Abstract
Background:
This study was designed to evaluate the effectiveness of a yoga-based exercise program (YBEP) in improving glycemic control in people with type 2 diabetes mellitus.
Materials and Methods:
Patients on stable oral glucose-lowering agents for at least 3 months and HbA1c 7.5%–10% were randomized in 1:1 ratio. The primary outcome measure was the difference of change in mean HbA1c between groups.
Results:
The participants (n = 81) had mean (±standard deviation) age of 50.6 (±8.5) years and HbA1c of 8.5 ± 0.7% (68.97 ± 7.42 mmol/mol). The follow-up data were available in 96% (78/81) of participants. Of 40 participants, 25 (62.5%) attended ≥75% (≥10 out of 13) of the sessions in YBEP. On the intention to treat analysis, a favorable reduction (0.21% 95% confidence interval [−0.34, 0.75], P = 0.454) in HbA1c was seen in YBEP group as compared to usual care. The reduction in HbA1c by ≥0.5% was observed in 44.7% of participants in YBEP as compared to 37.5% in usual care arm, respectively. Those who attended ≥75% of the sessions had better HbA1c reduction of 0.3% in comparison to 0.1% reduction seen in those who attended <75% of the sessions.
Conclusions:
YBEP demonstrated a clinically relevant HbA1c reduction compared to usual care in participants who had attended at least 75% of the yoga sessions. The reduction in HbA1c by >0.5% in 44.7% in the yoga group, suggests, that it can be prescribed as an exercise to individuals who are unable to walk either due to limited joint mobility, adverse weather conditions, lack of space for walking, cultural or religious prohibitions for women for outdoor physical activity, and so on.
CTRI registration no: CTRI/2017/05/008564.
Keywords: Asia, diabetes, exercise, India, yoga
Introduction
Type 2 diabetes mellitus (T2DM) has become a major health burden, globally. India has nearly 73 million people affected with diabetes, and by 2045 the numbers are projected to increase to 134 million, which would make it a nation with the highest number globally.[1] Medical nutrition therapy and physical exercise are essential pillars for the management of diabetes.[2] However, adherence to these lifestyle measures has been sub-optimal in usual care for diabetes,[3] resulting in poor glycemic control and a higher rate of diabetes-related morbidity and mortality.[4]
To improve outcomes for individuals with diabetes, structured lifestyle intervention programs have been designed and evaluated in multiple regions, and shown to be effective in improving glycemic and other metabolic parameters.[5,6] However, in clinical practice, there are many people who are unable to incorporate physical activity (aerobic and resistance forms of exercise) regimen in their management plan for diabetes. The reasons may be due to limited joint mobility, adverse weather conditions, lack of space for walking, cultural or religious prohibitions for women for outdoor physical activity, and so on. Sohal et al., systematically reviewed studies representing perspectives of South Asian people on the barriers and facilitators for diabetes management.[7] South Asian individuals were concerned with the lack of gender-appropriate exercise facilities and fear of injury and the worsening of health with exercise. The key facilitator considered was the use of culturally appropriate exercises.
For the above reasons, it becomes important to consider alternative forms of exercise (such as yoga), which can overcome some of the above-mentioned limitations, and are also culturally acceptable not only in South Asia but increasingly in other parts of the world. Yoga, an ancient discipline aimed at balancing and harmonizing the body, mind, and emotions,[8] is recognized by the American Diabetes Association as one of the forms of exercise for people with diabetes.[9] However, till date, yoga has been evaluated with rigorous training sections and supervision in most of the studies, which limits the potential of scalability. In this study, we evaluated the yoga program, designed and delivered in a manner that has the potential of scalability.
In our study, we aimed to evaluate the yoga-based exercise program (YBEP), in individuals with T2DM who had poor glycemic control. We also evaluated a video-based lifestyle education program as an additional arm in this randomized control trial (RCT). We used the same usual care group, against which each of the two-lifestyle intervention arms were compared. This design gave us benefit as a smaller number of participants (25% less) had to be recruited (using the same usual group) with potential savings in cost and time. In this manuscript, we present and discuss the results of Yoga-based lifestyle education program as compared to usual care. The results of video-based lifestyle education program have been published recently.[10]
Materials and Methods
Settings and study design
This RCT was performed from June 2017 to October 2018 at the All India Institute of Medical Sciences (AIIMS), New Delhi, a tertiary care hospital in North India and was approved by the institutional ethics committee (IECPG-97/22.03.2017, RT-15/26.04.2017. Written informed consent was obtained from all participants. The trial registration number is CTRI/2017/05/008564.
Patient identification, recruitment, and procedure on the day of testing
Individuals with T2DM, diagnosed at ≥30 years of age, and those with HbA1c 7.5%–10% and on stable oral glucose-lowering agents for the past 3 months were eligible. Participants were advised to fast for at least 10 h and were evaluated for fasting plasma glucose, lipid profile, and HbA1c in the morning. Additional information such as demographics, relevant medical, and treatment history was collected. Weight, height, waist circumference, and blood pressure were recorded in the fasting state using standard methods.[11,12]
Randomization, allocation concealment, and blinding
Patients were randomized in a 1:1 ratio using block randomization with varying block size, by computer generated random numbers. Allocation concealment was done by using sequentially numbered opaque sealed envelopes. Since the intervention was apparent, the trial was open-labeled and nonblinded. However, an endpoint outcome assessment was done by a person who was unaware about the group of the patient to remove bias. The details of inclusion and exclusion criteria, biochemical measurements, and sample size calculations have been described in our previous publication.[10]
Intervention and usual care details
Yoga based exercise program
An integrated module [details provided in Tables 1 and 2] was formulated using specific asanas (yoga postures), kriyas (cleansing practices), pranayama (breathing exercises), and meditation. Yoga sessions were conducted at the Centre for Integrative Medicine and Research, AIIMS. Yoga therapists in the Centre conducted the yoga sessions, which were supervised by yoga physician.
Table 1.
Yoga teaching plan
| Phase | Weeks/months | Training sessions in hospital |
|---|---|---|
| Training phase | First 2 weeks | 3 classes/week |
| Supervision phase | Week 3 and 4 | 2 classes/week |
| Supervisor has seen if the participants were doing yoga correctly or not | ||
| Query phase/re-supervision phase | Month 2, 3, 4 (First week of each month) | One class/month |
| Supervisor has seen if the participants were doing yoga correctly or not and try to alleviate the queries |
Table 2.
Integrated yoga module
| Step | Practice | Rounds | Duration (min) |
|---|---|---|---|
| 1 | Starting prayer | 1 | |
| 2 | Breathing practices | ||
| Hands stretch breathing | 10 | 2 | |
| Hands in and out breathing | 10 | 2 | |
| Ankle stretch breathing | 10 | 1 | |
| Tiger breathing | 5 | 1 | |
| Straight leg raise breathing (both legs) | 5 | 2 | |
| 3 | IRT | 1 | |
| 4 | Loosening exercises | ||
| Slow jogging/drill walking | 50 | 2 | |
| Twisting | 10 | 1 | |
| 5 | QRT | 3 | |
| 6 | Yogasana standing | ||
| Ardhakati chakrasana | 1 | ||
| Ardha chakrasana | 1 | ||
| Vrikshasana | 1 | ||
| Trikonasana | 2 | ||
| Sitting | |||
| Vakrasana | 1 | ||
| Ardha-matsyendrasana | 1 | ||
| 7 | DRT | 7 | |
| 8 | Pranayama | ||
| Sectional breathing | 12 | 3 | |
| Nadisuddi pranayama | 9 | 2 | |
| Shitali/sitkari | 9 | 2 | |
| Bhramari | 1 | ||
| 9 | Meditation | ||
| Om meditation | 7 | ||
| Total | 45 |
IRT=Instant relaxation technique, QRT=Quick relaxation technique, DRT=Deep relaxation technique
The participants in the usual care arm were prescribed dietary advice by a registered dietician and 30 min of walking at a speed of 5–6 km/h for at least 5 days a week.
Statistical analysis
Stata 12.0 (College Station, Texas, USA) was used for statistical analysis. Pearson Chi-square and student's t-test were used to comparing categorical and continuous baseline variables among the groups. The primary outcome measure was the difference of change in mean HbA1c between groups. Intention to treat analysis was done for the primary outcome. The difference of change in secondary outcomes in the two groups was assessed using per protocol analysis. The adjustment for baseline serum triglyceride and total cholesterol levels was made in the adjusted analysis as it was different at baseline between the two arms. The results are reported as a difference in changes between the two groups (95% confidence interval [CI]). Data are presented as number (%), mean ± standard deviation (SD), or median (q25–q75) as appropriate. A value of P < 0.025 was considered statistically significant.
Results
Baseline characteristics
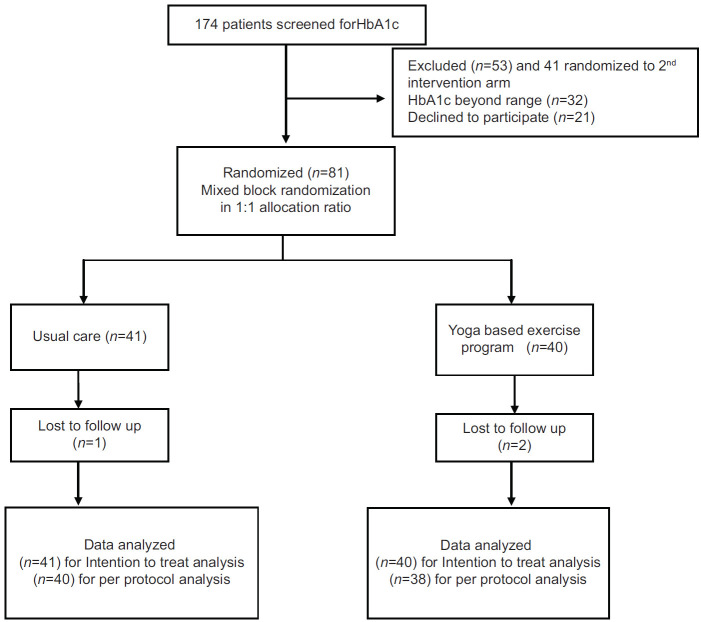
A total of 81 individuals were randomized, 41 participants in the usual care arm and 40 into YBEP arm. The participants (n = 81, women 44%) had mean (±SD) age of 50.6 (±8.5) years, HbA1c 8.5 ± 0.7% (68.97 ± 7.42 mmol/mol), and BMI (±SD) 27.9 ± 4.7 kg/m2. Family history of diabetes in first degree relatives was present in 69.1%, 42.0%, and 44.4% were on blood pressure and lipid-lowering medications, respectively. Twenty-seven individuals (33.3%) were taking >2 oral glucose-lowering agents. The main difference among the two study groups was in serum triglycerides (P = 0.041) and cholesterol (P = 0.025), which was adjusted during the intention to treat and per protocol analysis [Table 3]. Among 81 participants, 1 from usual care arm and 2 from YBEP were lost to follow-up [Figure 1, consort diagram]. Adherence was defined as ≥75% attendance to intervention (attending ≥10 out of 13 yoga sessions). Of 40 participants, 25 (62.5%) attended ≥75% of the sessions in YBEP.
Table 3.
Baseline characteristics of the participants
| Total (n=81) | Usual care (n=41) | YBEP (n=40) | P | |
|---|---|---|---|---|
| Age (years) | 50.6±8.5 | 50.2±8.6 | 51.1±8.6 | 0.636 |
| Male (%) | 45 (55.6) | 24 (58.5) | 21 (52.5) | 0.585 |
| Education, graduate and beyond (%)* | 35 (43.2) | 18 (43.9) | 17 (42.5) | 0.899 |
| Employed (%) | 40 (49.4) | 21 (51.2) | 19 (47.5) | 0.738 |
| Family h/o diabetes present (%) | 56 (69.1) | 26 (63.4) | 30 (75.0) | 0.259 |
| Anti-hypertensive drug (s) (%) | 34 (42.0) | 15 (36.6) | 19 (47.5) | 0.320 |
| Lipid lowering medication (%) | 36 (44.4) | 18 (43.9) | 18 (45.0) | 0.921 |
| Number of participants with oral glucose lowering agents >2 (%) | 27 (33.3) | 11 (26.8) | 16 (40.0) | 0.209 |
| Participants with diabetes related complication (s) (%) | 25 (30.9) | 12 (29.3) | 13 (32.5) | 0.753 |
| HbA1c (%) | 8.46±0.68 | 8.39±0.65 | 8.53±0.71 | 0.366 |
| HbA1c (mmol/mol) | 68.97±7.42 | 68.23±7.08 | 69.73±7.76 | 0.366 |
| Weight (kg) | 71.8±11.9 | 70.4±11.8 | 73.1±12.0 | 0.321 |
| Body mass index (kg/m2) | 27.9±4.7 | 27.1±4.1 | 28.8±5.2 | 0.116 |
| Waist circumference (cm) | 98.9±9.1 | 98.2±8.7 | 99.5±9.7 | 0.548 |
| Systolic blood pressure (mmHg) | 130.7±18.0 | 130.5±18.7 | 130.9±17.4 | 0.914 |
| Diastolic blood pressure (mmHg) | 83.5±8.5 | 83.0±9.1 | 84.1±8.0 | 0.557 |
| Fasting plasma glucose (mmol/L) | 8.6±1.9 | 8.4±1.5 | 8.9±2.3 | 0.235 |
| Total cholesterol (mmol/L) | 4.5±1.0 | 4.3±1.0 | 4.8±1.0 | 0.025 |
| Triglycerides (mmol/L) | 1.6 (1.3-2.1) | 1.5 (1.2-2.0) | 1.8 (1.4-2.4) | 0.041 |
| LDL cholesterol (mmol/L) | 2.5±0.8 | 2.4±0.7 | 2.7±0.8 | 0.171 |
| HDL cholesterol (mmol/L) | 1.1±0.3 | 1.1±0.3 | 1.1±0.2 | 0.544 |
*≥15 years of school/college/university education. Values expressed as n (%), mean±SD as appropriate. Triglycerides expressed as median (IQR). YBEP=Yoga based exercise program, LDL=Low density lipoprotein, HDL=High density lipoprotein, SD=Standard deviation, IQR=Interquartile range, HbA1c=Glycated haemoglobin
Figure 1.
Flowchart showing patient recruitment and follow up
Effect on the primary outcome measure
On intention to treat analysis, there was favorable difference (0.21% 95% C. I [−0.34, 0.75]; 2.24 mmol/mol 95% C. I.[−3.69,8.18], P = 0.454) in HbA1c in YBEP as compared to usual care [Table 4]. On further analysis, 6 (15%) participants from usual care, 10 (26.3%) from YBEP had HbA1c reduction of ≥1%. The reduction in HbA1c by ≥0.5% was observed in 44.7% participants in YBEP as compared to 37.5% in usual care arm. Those who were adherent had better HbA1c reduction of 0.3% in comparison to a 0.1% reduction in the nonadherent group.
Table 4.
Effect of intervention on HbA1c outcome (primary outcome) in YBEP vs usual care
| Usual care (n=41) | YBEP (n=40) | YBEP vs usual care Difference in difference (95% CI) | P | |
|---|---|---|---|---|
| At baseline (%) | 8.39±0.65 | 8.53±0.71 | ||
| After 4 months (%) | 8.38 ± 1.37 | 8.31 ±1.32 | ||
| Difference (%) | 0.01 ± 1.29 | 0.22 ±1.16 | 0.21 (-0.34,0.75) | 0.454 |
| 0.23 (-0.34,0.81)a | 0.424 | |||
| At baseline (mmol/mol) | 68.23±7.08 | 69.73±7.76 | ||
| After 4 months (mmol/mol) | 68.10±14.96 | 67.36±14.41 | ||
| Difference (mmol/mol) | 0.13±14.09 | 2.38±12.70 | ||
| 2.24 (-3.69,8.18) | 0.454 | |||
| 2.55 (-3.76,8.86)a | 0.424 | |||
| PP analysis: (n=78) (n=40) (n=38) | ||||
| At baseline (%) | 8.40±0.66 | 8.52±0.70 | ||
| After 4 months (%) | 8.38 ± 1.39 | 8.29 ± 1.34 | ||
| Difference (%) | 0.01±1.31 | 0.23±1.19 | 0.22 (-0.35,0.78) | 0.448 |
| 0.24 (-0.36,0.84)a | 0.427 | |||
| At baseline (mmol/mol) | 68.26±7.17 | 69.58±7.67 | ||
| After 4 months (mmol/mol) | 68.12±15.15 | 67.08±14.60 | ||
| Difference (mmol/mol) | 0.14±14.27 | 2.50±13.03 | 2.37 (-3.81,8.54) | 0.448 |
| 2.63 (-3.92,9.17)a | 0.427 |
YBEP: Yoga based exercise program, aAdjusted (for baseline triglycerideand cholesterol levels)
Effect on secondary outcome parameters
There was no change in any of the secondary outcome parameters in YBEP as compared to usual care [Table 5].
Table 5.
Effect of intervention on secondary outcomes at 4 months
| Usual care (n=40) | YBEP (n=38) | YBEP versus usual care Difference in (95% CI) | P | |
|---|---|---|---|---|
| HbA1c (%) | 8.38±1.39 | 8.29±1.34 | 0.24 (−0.36-0.84) | 0.427 |
| Weight (kg) | 70.0±11.7 | 72.4±12.2 | −0.10 (−0.86-0.66) | 0.795 |
| Body mass index (kg/m2) | 27.0±4.0 | 28.6±5.4 | 0.01 (−0.32-0.33) | 0.955 |
| Waist circumference (cm) | 97.9±8.4 | 98.7±9.4 | 0.30 (−1.57-2.18) | 0.748 |
| Systolic blood pressure (mmHg) | 125.2±14.2 | 127.4±13.7 | −1.21 (−9.05-6.63) | 0.759 |
| Diastolic blood pressure (mmHg) | 80.6±7.6 | 84.2±8.8 | −2.80 (−6.74-1.13) | 0.160 |
| FPG (mmol/L) | 8.5±2.8 | 8.7±3.1 | 0.38 (−0.91-1.67) | 0.557 |
| Total cholesterol (mmol/L) | 4.2±1.0 | 4.7±1.1 | −0.11 (−0.47-0.25) | 0.540 |
| Triglycerides (mmol/L) | 1.5 (1.1-2.0) | 1.9 (1.3-2.5) | ||
| LDL cholesterol (mmol/L) | 2.4±0.8 | 2.7±0.9 | −0.05 (−0.34-0.24) | 0.713 |
| HDL cholesterol (mmol/L) | 1.0±0.3 | 1.1±0.3 | −0.02 (−0.10-0.06) | 0.577 |
Values adjusted for baseline triglyceride, total cholesterol levels observed at baseline. LDL=Low density lipoprotein, HDL=High density lipoprotein, CI=Confidence interval, YBEP=Yoga-based exercise program, HbA1c=Glycated haemoglobin, FPG=Fasting plasma glucose
Discussion
In this trial, we evaluated the effect of a YBEP delivered over 13 sessions in participants with T2DM having poor glycemic control. We found a favorable reduction in HbA1c in YBEP as compared to usual care.
Yoga-based exercise program led to a reduction (0.21% 95% C. I. [−0.34, 0.75]; 2.24 mmol/mol 95% C. I. [−3.69, 8.18], P = 0.454) in HbA1c as compared to usual care. The reduction in HbA1c by more than 0.5% was seen in 44.7% of participants which was 7% more than that observed in the usual care arm. Given that people had to learn a new form of exercise, which was a novel introduction to their lifestyle, this level of HbA1c reduction at 4 months can be taken as clinically relevant. Cui et al. (2016) in a meta-analysis of 12 RCTs showed a pooled weighted mean difference of −0.47% (95% CI −0.87 to −0.07; P = 0.02) for HbA1c in yoga participants.[13] Subsequently, in a meta-analysis of 23 studies that evaluated different yoga components practiced over a median duration of 12 weeks, in comparison to the control group, yoga participants had a more favorable HbA1c reduction of 0.36% (95% CI = 0.16, 0.56; P < 0.001).[14] Jayawardena et al. (2018), reported results of a meta-analysis on eight studies (40 days to 9 months), including 6 RCTs, evaluating benefits of yoga practice compared to physical exercise in the management of type 2 diabetes.[15] Majority of studies had >75% attendance rate to yoga sessions. The HbA1c reduction observed was 0.39% (95% CI:–0.77, 0.00; P = 0.05) in yoga in comparison to control group. However, the results in their meta-analysis were driven by two trials, where yoga classes were nearly six times more as compared to yoga intervention in our study.[16,17] In the RCT reported by Vaishali et al., the average attendance rate was also 81.3% to yoga sessions.[17] Adherence to yoga sessions in our study was 62.5%. Those who were adherent had better HbA1c reduction of around 0.3% versus 0.1% reduction in nonadherent participants. It is possible that improving the attendance rate of training sessions, and supervision at home might increase the observed benefits of YBEP. However, this will also limit the potential for scalability. Furthermore, yoga, as such, is a broad area and includes components like yogic diet and instructions on other measures of life.[8] Our yoga module predominantly focused on physical activity. The inclusion of diet education could have enhanced the benefits of yoga practice. There was no significant change in secondary outcomes, consistent with what has been reported in the above meta-analysis.[15] Yoga being an art needs mastery through practice; hence, additional benefits may accrue over time.
The study results suggest that even limited sessions have the potential to provide benefits to the patient. This study will help in laying the basis of future studies, in which training sessions can be minimized, especially when imparted by tertiary care hospitals. However, supervision may have to be enhanced, preferably on the phone or watching some sessions through video consultations.
Strengths and limitations
This study has provided preliminary insights on the magnitude of effect that can be seen with different methods of education programs in people with diabetes and the scope of improvement in the formulation and delivery of the intervention. A key limitation of our study is the lack of long-term follow-up data as it is a pilot study of 4-months. Long follow-up periods may have different implications on outcomes and sustainability of benefits.
Conclusions
To conclude, YBEP is an effective strategy to achieve good glycemic control in people with type 2 diabetes in addition to usual care. The reduction in HbA1c by >0.5% in 44.7% in the yoga group, suggests, that it can be prescribed as an exercise to individuals who are unable to walk either due to limited joint mobility, adverse weather conditions, lack of space for walking, cultural or religious prohibitions for women for outdoor physical activity, and so on.
Future trials evaluating the combination of conventional forms of intervention and yoga, carried out over a longer period, in a larger population, can provide more insights into formulating effective means for improving outcomes of people with type 2 diabetes, especially in regions with a high burden and limited resources. It will also be important for future studies to evaluate which subset of patients gain maximum benefit from yoga and how. Similarly, it would be important to study the reasons why yoga does not show the desired benefits in some subgroups. It is equally important to understand the mechanism or physiological basis of benefit of yoga in diabetes. A holistic bedside to bench approach may help in the delineation of the biochemical effects and their clinical translation. This may set the stage of precision medicine for yoga in diabetes.
Financial support and sponsorship
Centre for Integrative Medicine and Research, All India Institute of Medical Sciences was partly funded under Centre of Excellence scheme, Ministry of Ayush, Government of India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to acknowledge the role of Centre for Integrative Medicine and Research, AIIMS in formulating the yoga module, conducting the yoga sessions and contributing to patient recruitment and data collection.
The authors are also thankful to Ankit Rajput, who provided technical assistance in carrying out this study. We are highly grateful to all the participants who gave their valuable time for this study
References
- 1.Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association 5. Lifestyle Management: Standards of medical care in diabetes-2019. Diabetes Care. 2019;42:S46–60. doi: 10.2337/dc19-S005. [DOI] [PubMed] [Google Scholar]
- 3.Gopichandran V, Lyndon S, Angel MK, Manayalil BP, Blessy KR, Alex RG, et al. Diabetes self-care activities: A community-based survey in urban southern India. Natl Med J India. 2012;25:14–7. [PubMed] [Google Scholar]
- 4.Khunti K, Ceriello A, Cos X, De Block C. Achievement of guideline targets for blood pressure, lipid, and glycaemic control in type 2 diabetes: A meta-analysis. Diabetes Res Clin Pract. 2018;137:137–48. doi: 10.1016/j.diabres.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Odgers-Jewell K, Ball LE, Kelly JT, Isenring EA, Reidlinger DP, Thomas R. Effectiveness of group-based self-management education for individuals with Type 2 diabetes: A systematic review with meta-analyses and meta-regression. Diabet Med. 2017;34:1027–39. doi: 10.1111/dme.13340. [DOI] [PubMed] [Google Scholar]
- 6.Huang XL, Pan JH, Chen D, Chen J, Chen F, Hu TT. Efficacy of lifestyle interventions in patients with type 2 diabetes: A systematic review and meta-analysis. Eur J Intern Med. 2016;27:37–47. doi: 10.1016/j.ejim.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Sohal T, Sohal P, King-Shier KM, Khan NA. Barriers and facilitators for type-2 diabetes management in South Asians: A systematic review. PLoS One. 2015;10:e0136202. doi: 10.1371/journal.pone.0136202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raveendran AV, Deshpandae A, Joshi SR. Therapeutic role of yoga in type 2 diabetes. Endocrinol Metab (Seoul) 2018;33:307–17. doi: 10.3803/EnM.2018.33.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, et al. Physical activity/exercise and diabetes: A position statement of the American diabetes association. Diabetes Care. 2016;39:2065–79. doi: 10.2337/dc16-1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta U, Gupta Y, Jose D, Mani K, Jyotsna VP, Sharma G, et al. Effectiveness of a video-based lifestyle education program compared to usual care in improving HbA1c and other metabolic parameters in individuals with type 2 diabetes: An open-label parallel arm randomized control trial (RCT) Diabetes Ther. 2020;11:667–79. doi: 10.1007/s13300-020-00769-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Section 4: Guide to Physical Measurements (Step 2) [[Last accessed on 2019 Mar 31]]. Available from: https://wwwwhoint/ncds/surveillance/steps/Section%204%20Step%202%20Physical%20Measurementspdf .
- 12.Goyal A, Gupta Y, Kalaivani M, Sankar MJ, Kachhawa G, Bhatla N, et al. Concordance of glycaemic and cardiometabolic traits between Indian women with history of gestational diabetes mellitus and their spouses: An opportunity to target the household. Diabetologia. 2019;62:1357–65. doi: 10.1007/s00125-019-4903-4. [DOI] [PubMed] [Google Scholar]
- 13.Cui J, Yan JH, Yan LM, Pan L, Le JJ, Guo YZ. Effects of yoga in adults with type 2 diabetes mellitus: A meta-analysis. J Diabetes Investig. 2017;8:201–9. doi: 10.1111/jdi.12548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thind H, Lantini R, Balletto BL, Donahue ML, Blotcher ES, Bock BC, Scott-Sheldon LA. J.The effects of yoga among adults with type 2 diabetes: A systematic review and meta-analysis. Prev Med. 2017;105:116–26. doi: 10.1016/j.ypmed.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jayawardena R, Ranasinghe P, Chathuranga T, Atapattu PM, Misra A. The benefits of yoga practice compared to physical exercise in the management of type 2 Diabetes Mellitus: A systematic review and meta-analysis. Diabetes Metab Syndr. 2018;12:795–805. doi: 10.1016/j.dsx.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 16.Nagarathna R, Usharani MR, Rao AR, Chaku R, Kulkarni R, Nagendra HR. Efficacy of yoga-based life style modification program on medication score and lipid profile in type 2 diabetes – a randomized control study. Int J Diabetes Dev Ctries. 2012;32:122–30. [Google Scholar]
- 17.Vaishali K, Kumar KV, Adhikari P, UnniKrishnan B. Effects of yoga-based program on glycosylated hemoglobin level serum lipid profile in community dwelling elderly subjects with chronic type 2 diabetes mellitus-a randomized controlled trial. Phys Occup Ther Geriatr. 2012;30:22–30. [Google Scholar]