Abstract
Background
The main barrier to the effective rheumatoid arthritis (RA) therapy is poor adherence. Coronavirus disease 2019 (COVID-19) pandemic have led to a significant change in the pattern and the number of medical visits. We assessed changing patterns of medical visits and no-show, and identified factors associated with no-show in patients with RA during COVID-19 pandemic.
Methods
RA patients treated with disease-modifying antirheumatic drugs at least 6 months who had been in remission or those with mild disease activity were observed for 6 months from February to July 2020. No-show was defined as a missed appointment that was not previously cancelled by the patient and several variables that might affect no-show were examined.
Results
A total of 376 patients and 1,189 appointments were evaluated. Among 376 patients, 164 patients (43.6%) missed appointment more than one time and no-show rate was 17.2% during COVID-19 pandemic. During the observation, face-to-face visits gradually increased and no-show gradually decreased. The logistic regression analysis identified previous history of no-show (adjusted odds ratio [OR], 2.225; 95% confidence interval [CI], 1.422–3.479; P < 0.001) and fewer numbers of comorbidities (adjusted OR, 0.749; 95% CI, 0.584–0.961; P = 0.023) as the independent factors associated with no-show.
Conclusion
Monthly analysis showed that the no-show rate and the pattern of medical visits gradually changed in patients with RA during COVID-19 pandemic. Moreover, we found that previous history of no-show and fewer numbers of comorbidities as the independent factors associated with no-show.
Keywords: COVID-19, No-show Patients, Rheumatoid Arthritis
Graphical Abstract
INTRODUCTION
Coronavirus disease 2019 (COVID-19) was first reported in China on December 31, 2019. Since then, it has spread throughout the world; consequently, the World Health Organization declared the COVID-19 outbreak as a pandemic on March 12. As of November 5, the pandemic disease had spread to 219 countries, resulting in approximately 48 million cases and over 1.2 million deaths.1 In Korea, the first case of COVID-19 was confirmed on January 20. As of November 6, there were 27,195 confirmed cases of COVID-19, with 476 deaths.2 Stay-at-home orders and social distancing compounded with COVID-19 concerns have caused significant disruptions in daily life. One notable effect is a change in the pattern and the number of medical visits. A study showed that the mean number of emergency department visits per week for the four weeks during the pandemic was significantly less than the four weeks prior to COVID-19 pandemic.3 A study conducted in a spine clinic in Korea also reported that the number of patients visiting outpatient clinics and the emergency department a day had been steadily decreasing since January and the decrease was statistically significant, compared to the previous 3 years.4
Rheumatoid arthritis (RA) is a chronic inflammatory disease characterized by synovial inflammation, which can lead to irreversible articular damage, a decrease in physical functioning and quality of life, and eventually increased healthcare expenditures.5,6 Disease-modifying antirheumatic drugs (DMARDs) are the cornerstone of RA treatment and are fundamental to prevent radiographic progression on long-term.5,7,8,9 Maximum treatment benefits can, however, only be achieved if patients adhere to their treatment.10
No-show (also commonly referred to as missed appointments) is a burden to essentially all healthcare systems, squandering revenue, cost and use of resources.11,12 It is well-known fact that no-show decreases the provider's productivity and efficiency capacity.13 It also negatively affects patients who keep their appointments, causing dissatisfaction with longer waiting time and lowering service quality.14,15 In addition to financial wasting for providers, non-attendance generates social costs related with unused staff time, ineffective use of equipment and possible misuse of patients' time.15 Many studies have examined variables contributing to no-show. These studies have shown factors such as lower socioeconomic status, race, younger age, lack of child care, transportation difficulties, being unemployed and receiving Medicaid to be associated with a lower attendance rate.16,17 In Korea, there was a cross-sectional survey study conducted with 775 human immunodeficiency virus (HIV)-infected patients. It was reported that 12.5% had missed a scheduled appointment for the past 12 months, and younger age and low socioeconomic status were strong predictors of missed appointment.18 Identification of such characteristics can facilitate targeted interventions that can potentially help reduced the no-show rate and subsequently improve treatment outcomes and conserve resources. To the best of our knowledge, there was no study focusing on the characteristics of no-show patients with RA.
The aims of this study were to assess changing patterns of medical visits and no-show, and to identify factors associated with no-show in patients with RA during COVID-19 pandemic.
METHODS
Participants
This prospective observational cohort study was originally designed to examine a no-show rate among patients with RA and associating factors in the rheumatology center of a local tertiary hospital in Korea during one year from May 2019. A total of 378 adults aged 19 years or older who were diagnosed with RA according to 2010 American College of Rheumatology/European League Against Rheumatism criteria19 between May 30, 2019 and December 30, 2019 were included. All patients had been treated with DMARDs more than 6 months prior to the participation and had remission or mild disease activity with a disease activity score 28 ≤ 3.2 at the time of the inclusion. However, there were changes in the pattern of medical visits and no-show rates after COVID-19 pandemic. Hence, we changed the purpose of study to assess changing patterns of medical visits and no-show, and to identify factors associated with no-show in patients with RA during COVID-19 pandemic between February 2020 and July 2020. Two patients dropped out before February 2020 and 376 patients were observed during the 6 months.
Definitions and variables
No-show was defined as a missed appointment that was not previously cancelled by the patient. If patients cancelled or delayed their appointments, these cases classified as not no-show. In Korea, telemedicine was prohibited before COVID-19 outbreak, but is temporarily allowed after March 2020. Face-to-face visits and telemedicine were classified as a group of show. Several variables that might affect no-show such as demographic factors, marital status, method of transportation, travel time to hospital and number of comorbidities (hypertension, hyperlipidemia, diabetes mellitus, cardiac disease and cerebrovascular disease) were examined. Prior no-show history (existence of previously missed appointments by the patient) was also evaluated. Moreover, factors associated with RA (disease duration, radiographic damage and treated with biologic or targeted synthetic DMARDs) were also examined. It was defined as radiographic damage, if joint erosion or narrowing were observed in the last image of patients.
Statistical analysis
All continuous variables (age, travel time to hospital, number of comorbidities and disease duration) were nonnormal distribution. Continuous variables were presented as medians (ranges) and categorical variables were presented as numbers and percentages. Mann-Whitney U test and χ2 analysis were used to measure differences between the groups. Multivariate analysis was performed employing a Cox's proportional hazard regression model. Multivariate models used a step-wise backward elimination procedure based on a likelihood ratio test with P values > 0.10 for removal and P values < 0.05 for the entry of variables. Statistically significant variable identified by univariate analysis were only included in the initial multivariate models. Variables with P values < 0.05 was considered statistically significant. All statistical calculations were performed using SPSS version 26 (SPSS Inc., Chicago, IL, USA).
Ethics statement
The present study was reviewed and approved by the Institutional Review Board of the Pusan National University Yangsan Hospital (approval No. 052019004). Informed consent was submitted by all subjects when they were enrolled.
RESULTS
A total of 376 patients and 1,189 appointments for 6 months were evaluated. Among 376 patients, 164 patients (43.6%) missed appointment more than one time and there were 204 no-shows (17.2%) during COVID-19 pandemic. The baseline characteristics of the patients are presented in Table 1. The median age of the patients was 57 years. The majority of the patients were female (79.3%) and married (91.8%). More patients came to the hospital by private car (66.5%) than by public transportation (30.6%) or on foot (2.9%), and the median travel time to the hospital was 40 minutes. The mean/median number of comorbidities was 0.6/0. A hundred twenty-three patients (32.7%) had a previous history of no-show. The median disease duration was 88 months and seventy-nine (21.0%) patients were treated with biologic or targeted synthetic DMARDs.
Table 1. Baseline characteristics of participants (n = 376).
| Characteristics | Values | |
|---|---|---|
| Age, yr | 57 (23–69) | |
| Sex, female | 298 (79.3) | |
| Marital status | ||
| Married | 345 (91.8) | |
| Unmarried | 31 (8.2) | |
| Transportation to hospital | ||
| Private car | 250 (66.5) | |
| Public transportation | 115 (30.6) | |
| Walking | 11 (2.9) | |
| Travel time to hospital, min | 40 (3–240) | |
| No. of comorbidities | 0 (0–5) | |
| Previous history of no-show | 123 (32.7) | |
| Characteristics of rheumatoid arthritis | ||
| Disease duration, mon | 88 (7–638) | |
| Radiographic damage | 166 (44.1) | |
| Biologic or targeted synthetic DMARDs | 79 (21.0) | |
Values are presented as median (range) or number (%).
DMARDs = disease-modifying antirheumatic drugs.
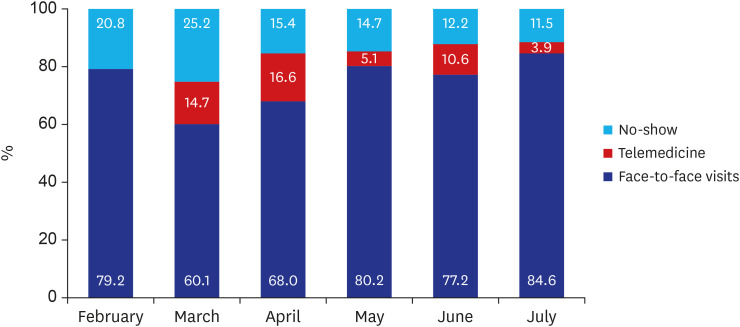
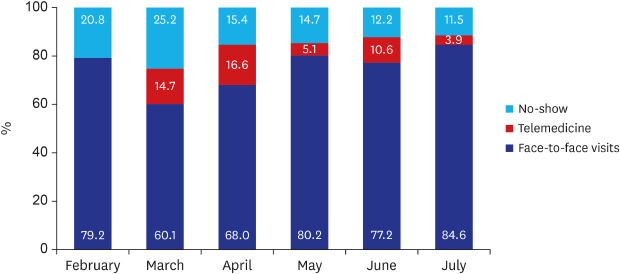
The 6-month observation revealed that face-to-face visits gradually increased and no-show gradually decreased. The percentages of face-to-face visits and no-show were 79.2% (152/192) and 20.8% (40/192) at February, 60.1% (143/238) and 25.2% (60/238) at March, 68.0% (164/241) and 15.4% (37/241) at April, 80.2% (142/177) and 14.7% (26/177) at May, 77.2% (183/237) and 12.2% (29/237) at June and 84.6% (88/104) and 11.5% (12/104) at July, respectively (Fig. 1).
Fig. 1. Changing patterns of medical visits and no-show rate during coronavirus disease 2019 pandemic.
Among 376 patients, 164 patients (43.6%) missed appointment more than one time. Differences in between the groups of no-show patients and show-up patients are presented in Table 2. No-show patients were younger (55 vs. 58 years, P = 0.041) than show-up patients and a private car was used more in the group of no-show patients (74.4 vs. 60.4%, P = 0.017). The number of comorbidities of no-show patients was significantly lower (P = 0.008) than that of show-up patients. Patients who had missed appointment were more likely to miss their appointment again comparing to patient who keep their appointment (42.7 vs. 25.0%, P < 0.001). Among factors associated with RA, there were no significant differences between the groups. The logistic regression analysis identified previous history of no-show (adjusted odds ratio [OR], 2.225; 95% confidence interval [CI], 1.422–3.479; P value < 0.001) and fewer numbers of comorbidities (adjusted OR, 0.749; 95% CI, 0.584–0.961; P value = 0.023) as the independent factors associated with no-show (Table 3).
Table 2. Differences in variables between the no-show patients and show-up patients.
| Characteristics | No-show (n = 164) | Show (n = 212) | P value | |
|---|---|---|---|---|
| Age, yr | 55 (23–69) | 58 (23–69) | 0.041 | |
| Sex, female | 131 (79.9) | 167 (78.8) | 0.793 | |
| Marital status | 0.856 | |||
| Married | 150 (91.5) | 195 (92.0) | ||
| Unmarried | 14 (8.5) | 17 (8.0) | ||
| Transportation to hospital | 0.017 | |||
| Private car | 122 (74.4) | 128 (60.4) | ||
| Public transportation | 38 (23.2) | 77 (36.3) | ||
| Walking | 4 (2.4) | 7 (3.3) | ||
| Travel time to hospital, min | 40 (3–150) | 40 (5–240) | 0.855 | |
| No. of comorbidities | 0 (0–5) | 0 (0–4) | 0.008 | |
| Previous history of no-show | 70 (42.7) | 53 (25.0) | < 0.001 | |
| Characteristics of rheumatoid arthritis | ||||
| Disease duration, mon | 88 (15–518) | 88 (7–638) | 0.994 | |
| Radiographic damage | 71 (43.3) | 95 (44.8) | 0.769 | |
| Biologic or targeted synthetic DMARDs | 36 (22.0) | 43 (20.3) | 0.694 | |
Values are presented as median (range) or number (%).
DMARDs = disease-modifying antirheumatic drugs.
Table 3. Independent factors associated with no-show.
| Characteristics | Adjusted odds ratio (95% CI) | P value | |
|---|---|---|---|
| History of no-show | 2.225 (1.422–3.479) | < 0.001 | |
| No. of comorbidities | 0.749 (0.584–0.961) | 0.023 | |
| Transportation to hospital | |||
| Private car | 1.805 (0.501–6.498) | 0.366 | |
| Public transportation | 0.928 (0.249–3.462) | 0.911 | |
| Age | 0.986 (0.962–1.010) | 0.250 | |
CI = confidence interval.
DISCUSSION
First, we assessed the no-show rate and changing patterns of medical visits in patients with RA during COVID-19 pandemic. Among total 1,189 appointments, the no-show rate was 17.2% (n = 204) for 6 months. This no-show rate was more than that prior COVID-19 pandemic. This rate is higher than the usual no-show rate prior to COVID-19 pandemic. Our unpublished data revealed that the no-show rate prior to COVID-19 pandemic was 10.0% (n = 128) between July 2019 and December 2019. Monthly analysis showed that the no-show rate and the pattern of medical visits gradually changed. Since the first confirmed COVID-19 case was reported in Korea on January 20, 2020, newly diagnosed cases continued to emerge mainly due to imported infections and secondary infection for the following months. After the nation's 31st patient was reported in one city on February 18, an exponential outbreak began to occur, starting with cluster infections related to the specific religious sect. At that time, Korea was on the verge of facing a continued surge in the COVID-19 outbreak with newly diagnosed cases per day amounting to 909, and there were 3,139 and 6,636 newly diagnosed cases in February and March, respectively.2 At that time, the no-show rate also rapidly increased in this study. The percentage of no-show was 20.8% in February and 25.2% in March. However, newly diagnosed cases gradually decreased owing to good compliance to preventative measures, active participation to extensive diagnostic testing for early detection and effective quarantine policy. There were 979 (April), 703 (May), 1331 (June) and 1506 (July) newly diagnosed cases in Korea and the no-show rate was 15.4% in April, 14.7% in May, 12.2% in June and 11.5% in July, respectively. Although the no-show rate is still higher than usual, the rate is gradually decreasing.
Secondly, we identified factors associated with no-show in patients with RA during COVID-19 pandemic. The previous history of no-show was the independent factor associated with no-show in this study which was consistent with previous studies: patients who had missed previous appointments were more likely to miss their next one.20,21,22,23,24 The type of disease and the investigated variables were different, but our previous study also reported that the previous history of non-persistence of urate-lowering therapy was the independent factor associated with non-adherence and non-persistence in patients with gout.25 Factors such as the patient's medical history and use of medication were also found to influence a no-show behavior in previous studies. Its effect was found to be dependent on the type of conditions; e.g., HIV patients were less likely to miss their appointments,26 while patients diagnosed with depression were more likely to no-show.27 Fewer numbers of comorbidities was the independent factor associated with no-show in this study. The number of comorbidities of no-show patients was significantly lower than that of the show-up patients. This is similar to the findings of previous studies related to adherence or persistence. Better adherence to medications in patients with multiple comorbidities was reported in many studies among patients with other chronic diseases. One possible explanation given for poorer adherence in patients with fewer comorbidities is the lack of experience in managing chronic diseases.25,28,29
This study has some limitations. First of all, it was conducted during COVID-19 pandemic. It is strength to evaluate changing patterns of medical visits during COVID-19 pandemic, but it is difficult to generalize no-show rate or the independent factors associated with no-show in other situations. Secondly, it was conducted with only RA patients. To our knowledge, it is the first study to evaluate no-show rate and independent factors associated with no-show in patients with RA, but it is also difficult to generalize with other diseases. Lastly, we could not identify reasons for no-show. We tried to ask and get some information about reasons for no-show during the follow-up period, but many participants refused to answer or simply answered “because of COVID-19” or “forgotten.” Further investigations are required.
Stay-at-home orders and social distancing compounded with COVID-19 concerns have changed in the pattern and number of medical visits. Although newly diagnosed cases is decreasing, considering that COVID-19 pandemic remained unresolved and therapeutic agents and vaccines have yet to be developed, it is meaningful to evaluate changing patterns of medical visits and no-show rate. Accurate assessment of no-show rate and its associated factors in a routine clinical setting is a necessary first step towards improving effectiveness to RA treatment. Physicians should emphasize the need for continuous medication use to their patients and modify no-show behaviors during follow-up appointments. Furthermore, predictive risk factors for no-show can be used to identify high risk patients. Interventions to decrease missed appointment should be implemented for high risk patients.
ACKNOWLEDGMENTS
We would like to acknowledge the invaluable collaboration of the rheumatology center nursing team of Pusan National University Yangsan Hospital.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kim Y, So MW.
- Data curation: Kim Y, Ahn EU.
- Methodology: Lee SG, Lim D-H.
- Writing - original draft: Ahn EU, So MW.
- Writing - review & editing: Kim AR, Lee SG.
References
- 1.World Health Organization. Coronavirus disease (COVID-2019) situation report-143. [Updated 2020]. [Accessed November 5, 2020]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 2.Korea Centers for Disease control and Prevention. Coronavirus disease-19 main website. [Updated 2020]. [Accessed November 6, 2020]. http://ncov.mohw.go.kr/en.
- 3.Boserup B, McKenney M, Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020;38(9):1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ham CH, Moon HJ, Kim JH, Park YK, Lee TH, Kwon WK. Coronavirus disease (COVID-19) outbreak and its impact on spinal daily practice: preliminary report from a single (regional) university hospital in Republic of Korea. J Korean Neurosurg Soc. 2020;63(4):407–414. doi: 10.3340/jkns.2020.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smolen JS, Landewé RB, Bijlsma JW, Burmester GR, Dougados M, Kerschbaumer A, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79(6):685–699. doi: 10.1136/annrheumdis-2019-216655. [DOI] [PubMed] [Google Scholar]
- 6.Lindqvist E, Jonsson K, Saxne T, Eberhardt K. Course of radiographic damage over 10 years in a cohort with early rheumatoid arthritis. Ann Rheum Dis. 2003;62(7):611–616. doi: 10.1136/ard.62.7.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weinblatt ME, Kremer JM, Bankhurst AD, Bulpitt KJ, Fleischmann RM, Fox RI, et al. A trial of etanercept, a recombinant tumor necrosis factor receptor:Fc fusion protein, in patients with rheumatoid arthritis receiving methotrexate. N Engl J Med. 1999;340(4):253–259. doi: 10.1056/NEJM199901283400401. [DOI] [PubMed] [Google Scholar]
- 8.Lipsky PE, van der Heijde DM, St Clair EW, Furst DE, Breedveld FC, Kalden JR, et al. Infliximab and methotrexate in the treatment of rheumatoid arthritis. N Engl J Med. 2000;343(22):1594–1602. doi: 10.1056/NEJM200011303432202. [DOI] [PubMed] [Google Scholar]
- 9.Keystone EC, Kavanaugh AF, Sharp JT, Tannenbaum H, Hua Y, Teoh LS, et al. Radiographic, clinical, and functional outcomes of treatment with adalimumab (a human anti-tumor necrosis factor monoclonal antibody) in patients with active rheumatoid arthritis receiving concomitant methotrexate therapy: a randomized, placebo-controlled, 52-week trial. Arthritis Rheum. 2004;50(5):1400–1411. doi: 10.1002/art.20217. [DOI] [PubMed] [Google Scholar]
- 10.Waimann CA, Marengo MF, de Achaval S, Cox VL, Garcia-Gonzalez A, Reveille JD, et al. Electronic monitoring of oral therapies in ethnically diverse and economically disadvantaged patients with rheumatoid arthritis: consequences of low adherence. Arthritis Rheum. 2013;65(6):1421–1429. doi: 10.1002/art.37917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alaeddini A, Yang K, Reddy C, Yu S. A probabilistic model for predicting the probability of no-show in hospital appointments. Health Care Manage Sci. 2011;14(2):146–157. doi: 10.1007/s10729-011-9148-9. [DOI] [PubMed] [Google Scholar]
- 12.Hallsworth M, Berry D, Sanders M, Sallis A, King D, Vlaev I, et al. Stating appointment costs in SMS reminders reduces missed hospital appointments: findings from two randomised controlled trials. PLoS One. 2015;10(9):e0137306. doi: 10.1371/journal.pone.0137306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peng Y, Erdem E, Shi J, Masek C, Woodbridge P. Large-scale assessment of missed opportunity risks in a complex hospital setting. Inform Health Soc Care. 2016;41(2):112–127. doi: 10.3109/17538157.2014.965303. [DOI] [PubMed] [Google Scholar]
- 14.Parikh A, Gupta K, Wilson AC, Fields K, Cosgrove NM, Kostis JB. The effectiveness of outpatient appointment reminder systems in reducing no-show rates. Am J Med. 2010;123(6):542–548. doi: 10.1016/j.amjmed.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 15.Bech M. The economics of non-attendance and the expected effect of charging a fine on non-attendees. Health Policy. 2005;74(2):181–191. doi: 10.1016/j.healthpol.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Odonkor CA, Christiansen S, Chen Y, Sathiyakumar A, Chaudhry H, Cinquegrana D, et al. Factors associated with missed appointments at an academic pain treatment center: a prospective year-long longitudinal study. Anesth Analg. 2017;125(2):562–570. doi: 10.1213/ANE.0000000000001794. [DOI] [PubMed] [Google Scholar]
- 17.Dantas LF, Fleck JL, Cyrino Oliveira FL, Hamacher S. No-shows in appointment scheduling - a systematic literature review. Health Policy. 2018;122(4):412–421. doi: 10.1016/j.healthpol.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 18.Kang CR, Bang JH, Cho SI. Factors contributing to missed visits for medical care among human immunodeficiency virus-infected adults in Seoul, Korea. J Korean Med Sci. 2018;33(42):e261. doi: 10.3346/jkms.2018.33.e261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO, 3rd, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–2581. doi: 10.1002/art.27584. [DOI] [PubMed] [Google Scholar]
- 20.Torres O, Rothberg MB, Garb J, Ogunneye O, Onyema J, Higgins T. Risk factor model to predict a missed clinic appointment in an urban, academic, and underserved setting. Popul Health Manag. 2015;18(2):131–136. doi: 10.1089/pop.2014.0047. [DOI] [PubMed] [Google Scholar]
- 21.Kempny A, Diller GP, Dimopoulos K, Alonso-Gonzalez R, Uebing A, Li W, et al. Determinants of outpatient clinic attendance amongst adults with congenital heart disease and outcome. Int J Cardiol. 2016;203:245–250. doi: 10.1016/j.ijcard.2015.10.081. [DOI] [PubMed] [Google Scholar]
- 22.Lee VJ, Earnest A, Chen MI, Krishnan B. Predictors of failed attendances in a multi-specialty outpatient centre using electronic databases. BMC Health Serv Res. 2005;5(1):51. doi: 10.1186/1472-6963-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cronin PR, DeCoste L, Kimball AB. A multivariate analysis of dermatology missed appointment predictors. JAMA Dermatol. 2013;149(12):1435–1437. doi: 10.1001/jamadermatol.2013.5771. [DOI] [PubMed] [Google Scholar]
- 24.Giunta D, Briatore A, Baum A, Luna D, Waisman G, de Quiros FG. Factors associated with nonattendance at clinical medicine scheduled outpatient appointments in a university general hospital. Patient Prefer Adherence. 2013;7:1163–1170. doi: 10.2147/PPA.S51841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee S, So MW, Ahn E. Long-term adherence and persistence with febuxostat among male patients with gout in a routine clinical setting. Mod Rheumatol. 2019;29(4):662–668. doi: 10.1080/14397595.2018.1483293. [DOI] [PubMed] [Google Scholar]
- 26.Ade S, Trébucq A, Harries AD, Ade G, Agodokpessi G, Wachinou P, et al. Follow-up and tracing of tuberculosis patients who fail to attend their scheduled appointments in Cotonou, Benin: a retrospective cohort study. BMC Health Serv Res. 2016;16(1):5. doi: 10.1186/s12913-015-1219-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Traeger L, O'Cleirigh C, Skeer MR, Mayer KH, Safren SA. Risk factors for missed HIV primary care visits among men who have sex with men. J Behav Med. 2012;35(5):548–556. doi: 10.1007/s10865-011-9383-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baggarly SA, Kemp RJ, Wang X, Magoun AD. Factors associated with medication adherence and persistence of treatment for hypertension in a Medicaid population. Res Social Adm Pharm. 2014;10(6):e99–112. doi: 10.1016/j.sapharm.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Rodriguez F, Cannon CP, Steg PG, Kumbhani DJ, Goto S, Smith SC, et al. Predictors of long-term adherence to evidence-based cardiovascular disease medications in outpatients with stable atherothrombotic disease: findings from the REACH Registry. Clin Cardiol. 2013;36(12):721–727. doi: 10.1002/clc.22217. [DOI] [PMC free article] [PubMed] [Google Scholar]