Abstract
Avian Pathogenic Escherichia coli (APEC) cause colibacillosis leading to significant economic losses in the poultry industry. This laboratory-based study aimed at establishing stocks of avian pathogenic Escherichia coli lytic bacteriophages, for future development of cocktail products for colibacillosis management. The study determined the antibiotic susceptibility; phylogenetic categories, occurrence of selected serotypes and virulence genes among Escherichia coli stock isolates from chicken colibacillosis cases; and evaluated bacteriophage activity against the bacteria. Escherichia coli characterization was done through phenotypic and multiplex PCR methods. Bacteriophage isolation and preliminary characterization was achieved using the spot assay and overlay plating techniques. Fifty-six (56) isolates were phenotypically confirmed as E. coli and all exhibited resistance to at least one antimicrobial agent; while multi-drug resistance (at least three drugs) was encountered in 50 (89.3%) isolates. The APEC isolates mainly belonged to phylogroups A and D, representing 44.6% and 39.3%, respectively; whereas serotypes O1, O2 and O78 were not detected. Of the 56 isolates, 69.6% harbored at least one virulence gene, while 50% had at least four virulence genes; hence confirmed as APEC. Virulence genes, ompT and iutA were the most frequent in 33 (58.9%) and 32 (57.1%) isolates respectively; while iroN least occurred in 23 (41.1%) isolates. Seven lytic bacteriophages were isolated and their host range, at 1×108 PFU/ml, varied from 1.8% to 17.9% of the 56 APEC isolates, while the combined lytic spectrum was 25%. Phage stability was negatively affected by increasing temperatures with both UPEC04 and UPEC10 phages being undetectable at 70°C; whereas activity was detected between pH 2 and 12. The high occurrence of APEC isolates resistant against the commonly used antibiotics supports the need for alternative strategies of bacterial infections control in poultry. The low host range exhibited by the phages necessitates search for more candidates before in-depth phage characterization and application.
Introduction
Avian colibacillosis refers to any localized or systemic infection caused by Avian Pathogenic Escherichia coli (APEC) belonging to several serogroups; and remains one of the most prevalent bacterial diseases affecting the poultry industry worldwide [1]. The disease causes mortality and morbidity on poultry farms leading to grave economic losses as the infected birds keep dying and those that survive are mostly underweight hence commercially not viable [2, 3]. In the Netherlands, economic losses to the poultry industry due to colibacillosis was estimated at € 0.4–3.7 million [4]. Not much information exists for African countries, but in Nigeria, 40% of broiler mortality was caused by APEC, which led to a loss of several millions of dollars [5]. In Uganda, information on economic significance of colibacillosis is not available but it is the most frequent bacterial infection among the chicken samples submitted to the Central Diagnostic Laboratory with a prevalence of 14% [6].
Colibacillosis is commonly associated with poultry under the intensive management systems and affects all age groups due to stress caused by concurrent infections and poor environmental conditions [7]. Depending on the system or organ affected, APEC gives rise to a myriad of conditions which include, colisepticaemia, egg peritonitis and yolk sac infection among others; and the clinical presentations vary accordingly [8–10]. Signs of colibacillosis are non-specific and include sudden death, weakness, lethargy, depression, reduced appetite, poor growth and may have pasted vent or diarrhoea. Disease severity is determined by age, duration of infection, management conditions and existing co-infections [11, 12].
Antimicrobial resistance is widespread but variations between drug type and among the APEC isolates from different countries exist [10, 13–15]. Several studies have reported resistance of E. coli isolates to some drugs such as tetracycline, ampicillin, sulphamethoxazole/trimethoprim, ciprofloxacin, gentamycin and nalidixic acid [2, 10, 13–15]. Frequent usage of antibiotics in commercial poultry production systems is considered as the reason for occurrence of drug resistance [15]. Multidrug resistance is very common and resistance to more than two or three antimicrobials has been reported [10, 11, 14–16]. In Uganda, one study reported 87% Escherichia coli, isolated from broiler farms kept under the deep litter system, being resistant to at least one antimicrobial agent [17].
Avian pathogenic E. coli can be characterized based on virulence factors, serotype, phylogenetic group and drug resistance. Avian pathogenic E. coli possess various virulence-associated genes that permit extra-intestinal survival; and among these genes, iutA, hlyF, iss, iroN, and ompT, were suggested as the minimum that can be used to identify an APEC strain with the highest pathogenicity [18]. Escherichia coli belong to four major phylogenetic groups that include A, B1, B2 and D, with APEC belonging mainly to group B2 and D [19, 20]. Various serotypes of E. coli, basing on the somatic (O) antigen serogroups are known but only a limited number is significant in relation to avian colibacillosis. Previous studies carried out in some other countries indicate that the most commonly circulating APEC serogroups are O1, O2 and O78 although others do exist [8, 9, 15].
Bacterial diseases of significance in animal production systems including avian colibacillosis affect productivity, may be zoonotic and some are associated with drug resistant pathogens [10, 21]. The high occurrence of drug resistant organisms warrants search for alternative strategies, such as, use of bacteriophages, in management of bacterial infections, like colibacillosis.
Bacteriophages are naturally occurring viruses in the environment that routinely control bacterial populations [22]. The action against specific bacteria, self-replicating and self-limiting nature; makes bacteriophages attractive alternatives to antibiotics to prevent and treat bacterial diseases [23–25]. In some developed countries, phages have been approved for use and are commercially available; for example ListShield™ and EcoShield™ have been approved by the United States Food and Drug Administration (FDA) for controlling foodborne pathogens [23, 26, 27].
The APEC strains circulating on poultry farms in Uganda have neither been characterized nor the virulence genes they harbor documented. Unlike most poultry diseases, there are no vaccines for controlling colibacillosis; hence, its management depends on hygienic measures as well as use of antibacterial agents. However, antibiotic use is associated with resistance development and undesirable drug residues in the poultry products. Therefore, in this study, we aimed at establishing a stock of APEC lytic bacteriophages, for future development of cocktail products for controlling colibacillosis in order to minimize use of antimicrobial drugs in the poultry production systems in Uganda. The research also sought to characterize the prevailing APEC isolates associated with poultry colibacillosis in Uganda by determining antibiotic susceptibility, phylogenetic groups, establish presence of APEC serotypes O1, O2 and O78 as well as virulent genes harbored.
Materials and methods
Bacterial isolates
Previously archived APEC isolates from post-mortem samples of colibacillosis suspect chicken collected between 2017 and 2018 from poultry farms around Kampala district were used for the study. The isolates had been stored at the microbiology laboratory of the College of Veterinary Medicine, Animal Resources and Biosecurity, Makerere University. Identity of 56 Escherichia coli isolates was confirmed by standard bacteriological and biochemical methods.
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing was carried out by the Disk diffusion method [28], as recommended by the Clinical and Laboratory Standards Institute [29]. Twelve antibiotics, including Tetracycline 25mcg, Chloramphenicol 5mcg, Nalidixic acid 30mcg, Ampicillin 10mcg, Streptomycin 10mcg, Sulphamethoxazole/Trimethoprim 25mcg, Ciprofloxacin 5mcg, Penicillin G 10mcg, Cefixime 30mcg, Amoxicillin 30mcg, Nitrofurantoin 300mcg, and Gentamicin 30mcg (Bioanalyse®) were tested on Mueller-Hinton agar (Oxoid, UK). Growth-inhibition zones were recorded and interpreted as susceptible (S), intermediate (I), and resistant (R). An E. coli reference strain (ATCC 25922) was used for quality control of the test.
DNA extraction
Template DNA was extracted using the boiling method as described by Wang et al [30]. Briefly, bacteria DNA was prepared by suspending one colony of the isolate in 100μL of distilled water. The suspension was rapidly boiled in a water bath at 95°C for 10 minutes and then cooled to room temperature. The cool suspension was then centrifuged (Eppendorf centrifuge 5424R, Germany) for 3 minutes at 12000rpm to remove cell debris; and the supernatant stored at -20°C formed the stock from which aliquots of template DNA were obtained for use in PCR.
Detection of the virulence genes and determination of phylogroups and serogroups of APEC using PCR
Amplification of the selected E. coli virulence genes was carried out following a method described by Johnson et al [18]. The positive controls used in PCR assays were E. coli strains BEN2268, BEN2908 which were kindly provided by Dr. Catherine Schouler.
A triplex PCR was carried out following a method described by Clermont et al [31] to determine the phylogenetic groups of the APEC isolates; where four major phylogenetic groups (A, B1, B2 and D) were targeted. The E. coli K-12 (phylogroup A), STEC O111 (phylogroup B1), and O157:H7 (phylogroup D) were used as positive controls.
Serogroup identification was done using an allele-specific PCR assay with primers designed for the most common serotypes (O1, O2 and O78) as described by Wang et al [32]. The E. coli strains BEN2268 and BEN2908 were used as positive controls with nuclease free water used as the negative control. The primers and the PCR conditions used are listed in the S1–S3 Files.
Isolation of bacteriophages
Escherichia coli specific phages were isolated through enrichment, from effluent and chicken droppings that were obtained from three selected chicken houses and slaughter places around Kampala district. The phage isolation process followed the procedure described by Oliveira et al [33] with slight modifications including use of Tryptic soy broth (Condalab, Madrid, Spain) instead of Luria Bertani broth (LB). Briefly, 50g of the chicken droppings were homogenized in 50 ml of Tryptic soy broth (TSB). The effluent (50 ml) and the homogenised samples were centrifuged at 10,000 ×g for 10 min. The supernatant was filtered through a 0.45μm membrane (ADVANTEC®, USA) and 10 ml of the filtrate was added to 10 ml of double strength TSB containing 40μL of 1M Calcium chloride (CaCl2). Then 100μL of overnight E. coli ATCC 25922 broth culture was added for enrichment. Due to lack of a well characterised APEC strain, the E. coli ATCC 25922 was used as a host. The mixture was incubated at 30°C for up to 48 hours on a shaker (New Brunswick™ Innova® 40, Germany) at 120 rev/min; after which it was centrifuged at 7000 rpm (Hermle Z32K, Germany) for 5 mins at 4°C. The supernatant was then filtered through 0.45μm syringe filters and presence of phages was determined using the spot assay method.
Spot assay method
A spot assay was carried out as described by Mirzaei & Nilsson [34] with slight modifications. Briefly, the soft agar overlay was prepared by mixing 100 μL of an overnight E. coli broth culture with 5mL of TSB containing 0.7% agar maintained in the molten form in a water bath at 45°C. The agar overlay was poured on to base plates containing 20–30mL of Tryptic Soy Agar (Condalab, Madrid, Spain) with 1.5% agar and then swirled to allow uniform spread. On solidifying, 10 μL of the phage filtrate was spotted on top of the soft agar and allowed to dry. The plates were examined for lysis or plaque formation after overnight incubation at 37°C. A clear zone indicated presence of phage.
Purification of bacteriophages
Phage purification was done using the agar overlay technique as described by Oliveira et al [33], with some modifications. The method employed base plates, containing 20–30mL of Tryptic Soy Agar (TSA) with 1.5% agar and soft agar overlays composed of TSB with 0.7% agar. Ten-fold serial dilutions (100–10−9) of the above filtered phage suspensions were prepared using the phage SM buffer (0.05M Tris, 0.1M NaCl, 0.008M MgSO4, 0.01% w/v gelatin, pH 7.5). Equal volumes (100 μL) of the diluted phage and of overnight host E. coli were mixed with 5mL of soft agar overlay, spread onto TSA plates and incubated overnight at 37°C. Basing on morphologies (size and shape), different single clear plaques were selected for further purification processes by successive single plaque isolation, from the higher dilutions plates where plaques were distinct. A single clear plaque was picked from the bacteria lawn, suspended into an overnight host E. coli culture, incubated overnight at 37°C and the lysate plated as described above. After repeating the cycle three more times, lysates from single clear plaques were centrifuged at 5000 g for 5 min. The phages were recovered from the supernatant by filtering through a 0.45 μm membrane. Purified phages were stored in SM buffer at 4°C as working stock, while for long term-storage, phage stocks were stored in 1 ml aliquots at -80°C in 7% Dimethyl Sulfoxide (DMSO).
Determination of phage titres by agar overlay method
Phage concentration (titre) was determined using a method described by Carey-Smith et al [35] with some modifications. Tryptic Soy broth instead of Luria Bertani broth was used as the culture medium. Ten-fold serial dilutions (100–10−8) of the purified phages were prepared using SM buffer. Overlays (5ml) were inoculated with 100 μL of overnight host E. coli and poured on a base plate previously marked with grid lines to allow identification of each phage dilution. Once the overlay was gelled and dried, 10 μL of each phage dilution was spotted. The plates were incubated at 37°C and examined for plaques after 24 hours. Distinct plaques obtained from the lowest dilution were counted and used to calculate the phage titre. The titres were expressed as plaque forming units (PFU) per ml.
Bacteriophage host range determination
The spot assay described above was used to determine the bacteriophage activity against the 56 APEC isolates by spotting 10 μL of 1×108 PFU/ml phage suspension. Presence of clear zones indicated sensitivity of a given APEC isolate to the lytic activity of the phage. Out of the seven phages, two phages with the broadest host ranges were selected for pH and thermal stability testing.
pH and thermal stability test
pH stability and thermal stability tests were carried out for the two phages with the broadest host ranges as described by Jung et al and Yu et al [36, 37]. Briefly, the phages (108 PFU/ml) were incubated at different temperatures (20°C to 70°C) for 30 mins. This range of temperatures was selected because it encompasses both the room temperature and body temperature of chicken among other temperatures. Afterwards, the phage suspensions were immediately placed in an ice bath.
The pH stability of the phages was evaluated using SM buffer solution adjusted to the required pH using concentrated (37% v/v) hydrochloric acid (HCl) or 5M Sodium hydroxide (NaOH). The phages (108 PFU/ml) were subjected to different ranges of pH from 2 to 12 for 30 mins at 25°C and at 40°C. The two temperatures were selected to represent the room temperature and the body temperature of chicken respectively; while pH was studied because it affects phage adsorption onto the bacteria and its subsequent propagation. Afterwards, the phage suspensions were immediately diluted with the SM buffer to limit further exposure. After both the heat and pH treatment, viable phages were quantified using the agar overlay method as described above. All assays were performed in duplicates.
Research approval
The study was endorsed by the Higher Degrees Research Committee of the College of Veterinary Medicine, Animal Resources and Biosecurity of Makerere University.
Results
Antimicrobial susceptibility testing
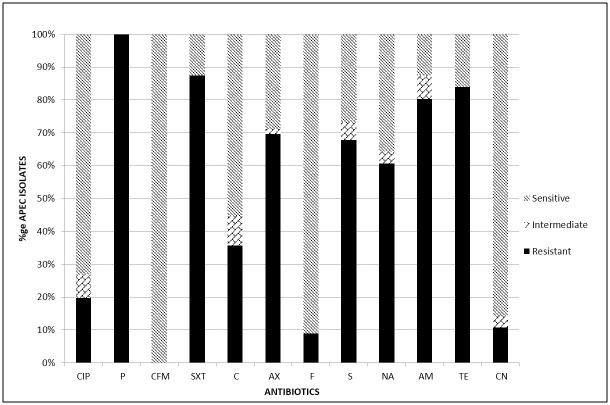
All the 56 (100%) isolates exhibited resistance to at least one antibiotic. Fig 1 presents the proportion of resistant isolates for each of the tested antibiotic. High frequency of resistance was encountered for the antibiotics: Penicillin G (100%), Sulphamethoxazole/Trimethoprim (87.5%), Tetracycline (83.9%), Ampicillin (80.4%), Amoxicillin (69.6%), Streptomycin (67.9%) and Nalidixic acid (60.7%). Average frequency of resistance was found in case of Chloramphenicol (35.7%). Low frequency of resistance was revealed in case of Gentamicin (10.7%) and Nitrofurantoin (8.9%); while all the 56 (100%) isolates were susceptible to Cefixime. Resistance to at least three antimicrobial drug classes; and hence multi-drug resistance (MDR), was encountered in 50 (89.3%) isolates.
Fig 1. Antimicrobial susceptibility test results for avian pathogenic E. coli.
The bars represent the percentages of the 56 APEC isolates that were resistant, intermediate or susceptible to the 12 antibiotics as determined by the Disk diffusion method. CIP—Ciprofloxacin, P—Penicillin G, CFM—Cefixime, SXT—Sulphamethoxazole/Trimethoprim, C—Chloramphenicol, AX—Amoxillin, F—Nitrofurantoin; S—Streptomycin, NA—Nalidixic acid, AM—Ampicillin, TE—Tetracycline, CN—Gentamicin.
Phylogenetic groups of the APEC isolates
The multiplex PCR amplification targeting the ChuA, yjaA and TspE4.C2 genes categorized the 56 APEC isolates into phylogenetic groups A, B1, B2 and D with 25 (44.6%), eight (14.3%), one (1.8%) and 22 (39.3%) isolates, respectively. Table 1 presents the genes and/or their combinations, the phylogenetic group and proportion of the E. coli isolates in each category.
Table 1. Phylogenetic groups of the APEC suspect isolates.
| ChuA | yjaA | TSPE4.C2 | Phylogroup assignment | Frequency n = 56 (100%) |
|---|---|---|---|---|
| - | +/- | - | A | 25 (44.6) |
| - | - | + | B1 | 8 (14.3) |
| + | + | +/- | B2 | 1 (1.8) |
| + | - | +/- | D | 22 (39.3) |
(+) Presence of gene; (-) Absence of gene
Frequency of APEC virulence genes
Table 2 presents the frequency of the APEC isolates harboring the selected virulence genes, that is, iroN, ompT, hlyF, iss, and iutA. Out of the 56 isolates, 39 (69.6%) had at least one virulence gene, while only 28 (50%) harboured four or more virulence genes and were thus confirmed as APEC, according to Johnson et al [18]. The virulence genes ompT and iutA had the highest prevalence at 33 (58.9%) and 32 (57.1%) respectively with iroN having the lowest prevalence at 23 (41.1%).
Table 2. Frequency of the selected virulence genes among the APEC suspect isolates.
| Gene | Description | Frequency n = 56 (100%) |
|---|---|---|
| iutA | Aerobactin siderophore receptor gene | 32 (57.1) |
| iss | Episomal increased serum survival gene | 31 (55.4) |
| hlyF | Putative avian hemolysin | 31 (55.4) |
| ompT | Episomal outer membrane protease gene | 33 (58.9) |
| iroN | Salmochelin siderophore receptor gene | 23 (41.1) |
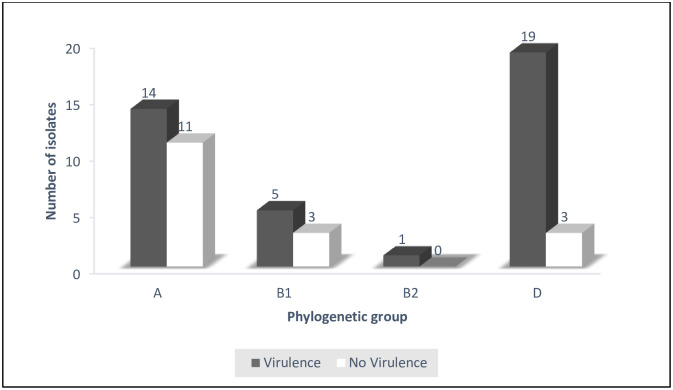
Relating presence of at least one virulence gene to the phylogroup, 14 out of 25 in group A, 5 out of 8 in group B and 19 out of 22 in group D, had virulence genes (Fig 2).
Fig 2. Virulence gene content of APEC isolates within each phylogenetic group.
The dark bars indicate the proportion of APEC isolates within a phylogenetic group that had virulence genes while the white ones indicate those without virulence genes.
Serological genotyping
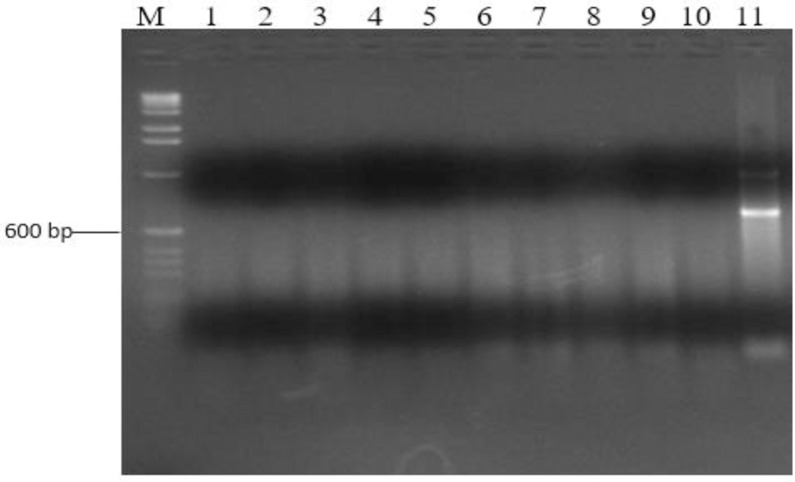
Of the 56 isolates, none generated amplicons of sizes expected for the O1, O2 and O78 serogroups (Fig 3).
Fig 3. Agarose gel showing PCR amplicons from selected APEC isolates for serogroup O78.
Lane M: DNA marker (100bp DNA ladder, ThermoFisher Scientific); Lanes 1–10: APEC isolates; Lane 11: APEC strain BEN2268 (O78 positive control).
Phage isolates and their host range
A total of 10 crude phage isolates were obtained but seven were successfully purified. The purified phages were code-named as UPEC01, UPEC03, UPEC04, UPEC06, UPEC08, UPEC09 and UPEC10. The phages produced round clear plaques with their respective host APEC isolates after overnight incubation at 37°C which confirmed them as being lytic. The phage host range, as exhibited by lytic activity against 56 APEC isolates varied from one (1.8%) to 10 (17.9%). Phage UPEC04 had the broadest host range, inhibiting 10 (17.9%) APEC isolates followed by UPEC06 and UPEC10 at 6 (10.7%) isolates each, then UPEC03 at 5 (8.9%) isolates, UPEC01 and UPEC08 at 4 (7.1%) isolates each; while UPEC09 had the narrowest host range of 1 (1.8%) isolate. Only 14 (25%) APEC isolates out of the 56 were sensitive to any one phage and the combined lytic spectrum of UPEC04 and UPEC10 phages includes all the total APEC isolates that were sensitive. Therefore, UPEC04 and UPEC10 phages were selected for further analysis. Out of the 14 APEC isolates sensitive to the phages, 11 were multi drug resistant. The phage sensitivity pattern of the seven phages on the 14 APEC isolates is presented in S1 Table.
Thermal and pH stability of UPEC04 and UPEC10 phages
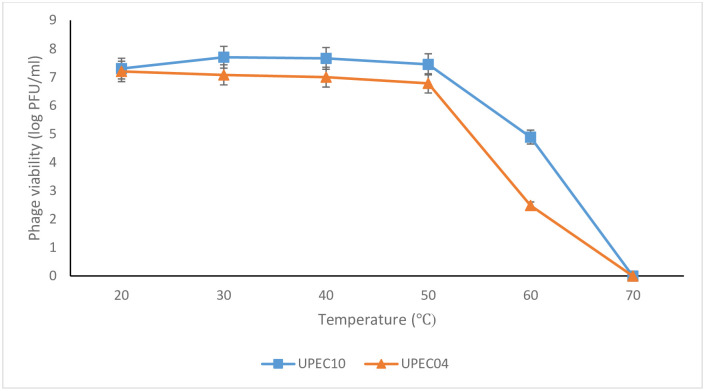
Phages UPEC04 and UPEC10 were selected for further investigation because they yielded the maximum host range of 14 out of the 56 tested APEC isolates. Therefore, the heat sensitivity of these two phages was determined for temperatures ranging from 20°C–70°C (Fig 4). The phages were stable to heat with only slight reductions in titers up to 50°C, followed by a steep decline up to 70°C; beyond which they were undetectable. The highest titers were obtained between 20°C–50°C making this the range of temperature at which the two phages are most stable.
Fig 4. Effect of temperature on UPEC04 and UPEC10 phage viability.
Phage viability was determined by obtaining the phage titers at the different temperatures using the agar overlay method. Values are an average for duplicate tests.
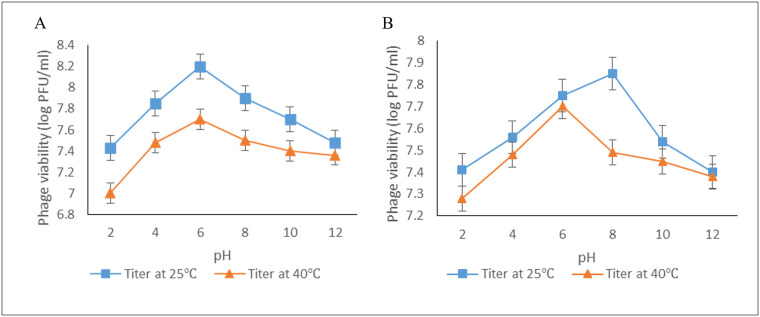
Effect of pH on phage titer
The stability of UPEC04 and UPEC10 to pH ranges from 2 to 12 at both 25°C and 40°C is presented in Fig 5. The phages retained viability across the different pH values with the lowest titers registered at the extremes of pH (2 and 12), while the highest titers were registered between pH 4 and 8. The changes in the titers followed a similar pattern at the two temperatures, though the titers were consistently higher at 25°C compared to 40°C.
Fig 5. Effect of pH on phage viability at 25°C and 40°C.
A) Phage UPEC04. B) Phage UPEC10. Phage viability was determined by obtaining the phage titers at the different pH using the agar overlay method. Values are an average for duplicate tests.
Discussion
The APEC isolates showed high resistance to commonly used antibiotics in poultry, such as tetracycline, ampicillin and sulphamethoxazole/trimethoprim. Similarly, high level resistance has been reported in E. coli from poultry and other sources [17, 38]. Indeed, phenotypic resistance of APEC exists in different regions including Africa; with varying resistance levels for each drug [13]. Occurrence of resistance is likely to be as a result of irrational drug use, especially among the poultry farmers and use of antibiotic supplemented feeds. Previously, Bashahun & Odoch reported that 96.7% of the poultry farmers in Uganda frequently used antibiotics for prevention and control of infectious diseases while 33.3% used the antibiotics to promote growth and enhance feed efficiency [39]. Resistance to antibiotics that are not commonly used in animal production systems, such as chloramphenicol, was unexpected but the ease of access to human drugs over the counter in pharmacies without a valid prescription results in their misuse in animals [40]. The latter is likely to be the explanation for the average frequency of resistance that was encountered in case of Chloramphenicol (35.7%). Low frequency of resistance was revealed in case of Gentamicin (10.7%) and Nitrofurantoin (8.9%); while all the 56 (100%) isolates were susceptible to Cefixime. Susceptibility of all the isolates to Cefixime, could be due to the fact that this is a recently introduced antibiotic, quite expensive and not readily available to the farmers. This is in agreement with a study done by Dou et al who found out that there was low resistance towards newly developed drugs [8]. A high rate of multidrug resistance has also been reported elsewhere [8, 10, 41]. The high level of antimicrobial resistance of APEC demonstrated in this study calls for stringent regulations on antibiotic use on poultry farms. Additionally, due to the challenges of developing new antibiotics, the high resistance rates reiterates the need to introduce alternatives to drug use, such as the bio-control agents, like the bacteriophages.
Phylogenetic typing determines the genetic background or ancestry of an organism as well as differentiating between the pathogenic E. coli strains (B2 and D) from commensals (A and B1) [42, 43]. Overall, phylogenetic analysis of APEC strains in this study revealed that majority belonged to Phylogenetic groups A and D. This is in agreement with several studies done elsewhere [30, 38, 44, 45]. Johnson et al found out that majority of the APEC isolates characterized belonged to A, B1 and D phylogenetic groups [18]. The 11 isolates from group A and the three isolates from group B1 that lacked the virulence genes but were isolated from colibacillosis suspect birds probably harbored other virulence genes that were not tested for during the current study or they were just opportunistic. This is in agreement with Picard et al who found out that some strains of E. coli belonging to Phylogenetic groups A and B1 exhibiting commensal characteristics would cause disease [20]. Alternatively, the 14 and five isolates from group A and B1, respectively; that possessed virulence genes could have acquired them by horizontal gene transfer from the pathogenic strains [8, 46]. The three isolates from phylogroup D that lacked the tested virulence genes probably caused colibacillosis by possessing other virulence genes not screened for in this study. The above findings agree with other studies that demonstrated diversity of Phylogenetic groups among APEC [47, 48].
The selected virulence genes occurred in 69.6% of the E. coli isolates with varying frequencies; indicating that they were potentially pathogenic. However, only 50% of the isolates that had four or more genes can be categorized as APEC according to Johnson et al [18]. The findings are supported by Kuhnert et al who concluded that pathogenicity of a given E. coli strain is mainly determined by specific virulence factors which include adhesins, invasins, toxins and capsule [49]. Seventeen isolates (30.4%) did not exhibit a single virulence gene. These isolates could have been commensals that had become opportunistic due to predisposing factors like concurrent infections, environmental stress, poor nutrition and hygiene [20, 47, 50]. Alternatively, these isolates could be harboring other virulence genes that were not screened for in the present study [18, 41]. Several studies show that it is rare for all the virulence genes to be present in the same isolate [8, 30, 51]. For instance, Delicato et al reported that 27.5% of the colibacillosis-derived isolates did not possess any of the virulence-associated genes that they investigated [52].
The Episomal outer membrane protease gene (ompT) showed the highest prevalence at 58.9%. This gene encodes a protease that cleaves colicin, an inhibitory protein produced by other E. coli [53]. The ompT gene is located on the ColV plasmid alongside other virulence genes like iss, hlyF and iroN [54]. A relatively high number of isolates harbor the ompT gene for protection against colicin produced by other E. coli.
The lowest frequency was shown by Salmochelin siderophore receptor gene (iroN) at 41.1%. Like the ompT gene, iroN is located on the ColV plasmid and is one of the genes responsible for iron acquisition [53, 54]. Presence of virulence genes distinguishes APEC from commensals and as a result these can be used as molecular markers for detection of colibacillosis in combination with other diagnostic tools [55]. However, this study did not determine whether the various APEC isolates are capable of establishing an infection in order to confirm their pathogenicity.
Out of the 56 APEC isolates, none belonged to the serogroups O1, O2 and O78 which were reported to be the most common elsewhere [9]. This means that the above serogroups are not common among APEC infecting chicken around Kampala. This can be explained by the fact that distribution of serogroups varies from one region to another and that the APEC serogroups O1, O2 and O78 may not be as common as indicated in other countries like China [8, 30]. Indeed, Riaz et al reported occurrence of serogroups O1 and O2 but not O78 [56]. Ewers et al also demonstrated that colibacillosis can be associated with serogroups other than O1, O2 and O78 [46]. Over 100 APEC serogroups have been reported and most of the previous research was carried out in Europe, Asia and some in Brazil, which are geographically distant from Uganda [8, 9, 30]. The difference in the prevalent serogroups is not unexpected and infers that vaccines against avian colibacillosis developed elsewhere may not offer protection to chicken in Uganda.
From the findings regarding host range, no single phage was able to lyse all the studied APEC strains. The maximum number that could be lysed was 14 out of 56 (25%). This is because phages are highly specific towards their hosts [57]. This is in agreement with other studies that demonstrated that phages usually have a limited host range [35, 58]. Apart from situations of compassionate use where a single bacterial strain associated with an infection is targeted, having a relatively broad host range is one of the desirable properties for selection of candidates for phage therapy [59, 60]. The two phages, UPEC04 and UPEC10, which had a combined lytic activity against 14 APEC isolates, are better candidates for formulation of cocktails for therapeutic intervention compared to the others. However, there is need to obtain more phages with a wider host range by using either a mix of multiple host strains of the same species for phage isolation or growth on multiple hosts sequentially, that is, one host at a time [59]. Lysis of the eleven multi-drug resistant APEC isolates by the phages demonstrates the potential of phages in controlling infections caused by multi drug resistant bacteria. Transmission electron microscopy (TEM) of the phage isolates allows morphological and particle stability assessment [61]. Unfortunately, this was beyond the scope of the current study due to resource limitations. However, in-depth characterization using other properties, such as whole genome sequencing and TEM will form the next steps before products for farm applications are availed.
The main physical factors affecting phage adsorption and growth include pH and temperature [62]. The different pH and temperature ranges in this study were selected to mimic those that would be encountered during the handling and application of these phages as therapeutic or sanitizing bio-control agents on poultry farms. Both UPEC04 and UPEC10 were stable to heat up to 60°C. At 70°C, the phages were inactivated which is in agreement with Lu et al (2003) and Shende et al (2017) who reported that phages get inactivated at 70°C and above [58, 62].
The effect of pH on phage viability at 25°C and at 40°C represented activity at room temperature and body temperature of chicken, respectively. The two phages were tolerant to a broad range of pH similar to what was observed in previous studies [36]. The tolerance to a broad range of temperature and pH coupled with a wide host range, makes the two phages suitable potential candidates for a cocktail product that can be used as an alternative to antibiotics in the control of APEC infections [37].
Conclusion
Over 80% of the APEC isolates exhibited multi drug resistance against the most commonly used antimicrobials. The E. coli isolates belonged to various phylogenetic groups, with the majority belonging to phylogroup A and the minority to phylogroup B2; however, none of the APEC isolates analysed belonged to the most common serotypes O1, O2 and O78 that are reported to be the most frequent elsewhere. The five selected virulence genes occurred at varying frequencies but 69.6% of the APEC isolates harboured at least one gene. Of the seven phages that were isolated, two had the highest combined host range of 25% and exhibited lytic activity under a wide range of temperatures and pH, making them potential candidates for a therapeutic cocktail product development.
Supporting information
The grid lines indicate the different dilutions of the phage suspension. Plaque assay was carried out by the spot assay method.
(TIF)
Sensitivity patterns of the seven phages on the 14 APEC isolates.
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
Dr. Wilfred Eneku for availing the post mortem tissues from poultry colibacillosis cases for E. coli isolation; Dr. Catherine Schouler of the Institut National de la Recherche Agronomique (INRA), France for providing the positive controls used in this study and the poultry farmers where samples for phage isolation were obtained; are greatly acknowledged.
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
The research was financed under the Competitive Small Grants of the Makerere-Sweden Bilateral Research Program Call 2018. The funders had no role in the study design, data collection and analysis; decision to publish or preparation of the manuscript.
References
- 1.Dziva F, Stevens MP. Colibacillosis in poultry: unravelling the molecular basis of virulence of avian pathogenic Escherichia coli in their natural hosts. Avian Pathol. 2008;37: 355–366. 10.1080/03079450802216652 [DOI] [PubMed] [Google Scholar]
- 2.Matin MA, Islam MA, Khatun MM. Prevalence of colibacillosis in chickens in greater Mymensingh district of Bangladesh. Vet World. 2017;10: 29–33. 10.14202/vetworld.2017.29-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stacy AK, Mitchell NM, Maddux JT, De La Cruz MA, Durán L, Girón JA, et al. Evaluation of the prevalence and production of Escherichia coli common pilus among avian pathogenic E. coli and its role in virulence. PLoS One. 2014;9 10.1371/journal.pone.0086565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Landman WJM, van Eck JHH. The incidence and economic impact of the Escherichia coli peritonitis syndrome in Dutch poultry farming. Avian Pathol. 2015;44: 370–378. 10.1080/03079457.2015.1060584 [DOI] [PubMed] [Google Scholar]
- 5.Ma R. General Overview of Escherichia coli Infections in Animals in Nigeria. Epidemiol Open Access. 2014;04 10.4172/2161-1165.1000153 [DOI] [Google Scholar]
- 6.Byaruhanga J, Tayebwa DS, Eneku W, Afayoa M, Mutebi F, Ndyanabo S, et al. Retrospective study on cattle and poultry diseases in Uganda. Int J Vet Sci Med. 2017;5: 168–174. 10.1016/j.ijvsm.2017.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Panth Y. Colibacillosis in poultry: A review. J Agric Nat Resour. 2019;2: 301–311. 10.3126/janr.v2i1.26094 [DOI] [Google Scholar]
- 8.Dou X, Gong J, Han X, Xu M, Shen H, Zhang D, et al. Characterization of avian pathogenic Escherichia coli isolated in eastern China. Gene. 2015;576: 244–248. 10.1016/j.gene.2015.10.012 [DOI] [PubMed] [Google Scholar]
- 9.Paixão AC, Ferreira AC, Fontes M, Themudo P, Albuquerque T, Soares MC, et al. Detection of virulence-associated genes in pathogenic and commensal avian Escherichia coli isolates. Poult Sci. 2016;95: 1646–1652. 10.3382/ps/pew087 [DOI] [PubMed] [Google Scholar]
- 10.Subedi M, Luitel H, Devkota B, Bhattarai RK, Phuyal S, Panthi P, et al. Antibiotic resistance pattern and virulence genes content in avian pathogenic Escherichia coli (APEC) from broiler chickens in Chitwan, Nepal. BMC Vet Res. 2018;14: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abalaka S, Sani N, Idoko I, Tenuche O, Oyelowo F, Ejeh S, et al. Pathological changes associated with an outbreak of colibacillosis in a commercial broiler flock. Sokoto J Vet Sci. 2017;15: 95–102. 10.4314/sokjvs.v15i3.14 [DOI] [Google Scholar]
- 12.Kabir LSM. Avian colibacillosis and salmonellosis: A closer look at epidemiology, pathogenesis, diagnosis, control and public health concerns. Int J Environ Res Public Health. 2010;7: 89–114. 10.3390/ijerph7010089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nhung NT, Chansiripornchai N, Carrique-Mas JJ. Antimicrobial resistance in bacterial poultry pathogens: A review. Front Vet Sci. 2017;4: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thapa DB, Chapagain A. Antibiogram of Escherichia coli Isolated from Avian Colibacillosis in Chitwan District of Nepal. Int J Appl Sci Biotechnol. 2020;8: 52–60. 10.3126/ijasbt.v8i1.28254 [DOI] [Google Scholar]
- 15.Halfaoui Z, Menoueri NM, Bendali LM. Serogrouping and antibiotic resistance of Escherichia coli isolated from broiler chicken with colibacillosis in center of Algeria. Vet World. 2017;10: 830–835. 10.14202/vetworld.2017.830-835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olarinmoye AO, Oladele OO, Adediji AA, Ntiwunka UG, Tayo GO. Antibiograms of avian pathogenic Escherichia coli isolates from commercial layers with colibacillosis in Southwest Nigeria. Malays J Microbiol. 2013;9: 317–325. [Google Scholar]
- 17.Majalija S, Oweka F, Wito GS, Musisi L, Vudriko P, Nakamya F. Antibiotic Susceptibility Profiles of Fecal Escherichia coli Isolates from Dip-Litter Broiler Chickens in Northern and central Uganda. Vet Res. 2010;3: 75–80. [Google Scholar]
- 18.Johnson TJ, Wannemuehler Y, Doetkott C, Johnson SJ, Rosenberger SC, Nolan LK. Identification of minimal predictors of avian pathogenic Escherichia coli virulence for use as a rapid diagnostic tool. J Clin Microbiol. 2008;46: 3987–3996. 10.1128/JCM.00816-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson JR, Stell AL. Extended virulence genotypes of Escherichia coli strains from patients with urosepsis in relation to phylogeny and host compromise. J Infect Dis. 2000;181: 261–272. 10.1086/315217 [DOI] [PubMed] [Google Scholar]
- 20.Picard B, Garcia S, Gouriou S, Duriez P, Brahimi N, Bingen E, et al. The Link between Phylogeny and Virulence in Escherichia coli Extraintestinal Infection †. Infect Immun. 1999;67: 546–553. 10.1128/IAI.67.2.546-553.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Knobl T, Moreno AM, Paixao R, Gomes TA, Vieira M, Leite S, et al. Prevalence of Avian Pathogenic Escherichia coli (APEC) Clone Harboring sfa Gene in Brazil. Sci world J. 2012;2012: 10–13. 10.1100/2012/437342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abedon ST. Kinetics of Phage-Mediated Biocontrol of Bacteria. Foodborne Pathog Dis. 2009;6 10.1089/fpd.2008.0242 [DOI] [PubMed] [Google Scholar]
- 23.Doffkay Z, Dömötör D, Kovács T, Rákhely G. Bacteriophage therapy against plant, animal and human pathogens. Acta Biol Szeged. 2015;59: 291–302. [Google Scholar]
- 24.Gill JJ. Phage applications in animal agriculture and food safety. J Anim Sci. 2016;94: 57–58. [Google Scholar]
- 25.Arthur TM, Kalchayanand N, Agga GE, Wheeler TL, Koohmaraie M. Evaluation of Bacteriophage Application to Cattle in Lairage at Beef Processing Plants to Reduce Escherichia coli. Foodborne Pathog Dis. 2016;20: 1–6. 10.1089/fpd.2016.2189 [DOI] [PubMed] [Google Scholar]
- 26.Miller RW, Skinner EJ, Sulakvelidze A, Mathis GF, Hofacre CL. Bacteriophage therapy for control of necrotic enteritis of broiler chickens experimentally infected with Clostridium perfringens. Avian Dis. 2010;54: 33–40. 10.1637/8953-060509-Reg.1 [DOI] [PubMed] [Google Scholar]
- 27.Wernicki A, Nowaczek A, Urban-chmiel R. Bacteriophage therapy to combat bacterial infections in poultry. Virol J. 2017;14: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hudzicki J. Kirby-Bauer Disk Diffusion Susceptibility Test Protocol. Am Soc Microbiol. 2016; 1–23. [Google Scholar]
- 29.CLSI. M100-S11, Performance standards for antimicrobial susceptibility testing Clin Microbiol Newsl. 26th ed 2001;23: 49 10.1016/s0196-4399(01)88009-0 [DOI] [Google Scholar]
- 30.Wang, Liao X, Zhang W, Jiang H, Sun J, Zhang M. Prevalence of Serogroups, Virulence Genotypes, Antimicrobial Resistance, and Phylogenetic Background of Avian Pathogenic Escherichia coli in South of China. Foodborne Pathog Dis. 2010;7: 1099–1106. 10.1089/fpd.2010.0542 [DOI] [PubMed] [Google Scholar]
- 31.Clermont O, Bonacorsi S, Bingen E. Rapid and Simple Determination of the Escherichia coli Phylogenetic Group. Appl Environ Microbiol. 2000;66: 4555–4558. 10.1128/aem.66.10.4555-4558.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang S, Meng Q, Dai J, Han X, Han Y, Ding C, et al. Development of an allele-specific PCR assay for simultaneous sero-typing of avian pathogenic Escherichia coli predominant O1, O2, O18 and O78 strains. PLoS One. 2014;9: 1–6. 10.1371/journal.pone.0096904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oliveira A, Sillankorva S, Quinta R, Henriques A, Sereno R, Azeredo J. Isolation and characterization of bacteriophages for avian pathogenic E. coli strains. J Appl Microbiol. 2009;106: 1919–1927. 10.1111/j.1365-2672.2009.04145.x [DOI] [PubMed] [Google Scholar]
- 34.Mirzaei MK, Nilsson AS. Isolation of phages for phage therapy: A comparison of spot tests and efficiency of plating analyses for determination of host range and efficacy. PLoS One. 2015;10: 1–13. 10.1371/journal.pone.0127606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carey-Smith G V., Billington C, Cornelius AJ, Hudson JA, Heinemann JA. Isolation and characterization of bacteriophages infecting Salmonella spp. FEMS Microbiol Lett. 2006;258: 182–186. 10.1111/j.1574-6968.2006.00217.x [DOI] [PubMed] [Google Scholar]
- 36.seung Jung L, Ding T, Ahn J. Evaluation of lytic bacteriophages for control of multidrug-resistant Salmonella typhimurium. Ann Clin Microbiol Antimicrob. 2017;16: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu YP, Gong T, Jost G, Liu WH, Ye DZ, Luo ZH. Isolation and characterization of five lytic bacteriophages infecting a Vibrio strain closely related to Vibrio owensii. FEMS Microbiol Lett. 2013;348: 112–119. 10.1111/1574-6968.12277 [DOI] [PubMed] [Google Scholar]
- 38.Kabiswa W, Nanteza A, Tumwine G, Majalija S. Phylogenetic Groups and Antimicrobial Susceptibility Patterns of Escherichia coli from Healthy Chicken in Eastern and Central Uganda. J Vet Med. 2018;2018: 1–6. 10.1155/2018/9126467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bashahun D, Odoch T. Assessment of antibiotic usage in intensive poultry farms in Wakiso District, Uganda. Livest Res Rural Dev. 2015;27. [Google Scholar]
- 40.Mukonzo JK, Namuwenge PM, Okure G, Mwesige B, Namusisi OK, Mukanga D. Over-the-counter suboptimal dispensing of antibiotics in Uganda. J Multidiscip Healthc. 2013;6: 303–310. 10.2147/JMDH.S49075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Solà-Ginés M, Cameron-Veas K, Badiola I, Dolz R, Majó N, Dahbi G, et al. Diversity of multi-drug resistant avian pathogenic Escherichia coli (APEC) Causing outbreaks of colibacillosis in broilers during 2012 in Spain. PLoS One. 2015;10: 1–14. 10.1371/journal.pone.0143191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Asadi A, Salehi TZ, Jamshidian M, Ghanbarpour R. ECOR phylotyping and determination of virulence genes in Escherichia coli isolates from pathological conditions of broiler chickens in poultry slaughter- houses of southeast of Iran. Vet Res Forum. 2018;9: 211–216. 10.30466/vrf.2018.30827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coura FM, Diniz SA, Silva MX, Arcebismo TLM, Minharro S, Feitosa ACF, et al. Phylogenetic Group of Escherichia coli Isolates from Broilers in Brazilian Poultry Slaughterhouse. Sci World J. 2017;2017 10.1155/2017/5898701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dissanayake DRA, Wijewardana TG, Gunawardena GA, Poxton IR. Distribution of lipopolysaccharide core types among avian pathogenic Escherichia coli in relation to the major phylogenetic groups. Vet Microbiol. 2008;132: 355–363. 10.1016/j.vetmic.2008.05.024 [DOI] [PubMed] [Google Scholar]
- 45.Kariyawasam S, Scaccianoce JA, Nolan LK. Common and specific genomic sequences of avian and human extraintestinal pathogenic Escherichia coli as determined by genomic subtractive hybridization. BMC Microbiol. 2007;7: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ewers C, Janßen T, Kießling S, Philipp HC, Wieler LH. Molecular epidemiology of avian pathogenic Escherichia coli (APEC) isolated from colisepticemia in poultry. Vet Microbiol. 2004;104: 91–101. 10.1016/j.vetmic.2004.09.008 [DOI] [PubMed] [Google Scholar]
- 47.Collingwood C, Kemmett K, Williams N, Wigley P. Is the concept of avian pathogenic Escherichia coli as a single pathotype fundamentally flawed? Front Vet Sci. 2014;1: 1–4. 10.3389/fvets.2014.00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kemmett K, Humphrey T, Rushton S, Close A, Wigley P, Williams NJ. A Longitudinal Study Simultaneously Exploring the Carriage of APEC Virulence Associated Genes and the Molecular Epidemiology of Faecal and Systemic E. coli in Commercial Broiler Chickens. PLoS One. 2013;8 10.1371/journal.pone.0067749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kuhnert P, Boerlin P, Frey J. Target genes for virulence assessment of Escherichia coli isolates from water, food and the environment. FEMS Microbiology Reviews. 2000. pp. 107–117. 10.1111/j.1574-6976.2000.tb00535.x [DOI] [PubMed] [Google Scholar]
- 50.Azeem T, Abid SA, Ahmad W, Aslam A, Sohail ML. Host immune responses and vaccination against avian pathogenic Escherichia coli. World’s Poult Sci. 2017;73: 29–44. 10.1017/S0043933916000866 [DOI] [Google Scholar]
- 51.Mbanga J, Nyararai YO. Virulence gene profiles of avian pathogenic Escherichia coli isolated from chickens with colibacillosis in Bulawayo, Zimbabwe. Onderstepoort J Vet Res. 2015;82: 1–8. 10.4102/ojvr.v82i1.850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Delicato ER, Guimarães B, Brito D, Carlos L, Gaziri J, Vidotto MC. Virulence-associated genes in Escherichia coli isolates from poultry with colibacillosis. Vet Microbiol. 2003;94: 97–103. 10.1016/s0378-1135(03)00076-2 [DOI] [PubMed] [Google Scholar]
- 53.Barnes HJ, Nolan LK, Vaillancourt J-P. Colibacillosis 12th ed In: Saif YM, Fadly AM, Glisson JR, McDougald LR, Nolan LK, Swayne DE, editors. Diseases of Poultry. 12th ed. Blackwell Publishing; 2008. pp. 691–732. [Google Scholar]
- 54.Johnson Siek KE, Johnson SJ Nolan LK, Acteriol JB. DNA Sequence of a ColV Plasmid and Prevalence of Selected Plasmid-Encoded Virulence Genes among Avian Escherichia coli Strains. J Bacteriol. 2006;188: 745–758.: 10.1128/JB.188.2.745-758.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rodriguez-Siek KE, Giddings C, Doetkott C, Johnson TJ, Nolan LK. Characterizing the APEC pathotype. Vet Res. 2004;35: 467–483. [DOI] [PubMed] [Google Scholar]
- 56.Riaz MA, Aslam A, Rehman M, Yaqub T. Pathological Investigation and Molecular Detection of Avian Pathogenic E. coli Serogroups in Broiler Birds. J Vet Sci Technol. 2016;7: 5–9. 10.4172/2157-7579.1000373 [DOI] [Google Scholar]
- 57.Naghizadeh M, Amir M, Torshizi K, Rahimi S, Dalgaard TS. Synergistic effect of phage therapy using a cocktail rather than a single phage in the control of severe colibacillosis in quails. Poult Sci. 2018;0: 1–11. [DOI] [PubMed] [Google Scholar]
- 58.Lu Z, Breidt F, Fleming HP, Altermann E, Klaenhammer TR. Isolation and characterization of a Lactobacillus plantarum bacteriophage, ΦJL-1, from a cucumber fermentation. Int J Food Microbiol. 2003;84: 225–235. [DOI] [PubMed] [Google Scholar]
- 59.Hyman P. Phages for Phage Therapy: Isolation, Characterization, and Host Range Breadth. Pharmaceuticals. 2019;12 10.3390/ph12010035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Patey O, McCallin S, Mazure H, Liddle M, Smithyman A, Dublanchet A. Clinical indications and compassionate use of phage therapy: Personal experience and literature review with a focus on osteoarticular infections. Viruses. 2019;11: 1–21. 10.3390/v11010018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Casey E, van Sinderen D, Mahony J. In vitro characteristics of phages to guide ‘real life’ phage therapy suitability. Viruses. 2018;10 10.3390/v10040163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shende RK, Hirpurkar SD, Sannat C, Rawat N, Pandey V. Isolation and characterization of bacteriophages with lytic activity against common bacterial pathogens. Vet World. 2017;10: 973–978. 10.14202/vetworld.2017.973-978 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The grid lines indicate the different dilutions of the phage suspension. Plaque assay was carried out by the spot assay method.
(TIF)
Sensitivity patterns of the seven phages on the 14 APEC isolates.
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting information files.