In collaboration with the National Heart, Lung, and Blood Institute, Operation Warp Speed, the US Food and Drug Administration, and as part of the Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) initiative, the 3 of us have been asked to lead nationwide randomized clinical trials of anticoagulant and antithrombotic therapies to improve clinical outcomes among coronavirus disease 2019 (COVID-19)–infected inpatients and outpatients and those convalescing from the disease. Known collectively as ACTIV-4 Antithrombotics, the need for these trials is clear because life-threatening deep vein thromboses, pulmonary emboli, systemic arterial thromboses, and microvascular thromboses occur commonly in patients with COVID-19, even among those who appear otherwise minimally symptomatic.
Lacking trial data, cardiologists caring for patients with COVID-19 have little guidance on how to proceed with thrombosis prevention and, as a result, are using a wide variety of interventions, none of which has been tested in trials of adequate sample size. Is the best choice of treatment for patients acutely ill with COVID-19 requiring hospitalization unfractionated or low-molecular-weight heparin? If so, at what dose should this medication be administered, or should alternative agents be considered? For patients being discharged after hospitalization for COVID-19, should anticoagulation be continued, and if so, for how long and can a simple oral regimen such as prophylactic-dose apixaban be used? For patients with COVID-19 who are not hospitalized and who will convalesce at home, should we treat at all, use an antithrombotic-like low-dose aspirin, an anticoagulant at a prophylactic dose, or an anticoagulant at a therapeutic dose? And across the full spectrum of COVID-19 illness, can we use biomarkers of thrombosis and inflammation to maximize benefit and minimize hemorrhagic risk?
Answering these questions challenges us to reconsider our understanding of equipoise in times of crisis. Equipoise and equilibrium derive from the same root that implies not only balance but uncertainty. In the clinical realm, this uncertain balance translates into inadequate knowledge of the risk-to-benefit ratio associated with a given therapeutic intervention for the population at large, for specific subgroups of patients with greater or lesser anticipated risk, and ultimately for the individuals we personally care for. The core principle of equipoise asserts that we as caregivers do not know what is best for patient care and that, in the setting of genuine uncertainty, we are willing to test different interventions through random allocation. In this time of international pandemic, we believe this willingness should be elevated to a professional obligation.
Equipoise demands trust and humility. When a thoughtful physician says to his or her patient, “I do not know what is best for you and I therefore think you should consider enrolling in a randomized trial,” the physician is not side-stepping professional responsibility. To the contrary, such a physician is being fully honest and transparent with the knowledge that only randomization can guarantee that all potential confounders, known and unknown, are equally distributed across study groups and, therefore, that a definitive answer to a life-threatening question can be ascertained. In a time of public health crisis, that honesty about what does and does not work is furthermore a statement of empathy for our communal lack of knowledge, a recognition that we are all in the same situation together, and that we must share the burden and risks of trial participation equably across society.
As clinical trialists, we are intimately aware that the monitoring of safety and efficacy during COVID-19 is complex. Our protocols must be adaptive and allow proven therapies such as remdesivir, proning, and dexamethasone to be used without altering overall equipoise for the novel intervention at hand. Our investigators must have a willingness to alter and rapidly update trial aims, protocols, treatment targets, sample size calculations, and manuals of operation on timetables that challenge long established traditions of deliberative caution. Our institutional review boards must show the flexibility and speed to address the needs of electronic-based consent, low-touch trial designs, and risk-based monitoring. Members of our Data and Safety Monitoring Boards must take on levels of responsibility for trial conduct that, in some instances, can require weekly virtual meetings as data evolve. Our statistical colleagues, many long engaged solely in frequentist approaches, are being asked to address both Bayesian and adaptive trial designs that can incorporate posterior probabilities calculated from accruing data to allow the addition or closure of specific study arms. We are pleased to report that all these innovations are incorporated into many federally sponsored trials addressing the infectious, respiratory, neurological, and cardiovascular complications of COVID-19.
Of utmost importance, however, we cannot lose the trust of our patients. Public reticence to enroll in an intervention trial or to consider a preventive vaccine trial will undermine our ability to know what truth is and how best to apply it to save lives. Consistent and accurate messaging from regulatory agencies and public health officials is crucial to maintaining this trust. At both home and abroad, we need to enroll participants in adequately powered COVID-19 trials as quickly as possible to provide firm clinical evidence for practitioners on what to do, in whom, and when. No obstruction to these goals should be introduced or tolerated.
Patients enter trials not only for themselves but also for the benefit of their neighbors, both those known and unknown. That is the generosity that our patients provide—it needs to be respected, and we need to insist that a strategy is in place to affirm these values during the time of pandemic.
We encourage cardiologists consulting on patients with COVID-19 to consider enrollment in the National Institutes of Health ACTIV trials. ACTIV-1 is addressing the role of immune modulators in hospitalized adults with moderate to severe COVID-19 disease as add-on therapy to remdesivir and dexamethasone. ACTIV-2 is addressing the potential utility of monoclonal antibodies and other novel therapeutics in outpatients with COVID-19, whereas ACTIV-3 is addressing similar questions of efficacy and risk in inpatients with COVID-19. The ACTIV-4 antithrombotic trials discussed above and most relevant to cardiologists are summarized in the Figure. Descriptions of all the ACTIV trials, how to refer potential trial participants, and how to be considered as a study site are available at “COVID-19 Therapeutics Prioritized for Testing in Clinical Trials" on the National Institutes of Health website.1
Figure.
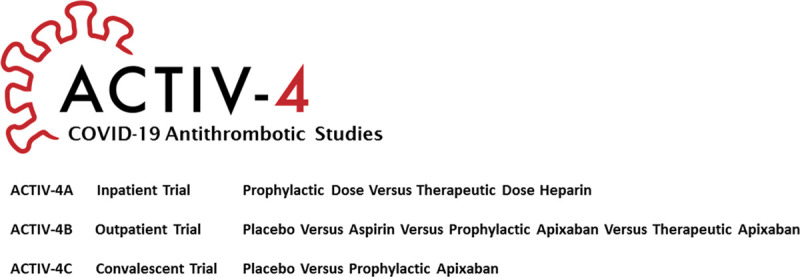
Overview of the ACTIV-4 COVID-19 antithrombotic studies. ACTIV indicates Accelerating COVID-19 Therapeutic Interventions and Vaccines; ACTIV-4, ACTIV protocol for antithrombotics; and COVID-19, coronavirus disease 2019.
Disclosures
Active drug and matching placebo for the ACTIV-4B Outpatient and ACTIV-4C Convalescent trials are generously provided by Bristol Myers Squibb and Pfizer, Inc. The institutions where Drs Ridker, Ortel, and Hochman are employed have received or will receive research grants from the National Heart, Lung, and Blood Institute to conduct the ACTIV-4 trials. Dr Ridker has received an investigator-initiated grant from Pfizer, Inc for research not related to this commentary.
Footnotes
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
Contributor Information
Thomas L. Ortel, Email: thomas.ortel@duke.edu.
Judith S. Hochman, Email: judith.hochman@nyumc.org.
Reference
- 1.COVID-19 therapeutics prioritized for testing in clinical trials. National Institutes of Health. Accessed October 25, 2020. https://www.nih.gov/research-training/medical-research-initiatives/activ/covid-19-therapeutics-prioritized-testing-clinical-trials.


