Abstract
Background:
The objective of this study was twofold. First, to update and estimate the economic burden of opioid use disorder (OUD) to the U.S. from the perspectives of the healthcare sector, taxpayer, and society, overall and by age. Second, to estimate the mean present value of averting an OUD, overall and by age, for use in economic evaluations of prevention-focused interventions.
Methods:
This was a retrospective secondary analysis using 2018 data from the National Survey on Drug Use and Health, and the CDC WONDER Database on all U.S. persons, at least 12 years old, with an OUD, or who died of opioid overdose. Total OUD-related costs were estimated according to age and stakeholder perspective. Mean costs weighted by insurance type and the probability of mortality were estimated for each age, then used to estimate the mean present value of OUD aversion according to age and stakeholder perspective.
Results:
The total annual OUD-related costs to the U.S. in 2018 were $786.8 billion to society, $93 billion to taxpayers, and $89.1 billion to the healthcare sector. The mean present value of averting an OUD, across all ages, was $2.2 million, $325,125, and $244,030 from the societal, taxpayer, and healthcare sector perspectives, respectively.
Conclusions and Relevance:
The age-specific values of averting an OUD allow for more robust and targeted economic evaluations of competing interventions to reduce the burden of opioids on multiple stakeholders. The rise in the annual OUD-related cost largely reflects the increase in overdose deaths attributable to synthetic opioids (e.g., fentanyl).
Keywords: opioid use disorder, economic evaluation, prevention, economic burden
1. Introduction
Understanding the economic burden of opioid misuse and use disorder is important in terms of drawing public attention and much-needed resources to the opioid epidemic. Numerous attempts at quantifying this burden have been undertaken (Meyer et al., 2014; Oderda et al., 2015; Reinhart et al., 2018; Strassels, 2009). The majority of past opioid-related economic-burden studies have focused on direct healthcare costs, often accounting for only one or two payer types, finding that persons who misuse opioids or have an opioid use disorder (OUD) are responsible for significantly higher healthcare costs than matched samples without opioid misuse or OUD. Some studies include additional costs that are of importance to society, such as lost productivity, criminal activity, and even premature mortality, and find that opioid misuse and OUD are also associated with high societal costs.
The two most recent, and comprehensive economic burden estimates come from Florence et al. (2016) and the U.S. Council of Economic Advisers (2017), who estimated the annual cost of the opioid crisis to the United States to be $84.6 billion [2018 USD] and $535.3 billion [2018 USD], respectively. Both studies incorporated costs associated with excess healthcare services, criminal justice resources, lost workplace productivity, and premature mortality. The primary driver of the burden difference between the two articles is the method used to estimate costs associated with premature mortality. Florence et al. (2016) adopted the human capital approach by utilizing the Centers for Disease Control and Prevention (CDC) Cost of Injury Reports application within the Web-based Injury Statistics Query and Reporting System (WISQARS) (2019b), which provides an estimate of an individual’s remaining expected lifetime earnings, based on age and sex. The human capital approach has largely fallen out of favor, given its assumption that the value of continuing life is solely a function of an individual’s earnings capacity. The alternative “value of a statistical life” (VSL) methodology utilized by the Council of Economic Advisers to estimate the cost of premature mortality is commonly used by federal agencies and others when conducting cost-benefit analyses of a proposed program, policy, etc. (Office of Management and Budget (OMB); U.S. Department of Health and Human Services (HHS), 2016; U.S. Department of Transportation (DOT), 2016; U.S. Environmental Protection Agency (EPA), 2016). The VSL approach adopts a more holistic view by accounting for preferences through the measurement of what individuals are willing to pay for reductions in risk of mortality (Viscusi, 2013).
The limitation of an economic burden estimate is that it does little to help policymakers and other key stakeholders determine the best use of their scarce resources, thereby limiting the potential impact on public health. Such decisions require comprehensive economic evaluations of competing interventions that include measures of both cost and effectiveness (Drummond et al., 2015). However, economic evaluations that rely on effectiveness measures not associated with an objective monetary value are limited in terms of their interpretation and generalizability.
The study of evidence-based OUD treatment and prevention measures has received a badly-needed influx of resources from the NIH HEAL initiative (2019), and others. A key outcome of many of these studies is the number OUDs averted; however, the value of averting an OUD remains unclear. One cannot simply calculate the arithmetic mean of the total annual costs associated with OUD, because cost-offsets resulting from an effective intervention will accrue over time, and are likely to vary across age groups.
The objective of this study was twofold. First, to update and estimate the economic burden of OUD to the U.S. from the perspectives of the healthcare sector, taxpayer, and society, overall and by age. Second, to estimate the mean present value of averting an OUD, overall and by age, for use in economic evaluations of interventions with a focus on prevention.
2. Methods
2.1. Measures
2.1.1. Stakeholder Perspectives
The healthcare sector perspective included all excess healthcare costs incurred on behalf of persons with OUD, regardless of insurance type. The taxpayer perspective included excess healthcare expenditures for persons insured by Medicare, Medicaid, VA/CHAMPUS, and other non-commercial insurance types, as well as by those who were uninsured; and costs to the criminal justice system. The societal perspective included excess healthcare expenditures for all persons (i.e., healthcare sector costs), criminal justice system costs, costs associated with lost workplace and home productivity, and costs associated with premature mortality.
2.1.2. Opioid Use Disorder
The estimated number of U.S. persons, 12 years of age and older, with OUD (prescription or heroin) was obtained from the 2018 National Survey on Drug Use and Health (NSDUH) (Substance Abuse and Mental Health Services Administration, 2019). NSDUH is a nationally representative survey of noninstitutionalized U.S. civilians 12 years of age and older, that focuses on substance use, substance use and mental health disorders, and use of associated treatment services. Substance use questions, like those asked in the NSDUH, are subject to misclassification bias due to their sensitive nature (Center for Behavioral Health Statistics and Quality, 2019). Although the primary focus of misclassification in the context of substance use is typically on underreporting, it is important to account for the possibility of both false positives and negatives (Biemer and Witt, 1997; Jordan et al., 2008; Murphy et al., 2015; Murphy and Rosenman, 2018). Only one study has evaluated the clinical validity of the NSDUH’s assessment of substance use disorders. Jordan et al. (2008) calculated the psychometric properties of the NSDUH’s assessment of alcohol, cocaine, and marijuana use disorders. The positive and negative predictive value estimates for cocaine use disorder from Jordan et al. (2008) were then combined with the NSDUH estimates of the total number of persons with, and prevalence of cocaine use disorder, to calculate the adjustment factor needed to align the observed and “actual” prevalence. Cocaine use disorder was chosen given its shared categorization with opioids as a “hard” substance (Janik et al., 2017), and consistent findings that such substances are more heavily stigmatized than “soft” substances such as alcohol and marijuana (Brown, 2015; Palamar et al., 2012). Thus, a ratio of 3.06 was applied to the aforementioned OUD figures from the 2018 NSDUH. This is similar to the OUD misclassification rate estimated for Massachusetts by Barocas et al. (2018) using a capture-recapture method. Adjusted cases of OUD were then categorized according to NSDUH-provided age categories and insurance types.
2.1.3. Excess Healthcare Costs
The majority of matched-cohort analyses providing rigorous, age- and sex-adjusted estimates of mean annual, per-person excess-healthcare costs associated with opioid misuse and OUD, do so for commercial insurers. A mean value of $14,001 was calculated from eight studies providing estimates from a commercial insurer perspective (Reinhart et al., 2018) and used in the base-case analysis; the estimates ranged from $3,274 to $24,125 after conversion to 2018 USD using the Medical component of the Consumer Price Index (CPI) (U.S. Department of Labor Bureau of Labor Statistics (BLS)). All inputs are displayed in Supplement Table 1.
Medicaid costs were obtained from three studies that conducted matched cohort analyses similar to those described above. Leslie et al. (2019) estimated the mean annual, per-patient excess Medicaid expenditures from 17 geographically dispersed states for the years 1999–2013. The mean cost associated with opioid misuse and OUD across all years was $8,427 [2018 USD]. Florence et al. (2016) estimated a mean annual, per-person excess-healthcare cost of $15,669 [2018 USD] using data from 11 geographically dispersed states. McAdam-Marx et al. (2010) utilized Medicaid data from all 50 states and the District of Columbia for the years 2002–2003, and found a mean annual, per-person excess-healthcare cost associated with opioid misuse and OUD of $21,281 [2018 USD]. The base-case analysis used the mean annual, per-person expenditure value from these three studies ($15,126, 2018 USD).
Annual adjusted mean excess healthcare expenditures incurred by the VA/CHAMPUS on behalf of persons with OUD were estimated by Baser et al. (2014) for the years 2006–2010. After adjusting for inflation as discussed above, the average annual, per-person cost was estimated to be $20,393 [2018 USD]. The mean per-person Medicaid cost was assigned to persons who were uninsured, or listed an insurance other than those discussed above.
2.1.4. Criminal Justice
Florence et al. (2016) estimated the 2013 criminal justice costs associated with opioid misuse and OUD. The total opioid-related costs attributed to the criminal justice system (i.e., police protection, legal and adjudication, and correctional facilities) were estimated to be $7.89 billion [2018 USD] after adjusting for inflation using the All Item CPI from the BLS. Since criminal justice costs are not distributed evenly over the lifespan, the above figure was apportioned according to the national annual number of arrests across all offenses, by age (Snyder et al., N.D.). The mean annual, per-person cost was then calculated for each age group based on the 2013 NSDUH estimates of persons with OUD, by age (Substance Abuse and Mental Health Services Administration, 2014); the estimates ranged from a low of $1,808 among persons 65 years of age and older, to a high of $7,301 among persons 45–49 years of age, with an overall mean of $4,140, all in 2018 USD.
2.1.5. Lost Productivity
The cost to society of lost productivity associated with non-fatal OUD was estimated using an approach similar to Florence et al. (2016). First, the estimated per-person annual production value of the U.S. population (market and household), by age (Grosse et al., 2009), was adjusted to 2018 USD. Second, the production value of each age group was multiplied by the predicted percentage reduction in productivity attributed to substance use disorder, estimated by the National Drug Intelligence Center (2011). The estimated production reduction values, adjusted for age, marital status, education, and alcohol use disorder, were 17% for females and 18% for males, thus an estimate of 17.5% was used.
2.1.6. Opioid-Related Mortality
The number of opioid-overdose deaths in 2018 was obtained from the CDC WONDER Online Database (2020). Although WONDER provides overdose death estimates for all ages, this study focused on persons 12 years of age and older, in order to align the economic costs of fatal and non-fatal OUD. Deaths of persons for whom an age was “not stated” were excluded from the analysis. Of the 46,802 opioid-overdose deaths reported by the CDC in 2018, across all ages, 99.9% (n=46,744) were confirmed to be among persons 12 years and older. Given the wide recognition that opioid-overdose deaths are underreported, these figures were then adjusted based on Ruhm’s (2017) finding that opioid-overdose deaths were 21% higher than reported in 2015, in accordance with the approach of the Council of Economic Advisers (2017).
According to the literature, willingness to pay for reductions in risk of mortality vary by age; thus, the cost associated with premature mortality was estimated by applying the VSL estimates calculated by Aldy and Viscusi (2008) for the following age groups: 18–24, 25–34, 35–44, 45–54, and 55–62. All VSL estimates were adjusted for real-income growth, inflation, and income elasticity to 2018 USD, commensurate with the most current guidelines set forth by the U.S. DOT (2016). The adjusted VSL estimates rise from $5.3 million among those 18–24 years of age, to a peak of $14 million among those 35–44 years, then fall to $4.9 million among persons 55–62 years of age, with an overall mean of $9.8 million. Of note, the central VSL estimates recommended by the U.S. DOT, EPA, and HHS, range from $9.96 million to $10.70 million [2018 USD] (The Council of Economic Advisers, 2017). The 18–24 VSL estimate was applied to opioid-overdose deaths among persons below the age of 18; similarly, the 55–62 VSL estimate was applied to opioid-overdose deaths among persons older than 62 years of age.
2.2. Analysis
Annual excess healthcare expenditures for each insurance type, by age, were calculated by multiplying the estimated number of persons with OUD in a given category, according to the 2018 NSDUH, by the relevant mean per-person cost, as described above. The costs to the criminal justice system and those associated with lost productivity were calculated for each age by multiplying the estimated number of persons with OUD in a particular age category by the relevant age-specific, mean per-person cost. Similarly, the cost associated with premature mortality was estimated for each age by multiplying the number of opioid-overdose deaths in a given age category by the relevant age-specific VSL. Costs were then summed by and across age(s) according to stakeholder perspective.
Averting an OUD in any given age category will result in saving the related costs that would have been incurred during the immediate time period, as well as those that would have been incurred downstream. Given that the mean per-person cost estimated for each age group is weighted according to insurance type and likelihood of mortality, it was assumed that, holding all else constant, the average person with OUD would accrue the mean per-person costs associated with each age group that they inhabit over time. However, because the benefits of downstream cost-offsets are not received immediately, they must be discounted to account for time-preference. Thus, downstream costs were discounted using the widely-recommended rate of 3% (Neumann et al., 2017). The average U.S. life expectancy at birth in 2017 was 78.7 years (Xu et al., 2020), but surprisingly little work exists to estimate the life expectancy among persons with OUD. Chang et al. (2017) recently estimated the expected years of life lost among U.S. persons with OUD who were seeking buprenorphine or methadone treatment to be 7.7; therefore, this study calculated the present value of OUD aversion for each age from 12 through 71 years, by stakeholder perspective.
2.3. Sensitivity Analysis
The ranges of excess healthcare expenditure estimates incurred by commercial insurers and Medicaid on behalf of persons with OUD (Supplement Table 1) were used to calculate: a) minimum and maximum total annual costs, by age and stakeholder perspective; and b) minimum and maximum values associated with averting an OUD, by age and stakeholder perspective. Additionally, the costs in (a) were estimated using the unadjusted figures for OUD and opioid-overdose deaths. It was not necessary to recalculate (b) using unadjusted figures, given that the same adjustments were effectively made to the numerator and the denominator, resulting in little-to-no change to the per-person figures.
3. RESULTS
Table 1 displays the unadjusted and adjusted number of persons with OUD in 2018, as well as the number of adjusted and unadjusted opioid-overdose deaths for persons 12 years of age and older, according to age categories provided by the NSDUH. In total, there were over 2 million U.S. persons, 12 years of age and older, with OUD in 2018 (Substance Abuse and Mental Health Services Administration, 2019). After adjusting for misclassification, as described above, the total number of persons with OUD rose to 6.3 million, ranging from a low of 18,293 among those 12 years of age, to a high of 1.6 million among those between the ages of 35 and 49 years. According to the CDC (2020) there were 46,744 overdose deaths attributed to opioids in 2018 among persons 12 years of age and older. Adjusting for the underreporting of opioid-overdose deaths brings this figure to 56,560 (Ruhm, 2017). The number of adjusted overdose deaths attributed to opioids ranged from 2 among persons 12 years of age, to 19,650 among those between the ages of 35 and 49 years.
Table 1.
Estimated Cases of Opioid Use Disorder (OUD) and Opioid-Related Overdose Deaths by NSUDH Age Category, 2018
| Persons with OUDa | Opioid Overdose Deathsb | |||
|---|---|---|---|---|
| Age | Unadjusted | Adjusted | Unadjusted | Adjusted |
| 12 | 5,978 | 18,293 | 2 | 2 |
| 13 | 8,824 | 27,001 | 4 | 5 |
| 14 | 8,026 | 24,560 | 12 | 15 |
| 15 | 30,197 | 92,403 | 16 | 19 |
| 16 | 35,007 | 107,121 | 27 | 33 |
| 17 | 22,417 | 68,596 | 82 | 99 |
| 18 | 31,386 | 96,041 | 154 | 186 |
| 19 | 27,919 | 85,432 | 233 | 282 |
| 20 | 48,911 | 149,668 | 375 | 454 |
| 21 | 32,212 | 98,569 | 488 | 590 |
| 22/23 | 86,021 | 263,224 | 1,344 | 1,626 |
| 24/25 | 77,314 | 236,581 | 1,900 | 2,299 |
| 26–29 | 212,021 | 648,784 | 5,144 | 6,224 |
| 30–34 | 268,159 | 820,567 | 6,694 | 8,100 |
| 35–49 | 527,936 | 1,615,484 | 16,240 | 19,650 |
| 50–64 | 492,529 | 1,507,139 | 12,017 | 14,541 |
| 65+ | 129,610 | 396,607 | 2,012 | 2,435 |
| Total | 2,044,467 | 6,256,069 | 46,744 | 56,560 |
Estimated number of persons with OUD, derived from NSDUH (Substance Abuse and Mental Health Services Administration, 2019). Adjusted based on findings from Jordan et al. (2008); see text for details.
Unadjusted opioid overdose deaths obt ained from CDC WONDER (2020); adjusted according to Ruhm’s(2017) finding that opioid overdose deaths were 21% higher than reported in 2015
As shown in Table 2, the total annual opioid-related cost to U.S. society in 2018 was $786.8 billion. Of that $89.1 billion was attributable to the healthcare sector in the way of excess healthcare expenditures, $64.6 billion to lost productivity, $29.9 billion to the criminal justice system, and $603.2 billion to premature mortality. The total opioid-related cost to the U.S. taxpayer was $93 billion, and was comprised of the $29.9 billion to the criminal justice system and $63 billion in excess healthcare expenditures. The cumulative distribution of total annual costs, by age and stakeholder perspective, can be viewed in Figure 1.
Table 2.
Annual Opioid Use Disorder (OUD) Costs, by Age and Perspective (2018 USD)
| 12 | $45,003,296 | $75,730,457 | $166,013,909 | $12,722,326 | $268,461,463 | $241,744,365 | $401,917,541 |
| 13 | $66,428,418 | $111,784,133 | $245,049,637 | $25,444,653 | $396,270,315 | $356,833,770 | $599,927,520 |
| 14 | $60,420,952 | $101,674,915 | $222,888,530 | $76,333,959 | $360,433,539 | $324,563,445 | $598,863,366 |
| 15 | $227,327,622 | $244,732,620 | $838,595,182 | $101,778,612 | $1,356,094,143 | $1,083,327,801 | $1,929,932,996 |
| 16 | $263,538,036 | $268,548,763 | $972,172,783 | $171,751,407 | $1,572,102,780 | $1,240,721,546 | $2,275,940,986 |
| 17 | $168,758,596 | $198,633,096 | $622,538,272 | $521,615,385 | $1,006,708,031 | $821,171,367 | $1,895,715,106 |
| 18 | $236,278,596 | $298,597,648 | $871,614,676 | $979,619,137 | $1,409,490,041 | $1,170,212,325 | $2,923,985,422 |
| 19 | $210,178,491 | $265,613,578 | $921,978,064 | $1,482,151,032 | $1,268,861,489 | $1,187,591,642 | $3,226,804,590 |
| 20 | $920,174,749 | $465,325,609 | $1,615,203,593 | $2,385,436,210 | $2,222,904,986 | $2,080,529,202 | $5,993,841,555 |
| 21 | $606,012,329 | $342,771,874 | $1,063,747,176 | $3,104,247,655 | $1,463,969,565 | $1,406,519,050 | $5,517,001,424 |
| 22/23 | $1,618,334,365 | $915,360,096 | $2,840,698,989 | $8,549,403,378 | $3,909,478,640 | $3,756,059,085 | $14,992,576,479 |
| 24/25 | $1,984,137,052 | $1,010,613,699 | $2,553,164,943 | $19,549,022,975 | $3,513,763,286 | $3,563,778,642 | $26,057,537,012 |
| 26–29 | $6,893,539,152 | $3,286,743,885 | $7,001,637,278 | $71,072,182,548 | $9,635,921,121 | $10,288,381,162 | $90,888,386,706 |
| 30–34 | $10,214,228,598 | $3,372,448,885 | $8,855,500,402 | $92,487,789,653 | $12,187,278,486 | $12,227,949,287 | $118,261,745,623 |
| 35–49 | $21,997,199,588 | $10,783,109,613 | $17,434,199,338 | $271,130,246,778 | $23,993,612,204 | $28,217,308,951 | $327,904,168,183 |
| 50–64 | $16,974,113,129 | $7,465,218,621 | $16,264,942,655 | $119,654,593,051 | $22,384,436,418 | $23,730,161,276 | $166,478,361,220 |
| 65+ | $2,076,391,174 | $717,035,909 | $557,562,993 | $11,940,441,203 | $2,167,920,123 | $1,274,598,902 | $16,901,788,408 |
| Total | $64,562,064,143 | $29,923,943,400 | $63,047,508,419 | $603,244,779,963 | $89,117,706,630 | $92,971,451,819 | $786,848,494,136 |
Figure 1.
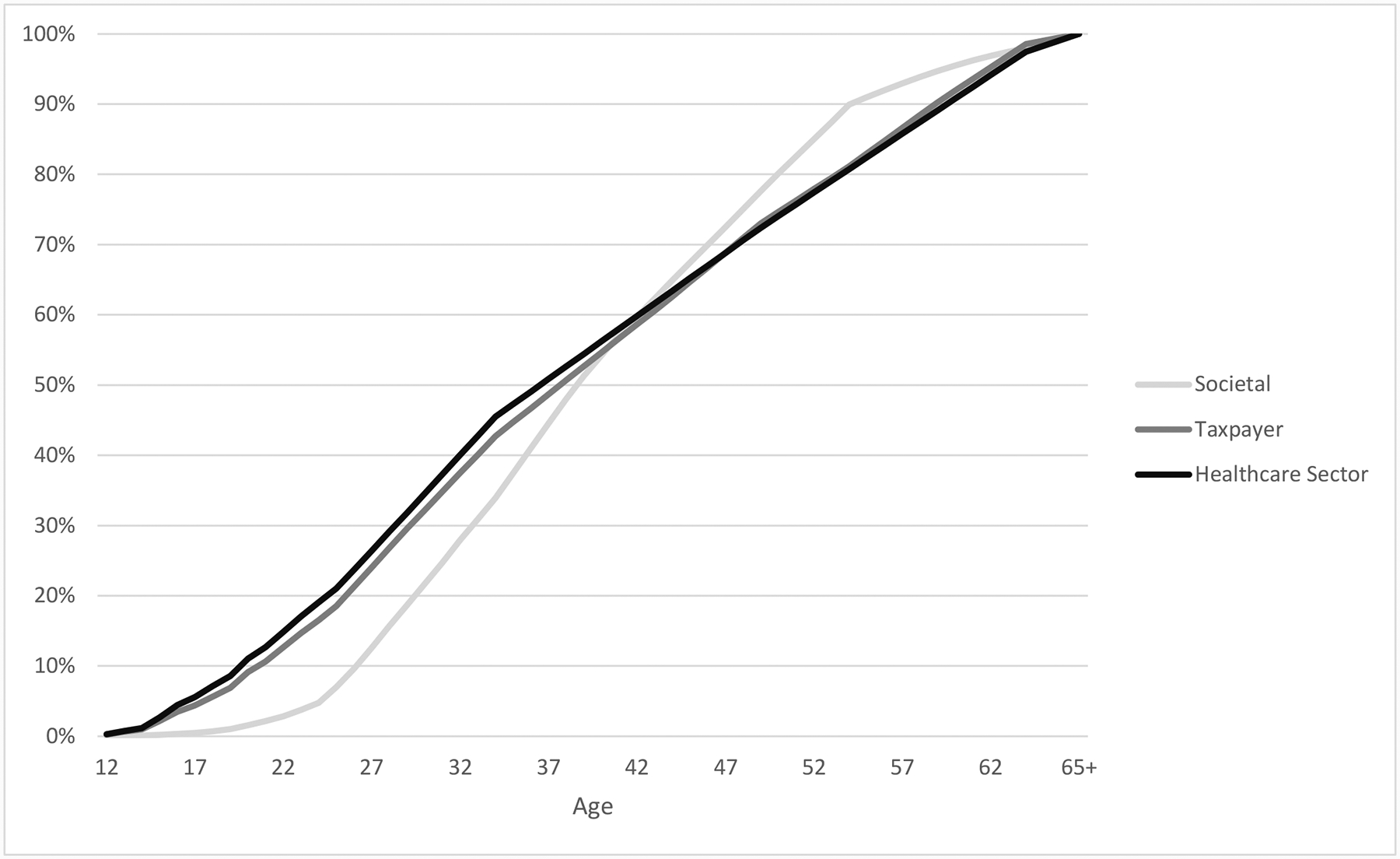
Cumulative Percentage of 2018 Total Opioid Use Disorder (OUD) Costs, by Age and Perspective
Table 3 displays the mean present value of averting an OUD, by age and stakeholder perspective. The mean present value of averting an OUD, across all ages, was $2.2 million from a societal perspective; $325,125 from a taxpayer perspective, and $244,030 from a healthcare sector perspective.
Table 3.
Value of Averting an Opioid Use Disorder (OUD), by Age and Perspective (2018 USD)
| Value of Preventing an OUD, by Age and Perspective | |||||||
|---|---|---|---|---|---|---|---|
| Age | Healthcare | Taxpayer | Societal | Age | Healthcare | Taxpayer | Societal |
| 12 | $409,671 | $543,244 | $3,046,085 | 42 | $269,325 | $367,466 | $2,559,787 |
| 13 | $406,845 | $539,698 | $3,114,837 | 43 | $262,107 | $356,362 | $2,451,182 |
| 14 | $403,934 | $536,045 | $3,185,397 | 44 | $254,672 | $344,925 | $2,334,947 |
| 15 | $400,936 | $532,283 | $3,255,843 | 45 | $247,015 | $333,145 | $2,216,520 |
| 16 | $397,848 | $529,944 | $3,332,006 | 46 | $239,127 | $319,964 | $2,100,578 |
| 17 | $394,667 | $527,680 | $3,410,082 | 47 | $231,003 | $306,386 | $1,977,454 |
| 18 | $391,391 | $524,949 | $3,483,920 | 48 | $222,636 | $292,402 | $1,852,488 |
| 19 | $388,017 | $521,915 | $3,557,079 | 49 | $214,017 | $277,998 | $1,719,915 |
| 20 | $384,359 | $518,715 | $3,624,888 | 50 | $205,140 | $263,162 | $1,583,982 |
| 21 | $380,592 | $515,418 | $3,692,385 | 51 | $195,996 | $251,075 | $1,438,433 |
| 22 | $376,712 | $511,643 | $3,745,506 | 52 | $186,578 | $238,626 | $1,295,630 |
| 23 | $372,716 | $507,754 | $3,803,188 | 53 | $176,877 | $225,803 | $1,147,385 |
| 24 | $368,599 | $503,749 | $3,854,635 | 54 | $166,886 | $212,596 | $992,873 |
| 25 | $364,359 | $499,624 | $3,895,267 | 55 | $156,595 | $198,992 | $828,268 |
| 26 | $359,992 | $493,739 | $3,860,239 | 56 | $145,995 | $182,980 | $760,570 |
| 27 | $355,494 | $487,677 | $3,844,563 | 57 | $135,077 | $166,487 | $693,213 |
| 28 | $350,861 | $481,433 | $3,813,150 | 58 | $123,831 | $149,499 | $624,505 |
| 29 | $346,089 | $475,002 | $3,777,198 | 59 | $112,248 | $132,001 | $558,542 |
| 30 | $341,174 | $468,379 | $3,741,921 | 60 | $100,318 | $113,979 | $495,223 |
| 31 | $336,111 | $462,541 | $3,706,496 | 61 | $88,029 | $97,089 | $437,911 |
| 32 | $330,897 | $456,528 | $3,672,003 | 62 | $75,373 | $79,693 | $381,070 |
| 33 | $325,526 | $450,335 | $3,627,196 | 63 | $62,336 | $61,774 | $328,850 |
| 34 | $319,994 | $443,956 | $3,588,590 | 64 | $48,908 | $43,318 | $278,349 |
| 35 | $314,296 | $437,385 | $3,549,779 | 65 | $35,077 | $24,308 | $232,721 |
| 36 | $308,427 | $428,217 | $3,410,192 | 66 | $30,500 | $21,136 | $185,939 |
| 37 | $302,382 | $418,775 | $3,260,103 | 67 | $25,784 | $17,868 | $146,276 |
| 38 | $296,156 | $409,049 | $3,109,721 | 68 | $20,928 | $14,503 | $109,092 |
| 39 | $289,742 | $399,031 | $2,958,876 | 69 | $15,926 | $11,036 | $76,834 |
| 40 | $283,137 | $388,712 | $2,814,355 | 70 | $10,773 | $7,466 | $48,355 |
| 41 | $276,333 | $378,246 | $2,690,069 | 71 | $5,466 | $3,788 | $24,003 |
| Mean Healthcare (All Ages) | $244,030 | ||||||
| Mean Taxpayer (All Ages) | $325,125 | ||||||
| Mean Societal (All Ages) | $2,238,441 | ||||||
Supplement Table 2 contains the estimated minimum and maximum values for total annual opioid-related costs, by age and stakeholder perspective. Supplement Table 3 contains the same information, but calculated using the unadjusted figures of OUD and opioid-overdose deaths. The estimated minimum-maximum range of total annual opioid-related costs to U.S. society in 2018 was $739.7 billion–$830.7 billion, which drops to $711.4 billion–$741.2 billion using the unadjusted figures for OUD and opioid-overdose death. Supplement Table 4 contains the estimated minimum and maximum values for averting an OUD, by age and stakeholder perspective. The average minimum-maximum ranges of OUD aversion values, across all ages, were $2.1 million–2.4 million from a societal perspective, $224,466–$417,624 from a taxpayer perspective, and $114,828–$364,199 from a healthcare sector perspective.
4. DISCUSSION
This study provided updated estimates of the economic burden associated with OUD; however, unlike prior estimates, these costs are broken down by both age and stakeholder perspective. The opioid-related cost to U.S. society in 2018 was $786.8 billion, which is substantially higher than the two most recent estimates of societal economic burden from Florence et al. (2016) ($84.6 billion, 2018 USD) and the Council of Economic Advisers (2017) ($535.3 billion, 2018 USD). Florence et al. estimated costs associated with excess healthcare services ($31.1 billion), criminal justice resources ($8.3 billion), lost workplace productivity ($22 billion), and premature mortality, calculated via the human capital approach ($23.2 billion). The Council of Economic Advisers used the total non-fatal opioid cost from Florence et al. (2016) to calculate mean per-person non-fatal opioid cost in 2013, which they then adjusted for inflation and applied to the number of persons with OUD in 2015. The Council of Economic Advisers estimated the non-fatal opioid-related cost in 2015 to be $77.9 billion (2018 USD). The Council then estimated the costs associated with premature mortality using the age-specific VSL methodology described above (Aldy and Viscusi, 2008), which came to $465.4 billion (2018 USD). As discussed previously, the VSL approach is typically preferred to the human capital approach, as it accounts for preferences by measuring the amount individuals are willing to pay for reductions in risk of mortality, as opposed to only accounting for earnings capacity (Viscusi, 2013).
The differences in total nonfatal opioid-related costs estimated in this study and those estimated by Florence et al. (2016), are primarily due to the adjustment for misclassification in OUD figures. The difference between the estimated $603.2 billion premature mortality cost and the comparable $465 billion estimate from the Council of Economic Advisers largely reflects the increase in overdose deaths attributable to synthetic opioids (e.g., fentanyl) during that timeframe (Centers for Disease Control and Prevention, 2019a).
The total opioid-related cost to the U.S. taxpayer was $93 billion, which accounted for excess healthcare expenditures incurred by all persons other than those who were commercially insured, and the direct costs to the criminal justice system. As displayed in Table 2 and Figure 1, approximately three-quarters of the annual costs associated with OUD can be attributed to persons in their mid-twenties to late forties, 57% by those between the ages of 30 and 49 years, alone.
The second aim of this paper was to develop objective values of averting an OUD, by age. The ability to assign an objective value to a key effectiveness measure like OUD aversion, greatly enhances its worth in economic evaluations. Otherwise, the use of OUD aversion in economic evaluations is largely limited to cost-effectiveness analyses where it could serve as the denominator of the incremental cost-effectiveness ratio; however, the interpretation of the cost-per-aversion outcome (i.e., whether the intervention of interest would be considered cost-effective) would be subjective, and only comparable to other studies that have used the same effectiveness measure. With an objective value of averting an OUD: a) the cost-per-aversion outcome from a cost-effectiveness analysis can be compared to an objective value threshold to assess cost-effectiveness; b) cases of OUD averted can be monetized and included in the numerator of the incremental cost-effectiveness ratio so that a more generalizable effectiveness measure like quality-adjusted life-years can be used in the denominator; or c) cases of OUD averted can be monetized and used in a cost-benefit or return-on-investment analysis.
Calculating the value of averting an OUD according to age is also critical, given that not only does the cost associated with premature mortality vary by age (Aldy and Viscusi, 2008), but so too does the time available to accrue the downstream cost-offsets. Thus, economic evaluations of OUD prevention interventions that target specific age groups should have age-specific values of aversion. On average, across all ages, the present value of averting an OUD was $244,030 to the healthcare sector, $325,125 to taxpayers, and $2.2 million to society.
4.1. Strengths and Limitations
One limitation of this study, as with all such studies, is the inability to capture all direct and indirect costs associated with OUD, such as: costs associated with use of social support programs; psychological costs incurred by persons with OUD, and their friends and families; costs associated with pain and suffering by victims of related crime; etc. To that end, the societal and taxpayer cost estimates in this study should be considered lower-bound. Another limitation is the necessary reliance on existing monetary estimates for inputs. In each instance a thorough search of the literature was conducted to find robust and relevant estimates; however, such estimates were not available in all cases. For example, in the absence of an excess healthcare expenditure estimate for persons who were either uninsured or reported an insurance other than commercial, Medicaid, Medicare, or VA/CHAMPUS, the Medicaid estimate was applied. Age-specific VSL estimates for calculating the cost of premature mortality were not available for persons under the age of 18, or above the age of 62; thus, the VSL for persons 18–24 years of age was applied to those under 18 years, and the estimate for persons 55–62 years of age was applied to those over the age of 62. There is sufficient evidence that national figures of OUD and opioid-overdose deaths are underestimated, to warrant an adjustment; however, the exact adjustment required is unknown. To address this uncertainty, the minimum-maximum value ranges for average annual total costs were also calculated using the unadjusted OUD and opioid-overdose figures, as part of the sensitivity analyses. Additionally, the estimate of NSDUH misclassification for OUD was based off of the psychometric properties of the NSDUH cocaine use disorder assessment, since the NSDUH OUD assessment has not been clinically validated; the rationale for this adjustment is provided above. Also, the life expectancy of the average person with an OUD was assumed to be 71 years, for the purposes of estimating the mean present value of averting an OUD, which could be a limitation; however, it was based off of recent estimates of average U.S. life expectancy and expected years of life lost among U.S. persons with OUD.
A major strength of this study is the robust estimation of age-specific costs associated with OUD, and values of its aversion. For example, this study estimated premature mortality costs using an age-specific VSL approach, whereas many prior opioid-related economic impact analyses have either ignored premature mortality, undervalued it by only considering the loss of expected earnings, or failed to account for variation by age (The Council of Economic Advisers, 2017). Similarly, unlike most prior studies, age-specific costs associated with reduced home and workplace productivity, as well as criminal activity were calculated. Another strength of this study is the compilation and integration of mean excess healthcare expenditures for multiple payer types, whereas prior studies have typically accounted for only one or two payer types.
5. Conclusions
Understanding the economic burden of the opioid crisis is crucial for drawing public attention and resources to it, but does little to help key stakeholders determine the best use of those resources. The optimal allocation of resources allotted to the prevention of OUD requires comprehensive economic evaluations of competing interventions that include measures of both cost and effectiveness. Effectiveness measures with objective monetary values allow for more flexible, robust, and meaningful economic evaluations. Prior to this study, no such value existed for the aversion of an OUD, which hindered economic evaluations of prevention-focused interventions.
Thus, the objectives of this study were to update and estimate the economic burden of OUD to the U.S. from the perspectives of the healthcare sector, taxpayer, and society, overall and by age; and to estimate the mean present value of averting an OUD, overall and by age. From a societal standpoint there was a substantial increase in the annual opioid-related economic burden between 2015 and 2018, in spite of a reduction in the number of observed persons with OUD from 2.4 million to just over 2 million. This increase largely reflects the rise in opioid-overdose deaths attributable to synthetic opioids, such as fentanyl, during that timeframe. The age-specific OUD-aversion estimates provided here will allow for enhanced, targeted economic evaluations of competing prevention-oriented interventions to reduce the burden of opioids on U.S. stakeholders.
Supplementary Material
Highlights.
Economic cost estimates of opioid use disorder (OUD) can draw attention & resources
Economic cost estimates do not help stakeholders determine best use of resources
Optimal resource allocation requires economic evaluation of cost and effectiveness
Total OUD-related costs were estimated according to age and stakeholder perspective
Age-specific values of OUD aversion allow for robust & targeted economic evaluatio
Role of funding source
The study was supported by the National Institute on Drug Abuse (NIDA) and from the National Institutes of Health (NIH) [grant numbers: R01DA046721 and P30DA040500].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflict declared.
REFERENCES
- Aldy JE, Viscusi WK, 2008. Adjusting the value of a statistical life for age and cohort effects. The Review of Economics and Statistics 90(3), 573–581. [Google Scholar]
- Barocas JA, White LF, Wang J, Walley AY, LaRochelle MR, Bernson D, Land T, Morgan JR, Samet JH, Linas BP, 2018. Estimated prevalence of opioid use disorder in Massachusetts, 2011–2015: A capture–recapture analysis. Am J Public Health 108(12), 1675–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baser O, Xie L, Mardekian J, Schaaf D, Wang L, Joshi AVJPP, 2014. Prevalence of diagnosed opioid abuse and its economic burden in the Veterans Health Administration. 14(5), 437–445. [DOI] [PubMed] [Google Scholar]
- Biemer PP, Witt M, 1997. Repeated measures estimation of measurement bias for self-reported drug use with applications to the National Household Survey on Drug Abuse. NIDA Res Monogr 167, 439–476. [PubMed] [Google Scholar]
- Brown SA, 2015. Stigma towards marijuana users and heroin users. Journal of psychoactive drugs 47(3), 213–220. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2019. 2018 National Survey on Drug Use and Health: Methodological Summary and Definitions. Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Centers for Disease Control and Prevention, 2019a. Synthetic Opioid Overdose. https://www.cdc.gov/drugoverdose/data/fentanyl.html. (Accessed 01/01/2020).
- Centers for Disease Control and Prevention, 2019b. Web-based Injury Statistics Query and Reporting System (WISQARS). https://www.cdc.gov/injury/wisqars/index.html. (Accessed 05/01/2020).
- Centers for Disease Control and Prevention, 2020. Wide-ranging online data for epidemiologic research (WONDER). https://wonder.cdc.gov. (Accessed 05/01/2020).
- Chang K-C, Wang J-D, Saxon A, Matthews AG, Woody G, Hser Y-I, 2017. Causes of death and expected years of life lost among treated opioid-dependent individuals in the United States and Taiwan. International Journal of Drug Policy 43, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond MF, Schulpher MJ, Claxton K, Stoddart GL, Torrance GW, 2015. Methods for the Economic Evaluation of Health Care Programmes, Fourth ed. Oxford university press. [Google Scholar]
- Florence C, Luo F, Xu L, Zhou C, 2016. The economic burden of prescription opioid overdose, abuse and dependence in the United States, 2013. Med Care 54(10), 901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosse SD, Krueger KV, Mvundura M, 2009. Economic productivity by age and sex: 2007 estimates for the United States. Med Care, S94–S103. [DOI] [PubMed] [Google Scholar]
- Janik P, Kosticova M, Pecenak J, Turcek M, 2017. Categorization of psychoactive substances into “hard drugs” and “soft drugs”: A critical review of terminology used in current scientific literature. Am J Drug Alcohol Abuse 43(6), 636–646. [DOI] [PubMed] [Google Scholar]
- Jordan BK, Karg RS, Batts KR, Epstein JF, Wiesen C, 2008. A clinical validation of the National Survey on Drug Use and Health assessment of substance use disorders. Addict Behav 33(6), 782–798. [DOI] [PubMed] [Google Scholar]
- Leslie DL, Ba DM, Agbese E, Xing X, Liu G, 2019. The economic burden of the opioid epidemic on states: the case of Medicaid. Am J Manag Care 25, S243–S249. [PubMed] [Google Scholar]
- McAdam-Marx C, Roland CL, Cleveland J, Oderda GM, 2010. Costs of opioid abuse and misuse determined from a Medicaid database. Journal of pain & palliative care pharmacotherapy 24(1), 5–18. [DOI] [PubMed] [Google Scholar]
- Meyer R, Patel AM, Rattana SK, Quock TP, Mody SH, 2014. Prescription opioid abuse: a literature review of the clinical and economic burden in the United States. Population health management 17(6), 372–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SM, Friesner DL, Rosenman R, 2015. Opioid misuse among adolescents: new evidence from a misclassification analysis. Applied health economics and health policy 13(2), 181–192. [DOI] [PubMed] [Google Scholar]
- Murphy SM, Rosenman R, 2018. The “Real” Number of Washington State Adolescents Using Marijuana, and Why: A Misclassification Analysis. Subst Use Misuse, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Drug Intelligence Center, 2011. The economic impact of illicit drug use on American society. United States Department of Justice, Washington, D.C. [Google Scholar]
- National Institutes of Health, 2019. Helping to End Addiction Long-term. https://heal.nih.gov. (Accessed 12/19/2019).
- Neumann PJ, Sanders GD, Russell LB, Siegel JE, Ganiats TG, 2017. Cost-Effectiveness in Health and Medicine, 2nd ed. Oxford University Press, New York, NY. [Google Scholar]
- Oderda GM, Lake J, Rüdell K, Roland CL, Masters ET, 2015. Economic burden of prescription opioid misuse and abuse: a systematic review. Journal of pain & palliative care pharmacotherapy 29(4), 388–400. [DOI] [PubMed] [Google Scholar]
- Office of Management and Budget (OMB), Regulatory Impact Analysis: A Primer.
- Palamar JJ, Kiang MV, Halkitis PN, 2012. Predictors of stigmatization towards use of various illicit drugs among emerging adults. Journal of Psychoactive Drugs 44(3), 243–251. [DOI] [PubMed] [Google Scholar]
- Reinhart M, Scarpati LM, Kirson NY, Patton C, Shak N, Erensen JG, 2018. The economic burden of abuse of prescription opioids: a systematic literature review from 2012 to 2017. Applied health economics and health policy 16(5), 609–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhm CJ, 2017. Geographic variation in opioid and heroin involved drug poisoning mortality rates. Am J Prev Med 53(6), 745–753. [DOI] [PubMed] [Google Scholar]
- Snyder H, Cooper A, Mulako-Wangota J, Arrest ND Data Analysis Tool. https://www.bjs.gov. (Accessed 05/01/2020).
- Strassels S, 2009. Economic burden of prescription opioid misuse and abuse. Journal of Managed Care Pharmacy 15(7), 556–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2014. Results from the 2013 National Survey on Drug Use and Health: Detailed Tables. [PubMed]
- Substance Abuse and Mental Health Services Administration, 2019. National Survey on Drug Use and Health (NSDUH). https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health. (06/04/2020). [PubMed]
- The Council of Economic Advisers, 2017. The Underestimated Cost of the Opioid Crisis. The White House Office of the Press Secretary. [Google Scholar]
- U.S. Department of Health and Human Services (HHS), 2016. Guidelines for Regulatory Impact Analysis.
- U.S. Department of Labor Bureau of Labor Statistics (BLS), http://www.bls.gov/cpi/. (Accessed 06/29/2020).
- U.S. Department of Transportation (DOT), 2016. Revised Departmental Guidance 2016: Treatment of the Value of Preventing Fatalities and Injuries in Preparing Economic Analyses.
- U.S. Environmental Protection Agency (EPA), 2016. Valuing Mortality Risk Reductions for Policy: A Meta-Analytic Approach.
- Viscusi WK, 2013. Using data from the Census of Fatal Occupational Injuries to estimate the value of a statistical life. Monthly Lab. Rev 136, 1. [Google Scholar]
- Xu JQ, Murphy SL, Kochanek KD, Arias E, 2020. Mortality in the United States, 2018, NCHS Data Brief. National Center for Health Statistics, Hyattsville, MD. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


