Abstract
Context:
Premature ejaculation (PME) is a common sexual disorder. Drugs used commonly used for its treatment have various side effects and disadvantages. Yoga is being increasingly studied in a variety of medical disorders with positive results. However, its evidence for patients with PME is very limited.
Aims:
The aims of this study were to investigate the effect of yoga on ejaculation time in patients with PME and to compare it with paroxetine.
Settings and Design:
This was a nonrandomized nonblinded comparative study in a tertiary care center.
Materials and Methods:
Among patients with PME, 40 selected paroxetine and 28 yoga. Intravaginal ejaculation latency time (IELT) was measured in seconds once before and three times after intervention.
Statistical Analysis Used:
Mean, standard deviation, paired and unpaired t-tests, and repeated measures ANOVA were used for statistical analysis.
Results:
IELT was significantly increased in both groups – paroxetine (from 29.85 ± 11.9 to 82.19 ± 32.9) and yoga (from 25.88 ± 16.1 to 88697 + 26.9). Although the effect of yoga was slightly delayed in onset, its effect size (η2 = 0.87, P < 0.05) was more than paroxetine (η2 = 0.73, P < 0.05). One-fifth of the patients in the paroxetine group (19.5%) and 8% in the yoga group continued to have the problem of PME at the end of the trial.
Conclusions:
Yoga caused improvement in both intravaginal ejaculation latency time and subjective sexual experience with minimal side effect. Therefore, yoga could be an easily accessible economical nonpharmacological treatment option for the patient with PME.
Keywords: Paroxetine, premature ejaculation, yoga
Introduction
Premature ejaculation (PME) is the most common sexual disorder of man that affects approximately 20%–30% of men at some point in their lifes.[1] A multinational survey conducted in a large sample of 12133 men reported the prevalence of PME 24.0% in the United States, 20.3% in Germany, and 20.0% in Italy.[2] Hospital-based studies in patients attending a sexual clinic in India have found the prevalence of 30% and 77.6%, respectively, in eastern India (Kolkata) and North India (Delhi).[3,4] Epidemiological studies conducted in the rural area of Haryana and Mysore reported the prevalence of PME 4.6% and 8.76%, respectively.[5,6]
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) defines PME as “A persistent or recurrent pattern of ejaculation occurring during partnered sexual activity within or approximately 1 min following vaginal penetration and before the individual wishes it. This symptom must have been present for at least 6 months and must experience on almost all (approximately 75%−100%) occasions of sexual activity. It causes clinically significant distress in the individual.”[7]
PME affects various aspects of a man's life such as health, emotions, and relationships.[8] It is particularly detrimental to his self-esteem and often leads to anxiety, embarrassment, and depressed feelings.[9]
Selective serotonin reuptake inhibitors (SSRIs), local anesthetics, phosphodiesterase inhibitors, and tramadol have commonly used drugs for the treatment of PME.[10]
Pharmacological treatment is not always effective and often leads to a variety of side effects such as headache, nausea, nasal congestion, flushing, dizziness, fatigue, and constipation.[11,12]
Moreover, they can adversely affect other phases of sexual cycle and therefore overall sexual experience.[10,13] For example, local anesthetics work quickly but can cause anorgasmia in both males and females because of penile hypoesthesia and vaginal numbness.[14] Among nonpharmacological interventions, psychological therapies such as psychoanalytical and behavioral therapies have not been found much effective for PME.[10,12,15]
Yoga is a very ancient interdisciplinary system of India and has been in practice from 2700 BC. Yoga therapy is defined as a form of treatment to practice meditation, breathwork, and asanas or poses with the goals of improving mental and physical health holistically.[16,17] The National Institutes of Health has recently reported that among natural and complementary therapies, yoga has the highest potential for growth.[18]
There are very few studies which have explored the effect of yoga in PME, and those tried to compare its effect to pharmacotherapy are minimal in number. This study tried to explore the effect of yoga on intravaginal ejaculation latency time (IELT) in patients with PME and also compared it to paroxetine, a commonly prescribed SSRI drug for this condition. For selecting useful yoga postures/techniques for PME patients in this study, investigators studied previous research, relevant yoga literature, and also consulted yoga experts.[19,20,21,22,23]
Materials and Methods
Sample and setting
Male individuals aged ≥18 years visiting the department of psychiatry and medicine for the problem of early ejaculation were approached for participation in the study. Inclusion criterion included the following: diagnosis of PME as per DSM-5, good general health with no clinically relevant abnormalities, heterosexual relationship with a consistent partner, willing to be sexually active during the study period, and tried investigational drug (paroxetine) within the past 1 month. The following subject was excluded from the study: use of any medication including psychotropics which may cause sexual dysfunction or are contraindicated or have a reported interaction with paroxetine; seropositive for the human immunodeficiency virus, hepatitis B surface antigen, or hepatitis C; a comorbid psychiatric condition which may either affect sexual functioning or their ability to adhere to study protocol; the history of alcohol dependence or nonalcohol psychoactive substance use disorder; and history of pelvic/retroperitoneal surgery or radiotherapy, multiple sclerosis, spinal cord injury.
Procedure
The flowchart of the study procedure is shown in Figure 1. After informed consent obtained, patients were given a choice to select the type of treatment (yoga or paroxetine 25–75 mg) for the treatment of PME. During the first 2 weeks (preparatory phase) of the study, individuals in both groups were educated about the study procedure and recording of IELT. Subjects who chose yoga as a treatment option were trained under the direct supervision ofa yoga expert. Patients in the yoga group were also provided pictures of yoga postures and audio-visual instructions in mobiles. During the next 12 weeks (intervention phase), participants were assessed at least three times at 4 weekly intervals (6 weeks, 10 weeks, and 12 weeks) with the recording of IELT and side effects of treatment.
Figure 1.
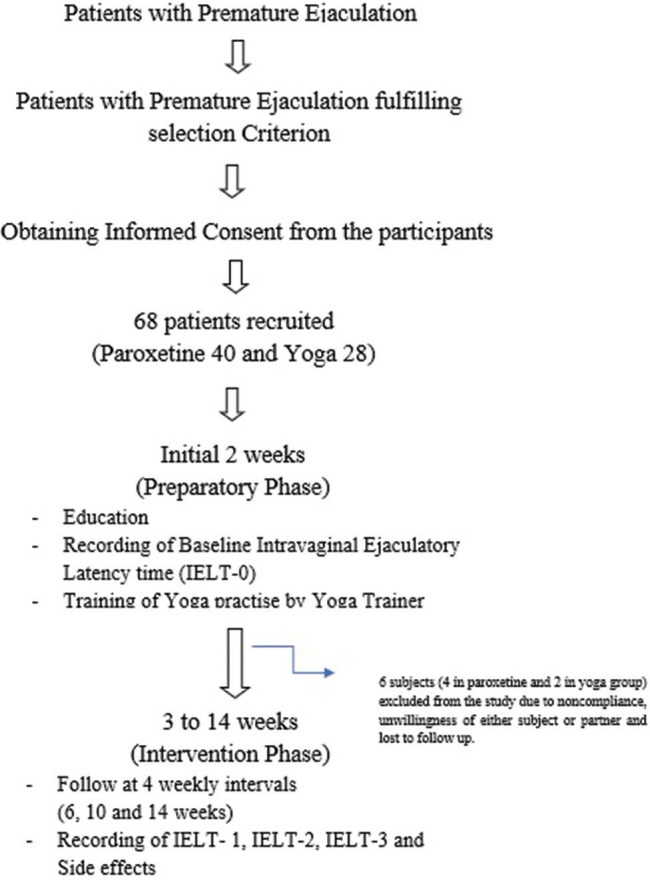
Study flowchart
Ethical consideration
The study was approved by the institutional ethics committee as a pilot study (letter no 5370-320/Academic-III/MCA/2017). Before data collection and intervention, the consent of both patient and his partner was obtained. No patient was coerced in any manner to participate in the study. They were informed about their right to withdraw from the study without any subsequent effect of their routine clinical care. The study followed a naturalistic observational design (nonrandomized nonblinded) where intervention applied was already in use as routine clinical practice and was based on participants' choice.
Results
Sixty-eight individuals participated in the study, and 62 completed the study. Six individuals were excluded from the study due to noncompliance, the unwillingness of either patient or partner, and lost to follow-up. Data could be obtained from 36 participants in the paroxetine group and 26 participants in the yoga group. Table 1 shows the yoga postures and techniques used in this study.
Table 1.
Yoga postures and techniques followed in the protocol
| Serial number | Name of yoga practice | Repetitions | Doses per day |
|---|---|---|---|
| 1 | Simhagarjanasana | Five times with 10 s Simha Mudra hold | Two times per day with empty stomach |
| 2 | Kashtha Takshanasana | Ten times | Two times per day with empty stomach |
| 3 | Malasana | Two times with 10 s posture hold | Two times per day with empty stomach |
| 4 | Uttanasana | Two times 10 s posture hold | Two times per day with empty stomach |
| 5 | Utthita Parsvakonasana | Two times with 10 s posture hold | Two times per day with empty stomach |
| 6 | Ekpad Rajkapot asana | Two times 10 s posture hold | Two times per day with empty stomach |
| 7 | Baddha Konasana | Two times 10 s posture hold | Two times per day with empty stomach |
| 8 | Janusirasana | Two times 10 s posture hold | Two times per day with empty stomach |
| 9 | Mandukasana | Two times 10 s posture hold | Two times per day with empty stomach |
| 10 | Nadi Shodhan pranayama | Five times | Three times per day with empty stomach |
| 11 | Bhramari pranayama | Five times | Three times per day with empty stomach |
| 12 | OM chanting | 8-10 times | Three times per day |
| 13 | Aswini mudra | Three times (10 s each time) | Three times per day |
| 14 | Vajroli mudra | Three times (10 s each time) | Three times per day |
| 15 | Yoga nidra (relaxation practice) | 10 to 15 min | Twice per day |
Patients in both the groups were comparable in terms of their age, and no difference was found in their mean age, t = 0.79, P = 0.43 [Table 2].
Table 2.
Comparison of age between the two groups
| Study group | Number of patients | Mean age±SD | Independent sample t-test | ||
|---|---|---|---|---|---|
| t | CI | P | |||
| Yoga | 26 | 30.38±4.79 | −0.793 | −3.439-1.486 | 0.431 |
| Paroxetine | 36 | 31.36±4.77 | |||
SD=Standard deviation, CI=Confidence interval
Mean IELTs of participants in both the groups are given in Table 3. Both the groups found an increase in their IELTs after the intervention phase started. Mean IELTs in both the groups at different time points in the study were significant as analyzed by repeated measures ANOVA: η2 = 0.870, P ≤ 0.005, and η2 = 0.729, P ≤ 0.005, respectively, in the yoga and paroxetine groups. A comparison of mean IELTs between the two groups did not find any significant difference during any time point in the study, P > 0.05.
Table 3.
Intravaginal ejaculation latency time in both the groups
| IELT | Mean (SD) | Independent sample t-test | |||
|---|---|---|---|---|---|
| Yoga | Paroxetine | t | CI | P | |
| Preintervention (0-2 week) | 25.88 (16.110) | 29.58 (11.876) | −1.041 | −10.803-3.405 | 0.302 |
| Postintervention 1 (6 weeks) | 49.19 (27.204) | 50.97 (27.486) | −0.253 | −15.870-12.310 | 0.801 |
| Postintervention 2 (10 weeks) | 78.38 (28.619) | 76.83 (32.326) | 0.195 | −14.323-17.426 | 0.846 |
| Postintervention 3 (12 weeks) | 88.69 (26.956) | 82.19 (32.926) | 0.826 | −9.245-22.241 | 0.412 |
| RMANOVA | |||||
| Wilks’ Λ | 0.130 | 0.271 | |||
| F (df, error df) | 51.320 (3, 23) | 29.580 (3, 33) | |||
| Partial η2 | 0.870 | 0.729 | |||
| P | <0.005 | <0.005 | |||
RMANOVA=Repeated measures ANOVA, IELT=Intravaginal ejaculation latency time, SD=Standard deviation, CI=Confidence interval
As shown in Figure 2, the effect of yoga on IELT was comparatively slower in onset in the first 8 weeks but comparable to paroxetine toward the end of the study. A comparison of mean IELTs before and after intervention found a significant difference in each group: Difference of means (DM) (standard deviation) 52.61 (5.4) s and 62.81 (4.9) s, respectively, in the paroxetine and yoga groups [Table 4].
Figure 2.
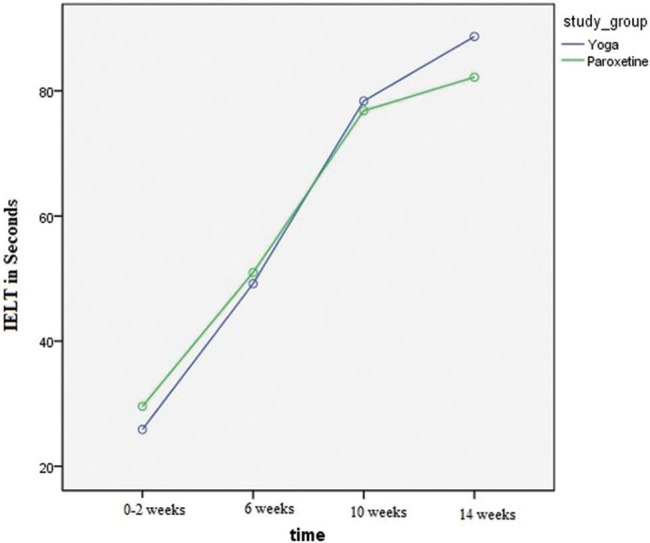
Intravaginal ejaculation latency times in both the groups
Table 4.
Comparison of pre- and postintervention intravaginal ejaculation latencies in both the groups
| Group | IELT (SD) | Paired sample t-test | |||
|---|---|---|---|---|---|
| Preintervention | Postintervention | Difference of mean (SEM) | t | P | |
| Paroxetine (n=36) | 29.58 (11.87) | 82.19 (32.93) | 52.611 (5.456) | 9.643 | <0.0001 |
| Yoga (n=26) | 25.88 (16.11) | 88.69 (26.95) | 62.808 (4.924) | 12.756 | <0.0001 |
SEM=Standard error of mean, IELT=Intravaginal ejaculation latency time, SD=Standard deviation
In nine participants (7 in the paroxetine group and 2 in the yoga group), IELT did not increase beyond 1 min. It means that 19.5% in the paroxetine group and 7.7% in the yoga group continued to have PME as per the DSM-5 criterion used in the study after the end of the study. Subjective sexual satisfaction and side effects experienced by participants in both the groups are shown in Table 5. Most of the patients, irrespective of intervention applied, found their sexual satisfaction either average or above average. More patients in the paroxetine group (22.2%) had below the average perception of sexual life than yoga (7.7%).
Table 5.
Subjective response regarding sexual life at the end of the study
| Paroxetine (n=36), n (%) | Yoga (n=26), n (%) | |
|---|---|---|
| Subjective sexual satisfaction level | ||
| Above average | 12 (33.3) | 14 (53.8) |
| Average | 16 (44.5) | 10 (38.5) |
| Below average | 8 (22.2) | 2 (7.7) |
| Adverse effects | Nausea: 8 (22.2) | Knee joint pain: |
| Dyspepsia: 3 (8.3) | 3 (11.4) | |
| Insomnia: 2 (5.6) | Perianal discomfort: | |
| Constipation: | 2 (7.7) | |
| 1 (2.8) | ||
| Anxiety: 6 (16.7) |
Discussion
PME is a common sexual disorder which adversely affects a different aspect of a man's life. Paroxetine is a commonly used SSRI used for the treatment of PME. However, like other drugs, it has many disadvantages in the form of negative effect on other phases of the sexual cycle, poor overall sexual experience, cost, frequent visits to hospital/clinic, side effects, and drug interaction in patients with medical comorbidities. This pilot study aimed to assess andcompare the effect of yoga with Paroxetine, a commonly used drug for treatment of patients with PME.
In our study, participants in the two groups were comparable in terms of their age and ejaculation time because no difference was found in comparing their mean age and preintervention IELT. This reduces the possibility of the effect of the above two factors (age and baseline ejaculation time) on the difference in their postintervention IELTs. Most of the participants in our study were in their thirties, as also found previously in both hospital-based prevalence and intervention studies among Indian patients with PME.[3,4,5,19]
There are no data to directly compare our findings as there is no previous study which compared yoga with paroxetine for the treatment of PME with measurement of IELT. Dhikav et al. compared yoga with fluoxetine in 65 males with PME and found that response in the yoga group was relatively delayed.[19] However, they did not find a significant increase in IELTs after intervention in both the groups before 8 weeks. However, in our study, the difference in mean IELTs in each group was significant at all points of measurement. The possible explanation could be the difference in frequency and type of yoga interventions. In our study, most of the yoga postures and mudras (such as Kashtha Takshanasana, Malasana, Baddha Konasana, and Vajroli mudra) were performed at least 2–3 times a day in sitting posture and involved activity of muscles of the pubic and perineal region. A study by Patil et al. comparing the effect of sitting and nonsitting yoga asanas also noticed that the former was more effective in increasing IELT in patients with PME.[22] It is important to mention that the above study included only 6 participants in each group (sitting and nonsitting). Participants in the yoga group in our study also performed yoga nidra which is known to reduced anxiety and stress.[24] PME patients commonly suffer from anxiety which is both effect and cause for PME.[8,9] This could explain above-average sexual satisfaction reported by more than half of subjects practicing yoga in our study.
Effect on IELT was more in the yoga group compared to paroxetine, as shown by effect size on repeated measures ANOVA and difference of mean. A similar finding was seen in the comparative study of fluoxetine and yoga.[19] Although the effect of yoga in patients with PME has also been seen in other studies, none of them compared it to pharmacotherapy.[20,22,23,25] Except few, most of these studies were of short duration, small sample size, and used questionnaire-based assessment tools. Ejaculation time is an essential part of the basic design of a PME trial irrespective of the type of intervention applied (pharmacotherapy, surgical, nonpharmacological).[26] Measurement of IELT, preferably by stopwatch technique, is considered as the most accurate and gold standard assessment method in PME.[27]
Although there are various explanations of how yoga affects sexual functioning, there is no exact mechanism which is uniformly accepted. Theories based on body–mind relationship proposes that yoga triggers neurohormonal mechanism leading to a reduction in the level of stress and thus improving sexual health.[28,29] Direct effects of yoga on sexual functions can be explained by its effect of suppressing sympathetic activity and activating parasympathetic activity. Physiological studies have demonstrated parasympathetic dominance in regular practitioners of yoga.[30,31] Yoga also increases the level of serotonin 5-hydroxytryptamine.[31] The above changes decrease the contraction of the epididymis, ejaculatory ducts, and seminal vesicles leading to enhanced ejaculatory control.[31,32]
Conclusions
The study demonstrated that yoga is effective in patients with PME. It was well tolerated and had minimal side effects with improvement in both intravaginal ejaculation latency time and subjective sexual experience. The results of this study can assist in future studies, particularly with respect to sample size and type of yoga intervention. It is needless to say that there are dire needs of further studies, particularly randomized to generate and strengthen the evidence of yoga in PME.
Strength
The study is an important step in the field of yoga's effect in patients with PME. During the preparation phase of the study (first 2 weeks), patients were educated about the study, how to record IELT, and trained in yoga protocol (only yoga group). The study used IELT as outcome measure which is the most accurate method for assessing effect in PME patients. The sample size was fairly adequate, considering it as a pilot study.
Limitation
This was a nonrandomized nonblinded comparative study, and intervention was based on patient choice. As this study was conducted in a tertiary care center, its findings cannot be generalized to the community population. This pilot study aimed to assess and compare the effect of yoga with Paroxetine, a commonly used drug for treatment of patients with PME. This study lasted for 14 weeks, and therefore, the long-term effect of yoga could not be observed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Montorsi F. Prevalence of premature ejaculation: A global and regional perspective. J Sex Med. 2005;2(Suppl 2):96–102. doi: 10.1111/j.1743-6109.2005.20369.x. [DOI] [PubMed] [Google Scholar]
- 2.Porst H, Montorsi F, Rosen RC, Gaynor L, Grupe S, Alexander J. The premature ejaculation prevalence and attitudes (PEPA) survey: Prevalence, comorbidities, and professional help-seeking. Eur Urol. 2007;51:816–23. doi: 10.1016/j.eururo.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Pal A, Mallik N, Acharya R, Mondal DK. Epidemiology of patients attending a special clinic on sexual dysfunction from Eastern India: A retrospective data review. Med J DY Patil Univer. 2017;10:542. [Google Scholar]
- 4.Verma KK, Khaitan BK, Singh OP. The frequency of sexual dysfunctions in patients attending a sex therapy clinic in North India. Arch Sex Behav. 1998;27:309–14. doi: 10.1023/a:1018607303203. [DOI] [PubMed] [Google Scholar]
- 5.Singh AK, Kant S, Abdulkader RS, Lohiya A, Silan V, Nongkynrih B, et al. Prevalence and correlates of sexual health disorders among adult men in a rural area of North India: An observational study. J Family Med Prim Care. 2018;7:515–21. doi: 10.4103/jfmpc.jfmpc_348_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rao TS, Manohar JS, Raman R, Darshan MS, Tandon A, Karthik KN, et al. The prospective, 24-week assessment of cost-efficacy of and compliance to antidepressant medications in a rural setting (PACECAR) study. Indian J Psychiatry. 2017;59:157–63. doi: 10.4103/psychiatry.IndianJPsychiatry_202_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Arlington: American Psychiatric Association; 2013. [Google Scholar]
- 8.Sotomayor M. The burden of premature ejaculation: The patient's perspective. J Sex Med. 2005;2(Suppl 2):110–4. doi: 10.1111/j.1743-6109.2005.20371.x. [DOI] [PubMed] [Google Scholar]
- 9.Rust J, Golombok S, Collier J. Marital problems and sexual dysfunction: How are they related? Br J Psychiatry. 1988;152:629–31. doi: 10.1192/bjp.152.5.629. [DOI] [PubMed] [Google Scholar]
- 10.McMahon CG. Management of ejaculatory dysfunction. Intern Med J. 2014;44:124–31. doi: 10.1111/imj.12344. [DOI] [PubMed] [Google Scholar]
- 11.Chung E, Gilbert B, Perera M, Roberts MJ. Premature ejaculation: A clinical review for the general physician. Aust Fam Physician. 2015;44:737–43. [PubMed] [Google Scholar]
- 12.Gillman N, Gillman M. Premature Ejaculation: Aetiology and Treatment Strategies. Med Sci (Basel) 2019;7 doi: 10.3390/medsci7110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McMahon CG. Emerging and investigational drugs for premature ejaculation. Transl Androl Urol. 2016;5:487–501. doi: 10.21037/tau.2016.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martyn-St James M, Cooper K, Ren K, Kaltenthaler E, Dickinson K, Cantrell A, et al. Topical anaesthetics for premature ejaculation: A systematic review and meta-analysis. Sex Health. 2016;13:114–23. doi: 10.1071/SH15042. [DOI] [PubMed] [Google Scholar]
- 15.Kaplan HS, Kohl RN, Pomeroy WB, Offit AK, Hogan B. Group treatment of premature ejaculation. Arch Sex Behav. 1974;3:443–52. doi: 10.1007/BF01541164. [DOI] [PubMed] [Google Scholar]
- 16.Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4:49–54. doi: 10.4103/0973-6131.85485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Penman S, Cohen M, Stevens P, Jackson S. Yoga in Australia: Results of a national survey. Int J Yoga. 2012;5:92–101. doi: 10.4103/0973-6131.98217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leonard K. Yoga Shows Highest Growth in Natural Therapy. Washington: US News & World Report; [[Last accessed on 2020 May 28]]. Available from: http://wwwusnewscom/news/articles/2015/02/10/ yoga-shows-highest-growth-in-naturaltherapy . [Google Scholar]
- 19.Dhikav V, Karmarkar G, Gupta M, Anand KS. Yoga in premature ejaculation: A comparative trial with fluoxetine. J Sex Med. 2007;4:1726–32. doi: 10.1111/j.1743-6109.2007.00603.x. [DOI] [PubMed] [Google Scholar]
- 20.Dhikav V, Karmarkar G, Verma M, Gupta R, Gupta S, Mittal D, et al. Yoga in male sexual functioning: A noncompararive pilot study. J Sex Med. 2010;7:3460–6. doi: 10.1111/j.1743-6109.2010.01930.x. [DOI] [PubMed] [Google Scholar]
- 21.Muktibodhananda S. Hatha Yoga Pradipika. 2nd ed. Munger: Yoga Publications Trust; 2005. pp. 370–3. [Google Scholar]
- 22.Patil P, Makwana JJ, Thakare GV, Patil SP. Effect of sitting & nonsitting yoga asanas on premature ejaculation. Inventi Impact Sex Reprod. 2012;2012:204–8. [Google Scholar]
- 23.Mamidi P, Gupta K. Efficacy of certain yogic and naturopathic procedures in premature ejaculation: A pilot study. Int J Yoga. 2013;6:118–22. doi: 10.4103/0973-6131.113408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferreira-Vorkapic C, Borba-Pinheiro CJ, Marchioro M, Santana D. The Impact of Yoga Nidra and seated meditation on the mental health of college professors. Int J Yoga. 2018;11:215–23. doi: 10.4103/ijoy.IJOY_57_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Makwana JJ, Patil PJ. Premature ejaculation: A comparative analysis between yoga and stop-start method. Indian J Res Rep Med Sci. 2012;2:17–20. [Google Scholar]
- 26.McMahon CG. The design and methodology of premature ejaculation interventional studies. Transl Androl Urol. 2016;5:508–25. doi: 10.21037/tau.2016.03.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Waldinger MD, Zwinderman AH, Schweitzer DH, Olivier B. Relevance of methodological design for the interpretation of efficacy of drug treatment of premature ejaculation: A systematic review and meta-analysis. Int J Impot Res. 2004;16:369–81. doi: 10.1038/sj.ijir.3901172. [DOI] [PubMed] [Google Scholar]
- 28.Gupta N, Khera S, Vempati RP, Sharma R, Bijlani RL. Effect of yoga based lifestyle intervention on state and trait anxiety. Indian J Physiol Pharmacol. 2006;50:41–7. [PubMed] [Google Scholar]
- 29.Sengupta P, Chaudhuri P, Bhattacharya K. Male reproductive health and yoga. Int J Yoga. 2013;6:87–95. doi: 10.4103/0973-6131.113391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vandana B, Saraswathy L, Pillai GK, Sunadaram KR, Kumar H. Meditation induces a positive response during stress events in young Indian adults. Int J Yoga. 2011;4:64–70. doi: 10.4103/0973-6131.85487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu X, Fumoto M, Nakatani Y, Sekiyama T, Kikuchi H, Seki Y, et al. Activation of the anterior prefrontal cortex and serotonergic system is associated with improvements in mood and EEG changes induced by Zen meditation practice in novices. Int J Psychophysiol. 2011;80:103–11. doi: 10.1016/j.ijpsycho.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Shobitha M, Tyagi P, Kohli S. Impact of yoga on mind-body management and its possible scientific mechanisms. Indian J Clin Anat Physiol. 2016;3:391–4. [Google Scholar]


