Abstract
Coronavirus disease (COVID-19) is responsible for a global pandemic and has impacted health care accessibility and delivery. Clinic data was reviewed for a sexually transmitted infection (STI) clinic from September, 2019 to May, 2020. A significant decrease in rates of STIs visits and treatments during the COVID-19 pandemic was observed.
Keywords: Public health, sexually transmitted infections, COVID-19
SUMMARY
During COVID-19 pandemic, access to services at a major sexually transmitted infections (STI) clinic significantly decreased. It is critical to implement novel approaches to maintain STI services during COVID-19.
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the cause of Coronavirus disease 2019 (COVID-19) and responsible for significant morbidity and mortality across the United States (US). There are currently over 1,787,680 confirmed cases in the US1. Restrictions and mitigation efforts to reduce COVID-19 have been broadly implemented across the US. The impact of these restrictions on access to clinical services, such as testing and treatment for sexually transmitted infections (STI), is largely unknown. Prior to COVID-19, rates of STIs, including syphilis, gonorrhea, and chlamydia had been significantly increasing across the US. The Centers for Disease Control and Prevention (CDC) reported a 3% increase in the rate of chlamydia, a 5% increase of gonorrhea, and a 14% increase in syphilis1, including a 40% increase in congenital syphilis in newborns in 20192.
STI clinics serve a critical role in addressing STIs and provide safety-net services in many states. However, in order to reduce risk of COVID-19 transmission, many STI clinics have limited or canceled clinical visits, limited elective procedures, shortened clinic hours, decreased number of staff in clinic, and switched from in-person to telemedicine visits. The interruption of STI services could lead to a further increase in STI rates. This study evaluated utilization of STI clinic services at the major STI clinic in Providence, Rhode Island as a result of COVID-19.
METHODS
We used bivariate analyses to compare the average weekly numbers of each type of visit during three phases: 1) Pre-COVID-19 (September 1st, 2019-February 29th, 2020), 2) Evolving (March 1st, 2020-April 11st, 2020, and 3) Plateau (April 12nd, 2020-May 13th, 2020). The first confirmed COVID-19 case was reported on February 29th, 2020 in Rhode Island. We defined the pre-COVID-19 phase as starting approximately six months prior to the first case and ending on February 29th, 2020. From March 1st to April 11st, 2020, we observed exponential growth in the number of COVID-19 confirmed cases in Rhode Island and defined this period as the evolving phase. After April 11th, 2020, the number of newly confirmed cases were stable over the time.
We reviewed all patients presenting for care at the major STI clinic in Providence, Rhode Island from September 1st, 2019 to May 13th, 2020. Clinic visits were categorized as: a) Screening visits, defined as visits for asymptomatic patients requiring STI testing only, b) Provider visits, defined as visits for patients with possible exposure and/or infection, potentially requiring empirical treatment, and c) Treatment visits, defined as visits for patients with known STIs requiring treatment. Prior to the COVID-19 pandemic, the clinic was open Wednesdays, Thursdays, and Fridays (three hours per day). During the evolving phase, the clinic was open three days a week for two weeks (three hours per day) and then switched to two days per week for four weeks (three hours per day). In the plateau phase, the clinic was open one day per week for five weeks (four hours per day). During the pre-COVID-19 phase, the clinic was open for 234 total hours; during the evolving phase, the clinical was open for 42 total hours; and during the plateau phase, the clinic was open for 20 total hours. Patients were seen on a walk-in basis, regardless of service needed, insurance status, and ability to pay.
During the pre-COVID-19 phase, all three types of clinic visits were available (testing, provider, treatment). During the pre-COVID-19 phase, screening and asymptomatic visits were performed by non-clinician qualified professional test counselors. In the evolving phase, the clinic moved to telemedicine visits for screening/asymptomatic exposures, although only about five hours’ total of telemedicine visits were completed during this phase. For the rest of the evolving phase, clinic staff and hours were significantly limited and screening visits were not made available to patients in order to reduce possible COVID-19 exposure and transmission to clinic patients/staff. In the plateau phase, clinic hours and visit availability were increased, but screening visits were still not available, as non-clinician staff, do not have the necessary credentials to perform these visits via telemedicine. Thus, all patients who seen in the evolving and plateau phases were seen by providers and were thus considered provider visits, many of which were done via telemedicine, and which addressed topics related to screening and exposure.
We excluded data from the week of November 25, 2019 (Thanksgiving week) and the week of February 10, 2020 (the STI clinic moved to a new location) for this analysis. Poisson regression was used to assess the trend of visit rates throughout these three phases. An alpha of 0.05 was used as the cutoff for significance. All analyses were conducted in Stata 15.0 (StataCorp LP, College Station, Texas). Review of clinic data was approved by the local institutional review board.
RESULTS
During the time period, the clinic had a total of 2,347 visits (875 screening, 1021 provider, and 451 treatment). In the pre-COVID-19 phase, the median of weekly visits was 67 (interquartile range [IQR]: 65-77). Of these visits this included 33 (IQR: 29-38) screening visits, 37 (IQR: 32-40) provider visits, and 17 (IQR: 13-21) treatment visits per week. In the evolving phase, the median of weekly visits was 20 (IQR: 13-44), including 6 (IQR: 6-20) screening visits, 14 (IQR: 8-24) provider visits, and 4 (IQR: 3-8) treatment visits per week. In the plateau phase, the median of weekly visits was 9 (IQR: 9-10), with 9 (IQR: 9-10) provider visits and 3 (IQR: 3-3) treatment visits (a provider visit may involve a patient receiving STI treatment and therefore the a visit would be counted as both a provider and treatment visit).
In the COVID-19 evolving phase, we observed a 55% (95% confidence interval [CI]:45%-63%, P<0.001) reduction in the total number of absolute visits, a 60% (95% CI: 46%-71%, P<0.001) reduction in the number of screening visits, a 50% (95% CI: 35%-62%, P<0.001) reduction in the number of provider visits, and a 62% (95% CI:40%-75%, P<0.001) reduction in the number of treatment visits compared to the pre-COVID-19 phase. In the COVID-19 plateau phase, we observed an 84% (95% CI: 68%-88%, P<0.001) reduction in total absolute clinic visits, a 100% reduction in screening visits, a 68% (95% CI: 56%-77%, P<0.001) reduction in provider visits, and a 77% (95% CI: 61%-86%, P<0.001) reduction in treatment visits compared to the pre-COVID-19 phase (Figure 1). The positivity rates of the most common STIs (chlamydia bacteria infection, CT; gonorrhea, GC; and syphilis) are shown in Table 1.
FIGURE 1.
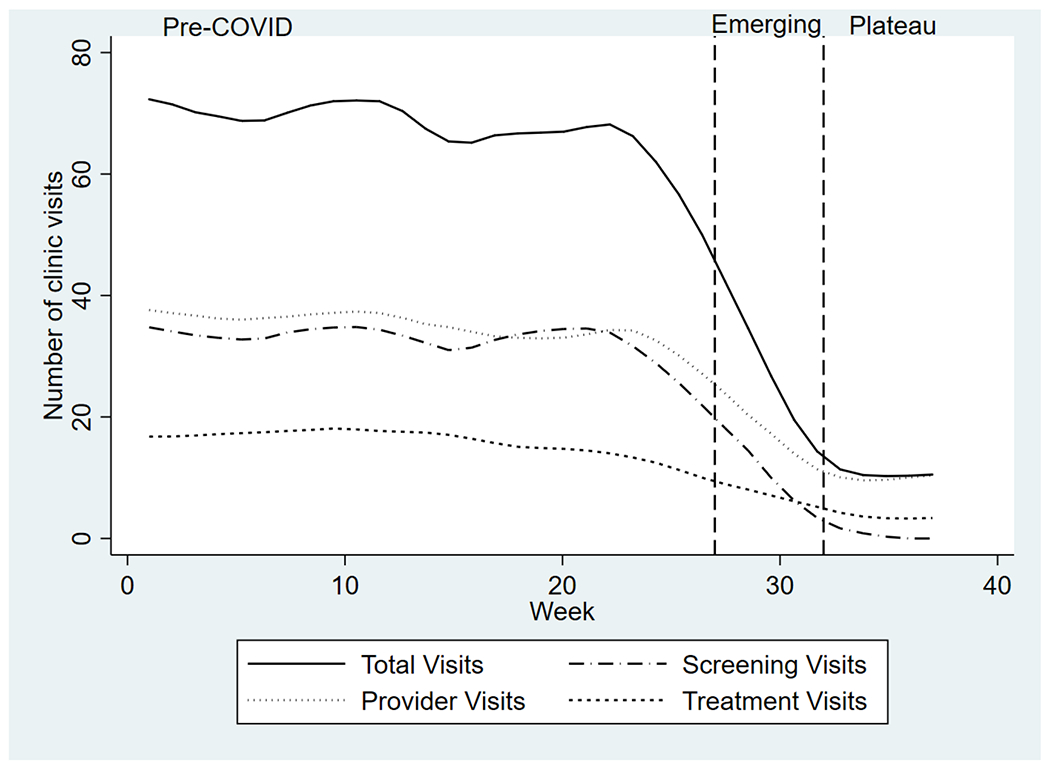
STI Clinic Average Visits per Week over Time
TABLE 1.
Positivity rates for STIs during three phases (Pre-COVID-19, Evolving, Plateau)
| Pre-COVID-19 (9/1/19-2/29/20) | |||
|---|---|---|---|
| Positivity Rate (%) | Positivity (n) | Tests Performed | |
| GC | 6.7% | 93 | 1384 |
| CT | 10.5% | 139 | 1328 |
| Syphilis | 4.3% | 52 | 1216 |
| Evolving (3/1/20-4/11/20) | |||
| GC | 3.2% | 4 | 124 |
| CT | 12.4% | 15 | 121 |
| Syphilis | 1.7% | 2 | 117 |
| Plateau (4/12/20-5/13/20) | |||
| GC | 13.3% | 6 | 45 |
| CT | 13.3% | 6 | 45 |
| Syphilis | 6.0% | 3 | 50 |
DISCUSSION
This is among the first studies to evaluate impact of COVID-19 on the number of visits at an STI clinic. Similar to other STI clinics3, recommended precautions were taken to reduce patient and staff risk of infection including screening patients over the phone for symptoms of COVID-19 before presenting to the clinic, limiting physical presentation to clinic to individuals needing treatment or with other urgent concerns, wiping down surfaces, handwashing, and using hand sanitizers with at least 60% alcohol4. These precautions led to significant reductions in the number of STI clinic visits. These findings are consistent with provider reports that COVID-19 has severely limited their ability to provide sexual health services5.
The reduction in access to STI clinics may exacerbate pre-COVID-19 barriers to testing. Barriers to STI care before COVID-19 included stigma around STI testing6, cost of testing7, accessibility, and availability of services8. The onset of the COVID-19 has presented additional barriers for patients needing STI care. For example, patients were, and remain, reluctant to go to hospitals and doctors’ offices to for medical issues due to fear of COVID-19 exposure and infection9,10,11. Additionally, patients may have lost their job, wages, or health insurance, thereby increasing the financial barriers to accessing medical care, including STI care12. It is important that STI services remain accessible throughout the COVID-19 pandemic; in the case of the clinic under study, this goal was accomplished via offering telemedicine visits and by gradually reopening the clinic to in-person visits, when it was determined safe to do so and with the appropriate infection control precautions in place. Prior research has demonstrated approaches in which STI clinics may continue to provide services while mitigating risk for COVID-19 transmission amongst staff and patients4.
The limitations of this study are related to potential generalizability, as data were collected from one site in an urban area. It is possible that STI clinics in other cities in the US, or in more suburban or rural areas, may have experienced a less noticeable impact visit rates during the COVID-19 pandemic, depending on the rates and risks of COVID-19 infection in those areas. Additionally, this study does not take into account STI testing done at community agencies, primary care offices, and other safety-net facilities. Although rates of STI clinic visits decreased, it is possible that patients who would have ordinarily visited the clinic sought STI testing and care from other sources during the COVID-19 pandemic. Finally, it is possible that the decrease in clinic visits was not due solely to the pandemic, but potentially also due to policy changes around the availability of telemedicine, fear of exposure to COVID-19 in a clinic setting, or other factors.
In conclusion, the COVID-19 pandemic did significantly reduce average the number of STI clinic visits per week. However, individuals still utilized the clinic services, including treatment for infections. Additionally, COVID-19 has created conditions that may lead to increases in rates of STIs and HIV. Sexual and reproductive care providers should consider this possibility in addition to catching up on providing services to individuals who may have continued to engage in high-risk sexual behavior during the COVID-19 pandemic, but whose care was interrupted by COVID-19. In this context, access to STI services remains a necessity, even in the face of the COVID-19 pandemic.
Acknowledgments
Sources of Support
This work supported by funding from the National Institute of Mental Health (R01MH114657).
Footnotes
Competing Interests
The authors declare that they have no competing interests.
REFERENCES
- 1.Centers for Disease Control and Prevention. 2020. Coronavirus Disease 2019 (COVID-19) In The U.S <https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html> [Accessed 3 June 2020].
- 2.Centers for Disease Control and Prevention. 2020. STD Facts - Congenital Syphilis. <https://www.cdc.gov/std/syphilis/stdfact-congenital-syphilis.htm> [Accessed 3 June 2020].
- 3.Barbee L, Dombrowski J, Hermann S, et al. “Sex in the Time of COVID”: Clinical Guidelines for Sexually Transmitted Disease Management in an Era of Social Distancing. Sexually Transm Dis 2020; 47(7): 427–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Napoleon SC, Maynard MA, Almonte A, et al. Considerations for STI Clinics During the COVID-19 Pandemic. Sex Transm Dis 2020;47(7):431–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagendra G, Carnevale C, Neu N, et al. The Potential Impact and Availability of Sexual Health Services During the COVID-19 Pandemic. Sexually Transm Dis 2020; 47(7): 434–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.James T and Ryan S HIV Knowledge Mediates The Relationship Between HIV Testing History And Stigma In College Students. Taylor & Francis 2018; 66:7, 561–569. [DOI] [PubMed] [Google Scholar]
- 7.Cuffe KM, Newton-Levinson A, Gift TL, et al. Sexually Transmitted Infection Testing Among Adolescents and Young Adults in the United States. J Adolesc Health 2016;58(5):512–9 [DOI] [PubMed] [Google Scholar]
- 8.Scheim A and Travers R Barriers And Facilitators To HIV And Sexually Transmitted Infections Testing For Gay, Bisexual, And Other Transgender Men Who Have Sex With Men. Taylor & Francis 2016; 29:8, 990–995. [DOI] [PubMed] [Google Scholar]
- 9.Moroni F, Gramegna M, Ajello S, et al. Collateral Damage: Medical Care Avoidance Behavior Among Patients With Myocardial Infarction During The COVID-19 Pandemic. JACC Case Rep. 2020. : 1620–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Douglas M, Katikireddi S, Taulbut M, et al. Mitigating The Wider Health Effects Of Covid-19 Pandemic Response. BMJ 2020; 369: m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frankel T and Romm T Historic Financial Decline Hits Doctors, Dentists And Hospitals — Despite Covid-19 — Threatening Overall Economy. The Washington Post 2020. <https://www.washingtonpost.com/business/2020/05/04/financial-distress-among-doctors-hospitals-despite-covid-19-weighs-heavily-economy/> [Accessed 3 June 2020].
- 12.Woolhandler S, Himmelstein DU. Intersecting U.S. Epidemics: COVID-19 and Lack of Health Insurance. Ann Intern Med 2020;173(1):63–64. [DOI] [PMC free article] [PubMed] [Google Scholar]


