Abstract
Background:
Dual use of tobacco cigarettes and e-cigarettes (“dual use”) is the most common poly-tobacco use pattern among U.S. adults. Whether dual use facilitates or inhibits smoking cessation is of concern, yet limited information exists regarding continuation of dual use over time.
Purpose:
This study examined variation in nicotine product use over a one-year period, and evaluated predictors of smoking abstinence among dual users.
Methods:
Data from 1,082 dual users of tobacco cigarettes and e-cigarettes were analyzed using Wave 1 (2013–2014) and Wave 2 (2014–2015) of the Population Assessment of Tobacco and Health Study. Descriptive analyses assessed variation in nicotine product use at Wave 2. Weighted logistic regression was used to identify correlates of smoking abstinence.
Results:
The majority of Wave 1 dual users (88.5%) continued using combustible tobacco at Wave 2: 59.2% were exclusive cigarette smokers, 25.5% remained dual users, and 3.8% reported some other combustible tobacco use pattern. The odds of being smoke-free at Wave 2 were higher among dual users who reported everyday (versus someday) e-cigarette use (aOR: 1.85; 95% CI: 1.18–2.89). Everyday use of tobacco cigarettes was inversely associated with smoking abstinence (aOR 0.33; 95% CI: 0.21–0.51).
Conclusions:
Over a one year period, most dual users still smoked tobacco cigarettes. Frequency of cigarette and e-cigarette use at Wave 1 were each associated with odds of smoking abstinence. Findings suggest that daily e-cigarette use may increase dual users’ chances of becoming smoke free.
Keywords: E-cigarettes, Cigarettes, Dual use, Nicotine dependence, Product use patterns
INTRODUCTION
In the United States, cigarette smoking remains one of the leading causes of preventable morbidity and mortality (GBD 2015 Tobacco Collaborators, 2017), even as the prevalence of smoking continues to decline (Jamal et al., 2018). The primary driver of the health consequences of tobacco smoking is the inhalation of combustion byproducts during use (Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, & Office on Smoking and Health, 2010). As such, alternative nicotine products might offer substantial health risk reductions if smokers’ transitioned to exclusive use of non-combusted products (Goniewicz et al., 2018).
Due to considerable popularity among current and former smokers (Coleman, Rostron, Johnson, & Ambrose, 2017), the potential utility of electronic cigarettes (hereafter ‘e-cigarettes’) as a harm-reduction tool has garnered scrutiny. A substantial knowledge base demonstrates that e-cigarettes (a non-combustible nicotine product) expose users to significantly lower levels of toxicants compared to cigarettes (Goniewicz et al., 2018; National Academies of Sciences, Engineering, and Medicine, 2018), and recent clinical data suggests they may serve as a long-term substitution for smoking and be an effective smoking cessation aid in highly controlled settings (Hajek et al., 2019). However, there is concern that “real-world” concurrent use of cigarettes and e-cigarettes (hereafter ‘dual use’) might prolong smoking behaviors, whereby smokers initiate e-cigarettes for situational use, rather than to quit smoking altogether. Population-based studies have not observed significant reductions in exposure to tobacco-related toxicants among dual users compared to exclusive smokers (Shahab et al., 2017), nor is there evidence of a reduction in all-cause mortality when smokers elect to reduce smoking amounts, as opposed to abstaining completely (Tverdal & Bjartveit, 2006). Additionally, a recent cross-sectional epidemiological study suggest potential cumulative cardiovascular health risk from vaping and smoking among dual users (Bhatta & Glantz, 2019). Alongside growing evidence regarding the health consequences of dual use (Goniewicz et al., 2018), these divergent tracks necessitate the evaluation of dual use patterns for public health consideration.
The current literature base regarding e-cigarettes’ smoking cessation utility within free-living populations is inconclusive: some studies suggest dual use is positively associated with smoking cessation, while others have observed the opposite (Maglia, Caponnetto, Di Piazza, La Torre, & Polosa, 2018). Notably, few prospective assessments of product use patterns have been conducted among highly-generalizable cohorts of dual users (Brose, Hitchman, Brown, & West, 2015; Johnson et al., 2018; Weaver et al., 2018). The present analysis assessed nicotine product use patterns over a one-year period among a sample of adult dual users enrolled in the Population Assessment of Tobacco and Health (PATH) study. Potential correlates of Wave 2 smoking abstinence were evaluated within the analytic sample.
METHODS
Data Source
Data were gathered from Waves 1 and 2 of the PATH Study Public Use Files (PUF), conducted from September 12, 2013 to October 30, 2015. The PATH Study is a nationally representative, longitudinal cohort examining tobacco use and health outcomes among youth and adults from the non-institutionalized, U.S. civilian population. Details on the survey design, sampling methodology, and interview procedures are described in detail elsewhere (Hyland et al., 2017). Among adults surveyed at Wave 1 (n=32,320), the weighted response rate for the Wave 2 survey was 83.2% (n=28,362).
Analytic Sample
A sample of adult dual users was identified from the PATH Wave 1 cohort. Those included met the following criteria: (a) smoked at least 100 cigarettes in their lifetime, (b) currently used both cigarettes and e-cigarettes everyday or some days, and (c) did not currently use any of the following tobacco products: traditional cigars, cigarillos, little filtered cigars, pipe tobacco, hookah, dissolvable tobacco, and snus/smokeless tobacco. The final analytic sample consisted of 1,082 exclusive dual users at Wave 1.
Wave 2 Nicotine Product Use
The primary outcome of interest was current nicotine product use at Wave 2. The following mutually-exclusive categories were developed to characterize participants: (a) continued dual use (using only tobacco cigarettes and e-cigarettes everyday or some days at Wave 2); (b) exclusive cigarette use (using only tobacco cigarettes at Wave 2); (c) exclusive e-cigarette use (using only e-cigarettes at Wave 2); (d) poly-nicotine product use (using one or more newly adopted nicotine-containing products at Wave 2); and (e) complete nicotine product abstinence.
Statistical Analysis
All analyses were conducted in SAS 9.4 using survey commands (i.e., PROC FREQ). Participant baseline characteristics at Wave 1 were described through frequency distributions. Multivariable logistic regression modeling estimated adjusted odds ratios (aOR) and 95% confidence intervals (95% CI) for predictors of smoking abstinence at Wave 2. The outcome was categorized to reflect those who continued to smoke combusted tobacco products at Wave 2 (i.e., continued dual users, exclusive cigarettes smokers, poly-users of combusted products) versus those who became smoke-free at Wave 2 (i.e., exclusive e-cigarette users, those who quit using nicotine-containing products completely). Models were adjusted for age (18–24/25+ years), sex (male/female), race-ethnicity (White/Non-White), and annual household income (<$50,000/$50,000+). In addition, models controlled for type of e-cigarette used (refillable/non-refillable; rechargeable/non-rechargeable), reason for e-cigarette use (Yes/no: “I [use/used] e-cigarettes because… using an e-cigarette [feels/felt] like smoking a regular cigarette”), and frequency of cigarette and e-cigarette use (everyday/some days). All analyses were weighted using longitudinal person-level and replicate weights. P-values < 0.05 were considered statistically significant.
RESULTS
Figure 1 depicts nicotine product use patterns among Wave 1 dual users after one year. Most dual users continued smoking, with 25.5% of dual users reporting dual use at Wave 2, and 59.2% of dual users switching to exclusive cigarette use; 3.8% reported switching to some other poly-tobacco use pattern at Wave 2, all of whom reported using some form of combustible tobacco. Abstinence from smoking was low, with 4.8% of dual users transitioning to exclusive e-cigarette use and 6.7% abstaining entirely from nicotine and tobacco at Wave 2.
Figure 1.
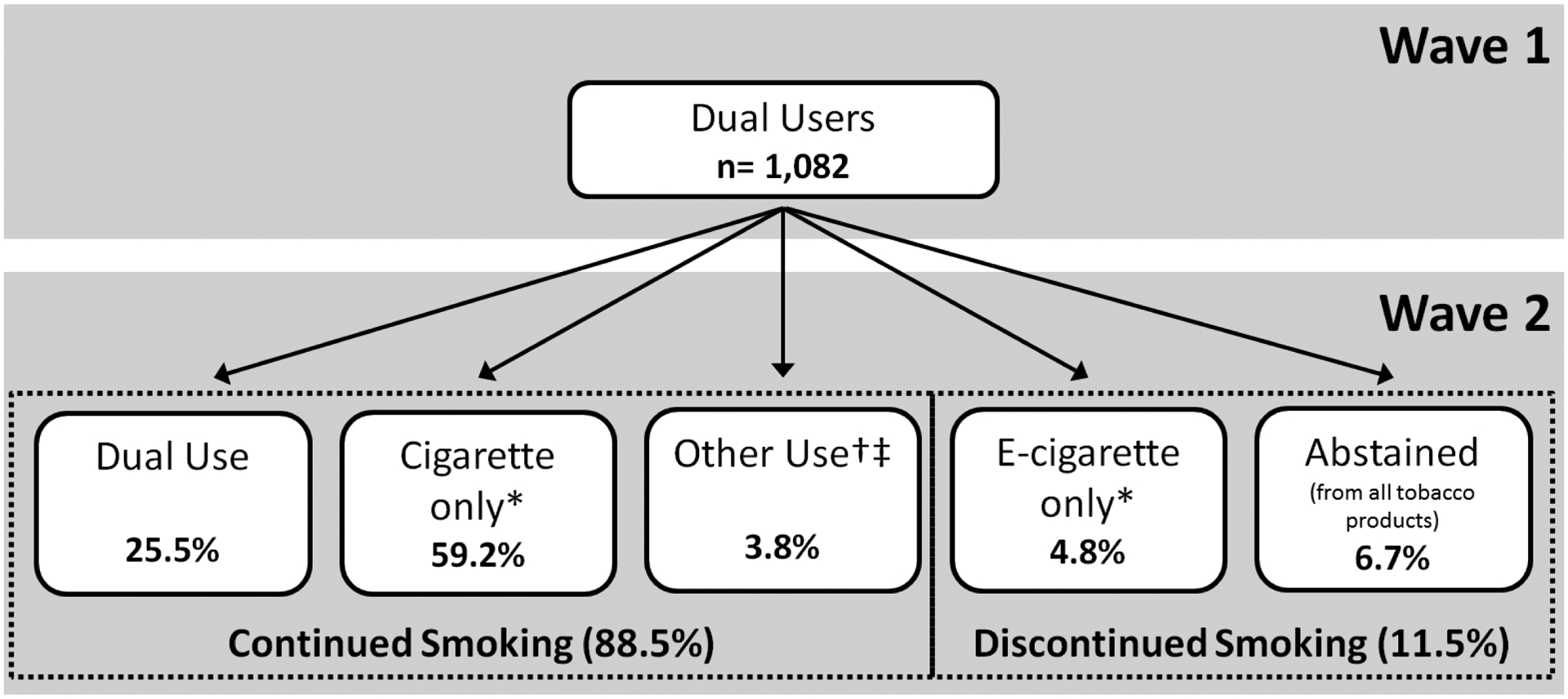
Transitions in tobacco use from Wave 1 to Wave 2 for baseline dual users.
* exclusive single-product use
† ≥ 1 newly adopted nicotine-containing product at Wave 2 (i.e, traditional cigars, hookah, snus, etc.)
‡ All ‘Other Use’ participants reported use of ≥ 1 combusted tobacco products (i.e., cigarette, traditional cigar, cigarillo, etc.)
Table 1 displays multivariable logistic regression results regarding the odds of smoking abstinence at Wave 2. Adjusted findings indicated that the likelihood of abstaining from smoking varied according to annual household income, e-cigarette frequency at Wave 1, and cigarette frequency at Wave 1. Compared with Wave 1 dual users with higher annual household incomes, those who reported annual incomes less than $50,000 had lower odds of smoking abstinence at Wave 2 (aOR: 0.54; 95% CI: 0.34–0.85). Additionally, Wave 1 dual users who used e-cigarettes every day at Wave 1 had 85% higher odds of smoking abstinence at Wave 2 compared with those who used e-cigarettes some days (aOR: 1.85; 95% CI: 1.18–2.89). In contrast, Wave 1 dual users who smoked cigarettes every day were less likely to abstain from smoking at Wave 2 compared to those who smoked some days at Wave 1 (aOR: 0.33; 95% CI: 0.21–0.51). Use of refillable e-cigarettes, use of rechargeable e-cigarettes, and use of e-cigarettes because it “feels like smoking a regular cigarette” were not significantly associated with abstaining from smoking at Wave 2.
Table 1.
Predictors of transitioning from any smoking to smoking abstinence*, among dual users of tobacco cigarettes and e-cigarettes, Waves 1–2, PATH Study (n=1,082).
| aOR (95% CI) | |
|---|---|
| Age (years) | |
| 18–24 | 0.77 (0.38–1.56) |
| 25+ | 1.00 (ref) |
| Sex | |
| Male | 1.08 (0.68–1.73) |
| Female | 1.00 (ref) |
| Race-ethnicity | |
| White | 1.44 (0.85–2.46) |
| Non-white | 1.00 (ref) |
| Annual household income | |
| < $50,000 | 0.54 (0.34–0.85) |
| ≥ $50,000 | 1.00 (ref) |
| Refillable e-cigarette | |
| Yes | 0.87 (0.51–1.48) |
| No | 1.00 (ref) |
| Rechargable e-cigarette | |
| Yes | 1.19 (0.66–2.15) |
| No | 1.00 (ref) |
| Cigarette feel † | |
| Yes | 0.78 (0.47–1.30) |
| No | 1.00 (ref) |
| Cigarette use frequency | |
| Every day | 0.33 (0.21–0.51) |
| Some days | 1.00 (ref) |
| E-cigarette use frequency | |
| Every day | 1.85 (1.18–2.89) |
| Some days | 1.00 (ref) |
Values are adjusted odds ratios (95% confidence intervals)
Dual users were exclusive users at Wave 1 (i.e., no use of other tobacco products besides cigarettes and e-cigarettes)
smoking abstinence = Wave 2 exclusive e-cigarette users or non-users of any nicotine products
Derived from the following questionnaire item: “I [use/used] e-cigarettes because… using an e-cigarette [feels/felt] like smoking a regular cigarette”
DISCUSSION
This study reported changes in nicotine product use over a one-year period among a nationally-representative sample of adult dual users of cigarettes and e-cigarettes in the U.S. The present analysis provides a broad context for scrutinizing dual use patterns and its relationship with smoking cessation. Similar to recently-published findings from a small sample of U.S. dual users (Piper, Baker, Benowitz, & Jorenby, 2019), our findings indicate that, after one year, the majority of dual users continued using tobacco cigarettes, either alone or in combination with other nicotine products. Although transition to smoking abstinence at Wave 2 was limited, dual users that used e-cigarettes on a daily basis had significantly higher odds of being smoke-free at Wave 2. Additionally, the opposite was observed regarding frequency of cigarette use: everyday smokers were significantly less likely to have abstained from smoking at Wave 2. Taken together, these findings illustrate that the frequency of cigarette and e-cigarette use among dual users may be a useful predictor of becoming smoke-free. This coincides with prior research noting key differences between dual users who predominantly use e-cigarettes versus those who predominantly use cigarettes, including for several indicators pertaining to quitting smoking (Borland et al., 2019). Our findings also underscore the need for continued surveillance of behavioral changes over time among dual users, in order to better understand the public health benefits and drawbacks related to e-cigarettes.
From a population health perspective, our findings are particularly relevant in light of results from a recent large, randomized trial assessing the efficacy of e-cigarettes as a smoking cessation aid. Relative to participants randomized to the nicotine-replacement group, Hajek et al. (2019) observed 83% greater odds of 1-year smoking abstinence among the e-cigarette group, providing the strongest evidence to date in support of e-cigarettes harm-reduction potential. Yet, our results from Waves 1 and 2 of the PATH Study indicate a minority of US adult dual users discontinued smoking over a 1-year period. Beyond substantial differences in study design, a couple notable factors differentiate our results from those of the randomized trial. First, the Hajek et al. trial (based in the United Kingdom) enrolled participants who were currently accessing the National Health Service stop-smoking services, and the trial worked in conjunction with the behavioral support network throughout the duration. In contrast, the typical U.S. adult dual user may not utilize or have access to such resources. Additionally, the time frame of data collection (2013–2015) for our study corresponds with first-generation e-cigarette products, which have substantially poorer nicotine delivery in comparison to the more recent e-cigarette technology utilized by Hajek et al. (Farsalinos et al., 2014). In the context of previous trials which used first generation products (Bullen et al., 2013; Caponnetto et al., 2013), improved nicotine delivery likely contributed to the relatively strong effect observed by Hajek et al. Therefore, alongside emphasis towards product use frequency, key differences in quitting resources and device nicotine delivery may highlight important considerations for improving smoking cessation outcomes among dual users.
Strengths of the present analysis include use of the sizable and nationally-representative PATH data. In addition to its rigorous probability-based sampling strategies (Hyland et al., 2017), the PATH Study ascertained highly detailed information pertaining to tobacco and nicotine product use that helps account for use of multiple products. The prospective nature of our analysis offers a unique contribution to the literature and lends credibility to the results. Regarding limitations, restriction of the sample to exclusive dual users may not reflect the most prevalent product use patterns among concurrent cigarette and e-cigarette users. Additionally, no significant associations were observed between e-cigarette device type (refillable or rechargeable) and smoking abstinence at Wave 2. This may have been due in part to suboptimal questionnaire items, as other studies with access to more detailed assessments of device type have observed associations (Chen, Zhuang, & Zhu, 2016; Hitchman, Brose, Brown, Robson, & McNeill, 2015). Finally, due to substantial missing data for relevant questionnaire items (65.8% of sample), the association between e-cigarette nicotine concentration and smoking at Wave 2 was not assessed in our primary analysis. In a brief sensitivity analysis (not published), no statistically significant associations were observed for nicotine concentration (<18 mg vs. ≥18 mg) in either crude or multivariable logistic regression models.
In conclusion, after a 1 year follow-up period, relatively few U.S. adult dual users had discontinued smoking behaviors. Those who did were more likely to use e-cigarettes on a daily basis, while the opposite was true regarding cigarette smoking. In educating the dual user base about maximizing the health benefits of dual use as a transition state, frequency of product use appears to be an important predictor of smoking cessation that should be emphasized.
Funding:
This work was supported by the Roswell Park Comprehensive Cancer Center and National Cancer Institute (NCI) grant P30CA016056.
Disclosure statement: Maciej L. Goniewicz receives fees for serving on an advisory board from Johnson & Johnson and a grant support from Pfizer. The other authors have no conflicts of interest to declare.
REFERENCES
- Bhatta DN, & Glantz SA (2019). Electronic cigarette use and myocardial infarction among adults in the US Population Assessment of Tobacco and Health. Journal of the American Heart Association, 8(12), e012317. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Borland R, Murray K, Gravely S, Fong GT, Thompson ME, McNeill A, … Heckman BW, 2019. A new classification system for describing concurrent use of nicotine vaping products alongside cigarettes (so‐called ‘dual use’): findings from the ITC‐4 Country Smoking and Vaping wave 1 Survey. Addiction, 114(S1), 24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brose LS, Hitchman SC, Brown J, & West R (2015). Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1‐year follow‐up. Addiction, 110(7), 1160–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullen C, Howe C, Laugesen M, McRobbie H, Parag V, Williman J, & Walker N (2013). Electronic cigarettes for smoking cessation: A randomised controlled trial. The Lancet, 382(9905), 1629–1637. [DOI] [PubMed] [Google Scholar]
- Caponnetto P, Campagna D, Cibella F, Morjaria JB, Caruso M, Russo C, & Polosa R (2013). EffiCiency and Safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: A prospective 12-month randomized control design study. PLoS One, 8(6), e66317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, & Office on Smoking and Health. (2010). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention. [PubMed] [Google Scholar]
- Chen C, Zhuang Y-L, & Zhu S-H (2016). E-cigarette design preference and smoking cessation: A US population study. American Journal of Preventive Medicine, 51(3), 356–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman BN, Rostron B, Johnson SE, & Ambrose BK (2017). Electronic cigarette use among US adults in the Population Assessment of Tobacco and Health (PATH) Study, 2013–2014. Tobacco Control, 26(e2), e117–e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farsalinos KE, Spyrou A, Tsimopoulou K, Stefopoulos C, Romagna G, & Voudris V (2014). Nicotine absorption from electronic cigarette use: Comparison between first and new-generation devices. Scientific Reports, 4, 4133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2015 Tobacco Collaborators. (2017). Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: A systematic analysis from the Global Burden of Disease Study 2015. The Lancet, 389(10082), 1885–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goniewicz ML, Smith DM, Edwards KC, Blount BC, Caldwell KL, Feng J, … Borek N (2018). Comparison of nicotine and toxicant exposure in users of electronic cigarettes and combustible cigarettes. JAMA Network Open, 1(8), e185937–e185937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, … Dawkins L (2019). A randomized trial of e-cigarettes versus nicotine-replacement therapy. New England Journal of Medicine, 380(7), 629–637. [DOI] [PubMed] [Google Scholar]
- Hitchman SC, Brose LS, Brown J, Robson D, & McNeill A (2015). Associations between e-cigarette type, frequency of use, and quitting smoking: Findings from a longitudinal online panel survey in Great Britain. Nicotine & Tobacco Research, 17(10), 1187–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland A, Ambrose BK, Conway KP, Borek N, Lambert E, Carusi C, … Cummings KM (2017). Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tobacco Control, 26(4), 371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A, Phillips E, Gentzke AS, Homa DM, Babb SD, King BA, & Neff LJ (2018). Current cigarette smoking among adults—United States, 2016. Morbidity and Mortality Weekly Report, 67(2), 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson L, Ma Y, Fisher SL, Ramsey AT, Chen L-S, Hartz SM, … Baker TB (2018). E-cigarette usage is associated with increased past-12-month quit attempts and successful smoking cessation in two US population–based surveys. Nicotine & Tobacco Research. https://doi.org/doi: 10.1093/ntr/nty211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maglia M, Caponnetto P, Di Piazza J, La Torre D, & Polosa R (2018). Dual use of electronic cigarettes and classic cigarettes: A systematic review. Addiction Research & Theory, 26(4), 330–338. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2018). Public health consequences of e-cigarettes. Washington DC: National Academies Press. [PubMed] [Google Scholar]
- Piper ME, Baker TB, Benowitz NL, & Jorenby DE (2019). Changes in use patterns over 1 year among smokers and dual users of combustible and electronic cigarettes. Nicotine & Tobacco Research. https://doi.org/doi: 10.1093/ntr/ntz065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahab L, Goniewicz ML, Blount BC, Brown J, McNeill A, Alwis KU, … West R (2017). Nicotine, carcinogen, and toxin exposure in long-term e-cigarette and nicotine replacement therapy users: A cross-sectional study. Annals of Internal Medicine, 166(6), 390–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tverdal A & Bjartveit K (2006). Health consequences of reduced daily cigarette consumption. Tobacco Control, 15(6), 472–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver SR, Huang J, Pechacek TF, Heath JW, Ashley DL, & Eriksen MP (2018). Are electronic nicotine delivery systems helping cigarette smokers quit? Evidence from a prospective cohort study of US adult smokers, 2015–2016. PLoS One, 13(7), e0198047. [DOI] [PMC free article] [PubMed] [Google Scholar]


