0.001–0.228] | .349 |
| T1 Dependent Stress** | .541 | .058 | 9.390 | <.001 | [0.424–0.649] | ||
| Age | .085 | .059 | 1.447 | .148 | [−0.029–0.200] | ||
| Gender | −.024 | .055 | −0.430 | .668 | [−0.134–0.085] | ||
| T3 Depression | T1 ADHD-H (direct effect c’) | .045 | .078 | 0.577 | .564 | [−0.109–0.194] | .278 |
| T2 Dependent Stress (b)** | .276 | .067 | 4.089 | <.001 | [0.137–0.402] | ||
| T1 Depression** | .322 | .078 | 4.132 | <.001 | [0.170–0.474] | ||
| Age | .089 | .059 | 1.501 | .133 | [−0.031–0.200] | ||
| Gender | .065 | .066 | 0.987 | .324 | [−0.064–0.193] | ||
| Longitudinal Mediation Path Model Indirect Effect | |||||||
| T1 ADHD-H → T2 Dependent Stress → T3 Depression | .032 | .018 | 1.728 | .084 | [0.000–0.071] | ||
Note. ADHD-I, inattentive ADHD symptoms; T1, time-point 1; T2, time-point 2; T3, time-point 3.
p < .05.
p < .01. Gender coded as female=2, male=1.
When tested in separate models, inattentive symptoms, but not hyperactive/impulsive symptoms, at time-point 1 significantly predicted increased depressive symptoms at time-point 3, covarying for age, gender, and time-point 1 depression.
ADHD symptom dimension mediation path models (Figure 2 and Table 4).
When tested separately, increased inattentive and hyperactive symptoms at time-point 1 predicted higher dependent stress at time-point 2, as was the case for total ADHD symptom scores. Increased dependent stress at time-point 2 significantly predicted increased depressive symptoms at time-point 3 in both subtype models. There was a significant indirect path to depression at time-point 3 mediated by dependent stress at time-point 2 for inattentive but not hyperactive symptoms. However, Wald tests indicated that there was no significant difference between the effects of inattentive and hyperactive/impulsive symptoms on dependent stress (χ2 (1) =.774, p = .379) or depression (χ2 (1) = 2.001, p = .157).
Gender Moderation (Tables S3 & S4)
Gender did not moderate the longitudinal relations between ADHD symptoms (total and dimensions) and dependent stress or dependent stress and depressive symptoms (Tables S3 & S4).
Discussion
Although previous research indicated that individuals with ADHD are at a higher risk for depression (Meinzer et al., 2016) and that specific types of life stressors (e.g., peer, academic) may mediate this relation in children and adolescents, stress generation as a mediating mechanism had not been tested in emerging adults and adulthood. The current study found that dependent (i.e., self-generated) stress longitudinally mediated the relation between ADHD and subsequent depressive symptoms, as hypothesized. There were no significant differences in the effects of inattentive and hyperactive/impulsive symptoms on dependent stress and depression, contrary to our hypothesis that these relations would be stronger for inattentive symptoms.
The finding that ADHD symptoms contribute to stress generation is consistent with previous research (Beiter et al., 2015; Jackson & Farrugia, 1997; Hartman et al., 2019). The primary characteristics of ADHD bring on a cascade of difficult life events, ranging from trouble creating strong social relationships to retaining employment. Specifically, impaired attention, interpersonal skills, initiative, and task persistence may hinder academic and occupational functioning (Combs et al., 2015). Additionally, college-age adults with ADHD demonstrate significantly lower task performance in the areas of concentration, motivation, and information processing (Combs et al., 2015), which may lead to the generation of stressors via academic difficulties (e.g., doing poorly on an exam).
The significant relation between dependent stress and subsequent depression in this study is also consistent with previous research (Hammen, 2018; Kendler et al., 1999; Technow et al., 2015). Dependent stressors are especially salient in creating risk for depression, more so than independent stressors (Kendler et al., 1999; Technow et al., 2015). Understanding that one played a role in causing a stressor could lead to depressive symptoms such as low self-esteem, and feelings of worthlessness and hopelessness. While this has not been tested directly, it is consistent with research on cognitive styles demonstrating that attributing stressful events to internal causes is a risk factor for depression (Huang, 2015; Scallion & Cummings, 2018).
Contrary to our hypothesis, there were no significant differences between the effects of inattentive and hyperactive/impulsive symptoms on dependent stress and depressive symptoms. Although this was not consistent with the majority of previous literature (Combs et al., 2015; Friedrichs et al., 2012; Humphreys et al., 2013, Willcutt et al., 2012), our findings are consistent with other studies which found no significant difference between ADHD symptom types (Eiraldi et al., 1997; Nelson & Gregg, 2012; Power et al., 2004). It is possible that there is no difference between inattentive and hyperactive/impulsive ADHD symptoms in predicting total frequency of dependent stressors because inattentive and hyperactive/impulsive symptoms are associated with different types of dependent stressors. For example, a review article concluded that hyperactivity is strongly associated with negative peer regard while inattention is strongly associated with social isolation (Willcutt et al., 2012). Thus, the different ADHD symptom types may lead to similar overall levels of stress, but via different mechanisms.
In the current sample, there were no gender differences in ADHD symptoms, dependent stress, or depressive symptoms, and gender did not moderate the relations between these variables. This is not consistent with past studies demonstrating higher dependent stress and depressive symptoms in women (Hankin et al., 2007; Rucklidge, 2008) and a higher probability of girls with ADHD developing MDD in late childhood or adolescence (Jerrell et al., 2015). Gender moderation should thus be tested in general population-representative samples.
Limitations and Future Directions
This study has several limitations which are important to note. First, the study used a non-selected sample of college students because ADHD symptoms at all levels may be especially impairing during this transition to independence, and this is a high-risk period for the onset and recurrence of depressive symptoms (Whisman & Richardson, 2015). However, future research is needed to determine if these results generalize to participants with more severe levels of ADHD and depression, other age groups, and non-college emerging adults. Additionally, the relatively short longitudinal design of this study aimed to capture symptom levels across a college semester, a salient time period for fluctuations in stress in the college population. The results thus cannot elucidate how ADHD symptoms predict stress generation and depressive symptoms over a longer time course. Furthermore, this study used self-report measures, potentially leading to recall or reporting bias and shared method variance across measures. However, these self-report measures are frequently used, reliable, and valid (Gray et al., 2014; Salla et al., 2017; Silverstein et al., 2014; Beck, et al., 1996).
The results of this study suggest many future directions. First, it is important to capture how ADHD symptoms relate to stress generation, mood, and psychopathology at different time scales and across different types of stress. Ecological momentary assessment could be used to test how ADHD symptoms relate to daily stressors and subsequent alterations in mood. Longer longitudinal models could additionally test how ADHD symptoms continue to relate to stress generation and depressive symptoms outside of the semester period. Furthermore, future research should test whether certain types of dependent stressors (e.g., academic, peer) are especially strong in mediating the ADHD-depression link.
Second, the current model assessed dependent stress frequency to test a stress generation mechanism. However, ADHD symptoms are also associated with higher perceived stress (Combs et al., 2015; Hirvikoski et al., 2009; Salla et al., 2017), altered physiological stress reactivity (Combs et al., 2015; Lackschewitz et al., 2008), and impaired coping ability (Hampel et al., 2008). Increased reactivity and trouble coping with stress could have an especially salient effect on psychopathology at the end of the college semester while experiencing the academic demands of finals. Thus, stress appraisals, stress reactivity, and maladaptive coping may be important additional mediators that should be tested in explaining the relation between ADHD and depressive symptoms in college students.
Finally, the current research suggests potential targets for intervention aimed at treating or preventing depression in those with ADHD symptoms, which could be explored in future translational research. Since disrupting the link between ADHD symptoms and dependent stress could prevent subsequent depressive symptoms in college students, interventions that combat dependent stress-generative tendencies characteristic of ADHD may be promising. Indeed, existing interventions for college students that teach skills such as organization, time management, and planning reduce inattentive and hyperactive ADHD symptoms and self-reported academic impairment, increase behavioral regulation, and decrease depressive symptoms (LaCount et al., 2018; Anastopoulos et al., 2020), potentially via decreasing stress generation. Additionally, disrupting the link between dependent stressors and depressive symptoms may also be an important point of intervention, especially given evidence for elevated stress reactivity in individuals with ADHD. The Behaviorally Enhancing Adolescents’ Mood (BEAM) depressive prevention program for adolescents with ADHD provides training on how to regulate responses to stressors in order to target emotion regulation deficits and decrease depressive symptoms (Meinzer et al., 2018). Future interventions could combine such therapies in order to teach skills aimed at preventing stress generation and regulating responses to these stressors.
Conclusions
In sum, the current study demonstrates that stress generation is an important mediating factor in the longitudinal relation between ADHD symptoms and depressive symptoms in college students, suggesting multiple targets for intervention. Future studies should test these relations at varying time scales (e.g., daily fluctuations in stress and affect vs long-term fluctuations in symptoms), and whether certain types of stressors (e.g., peer relations) are especially salient in mediating the ADHD-depressive symptom link.
Supplementary Material
Footnotes
All hypotheses were submitted in an honors thesis proposal prior to data analysis, and the proposal is now posted on OSF: https://osf.io/w8qak/?view_only=9056a571dc784dcca9bf7a0b9dfbc3e6
Data and syntax/results files are posted in OSF: https://osf.io/bkmj2/?view_only=e7576d6b9e934aebb8ab1471bbbff19e
Because a short-form version of the ALEQ-R was used for the time-point 2 dependent stress measure, we additionally conducted a cross-sectional analysis using time-point 1 measures (ADHD, full ALEQ-R, and depression). The pattern of results for the cross-sectional model was the same as the longitudinal model (see Supplemental Materials).
Tests for selective attrition showed that those who did not complete the study were higher in T1 ADHD symptoms than those who completed the study (Supplemental Table S5).
Winsorized analyses were also performed and results were largely the same (Supplemental Tables S6–S9).
References
- Abramson Lyn Y., & Hanklin Benjamin L. (2002). Measuring cognitive vulnerability to depression in adolescence: Reliability, validity, and gender differences. Journal of Clinical Child and Adolescent Psychology, 31(4), 491–504. doi: 10.1207/S15374424JCCP3104_8 [DOI] [PubMed] [Google Scholar]
- Adler LA, Spencer T, Faraone SV, Kessler RC, Howes MJ, Biederman J, & Secnik K (2006). Validity of pilot Adult ADHD Self-Report Scale (ASRS) to rate adult ADHD symptoms. Annals of Clinical Psychiatry, 18(3), 145–148. doi: 10.1080/10401230600801077 [DOI] [PubMed] [Google Scholar]
- American College Health Association (2014). American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. Hanover, MD. [Google Scholar]
- Anastopoulos AD, King KA, Besecker LH, O’Rourke SR, Bray AC, & Supple AJ (2020). Cognitive-Behavioral Therapy for College Students With ADHD: Temporal Stability of Improvements in Functioning Following Active Treatment. Journal of Attention Disorders, 24(6), 863–874. 10.1177/1087054717749932 [Google Scholar]. [DOI] [PubMed] [Google Scholar]
- Balázs J, Keresztény Á (2014). Subthreshold attention deficit hyperactivity in children and adolescents: a systematic review. Eur Child Adolesc Psychiatry, 23, 393–408. 10.1007/s00787-013-0514-7 [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck Depression Inventory manual (2nd ed.). San Antonio, TX: Psychological Corporation. doi: 10.1093/occmed/kqv087 [DOI] [Google Scholar]
- Beiter R, Nash R, McCrady M, Rhoades D, Linscomb M, Clarahan M, & Sammut S (2015). The prevalence and correlates of depression, anxiety, and stress in a sample of college students. Journal of Affective Disorders, 173, 90–96. doi: 10.1016/j.jad.2014.10.054 [DOI] [PubMed] [Google Scholar]
- Biedermann J, Mick E, & Faraone SV (1998). Depression in attention deficit hyperactivity disorder (ADHD) children: “True” depression or demoralization? Journal of Affective Disorders, 47, 113–122. 10.1016/S0165-0327(97)00127-4 [DOI] [PubMed] [Google Scholar]
- Brown GW, & Harris TO (Eds.). (1989). Life events and illness. Guilford Press. [Google Scholar]
- Colodro-Conde L, Couvy-Duchesne B, Zhu G, Coventry WL, Byrne EM, Gordon S, … & Eaves LJ (2017). A direct test of the diathesis–stress model for depression. Molecular psychiatry. 10.1038/mp.2017.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Combs MA, Canu WH, Broman-Fulks JJ, Rocheleau CA, & Nieman DC (2015). Perceived stress and ADHD symptoms in adults. Journal of Attention Disorders, 19(5), 425–434. doi: 10.1177/1087054712459558 [DOI] [PubMed] [Google Scholar]
- Daviss B (2008). A review of co-morbid depression in pediatric ADHD: etiologies, phenomenology, and treatment. Journal of Child Adolescent Psychopharmacology, 18, 565–71. doi: 10.1089/cap.2008.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiraldi RB, Power TJ, & Nezu CM (1997). Patterns of Comorbidity Associated With Subtypes of Attention-Deficit/Hyperactivity Disorder Among 6− to 12-Year-Old Children. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 503–514. doi: 10.1097/00004583-199704000-00013 [DOI] [PubMed] [Google Scholar]
- Fassett-Carman A, Hankin BL, & Snyder HR (2019). Appraisals of dependent stressor controllability and severity are associated with depression and anxiety symptoms in youth. Anxiety, Stress, & Coping, 32(1) 32–49. doi: 10.1080/10615806.2018.1532504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fassett-Carman AN, DiDomenico GE, Steiger, von J, & Snyder HR (2020). Clarifying stress-internalizing associations: Stress frequency and appraisals of severity and controllability are differentially related to depression-specific, anxiety-specific, and transdiagnostic internalizing factors. Journal of Affective Disorders, 260, 638–645. 10.1016/j.jad.2019.09.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM, & Beautrais AL (2005). Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry, 62(1), 66–72. 10.1001/archpsyc.62.1.66 [DOI] [PubMed] [Google Scholar]
- Friedrichs B, Igl W, Larsson H, & Larsson J-O (2012). Coexisting psychiatric problems and stressful life events in adults with symptoms of ADHD—A large Swedish population-based study of twins. Journal of Attention Disorders, 16, 13–22. doi: 10.1177/1087054710376909. [DOI] [PubMed] [Google Scholar]
- Jerrell JM, McIntyre RS, & Park YMM (2015). Risk factors for incident major depressive disorder in children and adolescents with attention-deficit/hyperactivity disorder. European Child & Adolescent Psychiatry, 24(1), 65–73. doi: 10.1007/s00787-014-0541-z [DOI] [PubMed] [Google Scholar]
- Gray S, Woltering S, Mawjee K, & Tannock R (2014). The Adult ADHD Self-Report Scale (ASRS): utility in college students with attention-deficit/hyperactivity disorder. PeerJ, 2, e324. doi: 10.7717/peerj.324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C (2018). Risk Factors for Depression: An Autobiographical Review. Annual Review of Clinical Psychology, 14, 1–28. 10.1146/annurev-clinpsy-050817-08481 [DOI] [PubMed] [Google Scholar]
- Hampel P, Manhal S, Roos T, & Desman C (2008). Interpersonal Coping Among Boys With ADHD. Journal of Attention Disorders, 11(4), 427–436. 10.1177/1087054707299337 [DOI] [PubMed] [Google Scholar]
- Hankin BL, Mermelstein R, & Roesch L (2007). Sex differences in adolescent depression: Stress exposure and reactivity models. Child Development, 78(1), 279–295. doi: 10.1111/j.1467-8624.2007.00997.x [DOI] [PubMed] [Google Scholar]
- Hankin BL, Snyder HR, Gulley LD, Schweizer TH, Bijttebier P, Nelis S, … Vasey MW (2016). Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Development and Psychopathology, 28(4 Pt 1), 987–1012. 10.1017/S0954579416000663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman CA, Rommelse N, van der Klugt CL, Wanders RBK, & Timmerman ME (2019). Stress Exposure and the Course of ADHD from Childhood to Young Adulthood: Comorbid Severe Emotion Dysregulation or Mood and Anxiety Problems. Journal of Clinical Medicine, 8(11), 1824–15. doi: 10.3390/jcm8111824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman KC, Lambert SF, Ialongo NS, & Ostrander R (2007). Academic pathways between attention problems and depressive symptoms among urban African American children. Journal of Abnormal Child Psychology, 35, 265–274. doi: 10.1007/s10802-006-9083-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirvikoski T, Lindholm T, Nordenström A, Nordström AL, & Lajic S (2009). High self-perceived stress and many stressors, but normal diurnal cortisol rhythm, in adults with ADHD (attention-deficit/hyperactivity disorder). Hormones and Behavior, 55(3), 418–424. doi: 10.1016/j.yhbeh.2008.12.004 [DOI] [PubMed] [Google Scholar]
- Huang C (2015). Relation between attributional style and subsequent depressive symptoms: A systematic review and meta-analysis of longitudinal studies. Cognitive Therapy and Research, 39(6), 721–735. doi: 10.1007/s10608-015-9700-x [DOI] [Google Scholar]
- Humphreys KL, Katz SJ, Lee SS, Hammen C, Brennan PA, & Najman JM (2013). The association of ADHD and depression: Mediation by peer problems and parent–child difficulties in two complementary samples. Journal of Abnormal Psychology, 122(3), 854–867. doi: 10.1037/a0033895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim AK, Kelly SJ, Adams CE, & Glazebrook C (2013). A systematic review of studies of depression prevalence in university students. Journal of Psychiatric Research, 47(3), 391–400. 10.1016/j.jpsychires.2012.11.015 [DOI] [PubMed] [Google Scholar]
- Jackson B, & Farrugia D (1997). Diagnosis and treatment of adults with attention deficit hyperactivity disorder. Journal of Counseling and Development, 75, 312–319. doi: 10.1002/j.1556-6676.1997.tb02346.x [DOI] [Google Scholar]
- Kendler KS, Karkowski LM, & Prescott CA (1999). Causal relationship between stressful life events and the onset of major depression. The American Journal of Psychiatry, 156, 837–848. doi: 10.1176/ajp.156.6.837 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Ames M, Delmer O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, Ustun TB, & Walters EE (2005). The World Health Organization Adult ADHD Self-Report Scale (ASRS): A Short Screening Scale for Use in the General Population. Psychological Medicine, 35, 245–256. doi: 10.1017/s0033291704002892 [DOI] [PubMed] [Google Scholar]
- Lackschewitz H, Hüther G, & Kröner-Herwig B (2008). Physiological and psychological stress responses in adults with attention-deficit/hyperactivity disorder (ADHD). Psychoneuroendocrinology, 33(5), 612–624. doi: 10.1016/j.psyneuen.2008.01.016 [DOI] [PubMed] [Google Scholar]
- LaCount PA, Hartung CM, Shelton CR, & Stevens AE (2018). Efficacy of an Organizational Skills Intervention for College Students With ADHD Symptomatology and Academic Difficulties. Journal of Attention Disorders, 22(4), 356–367. 10.1177/1087054715594423 [DOI] [PubMed] [Google Scholar]
- Liu RT (2013). Stress generation: Future directions and clinical implications. Clinical Psychology Review, 33(3), 406–416. doi: 10.1016/j.cpr.2013.01.005 [DOI] [PubMed] [Google Scholar]
- Liu RT, & Alloy LB (2010). Stress generation in depression: a systematic review of the empirical literature and recommendations for future study. Clinical Psychology Review, 30, 582–593. doi: 10.1016/j.cpr.2010.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazure CM (1998). Life stressors as risk factors in depression. Clinical Psychology: Science and Practice, 5(3), 291–313. 10.1111/j.1468-2850.1998.tb00151.x [DOI] [Google Scholar]
- Meinzer MC, Pettit JW, Leventhal AM, & Hill RM (2012). Explaining the covariance between attention-deficit hyperactivity disorder symptoms and depressive symptoms: the role of hedonic responsivity. Journal of clinical psychology, 68(10), 1111–1121. 10.1002/jclp.21884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer MC, & Chronis-Tuscano A (2017). ADHD and the development of depression: Commentary on the prevalence, proposed mechanisms, and promising interventions. Current Developmental Disorders Reports, 4(1), 1–4. doi: 10.1007/s40474-017-0106-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer MC, Hartley CM, Hoogesteyn K, & Pettit JW (2018). Development and open trial of a depression preventive intervention for adolescents with attention-deficit/hyperactivity disorder. Cognitive and Behavioral Practice, 25(2), 225–239. doi: 10.1016/j.cbpra.2017.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer MC, Pettit JW, Waxmonsky JG, Gnagy E, Molina BS, & Pelham WE (2016). Does childhood attention-deficit/hyperactivity disorder (ADHD) predict levels of depressive symptoms during emerging adulthood? Journal of Abnormal Child Psychology, 44(4), 787–797. doi: 10.1007/s10802-015-0065-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, & Han B (2016). National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics, e20161878. doi: 10.1542/peds.2016-1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naicker K, Galambos NL, Zeng Y, Senthilselvan A, & Colman I (2013). Social, demographic, and health outcomes in the 10 years following adolescent depression. The Journal of Adolescent Health, 52(5), 533–538. doi: 10.1016/j.jadohealth.2012.12.016 [DOI] [PubMed] [Google Scholar]
- Nelson JM, & Gregg N (2012). Depression and anxiety among transitioning adolescents and college students with ADHD, dyslexia, or comorbid ADHD/dyslexia. Journal of Attention Disorders, 16(3), 244–254. doi: 10.1177/1087054710385783 [DOI] [PubMed] [Google Scholar]
- Nugent K, & Smart W (2014). Attention-deficit/hyperactivity disorder in postsecondary students. Neuropsychiatric Disease and Treatment, 10, 1781–1791. doi: 10.2147/ndt.s64136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overbey GA, Snell WE, & Callis KE (2009). Subclinical ADHD, stress, and coping in romantic relationships of university students. Journal of attention Disorders, 20, 1–12. [DOI] [PubMed] [Google Scholar]
- Adler LA, Chua HC, 2002. Management of ADHD in adults. The Journal of Clinical Psychiatry, 63(Suppl 12), 29–35. doi: 10.1177/1087054709347257 [DOI] [PubMed] [Google Scholar]
- Pine DS, Cohen E, Cohen P, & Brook J (1999). Adolescent depressive symptoms as predictors of adult depression: moodiness or mood disorder? American Journal of Psychiatry, 156(1), 133–135. doi: 10.1176/ajp.156.1.133 [DOI] [PubMed] [Google Scholar]
- Power TJ, Costigan TE, Eiraldi RB, & Leff SS (2004). Variations in anxiety and depression as a function of ADHD subtypes defined by DSM-IV: Do subtype differences exist or not?. Journal of Abnormal Child Psychology, 32(1), 27–37. doi: 10.1023/b:jacp.0000007578.30863.93 [DOI] [PubMed] [Google Scholar]
- Rabiner DL, Anastopoulos AD, Costello J, Hoyle RH, & Swartzwelder HS (2008). Adjustment to college in students with ADHD. Journal of Attention Disorders, 11, 689–699. doi: 10.1177/1087054707305106 [DOI] [PubMed] [Google Scholar]
- Rodríguez MR, Nuevo R, Chatterji S, & Ayuso-Mateos JL (2012) Definitions and factors associated with subthreshold depressive conditions: a systematic review. BMC Psychiatry, 12(181). 10.1186/1471-244X-12-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rucklidge JJ (2008). Gender differences in ADHD: implications for psychosocial treatments. Expert Review of Neurotherapeutics, 8(4), 643–655. doi: 10.1586/14737175.8.4.643 [DOI] [PubMed] [Google Scholar]
- Salla J, Galéra C, Guichard E, Tzourio C, & Michel G (2017). ADHD symptomatology and perceived stress among French college students. Journal of Attention Disorders, 14, 1711–1718. doi: 10.1177/1087054716685841 [DOI] [PubMed] [Google Scholar]
- Scallion LM, & Cummings JA (2018). Comparison of Team and Participant Ratings of Event Dependence: Inferential Style, Cognitive Style, and Stress Generation. Journal of Social and Clinical Psychology, 37(9), 697–724. doi: 10.1521/jscp.2018.37.9.697 [DOI] [Google Scholar]
- Seymour KE, Chronis-Tuscano A, Halldorsdottir T, Stupica B, Owens K, & Sacks T (2012). Emotion regulation mediates the relationship between ADHD and depressive symptoms in youth. Journal of Abnormal Child Psychology, 40, 595–606. 10.1007/s10802-011-9593-4 [DOI] [PubMed] [Google Scholar]
- Seymour KE, Chronis-Tuscano A, Iwamoto DK, Kurdziel G, & Macpherson L (2014). Emotion regulation mediates the association between ADHD and depressive symptoms in a community sample of youth. Journal of abnormal child psychology, 42(4), 611–621. 10.1007/s10802-013-9799-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein MJ, Faraone SV, Alperin S, Biederman J, Spencer TJ, & Adler LA (2018). How informative are self-reported adult attention-deficit/hyperactivity disorder symptoms? An examination of the agreement between the adult Attention-Deficit/Hyperactivity Disorder Self-Report Scale V1. 1 and adult Attention-Deficit/Hyperactivity Disorder Investigator Symptom Rating Scale. Journal of child and adolescent psychopharmacology, 28(5), 339–349. doi: 10.1089/cap.2017.0082 [DOI] [PubMed] [Google Scholar]
- Technow JR, Hazel NA, Abela JR, & Hankin BL (2015). Stress sensitivity interacts with depression history to predict depressive symptoms among youth: Prospective changes following first depression onset. Journal of Abnormal Child Psychology, 43(3), 489–501. doi: 10.1007/s10802-014-9922-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesselhoeft R, Sørensen MJ, Heiervang ER, & Bilenberg N (2013). Subthreshold depression in children and adolescents – a systematic review. Journal of Affective Disorders, 151(1), 7–22. doi: 10.1016/j.jad.2013.06.010 [DOI] [PubMed] [Google Scholar]
- Whisman MA, & Richardson ED (2015). Normative Data on the Beck Depression Inventory - Second Edition (BDI-II) in College Students. Journal of Clinical Psychology, 71(9), 898–907. doi: 10.1002/jclp.22188 [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tannock R, … & Lahey BB (2012). Validity of DSM-IV attention deficit/hyperactivity disorder symptom dimensions and subtypes. Journal of Abnormal Psychology, 121(4), 991. doi: 10.1037/a0027347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S (2000). ADHD children grown up: an empirical review. Counselling Psychology Quarterly, 13(2), 191–200. doi: 10.1080/09515070041172 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


