Neurological manifestations of COVID-19 in children are not fully understood. Recently, Kaur et al. reported a child with transverse myelitis and McAbee et al. described a child with seizures and encephalitis, in the setting of an acute COVID-19 infection.1 , 2 Acute ischemic stroke (AIS) and focal cerebral arteriopathy have also been reported.3
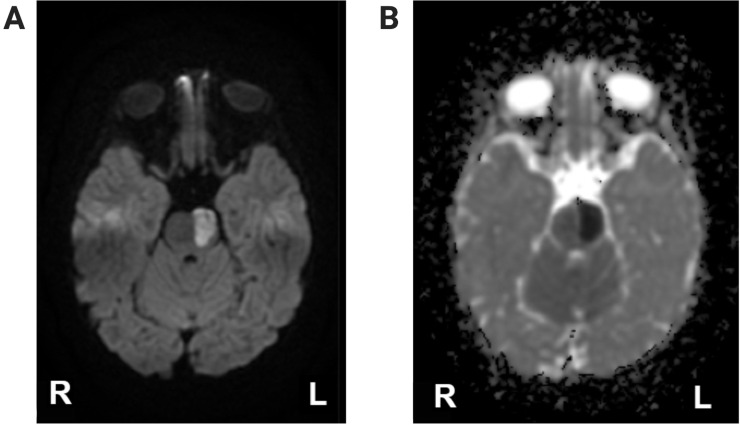
We describe a 17-month-old boy with acute-onset right arm and leg weakness due to a left pontine ischemic stroke. He had anti-COVID-19 antibodies, and his parents had experienced symptoms suggestive of a COVID-19 infection a few weeks earlier. Brain magnetic resonance imaging revealed an acute left pontine infarct (Fig ). Head and neck magnetic resonance angiography was normal. Transthoracic echocardiography was normal.
FIGURE.
Brain imaging of patient. (A) Magnetic resonance diffusion-weighted imaging sequence showing left pontine stroke; (B) magnetic resonance imaging apparent diffusion coefficient sequence.
He had a negative COVID-19 nasopharyngeal polymerase chain reaction (PCR) and positive COVID-19 serologies. Inflammatory, autoimmune, and hypercoagulable evaluation, including multisystem inflammatory syndrome markers, was unremarkable. Genetic testing was normal. The cerebrospinal fluid (CSF) contained 1000 red blood cells/μL, 2 white blood cells/μL, glucose 60 mg/dL (the serum glucose was 90 mg/dL), and protein 15 mg/dL. A CSF Filmarray meningitis/encephalitis PCR panel, New York State encephalitis panel, and varicella zoster virus antibodies were negative. CSF culture revealed no organisms. CSF COVID-19 PCR was not tested as he did not have an acute infection, and antibodies were deferred due to concern for false-positivity from CSF blood contamination.
He was discharged on aspirin 40.5 mg daily. At three-month follow-up, he could run with mild residual weakness.
Although COVID-19 has been associated with AIS in adults, there have been only a few reports in pediatrics. It has been postulated that the virus potentiates a prothrombotic and proinflammatory state via endothelial cell disruption and clotting cascade activation.4 In children, viral pathogens, most notably, varicella zoster virus, are associated with AIS, and vessel imaging can be normal in these cases.5 Although it is possible that our patient’s stroke is idiopathic, we believe that COVID-19 could have been a possible trigger for his stroke given the presence of antibodies, the association of AIS and COVID-19 in adults, and an extensive negative evaluation for other causes of AIS.
Footnotes
1These authors contributed equally to this manuscript.
Conflicts of interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Kaur H., Mason J.A., Bajracharya M. Transverse myelitis in a child with COVID-19. Pediatr Neurol. 2020;112:5–6. doi: 10.1016/j.pediatrneurol.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McAbee G.N., Brosgol Y., Pavlakis S., Agha R., Gaffoor M. Encephalitis associated with COVID-19 infection in an 11-year-old child. Pediatr Neurol. 2020;109:94. doi: 10.1016/j.pediatrneurol.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gulko E., Overby P., Ali S., Mehta H., Al-Mufti F., Gomes W. Vessel wall enhancement and focal cerebral arteriopathy in a pediatric patient with acute infarct and COVID-19 infection. AJNR Am J Neuroradiol. 2020;41:2348–2350. doi: 10.3174/ajnr.A6778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Y., Xiao M., Zhang S. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Askalan R., Laughlin S., Mayank S. Chickenpox and stroke in childhood: a study of frequency and causation. Stroke. 2001;32:1257–1262. doi: 10.1161/01.str.32.6.1257. [DOI] [PubMed] [Google Scholar]