Highlights
-
•
Intracranial branch of the RLN is a very rare variation with 0.2% prevalence rate.
-
•
We reported this rare RLN variation in the right side and unilaterally.
-
•
The RLN injury during thyroid surgery is common and surgeon needs to know now the anatomical variation well.
Keywords: Anatomy, Intracranial branch, RLN, Thyroidectomy
Abstract
Introduction
The recurrent laryngeal nerve (RLN) originates from the Vagus nerve intrathoracically. It passes through the tracheoesophageal groove (TEG) in the neck and different variations in this section were observed. The RLN is at highest risk for injury during the thyroid surgery. Therefore, it is important to know variations to decrease the injury effectively.
Presentation of case
A 50 years-old woman with no thyroid related complaints except for enlargement of the thyroid gland in recent 12-months that annoyed her during neck movement and for aesthetic features. Medical, surgical, drugs, irradiation history, laboratory data, and physical examination was unremarkable except for multi-lobulated enlarged thyroid gland. The CT scanning study revealed intrathoracic extension of the gland. Patient underwent total thyroidectomy with suspicious diagnosis of multinodular goiter which was confirmed later by pathologic study. Intraoperative exploration of the right RLN discovered an intracranial branch originating from the recurrent laryngeal trunk just beneath the inferior thyroid artery (ITA) at the level of the nerve intersection. The branch then passed laterally about 1 cm and penetrated in ipsilateral carotid sheath.
Discussion
The RLN has different anatomical variations in either the right or the left side of the neck. However extra-laryngeal nerve branching is the most common variation but other seldom variations including the non-RLN, and intracranial branch should be mentioned by surgeon intraoperatively.
Conclusion
To decrease iatrogenic injuries to RLN and its associated nerve branches knowledge of the nerve anatomy is mandatory for surgeon to prevent morbid side effects.
1. Introduction
The recurrent laryngeal nerves (RLN) are branches originate normally from the vagus nerves in the thoracic space that have different anatomical courses in the right and the left side [1]. The nerves pass from tracheosophageal grooves (TEG) bilaterally in the neck and finally innervate laryngeal components, esophagus and trachea [2]. The nerve compounds of sensory, motor and parasympathetic fibers [2]. Anatomical variations of the RLN in both sides are introduced. Considering the latter one branch nerve (68–80%), extra-laryngeal divergence (11–25%), fan-shaped divergence (5–7%), non-recurrent nerve (0.4–1%), and others (<0.5%) were described [[3], [4], [5], [6]]. Injury to the nerve or branches are probable during thyroid surgery. However, in one third of unilateral nerve injuries no symptom is appeared hoarseness, dysphonia, dyspnea, and dysphagia present among the others [2,7]. Bilateral nerve injury is a catastrophe; gastric content aspiration, pneumonia, glottal compromise, and complete airway obstruction which concern to perform emergent tracheotomy insertion to save patient’s life are included [1,2,[5], [6], [7], [8], [9], [10]]. Since thyroid cancer incidence has been grew recently RLN palsy as the most common hazardous complication of thyroid surgery is increased identically [5,8]. To decrease the latter novel technique like intra-operative neuromonitoring (IONM) was utilized. Despite the latter, visual identification of the nerve is still the gold standard of the nerve determination [6,8,10]. Regarding the aforementioned data awareness of the anatomical variations of the RLN is highly mandated for thyroid surgeons.
The current report introduces a patient with the intracranial branch of the right RLN as a very rare type of the nerve variation in lined with the SCARE 2018 criteria [11].
2. Case presentation
A 50 years old woman claiming of a lobulated large cervical mass referred to our surgical clinic. She was disturbed during neck movement. Mild dysphagia for hard foods was reported. There was neither dyspnea nor voice change. Pain, fever, weight loss, hyperhidrosis, gastro-intestinal symptoms, sleep disturbance, and narcolepsy were not mentioned. The mass had been enlarged during the previous year and the patient became worry about the size and aesthetic changes. There was no past medical and surgical history except of minor depression. She also had no history of neck irradiation in her life. She did not use any herbal or chemical medications regularly. She didn’t smoke and drink. The family history either for thyroid or for the multi-endocrine neoplasm was unremarkable. Allergy history was negative and patient had no recent travels during the last 2 years. On physical examination, she was afebrile (Toral: 37.2°c), blood pressure 125/65 mmHg, heart rate 77 and respiratory rate 14 per minute. The BMI was measured 28.6 kg.m−2. Classic neck examination for thyroid gland on semi-extended cervical position revealed multi-lobulated thyroid gland that was larger in left side of the neck and extended toward the thoracic inlet inferiorly, over the sternocleidomastoids laterally, and near to the hyoid bone superiorly. Malignant firmness, tenderness, discoloration, and immobility of the mass were not identified. Other body system physical examination including of the skin, eyes, heart, lungs, bones, joints, abdomen, and pelvic was non-diagnostic.
Biochemical laboratory studies showed normal results. The TSH was 3.6 (0.5–5 mIU/L). The free thyroxine (FT4) and free triiodothyronine (FT3) hormone were measured 1.2 (0.9–1.7 ng/dL) and 3.8 (2.3–4.1 pg/mL) respectively. Other tests including of complete blood count, BUN, Creatinine, ESR, CRP, PTH, calcium, phosphorus, PRL, FSH, LH, triglyceride, LDL-cholestrol, liver functional test, and β-hCG (non-pregnant) had normal values.
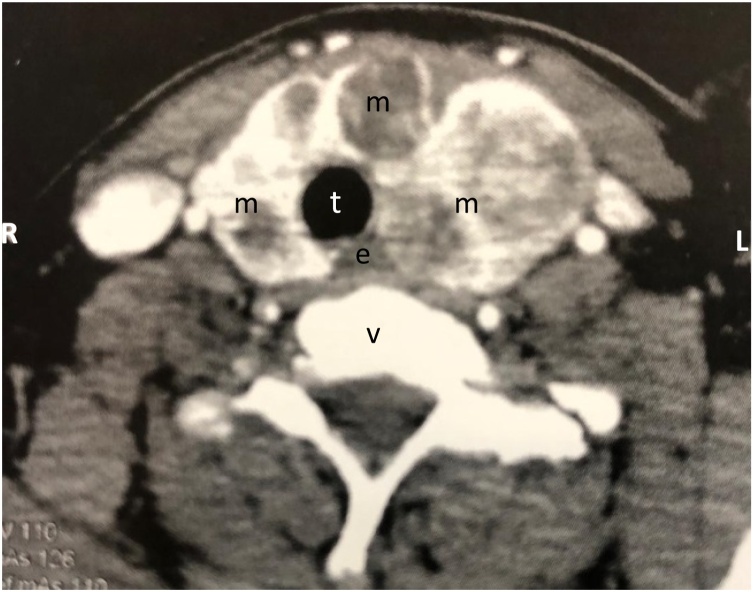
Based on above clinical findings patient was underwent multi-sliced computed tomography (CT) scan of the cervico-thoracic field to determine intra-thoracic extension of the mass and probable adjacent organ invasion. The CT showed a very large (48 and 92 mm in greatest horizontal and vertical dimensions respectively) multi-lobulated thyroid gland with diffused internal heterogeneity which extended to the superior mediastinum inferiorly and also made the trachea deviated to the right side without compromising and/or invasion to adjacent elements. Fig. 1 shows a slice of patient’s CT scan.
Fig. 1.
A slice of patient’s CT scan. e: esophagus, m:mass of thyroid gland, t:trachea, and v:vertebra.
Lastly patient was considered highly suspected for multi-nodular goiter and candidate to undergo total thyroidectomy.
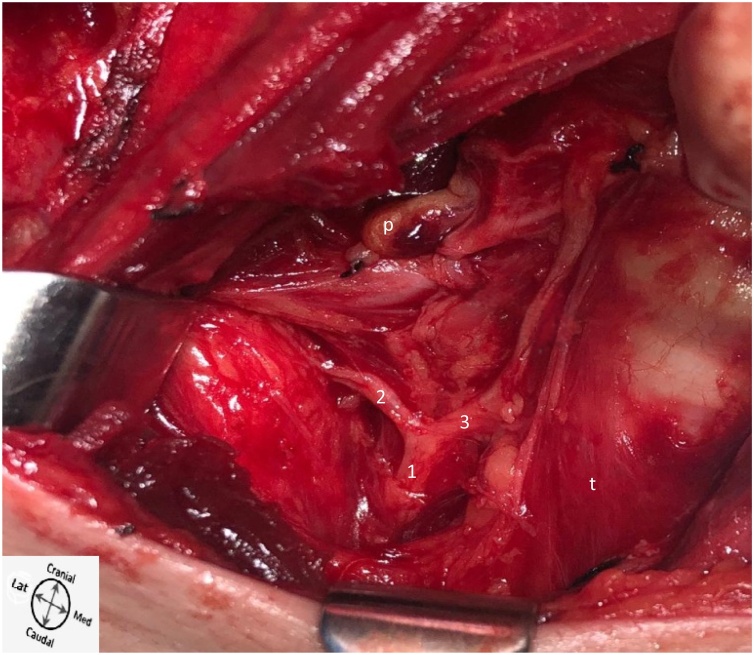
In operating room general anesthesia was induced followed by patient preparation and drape. A vascular surgeon, a general surgery chief resident and a licensed aid with operating room educational degree were present at the operating bed. Classic collar incision was made followed by soft tissue layers dissection up to thyroid membrane. Then middle thyroid veins were exposed and ligated bilaterally. Thyroid gland gently delivered from medial border of the SCMs in both sides. Then elements of superior poles were isolated, ligated and transected bilaterally. Intra-thoracic component of the gland was meticulously retracted out. To identify the RLNs visual approach was considered. In the left side the one branch RLN was crossed with inferior thyroid artery (ITA) posteriorly and passed through the TEG since penetrated to larynx superiorly at the level of the Berry’s ligament. The right RLN firstly was found in crossed with posterior aspect of the ITA adjacent to the inferior pole. Just behind the ITA and prior to that the RLN arrived to lay on the TEG, the intracranial branch was derived from the right RLN trunk. The intracranial nerve then travelled about 1 cm laterally and finally entered to the right carotid sheath. Fig. 2 shows observed intra-operative anatomy of the latter rare variation. After visual confirmation of that the RLNs were delivered to the larynx, inferior pole elements also were identified and transected following ligation. Total thyroidectomy then was completed by separation of the gland from the trachea at the level of the Berry’s ligament. Additionally, on the left side lymphadenopathy with benign appearance was detected in cervical zone III. The latter was also excised and sent to pathology lab with the removed thyroid. Two closed suction drains were fixed. The operation without complication was finished with soft tissue repairs followed by direct visual confirmation of non-paralytic symmetric position of the vocal cords through the laryngoscopy after tracheal tube was extubated.
Fig. 2.
Intracranial branch derived from the right RLN trunk. 1:RLN trunk, 2:intracranial branch, 3:RLN, p: parathyroid, and t:trachea.
The macroscopic pathologic study for thyroid sample revealed a total thyroid gland composed of two lobes that joined by the isthmus. Considering the size, the right lobe, isthmus, and left lobe were measured 7.5 × 5×3, 4 × 3×3, and 9 × 5 × 4.5 cm respectively. Finally 17 blocks of specimen were prepared for microscopic evaluation which showed the features of multi-nodular goiter in all blocks. Chronic lymphadenitis change was reported for the lymph node. After a week of surgery patient was visited. There was neither local complication for the site of the surgery nor RLN function including of voice changes, hoarseness, eating disorder, aspiration, and etc. Hence, patient was introduced to an endocrinologist to manage her thyroid drugs.
3. Discussion
The RLN palsy is the most serious complication of the thyroid surgery. Transient palsy is more prevalent than the permanent (3–10% Vs 0.3–3%, respectively) [1,4,8]. The larynx fundamentally protects from the inferior airway tree in addition to generate voice, allow the airway control, and produce positive intra-thoracic pressure for coughing, sneezing, and lifting [7]. The RLN injury disturbs laryngeal functions. The nerve contain sensory, motor and parasympathetic fibers [1]. The mechanisms of nerve morbidity including transection, clamping, stretching, ligature entrapment, electrothermal injury, and ischemia occur intraoperatively [8]. The extension of anatomical variation of the RLN makes it vulnerable to injury. Although new diagnostic method like the IONM is presented to identify the nerve, direct visual identification of the nerve is still the gold standard [1,8]. Therefore, having good awareness of the variations is mainstay to prevent nerve damage. Extra-laryngeal branching (11–30%) is the most common variation that surgeon encounter followed by fan-shaped divergence, distant laryngeal point of entry, distorted, intertwining with ITA, non-recurrent, sympathetic laryngeal anastomotic branch, and others [[1], [2], [3], [4], [5],8]. Autopsy studies revealed that unilateral variation of the RLNs is up to 65% while bilateral types in a same cadaver reached just to 9% [3]. Previous studies implied on that the right-sided variation whether for the type or for the prevalence happens more comparing to the left [[1], [2], [3],6]. The mostly reliable anatomical landmark to identify the RLNs is the nerve relation to the ITA. In both sides intersection of these two elements i.e. the nerve and the artery occurs adjacent to the inferior thyroidal pole beside the trachea [1,2,6]. However the intersection has itself variation types too. Considering relevant observations the RLNs may reside either superior or beneath the ITA in a single case contralaterally [1,2,6]. Nerve injury would be in association with no symptoms or hoarseness in patients with unilateral injury to complete airway obstruction and even death in bilateral nerve damage [1,2,6,7]. Thus, it seems very important for thyroid surgeon to have qualified anatomical knowledge of the operation field especially for the RLNs types. The current study presented a very rare intracranial nerve branch variation that derived from the right recurrent laryngeal nerve trunk just beneath the ITA and after travelling about 1 cm laterally penetrated to the ipsilateral carotid sheath. The prevalence of this type of nerve variation was reported up to 0.2% previously in a study with over 3270 RLN exploration [1].
4. Conclusion
The RLN anatomical variation is common. Concurrent to increased thyroidectomies RLN injury heightened as the most serious intraoperative complication. Visual identification of the nerve is the gold standard to prevent nerve damage. Obtaining this goal directly depends on the qualified anatomical knowledge about the RLN types intraoperatively. The intracranial branch accompanied by the RLN is one of the mostly rare anatomical nerve variations which should be mentioned by thyroid surgeon at the time of surgery.
Declaration of Competing Interest
We did not have any financial or non-financial conflict of interest for presenting this report.
Funding
We did our work under the setting of Yasrebi Hospital Complex, Kashan, Iran.
Ethical approval
This study was approved by ethics committee of Yasrebi Hospital Complex.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Arash Moradi: Direct surgeon, data collection, interpretation.
Abbas Hajian: First aid, data collection, manuscript drafting.
Registration of research studies
Not applicable.
Guarantor
Abbas Hajian.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgement
We present respectfully our great thanks to the Yesrebi Hospital Complex, Kashan, Iran; for preparing the high-tech setting to service patients.
Contributor Information
Arash Moradi, Email: dr.arash-moradi@hotmail.com.
Abbas Hajian, Email: abbashajian@ymail.com.
References
- 1.Shao T. Anatomic variants of the recurrent laryngeal nerve in Chinese patients: a prospective study of 2,404 patients. Sci. Rep. 2016;6 doi: 10.1038/srep25475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fahim D.K., Thomas A.M., Gemechu J.M. Anatomical variations of the recurrent laryngeal nerve and implications for injury prevention during surgical procedures of the neck. Int. J. Anat. Var. 2020;13:3. doi: 10.3390/diagnostics10090670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gurleyik E. Three variations of the laryngeal nerve in the same patient: a case report. J. Med. Case Rep. 2011;5:266. doi: 10.1186/1752-1947-5-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yin C., Song B., Wang X. Anatomical variations in recurrent laryngeal nerves in thyroid surgery. Ear Nose Throat J. 2020 doi: 10.1177/0145561320927565. [DOI] [PubMed] [Google Scholar]
- 5.Ling Xing Yao, Smoll Nicolas. A systematic review of variations of the recurrent laryngeal nerve. Clin. Anat. 2015:29. doi: 10.1002/ca.22613. [DOI] [PubMed] [Google Scholar]
- 6.Wojtczak B., Kaliszewski K., Sutkowski K., Bolanowski M., Barczyński M. A functional assessment of anatomical variants of the recurrent laryngeal nerve during thyroidectomies using neuromonitoring. Endocrine. 2018;59(1):82–89. doi: 10.1007/s12020-017-1466-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lalruatkimi K. Recurrent laryngeal nerve: anatomical perspective. Otolaryngol. Online J. 2015;5(3.5) [Google Scholar]
- 8.Chiang F.Y., Lu I.C., Chen H.C., Chen H.C.Y., Tsai C.J. Anatomical variations of recurrent laryngeal nerve during thyroid surgery: how to identify and handle the variations with intraoperative neuromonitoring. Kaohsiung J. Med. Sci. 2010;26(11):575–583. doi: 10.1016/S1607-551X(10)70089-9. [DOI] [PubMed] [Google Scholar]
- 9.Ng Caecilia, Woess C., Maier H., Schmidt V.M., Lucciarini P. Nerve at risk: anatomical variations of the left recurrent laryngeal nerve and implications for thoracic surgeons. Eur. J. Cardio-thoracic Surg. 2020:ezaa258. doi: 10.1093/ejcts/ezaa258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu G., Wang K. A novel variation of the recurrent laryngeal nerve. BMC Surg. 2017;17:66. doi: 10.1186/s12893-017-0263-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]