Abstract
The transmission of tuberculosis has been declared as an important occupational hazard for health care workers of tuberculosis dispensary. Here, we evaluated the filtration efficiency and respiratory resistance of different respirators along with the increase of wear time.
Filter efficiency and breathing resistance were tested to determine the performance of different types of respirators, and the N95 respirator were simulatively worn by volunteers to determine the optimal time for N95 respirator as a tuberculosis control measure.
N95 respirator had the highest filtration efficiency (97.4% ± 0.3%), whereas the surgical mask could only prevent 18.4% of aerosol particles to penetrate inside the respirator. In addition, N95 respirator and surgical mask had the highest and lowest exhalation resistance (13.8 ± 0.9 mmH2O vs. 1.8 ± 0.2 mmH2O), respectively. When the volunteers wore the N95 respirator for 3 days, the average filtration efficiency was 97.0%. In addition, there were no significant differences in the exhalation resistance of N95 respirator, ranging from 13.8 ± 0.9 mmH2O of 0 day to 11.6 ± 0.9 mmH2O of 14 days.
Our results demonstrate that only N95 respirator provides promising protective efficiency for health care workers against tuberculosis. In addition, N95 respirator could produce adequate protective efficacy after 3-day wear time.
Keywords: N95 respirator, optimal time, tuberculosis
1. Introduction
The transmission of Mycobacterium tuberculosis from individuals with tuberculosis to other individuals has been reported for many years.[1,2] Particularly, this risk of transmission is greater for the health care workers of tuberculosis dispensary, which has been declared as an important occupational hazard.[3] According to the estimation from the previous studies, 1% to 10% of health care workers may be infected annually in hospitals with more than 200 admissions per year for tuberculosis.[4] The World Health Organization has issued several guidelines to prevent the transmission of tuberculosis in health care workers.[5] Among these control measures, personal respiratory protection through the use of respirators is endorsed as the most effective individual measure.[4] Several types of protective measures, including surgical mask, 12-layer cotton mask, 24-layer cotton mask and N95 respirator, have been widely in healthcare settings, but only respirators can be used for respiratory protection against airborne chemical hazards. The surgical mask is effective to block large-particle droplets, whereas it fails to protect the wearer from “inhaling airborne contaminants.[6–8] As a consequence, the N95 respirators are endorsed by World Health Organization to reduce the nosocomial infection of M. tuberculosis for persons in settings with a high risk of transmission.[5]
China has the third highest tuberculosis burden globally, behind only India and Indonesia.[9] In a recent cross-sectional study from China, the tuberculosis disease prevalence is 530 cases per 100,000 among the health care facilities.[10] Inadequate tuberculosis infection control in China may contribute to the high prevalence of tuberculosis among this special population. In 2009, a guideline from China's Ministry of Health has recommended the use of a respirator, cap and gloves by the health care workers for specific tuberculosis infection control measures. Unfortunately, no specific standards, including the respirator types and the usage time, are not clearly defined till now. In this study, we evaluated the filtration efficiency and respiratory resistance of different respirators along with the increase of wear time. Our aim was to establish a cost-effective guideline for usage of personal respirator in China.
2. Material and methods
2.1. Masks
A total of 4 different personal masks were enrolled in this study, including surgical mask (Sinovo, Beijing, China), 12-layer cotton mask (Tianhong, Xinxiang, China), 24-layer cotton mask (Tianhong, Xinxiang, China), and N95 respirator (Sinovo, Beijing, China). All these masks were widely used as infection control measures in tuberculosis specialized hospitals of China.
2.2. Test for filtration efficiency and breathing resistance
Automated Filter Tester 8130 (Thermo-Systems Engineering Incorporated Model 8130, Thermo-Systems Engineering Incorporated, the United States) was utilized to generate NaCl aerosol with median particle diameter of 0.075 ± 0.020 μm. The NaCl aerosol flow went through the N95 respirator with a speed of 85 L/s and a concentration not exceeding 200 mg/m3. Filter efficiency and breathing resistance were tested according to the method recommended by the National Institute for Occupational Safety and Health,[11] which were represented by ratio of particles filtered by the respirator (%) and millimeter of water column(mmH2O), respectively.[12]
2.3. Simulated wearing N95 respirator
In order to mimic a common work condition of tuberculosis health care workers, the volunteers wore the respirators for 4 hours in the morning and 4 hours in the afternoon per day, and interrupted by a 2-hour lunch break. During the lunch break and in the evening, the respirators were put into envelope with air vents and hung at a ventilated place. To determine the optimal time for N95 respirator as a tuberculosis control measure, the volunteers wore the N95 respirators for 0.5 day (4 hours), 1 day (8 hours), 2 days (16 hours), 3 days (24 hours), 4 days (32 hours), 5 days (40 hours), 6 days (48 hours), 7 days (56 hours) and 14 days (112 hours), respectively. The filter efficiency and breathing resistance of the respirators were tested in 1 hour after the volunteers got off the respirators. All the experiments had been performed in 50 times by different volunteers.
2.4. Statistical analysis
Data analysis was performed using SPSS 19.0 (SPSS Inc.). The filter efficiencies and breathing resistances of different respirators were compared using t t-test. P values of <.05 were considered as statistically significant.
2.5. Ethical statement
This study was approved by the Ethics Committee of Beijing Chest Hospital, Capital Medical University. Written informed consent was obtained from each participate enrolled in this study. All the subjects had the right to refuse or withdraw from the study at any time.
3. Results
3.1. Filtration efficiency and exhalation resistance of different respirators
These filtration efficiency data have been used to evaluate the aerosol concentrations inside the respirator for the occupational environments shown in Figure 1. Overall, the N95 respirator had the highest filtration efficiency (97.4% ± 0.3%), whereas the surgical mask could only prevent 18.4% of aerosol particles to penetrate inside the respirator, which exhibited the lowest filtration efficiency. As expected, the N95 respirator and surgical mask had the highest and lowest exhalation resistance (13.8 ± 0.9 mmH2O vs. 1.8 ± 0.2 mmH2O), respectively. Interestingly, although the exhalation resistance of 24-layer cotton mask (6.6 ± 2.1) was about twice as great as that of 12-layer cotton mask (3.9 ± 0.5), the 24-layer cotton mask (43.9% ± 3.8%) only increased the filtration efficiency by 35.9% when compared with the 12-layer cotton mask (32.3% ± 2.2%).
Figure 1.
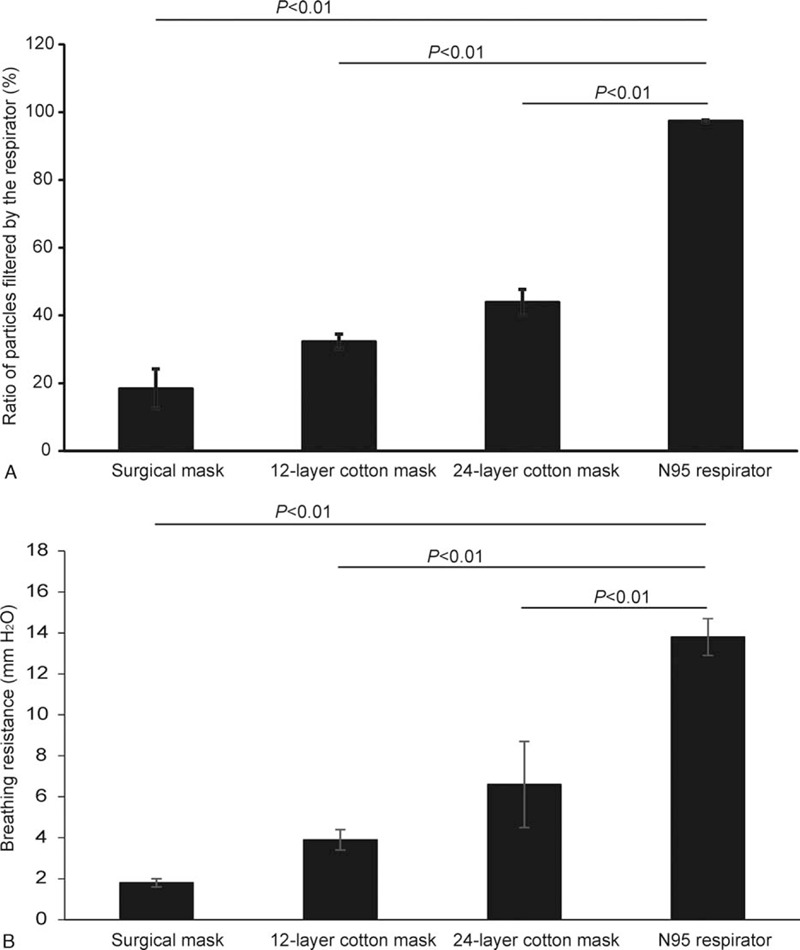
Comparison of the filtration efficiency and respiratory resistance of different respirators.
3.2. Efficiency loss of N95 respirator along with increasing wear time
We further assessed the efficiency loss of N95 respirator along with increasing wear time. As shown in Figure 2, with the expected increase in wear time, the filtration efficiency of N95 respirator was decreased gently. When the volunteers wore the N95 respirator for 3 days, the average filtration efficiency was 97.0%, which was higher than that recommended by European Certified-Filtering Facepiece Particle Respirators 2. In addition, only 19.4% of aerosol particles could penetrate the N95 respirator after 14-day wear time, exhibiting a filtration efficiency of 80.4%. Despite being decreased in filtration efficiency along with increasing wear time, there were no significant differences in the exhalation resistance of N95 respirator, ranging from 13.8 ± 0.9 mmH2O of 0 day to 11.6 ± 0.9 mmH2O of 14 days.
Figure 2.
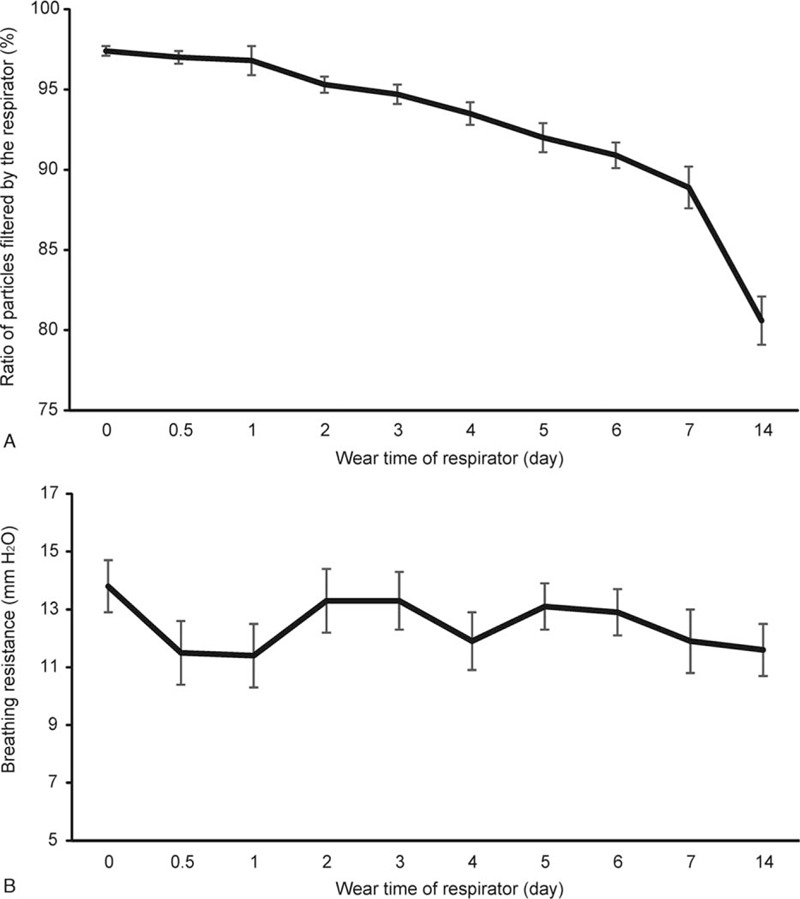
Description of the filtration efficiency and respiratory resistance of N95 respirator along with the increase of wear time.
4. Discussion
There is no doubt that tuberculosis is still an important occupational hazard for health care workers.[3] Respirator use is an efficient measure to prevent the tuberculosis infection among health care workers working.[13] In clinical practice, several different kinds of respirators are widely used in China, including surgical mask, cotton mask and N95 respirator. On the basis of our data, only N95 respirator can provide the reliable protective effectiveness against airborne transmission of tuberculosis for health care workers. Notably, the most frequently used surgical mask has unsatisfactory protection level in reducing the occupational risk of tuberculosis. In consistent to our observation, a recent study reported that surgical mask had an estimated efficacy within 1% of N95 respirator in preventing influenza.[14] The significantly different protection against tuberculosis infection between surgical mask and N95 respirator is associated with poor filtration efficiency for particles smaller than 20 μm in diameter.[14] Another interesting finding of this study was that the filtration efficiency produced by the double use of 12-lay cotton mask was not increased as great as the exhalation resistance. Our data indicate that the perfunctory increase of layers of cotton mask will not generate the expected beneficial changes against tuberculosis infection.
Although strong evidences have been reported that N95 respirator is the optimal choice in reducing the occupational risk of tuberculosis,[4] the high cost of N95 respirator is a major issue affecting the implementation of this expensive control measure, especially in the resource-limited settings. More importantly, the cost-effectiveness of this measure depends on its protective duration. In this study, our data have firstly demonstrated that N95 respirator could produce adequate protective efficacy after 3-day wear time. If the unit price of N95 is set as $1, the average daily cost of this effective measure is only $0.33. In contrast, despite having a relative low unit cost (∼$0.2), the intrinsically disposable characteristic of surgical mask may result higher daily cost if the health care workers use more than 2 surgical masks per day. In our recent study of the prevalence of tuberculosis among health care workers in tuberculosis specialized hospitals in China, health care workers from general hospitals with tuberculosis clinics had the highest prevalence ratio of tuberculosis compared with those from tuberculosis specialized hospitals, which is majorly attributed to the improper measures essential for prevention of nosocomial tuberculosis infection.[15] Given the relatively high cost-effective of N95 respirator and poor protective efficacy of other masks, the policy makers should formulate the appropriate infection control strategy based on the implementation of N95 respirator for health care workers.
There were also several obvious limitations in this study. First, the methodology used in this study was based on the modeling of NaCl aerosol particles. The authors were not trying to simulate actual modes of transmission of tuberculosis through aerosol particles. Second, only 1 N95 respirator and 1 surgical mask were evaluated in this study, and it is possible that this is not enough representativeness to fully demonstrate the variations within different N95 respirator models. Third, the hypothesized 8 hours per day were used to standardize the wear time of N95 respirator, while the work load of clinicians were not taken into consideration. Despite the above limitations, our data will provide important hints regarding the reasonable use of N95 respirator for health care workers against tuberculosis infection.
In conclusion, our results demonstrate that N95 respirator provides promising protective efficiency for health care workers against tuberculosis, whereas both cotton mask and surgical mask could only prevent the penetration of less than half of aerosol particles, which will bring the health care workers suffer from great inhalation hazard of tuberculosis infection. In addition, N95 respirator could produce adequate protective efficacy after 3-day wear time. Given the relative high cost-effective of N95 respirator, the policy makers should formulate the appropriate infection control strategy based on the implementation of N95 respirator for health care workers to prevent occupational tuberculosis transmission in hospitals.
Author contributions
Data curation: Wei Shu, Jingtao Gao.
Formal analysis: Yan Ma.
Investigation: Lijie Zhang, Wei Shu.
Methodology: Jian Du, Yan Ma.
Supervision: Yuhong Liu, Jingtao Gao.
Writing – original draft: Jian Du, Lijie Zhang, Yuhong Liu.
Writing – review & editing: Jian Du, Lijie Zhang, Yuhong Liu, liang li.
Footnotes
Abbreviations: CE = european certified, NIOSH = national institute for occupational safety and health, TSI = Thermo-Systems engineering incorporated, WHO = world health organization.
How to cite this article: Du J, Zhang L, Liu Y, Shu W, Ma Y, Gao J, Li L. Determination of the optimal time for N95 respirator for aerosol infection control. Medicine. 2020;99:50(e23709).
JD, LZ, and YL authors contributed equally to this paper.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Fennelly KP, Iseman MD. Health care workers and tuberculosis: the battle of a century. Int J Tuberc Lung Dis 1999;3:363–4. [PubMed] [Google Scholar]
- [2].Joshi R, Reingold AL, Menzies D, et al. Tuberculosis among health-care workers in low- and middle-income countries: a systematic review. Plos Medicine 2006;3:e494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Menzies D, Joshi R, Pai M. Risk of tuberculosis infection and disease associated with work in health care settings. Int J Tuberc Lung D 2007;11:593. [PubMed] [Google Scholar]
- [4].Biscotto CR, Pedroso ER, Starling CE, et al. Evaluation of N95 respirator use as a tuberculosis control measure in a resource-limited setting. Int J Tuberc Lung D 2005;9:545–9. [PubMed] [Google Scholar]
- [5].WHO guidelines on tuberculosis infection prevention and control, 2019 update. (WHO/CDS/TB/2019.1) Geneva: World Health Organization; 2019 (Available at: https://apps.who.int/iris/bitstream/handle/10665/311259/9789241550512-eng.pdf?ua=1, accessed 18 Sept. 2020). [Google Scholar]
- [6].Rengasamy SA, Miller A, Eimer BC, et al. Filtration performance of FDA-cleared surgical masks. J Int Soc Resp Prot 2009;26(I-II):54–70. [PMC free article] [PubMed] [Google Scholar]
- [7].N95 Respirators, Surgical Masks, and Face Masks. U.S. Food&Drug Administration, 2020 (Available at: https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-surgical-masks-and-face-masks#s2, accessed 18 Sept.2020). [Google Scholar]
- [8].Use of Respirators and Surgical Masks for Protection Against Healthcare Hazards. Centers for Disease Control and Prevention, 2018 (Available at: https://www.cdc.gov/niosh/topics/healthcarehsps/respiratory.html, accessed 18 Sept.2020). [Google Scholar]
- [9].Ormerod LP. Rifampicin and isoniazid prophylactic chemotherapy for tuberculosis. Arch Dis Child 1998;78:169–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Yang ZD, Wen MS, Jie WG, et al. Infection control and the burden of tuberculosis infection and disease in health care workers in china: a cross-sectional study. Bmc Infec Dis 2010;10:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Health EDo, Services H. NIOSH guide to the selection and use of particulate respirators certified under 42 CFR 84. NIOSH 1996. [Google Scholar]
- [12].Roberge RJ, Kim JH, Benson S. N95 filtering facepiece respirator deadspace temperature and humidity. J Occup Environ Hyg 2012;9:166–71. [DOI] [PubMed] [Google Scholar]
- [13].Lkp S, Yang L, Ssk H, et al. Reliability of N95 respirators for respiratory protection before, during, and after nursing procedures. Am J Infect Control 2017;45:974–8. [DOI] [PubMed] [Google Scholar]
- [14].Lee SA, Grinshpun SA, Reponen T. Respiratory performance offered by N95 respirators and surgical masks: human subject evaluation with NaCl aerosol representing bacterial and viral particle size range. Ann Occup Hyg 2008;52:177–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Du J, Pang Y, Ma Y, et al. Prevalence of tuberculosis among health care workers in tuberculosis specialized hospitals in China. J Occup Health 2017;59:292–5. [DOI] [PMC free article] [PubMed] [Google Scholar]


