Abstract
Objectives: The purpose of this analysis was to assess, from the patients’ perspective, the effectiveness and relative safety of tramadol as an off-label antidepressant and to determine if patients’ views and experiences are consistent with the biomedical literature. Method: A data mining approach was used to analyze databases available at drugs.com. Results: Tramadol was reported to be an effective or very effective antidepressant by 94.6% of patients (123/130) who provided ratings submitted to User Reviews for Tramadol to Treat Depression (https://www.drugs.com/comments/tramadol/for-depression.html). When compared to 34 other antidepressants in the database titled Drugs Used to treat Depression (https://www.drugs.com/condition/depression.html), for which there were ≥100 individual reviews for each drug, tramadol was rated as being the most effective (effectiveness rating = 9.1/10). Phenelzine (effectiveness rating = 8.7/10) was the only other antidepressant having ≥100 individual reviews coupled with a very high (8.0–10.0) effectiveness rating. Eleven patients reported significant symptoms of withdrawal upon cessation of tramadol, and five patients reported loss or reduction of libido as a side effect. Most (57/72, 79.2%) patients who reported a dose consumed experienced relief from depression at low therapeutic doses (25–150 mg/day). Fourteen patients reported taking this antidepressant for 5–10 years, and four patients reported taking tramadol for 10 or more years. Results demonstrated that most patients’ comments and beliefs are consistent with the biomedical literature. Conclusions: Patients’ reviews coupled with a survey of the biomedical literature indicate that at low therapeutic doses in the absence of interactions with other drugs, adult patients found tramadol to be a generally safe, effective, and fast-acting medication for relief from depression.
Keywords: tramadol, off-label, antidepressant, depression, data mining, opioid
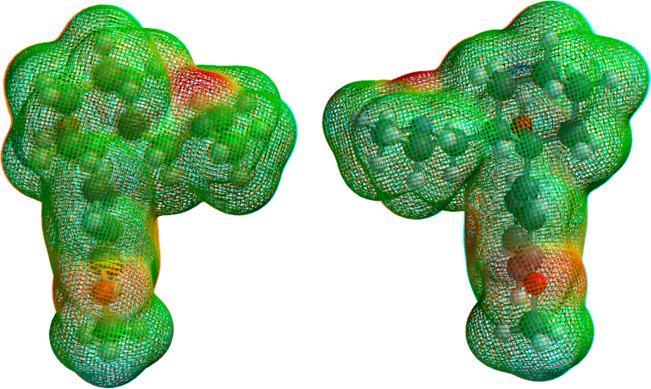
Tramadol, a widely prescribed
analgesic, is a racemic (1:1) mixture of (1R,2R)- and (1S,2S)-2-[(dimethylamino)methyl]-1-(3-methoxyphenyl)cyclohexanol)
(a.k.a. (1R,2R)- and (1S,2S)-tramadol).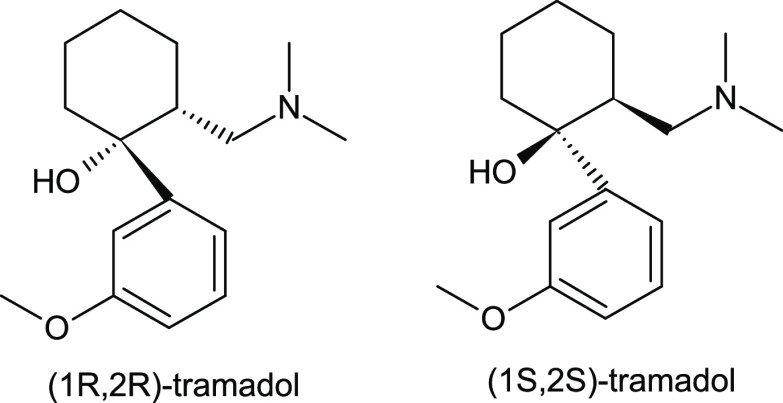 The article of commerce is the hydrochloride
salt of this
racemate. Its effectiveness as an analgesic is due mainly to the ability
of (1R,2R)-tramadol and its more
potent metabolite, the corresponding (1R,2R)-O-desmethyltramadol (known as M1), to
bind to μ-opioid receptors and function as weak, yet effective,
agonists of these receptors in the central nervous system. The parent
racemate also functions as both norepinephrine and serotonin reuptake
inhibitors. Thus, tramadol may be described as a mixed-function centrally
active analgesic. Tramadol addiction has been reported in individuals
who have consumed high doses for prolonged periods. However, addiction
appears to be less problematic than for high-affinity opioids such
as morphine, heroin, oxycontin, and fentanyl.1
The article of commerce is the hydrochloride
salt of this
racemate. Its effectiveness as an analgesic is due mainly to the ability
of (1R,2R)-tramadol and its more
potent metabolite, the corresponding (1R,2R)-O-desmethyltramadol (known as M1), to
bind to μ-opioid receptors and function as weak, yet effective,
agonists of these receptors in the central nervous system. The parent
racemate also functions as both norepinephrine and serotonin reuptake
inhibitors. Thus, tramadol may be described as a mixed-function centrally
active analgesic. Tramadol addiction has been reported in individuals
who have consumed high doses for prolonged periods. However, addiction
appears to be less problematic than for high-affinity opioids such
as morphine, heroin, oxycontin, and fentanyl.1
In addition to its use as an analgesic, there is substantial evidence that tramadol is an effective antidepressant. This evidence is presented and/or summarized in over 50 citations in the peer-reviewed biomedical literature in animal models,2−32 in humans,33−53 in the patent literature,54−57 and in reports provided by patients.58−60 The World Health Organization (WHO) Expert Committee on Drug Dependence published a comprehensive review of the chemistry, biochemistry, and biomedical aspects of tramadol in 2018.1 Much of the background information and review material presented here concerning this medication is from this reference and references therein.
The overall objectives of this analysis are to: (1) document, from the patients’ perspective, the effectiveness of tramadol as an off-label antidepressant; (2) determine if patients’ experiences and beliefs about this medication are consistent with the peer-reviewed biomedical literature; and (3) assess the relative safety of low-dose tramadol.
Methodology
Selection of the Medical Social Media Website Used in This Analysis
The informational website https://www.drugs.com/(58) was selected for this analysis. Embedded within this website are two databases:59,60 one containing a discussion forum specifically addressing tramadol as an off-label medication for depression,59 and the other comparing tramadol to 101 other antidepressants.60 Although the United States Food and Drug Administration (US FDA) recommends61 this website, comments by individual respondents, descriptions of their experiences, and opinions posted in the discussion forum are solely those of the respondents. Similarly, the analyses of these comments and drug comparisons are solely those of the author. Therefore, individual comments by respondents, their descriptions of experiences and opinions, and the author’s analysis claim no FDA endorsement.
Analytical Approach
The discussion forum/database regarding the effectiveness of tramadol as an antidepressant on the drugs.com website is titled User Reviews for Tramadol to treat Depression.59 This discussion forum contained 139 reviews by patients and descriptions of their experiences with this drug as well as their ratings of its effectiveness as an antidepressant. This discussion forum was last accessed on 09/8/2020, immediately before this manuscript was submitted for publication. Three respondents submitted two reviews each. Thus, the total number of patients involved in this analysis was 136. For the three respondents who submitted two reviews each, both effectiveness ratings were included in these analyses.
Data Mining
Data mining typically refers to the process of using sophisticated computer algorithms to abstract new information from very large data sets. Here a simpler data mining analysis was used to abstract information from a relatively small data set whose analysis was manageable using an MS Word table, manual data entry, and visual analysis. Tramadol reviews addressing depression which appear on the drugs.com website59 were accessed, each respondent was assigned a patient number in order of their submission starting with the first patient respondent who accessed this website on 6/17/2012. A list of anonymous patient respondents and all of their respective unedited comments and effectiveness ratings were placed in an MS Word table (Table S-1). Available numeric data and information regarding other descriptors and queries were examined, and appropriate information was manually recorded. Using the “Find” function, several keywords, numbers, and short phrases were used to locate information relevant to this analysis in the comments in Table S-1. Depression, antidepressant, addiction, dependence, pill, tablet, tolerance, and suicide are examples of the keywords used. A complete list of keywords used accompanies Table S-1.
Limitations and Strengths of This Analysis
Tramadol has undergone rigorous investigation and has received FDA approval for use as an analgesic.62 The use of tramadol as an antidepressant has not received such scrutiny. Nevertheless, its ability to function as an antidepressant has been well-documented.2−60
Although no substitute for large-scale, well-designed investigations, patient-reported experiences are important. Thus, evidence presented by patients on medical social media websites such as that reported here58−60 should not be dismissed or overlooked as merely anecdotal. Indeed, comments analyzed here can be regarded as “miniature or abbreviated case reports” from the perspective of the patient. This type of evidence is generally regarded as less reliable than peer-reviewed studies. However, such evidence is considered more robust as the number of reports increase. Even when a large number of similar reports occur, it is still necessary be circumspect when interpreting results. Nevertheless, multiple reports of experiences by patients coupled with corroborating independent biomedical research results lends credence to both. In almost all instances, patients’ comments and experiences analyzed here are discussed coupled with mutually supportive results reported in the peer-reviewed biomedical literature.
The lack of a comprehensive systematic questionnaire or survey is a limitation. Except for requesting information about the length of time patients had taken this medication and the patient’s rating of its effectiveness, no other pertinent information was specifically requested by the discussion forum. Thus, information shared in the comments section was that deemed important by the patient.
A third issue concerns the composition of the patient population. Certainly, the respondents are not a representative sample of the population at large. However, they do represent a population of individuals who have dealt with depression long-term, often over the course of many years. With only two possible exceptions (patients #69 and #116), all appear to have used tramadol as a treatment for their depression and have elected to share their unfiltered, practices, attitudes, and opinions and/or experiences. Rather than a limitation or liability, this is viewed as a major strength of this analysis.
Results
Effectiveness of Tramadol as an Antidepressant
Of 101 antidepressants, 34 had ≥100 individual reviews.60 Of this group, patients rated tramadol as being the most effective, having an average effectiveness rating of 9.1 out of 10 (Table 1). Phenelzine (effectiveness rating = 8.7) was the only other antidepressant having ≥100 individual reviews coupled with a very effective (8.0–10.0) rating.60 When the criteria was lowered to ≥40 individual reviews (n = 52), nine other antidepressants had effectiveness ratings in the 8.0–10.0 range. These antidepressants included alprazolam (8.8). methylphenidate (8.8), niacin (8.8), Parnate (8.8), Nardil (8.7), Xanax (8.7), modafinil (8.6), tranylcypromine (8.6), and amitriptyline (8.2). Alprazolam and Xanax, phenelzine and Nardil, and tranylcypromine and Parnate are generic and brand name versions of the same medication, respectively. In each case, the generic and the brand name versions had very similar effectiveness ratings, within 0.2 of each other.60 Interestingly, a few pairs of generic and brand name versions had somewhat greater differences for medications having antidepressant effectiveness ratings less than 8–10. The greatest difference was for the two brand names Effexor and Effexor XL and their generic venlafaxine which had effectiveness ratings of 5.5, 6.7, and 6.1, respectively.
Table 1. Effectiveness Rating of Tramadol to Treat Depression: Comparison with Other Antidepressants Having 40 or More Reviewsa,b.
| antidepressant | number of reviews | effectiveness rating | |
|---|---|---|---|
| 1 | tramadol (off-label) | 139 | 9.1 |
| 2 | alprazolam | 93 | 8.8 |
| 3 | methylphenidate | 53 | 8.8 |
| 4 | niacin (off-label) | 47 | 8.8 |
| 5 | Parnate | 76 | 8.8 |
| 6 | phenelzine | 102 | 8.7 |
| 6 | Nardil | 83 | 8.7 |
| 7 | Xanax | 74 | 8.7 |
| 8 | Modafinil (off-label) | 54 | 8.6 |
| 9 | tranylcypromine | 93 | 8.6 |
| 10 | amitriptyline | 99 | 8.2 |
| 11 | l-methylfolate | 122 | 7.8 |
| 12 | Wellbutrin | 257 | 7.4 |
| 13 | Deplin | 84 | 7.4 |
| 14 | Lamotrigine (off-label) | 124 | 7.3 |
| 15 | citalopram | 654 | 7.3 |
| 16 | Remeron | 144 | 7.3 |
| 17 | Seroquel XL | 47 | 7.3 |
| 18 | Celexa | 347 | 7.2 |
| 19 | Lexapro | 555 | 7.2 |
| 20 | bupropion | 1118 | 7.1 |
| 21 | escitalopram | 783 | 7.1 |
| 22 | fluoxetine | 592 | 7.1 |
| 23 | Prozac | 381 | 7.1 |
| 24 | Pristiq | 720 | 7.0 |
| 25 | sertraline | 1071 | 7.0 |
| 26 | trazodone | 107 | 6.9 |
| 27 | desvenlafaxine | 768 | 6.9 |
| 28 | brexpiprazole | 82 | 6.8 |
| 29 | Zoloft | 545 | 6.9 |
| 30 | Rexulti | 73 | 6.8 |
| 31 | mirtazapine | 500 | 6.8 |
| 32 | Wellbutrin SR | 97 | 6.8 |
| 33 | Effexor XR | 317 | 6.7 |
| 34 | quetiapine | 161 | 6.6 |
| 35 | paroxetine | 255 | 6.6 |
| 36 | Abilify | 269 | 6.5 |
| 37 | aripiprazole | 286 | 6.5 |
| 38 | nortriptyline | 52 | 6.5 |
| 39 | Paxil | 175 | 6.4 |
| 40 | Cymbalta | 548 | 6.3 |
| 41 | duloxetine | 633 | 6.3 |
| 42 | venlafaxine | 887 | 6.1 |
| 43 | Viibryd | 554 | 6.1 |
| 44 | vilazodone | 572 | 6.1 |
| 45 | Trintellix | 530 | 6.0 |
| 46 | vortioxetine | 769 | 5.9 |
| 47 | Zyprexa | 58 | 5.8 |
| 48 | Effexor | 322 | 5.5 |
| 49 | olanzapine | 120 | 5.5 |
| 50 | Risperidone (off label) | 43 | 5.4 |
| 51 | Fetzima | 81 | 4.5 |
| 52 | levomilnacipran | 90 | 4.5 |
10 = most effective, 1 = least effective. Data abstracted from ref (60), which contained information for a total of 101 antidepressants, not the 188 that is incorrectly listed.
The following are brand names and generic name pairs for many of the drugs appearing in this table: Xanax and alprazolam, Parnate and tranylcypromine, Nardil and phenelzine, Deplin and l-methylfolate, Celexa and citalopram, Remeron and mirtazapine, Seroquel XL and quetiapine, Lexapro and escitalopram, Wellbutrin SR and bupropion, Prozac and fluoxetine, Pristiq and desvenlafaxine, Rexulti and brexpiprazole, Zoloft and sertraline, Effexor (and Effexor XR) and venlafaxine, Paxil and paroxetine, Abilify and aripiprazole, Cymbalta and duloxetine, Viibryd and vilazodone, Trintellix and vortioxetine, Zyprexa and olanzapine, Fetzima and levomilnacipran.
It is also interesting to mention that two of the four other off-label antidepressants in Table 1 have effectiveness ratings in the “very effective” range. They include niacin (8.8) and Modafinil (8.6). Two other off-label antidepressants, Lamotrigine (7.3) and Risperidone (5.4), had ratings in the “Effective” and “Less Effective” range, respectively.”
Data for antidepressants with <40 individual reviews was not considered to be sufficiently robust for comparison.
For tramadol, 117 of 130 individual reviewers (90.0%) rated this medication as very effective (rating = 8–10) (Table 2). Six reviewers (4.6%) rated tramadol as effective (rating = 6–7) and seven reviewers (5.4%) gave it a low (less effective) effectiveness rating (rating = 1–5). Six patients provided comments, but did not provide an effectiveness rating. Thus tramadol was rated as effective or very effective by 94.6% of those patients who provided ratings.
Table 2. Patient Ratings for the Effectiveness of Tramadol to Relieve Depression.
| patient ratinga | percent | number of patients providing this rating |
|---|---|---|
| 10 | 66.2 | 86 |
| 9 | 14.6 | 19 |
| 8 | 9.2 | 12 |
| subtotal 8–10 (very effective) | 90.0 | 117 |
| 7 | 3.85 | 5 |
| 6 | 0.77 | 1 |
| subtotal 6–7 (effective) | 4.6 | 6 |
| 5 | 0.77 | 1 |
| 4 | 0.77 | 1 |
| 3 | 1.54 | 2 |
| 2 | 0 | 0 |
| 1 | 2.31 | 3 |
| subtotal 1–5 (less effective) | 5.4 | 7 |
| total | 100 | 130 |
The average effectiveness rating for tramadol was 9.1 (most effective = 10, least effective = 1). Data was abstracted from ref (59). The data presented here was recalculated and the table was slightly modified. Effectiveness ratings of very effective, effective and less effective are defined as follows. Patients’ ratings of 8–10 were designated as very effective. In this group patients indicated that tramadol relieved depression and typically provided very positive comments about this medication. Patients’ ratings of 6–7 were designated as effective. In this group patients’ comments indicated that tramadol relieved depression but gave it a rating lower than 8–10 because of adverse, but manageable, side effects. Patient ratings of 1–5 were designated as less effective based solely on the low numerical rating.
Table 3 presents comments from: (1) ten representative patients who gave very effective rating values (rating 8−10); (2) all patients who gave effective rating values (rating 6−7); and (3) all patients who gave low effectiveness rating values (rating 1−5).
Table 3. Patient Comments and Ratings Regarding the Effectiveness of Tramadol as an Antidepressanta.
| patient number | effectiveness rating | |
|---|---|---|
| Comments for Very Effective Ratings (8–10) | ||
| #2 | 10 | “I experienced only adverse reactions to SSRIs and TCAs thanks in part to being bipolar, but Tramadol has been a God send for my depression. I was sick and tired, literally, of trying different medicines only to have my mood get thrown around crazily. Tramadol worked when nothing else could touch the depression. I take it twice daily. Could not live without it. I am so thankful that my psychiatrist is open to new ideas and tried this, I only will encourage others to try this also. Because of the Tramadol I am now recovered from any form of self injury - I am free for over 3 years. It works. Simple.” |
| #4 | 9.0 | “I to went from one antidepressant to another. SSRIs (multiple), TCAs, SNRIs. Nothing worked and like others my moods were up and down the whole time. Twice a day Tramadol has kept me symptom free for 5 years now. Amazing.” |
| #16 | 10 | “I have been depression for over 7 years but in that short period of time I was immediately suicidal. By “fate” I found my salvation. One day I was saying my goodbye to all as I could not live any longer with such sadness and complete doom. I was sitting with my mom and during all the crying I told her I had a severe headache. She only had tramadol. I took two. It saved my life that day and is still. I had tried before and even after all kinds of other medicines and none worked.” |
| #33 | 10 | “I was given Tramadol about 12 years ago for endometriosis and severe menstrual cramping. It has made me feel so much better overall...it works wonders for my mood, anxiety, and depression. I am a better person because of this drug. I am motivated, and feel great...all the time. This has changed my life for the better.” |
| #42 | 10 | “I have had major depression my whole life and absolutely none of the anti depressants worked for me, I had intermitant periods in my life were I had suicidal thoughts but I always managed to tough it out I maintained decent employment but chronically underachieved because I was always fighting internal demons and social anxiety, then my children left home, I got a divorce and lost my home, suicidal thoughts were non stop no matter how hard I tried to talk myself into coping and turning my mood around, the suicidal thoughts persisted for 2 yrs, then I was prescribed tramadol for Fibro 50 mg twice a day, I have never felt so normal in my whole life took it 3 yrs no dose increase off it for six months too hard to get the RX now suicidal 24/7” |
| #68 | 10 | “Antidepressants have had no effect on my depression in the past. I was unable to find the motivation to support my family or even go to work which caused me to lose my job. I started tramadol for a back injury as it is a nonhabit forming pain reliever. It changed my life. immediately, it wiped out the depression. 100% gone. It is not much of a pain reliever, it is not very strong and I still am in pain. I can deal with it though and the lack of depression is worth it. The only downside is that when it wears off the depression comes right back, fast. So I have to take it throughout the day. I am back to work and enjoying life, i just take 3 or 4 pills per day. I do not know why this drug is not marketed as an antidepressant, it should be.” |
| #8 | 9 | “I have been on Tramadol (50 mg 3× per day) for about 6 years now. For the first few years is was a miracle cure. I have struggled with depression/anxiety/impulse and obsessive disorders my entire life. This made me finally feel free and human for the first time ever. The only downfall was after a few years, the effects wore off, and slowly my depression/anxiety began to creep back in. I took a break from it for a few months (warning: withdrawing from Tramadol is reallllly uncomfortable). I went back on it after my Dr assured me it was a good med (even long-term) for fibromyalgia/depression, etc. I’m up to about 4/day now. It still helps, but not nearly as much in the beginning.” |
| #112 | 9 | “I have taken tramadol off and on for 3 years for hip bursitis and I also have suffered from depression for the last 30 years. When I take it I feel any signs of depression lift...I feel motivation to engage in life, my mind feels clear, and I have more energy. I recently had an honest conversation with my psychiatrist about using low dose tramadol for depression. I’ve tried a dozen different antidepressants with ton of side effects and hardly any good long lasting results. I do not feel any side effects from the tramadol and 50 mg can last me all day. I do notice when it wears off but I do not mind as I’ve had a good 8 h feeling normal, not high. I am hopeful now. I’ve been able to just stop it without side effects when needed to so far...its such a low dose but does wonders.” |
| #102 | 8 | “I got prescribed Tramadol for Back pain. I have been taking one 50 mg pill a day and have seen such an enhancement in my mood. I’ve never wanted to take “antidepressants or anxiety” meds, because I did not want it to change my personality or make me a zombie. However, I really enjoy being on Tramadol, it makes my job in retail not such a drag. I do not have my normal mood swings, and by then end of the night I sleep great! I am afraid to tell my doctor as well that it helped me in that aspect because I do not want her to think I’m using it as a “high.” But I genuinely love this medication.” |
| Comments for Effective Ratings (6–7) | ||
| #74 | 7 | “Tramadol is NOT an opiate. It does act on the same pain receptors as opiates, but it does not have the same addictive quality as opiates and does not have the same risk of abuse as opiates. You can become dependent on Tramadol, just as you can be dependent on SSRI’s. You cannot cold turkey quit an SSRI without some really gnarly withdrawal symptoms and the same goes for Tramadol and opiates and tons of other drugs. I’ve been taking Tramadol for 4 years for general pain in my body due to end stage renal disease and osteodystrophy. Since I’ve been taking Tramadol I have not needed antidepressants and I find that I function at a higher level with Tramadol than with any SSRI I have ever taken. There are no negative side effects for me.” |
| #36 | 7 | “For sure tramadol is one of the best drugs for Depression and Anxiety. I have tried a lot of differents antidepressives like fluoxetine, sertraline, paroxetine, citalopram, escitalopram, venlafaxine, etc., and they all did not work very well for my depression and anxiety. I suffered a lot of side effects with these drugs. The only one that really works for depression and anxiety, for me, is Tramadol··· but··· but··· it destroyed my sexual life··· Who is using this drug for depression will feel much better, for sure, but, please, be aware of your sex life! For sure, when I take Tramadol my libido goes to ZERO, and I can not keep an erection for some time··· and, if a keep, it is impossible to ejaculate··· That is why a give a 7···” |
| #80 | 7 | “The comments resonate with me regards Tramadol. I was diagnosed it for back pain which it relieved and gave me a surge of energy and wellbeing which later disappeared with use, but it is still useful for relieving my dire morning depression, if taken 2 h before rising I can face getting out of bed.” |
| #35 | 7 | “Very affective for anxiety, but made me so tired I had to switch.” |
| #25 | 7 | “Tramadol is about the most effective drug in the world for depression - for immediate, short-term relief ONLY though. During the initial dosing period, 100 mg twice a day utterly obliterates any negative thinking or depression symptoms. It delivers results immediately, vs the necessary patience of waiting a few days or weeks with traditional SSRI drugs. However, tolerance DOES build to tramadaol at a pace far more rapidly then with traditional antidepressants. I had 2 months of solid relief from 100 mg 2x daily, but by the third month this does barely made a difference and my mood continued to sink. Instead of upping my dose, I went back on Zoloft which delivers less immediate, but more consistent long-term results for me.” |
| #116 | 6 | “There good for pain.” |
| Comments for Less (i.e., Low) Effective Ratings (1–5) | ||
| #108 | 5 | “good for very intermittent use–be careful extremely addicting” |
| #111 | 4 | “I placed a post earlier on 2019–07–10 under the name Jerry saying – I was a 65 year old male that takes Tramadol intermittently to reduce depression. the problem is that when I do take days off – I am extremely depressed 3 times as much. So you have to be very careful of this medication.” |
| #69 | 3 | “I see a recurring theme in a lot of these entries... (person x) was prescribed Tramadol for pain, and it did wonders for depression and mood. However, when discontinuing use, one’s symptoms quickly return, often worse than before... Tramodol is an OPIATE. Think Opium, Heroin, Oxycodone, Hydrocodone, Codeine, etc. What you are describing is the pattern of Opiate usage and it is dangers. This is why it is a poor choice for depression treatment - it is like giving a Mercedes to a guy who’s lost his job and his house is being foreclosed on...feels good for a couple days, but...” |
| #84 | 1 | “This medication was initially prescribed for back pain. As an unexpected side effect it dealt with my MDD perfectly. Unfortunately I am medication sensitive and started to have negative side effects so had to slowly get off this medication. For some reason the withdrawal was horrible. Everybody responds differently and even though this medication worked with the pain and depression it’s side effects made it impossible for me to remain on it and the withdrawal was the worst part ‘for me.’” |
| #94 | 1 | “Doesnt do a thing for me,” |
| #134 | 3 | “The tramadol helped my depression for a while. I took it on at off (50 mg per day) with various antidepressants. I would feel effects about 2 h in, but they would fade quickly - and they never fully took away symptoms. I then started taking 2 (50 mg) per day - one before getting up to help morning mood and then one later in the day. This was not effective at all. I’ve now been on the 2× per day dose for a month and am tapering down to 1 per day for a week, then will go to 1/2 per day for a week and stop. I’m going to try pregabalin as my depression has some anxiety and that might help?” |
| #138 | 1 | “Took first dose 2 years ago. Was 1 year sober (alcohol) and took unprescribed for pain. Took 2 weeks to go 300 mg/day. Six months later at 800 mg/day; had 2 seizures. After I maintained at 600 mg/day for 8 months. Was happy, energetic, and productive. Wanted out, not willing to give up benefits. Then pandemic came/shut down my source. Self-tapered, now at 100 mg/day, cannot taper further without physical withdrawal. Altered mental state to point of suicidal ideations during taper. Works as antidepressant, very addicting. Wish had never taken. I read these forums when I first started experimenting and thought I could manage it. I was wrong. I guess it treats everyone a little differently, but if this post could persuade one person to get out of it before it is too late then I have my purpose for posting. Please be very careful with this drug, I am still in so much psychological pain unlike anything I’ve experienced since getting sober.” |
Patients (136) submitted 139 user reviews available from ref (59). Ten representative reviews from patients submitting a very effective rating (8–10), and all reviews from patients submitting a rating of effective (6–7) and less effective (1–5) are presented here. All patient reviews are available in Table S-1 and ref (59). Patient numbers were assigned in order of their submission, starting with the first respondent who accessed this webpage on 6/17/2012. Minor corrections in grammar, spelling, and punctuation were made to patients' comments during the publication process.
Patients who gave tramadol a very effective rating were effusive in their comments. Among the phrases describing relief from depression are “it works wonders for my mood, anxiety, and depression”, “It changed my life”, “immediately, it wiped out the depression”, “100% gone”, “symptom free for 5 years now”, “Tramadol has been a God send for my depression”, and “Amazing”. Fourteen patients reported taking this medication for 5–10 years, and four patients reported taking tramadol for 10 or more years (Table 4).
Table 4. Length of Time Patients Used Tramadol to Treat Depressiona.
| time | number of patients | % |
|---|---|---|
| 10 or more years | 4 | 4.5 (4.494) |
| 5–10 years | 14 | 15.7 (15.730) |
| 2–5 years | 23 | 25.8 (25.843) |
| 1–2 years | 14 | 15.7 (15.730) |
| 0.5–1 year | 6 | 6.7 (6.742) |
| 1–6 months | 22 | 24.7 (24.719) |
| less than 1 month | 6 | 6.7 (6.742) |
| total responding | 89 | 99.8 (100) |
Data was abstracted from ref (59).
As noted in Table 5, entries f–h, 6 patients asserted that tramadol relieved symptoms associated with bipolar depression. Consistent with published reports,44,52 4 patients asserted that tramadol relieved depression associated with post-traumatic stress disorder, and 5 patients reported relief from treatment resistant depression.
Table 5. Analysis of Tramadol Consumption for Depression: Descriptors and Queriesa.
| descriptors and queries | comments | |
|---|---|---|
| (a) | patient’s age and gender | Limited patient response to these descriptors allowed only the general observation that adult males and females were included in the group of patients providing reviews. |
| (b) | How long has patient had to deal with depression? | Nine patients reported dealing with depression for a decade or more. Two asserted that they have dealt with depression for over 40 years. |
| (c) | How rapidly does tramadol work? | Nineteen patients noted that tramadol was a fast-acting antidepressant. |
| (d) | What was the patient’s assessment regarding efficacy of tramadol relative to other antidepressants; was tramadol superior? | Sixty-three patients explicitly or implicitly noted that they had tried other antidepressants and found them lacking, in comparison to tramadol. Eight patients reported taking tramadol with other antidepressants. |
| (e) | Were physicians, psychiatrists, and other healthcare providers willing to prescribe tramadol? | Physician awareness of tramadol’s effectiveness as an antidepressant and their willingness to prescribe tramadol as an antidepressant varied considerably. |
| (f) | Was tramadol effective for bipolar depression? | Six patients asserted that their depression was associated with bipolar disorder and that tramadol relieved their symptoms. |
| (g) | Was tramadol effective for treatment-resistant depression? | Five patients asserted that their depression was treatment-resistant and that tramadol relieved their symptoms. |
| (h) | Was tramadol effective for post-traumatic stress disorder (PTSD)? | Four patients reported that they suffered from depression associated with post-traumatic stress disorder (PTSD), and one patient thought he/she might be suffering from this affliction. All five patients reported that tramadol relieved their symptoms. |
| (i) | Was tramadol’s effectiveness for depression discovered when this medication was used for pain? | Half (68/136) of the patients reported the serendipitous discovery of tramadol’s effectiveness as an antidepressant after it was initially used for pain. |
| (j) | Did depression return following cessation? | Eighteen patients reported that they experienced a return of depression when they stopped taking tramadol. |
| (k) | Was withdrawal problematic? | Eleven patients reported that they experienced withdrawal upon cessation of tramadol. |
| (l) | Was addiction a concern? | Twenty patients provided comment or opinion regarding the possible addictive potential and withdrawal effects of tramadol. |
| (m) | Did addiction or dependence actually occur? | Four patients explicitly or implicitly acknowledged being addicted to tramadol. Three patients asserted they were dependent but not addicted. |
| (n) | Was a buildup of tolerance observed? | Three patients asserted or implied that tolerance was a problem for them. |
| (o) | Was fatigue a side effect? | Two patients reported that tramadol made them tired. |
| Did tramadol affect sleep? | Only one patient reported that tramadol interfered with sleep. In contrast, 5 patients reported that they slept well while taking tramadol, and 20 patients reported that tramadol made them more energetic. | |
| (p) | Was decreased libido a side effect? | Five patients reported loss or reduction of libido as a significant side effect. |
| (q) | Was tramadol an effective analgesic? | Ten patients noted that tramadol was, in general, only a marginally effective or noneffective analgesic but continued taking it because it relieved their depression. |
| (r) | Were adverse side effects (seizures or serotonin syndrome) encountered? | In the patient reviews, only one reported having seizures upon prolonged use at supratherapeutic doses. No patient reported experiencing serotonin syndrome. |
| (s) | Did patients find it difficult to obtain a prescription? | Twenty-nine patients commented about the unwillingness of healthcare providers to prescribe, or continue prescribing, this medication for depression. |
| (t) | Did tramadol relieve suicidal ideation? | No patient reported experiencing suicidal ideation or thoughts of self-injury as a result of taking tramadol. Thirteen patients reported that depression associated with suicidal ideation or thoughts of self-injury were relieved as a result of being treated with this medication. Six patients experienced or feared a return of suicidal ideation upon cessation of tramadol. |
| (u) | What other side effects were encountered? | There are a host of minor side effects that have been associated with tramadol administration. See text for further information, |
Six patients gave effective ratings of 6 or 7. Four patients acknowledged that tramadol relieved their depression and provided very positive comments. In general, these patients gave ratings lower than very effective because of adverse, but apparently manageable, side effects (e.g., “really gnarly withdrawal symptoms”, loss of libido, and buildup of tolerance) that were experienced. Two patients in this group did not provide comment regarding depression.
Seven patients provided ratings and comments in the less effective range (1–5). Five of these patients still acknowledged that tramadol relieved depression. One patient found it to be ineffective. One patient found that tramadol’s antidepressant effects wore off quickly, and elected to taper off and try another antidepressant. Most patients in this group gave tramadol low effectiveness ratings because of unacceptable adverse side effects.
Of the cohort of 136 patients, 63 patients (46.3%) reported that they had tried other antidepressants and found them lacking, in comparison to tramadol (Table 5, entry d). Other antidepressants mentioned by patients are presented in Table S-2, entry d. Half (68/136) of the patients reported the serendipitous discovery of tramadol’s effectiveness as an antidepressant during its use as an analgesic (Table 5, entry i). Ten patients noted that tramadol was, in general, only a marginally effective or noneffective analgesic but continued taking it because it relieved their depression (Table 5, entry q).
Discussion
Addiction, Dependence, Abuse, or Successful Treatment?
Tramadol was introduced to the market as a nonscheduled drug in 1995 with the caveat that a surveillance program be put in place to monitor for the possibility of high levels of abuse.1 On the basis of available data, which at that time did not detect substantial abuse, tramadol continued to be marketed for the rest of the 1990s and early 2000s as an unscheduled drug. However, monitoring between 2003 and 2009 revealed an increase in the incidence of diversion, abuse and overdose of this medication, leading Arkansas, Kentucky, Tennessee, and Wyoming to change the drug from unscheduled to Schedule IV.1 The federal government rescheduled tramadol as a Schedule IV drug in 2014.1
Patients’ comments (Table 5, entries l and m) regarding addiction to and dependence on tramadol are consistent with the Critical Review Report: Tramadol(1) by the World Health Organization’s Expert Committee on Drug Dependence in 2018, who reported the following: “The development of physical dependence from tramadol therefore appears dose-related, and administration of 800 mg/day tramadol leads to similar levels of opioid physical dependence as 60 mg/day morphine.”(1) The Expert Committee further stated that differences exist between high and low dose use of tramadol and that unlike those who used high dose tramadol the risks of “...physical dependence and withdrawal symptoms were lower than prototypic opioid effects...”(1) for those who used low-dose tramadol over an extended period of time. Patients’ reviews analyzed here (Table 6) demonstrate a clear preference (79.2%) for using low doses (25–150 mg/day) of tramadol to treat depression. This appears to be due to good medical practice, physicians prescribing the lowest effective dose, and some degree of self-selection by patients in favor of low-dose regimens.
Table 6. Dose of Tramadol Consumed by the 72 Patients Who Reported Dosea.
| dose (mg/day) | number | patient numberb |
|---|---|---|
| >400 | 2 | #129, #138 |
| 400 | 3 | #45, #106, #137 |
| 300 | 3 | #7, #135, #139 |
| 200 | 7 | #8, #15, #18, #20, #25, #31, #70 |
| 150 | 8 | #6, #22, #28, #32, #50, #86, #91, #126 |
| 125 | 1 | #98 |
| 100 | 25 | #2, #4, #14, #16, #19, #23, #26, #27, #38, #42, #43, #44, #60, #63, #76, #79, #89, #95, #117, #119, #122, #127, #133, #134, #136 |
| 50 | 21 | #10, #17, #30, #34, #41, #66, #71, #73, #78, #85, #88, #93, #99, #100, #102, #104, #110, #112, #121, #123, #130 |
| 25 | 2 | #77, #96 |
| total | 72 |
Data was abstracted from ref (59).
In some reviews, patients reported they took varying doses. Patients #96 took 25 or 50 mg/day. Patients #27, #95, #117, and #127 took 50 or 100 mg/day. Patient #8 took 150 or 200 mg/day. Patient #91 took 100 or 150 mg/day. Patient #20 took 100 or 200 mg/day. Patient #129 took up to 800 mg/day but “tapered down”. Patient #138 took from 100 to 800 mg/day. For the purposes of this table, the larger values were used except for Patients #50, #77, and #96. For Patient #50, the lower value was used because he/she indicated that was the typical dose. For Patients #77 and #96, the lower value was used because this value (25 mg/day) was representative of what appeared to be the lowest dose at which patients found tramadol effective in ameliorating symptoms of depression. Patient #96 took this medication only 4 days/week. Patient #89 took 100 mg/day for only 3 or 4 days/week. When patients reported dose in the number of tablets consumed, each tablet was considered to be equal to 50 mg.
Dunn et al.63 recently reviewed and compared the abuse potential of tramadol with other opioid receptor agonists. It was concluded “...that tramadol confers an equal or lower risk of abuse than the opioids to which it was compared, that its greatest risk for abuse is when it is being administered via oral formulations to non-dependent individuals, and that the likelihood it will be abused appears to decrease as the dose increases or when it is administered parenterally.” Dunn et al.63 further concluded that “The present literature therefore suggests that the human abuse potential of tramadol is different from and lower than other opioid agonists.” Dunn et al.’s63 analysis noted that in two of three studies oral administration of tramadol produced more “...bad effects as the dose increases...”, and this may be the reason why “...the likelihood it will be abused appears to decrease as the dose increases...”.63 Therefore, in the present analysis, it is reasonable to suggest that the majority of patients (Table 6) consumed a low dose of tramadol not only because it was effective at low doses but also because higher therapeutic (and supratherapeutic) doses produced more adverse (i.e., “bad”) effects.
The recreational abuse and/or addiction to supratherapeutic doses of tramadol is an important public health issue and requires appropriate medical and regulatory intervention, especially in countries where its use is unregulated.1 Discussion of the addictive and/or dependent nature of tramadol is, however, confounded by the reality that in an appropriately supervised clinical setting long-term relief from depression (i.e., mood enhancement) is the clinical goal. In such a setting, it does not seem appropriate to view long-term reliance/dependence on therapeutic low doses of an effective medication in the same pejorative context as addictive recreational abuse/use of supratherapeutic doses. Discussion of addiction and dependence is further confounded because cessation of tramadol in clinically depressed patients may result in a return of their depression and other symptoms (i.e., antidepressant discontinuation syndrome)64,65 that make it difficult to distinguish from withdrawal caused by cessation of a drug to which the patient may be truly addicted.
Physician Awareness and Willingness to Prescribe Tramadol for Depression and Patients’ Concerns Regarding Access to Tramadol
As noted in Table 5, entries e and s, patient reviews demonstrated that physician awareness of and willingness to prescribe tramadol as an antidepressant varied considerably. Some physicians accepted the patient’s observations that tramadol relieved their depression and continued prescribing this medication. Others were less willing to do so. Tramadol’s documented potential for abuse, the opioid epidemic, it is reclassification as a Schedule IV drug,1 and a lack of awareness of its effective off-label use as an antidepressant are likely reasons many healthcare providers are reluctant to prescribe this medication for depression. Twenty-nine patients commented about the unwillingness of healthcare providers to prescribe, or to continue prescribing, tramadol for depression. An unfortunate consequence is that denial of this medication may result in the perception of “doctor-shopping” and be interpreted as “drug-seeking behavior”, when in reality the patient is seeking an effective medication for depression. For 18 patients, this did indeed prove problematic when patients encountered the unwillingness of healthcare providers to prescribe or renew prescriptions for tramadol to treat depression. This was/is particularly worrisome for six patients who experienced or feared a return of suicidal ideation upon cessation of this medication (Table 5, entry t).
A related issue concerns patient–physician communication. A few patients reported problems or hesitancy explaining to their physicians that tramadol prescribed for pain actually relieved their depression because it was feared they would stop prescribing this medication. Cleary misunderstanding and lack of communication is problematic for these individuals. Patients should be able to communicate their observations to physicians without fear that an effective medication will be withdrawn.
Other Issues Concerning Possible Adverse Side-Effects
Misuse, Overdose, and Suicide
Tramadol abuse has been well-documented and is clearly a problem and a major reason why it was reclassified as a Schedule IV drug.1 Equally well-documented is the involvement of tramadol overdose in intentional and unintentional suicides.1 However, there is very little evidence suggesting that tramadol per se causes suicidal ideation. Only one short report was found suggesting tramadol was the cause of depression associated with suicidal ideation in one patient.66 In the analysis presented here 13 patients reported tramadol relieved suicidal ideation that was associated with their depression (Table 5, entry t) which is consistent with five published investigations.33,36,37,44,47 It should be noted, however, that current guidelines recommend against prescribing this medication for patients with existing suicidal ideation.67 This apparent inconsistency requires further scrutiny.
Seizures and the Serotonin Syndrome
Seizures and serotonin syndrome are the most serious and potentially lethal complications associated with the use of tramadol.1,68−80 Thus, it is important to view the risk of these complications in proper perspective. Seizures and/or serotonin syndrome have been reported to occur even when therapeutic doses of tramadol have been ingested.68,73 Idiosyncratic observations like these are important to consider. Nevertheless, the overwhelming incidence of tramadol associated seizures and serotonin syndrome are from overdoses due to suicide attempts, recreational use/abuse of supratherapeutic doses and interaction with drugs (e.g., antidepressants and/or monoamine oxidase inhibitors) that potentiate the occurrence of these complications.
The incidence of seizures associated with tramadol has been estimated to be 0.15 and 0.86%,79,80 and reputable drug advisory sites regard the occurrence of seizures, in therapeutic doses, as “less common”81 or “rare”,82 with one83 estimating that the risk was less than 1%. Furthermore, the Johns Hopkins University Peripheral Nerve Center84 estimates the risk of seizures due to tramadol to be less than 1 in 100 000. Finally, the World Health Organization Tramadol Update Review Report in 2014 stated that “Rarely, seizures occur at therapeutic doses of tramadol.”(85) Patient reviews are consistent with this. Only one patient (#138)) reported having seizures upon prolonged use of supratherapeutic doses. The incidence of serotonin syndrome is not known. However, it appears to be even less frequent than that of seizures.69,70 No patients in this analysis reported having to deal with serotonin syndrome.
Most reviews by patients indicated that low-dose tramadol alone was sufficient to successfully treat depression (Table 6). However, eight patients used tramadol in combination with another antidepressant (Table 5, entry d). Thus, the question remains, “Is it advisible to prescribe tramadol in combination with another antidepressant?” Park et al.86 concluded “Tramadol is only contraindicated in combination with MAOIs but not other antidepressants in common use today... Tramadol can be safely combined with antidepressants; however, monitoring and counseling patients are prudent when starting a new serotonergic agent or when doses are increased.”(86)
Other Potential Safety Concerns
Continued Use
Two research groups recently reported that some patients who were tramadol-naïve and/or had not used tramadol before surgery continued consumption of this medication (dose unknown) for several months following its use to treat pain after surgery.87,88 No information was presented by the authors, in either study, concerning why patients continued to take this medication. Thus, in lieu of other information, it is reasonable to suggest that patients did so under the continued supervision of a physician who appropriately prescribed tramadol for chronic pain and/or depression. In the investigation by Thiels et al.,87 it is interesting to note that in the group (n = 13 519) receiving tramadol only 194 (1.44%) and 78 (0.58%) were considered persistent or chronic users, respectively. These small numbers and percentages of persistent or chronic users are of interest to the current analysis when one considers that 460 (3.4%) patients in the study by Thiels et al.87 were experiencing depression as a comorbidity prior to surgery. Thus, it is reasonable to suggest that like many (68/136, 50.0%) of the patients in the analysis presented here some of the patients in the study by Thiels et al.87 continued to take tramadol because they too made the serendipitous discovery of this medication’s effectiveness as an antidepressant during its use as an analgesic.
All-Cause Mortality
The possible association of tramadol with all-cause mortality has also been investigated.89,90 Assessing the association of a drug with all-cause mortality is often a difficult and controversial endeavor. For example, Zeng et al.89 reported that in a population limited to patients with osteoarthritis over 50 years of age, all-cause mortality association was greater for tramadol when compared to naproxen, diclofenac, celecoxib, and etoricoxib but not with codeine. However, Felson91 and Manchikanti et al.92 as well as Zeng et al.89 in their original report and in a response by three of the authors93 noted that “...these findings may be susceptible to confounding by indication, and further research is needed to determine if the association is causal.”93 Manchikanti et al.92 further asserted that “...this study was based on a complex statistical model, had many inconclusive findings and was statistically underpowered making it far from precise.” A similar conclusion was reached by Kloppenburg and Berenbaum.94
In another recent investigation, Musich et al.,95 reported that a small increase in all-cause mortality and other adverse effects may be associated with tramadol consumption compared to nonusers. When compared to other opioids, tramadol users (older adults (≥65)) had fewer adverse event risks. However, tramadol users had higher risks than patients who did not consume opioids. Interestingly, Musich et al.95 also reported that a small increase in all-cause mortality was statistically significant for new users but not for patients taking tramadol long-term. This is of interest to the current analysis as 55 of 89 (61.8%) patients who reported the length of time they used tramadol to treat depression report having used this medication for a year or more, four patients for over a decade.
Other Side Effects
Interference with sleep or fatigue is one of the side effects thought to be caused by tramadol.81 In the present analysis, two patients reported that tramadol made them tired. Only one patient reported that this medication interfered with sleep. In contrast, four patients reported that they slept well while taking tramadol, and 19 patients reported that tramadol made them more energetic. There are a host of minor side effects that have been associated with tramadol administration.81 The following side effects were reported by only one patient each: constipation, headache, nausea if not taken with food, short-term memory loss upon cessation, and hot flashes at night. Three patients reported that tramadol helped them to lose weight. Two patients reported that tramadol helped him/her quit drinking alcohol, and one patient reported that this medication helped him/her quit both drinking alcohol and smoking.
The analysis provided here shows that, in the patient population submitting reviews and dose consumed, tramadol at low doses is an effective medication for most patients. This analysis also suggests that with regard to the most important and serious potential adverse side effects tramadol at these low doses is a generally safe medication. Nevertheless, for some patients, there may be adverse risks, and idiosyncratic responses have been reported66,73,86,96,97 for this medication. Thus, further clarification is needed to determine the level and incidence of such risks, especially the possible differences in risk and adverse effects (including possible association with all-cause mortality) within the therapeutic range between low dose (25–150 mg/day) and high dose (151–400 mg/day) tramadol.
Summary, Conclusions, and Observations
In 139 reviews written by 136 patients, tramadol was reported to be an effective or very effective antidepressant for 94.6% (123/130) of the patients who submitted ratings to drugs.com.59 Significantly, most (57/72, 79.2%) patients who reported dose consumed experienced relief from depression at low therapeutic doses (25–150 mg/day). When compared to thirty-four other antidepressants in the database titled Drugs Used to Treat Depression,60 for which there were ≥100 individual reviews for each drug, tramadol was rated by patients as being the most effective (effectiveness rating = 9.1/10) and was one of only two antidepressants to have a very effective rating (8.0–10.0) coupled with ≥100 individual reviews. Patient reviews coupled with a review of the literature indicate that when taken in low therapeutic doses under the supervision of a healthcare provider in the absence of drugs known to cause adverse interactions (specifically monoamine oxidases and serotonin reuptake inhibitors) tramadol is a generally safe, effective, and fast-acting medication for relief from depression. This analysis is translational in the sense that it provides a rationale and knowledge-base for physicians to consider including tramadol in the arsenal of medications available to them for treating depression, especially in those patients for whom other antidepressants have not been effective.
Supporting Information Available
The Supporting Information is available free of charge at https://pubs.acs.org/doi/10.1021/acsptsci.0c00132.
All patient comments and ratings regarding the effectiveness of tramadol as an antidepressant; analysis of tramadol consumption for depression: descriptors and queries (PDF)
The author declares no competing financial interest.
Supplementary Material
References
- World Health Organization . (2018) Critical Review Report: Tramadol. https://www.who.int/medicines/access/controlled-substances/Tramadol.pdf?ua=1.
- Halfpenny D. M.; Callado L. F.; Stamford J. A. (1999) Is tramadol an antidepressant?. Br. J. Anaesth. 82 (3), 480–481. 10.1093/bja/82.3.480. [DOI] [PubMed] [Google Scholar]
- Kalra B. S.; Tayal V.; Chawla S. (2008) Antidepressant-like activity of tramadol in mice. Indian J. Psychiatry 50 (1), 51–53. 10.4103/0019-5545.39760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faron-Górecka A.; Kuœmider M.; Inan S. Y.; Siwanowicz J.; Piwowarczyk T.; Dziedzicka-Wasylewska M. (2004) Long-term exposure of rats to tramadol alters brain dopamine and α1-adrenoceptor function that may be related to antidepressant potency. Eur. J. Pharmacol. 501 (1–3), 103–110. 10.1016/j.ejphar.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Yalcin I.; Aksu F.; Bodard S.; Chalon S.; Belzung C. (2007) Antidepressant-like effect of tramadol in the unpredictable chronic mild stress procedure: possible involvement of the noradrenergic system. Behav. Pharmacol. 18 (7), 623–631. 10.1097/FBP.0b013e3282eff109. [DOI] [PubMed] [Google Scholar]
- Yalcin I.; Coubard S.; Bodard S.; Chalon S.; Belzung C. (2008) Effects of 5, 7-dihydroxytryptamine lesion of the dorsal raphe nucleus on the antidepressant-like action of tramadol in the unpredictable chronic mild stress in mice. Psychopharmacology 200 (4), 497–507. 10.1007/s00213-008-1227-3. [DOI] [PubMed] [Google Scholar]
- Caspani O.; Reitz M. C.; Ceci A.; Kremer A.; Treede R. D. (2014) Tramadol reduces anxiety-related and depression-associated behaviors presumably induced by pain in the chronic constriction injury model of neuropathic pain in rats. Pharmacol., Biochem. Behav. 124, 290–296. 10.1016/j.pbb.2014.06.018. [DOI] [PubMed] [Google Scholar]
- Rojas-Corrales M. O.; Gibert-Rahola J.; Micó J. A. (1998) Tramadol induces antidepressant-type effects in mice. Life Sci. 63 (12), PL175–PL180. 10.1016/S0024-3205(98)00369-5. [DOI] [PubMed] [Google Scholar]
- Rojas-Corrales M. O.; Berrocoso E.; Gibert-Rahola J.; Mico J. A. (2002) Antidepressant-like effects of tramadol and other central analgesics with activity on monoamines reuptake, in helpless rats. Life Sci. 72 (2), 143–152. 10.1016/S0024-3205(02)02220-8. [DOI] [PubMed] [Google Scholar]
- Rojas-Corrales M. O.; Berrocoso E.; Gibert-Rahola J.; Micó J. A. (2004) Antidepressant-Like Effect of tramadol and its Enantiomers in Reserpinized Mice: Comparative study with Desipramine, Fluvoxamine, Venlafaxine and Opiates. J. Psychopharmacol. 18 (3), 404–411. 10.1177/026988110401800305. [DOI] [PubMed] [Google Scholar]
- Berrocoso E.; Rojas-Corrales M. O.; Mico J. A. (2006) Differential role of 5-HT 1A and 5-HT 1B receptors on the antinociceptive and antidepressant effect of tramadol in mice. Psychopharmacology 188 (1), 111–118. 10.1007/s00213-006-0464-6. [DOI] [PubMed] [Google Scholar]
- Berrocoso E.; Micó J. A.; Ugedo L. (2006) In vivo effect of tramadol on locus coeruleus neurons is mediated by α2-adrenoceptors and modulated by serotonin. Neuropharmacology 51 (1), 146–153. 10.1016/j.neuropharm.2006.03.013. [DOI] [PubMed] [Google Scholar]
- Berrocoso E.; Sánchez-Blázquez P.; Garzón J.; Mico J. A. (2009) Opiates as antidepressants. Curr. Pharm. Des. 15 (14), 1612–1622. 10.2174/138161209788168100. [DOI] [PubMed] [Google Scholar]
- Berrocoso E.; Ikeda K.; Sora I.; Uhl G. R.; Sánchez-Blázquez P.; Mico J. A. (2013) Active behaviours produced by antidepressants and opioids in the mouse tail suspension test. Int. J. Neuropsychopharmacol. 16 (1), 151–162. 10.1017/S1461145711001842. [DOI] [PubMed] [Google Scholar]
- Yang C.; Li W. Y.; Yu H. Y.; Gao Z. Q.; Liu X. L.; Zhou Z. Q.; Yang J. J. (2012) Tramadol Pretreatment Enhances Ketamine-Induced Antidepressant Effects and Increases Mammalian Target of Rapamycin in Rat Hippocampus and Prefrontal Cortex. J. Biomed. Biotechnol. 2012 (2012), 6. 10.1155/2012/175619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostadhadi S.; Norouzi-Javidan A.; Chamanara M.; Akbarian R.; Imran-Khan M.; Ghasemi M.; Dehpour A. R. (2017) Involvement of NMDA receptors in the antidepressant-like effect of tramadol in the mouse forced swimming test. Brain Res. Bull. 134, 136–141. 10.1016/j.brainresbull.2017.07.016. [DOI] [PubMed] [Google Scholar]
- Chowta M. N.; Manjunath M.; Gopalakrishna H. N.; Gokul P. (2011) Evaluation of role of noradrenergic system in the antidepressant activity of tramadol using tail suspension test in Albino mice. J. Pharmacol. Pharmacother. 2 (4), 281–282. 10.4103/0976-500X.85947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowta M. M.; Mukta N.; Gopalakrishna H. N.; Gokul P. (2011) Evaluation of role of noradrenergic system in the antidepressant activity of tramadol using forced swim test in albino mice. Pharmacologyonline 3, 243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanji N.; Jyothi C. H.; Dinakar K. R.; Vidya H. K. (2015) Evaluation of antidepressant activity of tramadol in swiss albino mice compared to desipramine. Int. J. Pharma Res. Health Sci. 3 (1), 538–543. [Google Scholar]
- Jesse C. R.; Bortolatto C. F.; Savegnago L.; Rocha J. B.; Nogueira C. W. (2008) Involvement of l-arginine–nitric oxide–cyclic guanosine monophosphate pathway in the antidepressant-like effect of tramadol in the rat forced swimming test. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 32 (8), 1838–1843. 10.1016/j.pnpbp.2008.08.010. [DOI] [PubMed] [Google Scholar]
- Jesse C. R.; Wilhelm E. A.; Barbosa N. B.; Nogueira C. W. (2009) Involvement of different types of potassium channels in the antidepressant-like effect of tramadol in the mouse forced swimming test. Eur. J. Pharmacol. 613 (1–3), 74–78. 10.1016/j.ejphar.2009.04.041. [DOI] [PubMed] [Google Scholar]
- Jesse C. R.; Wilhelm E. A.; Bortolatto C. F.; Nogueira C. W. (2010) Evidence for the involvement of the noradrenergic system, dopaminergic and imidazoline receptors in the antidepressant-like effect of tramadol in mice. Pharmacol., Biochem. Behav. 95 (3), 344–350. 10.1016/j.pbb.2010.02.011. [DOI] [PubMed] [Google Scholar]
- Micó J. A.; Rojas-Corrales M. O.; Moreno-Brea M. R.; Ortega-Alvaro A.; Roca-Vinardell A.; Gilbert-Rahola J. (2000) Effectiveness of tramadol as antidepressant in the learned-helplessness model of depression. Eur. Neuropsychopharmacol. 10 (10), 251–252. 10.1016/S0924-977X(00)80212-6. [DOI] [Google Scholar]
- Rojas-Corrales M. O.; Berrocoso E.; Gibert-Rahola J.; Mico J. A. (2002) Antidepressant-like effects of tramadol and other central analgesics with activity on monoamines reuptake, in helpless rats. Life Sci. 72 (2), 143–152. 10.1016/S0024-3205(02)02220-8. [DOI] [PubMed] [Google Scholar]
- Fox M. A.; Jensen C. L.; Murphy D. L. (2009) Tramadol and another atypical opioid meperidine have exaggerated serotonin syndrome behavioural effects, but decreased analgesic effects, in genetically deficient serotonin transporter (SERT) mice. Int. J. Neuropsychopharmacol. 12 (8), 1055–1065. 10.1017/S146114570900011X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkutnik-Fiedler D.; Kus K.; Balcerkiewicz M.; Grześkowiak E.; Nowakowska E.; Burda K.; Ratajczak P.; Sadowski C. (2012) Concomitant use of tramadol and venlafaxine--Evaluation of antidepressant-like activity and other behavioral effects in rats. Pharmacol. Rep. 64 (6), 1350–1358. 10.1016/S1734-1140(12)70932-5. [DOI] [PubMed] [Google Scholar]
- Sirisha G.; Prakash R.; Usha N. S. (2014) Evaluation of antidepressant effect of chronic administration of tramadol alone and in combination with fluoxetine in low doses in albino mice. Int. J. Pharm. Pharm. Sci. 6 (6), 101–105. [Google Scholar]
- Lourdu A. J.; Banupriya R.; Meher Ali R. (2013) Antidepressant effect of Tramadol on balb-c mice in animal models of depression. RJPBCS 4 (2), 1435–41. [Google Scholar]
- Tayal V.; Kalra B. S.; Chawla S. (2008) Evaluation of antidepressant activity of tramadol in mice. Indian journal of pharmacology 40 (3), 129. 10.4103/0253-7613.42307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ubale V. M.; Jaju J. B.; Gosavi P. A.; Pawar G. R.; Dharmadhikari S. C.; Parekar S. M. (2015) Evaluation of antidepressant activity of tramadol in mice: an experimental study. International Journal of Basic & Clinical Pharmacology 4 (3), 463–468. 10.18203/2319-2003.ijbcp20150017. [DOI] [Google Scholar]
- Askar S. J.; Chyad A. H.; Al-Janabi O. S. (2018) Involvement of biogenic amines in antidepressant effect of tramadol in male mice. JEZS 6 (1), 1288–1292. [Google Scholar]
- Varghese J.; Hotchandani S. C.; Shah S. M.; Mathew A. (2020) The Effectiveness of a Combination of Low Dose Citalopram and Tramadol in Reducing Immobility Time in Forced Swimming Test in Mouse Model of Depression. Indian J. Physiol. Pharmacol. 64 (1), 50–58. [Google Scholar]
- Fanelli J.; Montgomery C. (1996) Use of the analgesic tramadol in antidepressant potentiation. Psychopharmacol. Bull. 32 (3), 442–442. [Google Scholar]
- Markowitz J. S.; Patrick K. S. (1998) Venlafaxine-tramadol similarities. Med. Hypotheses 51 (2), 167–168. 10.1016/S0306-9877(98)90112-8. [DOI] [PubMed] [Google Scholar]
- Howland R. H.; Thase M. E. (1999) What to do with SSRI nonresponders?. J. Psychiatr. Pract. 5 (4), 216–223. 10.1097/00131746-199907000-00004. [DOI] [Google Scholar]
- Spencer C. (2000) The efficacy of intramuscular tramadol as a rapid-onset antidepressant. Australian & New Zealand Journal of Psychiatry 34 (6), 1032–1033. 10.1080/000486700284. [DOI] [PubMed] [Google Scholar]
- Shapira N. A.; Verduin M. L.; DeGraw J. D. (2001) Treatment of refractory major depression with tramadol monotherapy. J. Clin. Psychiatry 62, 205–206. 10.4088/JCP.v62n0312b. [DOI] [PubMed] [Google Scholar]
- Minenko S. (2007) P. 2. d. 003 Effect of tramadol on corticosteroid receptor function in patients with major depression. Eur. Neuropsychopharmacol. 17 (17), S363–S364. 10.1016/S0924-977X(07)70532-1. [DOI] [Google Scholar]
- Millan M. J. (2006) Multi-target strategies for the improved treatment of depressive states: conceptual foundations and neuronal substrates, drug discovery and therapeutic application. Pharmacol. Ther. 110 (2), 135–370. 10.1016/j.pharmthera.2005.11.006. [DOI] [PubMed] [Google Scholar]
- Cox S. A.; Reeves R. R. (2008) Similar effects of tramadol and venlafaxine in major depressive disorder. South. Med. J. 101 (2), 193–5. 10.1097/SMJ.0b013e3181616e66. [DOI] [PubMed] [Google Scholar]
- Reeves R. R.; Burke R. S. (2008) Tramadol: basic pharmacology and emerging concepts. Drugs Today 44 (11), 827–836. 10.1358/dot.2008.44.11.1308916. [DOI] [PubMed] [Google Scholar]
- Machado-Vieira R., Manji H. K., and Zarate C. A. (2010) Potential novel therapeutics for bipolar disorders, in Behavioral Neurobiology of Bipolar Disorder and its Treatment, pp 303–329, Springer, Berlin, Heidelberg. [DOI] [PubMed] [Google Scholar]
- Barber J. (2011) Examining the use of tramadol hydrochloride as an antidepressant. Exp. Clin. Psychopharmacol. 19 (2), 123. 10.1037/a0022721. [DOI] [PubMed] [Google Scholar]
- Geracioti T. D. (2014) Tramadol treatment of combat-related posttraumatic stress disorder. Ann. Clin. Psychiatry 26 (3), 217–221. [PubMed] [Google Scholar]
- Tetsunaga T.; Tetsunaga T.; Tanaka M.; Ozaki T. (2015) Efficacy of tramadol–acetaminophen tablets in low back pain patients with depression. J. Orthop. Sci. 20 (2), 281–286. 10.1007/s00776-014-0674-4. [DOI] [PubMed] [Google Scholar]
- Tetsunaga T.; Tetsunaga T.; Tanaka M.; Nishida K.; Takei Y.; Ozaki T. (2016) Effect of tramadol/acetaminophen on motivation in patients with chronic low back pain. Pain Res. Manage. 2016, 7. 10.1155/2016/7458534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rougemont-Bücking A.; Gamma F.; Panksepp J. (2017) Use of tramadol in psychiatric care: a comprehensive review and report of two cases. Swiss Med. Wkly. 147, w14428 10.4414/smw.2017.14428. [DOI] [PubMed] [Google Scholar]
- Duan G.; Wu Z.; Zhao P.; Peng J.; Chen Z.; Zhang Q.; Xu R.; Li H. (2018) Protocol for a randomised, double-blind, placebo-controlled trial to explore the effect of tramadol in the prevention of postpartum depression (ETPPD). BMJ. open 8 (10), e022538 10.1136/bmjopen-2018-022538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan G.; Bao X.; Yang G.; Peng J.; Wu Z.; Zhao P.; Zuo Z.; Li H. (2019) Patient-controlled intravenous tramadol versus patient-controlled intravenous hydromorphone for analgesia after secondary cesarean delivery: a randomized controlled trial to compare analgesic, anti-anxiety and anti-depression effects. J. Pain Res. 12, 49. 10.2147/JPR.S184782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkutnik-Fiedler D.; Grzeskowiak E. (2018) Coexistence of chronic pain and depression: A short review with a focus on the antidepressant effect of tramadol and buprenorphine. Neuropsychiatry 8 (1), 80–88. 10.4172/Neuropsychiatry.1000327. [DOI] [Google Scholar]
- Barakat A. (2019) Revisiting tramadol: a multi-modal agent for pain management. CNS Drugs 33 (5), 481–501. 10.1007/s40263-019-00623-5. [DOI] [PubMed] [Google Scholar]
- Bhusri L.; Bathla M.; Gupta P.; Singh A. H. (2018) Role of tramadol as an augmenting agent in treatment-resistant depression. J. Mental Health Hum. Behav. 23 (2), 137–138. [Google Scholar]
- Saxena P. P.; Bodkin J. A. (2019) Opioidergic Agents as Antidepressants: Rationale and Promise. CNS Drugs 33 (1), 9–16. 10.1007/s40263-018-0584-7. [DOI] [PubMed] [Google Scholar]
- Young M. P., Yates C. M., Idowu O. C., and Charlton J. A. (2009) Treatment of Depression. US12/143,421.
- Young M. P., and McKeown P. (April 2, 2015) Tramadol for Treating Depression. US14/398,201.
- Young M. P., Idowu O. C., and McKeown P. (September 1, 2011) Controlled Release Treatment of Depression. US12/997,643.
- Kugelmann H. (April 20, 2004) Pharmaceutical tramadol salts. US6,723,343.
- https://www.drugs.com/.
- Drugs.com . (1996–2020) User Reviews for Tramadol to treat Depression. https://www.drugs.com/comments/tramadol/for-depression.html (updated 1 July 2020).
- Drugs.com . Medications for Depression. https://www.drugs.com/condition/depression.html (including the database “Drugs Used to Treat Depression” (accessed on September 8, 2020).
- U.S. Food & Drug Administration . (2017) How can I stay better informed about drugs? Is there a reliable website FDA recommends? https://www.fda.gov/drugs/questions-answers/how-can-i-stay-better-informed-about-drugs-there-reliable-website-fda-recommends.
- Drugs@FDA: FDA-Approved Drugs . (1995) New Drug Application (NDA): 020281. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=020281.
- Dunn K. E.; Bergeria C. L.; Huhn A. S.; Strain E. C. (2019) A systematic review of laboratory evidence for the abuse potential of tramadol in humans. Front. Psychiatry 10, 704. 10.3389/fpsyt.2019.00704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall-Flavin D. K. (2019) Antidepressant withdrawal: Is there such a thing? https://www.mayoclinic.org/diseases-conditions/depression/expert-answers/antidepressant-withdrawal/faq-20058133.
- Dragic L., Raouf M., and Fudin J. (2017) What Type of Withdrawal Symptoms from Tramadol Might a Patient Experience? https://www.practicalpainmanagement.com/treatments/what-type-withdrawal-symptoms-tramadol-might-patient-experience.
- Senyasar K.; Balaban O. D.; Yazar M. S.; Eradamlar N. (2015) Tramadol induced depression: report of two cases/Tramadole bagli gelisen depresyon: Iki olgunun sunumu. Anadolu Psikiyatri Dergisi 16 (1), 75–77. [Google Scholar]
- Drugs.com . (2020) TraMADol. https://www.drugs.com/ppa/tramadol.html.
- Marquardt K. A.; Alsop J. A.; Albertson T. E. (2005) Tramadol exposures reported to statewide poison control system. Ann. Pharmacother. 39 (6), 1039–1044. 10.1345/aph.1E577. [DOI] [PubMed] [Google Scholar]
- Ryan N. M.; Isbister G. K. (2015) Tramadol overdose causes seizures and respiratory depression but serotonin toxicity appears unlikely. Clin. Toxicol. 53 (6), 545–550. 10.3109/15563650.2015.1036279. [DOI] [PubMed] [Google Scholar]
- Hassamal S.; Miotto K.; Dale W.; Danovitch I. (2018) Tramadol: understanding the risk of serotonin syndrome and seizures. Am. J. Med. 131 (11), 1382.e1. 10.1016/j.amjmed.2018.04.025. [DOI] [PubMed] [Google Scholar]
- Labate A.; Newton M. R.; Vernon G. M.; Berkovic S. F. (2005) Tramadol and new-onset seizures. Med. J. Aust. 182 (1), 42–43. 10.5694/j.1326-5377.2005.tb06556.x. [DOI] [PubMed] [Google Scholar]
- Sansone R. A.; Sansone L. A. (2009) Tramadol: seizures, serotonin syndrome, and coadministered antidepressants. Psychiatry (Edgmont) 6 (4), 17–21. [PMC free article] [PubMed] [Google Scholar]
- Aminiahidashti H.; Shafiee S.; Mousavi S.; Hajiaghaei G. (2016) Tramadol pill alone may cause serotonin syndrome. Chin. Med. J. (Beijing, China, Engl. Ed.) 129 (7), 877–878. 10.4103/0366-6999.178957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babahajian A.; Khomand P.; Manouchehri F.; Fakhimi R.; Ahsan B.; Amjadian M.; Yousefinejad V. (2019) Seizure Prevalence and Its Related Factors in Tramadol Intoxication; a Brief Report. Arch. Acad. Emerg. Med. 7 (1), e28. [PMC free article] [PubMed] [Google Scholar]
- Nakhaee S.; Amirabadizadeh A.; Brent J.; Miri-Moghaddam E.; Foadoddini M.; Farrokhfall K.; Hosseini M.; Abdollahi M.; Mehrpour O. (2019) Tramadol and the occurrence of seizures: a systematic review and meta-analysis. Crit. Rev. Toxicol. 49 (8), 710–723. 10.1080/10408444.2019.1694861. [DOI] [PubMed] [Google Scholar]
- Morrow R. L.; Dormuth C. R.; Paterson M.; Mamdani M. M.; Gomes T.; Juurlink D. N. (2019) Tramadol and the risk of seizure: nested case-control study of US patients with employer-sponsored health benefits. BMJ. open 9 (3), e026705 10.1136/bmjopen-2018-026705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talaie H.; Panahandeh R.; Fayaznouri M. R.; Asadi Z.; Abdollahi M. (2009) Dose-independent occurrence of seizure with tramadol. J. Med. Toxicol. 5 (2), 63–67. 10.1007/BF03161089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn L. H.; Alderfer R. J.; Graham D. J. (1997) Seizures reported with tramadol. Jama 278 (20), 1661–1661. 10.1001/jama.1997.03550200037026. [DOI] [PubMed] [Google Scholar]
- Jick H.; Derby L. E.; Vasilakis C.; Fife D. (1998) The risk of seizures associated with tramadol. Pharmacotherapy 18 (3), 607–611. 10.1002/j.1875-9114.1998.tb03123.x. [DOI] [PubMed] [Google Scholar]
- Gardner J. S.; Blough D.; Drinkard C. R.; Shatin D.; Anderson G.; Graham D.; Alderfer R. (2000) Tramadol and seizures: a surveillance study in a managed care population. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy 20 (12), 1423–1431. 10.1592/phco.20.19.1423.34854. [DOI] [PubMed] [Google Scholar]
- Drugs.com . (2019) Tramadol Side Effects. https://www.drugs.com/sfx/tramadol-side-effects.htm.
- Tramadol HCL Side Effects by Likelihood and Severity. https://www.webmd.com/drugs/2/drug-4398-5239/tramadol-oral/tramadol-oral/details/list-sideeffects.
- RxList . (2020) Ultram. https://www.rxlist.com/ultram-drug.htm#side_effect.
- Johns Hopkins University, Peripheral Nerve Center . Patient Information: Tramadol (Ultram). https://www.hopkinsmedicine.org/neurology_neurosurgery/centers_clinics/peripheral_nerve/patient_info/TRAMADOL_2007.pdf.
- Expert Committee on Drug Dependence . (2014) Tramadol Update Review Report Agenda item 6.1, World Health Organization, Geneva, Switzerland.
- Park S. H.; Wackernah R. C.; Stimmel G. L. (2014) Serotonin syndrome: is it a reason to avoid the use of tramadol with antidepressants?. Journal of pharmacy practice 27 (1), 71–78. 10.1177/0897190013504957. [DOI] [PubMed] [Google Scholar]
- Thiels C. A.; Habermann E. B.; Hooten W. M.; Jeffery M. M. (2019) Chronic use of tramadol after acute pain episode: cohort study. BMJ 365, l1849. 10.1136/bmj.l1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMik D. E.; Carender C. N.; Shamrock A. G.; Callaghan J. J.; Bedard N. A. (2020) Opioid Use After Total Knee Arthroplasty: Does Tramadol Have Lower Risk Than Traditional Opioids?. J. Arthroplasty 35, 1558. 10.1016/j.arth.2020.01.055. [DOI] [PubMed] [Google Scholar]
- Zeng C.; Dubreuil M.; LaRochelle M. R.; Lu N.; Wei J.; Choi H. K.; Lei G.; Zhang Y. (2019) Association of tramadol with all-cause mortality among patients with osteoarthritis. Jama 321 (10), 969–982. 10.1001/jama.2019.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong S.; Tchoe H. J.; Li J.; Shin J. Y. (2019) All-cause mortality associated with tramadol use: a case-crossover study. Drug Saf. 42 (6), 785–796. 10.1007/s40264-018-00786-y. [DOI] [PubMed] [Google Scholar]
- Felson D. (2019) Tramadol and mortality in patients with osteoarthritis. Jama 322 (5), 465–466. 10.1001/jama.2019.7216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchikanti L.; Kaye A. D.; Hirsch J. A.; Neuroradiology D. I. (2019) Description of Tramadol Mortality in Osteoarthritis May Not Be Accurate. Pain Phys. 22 (4), E364–E365. [PubMed] [Google Scholar]
- Lei G.; Choi H. K.; Zhang Y. (2019) Tramadol and Mortality in Patients With Osteoarthritis—Reply. Jama 322 (5), 466–466. 10.1001/jama.2019.7224. [DOI] [PubMed] [Google Scholar]
- Kloppenburg M.; Berenbaum F. (2020) Osteoarthritis year in review 2019: epidemiology and therapy. Osteoarthritis and Cartilage 28 (3), 242–248. 10.1016/j.joca.2020.01.002. [DOI] [PubMed] [Google Scholar]
- Musich S., Wang S. S., Schaeffer J. A., Slindee L., Kraemer S., and Yeh C. S. (2020). Safety Events Associated with Tramadol Use Among Older Adults with Osteoarthritis. Popul. Health Manage. 10.1089/pop.2019.0220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman M.; Mustafa M. (2018) Tramadol-Induced Mood Elevation in a Patient with No Previous Psychiatric History. Case Reports in Psychiatry 2018, 1. 10.1155/2018/9574395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafezi Moghadam P.; Zarei N.; Farsi D.; Abbasi S.; Mofidi M.; Rezai M.; Mahshidfar B. (2016) Electrocardiographic changes in patients with tramadol-induced idiosyncratic seizures. Turk. J. Emerg. Med. 16 (4), 151–154. 10.1016/j.tjem.2016.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


