Abstract
The COVID-19 pandemic has interrupted the usual mechanisms of healthcare delivery and exacerbated symptoms of mental illnesses. Telemedicine has morphed from niche service to essential platform, with newly released guidelines that cover various aspects of tele-mental health delivery. Rehabilitation services, which incorporate a range of psychosocial interventions and liaison services, have been significantly impacted too. They are currently more institute-based than community-based in India. However, recent legislation has mandated that community-based rehabilitation options be available. While a large treatment gap for mental health issues has always existed, telemedicine provides an opportunity to scale services up to minimize this gap. Community-based rehabilitation can be delivered over various platforms, from text to phone to videoconferencing, and various devices. Telemedicine is cost-effective, and enables delivery of services where existing services are inadequate. The recent guidelines allow other healthcare workers to be involved in mental health service delivery. Hence, in addition to direct delivery of services, telerehabilitation can facilitate task-shifting, with mental health professionals mentoring and supervising existing human resources, such as ASHA workers, VRWs, DMHP programme staff, and others.
Tele-rehabilitation also poses challenges - not all needs can be met; access and privacy can be a problem in resource-scarce settings; liaison with existing services is required; and organisations need to plan appropriately and re-allocate resources. Digital access to welfare benefits and interventions must be expanded without disadvantaging those without internet access. Yet, many rehabilitation interventions can be adapted to telemedicine platforms smoothly, and task-shifting can broaden access to care for persons with disability.
Keywords: Community psychiatry, rehabilitation, telemedicine/telecare, telerehabilitation
The COVID-19 pandemic has imposed change in most aspects of daily life and interrupted the regular delivery of health care. One of these changes is that telemedicine has accelerated from a niche service into an essential platform. This crisis has galvanized the release of guidelines for telemedicine,1 telepsychotherapy,2 and telepsychiatric social work practice3 in India. While created during COVID-19, these new guidelines have broad implications for mental health care delivery beyond the pandemic. These changes will not only continue to impact the care and rehabilitation of persons with disabilities (PwDs) but also raise new questions about how these services can be optimally delivered. This article explores how in today’s context, telemedicine can be tapped to provide rehabilitation services (i.e., telerehabilitation).
Rehabilitation in Psychiatry
Disability results from the interaction among the effects of illness, the environment a person lives in, and personal factors.4 Effective health services seek to minimize disability by addressing all these factors together. Psychiatric rehabilitation follows this theme and aims to help “persons with long-term psychiatric disabilities increase their functioning so that they are successful and satisfied in the environments of their choice, with the least amount of ongoing professional intervention.”5 A related term, “recovery,” ties the focus of services explicitly to the perspective of persons with mental illness (PMI) and their search for meaning and purpose.6 Thus, rehabilitation services must be personalized to each individual and help them obtain their unique goals. It is, therefore, imperative that PMIs, families, and caregivers should participate in the planning and implementation of these services. Ideally, the multidisciplinary teams providing the services should include psychiatrists, clinical psychologists (CPs), psychiatric social workers (PSWs), psychiatric nurses, and occupational therapists, who can collaborate to achieve common goals. In resource-sparse settings, these services may have to be delivered by other trained personnel, including peer specialists, who are persons in recovery with lived experience of mental illness. There are myriad resulting interventions that range from engaging PMI in clinical services to the ones that strive to empower PMIs to participate fully in community life. The latter includes supported education, supported employment, supported accommodation, case management, access to welfare benefits, and liaison with a range of stakeholders for accessing community support.
Worsening of the Treatment Gap
PMIs have been significantly impacted by COVID-19 pandemic, with symptom exacerbations and decreased access to mental health services, leading to relapses. Treatment for medical comorbidities has also been affected, resulting in overall worsening of health conditions like diabetes for example.7 Furthermore, the pandemic has been linked to worsening in anxiety and depressive symptoms,8 concerns about stigma, and suicide.9–11 COVID-19 and measures to mitigate it (e.g., lockdowns and social distancing) have disrupted routines of people with developmental disorders as well as their caregivers. Some PwDs could even experience the loss or incapacitation of a caregiver. Significant numbers of PwDs have experienced reduced access to clinical services, instead of the expansion of services that their care and rehabilitation requires. Overall, there is a widening of the treatment gap, which was substantial even before this pandemic. In India, mental illnesses have treatment gaps of greater than 60%; disability estimates across different domains (work, social, and family life) exceed 50% in those with severe mental illnesses.12 The World Health Organization (WHO) indicates that the cost of services for mental health care through primary care services, psychiatric services in general hospitals, and community mental health services is lower than that of long-stay and specialist services. In this reality, resource-scarce settings should focus on the base of the WHO Mental Health Service Organization pyramid (Figure 1),13 with the common goals of enabling PwDs, especially those with severe mental illness, to live in communities and experience equal participation.
Figure 1. WHO Service Organization Pyramid.
Source: Reprinted from the Organization of services for mental health. Mental health policy and service guidance package, integration of mental health services into general health services, Page No. 34, Copyright (2003).
Significance of Community-Based Rehabilitation
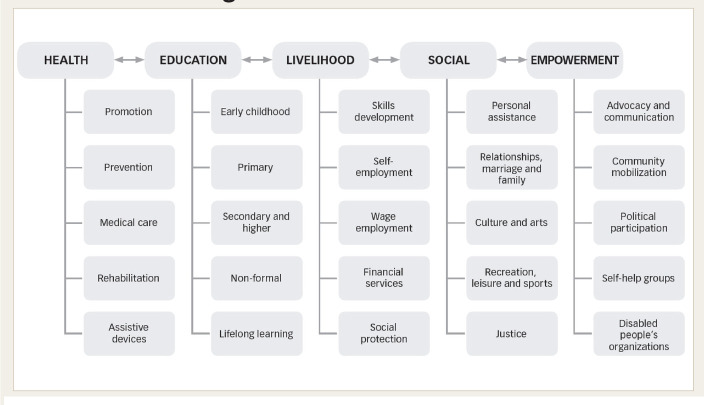
In India, rehabilitation services are mostly institute-based and include daycare services, skills training centers, residential facilities attached to hospitals, halfway homes, and long-stay facilities. Recent Indian legislation—specifically the Rights of Persons with Disability Act, 2016, and the Mental Healthcare Act, 2017—has codified the rights of PwDs to access to community- and home-based rehabilitation.14,15 Community-based services focus on continuity of care and coordination with locally available resources. The staff of the District Mental Health Programme (DMHP), doctors, nurses, and the Accredited Social Health Activists (ASHAs) of the Primary Health Center (PHC) address the health care needs of the PMI. Nongovernmental organizations (NGOs) can empower patients and caregivers through self-help groups, mobilization of aid from local governmental organizations (GOs), skills training facilities, and livelihood opportunities. A host of other grassroots programs and staff working at different levels in communities can provide rehabilitation inputs with professional supervision; these include vocational instructors, village rehabilitation workers, community health workers, etc. For effective rehabilitation, these stakeholders should collaborate to address the domains put forth in the community-based rehabilitation (CBR) matrix, namely health, education, livelihood, social needs, and empowerment (Figure 2).16
Figure 2. The World Health Organization’s CBR Matrix.
Source: Reprinted from community-based rehabilitation: CBR guidelines. Khasnabis C, Motsch, KH, Eds. Introduction, p. 25, Copyright (2010).
Role of Telerehabilitation
To implement a CBR approach effectively, we need to expand the reach and capacity of available human resources, with one solution being task shifting. Telerehabilitation can be defined as a spectrum of services that facilitate rehabilitation, or recovery-focused services, using telecommunication and internet-based communication services. In addition to delivering services directly, it can be used to build human resources and foster task shifting in communities that lack the personnel to offer these services. Rehabilitation services serve PMIs better when they are integrated with clinical services.13,17,18 Thus, changes in rehabilitation must parallel corresponding changes in mental health care delivery. Some areas in which telerehabilitation may play a role are as follows:
Telemedicine
Telepsychotherapy
Telepsychiatric social work and liaison
Supervision of home-based rehabilitation
Training and mentoring of grassroots workers by experts
Teleconsultations with rehab staff can help clients in gainful engagement, activity scheduling, skills training, and monitoring of progress toward goals. Some activities can be adapted for online groups. Long-term engagement and adherence are two important aims of any intervention, whether clinical or rehabilitative. A pilot study from an Indian tertiary care center has shown that this type of aftercare was acceptable, satisfactory, and associated with adequate privacy for patients recently discharged from the hospital.19 The mobile telepsychiatry service from the Schizophrenia Research Foundation (SCARF) comprises a bus with an onboard consultation room and a pharmacy, connects with a psychiatrist in Chennai over wireless internet, and maintains electronic health records. The intervention also includes community health workers who deliver psychosocial interventions, including psychoeducation for caregivers.20
SCARF described their pioneering telepsychiatry services in the southern state of Tamil Nadu, based on their community outreach program, in 2008 and identified key elements: a suitable technology; a convenient location, with local collaboration; building human resources and awareness; establishing peripheral telepsychiatry centers and ensuring case documentation; and accountability.21 The authors also emphasized the need for an Indian telemedicine act and regulatory authority. The Indian telemedicine practice guidelines,1 a guideline for telepsychotherapy services,2 as well as a guideline for telepsychiatric social work (tele-PSW)3 offer frameworks for rehabilitation services to expand their reach. A common feature is allowing the utilization of any platform or software. This frees providers and service users to use the optimal software accessible to both rather than expensive bespoke equipment or single platforms. These guidelines do not specify standards for data management and do not cover aspects such as research, continuing medical education, or remote surgical interventions. The three guidelines cover registered medical practitioners (RMPs), CPs, and qualified PSWs, respectively; the last one includes professional social workers who have been trained to deliver these online interventions. These guidelines could be used to enhance the DMHP and CBR services. Each DMHP team consists of a psychiatrist, nurses, a psychologist, and PSWs.22 Based on these guidelines, all these health care workers can connect with specialist or tertiary care services and deliver effective care to patients who would not otherwise have access to these services. The tele-PSW guidelines allow for group therapies in open (used primarily for psychoeducational purposes) or closed groups, which are homogeneous or heterogeneous, where participants share specific needs. They cover areas such as working with communities, advocacy, networking, and continuity of care. They also address capacity-building and hands-on training. Notably, they enable supervision of home-based rehabilitation, especially when daycare and other services are closed or unavailable. Thus, these guidelines provide several ways to connect PMIs and caregivers to primary and specialist services (Figure 3). The different DMHP personnel could deliver a range of complementary telehealth services, both directly and indirectly: from treatment engagement services by the nurse to psychosocial interventions and group therapies by the psychologist and social workers to supervised consultations by PHC doctors overseen by the psychiatrist.
Figure 3. Methods of Outreach Using Teleservices.
MHP: mental healthcare provider, TSP: healthcare worker who is trained in task shifting, PMI: persons with mental illness. solid lines: direct interactions, dashed lines: interaction via telecommunications platforms.
Indian telemedicine guidelines classify services according to (a) mode of communication (text, voice, video, etc.), (b) when information is transmitted between persons (real-time versus asynchronous responses), (c) stage of consultation (first-time versus follow-up consultations), and (d) individuals involved (patient to RMP, caregiver to RMP, RMP to RMP, and health worker to RMP). The last classification defines health workers as a “nurse, allied health professional, mid-level health provider, ANM, or any other health worker designated by an appropriate authority.” The guidelines thus explicitly allow a variety of rehabilitation professionals and members of the multidisciplinary team to interact with psychiatrists or RMPs via telemedicine services. Telemedicine guidelines provide for caregivers to be involved in consultations with patients. They also allow consultations with caregivers without the client in cases where the patient is a minor or where the “caregiver has a formal authorization or a verified document establishing his relationship with the patient and/or has been verified by the patient in a previous in-person consult (explicit consult).” These measures will address the issues concerning confidentiality and consent.
The “Best Practices in Videoconferencing-Based Telemental Health,” released by the American Psychiatric Association (APA) and the American Telemedicine Association (ATA), go beyond the Indian telemedicine guidelines in accepting the role of organizations involved in patient care, and it also guides specific clinical populations (geriatric age group, children and adolescents, etc.) who face different challenges (and opportunities) when using telemental health care services. Similar to the Indian guidelines, a recent notification from the U.S. Department of Health & Human Services allowed for “good faith provision of telehealth during the COVID-19 nationwide public health emergency” even if HIPAA privacy requirements—mandated by the APA/ATA guidelines—were not fully complied with.23
Evidence for Telemental Health Services
Reviews note that telemental health services are comparable to in-person services, in terms of reliability and treatment outcomes; are cost-effective, especially with a larger volume of patients, in isolated communities or those with limited professional resources; can involve nonprofessional providers to play effective roles in therapy.24–26 Behavioral therapies delivered through telepsychotherapy are consistently found to be effective: it improves drug compliance, indicates better functional performance, reduces symptoms, and improves quality of life in those with medical comorbidities.26 Likewise, telemental health services—including family and group services—are feasible across a spectrum of patients with special needs and across age groups, from children to the elderly to those who are incarcerated. Some advantages in the geriatric age group are avoidance of unneeded hospitalizations; reductions in travel time, fuel costs, physician travel time, and personnel costs;27 and the potential to match cultural, ethnic, and language matching with providers. The APA telepsychiatry toolkit observes that certain patient groups (e.g., children and adolescents in the autism spectrum, patients with disabling anxiety) can show greater acceptance for telepsychiatry services.28,29 Although telemedicine applications have been used for computer-based screening assessments, telephone-based recovery supports, and telephone-based therapy for addictive disorders,30 its use is limited otherwise. Hence, app-based interventions for a variety of interventions from craving management to supervised medications require further consideration. Similarly, evaluation of many other aspects when using telemedicine is required like prescribing controlled drugs like buprenorphine, the ideal frequency of in-person and telemedicine-based monitoring of patients who are at risk of relapse, and the effectiveness of supportive therapies, including group therapies.31
Reach of Teleservices in India
A recent report estimated that India has more than 504 million active internet users above the age of 5 years;32 internet penetration is around 40%, with rural sector growth outpacing the urban sector; users accessed the internet mostly on mobile devices ( 99%); nearly 70% of users accessed the internet daily. However, women have less access to internet access, and some families share devices. Overall, there is a rapidly growing user base to whom teleservices can reach today, even though access can always be further improved. Through a welcome move, the government has digitized applications and issue for disability certificates through the Unique Disability ID (UDID) scheme; several welfare benefits are also being disbursed through digital platforms. Currently, the UDID can only be issued by a medical board closest to the residence of PwD.
Experiences From an Academic Tertiary Care Center
In the National Institute of Mental Health and Neuro Sciences (NIMHANS), services have pivoted to deliver telemental health services during the COVID-19 crisis to ensure continuity of care for patients who were unable to avail outpatient services. The Psychiatric Rehabilitation Services unit temporarily closed its daycare services but connected with clients through telephone and videoconferencing-based consultations. A variety of needs were addressed like access to medicines (e-prescriptions, home delivery of drugs, free drugs for those in need, etc.), referrals for the treatment of medical comorbidities, financial support, liaison with employers, liaison with police for clients who went missing, and inpatient care for clients who required it. Community mental health services shifted from in-person consultations provided by mental health professionals at primary health centers to teleconsultations. A social worker coordinated follow-up consultations by working with the primary care doctor in one rural community service as he used voice and video-based consultation with professionals at NIMHANS. In another community service, a social worker coordinated follow-up teleconsultations between a patient or family member or a health worker with the psychiatrist at NIMHANS. Medications, as well as ration kits, could be delivered to remote areas by liaising with governmental and nongovernmental agencies and health workers who had travel passes during the lockdown period.
The Karnataka State Holistic Empowering Programme for Mental Ailments (KSHEMA) project, designed to address the rehabilitation needs of those with severe mental illness in rural areas, has begun in 10 taluks in Karnataka. Services will be delivered by social workers at the taluk level, under the supervision of a multidisciplinary team from NIMHANS, who would facilitate access to clinical services from the DMHP and local Primary Health Centers (PHCs). They focus on follow-up and liaison with medical officers and psychiatrists, and on access to disability welfare benefits. The project also seeks to build capacity by training and handholding the medical officers to treat persons with severe mental illnesses, so that clients may access help closer to home. Telemental health services will be used to connect with taluk social workers as well as medical officers to ensure that the continuity of care is maintained and that multiple rehabilitation needs are addressed. The project offers a glimpse of how to develop services that bring rehabilitation and recovery closer to clients, using teleservices.
Challenges and Limitations of Telerehabilitation
Telerehabilitation also has its challenges. There can be privacy concerns while accessing services. People may lack access to smart devices or computers, especially if multiple users use the same device, or may have difficulty using devices and software effectively. Daycare services fulfill different needs such as activity scheduling, socialization, building self-esteem, learning instrumental activities, making friends, mentorship, and hands-on training, which cannot be met via teleservices alone. Also, family members may find supervising home-based activities difficult. Expressed emotions and disclosure of symptoms may be different when PMIs pursue activities independently from their caregivers, a difficult need to address with telerehabilitation alone. Many organizations now face challenges of reviewing budget allocations, training their personnel, and realigning their patterns of work to deliver teleservices. Long-term institute-based services, which include halfway homes, long-stay homes, supported accommodation, and supported employment, have a prominent role for in-person delivery of services. However, teleservices can augment them through remote supervision of therapies provided by caregivers, liaison, and follow-up. These hold good for custodial settings for children who are in conflict with the law or in need of care and protection, as well as in other group settings such as orphanages and group housing facilities. In custodial settings such as prisons, while telepsychiatry can have greater potential to ensure access to services, the challenges—such as requiring buy-in from other prison staff; multiple reporting hierarchies for psychiatrists and other personnel; and a lack of contextual, day-to-day information about prison activities for telehealth professionals—must be planned for.33 For some critical indications, e.g., clinical emergencies such as suicidality, in-person services are recommended.
Agenda for the Future of Telerehabilitation in Psychiatry in India
Rehabilitation services do not occur in a vacuum. India needs to extend the reach of its telecommunications infrastructure, with initiatives such as BharatNet for rural broadband to reach the neediest people. There is a need for modification of the UDID system for the government to fulfill its commitment to issue disability certificates from the facilities where the PwD is receiving care. Current guidelines do not allow psychological assessments such as assessment of intelligence quotient (IQ), specific learning disability, etc., to be performed via teleservices. This aspect may be appropriate as these activities need accurate in-person observations (such as eye gaze), regard for the specific psychometric properties of tests, confidentiality, and need for the calm environment during testing necessitate in-person assessment. However, studies show that in the case of videoconference-based evaluation of psychiatric symptoms by using scales like the Brief Psychiatric Rating Scale (BPRS), the Hamilton Depression Rating Scale (HDRS), and the Positive and Negative Syndrome Scale (PANSS), comparable results have been obtained to in-person assessments. These studies also observe that better bandwidth and video quality improve assessment accuracy, especially for scales that assess negative symptoms or depend on nonverbal cues.34 The literature on social skills assessments is relatively sparse, though assessments and early interventions for autism have been shown to be broadly feasible and comparative to in-person services for some interventions, but more rigorously designed trials are required.35,36 Further research into the feasibility and accuracy of different types of assessments—for clinical symptoms and disability—could help policymakers understand which of them can and cannot be done over a telepsychiatry platform; this could ease access to disability benefits for the neediest PwDs. Hence, accessing welfare benefits will require a mix of in-person services and telemental health services. How these will be delivered will vary with local conditions. In some places, the camp approach may work best, but in other areas where travel and access to facilities are limited, mobile units like the SCARF telepsychiatry mobile unit20 may be better suited to reach out to PMIs. Governments must offer as many services as possible over telemental health services without disadvantaging those who lack access to digital services. The Central and State governments must also strive to allow for clients to remotely access benefits such as pensions and insurance, by using and improving the same protocols for identification that these telemedicine guidelines rely upon.
Many rehabilitation services can and should be delivered via telemedicine. Evidence for delivery of mental health services suggests that telemedicine provides comparable care and is cost-effective, but we need more studies on which local resources best complement telerehabilitation. Services need to adapt to populations with specialized needs, such as children, the elderly, and those in forensic settings, among others. Telemedicine services may thrive when we use existing services such as the DMHP program, or a program like a taluk mental health service delivery project, to help clients in their journey through recovery. As new frontiers of mental health like smartphone apps and sensors evolve to offer effective and personalized care, telemedicine services for psychiatry will continue to expand. A strong foundation today can take the first steps and reduce the large treatment gap by facilitating task shifting from specialists to health care workers based in the community.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Board of Governors in supersession of the Medical Council of India. Telemedicine Practice Guidelines—enabling registered medical practitioners to provide healthcare using telemedicine. New Delhi: Govt of India, 2020, p. 48. [Google Scholar]
- 2.Department of Clinical Psychology, NIMHANS. Guidelines for tele-psychotherapy services. Bengaluru: National Institute of Mental Health and Neuro Sciences, 2020. [Google Scholar]
- 3.Department of Psychiatric Social Work NIMHANS. Guidelines for tele-psychiatric social work practice. National Institute of Mental Health and Neuro Sciences, 2020, p.X+38. [Google Scholar]
- 4.World Health Organization. International classification of functioning, disability and health: ICF. Geneva: World Health Organization, 2001. [Google Scholar]
- 5.Farkas MD, Anthony WA. Psychiatric rehabilitation programs: Putting theory into practice. Boston, MA: Johns Hopkins University Press, 1989. [Google Scholar]
- 6.Anthony WA. Recovery from mental illness: The guiding vision of the mental health service system in the 1990s. Psychosocial Rehab J; 1993; 16: 11–23. [Google Scholar]
- 7.Li W, Yang Y, Liu ZH. et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci; 2020; 16: 1732–1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. Mental health—household pulse survey, https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm (2020).
- 9.Kar SK, Yasir Arafat SM, Kabir R. et al. Coping with mental health challenges during COVID-19. Coronavirus Disease 2019 (COVID-19) 2020: 199–213. [Google Scholar]
- 10.Goyal K, Chauhan P, Chhikara K. et al. Fear of COVID 2019: First suicidal case in India! Asian J Psychiatr; 2020; 49: 101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dsouza DD, Quadros S, Hyderabadwala ZJ. et al. Aggregated COVID-19 suicide incidences in India: Fear of COVID-19 infection is the prominent causative factor. Psychiatry Res; 2020; 290: 113145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gururaj G, Varghese M, Benegal V. et al. National Mental Health Survey of India 2015-16: Summary. Bengaluru: National Institute of Mental Health Neuro Sciences NIMHANS, 2016. [Google Scholar]
- 13.World Health Organization. Organization of services for mental health. Geneva: World Health Organization, 2003 (Mental health policy and service guidance package). [Google Scholar]
- 14.The Mental Healthcare Act, 2017. India: 2017. https://www.indiacode.nic.in/handle/123456789/2249?view_type=browse&sam_handle=123456789/1362 [Google Scholar]
- 15.The Rights of Persons With Disabilities Act, 2016. India: 2016. https://www.indiacode.nic.in/handle/123456789/2155?view_type=browse&sam_handle=123456789/1362 [Google Scholar]
- 16.World Health Organization. Community-based rehabilitation: CBR guidelines. Malta: World Health Organization, 2010. [PubMed] [Google Scholar]
- 17.Kopelowicz A and Liberman RP.. Integrating treatment with rehabilitation for persons with major mental illnesses. Psychiatr Serv; 2003; 54: 1491–1498. [DOI] [PubMed] [Google Scholar]
- 18.Nieuwenhuijsen K, Faber B, Verbeek JH. et al. Interventions to improve return to work in depressed people. Cochrane Database Syst Rev; 2014; 12: CD006237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Das S, Manjunatha N, Kumar CN. et al. Tele-psychiatric after care clinic for the continuity of care: A pilot study from an academic hospital. Asian J Psychiatr; 2020; 48: 101886. [DOI] [PubMed] [Google Scholar]
- 20.Thara R and Sujit J.. Mobile telepsychiatry in India. World Psychiatry; 2013; 12: 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thara R, John S, Rao K. Telepsychiatry in Chennai, India: the SCARF experience. Behav Sci Law; 2008; 26: 315–322. [DOI] [PubMed] [Google Scholar]
- 22.van Ginneken N, Jain S, Patel V. et al. The development of mental health services within primary care in India: Learning from oral history. Int J Ment Health Syst; 2014; 8: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United States Department of Health & Human Services. Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency, https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html (2020, accessed 21 July 2020).
- 24.Hubley S, Lynch SB, Schneck C. et al. Review of key telepsychiatry outcomes. World J Psychiatry; 2016; 6: 269–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Langarizadeh M, Tabatabaei MS, Tavakol K. et al. Telemental health care, an effective alternative to conventional mental care: a systematic review. Acta Inform Med; 2017; 25: 240–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bashshur RL, Shannon GW, Bashshur N. et al. The empirical evidence for telemedicine interventions in mental disorders. Telemed J E Health; 2016; 22: 87–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hilty D, Yellowlees PM, Parrish MB. et al. Telepsychiatry: effective, evidence-based, and at a tipping point in health care delivery? Psychiatr Clin North Am; 2015; 38: 559–592. [DOI] [PubMed] [Google Scholar]
- 28.The American Psychiatric Association. The American Psychiatric Association telepsychiatry toolkit—clinical outcomes, https://www.psychiatry.org/psychiatrists/practice/telepsychiatry/toolkit/clinical-outcomes(2020).
- 29.Nelson E-L, Duncan AB, Lillis T. Special considerations for conducting psychotherapy over videoteleconferencing. In: Myers K and Turvey CL (eds) Telemental health: clinical, technical, and administrative foundations for evidence-based practice. San Francisco, CA: Elsevier, 2013, pp. 295–314. [Google Scholar]
- 30.Molfenter T, Brown R, O’Neill A. et al. Use of telemedicine in addiction treatment: Current practices and organizational implementation characteristics. Int J Telemed Appl; 2018; 2018: 3932643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin LA, Fernandez AC, Bonar EE. Telehealth for substance-using populations in the age of coronavirus disease 2019: recommendations to enhance adoption. JAMA Psychiatry; 2020. DOI: 10.1001/jamapsychiatry20201698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Internet and Mobile Association of India (IAMAI) and Nielsen. Digital in India 2019—Round 2 Report. 2019. https://cms.iamai.in/Content/ResearchPapers/2286f4d7-424f-4bde-be88-6415fe5021d5.pdf
- 33.Kaftarian E. Lessons learned in prison and jail-based telepsychiatry. Curr Psychiatry Rep; 2019; 21: 15. [DOI] [PubMed] [Google Scholar]
- 34.Sharp IR, Kobak KA, Osman DA. The use of videoconferencing with patients with psychosis: A review of the literature. Ann Gen Psychiatry; 2011; 10: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Knutsen J, Wolfe A, Burke BL. et al. A systematic review of telemedicine in autism spectrum disorders. Rev J Autism Dev Disord 2016; 3: 330–344. [Google Scholar]
- 36.Sutherland R, Trembath D, Roberts J. Telehealth and autism: A systematic search and review of the literature. Int J Speech Lang Pathol; 2018; 20: 324–336. [DOI] [PubMed] [Google Scholar]