Abstract
Introduction
Electronic cigarette use (vaping) has been found to be associated with respiratory symptoms like wheezing or whistling in the chest. Whether or not lifetime vaping occurrences are associated with wheezing has not yet been investigated.
Methods
Population Assessment of Tobacco and Health (PATH) Study Wave 4 data with 22,233 adults collected from December 2016 to January 2018 were used. The cross-sectional association of lifetime vaping occurrences with wheezing and related respiratory symptoms was examined using multivariable weighted logistic regression models considering the complex sampling design.
Results
According to the weighted PATH Wave 4 data, about 89.9% adults never vaped, 3.2% adults vaped one time, 3.2% vaped 2–10 times, 1.3% vaped 11–20 times, 1.1% vaped 21–50 times, 0.4% vaped 51–99 times, and 0.9% vaped 100 or more times in their entire life. Compared to adults who never vaped, adults who vaped 2–10 times had a significantly higher association with ever wheezing (aOR = 1.4, 95% CI: 1.1 to 1.6), past 12-month wheezing (aOR = 1.5, 95% CI: 1.2 to 1.9) and the number of wheezing attacks in the past 12 months (aOR = 1.5, 95% CI: 1.2 to 1.8). Adults who vaped 11–20 times and 100 or more times had similar associations with wheezing as that for adults who vaped 2–10 times. Controlling other tobacco use attenuated the associations.
Conclusions
Lifetime vaping occurrences were found to be associated with some definitions of self-reported wheezing in cross-sectional analyses adjusted for other tobacco use.
Implications
Using the cross-sectional PATH Wave 4 data with 22,233 adults, we found significant associations between lifetime vaping occurrences and ever wheezing or whistling in the chest, past 12 months wheezing or whistling in the chest, as well as the number of wheezing attacks in the past 12 months. The study results suggest that larger studies with more precise time frames and measures are needed to further understand possible connections between vaping experimentation and wheezing symptoms that could inform our understanding of the health effects of electronic cigarettes and resultant policy decisions.
Introduction
Electronic cigarette use (vaping) has become increasingly popular in recent years, especially among youth and young adults.1,2 Using the cross-sectional Behavioral Risk Factor Surveillance System (BRFSS) data in 2016, the estimated prevalence of vaping in US adults was 4.5%, corresponding to 10.8 million vapers.3 Besides nicotine, e-cigarette aerosol contains many toxic substances such as volatile organic compounds, cancer-causing chemicals, flavorings, ultrafine particles, and heavy metals such as nickel, tin, and lead.4–8 Although electronic cigarettes were marketed as a harm reduction tool to assist with smoking cessation, its potential effectiveness is controversial, and its long-term health consequence is still unknown.9–16
Wheezing is a common symptom of various respiratory disorders such as asthma and chronic obstructive pulmonary disease (COPD). Wheezing could be caused by inflammation and narrowing of airways.17 Previous studies have shown that vaping can lead to an inflammatory and oxidative response in human cell lines.18,19 Our previous study using the PATH Wave 2 data has shown that vaping is significantly associated with wheezing and related respiratory symptoms compared to nonusers.20 Our investigation on the association of vaping with self-reported COPD using the combined cross-sectional 2016–2017 BRFSS data also indicated that vaping is associated with self-reported COPD.21 A longitudinal study using PATH data also showed the association of vaping with self-reported COPD.22
No study has investigated whether there is an association between lifetime vaping occurrences and self-reported wheezing or related respiratory symptoms. Depending on strict inclusion criteria, we investigated the association between lifetime vaping occurrences and self-reported wheezing and related respiratory symptoms using a subset of the nationally representative PATH Study Wave 4 data collected from December 2016 to January 2018 on 22,233 adults.
Methods
Study Population
The PATH Study is a household-based longitudinal cohort study of nationally representative 45,971 youth and adults in the United States to inform and monitor tobacco use and health in the United States.23 The PATH Study is a collaborative effort between National Institute of Health (NIH) National Institute on Drug Abuse (NIDA) and the US Food and Drug Administration (FDA) Center for Tobacco Products.23 The PATH Study was launched in 2011 with its first Wave of data collected in 2013. The PATH Wave 4 data used in the current study were collected between December 2016 and January 2018 including 33,822 adult participants. The de-identified PATH Wave 4 data are publicly available from the National Addiction & HIV Data Archive Program (NAHDAP) website (https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/36498/datadocumentation).
Our current study focused on the association of lifetime vaping occurrences with wheezing and related respiratory symptoms. To obtain a clean sample for our study, we excluded all subjects who were currently established users of traditional cigars, cigarillos, filtered cigars, blunts only, pipes, hookah, snus pouches, smokeless tobacco, or dissolvable tobacco, as well as all subjects who had ever used marijuana, hash, tetrahydrocannabinol, grass, pot, or weed. As a large proportion of vapers were dual users of electronic nicotine products and cigarettes, we did not exclude cigarette smokers from the sample. After exclusion, we included 22,233 adult subjects in our current study.
Lifetime Vaping Occurrences
The lifetime vaping occurrences variable was defined as the number of times used electronic nicotine products in entire life. The lifetime vaping occurrences variable had seven levels: vaping 0 time (never-users); vaping one time, even just a few puffs; vaping 2–10 times; vaping 11–20 times; vaping 21–50 times; vaping 51–99 times; vaping 100 or more times.
Outcome Variables and Covariates
Self-reported wheezing and related respiratory symptoms were examined in the current study. The outcome variables are (1) ever wheezing—ever had wheezing or whistling in the chest at any time in the past (PATH questions: “Have you ever had wheezing or whistling in the chest at any time in the past?”); (2) Wheezing or whistling in the chest in the past 12 months (PATH question: “Have you had wheezing or whistling in the chest in the past 12 months?”); (3) Chest has sounded wheezy during or after exercise in the past 12 months (PATH question: “In the past 12 months, has your chest sounded wheezy during or after exercise?”); (4) In past 12 months, had a dry cough at night not associated with a cold or chest infection (PATH question: “A dry cough is a cough without phlegm or mucus. In the past 12 months, have you had a dry cough at night?”); (5) In past 12 months, number of wheezing attacks (PATH question: “How many attacks of wheezing have you had in the past 12 months?”).24 Covariates controlled for in the data analysis include age, sex, race/ethnicity, education level, income level, body mass index (BMI), self-perception of physical health, self-perception of mental health, ever smoked a traditional cigar (even one or two puffs), ever smoked a cigarillo or filtered cigar (even one or two puffs), ever smoked a pipe filled with tobacco (even one or two puffs), ever used snus (even one or two times), ever used smokeless tobacco (even one or two times), ever used dissolvable tobacco (even one or two times), ever used any other tobacco products besides cigarettes, electronic nicotine products, traditional cigars, cigarillos, filtered cigars, pipe tobacco, hookah tobacco, snus, smokeless tobacco and dissolvable tobacco, currently lived with anyone who used tobacco or e-cigarettes, asthma, lived with a regular smoker during childhood, home smoking policies, home vaping policies, average number of cigarettes now smoked each day (for included dual users of e-cigarette and combustible cigarette), and duration of cigarette smoking in years. All covariates were categorical variables except the average number of cigarettes now smoked each day and the duration of smoking in years. Covariates were selected according to previously published literatures20 as well as using the purposeful model selection procedures.25 Potential multicollinearity problems among covariates were examined using variance inflation factor values and no multicollinearity problems were identified for our current data analysis.
Statistical Analysis
The association of lifetime vaping occurrences with the covariates and the outcome variables were first examined using weighted frequency distributions and the Rao-Scott Modified Likelihood Ratio tests. The association of lifetime vaping occurrences with the outcome variables were further investigated using both univariable and multivariable weighted logistic regression models with covariates adjusted for in the multivariable weighted logistic regression models. The number of wheezing attacks in the past 12 months was modeled using a multivariable weighted ordinal logistic regression model with the direction on the increasing number of wheezing attacks. The variance in the PATH Wave 4 survey data analysis was estimated using Fay’s method with the value of 0.3 used in the data analysis. The Fay’s method is a variant of the balanced repeated replication method with replicated weights used for variance estimation in survey data analysis. Listwise deletion was used for dealing with missing data in the statistical analyses. The association of lifetime vaping occurrences with the outcome variables was quantified using the estimated odds ratios and their associated 95% confidence intervals. The proc survey procedures in SAS v9.4 (SAS Institute Inc., Cary, NC) were used for all data analysis with a significance level set at 5% for two-sided tests. The goodness of fit of the weighted logistic regression models was examined using the F-adjusted mean residual goodness-of-fit test.
Results
Lifetime Vaping Occurrences Distribution Across Demographic Characteristics
Among the 22,233 adult participants, 21,976 adults indicated their number of times used electronic nicotine products in the entire life (lifetime vaping occurrences). There were 17,248 adult participants indicated that they never vaped (89.9%, 95% CI: 89.4% to 90.3%). Among the adult participants who indicated that they have vaped, 1,520 adults just vaped one time, even just a few puffs (3.2%, 95% CI: 3.0% to 3.4%), 1,448 adults vaped 2–10 times (3.2%, 95% CI: 3.0% to 3.5%), 601 adults vaped 11–20 times (1.3%, 95% CI: 1.1% to 1.4%), 524 adults vaped 21–50 times (1.1%, 95% CI: 1.0% to 1.3%), 202 adults vaped 51–99 times (0.4%, 95% CI: 0.4% to 0.5%), and 433 adults vaped 100 or more times (0.9%, 95% CI: 0.8% to 1.0%).
Supplementary Table 1 shows the weighted prevalence of lifetime vaping occurrences across different demographic characteristics. The young adults group (18–34 years old) had the highest weighted prevalence of having vaped one or more times across the three age groups, followed by the middle-aged adults group (35–64 years old) and older adults group (65 years old or older). The weighted prevalence of vaping 100 or more times was higher for males than for females. Compared to non-Hispanics, there was a higher prevalence of Hispanics who vaped one time, even just a few puffs in their entire life. For race, a higher proportion of Black vaped one time than White and other races. A higher proportion of White adult participants had vaped 100 times or more in their lifetime than Black adults. Adults who had a Bachelor’s degree or advanced degree had a lower weighted prevalence of having vaped one or more times than adults with other educational levels did. In general, the weighted prevalence of having vaped one or more times decreased as the income levels increased across all lifetime vaping occurrences categories. In general, it seems there is a reverse relationship between the self-perception of physical health and having vaped two or more times. Subjects who self-perceived their physical health as fair or poor were more likely to have vaped one or more times than subjects who self-perceived their physical health as very good or excellent. Similarly, there is a reverse relationship between the self-perception of mental health with having vaped two or more times in their lifetime.
Adults who lived with tobacco product users were more likely to have vaped two or more times than adults who did not live with tobacco product users. Marginal significant differences were observed between adults who lived with a regular smoker during childhood and adults who did not live with a smoker during childhood. Adults who allow either smoking or vaping inside their home were more likely to vape at least one time compared to adults who do not allow smoking and vaping inside their home. The average number of cigarettes now smoked every day was higher for adults who vaped between 2 and 99 times than adults in other lifetime vaping occurrences categories. In general, the mean duration of cigarette smoking in years increased as the lifetime vaping occurrences increased. No significant associations of lifetime vaping occurrences with BMI and self-reported asthma were identified.
Association of Wheezing and Related Respiratory Symptoms with Lifetime Vaping Occurrences
There were 3,340 out of 22,233 adult participants reported wheezing or whistling in the chest in the past 12 months (weighted prevalence is 13.5% with 95% CI: 12.9% to 14.2%), while 5,664 adult participants reported ever wheezing (weighted prevalence is 24.1% with 95% CI: 23.2% to 25.0%). In total, 2,446 participants reported that their chest have sounded wheezy during or after exercise in the past 12 months (weighted prevalence is 9.3% with 95% CI: 8.7% to 10.0%). There were 4,216 adults reported dry cough at night not associated with a cold or chest infection during past 12 months (weighted prevalence is 18.3% with 95% CI: 17.3% to 19.3%). Among 22,233 adult participants, 1,901 participants reported one to three wheezing attacks in the past 12 months (weighted prevalence is 7.9% with 95% CI: 7.4% to 8.5%); 625 participants reported 4 to 12 wheezing attacks in the past 12 months (weighted prevalence is 2.4% with 95% CI: 2.1% to 2.7%); 500 participants reported more than 12 wheezing attacks in the past 12 months (weighted prevalence is 2.0% with 95% CI: 1.7% to 2.3%).
Adults who had ever wheezing or had wheezing or whistling in the chest in the past 12 months had a higher weighted prevalence of having vaped two or more times in their entire life than adults who did not have ever wheezing or adults who did not have wheezing or whistling in the chest in the past 12 months (Supplementary Table 1). Similarly, adults who reported one or higher number of wheezing attacks in the past 12 months had a higher weighted prevalence of having vaped two or more times than adults who did not report wheezing attacks in the past 12 months in general. Similarly, adults whose chest have sounded wheezy during or after exercise or had a dry cough at night not associated with a cold or chest infection in the past 12 months, had a higher weighted prevalence of having vaped at least one time in their entire life than adults who did not have those symptoms in the past 12 months (Supplementary Table 1). The unadjusted odds ratios of ever wheezing, past 12 months wheezing, wheezy chest in the past 12 months as well as the number of wheezing attacks in the past 12 months were significantly higher in adults who vaped at least one time than never-users (Table 1). The unadjusted odds ratios of dry cough at night not associated with a cold or chest infection in the past 12 months were significantly higher in adults who vaped two or more times compared to never-users.
Table 1.
Unadjusted and adjusted odds ratios of wheezing and related respiratory symptoms for different lifetime vaping occurrences groups using never-users as the reference
| Ever wheezing–ever had wheezing or whistling in the chest at any time in past (n = 4, 941 for Yes; 13,551 for No) | Wheezing or whistling in the chest in the past 12 months (n = 2,849 for Yes; 15,640 for No) | Wheezy chest during or after exercise in the past 12 months (n = 2,078 for Yes; 16,401 for No) | Dry cough not associated with cold or chest infection in past the 12 months (n = 3,580 for Yes; 14,908 for No) | Number of wheezing attacks in the past 12 months (n = 434 for more than 12; 533 for 4 to 12; 1,632 for 1 to 3; 242 for 0; 15,665 for never in lifetime) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lifetime vaping occurrences | Unadjusted ORs and 95% CI | Adjusted ORs and 95% CI | Unadjusted ORs and 95% CI | Adjusted ORs and 95% CI | Unadjusted ORs and 95% CI | Adjusted ORs and 95% CI | Unadjusted ORs and 95% CI | Adjusted ORs and 95% CI | Unadjusted ORs and 95% CI | Adjusted ORs and 95% CI |
| 1 time, even just a few puffs (n = 1,520) | 1.2 (1.0 to 1.5) | 1.1 (0.9 to 1.4) | 1.3 (1.0 to 1.6) | 1.1 (0.8 to 1.4) | 1.4 (1.2 to 1.8) | 1.1 (0.8 to 1.4) | 1.1 (0.9 to 1.4) | 1.0 (0.8 to 1.2) | 1.3 (1.0 to 1.6) | 1.1 (0.9 to 1.4) |
| 2 to 10 times (n = 1,448) | 1.9 (1.6 to 2.2) | 1.4 (1.1 to 1.6) | 2.2 (1.8 to 2.6) | 1.5 (1.2 to 1.9) | 1.9 (1.6 to 2.4) | 1.2 (0.9 to 1.6) | 1.6 (1.3 to 1.8) | 1.1 (0.9 to 1.4) | 2.2 (1.8 to 2.7) | 1.5 (1.2 to 1.8) |
| 11 to 20 times (n = 601) | 2.5 (2.0 to 3.2) | 1.9 (1.4 to 2.5) | 2.3 (1.8 to 3.0) | 1.6 (1.2 to 2.1) | 2.3 (1.8 to 3.1) | 1.4 (1.0 to 2.0) | 1.5 (1.2 to 2.0) | 1.1 (0.8 to 1.4) | 2.4 (1.8 to 3.1) | 1.6 (1.2 to 2.2) |
| 21 to 50 times (n = 524) | 2.3 (1.9 to 2.8) | 1.4 (1.1 to 1.7) | 2.1 (1.6 to 2.7) | 1.1 (0.8 to 1.6) | 1.9 (1.3 to 2.6) | 1.0 (0.6 to 1.5) | 1.5 (1.2 to 1.9) | 1.0 (0.8 to 1.3) | 2.1 (1.7 to 2.7) | 1.2 (0.9 to 1.7) |
| 51 to 99 times (n = 202) | 3.1 (2.1 to 4.4) | 1.4 (0.9 to 2.2) | 2.6 (1.6 to 4.2) | 1.0 (0.5 to 2.1) | 2.1 (1.4 to 3.1) | 0.9 (0.5 to 1.5) | 1.6 (1.1 to 2.4) | 1.0 (0.6 to 1.7) | 2.7 (1.7 to 4.2) | 1.1 (0.5 to 2.1) |
| 100 or more times (n = 433) | 1.9 (1.5 to 2.5) | 1.4 (1.0 to 2.0) | 2.0 (1.4 to 2.7) | 1.6 (1.1 to 2.3) | 1.7 (1.2 to 2.4) | 1.1 (0.7 to 1.6) | 1.4 (1.1 to 1.8) | 1.1 (0.8 to 1.5) | 1.9 (1.4 to 2.6) | 1.5 (1.1 to 2.1) |
| 0 time, never-users (n = 17,248) | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
Note: The adjusted odds ratios are from multivariable weighted logistic regression and weighted cumulative logistic regression models controlled for age, sex, race/ethnicity, education level, income level, BMI, self-perception of physical health, self-perception of mental health, ever smoked a traditional cigar (even one or two puffs), ever smoked a cigarillo or filtered cigar (even one or two puffs), ever smoked a pipe filled with tobacco (even one or two puffs), ever used snus (even one or two times), ever used smokeless tobacco (even one or two times), ever used dissolvable tobacco (even one or two times), ever used any other tobacco products besides cigarettes, electronic nicotine products, traditional cigars, cigarillos, filtered cigars, pipe tobacco, hookah tobacco, snus, smokeless tobacco and dissolvable tobacco, currently lived with anyone who used tobacco or e-cigarettes, asthma, lived with a regular smoker during childhood, home smoking policies, home vaping policies, average number of cigarettes now smoked each day (for included dual users of e-cigarette and combustible cigarette), and duration of cigarette smoking in years.
After adjusting all the covariates in the model, the unadjusted significant differences between having vaped one time category and never-users were no longer significant for ever wheezing or wheezing in the past 12 months or related respiratory symptoms in the past 12 months (Table 1). For ever wheezing, wheezing or whistling in the chest in the past 12 months, and number of wheezing attacks in the past 12 months, having vaped 2–10 times, 11–20 times, and 100 or more times in entire life remained significant compared to never-users. Having vaped 21–50 times remained significant for ever wheezing, while having vaped 20–50 times and 51–99 times were no longer significant for wheezing or whistling in the chest in the past 12 months and number of wheezing attacks in the past 12 months compared to never-users. For wheezy chest during or after exercise in the past 12 months, only having vaped 11–20 times was significantly different from never-users. Other lifetime vaping occurrences categories were not significantly different from never-users in the estimated odds of wheezy chest during or after exercise in the past 12 months. No observed significant differences were found between subjects who have vaped one or more times and never-users for dry cough at night not associated with a cold or chest infection in the past 12 months after adjusting for covariates.
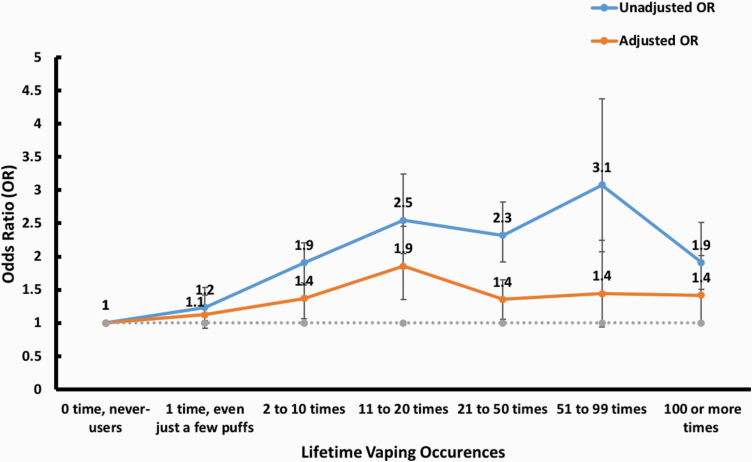
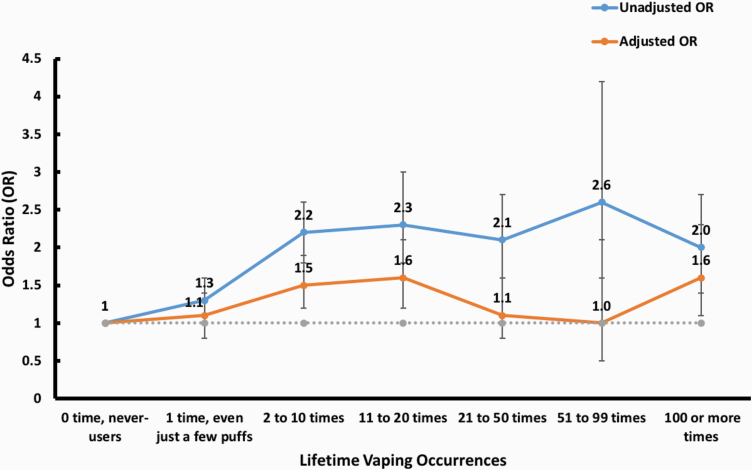
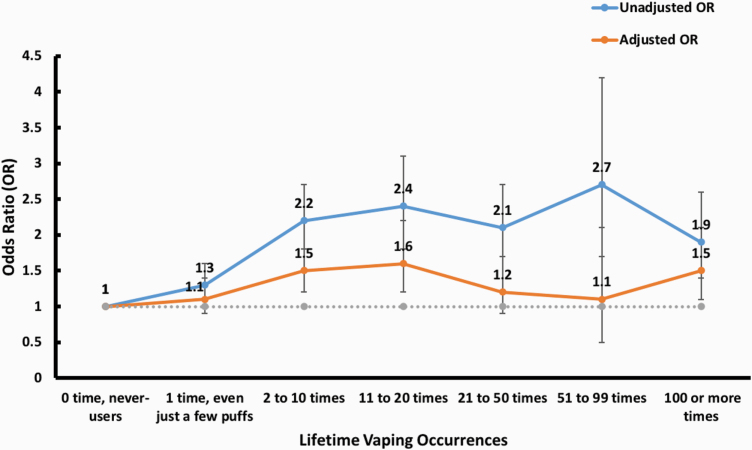
We noticed that there was an increase in estimated odds ratios of ever wheezing and wheezing or whistling in the chest in the past 12 months when lifetime vaping occurrences increased from zero time to one time and further to 2–10 times and 11–20 times (Figures 1 and 2). As the lifetime vaping occurrences further increased to 21–50 times, the estimated odds ratios started to decrease and increased again when the lifetime vaping occurrences increased to 100 or more times (Figures 1 and 2). The estimated odds of having a larger number of wheezing attacks in the past 12 months reached the highest at the lifetime vaping occurrences of 11–20 times and decreased after that until the lifetime vaping occurrences increased to 100 or more times (Figure 3). The estimated odds of having a wheezy chest during or after exercise in the past 12 months reached the maximum at lifetime vaping occurrences of 11–20 times and started to decrease after that (Supplementary Figure 1). For dry cough at night not associated with a cold or chest infection in the past 12 months, the estimated odds reached the maximum at the lifetime vaping occurrences of 2–10 times and remained relatively constant after that (Supplementary Figure 2).
Figure 1.
The association between lifetime vaping occurrences and wheezing or whistling in the chest at any time in the past. The unweighted sample size is 18,492 in this association analysis. The adjusted odds ratios are from the multivariable weighted logistic regression model controlled for age, sex, race/ethnicity, education level, income level, BMI, self-perception of physical health, self-perception of mental health, ever smoked a traditional cigar (even one or two puffs), ever smoked a cigarillo or filtered cigar (even one or two puffs), ever smoked a pipe filled with tobacco (even one or two puffs), ever used snus (even one or two times), ever used smokeless tobacco (even one or two times), ever used dissolvable tobacco (even one or two times), ever used any other tobacco products besides cigarettes, electronic nicotine products, traditional cigars, cigarillos, filtered cigars, pipe tobacco, hookah tobacco, snus, smokeless tobacco and dissolvable tobacco, currently lived with anyone who used tobacco or e-cigarettes, asthma, lived with a regular smoker during childhood, home smoking policies, home vaping policies, average number of cigarettes now smoked each day (for included dual users of e-cigarette and combustible cigarette), and duration of cigarette smoking in years.
Figure 2.
The association between lifetime vaping occurrences and wheezing or whistling in the chest in the past 12 months. The unweighted sample size is 18,489 in this association analysis. The adjusted odds ratios are from the multivariable weighted logistic regression model controlled for age, sex, race/ethnicity, education level, income level, BMI, self-perception of physical health, self-perception of mental health, ever smoked a traditional cigar (even one or two puffs), ever smoked a cigarillo or filtered cigar (even one or two puffs), ever smoked a pipe filled with tobacco (even one or two puffs), ever used snus (even one or two times), ever used smokeless tobacco (even one or two times), ever used dissolvable tobacco (even one or two times), ever used any other tobacco products besides cigarettes, electronic nicotine products, traditional cigars, cigarillos, filtered cigars, pipe tobacco, hookah tobacco, snus, smokeless tobacco and dissolvable tobacco, currently lived with anyone who used tobacco or e-cigarettes, asthma, lived with a regular smoker during childhood, home smoking policies, home vaping policies, average number of cigarettes now smoked each day (for included dual users of e-cigarette and combustible cigarette), and duration of cigarette smoking in years.
Figure 3.
The association between lifetime vaping occurrences and the number of wheezing attacks in the past 12 months. The unweighted sample size is 18,506 in this association analysis. The adjusted odds ratios are from the multivariable weighted cumulative logistic regression model controlled for age, sex, race/ethnicity, education level, income level, BMI, self-perception of physical health, self-perception of mental health, ever smoked a traditional cigar (even one or two puffs), ever smoked a cigarillo or filtered cigar (even one or two puffs), ever smoked a pipe filled with tobacco (even one or two puffs), ever used snus (even one or two times), ever used smokeless tobacco (even one or two times), ever used dissolvable tobacco (even one or two times), ever used any other tobacco products besides cigarettes, electronic nicotine products, traditional cigars, cigarillos, filtered cigars, pipe tobacco, hookah tobacco, snus, smokeless tobacco and dissolvable tobacco, currently lived with anyone who used tobacco or e-cigarettes, asthma, lived with a regular smoker during childhood, home smoking policies, home vaping policies, average number of cigarettes now smoked each day (for included dual users of e-cigarette and combustible cigarette), and duration of cigarette smoking in years.
Discussion
Through analyzing the nationally representative cross-sectional PATH Wave 4 data collected from December 2016 to January 2018, we investigated the association of lifetime vaping occurrences with wheezing and related respiratory symptoms after controlling for potentially confounding covariates. Overall, it seems that there is an association between lifetime vaping occurrences and ever wheezing and past 12 months wheezing as well as number of wheezing attacks in the past 12 months. We noticed that once other tobacco use (including various levels of cigarette use) were included in the adjusted model, the associations between lifetime vaping occurrences and ever wheezing as well as past 12-month wheezing symptoms are attenuated. In general, our study showed vaping 2–10 times and 11–20 times were significantly associated with self-reported wheezing and whistling in the chest at any time in the past and in the past 12 months as well as the number of wheezing attacks in the past 12 months. With the lifetime vaping occurrences increasing, the estimated odds of wheezing related respiratory symptoms slightly increased or remained at similar levels. Vaping one time, even just a few puffs, was not significantly associated with wheezing and related respiratory symptoms. These findings filled in the current knowledge gap on the association of lifetime vaping occurrences with wheezing and related respiratory symptoms. An association between lifetime vaping occurrences of 2–10 and 11–20 times and the odds of ever wheezing and past 12-month wheezing as well as the past 12-month number of wheezing attacks were found.
The insignificant associations of vaping 21–50 times and 51–99 times with ever wheezing, past 12-month wheezing, and the number of wheezing attacks in the past 12 months were likely due to the relatively small sample size in those high lifetime vaping occurrences groups, especially for the lifetime vaping occurrences of 51– 99 times (n = 202). With more samples in those lifetime vaping occurrences groups in future studies, we might have enough power to check whether there is a significant association of those lifetime vaping occurrences groups with ever wheezing, past 12 months wheezing, and the number of wheezing attacks in the past 12 months.
We noticed that most of the comparisons of high frequency of vaping vs. never-users were not significant for wheezy chest during or after exercise past 12 months and dry cough at night not associated with cold or chest infection past 12 months, after adjusting for the covariates in the model (Table 1). The nonsignificances are likely due to the less effect of vaping on those respiratory symptoms compared to ever wheezing or past 12-month wheezing, which is consistent with our previous results comparing current vapers with nonusers.20 We noticed that the average numbers of cigarettes now smoked every day were significantly higher in the lifetime vaping occurrences groups of having vaped 2–99 times than other lifetime vaping occurrences groups (0 time, 1 time, and 100 or more times), indicating a potential moderation effect on wheezing and related respiratory symptoms. We tested the potential moderation effects of the average number of cigarettes now smoked and did not find a significant moderation effect. The test of moderation effects could be underpowered due to the small sample size in some of these lifetime vaping occurrences groups. Therefore, the effects of cigarettes could not be teased out from the effects of vaping. As the majority of the vapers were aged 18–34 years old, we also tested the potential moderation effects of age group and did not find a significant moderation effect. Although we observed longer duration of smoking for adults who had higher lifetime vaping occurrences, the associations of the duration of smoking with all wheezing outcomes were not statistically significant in all multivariable weighted logistic regression models.
To the best of our knowledge, our study is the first one to examine the association of lifetime vaping occurrences with wheezing and related respiratory symptoms. The previous study on the association between exposure to environmental tobacco smoking and respiratory health symptoms among 2,038 adults identified a significant association.26 We also identified a significant association between vaping and wheezing. We found that vaping 11–20 times had the highest association with ever wheezing and past 12-month wheezing as well as the past 12-month number of wheezing attacks among all examined lifetime vaping occurrences.
The current study examined the cross-sectional association between lifetime vaping occurrences and wheezing symptoms using large nationally representative PATH Wave 4 adults in the United States. Our study has several limitations. First, there could be recall bias in this self-reported PATH data. However, self-reported chronic conditions have been found being consistent with medical diagnosis.27 Second, the cross-sectional association does not infer a causal effect relationship as well as the direction of association of lifetime vaping occurrences with wheezing and related respiratory symptoms. The timing of the lifetime vaping occurrences and ever wheezing or past 12-month wheezing symptoms could not be determined from the available information in the PATH survey data. Thus, the direction of the association could not be determined from the cross-sectional exploratory analyses. Third, the small sample size in some of the lifetime vaping occurrences groups limited the power of teasing apart the influence of cigarette smoking from vaping, although the effects of cigarette smoking could be observed from the attenuated odds ratios in the adjusted multivariable weighted logistic regression models after controlling for cigarette smoking and other tobacco product use. Therefore, further studies with a larger sample size are needed to tease out the attributions of lifetime cigarette or other tobacco use in the associations of lifetime vaping occurrence with wheezing symptoms. Finally, some important potential cofounding variables could be missed in the analysis such as the diet and physical activity of the adult participants.
This study found that having vaped 2–20 times and 100 or more times were significantly associated with ever wheezing and past 12-month wheezing as well as the past 12-month number of wheezing attacks in US adults. The study results suggest that larger studies with more precise time frames and measures are needed to further understand possible connections between vaping experimentation and wheezing symptoms that could inform our understanding of the health effects of electronic cigarettes and resultant federal policy decisions.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Funding
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health (NIH) and the Food and Drug Administration (FDA) Center for Tobacco Products under Award Number U54CA228110. Dr. Li’s time is supported in part by the University of Rochester CTSA award number UL1 TR002001 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration (FDA).
Declaration of Interest
Both authors have no potential conflict of interest to declare.
References
- 1. Cullen KA, Gentzke AS, Sawdey MD, et al. e-Cigarette use among youth in the United States, 2019. Jama-J Am Med Assoc. 2019;322(21): 2095–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jenssen BP, Boykan R. Electronic cigarettes and youth in the United States: A call to action (at the local, national and global levels). Children (Basel). 2019;6(2):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mirbolouk M, Charkhchi P, Kianoush S, et al. Prevalence and distribution of E-cigarette use among U.S. adults: Behavioral risk factor surveillance system, 2016. Ann Intern Med. 2018;169(7):429–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bharadwaj S, Mitchell RJ, Qureshi A, Niazi JH. Toxicity evaluation of e-juice and its soluble aerosols generated by electronic cigarettes using recombinant bioluminescent bacteria responsive to specific cellular damages. Biosens Bioelectron. 2017;90:53–60. [DOI] [PubMed] [Google Scholar]
- 5. Behar RZ, Luo W, Lin SC, et al. Distribution, quantification and toxicity of cinnamaldehyde in electronic cigarette refill fluids and aerosols. Tob Control. 2016;25(Suppl 2):ii94–ii102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Blair SL, Epstein SA, Nizkorodov SA, Staimer N. A real-time fast-flow tube study of VOC and particulate emissions from electronic, potentially reduced-harm, conventional, and reference cigarettes. Aerosol Sci Technol. 2015;49(9):816–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Allen JG, Flanigan SS, LeBlanc M, et al. Flavoring chemicals in E-cigarettes: diacetyl, 2,3-pentanedione, and acetoin in a sample of 51 products, including fruit-, candy-, and cocktail-flavored E-cigarettes. Environ Health Perspect. 2016;124(6):733–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Canistro D, Vivarelli F, Cirillo S, et al. E-cigarettes induce toxicological effects that can raise the cancer risk. Sci Rep. 2017;7(1):2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yeh JS, Bullen C, Glantz SA. CLINICAL DECISIONS. E-Cigarettes and smoking cessation. N Engl J Med. 2016;374(22):2172–2174. [DOI] [PubMed] [Google Scholar]
- 10. Hajek P, McRobbie H, Bullen C. E-cigarettes and smoking cessation. Lancet Respir Med. 2016;4(6):e23. [DOI] [PubMed] [Google Scholar]
- 11. Borrelli B, O’Connor GT. E-Cigarettes to assist with smoking cessation. N Engl J Med. 2019;380(7):678–679. [DOI] [PubMed] [Google Scholar]
- 12. Gottlieb MA. E-Cigarettes versus nicotine-replacement therapy for smoking cessation. N Engl J Med. 2019;380(20):1974. [DOI] [PubMed] [Google Scholar]
- 13. Hajek P, Phillips-Waller A, Przulj D, et al. A Randomized trial of E-cigarettes versus nicotine-replacement therapy. N Engl J Med. 2019;380(7):629–637. [DOI] [PubMed] [Google Scholar]
- 14. Przulj D, Hajek P, Phillips-Waller A. E-Cigarettes versus nicotine-replacement therapy for smoking cessation. reply. N Engl J Med. 2019;380(20):1974–1975. [DOI] [PubMed] [Google Scholar]
- 15. Stein JH, Korcarz CE. E-Cigarettes versus nicotine-replacement therapy for smoking cessation. N Engl J Med. 2019;380(20):1973–1974. [DOI] [PubMed] [Google Scholar]
- 16. Zhang Y, Upson D. E-Cigarettes versus nicotine-replacement therapy for smoking cessation. N Engl J Med. 2019;380(20):1973. [DOI] [PubMed] [Google Scholar]
- 17. Luo C, Zou L, Sun H, et al. A review of the anti-inflammatory effects of rosmarinic acid on inflammatory diseases. Front Pharmacol. 2020;11:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Muthumalage T, Prinz M, Ansah KO, Gerloff J, Sundar IK, Rahman I. Inflammatory and oxidative responses induced by exposure to commonly used e-cigarette flavoring chemicals and flavored e-liquids without nicotine. Front Physiol. 2017;8:1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Muthumalage T, Lamb T, Friedman MR, Rahman I. E-cigarette flavored pods induce inflammation, epithelial barrier dysfunction, and DNA damage in lung epithelial cells and monocytes. Sci Rep. 2019;9(1):19035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Li D, Sundar IK, McIntosh S, et al. Association of smoking and electronic cigarette use with wheezing and related respiratory symptoms in adults: Cross-sectional results from the Population Assessment of Tobacco and Health (PATH) Study, Wave 2. Tob Control. 2020;29(2):140–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Xie Z, Ossip DJ, Rahman I, Li D. Use of electronic cigarettes and self-reported chronic obstructive pulmonary disease diagnosis in adults. Nicotine Tob Res. 2020;22(7):1155–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bhatta DN, Glantz SA. Association of E-cigarette use with respiratory disease among adults: A longitudinal analysis. Am J Prev Med. 2020;58(2):182–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) study. Tob Control. 2017;26(4):371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/36498/datadocumentation.
- 25. Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Maziak W, Ward KD, Rastam S, Mzayek F, Eissenberg T. Extent of exposure to environmental tobacco smoke (ETS) and its dose-response relation to respiratory health among adults. Respir Res. 2005;6:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Martin LM, Leff M, Calonge N, Garrett C, Nelson DE. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med. 2000;18(3):215–218. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.