Abstract
Objective
This study examined the association between baseline substance use and mental health, and non-partner violence trajectories among youth presenting to an urban emergency department who screened positive for drug use. Non-partner violence is physically violent victimization or aggression involving someone other than a dating partner.
Methods
Group-based trajectory modeling was used to identify longitudinal trajectories of non-partner violence in N=599 youth (14–24 years old) at baseline, 6, 12, 18 and 24 month follow-ups. Multinomial logistic regression analyses were used to examine associations between baseline substance use and mental health conditions (i.e., anxiety, depression, and post-traumatic stress disorder [PTSD]), and non-partner violence trajectories.
Results
Six trajectory groups were identified for non-partner violence. Binge drinking and cannabis, illicit drug, nonmedical prescription stimulant, and polysubstance use in the 30 days leading up to their initial ED visit were associated with the likelihood of medium to high non-partner violence group membership during the two years following their ED visit. Post-traumatic stress disorder (PTSD) and depression/anxiety at baseline were also associated with greater risk of belonging to medium to high non-partner violence trajectory groups.
Conclusions
Our findings highlight distinct trajectories of violent behavior, with roughly 60% of young adults belonging to one of the non-partner violence groups. Although general trajectory trends were of decreasing violent behavior, the constellation of baseline risk factors differentially predicted group membership. These findings indicate that violence does not operate in a vacuum; interventions to reduce violence should also address previous trauma, substance use, and mental health issues.
Keywords: peer violence, youth violence, alcohol, marijuana, emergency department, Group-based trajectory modeling
1. Introduction
Youth violence is a serious public health issue associated with a myriad of adverse health concerns including injury, repeated involvement in violence, and mortality, with an estimated cost of 18 billion dollars annually in medical care and lost days of work (CDC, 2016). In 2014, over 500,000 youth were treated in hospital emergency departments (EDs) for physical assault injuries, with homicide being the third leading cause of death for those between 15–24 years of age (CDC, 2016). Ample evidence supports the association between substance use and youth violence and aggression (Cunningham et al., 2006; Epstein-Ngo et al., 2013; Rothman et al., 2012 Stoddard et al., 2015; White et al., 2012; Walton et al., 2009). Yet, less is known about the effect of substance use on the trajectories of youth violence over time in the presence of other risk factors such as mental health (e.g., anxiety or depression).
General criminological and developmental theories posit variations in individual’s trajectories of violence and other antisocial behaviors (which can include substance abuse), including differences in the onset, continuity, and severity of these behaviors (Moffitt, 1993). Moffit (1993) suggests that adolescent antisocial behavior and violent behavior in particular may have different patterns and therefore different antecedents. His developmental taxonomy of antisocial behavior suggests that violent behavior develops or desists across the life span due to individual differences in experiences and concomitant coping strategies, skills, and responses to perceived threats. Yet, although Moffit’s developmental taxonomy helps to raise the idea of change over time, he only identified two distinct categories of youth with unique etiology of antisocial and violent behavior. He also only focused on persistent and desisting groups, but it is possible that some youth start later or start and stop over time depending on several issues that include how well they navigate developmental milestones and what other experiences they have in their peer relationships, families, and neighborhoods. Nevertheless, Moffitt’s work direct us to consider the developmental nature and different possible trajectories of violent behavior.
Similarly, Problem Behavior Theory suggests that youth substance use and violence tend to co-vary and may also share common antecedents, resulting in a “syndrome of problem behaviors” (Jessor, 1991). Theoretically, substance use is also a risk factor for youth violence due to its acute and chronic pharmacological effects on individual functioning, such as reduced inhibition and disruption of cognitive processes (Chermack and Giancola, 1997; Ito et al., 1996; Pihl and Peterson, 1995; Rothman et al., 2012; Virkkunen and Linnoila, 1993). These theories are generally supported by research, with some unique findings based on the specific substance used. For example, daily calendar studies to examine within-day associations indicate that alcohol increases the risk for non-partner violence, whereas findings for marijuana are mixed (Stoddard et al., 2015). Preliminary research findings also suggest that use of opiates and sedatives is associated with violence perpetration and victimization (Epstein-Ngo et al., 2013; Stoddard et al., 2015; for a review, see McGinty, Choksy, & Wintemute, 2016). Longitudinal studies suggest reciprocal relationships between substance use and violence perpetration, with some studies finding substance use frequency or changes in use predicting later aggression among at-risk youth (White, Loeber, Stouthamer-Loeber, & Farrington, 1999; Xue, Zimmerman, & Cunningham, 2009; for reviews, Stoddard et al., 2015, White, 2002).
Mental health conditions such as post-traumatic stress disorder, anxiety, and depression are also associated with violent behavior. PTSD symptoms have been linked to more aggressive behavior among adolescents and young adults exposed to traumatic events (Jakupcak & Tull, 2005; Marsee, 2008) and among veterans (Taft et al., 2007). Furthermore, having a diagnosis of a drug use disorder and PTSD predicted future violent injury, as well as subsequent involvement in more severe forms of violence such as firearm violence (Carter et al., 2015). Other mental health disorders that effect social functioning, such as depression and anxiety, are also associated with aggressive behavior (Fava, 1998; Neumann et al., 2010).
High-risk urban youth seeking treatment in hospital EDs are more likely to report involvement with youth violence (Walton et al., 2009), substance use (Naeger, 2017), and mental health problems (Dorfman et al., 2010; Wilson & Klein, 2000). Yet, longitudinal studies examining trajectories of violence for youth presenting to urban emergency departments are generally lacking (for exception, see Heinze, Carter, et al., 2018). The present study has two aims: 1) to describe the non-partner violence patterns of high-risk youth presenting to an urban ED over 24 months; and 2) to examine baseline covariates of non-partner violence patterns, with particular examination of the relative contribution of substance use. We define non-partner youth violence as physical violent victimization or aggression involving someone other than a dating partner.
2. Methods
2.1. Procedures
Data are from the Flint Youth Injury (FYI) Study, a two-year longitudinal, observational study examining substance use and violence outcomes among drug-using youth treated in an urban ED. Participants were recruited at Hurley Medical Center (HMC), a Level 1 Trauma Center in Flint, Michigan between December 2009 and September 2011. The University of Michigan and HMC Institutional Review Boards approved all study protocols. A National Institute of Health Certificate of Confidentiality was obtained. Youth (14–24 years) being treated at the ED for assault were eligible for screening. Comparison youth who presented for non-assault-related complaints (e.g., abdominal pain, fever) were approached based on triage time, to mirror the proportion of participants in each age/sex group of assault-injured participants (See Bohnert et al., 2015). Patients in the assault-injured group and the comparison group completed screening and were enrolled in the longitudinal trial if they screened positive for past 6-month drug use. Those enrolling in the longitudinal trial then completed a baseline survey. Unstable trauma patients were re-approached for enrollment if they stabilized within 72 hours of their ED triage time. Patients presenting to the ED for an acute sexual assault, child abuse, suicidal ideation/attempt, or with medical conditions precluding consent (e.g., alcohol intoxication) were excluded. Non-English speaking youth (<1%) were also excluded.
Upon written consent from the patient (and parent/guardian consent with youth assent if age <18), participants self-administered a computerized screening survey (approximately 25 minutes) and received a $1.00 gift (e.g., keychain). Screened participants in the assault-injured and comparison group reporting past 6-month substance use on the ASSIST (i.e., marijuana, prescription stimulants, opioids, or sedatives/sleeping medication, cocaine, methamphetamine, heroin; World Health Organization ASSIST Working Group, 2002) were enrolled in the longitudinal study and completed a baseline assessment (approximately 90 minutes; $20 remuneration), urine drug screen ($5), and oral HIV testing ($5; not reported here). The baseline interview included self-administered and research assistant (RA) administered portions (e.g., Time Line Follow Back (TLFB) interview). Follow-up assessments at 6-, 12-, 18, and 24-months mirrored the baseline assessment, and took place at the study ED, community locations, the patient’s home or prison/jail (if incarcerated). Compensation consisted of $35 for 6-month, $40 for 12-month, $40 for 18-month, and $50 for 24-month follow-up.
2.2. Characteristics of Sample
Overall, 599 youth (Assault-injured Group=349; Comparison Group=250) were enrolled in the longitudinal study. Enrolled youth were mostly male (58.8%), African-American (58.3%), and 73.0% were in receipt of public assistance. As past 6-month drug use was an entry criterion, all youth in our sample reported recent drug use, with cannabis the most frequently reported drug (97%). Nearly half of the sample used cannabis around every other day on average in the thirty days leading up to their baseline ED visit. Half of the total sample met diagnostic criteria for a drug use disorder, and 20% met criteria for an alcohol use disorder. Among youth in the assault-injured group, most sustained injury from a blunt mechanism (i.e., struck by/against; n = 226 [64.8%]), firearm injury (n = 70 [20.0%]; mean ISS, 7.2), or cut/pierced wounds (n = 53 [15.2%]; mean ISS=2.2). Among youth in the comparison group, 61 (24.4%) presented for an unintentional injury, with the remaining participants (189 [75.6%]) seeking care for acute medical issues (Cunningham et al., 2014). Follow-up rates for the longitudinal study were 85.3%, 83.7%, 84.2%, and 85.3% at 6, 12, 18, and 24-months, respectively.
2.3. Measurement
2.3.1. Non-partner violence.
Past 6-month non-partner violence (e.g., violence that occurred with a friend, stranger, acquaintance, etc.) was assessed using a modified version of the physical assault scale of the Conflict Tactics Scale 2 (Straus et al., 1996), assessing frequency and severity of physical victimization (someone did the behavior to you) and aggression (you did the behavior to someone else). Severity of aggression or victimization was coded: moderate (pushed, grabbed or shoved, slapped) (assigned a value of 1 per act); severe (beat up, hit with a hard object, used a knife assigned a value of 2 per act); and shooting with or being shot by a gun (assigned a value of 3 per act), consistent with CTS-2 categories. The sum of these values was used to quantify the severity of non-partner violence for each respondent.
2.3.2. Substance use.
Drug and alcohol use for the 30 days leading up to and including the day of the ED visit were assessed using the Time Line Follow Back (TLFB) semi-structured interview in order to provide data regarding frequency of daily substance use (Maisto et al., 1979; Sobell et al., 1979, 1988). Use was assessed with monthly calendars beginning on (and including) the day of the baseline assessment and working backwards (Sobell et al., 1979). Data from the semi-structured interviews were coded for quantitative analysis. Participants reported past 30-day alcohol use (drinks per day); cannabis use; nonmedical use (i.e., to get high, taking someone else’s prescription, taking more than prescribed) of prescription stimulants, opioids, and sedatives/sleeping medication; and other illicit drug use (crack/cocaine, methamphetamine/speed, heroin/street opiates, LSD/other hallucinogens). Polysubstance use was defined as using two or more of any of these substances on a single day, excluding alcohol. Binge drinking was defined as drinking five or more drinks in one day, and was adjusted for in the analysis.
2.3.3. Mental Health Problems.
At baseline, depressive and anxiety symptoms in the past week were assessed with six items each from the Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983). For the purposes of this study, we created a four-level mental health indicator variable: (1) no anxiety or depression, (2) anxiety only, (3) depression only, or (4) both anxiety and depression. Mental health disorders were assessed using the MINI and MINI KID (version 6.0, 01/01/10; Sheehan et al., 1998; Sheehan et al., 2010), which was RA-administered. The presence or absence of posttraumatic stress disorder (PTSD) was assessed for the month prior to the ED visit, excluding the day of ED visit. Items for each disorder reflected DSM-IV diagnostic criteria.
2.3.4. Assault-Related Injury (baseline through two years).
At baseline, chart review data for current visit was abstracted from the ED medical record for all participants, including visit type (assault-related, non-assault related injury/medical).
2.3.5. Demographics.
Demographic items including age, sex, and race (Harris et al., 2003) were ascertained at baseline. Binary variables were created for race (African American = 0, Other Race = 1) and age (Ages 19–24 years = 0, and Ages 14–18 years = 1).
2.4. Analytic approach
Data were analyzed using Stata (version 13: traj plugin). First, group-based trajectory modeling was applied to determine the number of distinct trajectory patterns for non-partner violence. A zero inflated Poisson model was used, as a portion of participants reported no non-partner violence at certain time points. The zero inflated Poisson (ZIP) model was designed for the analysis of longitudinal count data that contains more zeroes than would be expected for a Poisson model (Jones and Nagin, 2013). In this study, the count data represented the number of non-partner violence acts perpetrated by or experienced by the participant in the past 6-months (weighted by severity), measured at 5 time points over the 24-month study. Models included quadratic terms to allow for non-linear trajectories. Model parameters were estimated using the maximum likelihood approach, which utilized all available data for parameter estimation. Non-partner violence trajectory group membership did not significantly co-vary with age, sex, or race, so these variables were excluded from the final models tested. From a series of fitted models with a different number of trajectory groups, the best model was selected based on the Bayesian Information Criterion (BIC; Schwarz, 1978).
Second, multinomial logistic regression analyses were conducted to examine potential relationships between non-partner violence trajectories and baseline substance use, mental health, and assault-related injury. The analyses included age, gender, and race/ethnicity as covariates to control for potential confounding effects. Model 1 adjusted for all of the variables listed under Model 1 in Table 2. Model 2, examining polysubstance use, also adjusted for binge drinking. Adjusted risk ratios of non-partner violence trajectories, given each type of substance used, mental health status, and assault-related injury status, were estimated.
Table 2:
Adjusted risk ratioa of non-partner violence trajectories over the two-year study, according to pattern of substance use and mental health at baseline, with the “Non-violent” trajectory (n=238, 39.7%) as the reference category for comparison (N=599)
| Outcome | |||||
|---|---|---|---|---|---|
| Baseline Variables | Low baseline initiators (group 1) (n=35, 5.8%) | Moderate baseline persistent (group 3) (n=126, 21%) | Moderate baseline desistance (group 4) (n=108, 18%) | High baseline desistance (n=57, 9.5%) (group 5) | High baseline persistent (n=35, 5.8%) (group 6) |
| Adjusted Risk Ratios (95% CI) | Adjusted Risk Ratios (95% CI) | Adjusted Risk Ratios (95% CI) | Adjusted Risk Ratios (95% CI) | Adjusted Risk Ratios (95% CI) | |
|
Model 1:
Past 30-Days Substance Use at Baseline |
|||||
| Binge Drinking Days | 1.05 (.92–1.20) | 1.12 (1.04–1.22) ** | 1.09 (1.00–1.18) * | 1.13 (1.04–1.23) ** | 1.18 (1.08–1.29) *** |
| Cannabis Days | 1.02 (.99–1.05) | 1.02 (1.00–1.04) | 1.02 (1.00–1.04) | 1.03 (1.00–1.06) * | 1.04 (1.00–1.07) * |
| Illicit Drugsb | 1.16 (.94–1.43) | 1.03 (.81–1.30) | 1.12 (.91–1.38) | 1.24 (1.02–1.51) * | .86 (.48–1.55) |
| Prescription Opioidsc | .002 (.00-.00) | 1.00 (.87–1.16) | .87 (.65–1.17) | .87 (.66–1.13) | .70 (.33–1.49) |
| Prescription Sedatives | 1.09 (.96–1.24) | 1.05 (.93–1.19) | .68 (.40–1.17) | 1.07 (.94–1.21) | 1.02 (.83–1.25) |
| Prescription Stimulants | .002 (.00-.00) | 1.04 (.53–2.05) | .002 (.00-.00) | 1.37 (.66–2.86) | 1.96 (1.03–3.75) * |
| Baseline Characteristics | |||||
| Adolescent vs. Adultd | 1.68 (.73–3.85) | 2.36 (1.40–3.97) ** | 1.77 (1.02–3.08) * | 2.34 (1.15–4.76) * | 2.33 (.99–5.46) |
| Female vs. Male | 1.21 (.57–2.58) | 1.01 (.63–1.63) | 1.15 (.70–1.89) | 1.34 (.70–2.56) | .89 (.40–1.98) |
| Other Race vs. African American | 1.78 (.85–3.74) | 1.55 (.97–2.49) | 1.10 (.67–1.82) | 1.41 (.74–2.68) | 1.25 (.57–2.74) |
| Assault-Related Injury | 1.44 (.69–3.00) | 2.02 (1.26–3.23) ** | 2.38 (1.45–3.92) * | 2.62 (1.32–5.20) ** | 1.38 (.63–3.01) |
| Baseline Mental Health | |||||
| Post-Traumatic Stress Disorder | 1.46 (.42–5.05) | 2.22 (1.00–4.89) * | 0.91 (.36–2.30) | 1.43 (.53–3.88) | 3.43 (1.14–10.33) * |
| (b) Depression but no Anxietye | 2.42 (.63–9.27) | 2.21 (1.00–4.88) | 1.27 (.48–3.34) | .62 (.11–3.42) | 2.24 (.47–10.77) |
| (c) Anxiety but no Depression | 2.30 (.47–11.37) | 2.26 (.89–5.74) | 2.84 (1.03–7.75) * | .40 (.04–4.20) | 4.37 (.92–20.78) |
| (d) Depression and Anxiety | 2.87 (.92–8.93) | 2.29 (1.19–4.39) * | 3.72 (1.84–7.50) *** | 4.17 (1.53–11.39) ** | 2.98 (.82–10.91) |
| Model 2: | |||||
| Polysubstance Use in the Past 30-Days? (Yes/No) | 1.05 (.34–3.27) | 1.99 (1.07–3.70) * | 1.44 (.72–2.88) | 2.67 (1.25–5.71) * | 2.90 (1.20–7.00) * |
=P<.05;
=P<.01;
=P<.001
Model 1 adjusted for each variable listed under Model 1. Model 2 examined whether each respondent engaged in polysubstance use with any of the following combination of substances: cannabis, prescription opioids, prescription sedatives, prescription stimulants, meth/speed, crack/cocaine, heroin/street opiates, and LSD/Hallucinogens. Model 2 adjusted for age group, gender, race/ethnicity, and assault-related injury at baseline.
Illicit drugs (crack/cocaine, heroin/street opiates, meth, LSD/Hallucinogens) were tested individually in Model 1. No individual illicit drug was significant, so the values were summed to create a composite variable.
References to prescription medication use are specifically to nonmedical use of the listed compounds.
Youth ages 14 – 18 were the reference group.
Reference group was participants reporting no symptoms of depression or anxiety.
3. Results
3.1. Non-Partner (i.e. Peer) violence trajectories from baseline to 24 months
We tested one-, two-, three-, four-, five-, six-, and seven-group-based trajectory models. The six-group solution proved to be the best fitting model (BIC = −12,637; AIC = −12,591; entropy = .96), as compared to the two-group (BIC = −18,568; AIC = −18,552), three-group (BIC = −15,751; AIC = −15,729), four group (BIC = −14,390; AIC = −14,357), and five-group (BIC = −13,424; AIC = −13,382) models. The seven-group model did not converge. For the six-group solution, four groups had moderate-to-high frequencies of non-partner violence initially (at baseline; Figure 1, Groups 3 – 6). A small percent of youth followed a pattern of high chronic non-partner violence throughout the study period (5.8%; high baseline persistent group; group 6). In contrast, 9.7% showed initially high levels of non-partner violence, yet by 6 months after their ED visit, showed a steep decline in non-partner violence and maintained lower levels of non-partner violence (high baseline desistance group, group 5). Eighteen percent followed a pattern of moderate non-partner violence initially that decreased to very low-to-no non-partner violence 6 months after their ED visit, and remained low throughout the study period (moderate baseline desistance group, group 4). Twenty-one percent had low-to-moderate levels of violence initially, then showed increased violence 6 months after their ED visit, followed by decreased levels over the remaining 18-month study period (moderate baseline persistent group; group 3). Two groups showed lower levels of non-partner violence at baseline. Approximately 40 percent followed a pattern of very low-to-no non-partner violence across the study period (non-violent group; group 2). Finally, 5.8% showed a steady increase in non-partner violence, with peak levels of non-partner violence at the final 24-month assessment period (low baseline initiators group; group 1).
Figure 1.
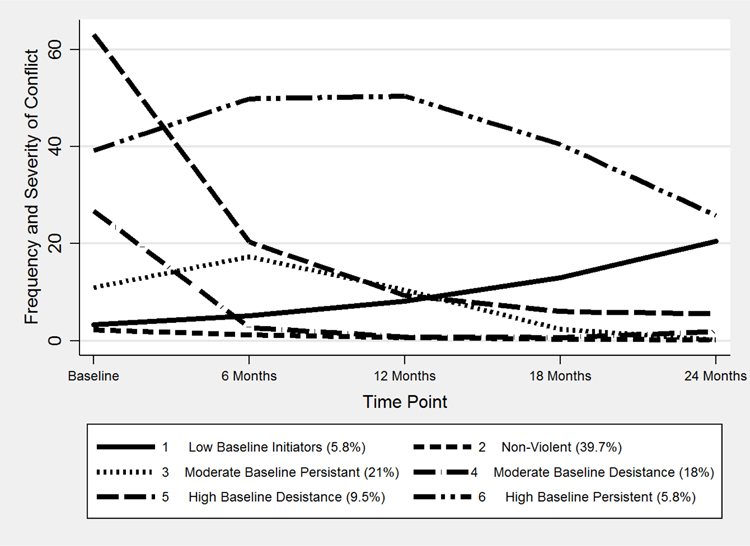
Group-based developmental trajectories of non-partner violence in a high-risk urban youth sample at their baseline Emergency Department visit and during the following 24-month period (N=599)a
a Percentages reported in the figure are percentages of the total sample. Baseline non-partner violence levels represent the frequency and severity of non-partner violence in the six months leading up to participants’ initial ED visit. Groups 1, 3, and 6 increased (P < .001). Groups 2, 4, and 5 decreased (P < .001). Groups 3, 4, 5, and 6 had curvilinear relationships (P < .001).
3.2. Risk ratios of non-partner violence trajectories given substance use and mental health at baseline
3.2.1. Substance use.
Model 1 adjusted for all of the variables listed under the model in Tables 1 and 2, including age, gender, race, and presenting to the ED with an assault-related injury at baseline. Youth who drank more than four drinks of alcohol per day (binge drank) on a greater number of days had a higher risk of belonging to any of the trajectory groups that had moderate-to-high levels of non-partner violence at baseline (groups 3 – 6; see Table 2). The comparison group (non-violent group, group 2) binge drank 3.2% of days, compared with 6.2% – 13.6% of days for the four moderate to high baseline trajectory groups (Table 1). A one-day increase in the number of days youth respondents used cannabis in the 30 days leading up to their baseline ED visit was associated with a greater risk of belonging to the high baseline groups (groups 5 and 6; Table 2). Youth in the high baseline groups used cannabis 58.9%–63.8% of the past 30 days; whereas the non-violent group used cannabis 45.8% of the past 30 days (Table 1). A one-day increase in illicit drug use was associated with 1.24 times the risk of belonging to the high baseline desistence group (group 5), while a one-day increase in nonmedical use of prescription stimulants was associated with nearly twice the risk of belonging to the high baseline persistence group (group 6).
Table 1:
Across non-partner violence trajectories over the two-year study, mean percentage of days of substance use, by substance, in the past 30-days at baseline, and percentage distribution by age group, gender, race, assault-related injury, PTSD, depression/anxiety, and polysubstance use at baseline (N = 599)
| Outcome | |||||||
|---|---|---|---|---|---|---|---|
| Baseline Variables | Non-violent group (or low) (group 2) (n=238, 39.7%) | Low baseline initiators (group 1) (n=35, 5.8%) | Moderate baseline persistent (Group3) (n=126, 21%) | Moderate baseline desistance (group 4) (n=108, 18%) | High baseline desistance (group 5) (n=57, 9.5%) | High baseline persistent (group 6) (n=35, 5.8%) | |
| Model 1: Past 30-Days-Substance-Use at Baseline | % of Days (SE) | % of Days (SE) | % of Days (SE) | % of Days (SE) | % of Days (SE) | % of Days (SE) | Chi-Square P Value b |
| Binge Drinking Days | 3.2% (.49) | 4.1% (1.96) | 8.2% (1.54) | 6.2% (1.42) | 10.0% (2.95) | 13.6% (3.77) | .001 |
| Cannabis Days | 45.8% (2.62) | 52.8% (7.23) | 54.3% (3.67) | 52.5% (3.87) | 58.9% (5.68) | 63.8% (6.87) | .079 |
| Illicit Drugs | 0.3% (.14) | 2.1% (1.74) | 0.6% (.40) | (.73) | 7.3% (3.93) a | 0.1% (.19) | .005 |
| Prescription Opioids | 0.7% (.38) | 0.0% (.00) | 1.6% (.88) | 0.3% (.15) | 0.5% (.42) | 0.4% (.47) | .785 |
| Prescription Sedatives | 0.5% (.21) | 2.8% (2.49) | 1.5% (.84) | 0.1% (.12) | 2.4% (1.7) | 1.5% (.86) | .304 |
| Prescription Stimulants | 0.0% (.07) | 0.0% (.00) | 0.1% (.10) | 0.0% (.00) | 0.1% (.17) | 0.8% (.85) | .088 |
| Baseline Characteristics | Count (%) | Count (%) | Count (%) | Count (%) | Count (%) | Count (%) | |
| Age14–18 vs. 19–24 c | 52 (21.8%) | 10 (28.6%) | 41 (32.5%) | 31 (28.7%) | 17 (29.3%) | 10 (28.6%) | .097 |
| Female vs. Male | 94 (39.5%) | 15 (42.9%) | 50 (39.7%) | 47 (43.5%) | 27 (46.6%) | 14 (40.0%) | .743 |
| Other Race vs. African American | 89 (37.4%) | 17 (48.6%) | 59 (46.8%) | 43 (39.8%) | 28 (48.3%) | 15 (42.9%) | .201 |
| Assault-Related Injury | 110 (46.2%) | 20 (57.1%) | 82 (65.1%) | 74 (68.5%) | 43 (74.1%) | 21 (60.0%) | < .001 |
| Baseline Mental Health | Count (%) | Count (%) | Count (%) | Count (%) | Count (%) | Count (%) | |
| Post-Traumatic Stress Disorder | 14 (5.9%) | 4 (11.4%) | 18 (14.3%) | 9 (8.3%) | 9 (15.5%) | 7 (20.0%) | .005 |
| (a) No Depression or Anxiety | 65 (27.3%) | 4 (11.4%) | 17 (13.5%) | 12 (11.1%) | 6 (10.3%) | 3 (8.6%) | |
| (b) Depression but no Anxiety | 41 (17.2%) | 6 (17.1%) | 20 (15.9%) | 9 (8.3%) | 3 (5.2%) | 4 (11.4%) | |
| (c) Anxiety but no Depression | 21 (8.8%) | 3 (8.6%) | 12 (9.5%) | 10 (9.3%) | 1 (1.7%) | 5 (14.3%) | |
| (d) Depression and Anxiety | 111 (46.6%) | 22 (62.9%) | 77 (61.1%) | 77 (71.3%) | 48 (82.8%) | 23 (65.7%) | < .001 |
| Model 2: Polysubstance Use in the Past 30-Days? | Count (%) | Count (%) | Count (%) | Count (%) | Count (%) | Count (%) | |
| Yes vs. No | 25 (10.5%) | 4 (11.4%) | 25 (19.8%) | 16 (14.8%) | 14 (24.6%) | 9 (25.7%) | .005 |
High-Decreasing Peer Conflict trajectory group illicit drug % of days breakdown: meth 0.0%, cocaine/crack 3.4%, heroin/street opiates 3.6%, and LSD/hallucinogens 0.1%.
Pearson Chi-Square tests for differences in distribution between the Low, Medium (combined), and High (combined) Peer Conflict groups.
Youth ages 14 – 18 were the reference group.
3.2.3. Mental Health Status.
Approximately a quarter of youth in the non-violent group (27.3%) reported no depressive or anxiety symptoms at baseline, while the proportion of those reporting no anxiety or depressive symptoms in the non-partner violence groups was much smaller (ranging 8.6% [high baseline persistence group] to 13.5% [moderate baseline persistence group], Table 1). Depression without anxiety was not a risk factor for violence, but respondents with anxiety symptoms and no depressive symptoms had more than twice the risk of belonging to the moderate baseline desistence group (group 4) (Table 2). Less than half of the youth in the non-violent group reported symptoms of both depression and anxiety (46.6%), while 61.6%–82.8% of respondents in the non-partner violent groups reported both types of symptoms (Table 1). Youth with a combination of depressive and anxiety symptoms had two- to four-times the risk of belonging to the moderate baseline persistence, moderate baseline desistence or high baseline desistence groups (groups 3 – 5, Table 2). Less than 6% of youth in the nonviolent group met the clinical criteria for post-traumatic stress disorder (PTSD), compared with 14.3% – 20% in the moderate baseline persistence, high baseline desistence and high baseline persistence groups (groups 3, 5–6, Table 1). Youth with PTSD at baseline had 2.2 times the risk of belonging to the moderate baseline persistence group, and 3.4 times the risk of belonging to the high baseline persistence group (Table 2).
Youth who presented with assault-related injuries at baseline had approximately twice the risk of belonging to the moderate baseline persistence, moderate baseline desistence, and high baseline desistence groups (groups 3–5), as compared to the non-violent group (Table 2).
3.3. Risk ratios of non-partner violence trajectories over time given polysubstance use at baseline
Model 2 examined the relationship between polysubstance use and non-partner violence, adjusting for binge drinking days, age, gender, and race/ethnicity. Approximately 1 in 10 respondents in the non-violent group engaged in polysubstance use, compared to approximately 25% in the high baseline groups (groups 5 & 6, Table 1). Youth who engaged in polysubstance use in the 30 days leading up to (and including) the day of their baseline ED visit had over two times the risk of belonging to the high baseline desistance and persistence groups (groups 5 & 6, Table 2).
4. Discussion
4.1. Main Findings
Our study contributes to a growing literature on identifying subgroups of youth violent offenders with different causes and correlates (DeLisi & Vaughn, 2014; Heinze, Carter, et al., 2018; Vaughn, et al., 2014). For the past fifty years, theorists and researchers have sought to identify distinct differences in both patterns of violent and antisocial behavior over time and factors that contribute to those differences in order to guide identification, prevention, and intervention efforts (DeLisi & Vaughn, 2014; Moffitt, 1993; White, 2002; Wolfgang, Figlio, and Sellin, 1972). Our findings are consistent with research in other samples of youth and young adults noting different developmental trajectories of non-partner violence were identified among high-risk youth (Brame, Nagin, & Tremblay, 2001; Moffitt, 1993; Moffitt, Caspi, Dickson, Silva, & Stanton, 1996; Raskin White, Bates, & Buyske, 2001; van der Geest, Blokland, & Bijleveld, 2009). Our high baseline persistent group is consistent with general criminological theories and the notion that there is a small subset of individuals who exhibit stable and persistent antisocial behaviors across the life course (i.e., life-course persistent) (Moffitt, 1993) and identified in other analyses as the severe 5% (Vaughn et al., 2011; Vaughn et al 2014). Although many respondents in our study were non-violent at baseline and throughout the study period, over half of the sample reported moderate to high levels of violence at baseline. For many of these initially violent respondents, violence desisted by the conclusion of the study and potentially reflects a temporary involvement in violence. This finding is consistent with Moffitt’s (1993) developmental taxonomy. Yet, about 6% of respondents continued to report high levels of non-partner violence across the two year period (i.e., high baseline persistent group) and an additional 6% of youth started with low levels of non-partner violence but showed patterns of high levels by the end of the study (i.e., low baseline initiator group). It is possible this low baseline initiator group falls within what Moffitt (1993) refers to as the adolescence-limited taxonomy and we observed them at a time of increased violent behavior. These findings all suggest the developmental nature of violent behavior and the notion that different trajectories may be a result of different experiences through the life course. Our results underscore the necessity of using a life course perspective for understanding youth violent as one model may not adequately fit youths’ experience. This also means that prevention strategies may also need to be tailored to address risks pertinent for different experiences.
The constellation of baseline risk factors examined in this study, including alcohol and drug use and PTSD, were differentially associated with non-partner violence groups. Binge drinking in the 30 days prior to participants’ ED visit (baseline) was associated with greater risk of belonging to any non-partner violence group, while marijuana use, illicit drug use, and misuse of prescription drugs were associated with an elevated risk of belonging to the group exhibiting high levels of non-partner violence at baseline (groups 5 and 6). This is not surprising, as previous research has linked alcohol and drug use to violent, aggressive, and antisocial behavior (Stoddard et al., 2015; Vaughn et al., 2011). For example, there is a strong link between alcohol use and the perpetration of violent behavior, particularly in the case of acute alcohol intoxication, which may be associated with cognitive deficits, reduced inhibition, and misperception of others’ behaviors (for review, Chermack & Giancola, 1997). Marijuana use in the present study was not associated with low or moderate levels of non-partner violence. This is consistent with laboratory studies on marijuana use and aggression (Myerscough & Taylor, 1985). Yet, marijuana use was associated with groups exhibiting high levels of non-partner violence. This may be explained by the notion that marijuana use may be occurring within contexts or situations prone to high levels of violent conflict (e.g., buying or selling illicit drugs; Goldstein, 1985), thus contributing to increased risk for violence perpetration or victimization. Furthermore, illicit drug use and prescription stimulant misuse has been linked to violent behavior in numerous studies (for review, White, 2002). In our study, polysubstance users had over two times the risk of belonging to the high baseline violence groups compared to the non-violent group, which is an important co-morbid risk behavior to address in interventions for violence. Further, future studies including daily assessments of substance use in relation to violence are warranted, as prior work has identified type of substance use differentially related to type of violence (e.g., non-partner violence was more likely on days when alcohol and non-medical sedatives were used; Stoddard et al., 2015).
PTSD symptoms at baseline were associated with a higher risk of belonging to the moderate persistent and high persistent groups. It is important to note that these trajectories were curvilinear; youth in both groups reported initial increases and later decreases in non-partner violence. Acute symptoms of PTSD at baseline may have led to violence in the period immediately following ED treatment. PTSD symptoms such as hyperarousal may contribute to an increased potential for violent aggression, while impaired processing, hypervigilance, and co-occurring substance use may decrease defensive signals that protect against victimization. (Orcutt et al., 2002; Rich and Sullivan, 2001). PTSD may also be associated with emotional dysregulation which can contribute to impulsive and aggressive behaviors (Miles et al., 2016; Weiss et al., 2012). In a sample of violent offenders, greater levels of emotion dysregulation were associated with higher psychopathic traits, especially lifestyle (i.e., impulsivity) traits (Garofalo et al., 2018). Poor temperaments, such as low effortful control (i.e., impulsivity) and negative emotionality (i.e., anger, frustration, depression) have also been associated with re-offending in juvenile justice-involved youth and incarcerated male violent offenders (Baglivio et al., 2016; Garofalo et al., 2017; Wolff et al., 2016). The eventual decrease in non-partner violence may reflect reductions in or stabilization of PTSD symptoms over time, however, more research is needed to explore this relationship overtime. Yet, our findings do indicate the importance of continued PTSD screening among high-risk youth during ED visits to reduce additional incidents of violence in the months immediately following their ED visit.
Subsequent involvement with peer violence over time, as demonstrated by youth in the moderate baseline persistence group (group 3) and high baseline persistent group (group 6), is important because one-third of assault-injured youth experience another violent injury requiring medical care within 2-years; twice the rate of a comparison sample of non-assault-injured drug-using youth (Cunningham et al., 2015). Further, among the baseline sample, almost half of those seeking care for assault indicated that they did not feel that the altercation prompting their visit was over, and almost a quarter indicated that they, or their friends or family would likely retaliate (Carter et al., 2017; Cunningham et al., 2014), increasing risk for involvement in the criminal justice system. This is consistent with prior research identifying the immediate post-ED time period as a high-risk time for retaliatory violence, as well as literature noting that retaliation is a key motivation for adolescent fighting behaviors (Carter et al., 2015; Copeland-Linder et al., 2012; Rich and Stone, 1996; Wiebe et al., 2011). Future research analyzing daily data could aid in clarifying if later violent events are related to retaliation for the assault that prompted the ED visit for assault at baseline. Regardless, these persistent violence groups may indicate greater anti-sociality, as a prior paper from this study showed that although membership in partner only, or non-partner only, violence was more common than involvement with both over time, antisocial personality disorder was associated with all violence types over time (Heinze, Cater, et al., 2018). Future studies should examine low effortful control and negative emotionality in relation to persistence of violence, particularly in the context of neighborhood disadvantage, exacerbate violence risk (DeLisi & Vaughn, 2014; Vaughn et al., 2011). Although ideally community-level interventions would mitigate such factors associated with youth violence (e.g., Branas et al., 2016; Heinze, Krusky-Morey, et al., 2018), individual efforts could also be provided, tailoring intervention content to focus on self-regulation and/or future orientation (Stoddard et al, 2015).
The findings highlight several potential avenues for intervention, including screening and brief intervention for substance use and mental health symptoms in the ED setting, and post ED treatment for substance use and mental health to alter the trajectory of non-partner violence. The ED is increasingly recognized as a setting in which high-risk youth can be engaged for further interventions, as these youth are often not enrolled in school, and typically do not have a primary care physician (Cunningham et al., 2010; Waldrop et al., 1996; Wilson and Klein, 2000) but are not yet engaged in the criminal justice system (Cunningham, 2014). Thus, presentation in the ED may be an optimal venue in which to initiate intervention efforts to prevent future violence, with the content and intensity of interventions requiring tailoring based on substance use severity (e.g., polysubstance use), as well as mental health factors such as PTSD, and comorbid depression and anxiety.
4.2. Limitations
Characteristics of our sample limit the generalizability of our findings. Our sample included only youth who reported past drug use or non-medical use of a prescription drug in the previous six months. Additionally, youth with assault-related injuries were oversampled. Thus, the high prevalence of substance use and assault-related injury in our sample does not reflect the general urban ED youth population. Yet, victimization more broadly is incredibly common among youth and young adults, even if not assault specifically. In addition, our sample was drawn from a single urban ED, so may not reflect youth presenting to other urban ED, and may not generalize to patients from other settings (e.g., suburban, rural). Data were based on self-report, however, several procedures shown to facilitate accuracy were used, including assurance of confidentiality, as well as collection of urine drug screens for substance use data (Brener, Billy, & Grady, 2003). Next, substance use and mental health were only examined at baseline. Although this advances our understanding of risk factors that may be predictive of differential patterns of violence among high-risk youth seeking treatment at urban EDs, examination of the longitudinal co-variation in these factors over time is needed. Finally, this paper focused on sub-groups of non-partner violence trajectories, but did not examine partner violence. Future papers examining sub-groups of partner violence are also warranted, as prior data from this study shows differences between substance use in relation to violence type at the daily level (Epstein-Ngo et al., 2014).
5. Conclusions
Distinct trajectories of violent behavior were identified among drug-involved youth who present to the ED, with 60% belonging to one of the non-partner violence groups, indicating that these young adults were exhibiting some pattern of non-partner violence victimization or aggression in the two years following the ED visit. Although general trajectory trends were of decreasing non-partner violence, the constellation of baseline risk factors (e.g., substance use and mental health) differentially predicted group membership, including groups with higher baseline non-partner violence even if their non-partner violence decreased after initial ED visit, and non-partner violence groups in which aggression remained steady or even increased over time. Our findings indicate that youth violence does not operate in a vacuum, and interventions to reduce violence also need to address other factors including previous trauma, mental health, and substance use. Future research should examine additional upstream factors, such as low effortful control and negative emotionality, to inform tailoring individual-level intervention content to enhance effects. Such interventions could be provided in concert with broader community-level interventions to reduce health disparities in youth violence (Heinze, Krusky-Morey, et al., 2018).
Highlights.
Results suggest six distinct patterns of non-partner violence over time with variability in timing and severity. Mental health and substance use were both consistent predictors of class membership.
Although about 6% of individuals continued to report high levels of non-partner violence across the two-year period (i.e., high baseline persistent group) and 6% of youth started with low levels of non-partner violence but showed patterns of high levels by the end of the study (i.e., low baseline initiator group), most individual’s involvement with violence decreased over time.
Post-traumatic stress disorder (PTSD) and comorbid depression and anxiety at baseline were associated with greater risk of belonging to medium to high non-partner violence trajectory groups.
Interventions to reduce violence should also address previous trauma, substance use, and mental health issues.
Acknowledgements:
The authors wish to acknowledge project staff, including Jessica Roche MPH, Linping Duan, MS, Sonia Kamat, and Wendi Mohl, BS, for their assistance in data and manuscript preparation. Finally, special thanks are owed to the patients and medical staff of the Hurley Medical Center (HMC) for their support of this project.
Funding Sources/Disclosures: This work was funded by NIDA R01 024646 and in part, by CDCP 1R49CE002099 and R03 HD083397. Dr. Stoddard was supported through NIH/NIDA K01 DA034765 at the time of this work. Dr. Ngo was supported by NIH/NIAAA K23 AA022641. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agencies. No honoraria, grants or other form of payment were received for producing this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: No conflict declared
References
- Baglivio MT, Wolff KT, DeLisi M, Vaughn MG, Piquero AR, 2016. Effortful control, negative emotionality, and juvenile recidivism: an empirical test of DeLisi and Vaughn’s temperament-based theory of antisocial behavior. J Forensic Psychol Res Pract. 27, 376–403. doi: 10.1016/j.ijlp.2018.01.006. [DOI] [Google Scholar]
- Bohnert KM, Walton MA, Ranney M, Bonar EE, Blow FC, Zimmerman MA, Booth BM, Cunningham RM, 2015. Understanding the service needs of assault-injured, drug-using youth presenting for care in an urban Emergency Department. Addict. Behav 41, 97–105. doi: 10.1016/j.addbeh.2014.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brame B, Nagin DS, Tremblay RE, 2001. Developmental trajectories of physical aggression from school entry to late adolescence. J Child Psychol Psychiatry. 42, 503–512. 10.1017/S0021963001007120 [DOI] [PubMed] [Google Scholar]
- Branas CC, Kondo MC, Murphy SM, South EC, Polsky D, & MacDonald JM, 2016. Urban blight remediation as a cost-beneficial solution to firearm violence. Am J Public Health. 106, 2158–2164. doi: 10.2105/AJPH.2016.303434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, Billy JO, Grady WR, 2003. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J. Adolesc. Heal 33, 436–457. doi: 10.1016/S1054-139X(03)00052-1 [DOI] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Goldstick J, Epstein-Ngo QM, Zimmerman MA, Mercado MC, … & Cunningham RM, 2017. Violent firearm-related conflicts among high-risk youth: An event-level and daily calendar analysis. Prev Med. 102, 112–119. doi: 10.1016/j.ypmed.2017.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Roehler DR, Goldstick J, 2015. Firearm Violence Among High-Risk Emergency Department Youth After an Assault Injury. Pediatrics 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center of Disease Control and Prevention, 2016. Youth violence: Facts at a glance. Retrieved 01/2019 from https://www.cdc.gov/violenceprevention/pdf/yv-datasheet.pdf.
- Chermack ST, Giancola PR, 1997. The relation between alcohol and aggression: an integrated biopsychosocial conceptualization. Clin. Psychol. Rev 17, 621–649. doi: 10.1016/S0272-7358(97)00038-X [DOI] [PubMed] [Google Scholar]
- Copeland-Linder N, Johnson SB, Haynie DL, Chung S, Cheng TL, 2012. Retaliatory Attitudes and Violent Behaviors Among Assault-Injured Youth. J. Adolesc. Heal 50, 215–220. doi: 10.1016/j.jadohealth.2011.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Carter PM, Ranney M, Zimmerman MA, Blow FC, Booth BM, Goldstick J, Walton MA, 2015. Violent Reinjury and Mortality Among Youth Seeking Emergency Department Care for Assault-Related Injury. JAMA Pediatr. 169, 63–70. doi: 10.1001/jamapediatrics.2014.1900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Ranney M, Newton M, Woodhull W, Zimmerman M, Walton MA, 2014. Characteristics of youth seeking emergency care for assault injuries. Pediatrics 133, e96–105. doi: 10.1542/peds.2013-1864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Resko SM, Harrison SR, Zimmerman M, Stanley R, Chermack ST, Walton MA, 2010. Screening Adolescents in the Emergency Department for Weapon Carriage. Acad. Emerg. Med 17, 168–176. doi: 10.1111/j.1553-2712.2009.00639.x ER [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham R, Walton M, Trowbridge M, Weber J, Outman R, Benway A, Maio R, 2006. Correlates of violent behavior among adolescents presenting to an urban emergency department. J. Pediatr 149, 770–6. doi: 10.1016/j.jpeds.2006.08.073 [DOI] [PubMed] [Google Scholar]
- DeLisi M, & Vaughn MG, 2014. Foundation for a temperament-based theory of antisocial behavior and criminal justice system involvement. J Crim Justice. 42, 10–25. [Google Scholar]
- DeLisi M, Fox BH, Fully M, & Vaughn MG, 2018. The effects of temperament, psychopathy, and childhood trauma among delinquent youth: A test of DeLisi and Vaughn’s temperament-based theory of crime. Int J Law Psychiatry. 57, 53–60. doi: 10.1016/j.ijlp.2018.01.006. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N, 1983. The Brief Symptom Inventory: an introductory report. Psychol. Med doi: 10.1017/S0033291700048017 [DOI] [PubMed]
- Dorfman DH, Trokel M, Lincoln AK, Mehta SD, 2010. Increased prevalence of behavioral risks among adolescent and young adult women with psychological distress in the emergency department. Pediatr Emerg Care. 26, 93–8. doi: 10.1097/PEC.0b013e3181cdb883. [DOI] [PubMed] [Google Scholar]
- Epstein-Ngo QM, Cunningham RM, Whiteside LK, Chermack ST, Booth BM, Zimmerman MA, Walton MA, 2013. A daily calendar analysis of substance use and dating violence among high risk urban youth. Drug Alcohol Depend. 130, 194–200. doi: 10.1016/j.drugalcdep.2012.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein-Ngo QM, Walton MA, Chermack ST, Blow FC, Zimmerman MA, Cunningham RM, 2014. Event-level analysis of antecedents for youth violence: Comparison of dating violence with non-dating violence. Addict Behav. 39, 350–353. doi: 10.1016/j.addbeh.2013.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fava M, 1998. Depression with anger attacks. J. Clin. Psychiatry, 59 Suppl 18, 18–22. [PubMed] [Google Scholar]
- Garofalo C, Neumann CS, Velotti P, 2018. Difficulties in emotion regulation and psychopathic traits in violent offenders. J Crim Justice. 57, 116–125. [Google Scholar]
- Garofalo C, Velotti P, 2017. Negative emotionality and aggression in violent offenders: The moderating role of emotion dysregulation. J Crim Justice. 51, 9–16. [Google Scholar]
- Harris KM, Florey F, Tabor J, Bearman PS, Jones J, Udry RJ, 2003. The National Longitudinal Study of Adolescent Health: Research Design [WWW Document]. URL http://www.cpc.unc.edu/projects/addhealth/design (accessed 9.7.17).
- Heinze JE, Carter PM, Ngo Q, Zimmerman MA, Walton MA, Cunningham RM, 2018. Patterns of Partner and Nonpartner Violence Among High-Risk Youth. J Adolesc Health. 62, 598–604. doi: 10.1016/j.jadohealth.2017.11.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinze JE, Krusky-Morey A, Vagi KJ, Reischl TM, Franzen S, Pruett NK, … Zimmerman MA, 2018. Busy Streets Theory: The effects of community-engaged greening on violence. Am J Community Psychol. 62, 101–109. doi: 10.1002/ajcp.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito T. a, Miller N, Pollock VE, 1996. Alcohol and aggression: a meta-analysis on the moderating effects of inhibitory cues, triggering events, and self-focused attention. Psychol. Bull 120, 60–82. doi: 10.1037/0033-2909.120.1.60 [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Tull MT, 2005. Effects of trauma exposure on anger, aggression, and violence in a nonclinical sample of men. Violence Vict. 20, 589–598. doi: 10.1891/vivi.2005.20.5.589 [DOI] [PubMed] [Google Scholar]
- Jessor R, 1991. Risk behavior in adolescence: A psychosocial framework for understanding and action. J. Adolesc. Heal 12, 597–605. [DOI] [PubMed] [Google Scholar]
- Jones BL, Nagin DS, 2013. A Note on a Stata Plugin for Estimating Group-based Trajectory Models. Sociol. Methods Res. 0, 1–6. doi: 10.1177/0049124113503141 [DOI] [Google Scholar]
- Maisto SA, Sobell MB, Cooper AM, Sobell LC, 1979. Test-retest reliability of retrospective self-reports in three populations of alcohol abusers. J. Behav. Assess 1, 315–326. [Google Scholar]
- Marsee MA, 2008. Reactive Aggression and Posttraumatic Stress in Adolescents Affected by Hurricane Katrina. J. Clin. Child Adolesc. Psychol 37, 519–529. doi: 10.1080/15374410802148152 [DOI] [PubMed] [Google Scholar]
- McGinty EE, Choksy S, Wintemute GJ, 2016. The Relationship Between Controlled Substances and Violence. Epidemiol. Rev 38, 5–31. doi: 10.1093/epirev/mxv008 [DOI] [PubMed] [Google Scholar]
- Miles SR, Menefee DS, Wanner J, Teten Tharp A, Kent TA, 2016. The relationship between emotion dysregulation and impulsive aggression in veterans with Posttraumatic Stress Disorder Symptoms. J Interpers Violence. 31, 1795–1816. 10.1177/0886260515570746 [DOI] [PubMed] [Google Scholar]
- Moffitt TE, 1993. Adolescence-limited and life-course-persistent antisocial behavior: A Developmental Taxonomy. Psychol Rev. 100, 674–701. [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Dickson N, Silva P, Stanton W, 1996. Childhood-onset versus adolescent-onset antisocial conduct problems in males: Natural history from ages 3 to 18 years. Dev Psychopathol. 8, 399–424. [Google Scholar]
- Myerscough R, Taylor SP., 1985. The effects of marijuana on human physical aggression. Journal of Personality and Social Psychology. 49, 1541. [DOI] [PubMed] [Google Scholar]
- Naeger S Emergency department visits involving underage alcohol use: 2010 to 2013. The CBHSQ Report: May 16, 2017. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD. [PubMed] [Google Scholar]
- Neumann ID, Veenema AH, Beiderbeck DI, 2010. Aggression and anxiety: social context and neurobiological links. Front. Behav. Neurosci 4, 12. doi: 10.3389/fnbeh.2010.00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orcutt HK, Erickson DJ, Wolfe J., 2002. A prospective analysis of trauma exposure: the mediating role of PTSD symptomatology. J Trauma Stress. 15, 259–266 [DOI] [PubMed] [Google Scholar]
- Pihl RO, Peterson JB, 1995. Alcoholism: The role of different motivational systems. J. Psychiatry Neurosci 20, 372–396. [PMC free article] [PubMed] [Google Scholar]
- Raskin White H, Bates ME, Buyske S, 2001. Adolescence-limited versus persistent delinquency: Extending Moffitt’s hypothesis into adulthood. J Abnorm Psychol, 110, 600–609. https://doi-org.proxy.lib.umich.edu/10.1037/0021-843X.110.4.600 [DOI] [PubMed] [Google Scholar]
- Rich JA, Stone DA, 1996. The experience of violent injury for young African-American men. J. Gen. Intern. Med 11, 77–82. doi: 10.1007/BF02599582 [DOI] [PubMed] [Google Scholar]
- Rich JA, Sullivan LM., 2001. Correlates of violent assault among young male primary care patients. J Health Care Poor Underserved. 12, 103–112 [DOI] [PubMed] [Google Scholar]
- Rothman EF, McNaughton Reyes L, Johnson RM, LaValley M, 2012. Does the alcohol make them do it? Dating violence perpetration and drinking among youth. Epidemiol. Rev 34, 103–119. doi: 10.1093/epirev/mxr027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz G, 1978. Estimating the dimension of a model. Ann. Stat 6, 461–464. doi: 10.1214/aos/1176344136 [DOI] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC, 1998. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 59. [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, Milo KM, Stock SL, Wilkinson B, 2010. Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). J. Clin. Psychiatry 71, 313–326. doi: 10.4088/JCP.09m05305whi [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla, a, 1988. Reliability of a timeline method: assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. Br. J. Addict 83, 393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM, 1979. Reliability of alcohol abusers’ self-reports of drinking behavior. Behav. Res. Ther 17, 157–160. doi: 10.1016/0005-7967(79)90025-1 [DOI] [PubMed] [Google Scholar]
- Stoddard SA, Heinze JE, Choe DE, Zimmerman MA., 2015. Predicting violent behavior: The role of violence exposure and future educational aspirations during adolescence. J Adolesc. 44:191–203. doi: 10.1016/j.adolescence.2015.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoddard SA, Epstein-Ngo Q, Walton MA, Zimmerman MA, Chermack ST, Blow FC, Booth BM, Cunningham RM, 2015. Substance use and violence among youth: a daily calendar analysis. Subst Use Misuse 50, 328–339. doi: 10.3109/10826084.2014.980953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB, 1996. The Revised Conflict Tactics Scale (CTS2). J. Fam. Issues 17, 283–316. [Google Scholar]
- Taft CT, Vogt DS, Marshall AD, Panuzio J, Niles BL, 2007. Aggression among combat veterans: Relationships with combat exposure and symptoms of posttraumatic stress disorder, dysphoria, and anxiety. J. Trauma. Stress 20, 135–145. doi: 10.1002/jts.20197 [DOI] [PubMed] [Google Scholar]
- van der Geest V, Blokland A, & Bijleveld C, 2009. Delinquent development in a sample of high-risk youth. J Res Crime Delinq. 46, 111–143. 10.1177/0022427808331115 [DOI] [Google Scholar]
- Vaughn MG, Salas-Wright CP, DeLisi M, & Maynard BR, 2014. Violence and externalizing behavior among youth in the United States: Is there a severe 5%?. Youth Violence Juv Justice. 12, 3–21. [Google Scholar]
- Vaughn MG, DeLisi M, Gunter T, Fu Q, Beaver KM, Perron BE, & Howard MO, 2011. The severe 5%: A latent class analysis of the externalizing behavior spectrum in the United States. J Crim Justice. 39, 75–80. doi: 10.1016/j.jcrimjus.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virkkunen M, Linnoila M, 1993. Serotonin in personality disorders with habitual violence and impulsivity. Ment. Disord. Crime
- Waldrop RD, Reine GM, Stuart MO, 1996. Influence of school enrollment on adolescent emergency department visits. J. Adolesc. Heal 19, 416–419. doi: 10.1016/S1054-139X(96)00031-6 [DOI] [PubMed] [Google Scholar]
- Walton MA, Cunningham RM, Goldstein AL, Chermack ST, Zimmerman MA, Bingham CR, Shope JT, Stanley R, Blow FC, 2009. Rates and Correlates of Violent Behaviors Among Adolescents Treated in an Urban Emergency Department. J. Adolesc. Heal 45, 77–83. doi: 10.1016/j.jadohealth.2008.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Ngo Q, Carter PM, Zimmerman MA, Blow FC, Buu A, Goldstick J, Cunningham RM, 2017. Marijuana use trajectories Among drug-using youth presenting to an urban emergency department: Violence And social influences. Drug Alcohol Depend. 173, 117–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Davis LT, Dehon EE, Fulton JJ, Gratz KL, 2012. Examining the association between emotion regulation difficulties and probable posttraumatic stress disorder within a sample of African Americans. Cogn Behav Ther. 41, 5–14. doi: 10.1080/16506073.2011.621970. [DOI] [PubMed] [Google Scholar]
- White HR, 2002. Longitudinal Perspective on Alcohol Use and Aggression during Adolescence, in: Recent Developments in Alcoholism. Springer US, Boston, MA, pp. 81–103. doi: 10.1007/0-306-47141-8_5 [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Blackstone MM, Mollen CJ, Culyba AJ, Fein JA, 2011. Self-reported Violence-related Outcomes for Adolescents Within Eight Weeks of Emergency Department Treatment for Assault Injury. J. Adolesc. Heal 49, 440–442. doi: 10.1016/j.jadohealth.2011.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson KM, Klein JD, 2000. Adolescents who use the emergency department as their usual source of care. Arch. Pediatr. Adolesc. Med 154, 361–365. [DOI] [PubMed] [Google Scholar]
- Wolff KT, Baglivio MT, Piquero AR, Vaughn MG, DeLisi M, 2016. The triple crown of antisocial behavior: Effortful control, negative emotionality, and community disadvantage. Youth Violence Juv Justice. 14, 350–366. [Google Scholar]
- Xue Y, Zimmerman MA, Cunningham R, 2009. Relationship between alcohol use and violent behavior among urban African American youths from adolescence to emerging adulthood: a longitudinal study. Am. J. Public Health 99, 2041–8. doi: 10.2105/AJPH.2008.147827 [DOI] [PMC free article] [PubMed] [Google Scholar]


