Abstract
Background:
Physical activity is strongly associated with lower risk of recurrent cardiac events in patients who experience an acute coronary syndrome (ACS), yet most patients do not meet recommended levels of physical activity. Psychological well-being is associated with higher levels of physical activity, but midlife adults experience a multitude of stressors that can reduce well-being. The aim of this study was to compare midlife (age 45–64) and older (age 65+) participants in a positive psychology (PP) intervention to increase physical activity and psychological well-being after an ACS.
Methods:
This was a secondary analysis across three phases of a telephone-delivered PP intervention development project. Participants were hospitalized for an ACS and had low pre-ACS health behavior adherence. They received 8–12 weekly intervention sessions. Psychological outcomes, self-reported adherence, and physical activity were measured pre- and post-treatment. Mixed regression models were used to compare session completion rates and change in outcome measures between midlife and older participants.
Results:
Across 164 participants, midlife participants showed larger improvements in depression, positive affect, and physical activity, but not anxiety or optimism, compared to older participants; session completion rates did not significantly differ.
Discussion:
Midlife patients post-ACS may be particularly responsive to a telephone-delivered PP intervention. Clinically, the post-ACS period may be uniquely motivating for midlife patients to improve their physical and psychological health. Future work could customize PP for unique midlife stressors.
Keywords: Midlife, health behaviors, physical activity, positive psychology, acute coronary syndrome
Introduction
Midlife, defined as the time period from age 45–64,1 is a critical life period related to the onset of cardiovascular disease. The median age of onset of multiple major cardiac risk conditions (e.g., hypertension, type 2 diabetes) is during midlife,2,3 and acute cardiac events, such as myocardial infarction, occur frequently during this life stage.4 Midlife individuals who experience these events are at high risk of recurrent cardiac events,5 making it critical to address cardiac health in midlife adults with prior cardiovascular events. Despite the existence of medications and interventions to manage cardiac risk factors and prevent recurrent events,6 rates of cardiac risk factor development are either not improving or increasing2,3 and rates of recurrent cardiac events remain high,5 underscoring the need for new programs to improve midlife cardiac health.
Health behaviors, such as diet, smoking, and physical activity, play a major role in the prevention of initial and recurrent cardiac events. Eating in line with a Mediterranean Diet (high in fruits and vegetables, whole grains, fish, and healthy fats) has been associated with reduced risk of recurrent heart disease,7 quitting smoking can reduce the death rate in cardiovascular disease patients by about 40%,8 and physical activity in midlife in particular is associated with both the prevention of heart disease and greater survival.9,10 However, adherence to such recommendations is low in midlife.1 For example, fewer than 10% of midlife adults achieve recommended levels of physical activity,11 and while it has improved somewhat over the past 20 years, dietary quality is still low in midlife adults.12 Making changes to health behaviors in midlife can be highly challenging, as midlife is a phase of life marked by a confluence of stressors, often financial, occupational, and due to caregiving, that place many under significant pressure and can interfere with the time and effort needed to make sustained health behavior change.13
Psychological well-being also likely plays a role in physical activity engagement and cardiovascular health in midlife. Many midlife adults experience low levels of positive psychological well-being,14 and across the lifespan well-being appears to be at its lowest during midlife.15,16 This has important health implications, as low optimism and positive affect are prospectively associated with less physical activity, less healthy diet, and lower smoking rates, along with higher rates of heart disease and cardiac mortality, independent of sociodemographic/medical factors, and above and beyond the adverse effects of depression.17–22
Given these connections, interventions that increase well-being have the potential to also improve health behavior adherence and cardiovascular health. Positive psychology (PP) interventions, which use specific, systematic exercises (e.g., performing kind acts, using personal strengths) to promote psychological well-being,23 are one promising option. These interventions have indeed been used successfully either alone or in combination with behavioral interventions like motivational interviewing24 in cardiac-related populations to improve well-being and promote physical activity.25–28 However, the utility of PP-based health behavior interventions in midlife adults—who have limited time and unique stressors—remains unknown.
Accordingly, we analyzed data from three phases of a PP intervention study in patients with acute coronary syndrome (ACS) to examine the efficacy of PP-based interventions to improve psychological well-being and health behavior adherence in midlife compared to older adults. Given the aforementioned challenges that commonly occur during midlife, we hypothesized that midlife participants would benefit less than older participants from these interventions as evidenced by lower session completion rates and smaller magnitude of improvement in psychological well-being components and health behavior adherence.
Material and Methods
Setting.
This analysis used data from three phases of Positive Emotions after Acute Coronary Events (PEACE), a project that utilized the Multiphase Optimization Strategy29 to develop and optimize a PP-based intervention to promote physical activity in post-ACS patients. The intervention was delivered by telephone and involved weekly instruction by a study trainer to complete PP activities with associated written materials. PP activities were based in gratitude (e.g., identifying positive events in the past week, expressing gratitude via a gratitude letter), strengths (e.g., remembering a past success, identifying and using a personal strength), and meaning (e.g., planning and engaging in acts of kindness, enjoyable and meaningful activities).
Given the focus of these trials on treatment development, each phase differed in its study design and primary aim:
PEACE II30 was a non-randomized proof-of concept trial (PP N=23) comparing an eight-week PP intervention to treatment-as-usual control. This found the intervention to be feasible, acceptable, and associated with moderate effect size improvements on positive affect, anxiety, and depression.
PEACE III25 was a randomized factorial trial (N=128) comparing eight variations of the PP intervention. All participants received a core, eight-week PP intervention. However, additionally: (1) half of participants received booster sessions over the subsequent eight weeks after completing the core intervention, (2) half received motivational interviewing to increase physical activity, and (3) half were instructed to engage in PP activities daily, while the other half were instructed to do so weekly. Results from this trial suggested that a longer intervention duration and the addition of motivational interviewing were associated with greater improvements in adherence.
PEACE IV26 was a randomized pilot trial (PP N=24) of an optimized 12-week, PP-plus-motivational interviewing intervention aimed to examine its feasibility and preliminary impact compared to a motivational interviewing-based health education condition. This trial found the optimized PP-plus motivational interviewing intervention to lead to greater improvements in positive affect, depression, anxiety, and physical activity than the motivational-interviewing condition.
Each phase was approved by the Partners Healthcare Institutional Review Board and PEACE III and IV were prospectively registered on ClinicalTrials.gov (NCT02754895; NCT03122184). Primary results of each study have been previously published. This analysis combined data from all participants who received PP in any phase of PEACE.
Participants.
Participants were recruited from inpatient cardiology units at one of two urban academic medical centers between November 2014 and April 2018. To be eligible for inclusion, participants must have been admitted for ACS (myocardial infarction or unstable angina), defined by consensus criteria,31 and to have suboptimal health behavior adherence as measured by the Medical Outcomes Study Specific Adherence Scale (MOS-SAS) items on physical activity, diet, and medications.32 Suboptimal adherence was defined as a summed MOS score of ≤14/18, or a total score of 15 with a physical activity score ≤5, and was included as an inclusion criterion to ensure participants had room to improve. Participants were excluded if they exhibited cognitive impairment (as measured by a six-item cognitive screen including orientation to time and a 3-word delayed recall),33 medical conditions likely to lead to death within 6 months, or inability to communicate in English or participate in physical activity. To be included in the present study’s analyses, participants must have been at least 45 years old.
Measures.
Questionnaires related to psychological well-being and health behavior adherence were completed at baseline and following the completion of the intervention (8 weeks for PEACE II and III, 12 weeks for PEACE IV). Information about medical comorbidities and peak troponin levels were collected via chart review at baseline. All measures were identical across studies unless otherwise noted.
Study engagement was measured via session completion, as the percentage of phone sessions completed out of the total offered to participants. Depression and anxiety were measured using the Hospital Anxiety and Depression Scale (HADS),34 which consists of two seven-item subscales for depression (HADS-D) or anxiety (HADS-A) (range 0–21 for each subscale). Dispositional optimism was measured by the Life Orientation Test – Revised (LOT-R; range 6–24),35 a six-item scale. Positive affect was measured with the positive affect subscale of the Positive and Negative Affect Schedule (PANAS; range 10–50),36 which asks participants to rate their experience of ten types of positive affect over the past week. Overall adherence was measured with the MOS-SAS, which included items asking about frequency of exercising regularly, following a low-fat, low-salt, or diabetic diet, and of taking prescribed medications (range 3–18).32
Physical activity was measured in PEACE III and IV through waist-worn Actigraph G3TX+ accelerometers (Actigraph, Pensacola, Florida), which were worn for 1 week, immediately following intervention completion (8 weeks for PEACE III, 12 weeks for PEACE IV). Consistent with previous research,37 participants were required to have 8 hours of wear time for 4+ days. Moderate-to-vigorous physical activity (MVPA; using a cutoff of 1,952 counts/minute) and steps were calculated. Physical activity level prior to ACS was estimated using the physical activity item from the MOS-SAS.32
Statistical analyses.
Descriptive information about the midlife and older adult samples was calculated using means, standard deviations, and percentages, and between-group differences in baseline demographic and medical characteristics were calculated using t-tests for continuous variables and chi-square tests of independence for categorical ones. Differences between midlife and older adults in rates of session completion were calculated with multiple regression analysis. Furthermore, between-group differences in change in psychological variables and overall adherence were examined with mixed effects regression models, controlling for sex, Charlson Comorbidity Index score (an aggregate of a variety of health risk conditions, including, among other things, cardiovascular, neurologic, and connective tissue disorders), and peak troponin levels. Finally, to examine the effect of midlife on post-intervention physical activity, mixed effect regression models were performed controlling for pre-ACS physical activity (MOS-SAS physical activity item), as well as the aforementioned covariates.
Results
Baseline Characteristics.
Across the three study phases, there were 94 midlife participants (57%) and 70 older participants (43%). This included 22 participants from PEACE II, 119 participants from PEACE III, and 23 participants from PEACE IV. Eleven participants were excluded due to being younger than 45 years old. Baseline characteristics by age group can be found in Table 1. Of note, compared to midlife participants, older participants were less likely to be male, more likely to be white, and had more medical comorbidities. They also had higher positive affect and overall adherence than midlife participants did.
Table 1.
Baseline characteristics of participants.
| Characteristic | Midlife (age 45–64) | Older (age 65+) | Test statistic | p-value |
|---|---|---|---|---|
| Age (years) | 56.49 ± 5.87 | 73.63 ± 6.05 | 18.25 | <0.001 |
| Men (%) | 53 (56.38) | 21 (30.00) | 11.28 | 0.001 |
| White race (%) | 69 (73.40) | 64 (90.00) | 7.04 | 0.008 |
| Lives alone (%) | 22 (23.50) | 21 (30.43) | 1.67 | 0.43 |
| Diabetes (%) | 29 (30.85) | 15 (21.43) | 1.81 | 0.18 |
| Current smoker (%) | 16 (17.02) | 13 (18.84) | 0.09 | 0.76 |
| Hyperlipidemia (%) | 72 (76.60) | 60 (85.71) | 2.12 | 0.15 |
| Hypertension (%) | 73 (77.66) | 62 (88.57) | 3.28 | 0.07 |
| Prior ACS (%) | 27 (28.72) | 26 (37.14) | 1.30 | 0.25 |
| Charlson Comorbidity Index | 2.09 ± 1.38 | 2.93 ± 2.17 | 7.83 | <0.001 |
| Peak TnT (ng/ml) | 1.39 ± 2.66 | 1.66 ± 4.34 | 0.46 | 0.65 |
| Body mass index (kg/m2) | 30.39 ± 6.68 | 28.75 ± 5.19 | −1.70 | 0.09 |
| Anxiety (HADS-A; range 0–21) | 7.28 ± 5.14 | 6.51 ± 4.08 | −1.01 | 0.31 |
| Depression (HADS-D; range 0–21) | 4.93 ± 4.15 | 4.50 ± 2.90 | −0.73 | 0.47 |
| Dispositional Optimism (LOT-R; range 0–24) | 16.62 ± 5.80 | 17.51 ± 5.37 | 1.00 | 0.32 |
| Positive affect (PANAS; range 10–50) | 33.79 ± 8.55 | 36.71 ± 7.09 | 2.33 | 0.02 |
| Self-reported adherence (MOS-SAS; range 3–18) | 10.68 ± 2.83 | 12.03 ± 2.01 | 3.41 | <0.001 |
| Self-reported physical activity (MOS-SAS physical activity item; range 1–6) | 2.32 ± 1.49 | 2.73 ± 1.39 | 1.69 | 0.09 |
| Motivational Interviewing intervention component (%) | 48 (51.06) | 34 (49.06) | 0.10 | 0.75 |
Group differences calculated with t-test for continuous variables and with χ2 test of independence for categorical variables.
Differences in intervention outcome by age group.
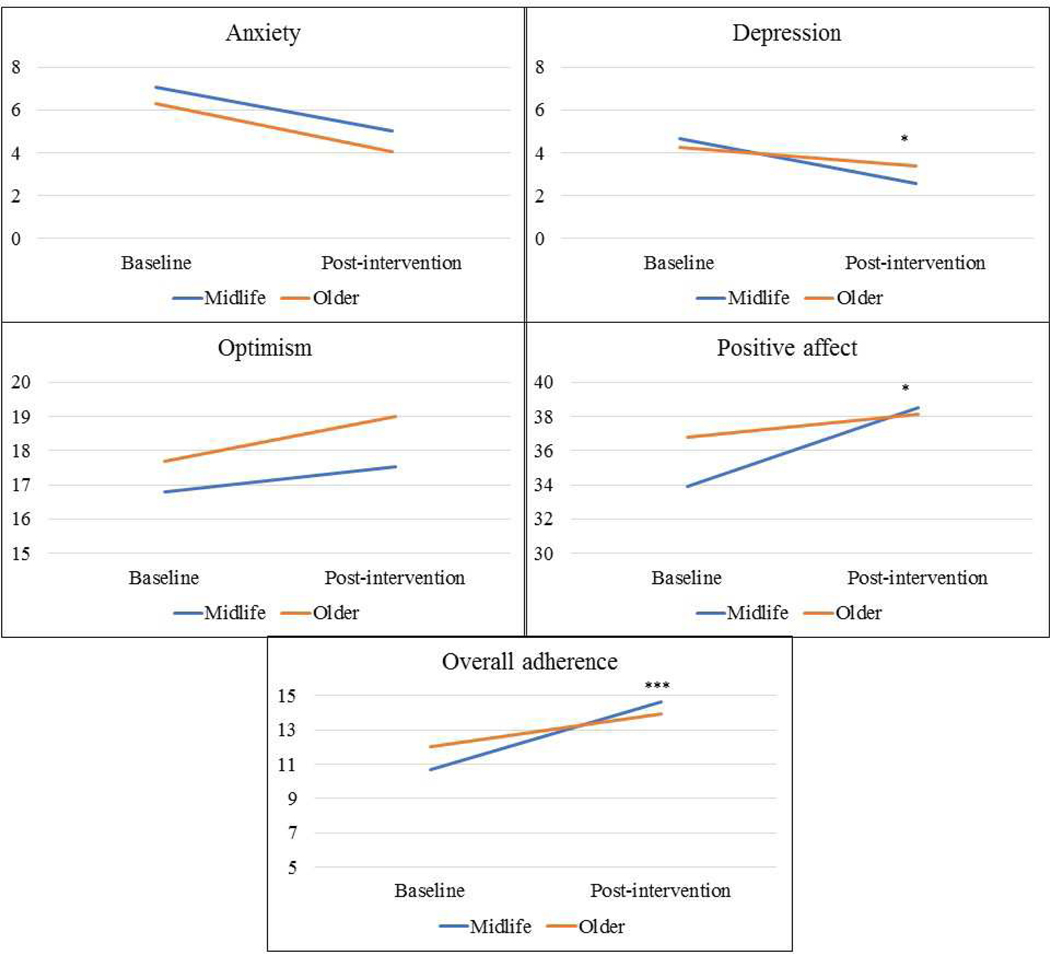
Midlife and older adults did not significantly differ in adherence to the study intervention as measured by percent of sessions completed (midlife: 64.70% ± 40.37, older: 70.83% ± 40.69). Compared to older participants, midlife participants had a larger reduction in depressive symptoms and a larger increase in positive affect post-intervention. Groups did not differ in change in anxiety symptoms or dispositional optimism. Midlife participants had a larger improvement in self-reported overall health behavior adherence at post-treatment [Table 2 and Figure 1]. Finally, for the subset of participants in whom physical activity was measured (n = 84), midlife participants had higher objectively measured mean minutes of MVPA per day and steps per day post-intervention compared to older participants, controlling for baseline self-reported physical activity level [Table 2].
Table 2.
Associations between midlife compared to older participants in intervention outcomes.
| b | 95% C.I. | p-value | |
|---|---|---|---|
| Session completiona | −7.74 | −21.89, 6.42 | 0.28 |
| Depressionb | −1.39 | −2.63, −0.16 | 0.03 |
| Anxietyb | −0.21 | −1.53, 1.18 | 0.75 |
| Positive affectc | 3.57 | 0.52, 6.63 | 0.02 |
| Optimismd | −0.68 | −2.52, 1.16 | 0.47 |
| Overall adherencee | 2.37 | 1.37, 3.36 | <0.001 |
| MVPAf,g | 9.83 | 1.55, 18.13 | 0.02 |
| Stepsg | 1877.02 | 684.44, 3069.73 | 0.002 |
Percent of intervention sessions completed.
Measured with the Hospital Anxiety and Depression Scale.
Measured with the Positive and Negative Affect Scale positive affect subscale.
Measured with the Life Orientation Test – Revised.
Measured with the Medical Outcomes Study Specific Adherence Scale.
MVPA = moderate-to-vigorous physical activity.
Objectively measured via accelerometer, controlling for baseline self-reported physical activity. All analyses controlled for gender, Charlson comorbidity score, and peak TnT.
Figure 1.
Pre-post change in psychological measures and behavioral adherence in midlife compared to older PEACE participants. *p < 0.05. ***p < 0.001.
Discussion
This analysis aimed to examine differences between midlife and older adults in the impact of telephone-delivered PP-based interventions to increase physical activity and psychological well-being. Contrary to our initial hypothesis, we found that midlife participants had larger improvements in depressive symptoms, positive affect, and health behavior adherence during the intervention compared to their older counterparts.
A prior meta-analysis of 51 PP interventions found that older participants and those with depression had larger benefit from such interventions,38 which differs from our findings that younger participants showed greater improvement. This difference may be because the meta-analysis included a number of studies of young adults whereas the present study only included midlife and older adults. It could also be explained by the unique situation of post-ACS participants. Because midlife participants are younger, they are less likely to already be suffering from comorbid medical conditions, and the ACS may be the first major medical event they have experienced. Therefore, it may be more of a “wake up call” for these individuals compared to those who have been managing multiple comorbid conditions for many years. However, analyses controlled for participants’ medical comorbidities, suggesting that findings are not due only to severity of illness.
Baseline characteristics could also play a role in this study’s findings. Older participants reported higher positive affect and adherence to health behaviors at baseline than midlife participants. This is in line with prior research showing higher psychological well-being in older age compared to midlife.15 It may be that midlife participants had more potential to improve given that they started the intervention with lower positive affect (along with higher depression and anxiety and lower optimism, although these between-group differences were nonsignificant).
In addition to differences in psychological changes during the intervention, midlife participants had higher objectively measured MVPA and steps post-intervention compared to older participants, when controlling for pre-ACS self-reported physical activity. While our inability to obtain objective physical activity measurements at baseline due to the patient population (i.e., immediately post-ACS) does somewhat limit interpretability of these findings, the results are in line with our findings for overall health behavior adherence that midlife participants showed a larger improvement during the intervention than did older participants. Despite reporting lower physical activity prior to their ACS, midlife adults ended the intervention with about double the minutes of MVPA and 1.5 times the number of steps per day compared to older participants. These findings further support the idea that an ACS at a younger age can be a major impetus for health behavior change, perhaps more so than when it is experienced later in life.
This study’s results should be examined in the broader context of psychological treatments in patients with coronary heart disease. Cognitive behavioral therapy focused on stress management and coping has been found to reduce risk for recurrent cardiovascular events.39,40 The PEACE study’s combined focus on psychological well-being and physical activity, use of positive psychological tools, and remote delivery are unique aspects of the present intervention. The mean session completion rate in PEACE (65–70%) is in a similar range to studies of CBT (e.g., 85% in-person group attendance in one study,40 59% homework completion in another).39
Results of this study are promising for midlife ACS patients. Given that individuals who experience an ACS in midlife have a strong opportunity to reduce their risk of another cardiac event via behavior change,7,9,10 a remote PP-based intervention may be ideal for helping individuals in this age group make changes at this critical time period. With just weekly phone calls, these midlife participants demonstrated improvements in important aspects of psychological and physical well-being that are not always so responsive to intervention. Further, despite the significant time pressure that midlife adults often face in comparison with their older counterparts who are more often retired, there were no significant differences between age groups in percentage of study sessions completed, suggesting that a phone-based intervention like this one is feasible in midlife. Clinicians treating midlife post-ACS patients should capitalize on this window of opportunity by engaging patients in conversations about the importance of physical activity and psychological well-being for their recovery and future health. They may also consider providing PP activities, which are simple and easy to deliver, at the bedside.
To our knowledge this study is the first to compare responses to a health behavior intervention in midlife and older cardiac patients. Strengths of this study include its sample size, the inclusion of relevant controls, and objective measurement of physical activity. Several limitations should be noted. Because not all study phases included a control condition, pre-post changes cannot be definitively attributed to the intervention. Long-term follow-up was not measured, so durability of effects is unknown. A lack of objectively measured physical activity at baseline limits interpretation of between-group differences in post-intervention physical activity. The sample was primarily white which may limit generalizability. Further, psychiatric history and substance abuse were not measured, both of which are associated with reduced adherence. Finally, cardiac rehabilitation has been associated with improved physical and psychological outcomes post-ACS in other studies, but attendance in such a program was not measured for the majority of patients in the present study and could not be included in our analyses.
Conclusions
In conclusion, midlife participants of a PP-based remote intervention to improve psychological well-being after an ACS had larger pre-post improvements in depressive symptoms, psychological well-being, behavioral adherence, and physical activity compared to participants age 65 and older. Despite the significant stress and time pressure that midlife adults typically face, this type of intervention appears to be feasible and well-accepted by patients in this age range. Such an intervention has the potential to improve cardiac risk factors and health behavior adherence in this high-risk, potentially high-yield group. Midlife patients hospitalized for an ACS should be identified and approached about improving physical activity and psychological well-being, as this time period may be uniquely associated with increased motivation to improve health.
Acknowledgments
Source of Funding
Funding: This study was supported by the National Heart, Lung, and Blood Institute through grant R01HL113272 (to Dr. Huffman). Time for analysis and article preparation was supported by the National Heart, Lung, and Blood Institute through grant R01HL133149 (to Dr. Huffman) and grant K23HL123607 (to Dr. Celano), and by the National Institute of Diabetes and Digestive and Kidney Diseases through grant R21DK109393 (to Dr. Huffman). The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health. The sponsor had no role in the design, analysis, interpretation, or publication of the study. The authors have no other relevant conflicts of interest to report.
Footnotes
Conflicts of Interest
The authors have no other relevant conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Holman DM, Grossman M, Jane Henley S, Peipins LA, Tison L, White MC: Opportunities for cancer prevention during midlife: Highlights from a meeting of experts. Am J Prev Med 2014; 46(3): S73–80. Doi: 10.1016/j.amepre.2013.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D: Hypertension Prevalence and Control Among Adults: United States, 2015–2016. 2017. [PubMed] [Google Scholar]
- 3.United States Centers for Disease Control and Prevention: National Diabetes Statistics Report, 2017. Estimates of Diabetes and Its Burden in the United States. Available at https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed September 17, 2019.
- 4.Benjamin EJ, Muntner P, Alonso A, et al. : Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019; 139(10): e56–528. Doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 5.Briffa TG, Hobbs MS, Tonkin A, et al. : Population trends of recurrent coronary heart disease event rates remain high. Circ Cardiovasc Qual Outcomes 2011; 4: 107–13. Doi: 10.1161/CIRCOUTCOMES.110.957944. [DOI] [PubMed] [Google Scholar]
- 6.Anderson L, Thompson DR, Oldridge N, et al. : Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016; 67(1): 1–12. Doi: 10.1002/14651858.CD001800.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trichopoulou A, Bamia C, Norat T, et al. : Modified Mediterranean diet and survival after myocardial infarction: The EPIC-Elderly study. Eur J Epidemiol 2007; 22(12): 871–81. Doi: 10.1007/s10654-007-9190-6. [DOI] [PubMed] [Google Scholar]
- 8.Notara V, Panagiotakos DB, Pitsavos CE: Secondary prevention of acute coronary syndrome. Socio-economic and lifestyle determinants: A literature review. Cent Eur J Public Health 2014; 22(3): 175–82. Doi: 10.21101/cejph.a3960. [DOI] [PubMed] [Google Scholar]
- 9.Sun Q, Townsend MK, Okereke OI, Franco OH, Hu FB, Grodstein F: Physical activity at midlife in relation to successful survival in women at age 70 years or older. Arch Intern Med 2010; 170(2): 471–9. Doi: 10.1001/archinternmed.2009.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Willis BL, Gao A, Leonard D, DeFina LF, Berry JD: Midlife fitness and the development of chronic conditions in later life. Arch Intern Med 2012; 172(17): 1333–40. Doi: 10.1001/archinternmed.2012.3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tucker JM, Welk GJ, Beyler NK: Physical activity in U.S. adults: Compliance with the physical activity guidelines for Americans. Am J Prev Med 2011; 40(4): 454–61. Doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 12.Shan Z, Rehm C, Rogers G, et al. : Trends in Dietary Carbohydrate, Protein, and Fat Intake and Diet Quality Among US Adults, 1999–2016. JAMA 2019; 322(12): 1178–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lachman ME, Teshale S, Agrigoroaei S: Midlife as a pivotal period in the life course: Balancing growth and decline at the crossroads of youth and old age. Int J Behav Dev 2015; 39(1): 20–31. Doi: 10.1177/0165025414533223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Madva EN, Gomez-Bernal F, Millstein RA, et al. : Magnitude and sources of distress in mid-life adults with chronic medical illness: An exploratory mixed-methods analysis. Psychol Heal Med 2018; 23(5): 555–66. Doi: 10.1080/13548506.2017.1384554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blanchflower DG, Oswald AJ: Is well-being U-shaped over the life cycle? Soc Sci Med 2008; 66(8): 1733–49. Doi: 10.1016/j.socscimed.2008.01.030. [DOI] [PubMed] [Google Scholar]
- 16.Graham C, Ruiz Pozuelo J: Happiness, stress, and age: how the U curve varies across people and places. J Popul Econ 2017; 30(1): 225–64. Doi: 10.1007/s00148-016-0611-2. [DOI] [Google Scholar]
- 17.Tindle HA, Chang Y-F, Kuller LH, et al. : Optimism, cynical hostility, and incident coronary heart disease and mortality in the women’s health initiative. Circulation 2009; 120(8): 656–62. Doi: 10.1161/circulationaha.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ronaldson A, Molloy GJ, Wikman A, Poole L, Kaski JC, Steptoe A: Optimism and recovery after acute coronary syndrome: A clinical cohort study. Psychosom Med 2015; 77: 311–8. Doi: 10.1097/PSY.0000000000000155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huffman JC, Beale EE, Celano CM, et al. : Effects of optimism and gratitude on physical activity, biomarkers, and readmissions after an acute coronary syndrome: The Gratitude Research in Acute Coronary Events study. Circ Cardiovasc Qual Outcomes 2016; 9(1): 55–63. Doi: 10.1161/CIRCOUTCOMES.115.002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chida Y, Steptoe A: Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosom Med 2008; 70(7): 741–56. Doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 21.DuBois CM, Lopez OV, Beale EE, Healy BC, Boehm JK, Huffman JC: Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: A systematic review. Int J Cardiol 2015; 195: 265–80. Doi: 10.1016/j.ijcard.2015.05.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boehm JK, Chen Y, Koga H, Mathur MB, Vie LL, Kubzansky LD: Is Optimism Associated With Healthier Cardiovascular-Related Behavior? Circ Res 2018; 122(8): 1119–34. Doi: 10.1161/CIRCRESAHA.117.310828. [DOI] [PubMed] [Google Scholar]
- 23.Seligman MEPP, Steen TA, Park N Peterson C: Positive psychology progress: Empirical validation of interventions. Am Psychol 2005; 60(5): 410–21. Doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- 24.Rollnick S, Miller WR: What is motivational interviewing? Behav Cogn Psychother 1995; 23(1): 325–34. Doi: 10.1017/S135246580001643X. [DOI] [PubMed] [Google Scholar]
- 25.Celano CM, Albanese AM, Millstein RA, et al. : Optimizing a positive psychology intervention to promote health behaviors following an acute coronary syndrome: The Positive Emotions after Acute Coronary Events-III (PEACE-III) randomized factorial trial. Psychosom Med 2018; 80(6): 526–34. Doi: 10.1097/PSY.0000000000000584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huffman JC, Feig EH, Millstein RA, et al. : Usefulness of a positive psychology-motivational interviewing intervention to promote positive affect and physical activity after an acute coronary syndrome. Am J Cardiol 2019; 123(12): 1906–14. Doi: 10.1016/j.amjcard.2019.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peterson JC, Charlson ME, Hoffman Z, et al. : A randomized controlled trial of positive-affect induction to promote physical activity after percutaneous coronary intervention. Arch Intern Med 2012; 172(4): 329–36. Doi: 10.1001/archinternmed.2011.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Redwine LS, Henry BL, Pung MA, et al. : Pilot randomized study of a gratitude journaling intervention on heart rate variability and inflammatory biomarkers in patients with Stage B heart failure. Psychosom Med 2016; 78(6): 667–76. Doi: 10.1097/PSY.0000000000000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Collins LM, Baker TB, Mermelstein RJ, et al. : The multiphase optimization strategy for engineering effective tobacco use interventions. Ann Behav Med 2011; 41: 208–26. Doi: 10.1007/s12160-010-9253-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huffman JC, Millstein RA, Mastromauro CA, et al. : A positive psychology intervention for patients with an acute coronary syndrome: Treatment development and proof-of-concept trial. J Happiness Stud 2016; 17(5): 1985–2006. Doi: 10.1007/s10902-015-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD: Third universal definition of myocardial infarction. Glob Heart 2012; 60: 1581–98. Doi: 10.1016/j.gheart.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 32.DiMatteo MR, Hays RD, Sherbourne CD: Adherence to cancer regimens: implications for treating the older patient. Oncology (Williston Park) 1992; 6: 50–7. [PubMed] [Google Scholar]
- 33.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC: Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 2002; 40(9): 771–81. Doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Bjelland I, Dahl A, Haug TT, Neckelmann D: The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002; 52(2): 69–77. Doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 35.Scheier MF, Carver CS, Bridges MW: Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994; 67(6): 1063–78. Doi: 10.1037/0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 36.Watson D, Clark LA, Tellegen A: Development and validation of brief measures of positive and negative affect: The PANAS scales. J Pers Soc Psychol 1988; 54(6): 1063–70. Doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 37.Cain KL, Geremia CM: Accelerometer data collection and scoring manual for adult & senior studies. 2011. [Google Scholar]
- 38.Sin NL, Lyubomirsky S: Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. J Clin Psychol 2009; 65(5): 467–87. Doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- 39.Carney RM, Freedland KE, Steinmeyer BC, Rubin EH, Rich MW: Clinical predictors of depression treatment outcomes in patients with coronary heart disease. J Psychosom Res 2016; 88: 36–41. Doi: 10.1016/j.jpsychores.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gulliksson M, Burell G, Vessby B, Lundin L, Toss H, Svärdsudd K: Randomized controlled trial of cognitive behavioral therapy vs standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease: Secondary prevention in Uppsala primary health care project (SUPRIM). Arch Intern Med 2011; 171(2): 134–40. Doi: 10.1001/archinternmed.2010.510. [DOI] [PubMed] [Google Scholar]