Abstract
Racial and ethnic disparities in pediatric anesthesia health services could result in minority children being at increased risk of poor outcomes, such as pain, anxiety or over-exposure to medications. Yet a comprehensive understanding of the literature on such disparities does not exist to date. The objective of this study is to describe health services disparities in pediatric anesthetic care in the pre-, intra-, or post-operative period by synthesizing current literature. We searched National Library of Medicine’s PubMed/Medline, Embase, and Web of Science for articles published between January 1, 2007 and May 9, 2020 to identify literature on racial and ethnic health services disparities in pediatric anesthesia. We used the Institute of Medicine’s definition of disparities. Health services were related to pre-, intra-, or post-operative anesthetic care of pediatric patients (<18 years old). Out of 2110 studies, 10 studies met the criteria for inclusion. Nine out of the ten articles were single-institutional observational studies, based at tertiary hospitals. Sample sizes ranged from 74 to 37,618 discrete participants, for a total of 69,350 subjects across all studies. Results of these studies present low-quality evidence and heterogenous conclusions regarding pediatric anesthesia health services disparities. This review demonstrates the paucity and diversity of research on racial and ethnic disparities in pediatric anesthesia health services and suggests how future work might utilize improved data and rigorous study designs.
Keywords: anesthesia, pediatrics, health services, review
Introduction:
Racial and ethnic health services disparities in the United States are well-described phenomena and may negatively affect health and health outcomes across all medical specialties [1-2]. These disparities are defined by the Institute of Medicine (IOM) as unfair differences in provision of care, access, or quality of outcomes for racial or ethnic minority patients that exist even when clinical need and patient preferences are considered [1, 3]. Most studies of racial and ethnic disparities in anesthetic care have focused on adult populations. A 2006 study found that “black” and “minority” (including American Indian, Alaskan Native, Asian, and Pacific Islander) adult patients were more than twice as likely as white patients to have general anesthesia over regional techniques for inguinal hernia repairs while a 2016 article demonstrated that Latino patients were almost half as likely to have a peripheral nerve block for hip and knee surgery as compared to white patients [4-5]. In the setting of obstetrical anesthesia, white women are more likely both to receive labor epidurals than black and Latino women and to have neuraxial anesthetics for cesarean sections than black women [6-7]. Another study demonstrated that black Medicare patients had significantly longer operative times than white patients for hip, knee, thoracic, and colorectal surgeries [8]. These differences suggest that black and Latino patients may disproportionately bear the risks of general anesthesia and/or not benefit from adjuvant techniques such as regional anesthesia.
To date, there has been one narrative summary review of racial and ethnic health services disparities in pediatric anesthesia, even while millions of children in the United States may be exposed to deleterious side effects of disparate anesthetic care [9]. The purpose of this scoping review is to describe the literature on racial and ethnic health disparities in pediatric anesthesia in order to create a comprehensive model of this phenomenon, including associated services and affected populations. Given that searches resulted in ten articles, we considered it premature to perform a systematic review or investigate mechanisms related to disparities such as access to surgical care or specialty hospitals. Moreover, we aimed to examine studies of racial and ethnic health services disparities in pediatric anesthetic care in the United States with the knowledge that disparities due to other sociodemographic factors (such as sex or geographic location) would require additional review studies. Specifically, our interest is in the services provided by anesthesiologists to pediatric patients (1) and the outcomes of any such disparities in health services (2). This scoping review synthesizes the existing literature on racial and ethnic disparities in pediatric anesthetic care and subsequent differences in health outcomes.
Methods:
This is a scoping review; we adhere to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement standards in this article [10].
Data sources:
We searched the online databases National Library of Medicine’s PubMed/Medline, Embase, and Web of Science for articles published between January 1, 2007 and May 9, 2020. The dates were selected so as to be most likely to reflect both the evolving interest in disparities research in anesthesia and current anesthesia health services. [4-8]. The search strategy included manual searching of citation lists. The initial search was performed in June-July 2018 for publications between January 1, 2007 and June 15, 2018. We updated this search on May 9, 2020 for publications between June 15, 2018-May 9, 2020.
Inclusion/Exclusion:
All relevant clinical studies, clinical trials, observational studies (prospective or retrospective), or randomized control trials on health services disparities in pediatric anesthesia were considered eligible for inclusion. For this article, racial and ethnic disparities in health services were defined according to the IOM definition: “racial or ethnic differences … that are not due to access-related factors or clinical needs, preferences, and appropriateness of intervention” [1]. This definition does not allow for adjustment based on markers of socio-economic status (SES) as these may be mediators of disparities [1].
Studies were included if they were published in English. Study subjects had to include pediatric patients (inclusive of children <18 years old) who received pediatric anesthetic care in the United States. We elected to limit our search to anesthetics performed in the United States due to the particularities of race as a social construct within different countries [11]. Additionally, studies that did not distinguish between data on pediatric patients and data on adult patients or did not perform separate analyses were excluded. We excluded studies focused on outcomes not specific to pediatric anesthesia care—such as surgical care/evaluation/outcomes or chronic/at-home pain management. Unpublished studies or those published before 2007 were also excluded. Finally, studies had to be comparative across at least two racial or ethnic groups. White non-Latino patients were selected as the reference group given previous adult anesthesia literature demonstrating better health services for white patients in comparison to racial and ethnic minority patients [4-8]. We did not exclude studies based on sample size.
Primary Endpoints:
The research team assigned outcomes a rank of importance, using Grading of Recommendations, Assessment Development and Evaluation (GRADE) framework of critical, important, or low importance [12-13].
Outcomes had to be related to one of the following aspects of pediatric anesthetic health services: provision of routine pre-, intra-, and post-operative care including, but not limited to management of anxiety, induction (initiation of anesthesia with intravenous or inhalational methods), airway, intravenous fluids, emergence (awakening from anesthesia) and placement of intravenous/intra-arterial lines or regional blocks (critical outcome); pre-, intra-, and post-operative medication administration (important outcome); management of intra-and post-operative complications including, but not limited to laryngospasm, bronchospasm, aspiration, postoperative nausea and vomiting, and pain (critical outcome).
Secondary Endpoint:
Given that health services disparities may signify adverse clinical outcomes, the secondary endpoints were consequences due to any racial and ethnic differences in health services provided in the primary endpoint (above). This could include, for example, higher pain scores due to fewer administered pain medications or higher anxiety in the absence of pre-operative medication administration for racial and ethnic minority patients as compared to white patients.
Search:
We consulted with a medical librarian at our institution to design our search. We searched by both subject headings (Medical Subject Headings (MeSH) for PubMed and Emtree for Embase) for the respective databases and by keywords. Web of Science does not use subject headings and this search was done by keywords only. We did not include any specific endpoints (such as pain medicine or anxiolysis) in our search terms so that our review might include as many outcomes that might fit under the category of ‘pediatric anesthesia health services.’ Our search combined terms related to anesthesia (1), health disparities and/or race (2) and children (3).
The following MeSH terms were used jointly to search PubMed: ‘anesthesia and analgesia’ OR ‘anesthesiology’ OR ‘perioperative care’ AND ‘healthcare disparities’ OR ‘ethnic groups’ AND ‘adolescent’ OR ‘child’ OR ‘infant.’
The following Emtree terms were used jointly to search Embase: 'anesthesiological procedure' OR ‘anesthesiology’ OR ‘anesthesiologist’ OR 'perioperative period' OR 'intraoperative period' OR 'postoperative period' OR ‘anesthesia’ AND ‘healthcare disparity’ OR ‘ethnic group’ OR ‘minority group’ OR ‘minority health’ OR ‘race difference’ AND ‘juvenile’ OR ‘parent’ OR ‘pediatrics.’
The following keywords were used jointly to search PubMed, Embase, and Web of Science: ‘anesthesia & analgesia’ OR ‘anaesthesia & analgesia’ OR ‘anesthesia’ OR ‘anaesthesia’ OR ‘anesthesiology’ OR ‘anaesthesiology’ OR ‘anesthesiologist’ OR ‘anesthesiologists’ OR ‘anaesthesiologist’ OR ‘anaesthesiologists’ OR ‘perioperative care’ OR ‘peri-operative care’ OR ‘intraoperative care’ OR ‘intra-operative care’ OR ‘postoperative care’ OR ‘post-operative care’ OR ‘operating room management’ AND 'disparities' OR 'healthcare disparities' OR 'health care disparities' OR 'racial disparities' OR 'minority' OR 'nonwhite' OR 'race' OR 'ethnicity' OR 'ethnic groups' OR 'African American' OR 'Hispanic American' OR 'Asian American' OR 'Latino' OR 'Latina' OR 'Latinos' OR 'minority health' OR 'ethnic minority' AND ‘adolescent’ OR ‘adolescents’ OR ‘child’ OR ‘children’ OR ‘infants’ OR ‘infant’ OR ‘parent’ OR ‘parents’ OR ‘pediatric’ OR ‘paediatric’ OR ‘pediatrics’ OR ‘paediatrics.’
Data Extraction:
For the initial search in 2018, two authors (JMR and JM) independently screened titles and abstracts using the Covidence platform (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org). Disagreements on inclusion of the articles were resolved by discussion among the evaluators and by a third (blinded) reviewer (LET). For the subsequent search in 2020, JMR screened titles and abstracts. Questions about inclusion of articles were resolved by LET. Data on primary author’s name, publication year, study design, groups under study, outcome measured, and study findings were then extracted.
Using GRADE, the authors assessed the quality of evidence for each outcome [12-13]. In this scale, randomized controlled trials are a priori assigned a high ranking whereas observational studies are a priori assigned a low ranking. This scale then ranks each outcome upwards or downwards based on five areas: risk of bias, imprecision, inconsistency, indirectness, and publication bias. Evidence can be upgraded based on magnitude of effect, dose-response relation, and effect of residual confounding [12-13].
Statistical analysis:
Given that this is a scoping review, we describe the studies and their adjusted findings in their original summary measures.
The Evidence Profile Table and Summary of Findings (SoF) Table was produced using Gradepro (GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University, 2015, developed by Evidence Prime, In. Available from gradepro.org).
Results:
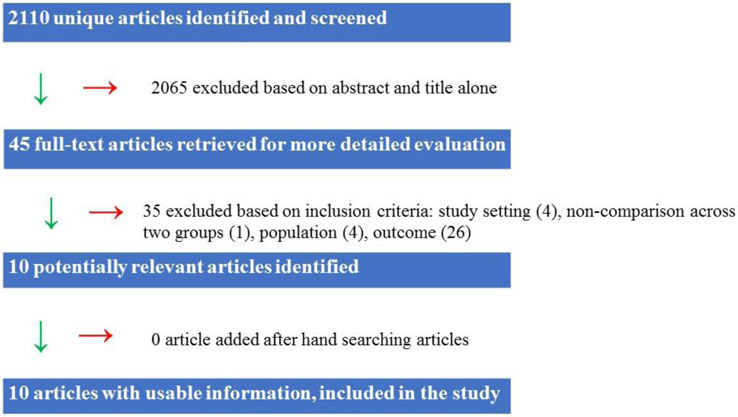
Database searches initially identified 2110 articles which were screened by title and abstract. 10 met the inclusion criteria for this review. (Figure 1).
Figure 1:
Flowchart of screening and eligibility evaluation process
Study Characteristics:
Nine of the ten studies were single-institutional and observational, based at tertiary hospitals. One study used a national database, Pediatric National Surgical Quality Improvement Program (P-NSQIP). Sample sizes ranged from 74 to 37,618 discrete participants, for a total of 69,350 subjects across all studies. All subjects were patients; no studies focused on anesthesiologists or parents. The study locations represented all five regions across the United States (Mid-Atlantic, Midwest, Northwest, Southwest and Southeast). (Table 1). In all studies, race and ethnicity was self-reported by patients/parents [14-23].
Table 1:
Included Publications
| Publication | Publication Type | Patients (N=69350) | Location of study |
|---|---|---|---|
| Jimenez et al. (2010)14 | retrospective cohort study | 94 (W=47; L=47)a | Seattle, WA |
| Sadhasivam et al (2012)15 | prospective observational | 194 (W=160; B=34)a | Cincinnati, OH |
| Rosenbloom et al. (2017)16 | retrospective cohort study | 1680 (W=1329; B=351)a | Philadelphia, PA |
| Nafiu et al. (2017)17 | prospective observational study | 771 (W=619; M=152)a | Ann Arbor, MI |
| Maher et al (2018)18 | retrospective cohort study | 74 (W=41; B=22; O=11)a | Durham, NC |
| Wallace et al (2019)19 | retrospective observational study | 1982 (W=1447; L=317; M=218 )a | NSQIP |
| Nafiu et al (2019)20 | prospective cross-sectional study | 1134 (W=898; M=236)a | Ann Arbor, MI |
| Baetzel et al (2019)21 | retrospective cohort study | 37618 (W=33717; B=3901)a | Ann Arbor, MI |
| King et al (2019)22 | retrospective cohort study | 25664 (W=8884; M=16780)a | Palo Alto, CA |
| Owusu-Agyemang et al (2019)23 | retrospective observational study | 139 (W=80; M=59)a | Houston, TX |
W=White; L=Latino
B=black; M=minority
O=other patient
The ten studies had different groups for comparison and slightly different clinical contexts (i.e. physical location and specific point in peri-operative period). One study compared Spanish-speaking Latino and white patients undergoing tonsillectomy-adenoidectomy [14]. A second study compared black and white patients undergoing tonsillectomy [15]. A third study compared black and white patients undergoing laparoscopic appendectomy [16]. A fourth study compared ‘minority’ (aggregated) and white patients undergoing outpatient surgery [17]. The fifth study compared black, ‘other,’ and white patients undergoing primary scoliosis surgery (spinal fusion) [18]. A sixth study compared white non-Latino, Latino, and nonwhite non-Latino (aggregated) patients presenting for craniosynostosis repair [19]. The seventh study was an expansion of a previous study examining “Caucasian” and “non-Caucasian” (aggregated) children undergoing painful ambulatory surgeries [20]. The eighth study investigated white and black children undergoing non-emergent weekday surgeries [21]. The ninth study compared white and ‘minority’ (aggregated) children presenting for any anesthetic (except diagnostic radiology) [22]. And the ninth study compared white and ‘minority’ (aggregated) children undergoing tumor resection [23]. (Table 2).
Table 2:
Findings and primary endpoints of included publications.
| Publication | Clinical Setting | Outcome | Finding |
|---|---|---|---|
| Jimenez et al. (2010)14 | White/Latino Tonsillectomy/adenoidectomy <18 years old |
Pre-operative medication Intra-operative medication Post-operative medication Provision of intra-operative care Parental presence Inhalational induction |
No difference No difference L less likely to receivea L more likely to receivea No difference |
| Sadhasivam et al. (2012)15 | White/Black Tonsillectomy 6-15 years old |
Post-operative medication | B more likely to receivea |
| Rosenbloom et al. (2017)16 | White/Black Appendectomy 3-17 years old |
Pre-operative medication Intra-operative medication |
No difference No difference |
| Nafiu et al. (2017)17 | White/Minority Outpatient surgery 4-17 years old |
Post-operative medication | M more likely to receivea |
| Maher et al. (2018)18 | White/Black/Other Scoliosis surgery <18 years old |
Management of intra-operative complications -Blood transfusion |
B more likely to receivea No difference for Oa |
| Wallace et al. (2019)19 | White/Black/Latino Craniosynostosis </= 24 months |
Intra-operative care -Anesthesia time |
Longer for B and La |
| Nafiu et al. (2019)20 | White/Non-white | Post-operative medications | M more likely to receivea |
| Baetzel et al. (2019)21 | White/Black Elective surgery <18 years old |
Pre-operative medication Provision of intra-operative care -Family presence -Inhalational induction |
B <5yo less likely to receivea B <15yo less likely to receivea B 10-14yo more likely to receivea |
| King et al. (2019)22 | White/Minority All anesthetics |
Provision of intra-operative care -Regional anesthesia use |
No difference |
| <18 years old | |||
| Owusu-Agyemang et al. (2019)23 | White/non-white Tumor resection </=19 years old |
Provision of intra-operative care -Epidural placement Management of intra-operative complication -Blood transfusion |
No difference No difference |
W=White; L=Latino; B=black; M=minority; O=other patients
Primary Outcomes:
Six studies focused on disparities in medication administration, two of which also examined management of intraoperative care [14-17; 20; 21]; two studies investigated disparities in receipt of blood transfusion [18; 23]; one study looked at anesthesia time [19]; and two studies studied use of regional anesthesia [22-23]. (Table 2).
Publication 1:
In an unadjusted matched retrospective cohort analysis of children less than 18 years old undergoing tonsillectomy/adenoidectomy from 2003-2005, Jimenez and colleagues found that 19/44 (42%) white children and 11/47 (23%) Latino children received oral anxiolytic (p=0.05) pre-operatively [14]. As a corollary, the authors also found that Latino parents were more likely to be present at induction (initiation) of anesthesia than white parents, 73% as compared to 47%, p=0.02 [14]. Results showed that 84% of white children and 78% of Latino children underwent inhalational induction (p=0.51) [14].
Intra-operatively, there was no difference in receipt of non-opioid analgesics between white and Latino children (p=0.81): 13/47 (28%) white children and 10/47 (21%) Latino children received acetaminophen and 1/47 white children and 1/47 (2%) Latino children received both ketorolac and acetaminophen [14]. Jimenez and others did not find a statistically significant difference in administered intra-operative opioids in morphine equivalents (MEQ) per kilogram (kg−1). However, there was a difference in type of opioid administered: 55% of Latino children received short-acting agents and 43% received long-acting agents as compared to 28% and 64% of white children respectively (p=0.01) [14].
Latino pediatric patients were less likely to receive opioids than white patients in the early recovery period: median of 0.05 (0-0.14) MEQ kg−1 for Latino patients and 0.07 (0-0.90)
MEQkg−1 for white patients (p=0.04, unstratified by type of opioid; p=0.02, stratified by type of opioid, none, long-acting, and short-acting) [14]. There was no significant difference in opioid receipt for the late recovery period (p=0.24, unstratified by type of opioid; p=0.16, stratified by type of opioid) [14].
Publication 2:
Sadhasivam and colleagues conducted a prospective study focused on post-operative analgesic administration to 194 children ages 6-15 undergoing tonsillectomy [15]. In multivariable analysis adjusting for age, sex, weight, body mass index (BMI), obstructive sleep apnea (OSA), intra-operative opioids and total morphine requirement, the authors demonstrated that black children as compared to white children were more likely to receive intravenous morphine (no point estimate provided, p=0.0029), received more analgesic interventions (i.e. number of times analgesia was provided) (no point estimate provided, p<0.0001, and received more morphine (no point estimate provided, p=0.0011) in the post-operative period [15]. In the setting of black children having higher maximum pain scores than white children, the authors interpreted their findings as black children requiring more analgesics than white children [15]. In this model, no interaction was found between OSA and race for receipt of morphine [15].
Publication 3:
Rosenbloom and colleagues conducted a retrospective cohort study of 1680 children aged 3-17 undergoing laparoscopic appendectomies from 2010 to 2015 [16]. The authors showed that 753/1329 (56.7%) white children and 172/351 (49.0%) black children received pre-operative midazolam, likely for pre-operative anxiolysis. Adjusting for anesthesiologist, child’s age and gender, this effect was non-significant (OR 0.77, 95% CI 0.57-1.02, p=0.07) [16].
There was also no significant difference in any intra-operative medication administrations to black as compared to white patients in analyses adjusted for provider (surgeon for ketorolac, anesthesiologist for other medications), child’s age and gender [16]. Black children were not more or less likely to receive ketorolac (OR 0.99, 95% CI 0.81-1.22, p=0.94), intravenous lidocaine (OR 1.12, 95% CI 0.87-1.43, p=0.38), or ondansetron (OR 1.34, 95% CI 0.81-2.22, p=0.25) [16]. Doses per weight of the opioids fentanyl and morphine were also not significantly different for black and white patients: mean differences of −0.01 micrograms (mcg) kg−1 fentanyl (95% CI −0.15-0.13, p=0.87) and −0.003 milligrams (mg) kg−1 morphine (95% CI −0.071-0.0015, p=0.19), respectively [16].
Publication 4:
Nafiu and colleagues conducted a prospective study of 771 children less than 18 years old undergoing outpatient surgery from January 2015 through December 2015 [17]. The researchers used a multivariable logistic regression model, adjusting for patient age, gender, race, first recorded recovery room score and intra-operative opioid use to examine differences in likelihood of analgesia receipt between minority and white children [17]. Minority children were “black/ African American, Latino, Asian, Pacific Islander, and American Indian/Alaska Native” [17]. There was no significant difference in likelihood of receipt of any analgesia (OR 1.30, 95% CI 0.86-1.97, p=0.21), but minority children were more likely to receive intravenous opioids than white children (OR 1.63, 95% CI 1.05-2.62, p=0.03) [17]. This difference was not present when the authors examined the subset of children who had undergone tonsillectomy & adenoidectomy [17]. An interaction between race and arousal pain score suggested that white children were less likely to receive opioids than minority children by first pain score (OR 0.86, 95% CI= 0.74–0.99, p=0.046) [17]. The investigators interpreted the negative interaction term to signify that this difference decreased as first pain scores increased [17].
Publication 5:
Maher and colleagues examined retrospective data on 74 children (<18 years old) who underwent pediatric scoliosis surgeries performed at a single center by a single surgeon between 2013-2015 [18]. In this study, black patients had significantly higher blood loss (1.61 ml kg−1 95% CI 1.16-2.23, p=0.0152) after adjusting for scoliosis type, surgical duration, and BMI [18]. The authors then conducted a statistical screen to select covariates for a multivariable model. The subsequent multivariable model adjusted for race and ethnicity and scoliosis type (other potential covariates such as surgery duration and pre-operative hematocrit did not pass the screen): black patients had a 6.25 higher likelihood of receiving a transfusion than white patients (95% CI 1.56-25.06, p<0.01) [18]. There was no difference, however, in the odds of transfusion between white and ‘other’ children [18]. Among patients who were transfused, black patients received 2.61 times higher volume in milliliters (ml) kg−1 of blood than white patients (blood transfusion than White patients (95% CI 1.54-4.41, p<0.01) [18]. The authors were able to replicate the finding that black children had a higher likelihood of transfusion and a greater volume of transfused blood products than white children, even after a sub-group analysis excluding two patients (one white, one black) with extreme blood loss and a sensitivity analysis controlling for use of anti-fibrinolytics [18].
Publication 6:
Wallace and researchers performed a retrospective study on children aged 0-24 months undergoing craniosynostosis repair from 2012 to 2015 [19]. The researchers used Pediatric National Surgical Quality Improvement Program, a national database run by the American College of Surgeons, with peri-operative data from 112 US pediatric institutions [19]. Among other outcomes (mostly related to surgical technique), the authors investigated the duration of “anesthesia time” [19]. Overall, the authors found longer duration of anesthesia for Latino and nonwhite non-Latino children compared to white children. The mean difference between Latino and white non-Latino children was 18.5 minutes (95 CI% 4.7-32.2, p=0.01) and between nonwhite non-Latino children and white non-Latino children was 19.0 minutes (95% CI 2.0- 35.9, p=0.03) [19]. After adjustment for surgical approach, the authors found that the mean difference in anesthesia time between Latino and white non-Latino children was 17.4 min (95 CI% 2.4-32.4, p=0.02) and between nonwhite non-Latino children and white non-Latino children was 15.2 minutes (95% CI −1.3-31.6, p=0.07) [19].
Publication 7:
Nafiu and colleagues expanded upon their 2017 study in this prospective observational study that collected data on children aged 4-17 years who presented for “painful ambulatory surgeries” from January 2015 to June 2016 [20]. The authors’ stated purpose was to create a predictive model for children at risk of requiring intravenous opioids in the recovery room. To do so, they ran three multivariable models with covariates based on the patient’s history, the procedure, and the recovery room [20]. The first model included variables related to patient history alone (sex, age, white/non-white ethnicity, and surgical history); the second model included patient history and procedure-related variables (duration of surgery, pharyngeal surgery, intra-operative morphine equivalents per kilogram, and use of intra-operative multimodal analgesia); the third was patient history, procedure-related variables and recovery room variables (first-recorded recovery room pain score and presence of emergence agitation) [20]. In all three models, non-white children had higher odds of receiving intravenous opioids (OR: 1.48, 95% CI 1.09–2.01, p= .012; OR: 1.49, 95% CI 1.07–2.08, p=.020; OR: 1.61, 95% CI 1.08–2.39, p=.018) [20].
Publication 8:
Baetzel and colleagues conducted a retrospective study of children, aged 0-17 undergoing non-emergent, elective weekday surgeries from January 1, 2012 to January 1, 2018 [21]. The independent variable was race (white/black non-Hispanic) and analysis was stratified by age (<5 years old, 5-9, 10-14, 15-17 years old). Of note, the authors set statistical significance at .05/4=0.013 [21]. In a model adjusting for gender, body mass index, American Society of Anesthesiologist Physical Status 1-4, outpatient procedure, and cardiac procedure, the authors found that black children aged 10-14 years old were more likely than white children to undergo inhalational rather than intravenous inductions of anesthesia (OR 1.32, 95% CI 1.12-1.56, p=0.001) (primary outcome) [21]. This difference did not exist for black children who were younger than 10 years old (age <5 years: OR 0.80, 95% CI 0.60-1.07, p=0.136; age 5–9 years: OR 1.28, 95% CI 0.92-1.76, p=0.139) or older than 14 years (15 years old and older: OR 1.38, 95% CI 1.04-1,82, p=0.025) [21].
The authors had two additional findings. First, black children younger than 15 years old were less likely to have family present at induction (OR range, 0.43–0.69, 95% CI range 0.31–0.84, p < .010 for all). Second, black children less than 5 years old were less likely to receive midazolam (OR 0.87, 95% CI 0.78–0.97, p= .012) [21]. The authors term the findings related to pre-operative midazolam use and presence of family at induction the ‘adultification of black children,’ given that these two strategies are used to allay pediatric patient pre-operative anxiety [21].
Publication 9:
King et al. used anesthetic records of 25,664 children who underwent surgical procedures between May 4, 2014 and May 31, 2018 [22]. In order to examine the primary outcome of receipt of regional anesthesia techniques (which include peripheral nerve and neuraxial blocks), the authors selected covariates using a statistical screen [22]. After adjustment for patient disposition, year, American Society of Anesthesiologist physical status 1-3, surgical/procedural service, need for interpreter, case complexity, patient age, and anesthesiologist, the final model showed no difference in the odds of receiving regional anesthesia for minority as compared to white children (OR 0.95, 95% CI 0.86–1.06, p= 0.36) [22].
King and colleagues also performed sensitivity analyses comparing receipt of regional anesthesia between white children and children of racial and ethnic groups (black, Asian, Pacific Islander, Latino and Other) [22]. Although there was no statistical significance among these results, the point estimates were in different directions: the likelihood of receiving regional anesthesia for black children as compared to white children was 1.21 (95% CI 0.92-1.59) and for Pacific Islander children as compared to white children 0.69 (95% CI 0.45-1.04) [22]. Finally, the authors examined the likelihood of receipt of regional anesthesia for children undergoing orthopedic and urologic procedures, the two services with the highest utilization of regional anesthesia [22]. The authors found no difference in the odds of regional anesthesia for white children as compared to either minority children or children each racial or ethnic group [22].
Publication 10:
In a retrospective study of 139 children who underwent open abdominal or pelvic surgery for tumor resection by a single surgeon between January 2006 and January 2017, Owusu-Agyemang and colleagues studied the odds of receiving two intraoperative health services for “Caucasian” and “non-Caucasian” patients: an epidural for pain control or an intra-operative blood transfusion [23]. The authors did not find a statistical difference for either outcome. For epidural use, the multivariable model adjusted for abnormal coagulation labs and pre-operative opioid use (OR 0.53, 95% CI 0.23-1.21, p=0.132); for intra-operative blood transfusion, the multivariable model adjusted for American Society of Anesthesiologists status 1-4, body mass index, pre-operative opioid use, and anesthesia duration (OR 0.77, 95% CI 0.29-2.04, p=0.60) [23].
Secondary Outcomes: Outcomes of health services
Publication 1:
Jimenez and co-investigators did not report data about child’s level of anxiety after the administration of medication nor about parental or patient anxiety during the course of induction [14]. No data on outcomes resulting from the intra-operative administration of pain medication (i.e. heart rate, blood pressure, electroencephalogram monitoring) were reported [14].
Jimenez and colleagues reported no significant difference in pain scores after surgery [14]. The investigators did not find any differences in early or late pain scores or time spent in the recovery areas between Latino and white children [14]. In addition, there was no difference in opioid side effects of nausea/vomiting; one white child had pruritus and one Latino child had respiratory depression [14].
Publication 2:
Sadhasivam and colleagues found that black children had higher pain scores overall in the recovery room [15]. However, white children had higher opioid-related adverse effects than black children in the recovery room (OR 2.8, 95% CI 1.1-7.6, p=0.039) [15]. White patients also “tended” to have longer lengths of stay in the recovery room as compared to black children (OR 3.4, 95% CI 0.9-13.9, p=0.079) [15]. A race-OSA interaction was found for black children (but not white children) such that they had an increased likelihood of prolonged recovery room stay [15].
Publication 3:
In Rosenbloom and colleagues’ study of black and white children, no data was reported about child’s level of anxiety after the administration of pre-operative midazolam [16]. The authors also did not describe intra-operative outcomes due to the administration of pain medication (i.e. heart rate, blood pressure, electroencephalogram monitoring) [16]. The authors did not find a significant difference in first or highest pain scores in the recovery room (unadjusted analysis) [16].
Publication 4:
Nafiu and colleagues found that minority children (an aggregate of all non-white patients) had longer stays in the post-anesthesia care unit (no point estimates provided) [17]. The authors associated this phenomenon with pain as children with higher first pain scores and children who received any analgesia remained longer in the recovery room: 117.7±72.7 minutes vs. 98.9±52.0 minutes, p<0.001 and 124.1±70.8 minutes vs. 91.5±45.6 minutes, p<0.001 respectively [17].
Publication 5:
Maher and co-investigators collected data on first post-operative hematocrit, any post-operative transfusion, post-operative surgical site infection, and hospital length of stay. In univariate analyses, there was no significant difference in these sequelae among white, black, or ‘Other” patients [18].
Publication 6:
Wallace and researchers did not report any negative outcomes related to longer anesthesia duration for black and Latino patients, including increased risk of anesthetic complications or decreased parent satisfaction [19]. The authors mentioned the risk of neurocognitive deficits for children who underwent anesthesia in infancy, but this outcome was not investigated (likely due to the time course of the study) [19].
Publication 7:
Nafiu and colleagues did not investigate whether non-white children were more likely to have adverse events (nausea and vomiting, prolonged stay in the recovery room) as a consequence of having higher odds of receiving intravenous analgesia [23].
Publication 8:
Baetzel and colleagues did not report any specific data related to clinical consequences of their outcomes. The authors did not, for example, investigate sequelae related to increased odds of inhalational inductions for children aged 10-14 years old, such as airway complications. The study provided no data on how administration of pre-operative midazolam or presence of family members impacted patient or parent anxiety [21].
Publication 9:
The authors did not describe intra-operative outcomes due to the use of regional anesthesia such as markers of adequate pain control or of regional anesthesia complications. The authors also did not report pain scores in the recovery room or in the early post-operative period [22].
Publication 10:
Owusu-Agyemang and researchers found no differences between white and minority patients with regards to the first postoperative hemoglobin value or average pain scores over the first 24 hours after surgery in univariate analysis [23].
Quality of evidence:
We employed the GRADE Criteria to evaluate the quality of evidence regarding each outcome. Overall, the evidence for the 5 outcomes studied was “very low”: all were observational studies and there was serious concern for either bias, indirectness, inconsistency, or publication bias [12-13]. These results are presented in a SoF Table (Supplementary Table).
Discussion:
The objective of this scoping review was to systematically describe the literature on health services disparities in pediatric anesthesia in order to model the populations and services most affected, leading to a foundation for future hypotheses. We found that racial and ethnic minority children may sometimes receive different care than white children. Compared with white children, Latino patients may receive fewer post-operative medications for tonsillectomy and adenoidectomy [14]; black patients may receive more post-operative analgesia for tonsillectomy [15]; minority children may receive more post-operative analgesia for outpatient surgery [17, 20]; black children may receive more transfusions for spinal surgery [18]; black and Latino children may have longer duration of anesthesia when undergoing craniosynostosis [19]; black children may be less likely than white children to receive midazolam or have family present at anesthesia induction and more likely to have inhalational inductions depending on their age [21]. Additionally, we found that, in comparison to white children, black children may not be more likely to receive pre-operative or intra-operative medications when presenting for laparoscopic appendectomy [16] and that minority children may not have different odds of receiving regional anesthesia [22-23]. Five studies examined the clinical outcome of these differences in care [14, 15, 17, 18, 23].
Taken all together, the findings of our review suggest that disparities research in pediatric anesthesia is in early stages. As a recent narrative review notes, the evidence for racial and ethnic health services disparities in pediatric anesthesia is sparse and fragmented [24]. Secondly, the quality of evidence is limited: studies are primarily single-institution and observational studies from tertiary care centers, with only one more recent study utilizing a national database, and examine varied outcomes [24]. While existing studies may present a ‘proof of concept,’ these two observations suggest that disparities research in pediatric anesthesia is nascent.
To develop disparities research in anesthesia, attention to study design, data quality, and selection of outcomes is required. Existing studies offer heterogeneous variables of reported racial and ethnic identity (black vs. Latino vs. minority), procedures included (appendectomies vs. outpatient procedures vs. tonsillectomies vs. tumor resections vs. craniosynostosis), and location under study (recovery room vs. operating room vs. pre-operative area) [14-23]. Although this diversity in studies may be useful in creating a mechanistic model, it also constrains making large-scale conclusions or comparing results across studies. Future studies should seek to create cohesive investigations with covariates that help identify disparities, such as granular indicators of patients’ clinical needs and preferences [3] and detailed information about providers and their practices.
We also need to optimize data quality and quantity. The results of many of the existing studies, limited by small sample sizes and thus potentially under-powered to detect differences, point to the need for large datasets, ideally from multiple institutions and diverse providers. Two of the more recent articles in this review utilized large sample sizes of more than 25, 000 patients [20-21], and future work should expand by examining these questions with national data. Multi-center institutional data could nuance analyses by providing covariates of geographic region, urban/rural settings, and hospital types. In addition, information on parent-provider interactions, infants/neonates, complex procedures such as thoracic or cardiac, and the impact of type of provider (attending physician, training physician, nurse anesthetist) may begin to delineate a comprehensive picture of disparities in care. Currently, few large-scale databases focusing on anesthesia care exist; and among those that do, few provide enough details on all of these variables, particularly race and ethnicity.
Secondly, studies of disparities in health services need well-defined outcomes of both poor and optimal care. To date, core outcomes for anesthesia have not been well-defined, although groups of anesthesiology-researchers are working to change this for both adult and pediatric populations [25-27]. Understanding what constitutes quality and safe care will help to determine goalposts for investigations and naming of disparate anesthetic management. Based on the reviewed studies, for example, it is not wholly clear whether receipt of more opioids is better or worse than receipt of fewer: does it signal a “burden of perioperative pain” [15] or an “advantage” [17]? Likewise, is best care of pediatric tonsillectomy patients to administer short-acting opioids or long-acting ones [14]? And by how much should the odds of transfusion increase in the setting of increased blood loss [18]? Core outcomes for disparities research will also need to consider how anesthesiologists provide information to parents and the process of informed consent.
Our review had several limitations. First, we focused on health services disparities in the United States alone. This choice was purposeful to do justice to the topics: investigations on other sociodemographic factors, other countries, or underlying mechanisms each require their own reviews. Relatedly, we focused solely on anesthesia health services; important associated topics, such as post-operative pain control on surgical wards or at home, were not included. A second limitation is our choice of search terms, although we tried to be as expansive and inclusive as possible. We did not, for example, use terms for particular endpoints such as opioids or anxiolysis. We believe, however, our search allowed us to include as many health services endpoints as possible and that a search with particular outcome terms would not yield different results. Thirdly, although the IOM definition adjusts for “patient preferences” to explain disparities in care [1], recent work has suggested that patient preferences may themselves be formed by disparities in health services such as health education [28]. Our work did not attempt to tease out this link, but this too would be a worthy subject of study, one that is underway [29-32]. Patient/parent preferences, for example, might be informed by parental access to knowledge about opioids or regional anesthesia techniques [29-30]. Fourthly, we used GRADE to characterize the quality of the evidence which does not take into account investigator bias or the willingness of pediatric anesthesia health service researchers to study disparities. Finally, this review did not examine how each identified study might individually provide insight into the mechanisms of disparities in pediatric care: how, for example, does patient language or provider type facilitate equitable care or contribute to disparities? Baetzel et al.’s narrative review offers a patient-provider-systems mechanistic framework which may help to organize future work [24]. Such work will need high-quality study designs and ample data. This review has demonstrated that research on racial and ethnic health services disparities in pediatric anesthesia is in progress. Future work can optimize research methodologies with consideration of outcomes, study design, and granular data across multiple institutions.
Supplementary Material
Acknowledgments:
The authors thank Timothy T. Houle, PhD (Associate Professor, Massachusetts General Hospital, Boston MA, USA) who served as a scientific advisor for this work.
Funding sources: Dr. Rosenbloom’s work on this research was supported by the National Institutes of Health T32 GM007592 grant (Research Training for Anesthetists). All other support was provided from institutional and/or departmental sources.
Footnotes
Conflict of Interests: None
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References:
- 1.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington DC: NAP; 2003. [PubMed] [Google Scholar]
- 2.Agency for Healthcare Research and Quality. 2017 National Healthcare Quality and Disparities Report. November 2018, https://www.ahrq.gov/research/findings/nhqrdr/nhqdr17/index.html (accessed 5/15/2019). [PubMed]
- 3.Cook BL, Mcguire TG, Zaslavsky AM. Measuring racial/ethnic disparities in health care : Methods and Practical Issues. HSR 2012; 47: 1232–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Memtsoudis SG, Besculides MC, Swamidoss CP. Do race, gender, and source of payment impact on anesthetic technique for inguinal hernia repair? J Clin Anesth. 2006; 18: 328–333. [DOI] [PubMed] [Google Scholar]
- 5.Memtsoudis SG, Poeran J, Zubizarreta N, Rasul R, Opperer M, Mazumdar M. Anesthetic care for orthopedic patients: is there a potential for differences in care? Anesthesiology. 2016; 124: 608–623. [DOI] [PubMed] [Google Scholar]
- 6.Glance LG, Wissler R, Glantz C, Osler TM, Mukamel DB. Racial differences in the use of epidural analgesia for labor. Anesthesiology 2007; 106: 19–25. [DOI] [PubMed] [Google Scholar]
- 7.Butwick AJ, Blumenfeld YJ, Brookfield KF, Nelson LM, Weiniger CF. Racial and ethnic disparities in mode of anesthesia for cesarean delivery. Anesth Analg 2016; 122: 472–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silber JH, Rosenbaum PR, Ross RN, et al. Racial disparities in operative procedure time: the influence of obesity. Anesthesiology 2013; 119: 43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Food and Drug Administration. "Pediatric Anesthesia," April/27/2017. https://www.fda.gov/Drugs/DrugSafety/InformationbyDrugClass/ucm527779.htm, (accessed 05/14/2018).
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses : the PRISMA statement. PLoS Med 2009; 6: 1–6. [PMC free article] [PubMed] [Google Scholar]
- 11.Onwuachi-Willig A. Race and racial identity are social constructs. NYT September/06/2016, https://www.nytimes.com/roomfordebate/2015/06/16/how-fluid-is-racial-identity/race-and-racial-identity-are-social-constructs (accessed 07/10/2019).
- 12.Centers for Disease Control and Prevention. The GRADE Approach, an introductory workshop on making recommendations, Part 1. Published March/7/2012, https://www.youtube.com/watch?v=OkejJEmpowA (accessed 10/29/2018).
- 13.Centers for Disease Control and Prevention. The GRADE Approach, an introductory workshop on making recommendations, Part 2. Published March/7/2012, https://www.youtube.com/watch?v=p-5VAqQzsho (accessed 10/29/2018).
- 14.Jimenez N, Seidel K, Martin LD, Rivera FP, Lynn AM. Perioperative analgesic treatment in Latino and non-Latino Pediatric Patients. J. Health Care Poor Underserved 2010; 21: 229–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sadhasivam S, Chidambaran V, Ngamprasertwong P, et al. Race and unequal burden of perioperative pain and opioid related adverse effects in children. Pediatrics 2012; 129: 832–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenbloom JM, Senthil K, Long AS, et al. A limited evaluation of the association of race and anesthetic medication administration: A single-center experience with appendectomies. Paediatr Anaesth 2017; 27: 1142–1147. [DOI] [PubMed] [Google Scholar]
- 17.Nafiu OO, Chimbira WT, Stewart M, Gibbons K, Porter LK, Reynolds PI. Racial differences in the pain management of children recovering from anesthesia. Paediatr Anaesth 2017; 27: 760–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maher KM, Owusu-Akyam K, Zhou J, et al. Analysis of the impact of race on blood transfusion in pediatric scoliosis surgery. Paediatr Anaesthes 2018; 28:352–360. [DOI] [PubMed] [Google Scholar]
- 19.Wallace ER, Birgfeld C, Speltz ML, Starr JR, Collett BR. Surgical approach and periprocedural outcomes by race and ethnicity of children undergoing craniosynostosis surgery. Plast Reconstr Surg 2019; 144: 1384–1391. [DOI] [PubMed] [Google Scholar]
- 20.Nafiu OO, Thompson A, Chiravuri SD, Cloyd B, Reynolds PI. Factors assoociated with recovery room intravenous opiate requirement after pediatric outpatient operations. Anesth Analg 2019; 128: 1225–1233. [DOI] [PubMed] [Google Scholar]
- 21.Baetzel A, Brown DJ, Koppera P, Rentz A, Thompson A, Christensen R. Adultification of black children in pediatric anesthesia. Anesth Analg 2019; 129: 1118–1123. [DOI] [PubMed] [Google Scholar]
- 22.King MR, De Souza E, Rosenbloom JM, Wang E, Anderson TA. Association between race and ethnicity in the delivery of regional anesthesia for pediatric patients: a single-center study of 3189 regional anesthetics in 25,664 surgeries. Anesth Analg 2019; epub [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Owusu-Agyemang P, Cata JP, Kapoor R et al. A retrospective evaluation of the impact of patient ethnicity on the use of epidural analgesia or blood transfusions in children undergoing major oncologic surgery. Periop Med 2019; 20: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baetzel AE, Holman A, Dobija N, Reynolds PI, Nafiu OO. Racial disparities in pediatric anesthesia. Anesthesiol Clin 2020; 38: 327–339. [DOI] [PubMed] [Google Scholar]
- 25.Stricker PA, de Graaff JC, Vutskits L et al. Anaesthesia A. Pediatric perioperative outcomes group : Defining core outcomes for pediatric anesthesia and perioperative medicine. Paediatr Anaesth 2018; 28: 314–315. [DOI] [PubMed] [Google Scholar]
- 26.Myles PS, Grocott MPW, Boney O, Moonesinghe SR, COMPAC-StEP Group. Standardizing end points in perioperative trials: towards a core and extended outcome set. BJA. 2016; 116:586–589. [DOI] [PubMed] [Google Scholar]
- 27.Cravero JP, Sriswasdi P, Lekowski R, et al. Creation of an integrated outcome database for pediatric anesthesia. Paediatr Anaesth 2016; 26: 345–355. [DOI] [PubMed] [Google Scholar]
- 28.Kwoh CK, Vina ER, Cloonan YK, Hannon MJ, Boudreau RM, Ibrahim SA. Determinants of patient preferences for total knee replacement : African-Americans and whites. Arthritis Res Ther. 2015: 17: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosales A, Fortier MA, Campos B, Kain ZN. Postoperative pain management in Latino families: parent beliefs about analgesics predict analgesic doses provided to children. Pediatr Anesth 2016; 26: 307–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown R, Fortier MA, Zolghadr S, Gulur P, Jenkins BN, Kain ZN. Postoperative pain management in children of Hispanic origin: A descriptive cohort study. Anesth Analg 2016; 122: 497–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martin SR, Fortier MA, Kain DI, Tan ET, Huszti H, Wahi A. Desire for perioperative information and parental ethnicity. Pediatr Anesth 2011; 21: 1046–1051. [DOI] [PubMed] [Google Scholar]
- 32.Fortier MA, Gomez SH, Kain A. Motivation and parental presence during induction of anesthesia : an examination of the role of ethnicity and language. Pediatr Anesth 2012; 22: 1094–1099. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.