Abstract
Background:
Although randomized controlled trials have revealed the considerable effectiveness of acupuncture in breast cancer patients, there have been no studies exploring current acupuncture research trends for treatment induced various symptoms in breast cancer patients. This review evaluated the effectiveness of acupuncture for treatment-induced symptoms in breast cancer patients.
Methods:
We performed a systematic review and meta-analysis of the literature regarding acupuncture to treat symptoms associated with breast cancer therapies. The following databases were searched for relevant RCTs published before June 2018: MEDLINE, EMBASE, the Cochrane Library, AMED, CINAHL, OASIS, CNKI, and CiNii.
Results:
Among the 19,483 records identified, 835 articles remained after screening titles and abstracts. A total of 19 RCTs were included in this qualitative synthesis. Among the studies, 8 explored climacteric symptoms, 4 explored pain, 2 explored lymphedemas, 2 explored nausea and vomiting and 3 investigated miscellaneous symptoms.
explored miscellaneous symptoms due to cancer treatments. Most of the studies reported that acupuncture can alleviate various symptoms of breast cancer treatment. However, there is a lack of evidence as to whether accupuncture can alleviate chemotherapy associated side effects
Conclusions:
Acupuncture may alleviate the treatment-related symptoms of breast cancer; however, further studies are necessary to obtain conclusive evidence of the effectiveness of acupuncture in treating breast cancer.
Registration number:
CRD42018087813
Keywords: acupuncture, complementary and alternative medicine, electro-acupuncture, Korean medicine
1. Introduction
Breast cancer (BC) is the most common type of cancer among women globally. The estimated incidence and the age-standardized incidence rate for female BC patients was 2.4 million and 65.5 per 100,000 women in 2015.[1,2] The increasing incidence of BC may have an impact on the economic burden of care and productivity of patients.
In general, BC patients experience multiple symptoms related to cancer treatment, including fatigue, pain, sleep disturbances, depression, nausea, and vomiting.[3] Dong et al reported that these symptoms are often concurrent, with more than 8 symptoms occurring at any given time.[4] Several studies have used non-pharmacological approaches to treat these symptoms, such as pain, fatigue, sleep disturbance, and quality of life, in a safe and effective manner.[5–8]
A substantial number of BC patients visit complementary and alternative medicine (CAM) clinics to receive treatment for cancer as well as for treatment-related symptoms, such as psychosocial distress, hot flushes, insomnia, and fatigue.[9–11] Currently, acupuncture is widely used as a safe and highly accessible adjunctive treatment for various symptoms induced by BC treatment.[12] Based on the principles of traditional medicine, acupuncture regulates energy pathways and controls the balance of energy circulation to alleviate various symptoms of cancer, as evidenced by the changes in neurophysiologic and neurohormonal activities.[13]
Previous studies have explored the efficacy of a broad range of CAMs in improving the symptoms of BC treatment-related symptoms.[14–17] Kim et al. recently reviewed the current clinical evidence of acupuncture for Korean BC survivors and reported that there is a lack of evidence for the benefits of acupuncture in BC patients within Korea.[18]
There has been no thorough systematic review of various acupuncture treatments for BC treatment-induced symptoms. Thus, we reviewed all relevant studies and conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) to investigate the efficacy and safety of acupuncture in relation to the various symptoms induced by BC treatment.
2. Methods
All data of this study analyzed were collected from published trials, so ethical approval is not necessary.
2.1. Search method for identification of studies
2.1.1. Search databases
The following 8 electronic databases were used for the study: MEDLINE, EMBASE, the Cochrane Library, AMED, CINAHL, 1 Korean database (OASIS), 1 Chinese database (China National Knowledge Infrastructure, CNKI), and 1 Japanese database (CiNii). The reference lists of the retrieved articles were manually searched, and previously published review articles were also examined.
2.1.2. Search strategy
Acupuncture and BC were selected as the basic search terms for this study. The keywords used for searching the databases were ‘breast cancer’, ‘breast carcinoma’, ‘breast neoplasm’, and ‘acupuncture’. To increase the sensitivity of the search, the terms ‘traditional medicine’, ‘complementary and alternative medicine’, ‘Chinese medicine’, ‘Korean medicine’, and ‘Kampo medicine’ were also included as keywords. Language and publication dates were not restricted. Data were searched on June 20, 2018. The search strategy for PubMed is shown in Table 1.
Table 1.
Search strategies used in PubMed database.
| No | Search Items |
| 1 | breast neoplasm[MeSH Terms] |
| 2 | breast cancer |
| 3 | breast carcinoma |
| 4 | acupuncture∗[Text Word] |
| 5 | traditional medicine[Text Word] |
| 6 | complementary and alternative medicine[Text Word] |
| 7 | Korean medicine[Text Word] |
| 8 | Chinese medicine[Text Word] |
| 9 | kampo medicine[Text Word] |
| 10 | or/1–3 |
| 11 | or/5–9 |
| 12 | 4 AND 10 AND 11 |
In addition, this review has been registered on PROSPERO (registration number CRD42016049463). The protocol was strictly developed in accordance with the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses protocols (PRISMA-P).
2.2. Inclusion criteria for this review
2.2.1. Types of studies
This systematic review included only those RCTs that had been peer-reviewed. Other designs such as observational studies, cohort studies, case reports, case series, non-RCT studies, animal and experimental studies, and theses were excluded.
2.2.2. Participants
Participants were women currently being treated for BC. No restrictions were used with respect to the diagnosis criteria for BC and stage of cancer. Both metastatic and non-metastatic BC patients were included. Patients with other types of cancer were excluded.
2.2.3. Types of interventions
We included studies that evaluated the effect of various types of acupuncture in the management of treatment-related symptoms in breast cancer patients. Interventions including manual acupuncture, ear acupuncture, and electro-acupuncture (EA) were included. There were no restrictions on concomitant conventional treatment, such as chemotherapy and hormone therapy, if the study applied concomitant treatment for all groups homogeneously. Studies were excluded if they did not mention penetration of the skin during the procedure of acupuncture, which, for example, occurs with acupressure.
2.2.4. Types of comparisons
There were no special restrictions on comparisons. Sham acupuncture, active-control (such as conventional medicine and exercise), no-treatment, and wait-list control groups were all permitted.
2.2.5. Outcome measures
There were no designated primary outcomes in this review. Outcomes used for the evaluation of BC-related symptoms were accepted without restriction.
2.3. Data collection, extraction, and assessment
2.3.1. Selection of studies
Two authors (SJ and YK) independently screened the titles and abstracts of the searched studies, after excluding duplicate articles from 8 databases. Then, the full text of the selected articles was reviewed to verify that each article met the inclusion criteria. Another reviewer (BHJ) made the final decision when the earlier two authors had a difference in opinion. This process is summarized in a flow diagram in the PRISMA (Fig. 1).[19]
Figure 1.
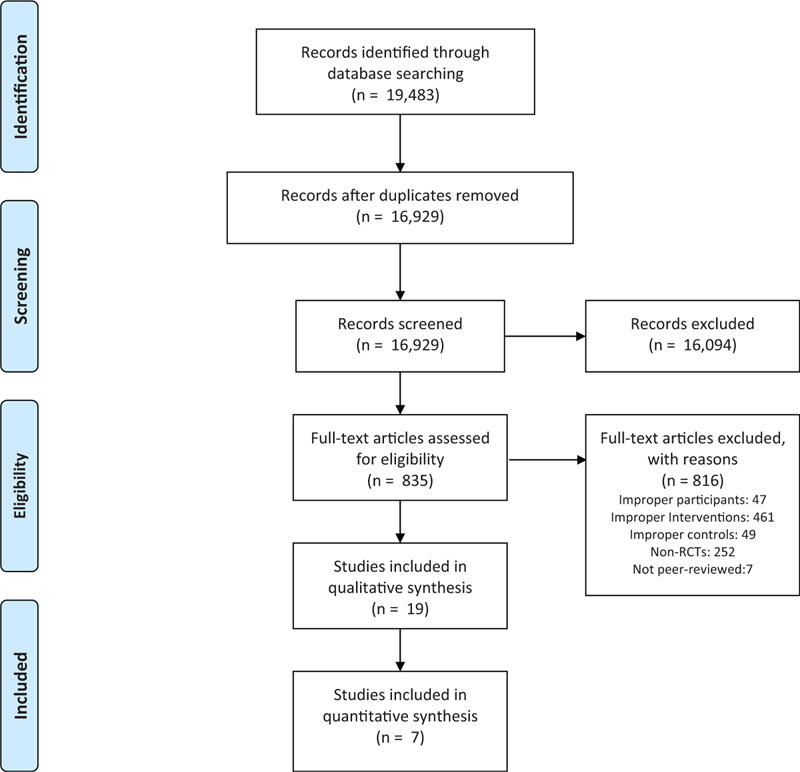
The PRISMA Flow Diagram of Study Selection.
2.3.2. Data extraction
One author (SJ) conducted data extraction, and another author (YK) reviewed the extracted document. Extracted items regarding study population, type of symptom, intervention, outcomes, and conclusion were collected from the studies.
2.3.3. Risk bias assessment
Two reviewers (SJ and YK) assessed the quality of the included studies using the Risk of Bias (RoB) tool developed by Cochrane.[20] RoB consists of the following seven items:
-
1)
random sequence generation,
-
2)
allocation concealment,
-
3)
blinding of participants and personnel,
-
4)
blinding of outcome assessment,
-
5)
completeness of outcome data,
-
6)
completeness of reporting, and
-
7)
other sources of bias.
Each item of every RCT was categorized as “high risk (H),” “unclear (U),” or “low risk (L).” The RoB graph was generated using Review Manager (Cochrane Collaboration Software, RevMan) version 5.3.
2.3.4. Meta-analysis
We planned to perform a meta-analysis if sufficient studies were identified for symptoms or outcome measurements. We used the risk ratio (RR) for dichotomous variables and mean difference (MD) for continuous variables as effect estimates.
3. Results
3.1. Results of the search
In total, 19,483 records were identified from the eight databases. Of these, 16,929 articles remained after eliminating duplicates. After screening titles and abstracts, 835 articles were retained, and finally, through reviewing the full texts, 19 RCTs[21–40] (described in 20 articles) fulfilled the eligibility criteria for inclusion. The flow chart of the study selection and exclusion criteria is shown in Figure 1. Hervik's studies were published twice, in 2009[27] and 2014.[28] Both were based on the same trial, and the 2014 article was the result of a follow-up study. Therefore, these 2 studies were examined together as 1 study in this review.
3.2. Included studies
A detailed description of the characteristics of the included studies is presented in Tables 2 and 3. The following is a brief overview of the studies.
Table 2.
Basic information of included studies.
| Characteristics of study | Interventions | ||||||||||
| Study ID | Sample size (enrolled) | Age (mean, SD) | Stage | Main symptoms | Acu-type | Control intervention | Total duration of treatment | Outcomes | Effect estimates (Mean difference after-before treatment, event (n or %)) | Adverse events | Conclusion |
| Climacteric symptoms (8) | |||||||||||
| Nedstrand (2006) Sweden (21) | 38 I:19, C:19) | 53 | n.r. | Hot flush | EA | Applied relaxation | 12 w + 3 m (F/U) | 1. Mood scale 2. SCL∗, 3. Intensity of climacteric symptom (VAS)∗ 4. KI∗ 5. Hot flush FREQ∗ | 1. -0.90 [-1.02, -0.78] 2. 5.10 [1.75, 8.45] 3. -0.10 [-0.22, 0.02] 4. 1.90 [1.63, 2.17] 5. 0.40 [-0.68, 1.48] | n.r. | “.. improved in both groups, bur did not differ significantly..” |
| Deng (2007) US (22) | 72 (I:42, C:30) | I: 55 C: 56 | n.r. | Hot flush | AT | Sham | 4 w + 5 m (F/U) | Hot flush FREQ∗ | -0.10 [-0.28, 0.08] | I: 12: slight bleeding or bruising at the needle site | “.. cannot exclude the possibility that a longer and more intense acupuncture intervention could produce a larger reduction of these symptoms.” |
| Walker (2010) US (23) | 50 (I:25, C:25) | Median 55 (35–77) | 0-III | Hot flush | AT | VNF | 12 w + 9 m (F/U) | 1. Hot flush FREQ∗ 2. Severity of Hot flush∗ 3. MenQoL (total)∗ 4. BDI-PC∗ | 1. P < .05 2. P < .001 3. P < .002 4. P < .001 | C: 18: nausea, headache, difficulty sleeping, dizziness, etc. | “.. a safe, effective and durable treatment for vasomotor symptoms secondary to long-term antiestrogen hormone use in patients with BC.” |
| Frisk (2012) Sweden (24) | 45 (I:27, C:18) | I: 54.1 C: 53.4 | T1 or T2 with max 4 MLN, T3 without metastasis | Climacteric symptoms | EA | HT | · 12 w+ 21 m (F/U) (AT) · 24 m (HT) | 1. Hot flush FREQ∗ (No of hr slept/night; Times woken up/night; No of flushes/night; Distress flushes/night) 2. HFS (Reduction rate)† 3. WHQ (Total, sleep)∗ 4. PGWB | 1. 0.60 [0.47, 0.73] -0.40 [-0.65, -0.15] -0.50 [-0.90, -0.10] -0.40 [-1.23, 0.43] 2. 80%/100% 3. 0.06 [0.04, 0.08] 0.16 [-0.88, 1.20] 4. -14.00 [-15.51,-12.49] | none | “EA should be further evaluated as treatment for women with BC and climacteric complaints, since HT no longer can be recommended for these women.” |
| Liljegren (2012) Sweden (25) | 84 (I:42, C:42) | I: 58 ± 6.8 C: 58 ± 9.3 | n.r. | Climacteric symptoms | AT | Sham | 5 w + 12 w (F/U) | 1. Hot flush FREQ∗ 2. Sweating FREQ∗ 3. FSH, LH, estradiol, progesterone, SHBG, prolactin, testosterone | 1. -0.10 [-0.60, 0.40] 2. -0.90 [-1.02, -0.78] 3. no statistical significant (data not shown | n.r. | “..shows that both true and CTRL reduce vasomotor symptoms in BC patients treated with adjuvant tamoxifen.” |
| Bao (2014) US (26) | 51 (I:25, C:26) | Median I: 61 (44–82) C: 61 (45–85) | 0-III | Aromatase Inhibitor-induced Musculo-skeletal Symptoms | AT | Sham | 8 w + 4 w (F/U) | 1. Hot flush FREQ∗ 2 Severity of Hot flush∗ 3. CES-D∗ 4. HADS 5. Euro QOL 6. PSQI∗ 7. NSABP 8. Hot Flush Related Daily Interference Scale∗ | 1. 1.50 [-4.01, 7.01] 2. -5.50 [-17.79, 6.79] 3. 1.50 [-1.30, 4.30] 4. 1.50 [0.43, 2.57] 5. -1.00 [-7.11, 5.11] 6. -0.50 [-1.34, 0.34] 7. 2.00 [-7.82, 11.82] 8. -1.00 [-12.13, 10.13] | none | “RA and SA were both associated with improvement in PROs in BC patients taking Ais and detected no significant difference between arms.” |
| Hervik (2009) (27) & Hervik (2014) Norway (28) | 59 (I:30, C:29) | I: 52 ± 8.4 C: 52 ± 9.5 | n.r. | Hot flush | AT | Sham | 10 w + 2 y (F/U) | KI∗ | -5.69 [-5.71, -5.67] | n.r. | “Acupuncture seems to have a positive effect on health related quality of life for up 3 months post-treatment, but no significant effect 2 years FU.” |
| Lesi (2016) Italy (29) | 190 (I:85, C:105) | I: 50 ± 9 C: 49 ± 8.5 | n.r. | Hot flushes | AT + Enhanced self-care based on Brochure | Enhanced self-care based on Brochure | 12 w + 6 m (F/U) | 1. HFS∗ 2. GCS 3. MenQoL (Vasomotor, Psychosocial, Physical, Sexual) | 1. -11.4[-16.4, -6.3] 2. -6.8 [-9.4, -4.2] 3. -1.6[-2.1, -1.1] -0.8[-1.3, -0.3] -0.7[-1.1, -0.3] -0.3[-0.9, 0.3] | I: 12 mild adverse events (muscle pain, headache, menstrual bleed) | “.. is an effective integrative intervention for managing hot flashes and improving QoL in women with BC.” |
| PAIN (4) | |||||||||||
| Crew (2010) US (30) | 43 (I:23, C:20) | Median I: 58 (44–77) C: 57 (37–77) | I-III | Joint pain or stiffness | AT + Auricular AT | Sham | 6 w | 1. WOMAC (pain, stiffness, function, normalized)∗ 2. M-SACRAH (pain, stiffness, function, normalized)∗ 3. BPI-SF (worst pain, pain severity, pain related interference)∗ 4. FACT-G (physical, social/family, emotional, functional) | 1. -174.00 [-212.22, -135.78] -81.00 [-98.45, -63.55] -231.00 [-293.37, -168.63] -99.00 [-117.90, -80.10] 2. -15.00 [-15.64, -14.36] -15.00 [-25.99, -4.01] -182.00 [-257.91, -106.09] -59.00 [-76.15, -41.85] 3. -3.59 [-3.91, -3.27] -3.44 [-3.89, -2.99] -1.97 [-2.95, -0.99] 4. 6.40 [6.05, 6.75] 0.70 [-0.63, 2.03] 3.00 [2.43, 3.57] 2.90 [1.73, 4.07] | I: 2: pain from needling C: 1: pain from needling | “Acupuncture is an effective and well-tolerated strategy for managing this common treatment-related side effect.” |
| Bao (2013) US (31) | 51 (I:25, C:26) | Median I: 61 (44–82) C: 61 (45–85) | 0-III | Musculo-skeletal Symptoms | AT | Sham | 8 w + 4 w (F/U) | 1. HAQ-DI∗ 2. VAS∗ 3. LAB | 1. P > .05 2. P > .05 3. P > .05 | none | “..did not observe a significant difference in AIMSS changes between real and sham acupuncture.” |
| Oh (2013) Australia (32) | 32 (I:16, C:16) | n.r. | I, II or IIIa hormone receptor-positive BC | Joint pain or stiffness | AT | Sham | 6 w + 6 w (F/U) | 1. BPI-SF∗ 2. WOMAC∗ 3. FACT-G 4. Handgrip strength test 5. CRP, ESR | 1–5. no significant differences (graph only) | I: 5: minor bruising | “..suggest that acupuncture is feasible and safe in patients with BC with joint pain caused by AI.” |
| Giron (2016) Brazil (33) | 50 (I:25, C:25) | 53.7 ± 11.1 | n.r. | Pain in scapular girdle and upper limb region | AT + Kinesio therapy | Kinesio-therapy | 10 w | 1. BDI∗ 2. DASH∗ 3. ROM (FL, EX, AD, AB, IR, ER) | 1. -1.70 [-3.06, -0.34] 2. 6.10 [4.59, 7.61] 3. 9.00 [5.45, 12.55] -3.90 [-5.94, -1.86] 2.30 [1.36, 3.24] 10.00 [4.38, 15.62] -2.00 [-6.37, 2.37] -3.00 [-7.13, 1.13] | n.r. | “Both groups showed statistically significant improvement and there was no difference between them.” |
| Cancer treatment induced Nausea & Vomiting (2) | |||||||||||
| Beith (2012) Australia (34) | 32 (I:16, C:17) | I: 52 ± 8.4 C: 52 ± 9.5 | 0-II | Nausea & Vomiting | EA | Sham EA | 3 cycles of chemo (9 w) | 1. Incidence of nausea (Acute; Delayed)† 2. Incidence of vomiting (Acute; Delayed)† 3. Lab (WCC, NEU, GCSF) | 1. 9/11;10/11 (p > 0.05) 2. 2/1;1/0 (P > .05) 3. P = .01, P = .01, P = .19 | none | “.. EA during chemotherapy is a promising option for controlling side-effects of chemo.” |
| He (2017) China (35) | 64 (I32, C32) | I:42.1 ± 4.29 C:42.2 ± 4.11 | I-IIIa | Nausea & Vomiting | AT | Sham | 1 w | 1. Severity of N/V (NCI- CTC 4.0, ≥ III)† 2. TCM symptoms (loss of appetite; fatigue; bloating)∗ 3. HADS (anxiety, depression)∗ | 1. 2/4 (p < 0.05) 2. -1.27 [-1.31, -1.23] -1.21 [-1.33, -1.09] -0.10 [-0.25, 0.05] 3. -1.46 [-1.94, -0.98] -1.14 [-1.26, -1.02] | n.r. | “..could help BC patients relieving N/V, improving the symptoms of poor appetite and body tired fatigue, and reducing HADS..” |
| Lymphedema (2) | |||||||||||
| Zhan (2017) China (36) | 60 (I:30, C:30) | n.r. | n.r. | BC related upper limb lymphedema | Abdominal acupuncture + Upper limb exercise | Upper limb exercise | 4 w | 1. Pain (VAS)∗ 2. Arm circumference∗ 3. Incidence of severe edema† | 1. -1.22 [-1.48, -0.96] 2.-1.47 [-1.62, -1.32] 3. 5/8 | n.r. | “.. is of better curative effect in eliminating edema and improving pain in phantom, which is worthy of promotion.” |
| Bao (2018) US (37) | 82 (I:40, C:42) | I: 65 C: 58 | ≥ II | BC-related lymphedema | AT | Wait-list | 6 w | 1. Arm circumference∗ 2. Bio-impedance∗ | 1. -0.38 [- 0.89, 0.12] 2. −1.06 [-7.85, 5.72] | I: 45:bruises, 2: hematoma, 2: pain, 1: skin infection | “..did not significantly reduce BCRL in pretreated patients receiving concurrent lymphedema treatment.” |
| Miscellaneous Symptoms (3) | |||||||||||
| Greenlee (2016) US (38) | 63 (I:31, C:32) | I: 51.8 ± 10.7 C: 48.3 ± 12.0 | I-III | Taxane-induced peripheral neuropathy | EA | Sham EA | 12 w | 1. BPI-SF∗ 2. FACT-NTX 3. FACT-TAX 4. NPS∗ | 1. -0.90 [-2.66, 0.86] 2. 1.40 [-2.87, 5.67] 3.-0.70 [-1.69, 10.29] 4. -6.00 [-19.64, 7.64] | I: 1:minor swelling and bruising at needle site | “.., there were no differences in pain or neuropathy between groups…” |
| Tong (2018) China (39) | 80 (I:40, C:40) | I:43.1 ± 4.23 C:42.3 ± 4.42 | 0-II | Chemo-related cognitive impairment | AT | No treatment | 8 w | 1. FACT-COG 2. AVLT (immediate recall, delayed recall, recognition) 3. VFT 4. SDMT 5. CDT 6. TMT-B∗ 7. BDNF | 1. 3.43 [3.15, 3.71] 2. -0.21 [-0.30, -0.12] 0.01 [-0.05, 0.07] 0.55 [0.46, 0.64] 3. -0.32 [-0.54, -0.10] 4. -0.39 [-0.78, 0.00] 5. 0.51 [0.39, 0.63] 6. 1.83 [1.54, 2.12] 7. 3.65 [3.53, 3.77] | n.r. | “..is effective in the treatment of CRCI in BC patients through a mechanism that may be related to an increase of BDNF.” |
| Zhang (2018) China (40) | 70 (I:35, C:35) | I:49.9 ± 3.20 C:50.5 ± 3.16 | n.r. | Chemo-induced gastro-intestinal symptoms | AT + Umbilical application+ Symptomatic therapy | Symptomatic therapy (Granisetron loperamide, Simo decoction) | 3 d | Response rate† (diarrhea, constipation, N/V) | 91.4%/82.9% 94.3%/80.0% 91.4%/77.1% (all P < .05) | n.r. | “..can effectively relieve the symptoms of diarrhea, constipation, N/V, and improve clinical efficacy.” |
AI = aromatase inhibitor, AT = acupuncture, AVLT = Auditory-verbal learning test, BDI = Beck depression inventory, BDNF = Brain-derived neurotrophic factor, BFI = Brief fatigue inventory, BPI-SF = Brief pain inventory - short form, C = control, CDT = Clock-drawing test, CES-D = Center for epidemiological studies depression scale, CRP = C reactive protein, DASH = Disabilities of the arm, shoulder and hand score, EA = electroacupuncture, ESR = Erythrocyte sedimentation rate, EXE = Exemestane, F/U = follow-up, FACT-COG = Functional assessment of cancer treatment cognition, FACT-G = Functional assessment of cancer therapy–general, FACT-NTX = Neurotoxicity component of functional assessment of cancer therapy taxane scale, FACT-TAX = Functional assessment of cancer therapy taxane scale, GCS = Greene climacteric scale, HADS = Hospital anxiety and depression scale, HAQ-DI = Health assessment questionnaire disability index, HFCS = Hot flush composite score, HFS = Hot flush score, HT = hormone therapy, I = intervention, KI = Kupperman's index, MenQoL = Menopause specific quality of life, MLN = metastatic lymph node, M-SACRAH = Modified score for the assessment and quantification of chronic rheumatoid affections of the hands, MYCaW = Measure yourself concerns and wellbeing questionnaire, n.r. = not reported, NPS = Neuropathic pain scale, PGWB = Psychological and general well-being index, PSQI = Pittsburgh sleep quality index, SDMT = Symbol digit modality test, SHBG = Sex hormone binding globulin, TAM = tamoxifen, tgAI = third generation of AI, TMT-B = Trail-making test part B, TROP = Tropisetron, VAS = Visual analog scale, VFT = Verbal fluency test, VNF = Venlafaxine, W-BQ12 = Wellbeing questionnaire, WHQ = Women's health questionnaire, WOMAC = Western Ontario and McMaster Universities osteoarthritis index.
Higher score indicates severe symptoms.
Dichotomous variables.
Table 3.
Details of Characteristics of Acupuncture.
| Acupuncture features | ||||||||
| Study ID | Acupuncture rationale | Acupoint selection principle | Acupuncture points used | Number of needles | Needle stimulation | Number of sessions | Frequency of acupuncture treatment | Concurrent treatment |
| Climacteric Symptoms (8) | ||||||||
| Nedstrand (2006) Sweden (21) | n.r. | Fixed acupoints | BL23, BL32 | 4 | Manual stimulation+EA | 14 | Twice a week for the first 2 w + once a week for remaining 10 w | n.r. |
| Deng (2007) US (22) | derived from previous reports & standard acupuncture textbooks | Semi-fixed acupoints according to symptoms | GV14, GB20, BL13, PC7, HT6, KI7, ST36, SP6 Ear AT (Shenmen, Sympathetic) | 19 | Manual stimulation | 8 | Twice a week, 4w | SERMs, GnRH or AI |
| Walker (2010) US (23) | n.r. | Fixed acupoints | KI3, BL23, SP6, GB20, GV14, GV20, ST36, LR3, HT7, PC7, CV6, LU9 | 12 | Manual stimulation | 16 | Twice a week for the first 4 w + once a week for remaining 8 w | hormone therapy with Tamoxifen or Arimidex |
| Frisk (2012) Sweden (24) | Based on earlier studies | Fixed acupoints | BL15, BL23, BL32, GV20, HT7, PC6, LR3, SP6, SP9 | 12 | Manual stimulation+EA | 14 | Twice a week for the first 2 w + once a w for remaining 10 w | n.r. |
| Liljegren (2012) Sweden (25) | According to previous reports and from expert opinion, as found in standard acupuncture textbooks | Fixed acupoints | LI4, HT6, LR3, ST36, SP6, KI7 | 8 | Manual stimulation | 10 | Twice a week, 5 w | Tamoxifen |
| Bao (2014) US (26) | Based on our clinical experience suggesting that AIMSS resulted from Qi deficiency | Fixed acupoints | CV4, CV6, CV12, LI4, MH6, GB34, ST36, KI3, BL65 | 15 | Manual stimulation | 8 | Once a week, 8w | AI therapy |
| Hervik (2009) (27) & Hervik (2014) Norway (28) | n.r. | Fixed acupoints | LI3, GB20, LU7, KI3, SP6, CV4, PC7, LI8 | 8 | Manual stimulation | 15 | Twice a week for the first 5 w + once a week for remaining 5 w | AI therapy (anastrozole, letrozole, or exemestane) |
| Lesi (2016) Italy (29) | According to Maciocia's recommendations | Semi-fixed acupoints according to pattern identification | SP6, LI11, CV4 + additional points according to TCM syndrome | ≥3 | Manual stimulation | 10 | Once a week, 10w | Cisplatin + chemotherapy |
| PAIN (4) | ||||||||
| Crew (2010) US (30) | based on a standard TCM point prescription to treat musculoskeletal pain | Semi-fixed acupoints according to pain location (max.3 points) | full body + auricular acupuncture + 3 most painful areas | ≥3 | Manual stimulation | 12 | Twice a week, 6w | tgAI (anastrozole, letrozole, or exemestane) |
| Bao (2013) US (31) | Based on our clinical experience suggesting that AIMSS resulted from Qi deficiency. | Fixed acupoints | CV4, CV6, CV12, LI4, MH6, GB34, ST36, KI3, BL65 | 15 | Manual stimulation | 8 | Once a week, 8w | tgAI |
| Oh (2013) Australia (32) | derived from standard acupuncture textbooks | Fixed acupoints | Day1: LI4, Li11, GB34, ST40, LR3, GV20, EX-HN1, EX-UE9 Day2: GB21, TE5, ST36, SP6, LR3, GV20, EX-HN1, EX-UE9 | 12 | Manual stimulation + EA | 12 | Twice a week, 6w | tgAI |
| Giron (2016) Brazil (33) | in accordance with the recommendations of Standards for Reporting of Controlled Trials in Acupuncture (RCTA) | Fixed acupoints | CV3, SP9, ST36, KI7, LR3, GB21, LI15, HT14, LU5, LI4, ST38, BL60 | 12 | Manual stimulation | 10 | Once a week, 10w | Adjuvant or neo-adjuvant Paclitaxel |
| Treatment Induced Nausea & Vomiting (2) | ||||||||
| Beith (2012) Australia (34) | n.r. | Fixed acupoints | PC6 (left), LI4 (right), ST36 (both) | 3 | Manual stimulation | 4 | 2 hr prior to chemo; on day 1 & 2 of the first two cycles | AC or FEC; Antiemetics |
| He (2017) China (35) | Based on the expert opinion Prof. Wang from Capital Medical University Beijing Hospital of Traditional Chinese Medicine | Fixed acupoints | CV12, LR13, CV6, ST25, PC6, ST36 | 6 | Manual stimulation | 4 | Every other day, 8d | ODT |
| Lymphedema (2) | ||||||||
| Zhan (2017) China (36) | Based on the theory of meridians | Fixed acupoints | CV12, CV10, CV6, CV4, ST24, ST26 | 6 | Manual stimulation | 28 | Once a day, 28d | n.r. |
| Bao (2018) US (37) | based on previous pilot study | Fixed acupoints | CV12, CV3, TE14, LI15, LU5, LI4, ST36, SP6 | 8 | Manual stimulation | 12 | Twice a week, 6w | Common standard dose chemotherapy regimens |
| Miscellaneous Symptoms (3) | ||||||||
| Greenlee (2016) US (38) | Developed based on a standard TCM protocol for qi and xue deficiency and stagnation and informal practitioner query. | Semi-fixed acupoints according to pain location | GB34, ST36, LI4, LI10, LU3, LU5, GV14 | 4–8 | Manual stimulation + EA | 12 | Once a week, 12w | Hormonal treatment |
| Tong (2018) China (39) | n.r. | Semi-fixed acupoints according to symptoms | GV20, EX-HN1, GV24, ST36, KI13, KI14, GB39 | 3-10 | Manual stimulation | 40 | Once a day for 5 days, 2 days of rest/w, 4w/cycle, 3d rest between cycle, 2 cycles | Chemotherapy |
| Zhang (2018) China (40) | n.r. | Fixed acupoints | RN4, RN6, RN10, RN12, ST24, ST25, SP15 | 8 | Manual stimulation | 9 | 30 min/ session, twice a day, 3 d | Granisetron hydrochloride |
3.3. Study designs
Data were extracted from the included studies and 19 RCTs[21–40] were included in the qualitative synthesis of this review.
3.4. Settings
Of the 19 studies, 7[22,23,26,30,31,37,38] were conducted in the United States, 5[21,24,25,27–29] in Europe, 2[32,34] in Australia, 1[33] in Brazil, and 4[35,36,39,40] in China. The published year of each trial varied between 2006 and 2018.
3.5. Participants
The number of participants in the trials ranged between 32 and 190. All trials contained women with breast cancer. The mean participant age was distributed between the 40 seconds and 60 seconds. Of the seven trials that targeted women with breast cancer below stage 3,[23,26,30–32,35,38] two trials enrolled patients below stage 2,[34,39] one trial recruited patients with breast cancer higher than stage 2,[37] one trial[24] used TNM stage as inclusion criteria, and the remaining 8 trials did not mention specific stages of BC.[21,22,25,27–29,33,36,40] The symptoms accompanying breast cancer were as follows: climacteric symptoms 8 [21–29], pain 4 [30–33], nausea and vomiting 2,[34,35] breast cancer-related lymphedema 2,[36,37] peripheral neuropathy 1,[38] cognitive impairment 1,[39] and gastrointestinal symptom 1.[40] Chemotherapy, aromatase inhibitor (AI) therapy, hormone therapy, surgery, and symptom-specific treatments were mentioned as concurrent treatments during the trial period (Table 2).
3.6. Interventions
Interventions used in all included studies were manual acupuncture and EA. Four trials[21,24,34,38] used EA, and the remaining 15 trials used manual acupuncture.[22,23,25–33,35–37,39,40] Among the manual acupuncture trials, one trial[40] employed a combination of symptomatic therapy, umbilical application with acupuncture, one[30] applied integrated therapy with acupuncture and auricular acupressure, two trials[33,36] employed various exercises in addition to acupuncture, and one trial[29] used a booklet with acupuncture. All of the studies applied manual acupuncture stimulation to treat certain symptoms caused by cancer treatment, of the four studies that used a combination of EA.[21,24,34,38] Most of the studies mentioned acupuncture points and mostly included a range between 3 and 19 points. However, Crew et al. did not mention specific acupoints other than full body and auricular acupuncture.[30] fourteen studies applied fixed acupuncture points based on previous studies, textbooks, and expert opinions,[21,23–28,31–37,40] while the remaining five studies used semi-fixed acupuncture points as indicated by primary patient complaints, pain locations, and pattern identifications.[22,29,30,38,39]
Acupuncture and EA treatment were administered at least once or twice per week. The treatment period ranged from 3 days to 12 weeks; four trials had periods of 4 weeks or under,[22,35,36,40] seven trials had periods of 5–8 weeks,[25,26,30–32,37,39] and 8 had periods of 9 to 12 weeks.[21,23,24,27–29,33,34,38] The total number of treatment sessions ranged from 4 to 40 sessions. Of the ten studies,[21–29,31,32] follow-up investigation was conducted in those identified in Tables 2 and 3.
3.7. Comparisons
There were three types of comparisons in this review. Active-control, placebo, and no-treatment groups were included as the control groups. Sham acupuncture was applied as a placebo in 8 trials,[22,25–28,30–32,35] and sham EA was used in 2 trials.[34,38] The conventional medicine, venlafaxine (VNF), was used as an active control in one trial.[23] Hormone therapy,[24] various exercises,[33,36] relaxation,[21] enhanced self-care by clinicians by providing a brochure,[29] and symptomatic therapy[40] were also selected for comparisons. Furthermore, no treatment[39] and wait-list[37] control groups were also used.
3.8. Outcomes
The outcomes of each trial were used to assess the common accompanying symptoms that were caused by cancer treatment; for example, climacteric symptoms (frequency and severity of hot flush and sweating),[21–29] pain (severity, functional disability, quality of life including sleep and emotional status),[30–33] nausea and vomiting (frequency, severity, and WHO grading),[34,35] lymphedema (level of edema, arm circumference),[36,37] neuropathic pain (severity and function),[38] cognitive impairment (functional assessment and neuropsychological tests),[39] and gastrointestinal symptoms (overall response rate).[40] The details of the effectiveness of acupuncture for the management of treatment-induced discomfort of the main problematic symptoms indicated in each study were as follows:
In patients experiencing climacteric symptoms, Hervik et al reported that general climacteric symptoms after treatment significantly reduced in the acupuncture group compared to the sham group using Kupperman's Index,[27,28] but Nedstrand et al. reported a significant effect in the applied relaxation group compared to the EA group.[21] Walker et al reported that the acupuncture group had a significant decrease in the daily frequency and severity of hot flushes after treatment compared to the Venlafaxine group (P < .05).[23] Frisk et al reported that compared to hormone therapy, the EA group demonstrated a significantly lower frequency of hot flushes (MD -0.5; 95%CI -0.9, -0.1).[24] Assessing the reduction rate of hot flushes with the Hot Flush Score, Lesi et al. reported that acupuncture with an enhanced self-care group had a higher reduction rate than did the single self-care group (64.9%/16.9%, P < .05).[29] However, Frisk et al showed that the hormone therapy group had a higher reduction rate than the EA group (100%/80%).[24] Two studies reported a significant effect of the intervention with respect to menopause-specific quality of life (P < .05).[23,29]
In patients experiencing pain induced by cancer treatment, Crew et al. demonstrated significant differences after treatment between acupuncture and sham groups using the Western Ontario and McMaster Universities Arthritis Index (WOMAC), Brief Pain Inventory-short form (BPI-SF), and Functional Assessment of Cancer Therapy–General (FACT-G), except the pain domain in the WOMAC and the social/family domain in the FACT-G (P < .05).[30] However, in Oh et al, none of the outcomes that Crew reported significant differences for showed any significant differences.[32] Giron et al showed significant differences in functional measures of flexion (MD 9.0; 95%CI 5.45, 12.55), adduction (MD 2.30; 95%CI 1.36 3.24), and abduction (MD 10.0; 95%CI 4.38 15.62), and significant reduction in depression measures (MD -1.7; 95%CI -3.06, -0.34).[33]
Of the 4 studies that assessed the effect of acupuncture on cancer treatment-induced nausea and vomiting. Beith et al. reported a higher incidence of acute (9/11) and delayed (10/11) nausea in the sham group, but there were no significant differences between groups (P > .05).[34] Incidence vomiting also resulted in a higher incidence of acute (2/1) and delayed (1/0) vomiting in the EA group (P > .05).[34] The incidence of severe nausea and vomiting after treatment was reported in one study using the US National Cancer Institute Common Terminology Criteria for Adverse Events v 4.0 (NCI- CTC 4.0) and showed a significantly higher incidence of severe nausea and vomiting in the control group (2/4, P < .05).[35] The concomitant symptoms associated with treatment induced nausea and vomiting, such as anxiety, depression, loss of appetite, abdominal bloating, and fatigue, were measured using the Hospital Anxiety and Depression Scale and TCM symptom grading scale. He et al. showed a significant reduction in the severity of anxiety (MD -1.46; 95%CI -1.94, -0.98), depression (MD –1.14; 95%CI -1.26 -1.02), fatigue (MD -1.21; 95%CI -1.33, -1.09), and loss of appetite (MD -1.27; 95%CI -1.31 -1.23) in acupuncture with ondansetron group compared to controls.[35]
In patients experiencing lymphedema, Zhan et al. reported a significant decrease in the change of arm circumference compared to upper limb exercises (MD -1.47; 95%CI -1.62, -1.32),[36] but Bao et al did not show any significant difference compared to the wait-list group (MD -0.38; 95%CI -0.89, 0.12).[37] The intensity of joint-related pain using the Visual Analog Scale was statistically significant after acupuncture and upper limb exercise treatment compared to the upper limb exercises group (MD -1.22; 95%CI -1.48, -0.96).[36]
Taxane-induced peripheral neuropathy was assessed over time in one study. Greenlee et al. assessed symptoms or concerns associated with chemotherapy and pain by using the Neurotoxicity Component of Functional Assessment of Cancer Therapy (FACT-NTX), Functional Assessment of Cancer Therapy Taxane Scale (FACT-TAX), BPI-SF, and neuropathy pain scale (NPS), but there were no significant differences between groups.[38]
In patients experiencing chemotherapy-related cognitive impairment, Tong et al. reported a greater improvement in the Functional Assessment of Cancer Treatment Cognition (FACT-COG) (MD 3.43; 95%CI 3.15, 3.71), recognition of Auditory-Verbal Learning Test (MD 0.55; 95%CI 0.46, 0.64), Clock-Drawing Test (MD 0.51; 95%CI 0.39, 0.63), and serum brain-derived neurotrophic factor (BDNF) (MD 3.65; 95%CI 3.53, 3.77) in the acupuncture group.[39]
In patients complaining of chemo-induced gastrointestinal symptoms, Zhang et al reported greater improvement in diarrhea (91.4%/82.9%), constipation (94.3%/80.0%), as well as nausea and vomiting (91.4%/77.1%) in the acupuncture group, with significant differences between groups.[40] Due to the heterogeneity of assessment measurements, we could not thoroughly analyze this section. Table 2 summarizes the details of the outcomes.
3.9. Adverse events
Adverse events were assessed in 11 trials.[22–24,26,29–32,34,37,38] Four studies[24,26,31,34] reported no incidence of adverse events. Five studies[22,30,32,37,38] reported mild adverse events such as, pain, bleeding or bruising from the needles. In one study, various adverse reactions (i.e., nausea, headache, dizziness, and sleeping difficulty) were reported in the control group treated with VNF,[23] and the remaining study showed muscle pain, headache, or menstrual bleeding in the treatment group.[29]
3.10. RoB in the included studies
The methodological quality of the included studies was assessed using the RoB tool, which evaluated 7 areas. In the performance bias category, only three studies used participant and assessor blinding and were assessed as ‘low-risk’.[22,30,38] Seven studies did not report random sequence generation[23,27–29,34,35,39,40] and 14 studies did not mention an allocation concealment method.[21–25,27–29,31,33–36,39,40] Thus, the category of selection bias was largely assessed as ‘unclear’. The detection bias was high because self-reporting questionnaires were generally used. The majority of studies reported what they mentioned in the methodology section and thoroughly collected outcome results. Thus, attrition bias and reporting bias were assessed as low-risk. Additionally, the category of other bias was assessed as unclear, since 9 studies did not adequately describe the baseline data.[22,23,27,28,30–32,34,39,40] The details of the RoB assessment are presented in Figure 3.
Figure 3.
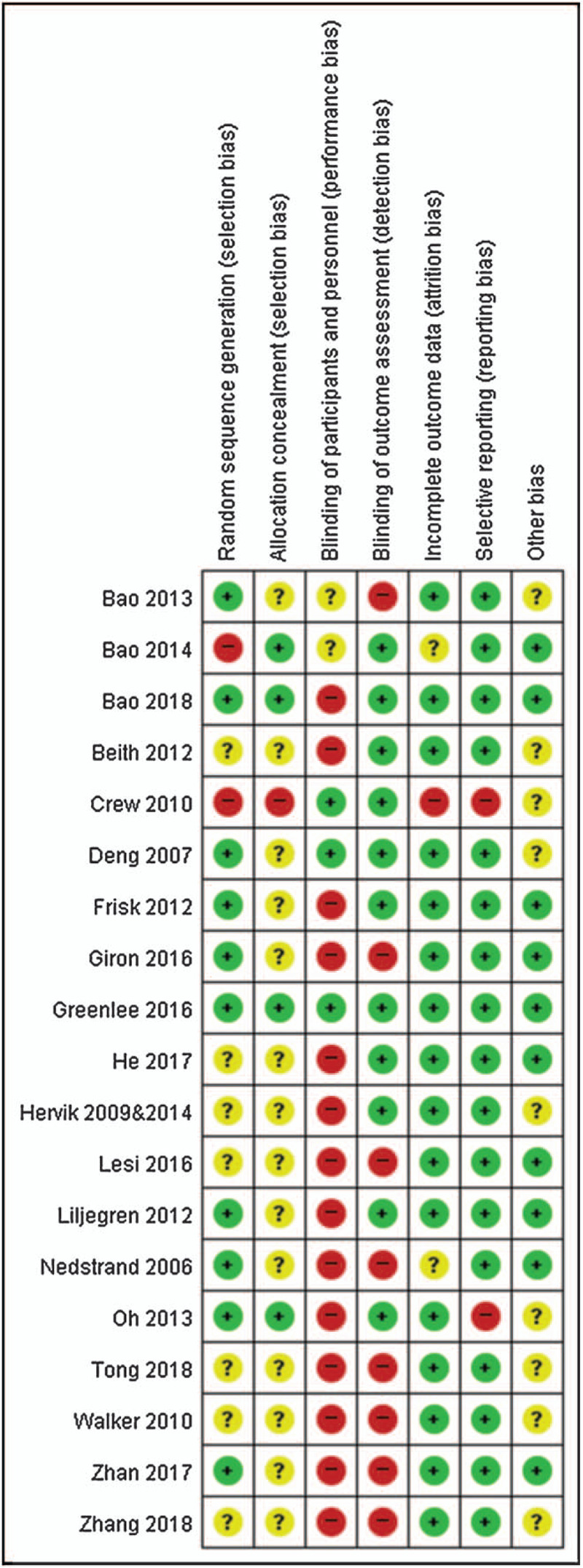
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study. ”+”: low risk, “?”: unclear risk, and “-“: high risk.
3.11. Meta-analyses
Due to the variety of outcomes, we only included 7 studies in the quantitative synthesis.[21,22,24,25,27,28,36,37] Overall, acupuncture was significantly effective for improving arm circumference due to cancer-related lymphedema and quality of sleep. On the other hand, menopausal symptoms such as hot flushes and KI did not improve compared to the control group (Fig. 2). The following is a brief overview of the meta-analysis results.
Figure 2.
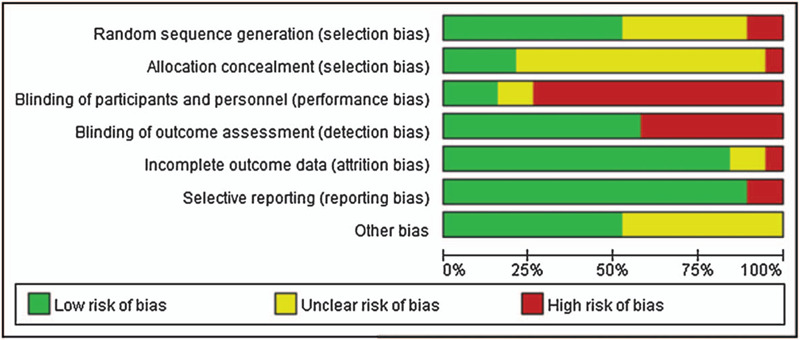
Risk of Bias Graph: Reviewer's assessments about each risk of bias item presented as percentages of all included studies.
3.11.1. Hot flash frequency (overall, nighttime time)
Five trials were suitable for meta-analysis.[21,22,24,25,27,28] The mean differences in daily hot flash frequency between the acupuncture and sham acupuncture or relaxation therapy groups (MD 0.3; 95%CI -0.84, 1.44; P = .61; I2 = 47%; 177 participants; 3 trials) (Fig. 4) and night time frequency between the acupuncture and wait-list groups (MD -0.83; 95%CI -1.94, 0.28; P = .14; I2 = 95%; 96 participants; 2 trials) were not statistically significant (Fig. 5).
Figure 4.
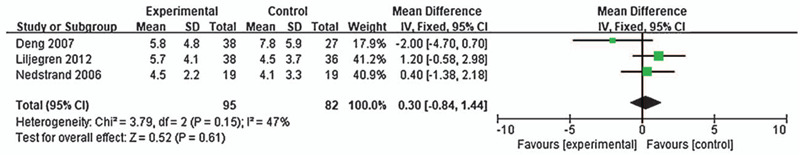
Forest plot of the effect of acupuncture on the frequency of hot flush (Overall).
Figure 5.
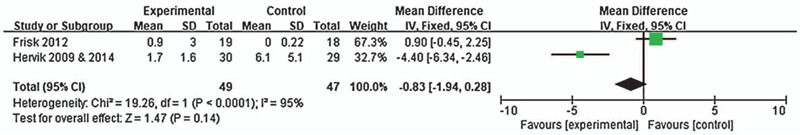
Forest plot of the effect of acupuncture on the frequency of hot flush (Night time).
3.11.2. Menopausal symptoms
Sufficient data on menopausal symptom assessments by KI were reported in two studies.[21,27,28] There were no statistically significant differences in the total KI score between the acupuncture and wait-list or relaxation therapy groups (MD -2.61; 95%CI -7.35, 2.14; P = .28; I2 = 99%; 126 participants; 2 trials) (Fig. 6).
Figure 6.
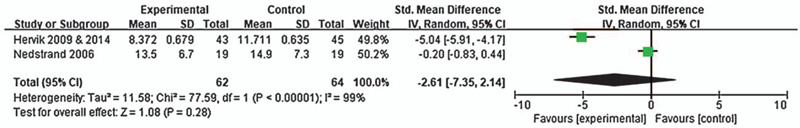
Forest plot of the effect of acupuncture on menopausal symptoms (Kupperman's Index).
3.11.3. Arm circumference
Two trials compared mean differences in arm circumference between the acupuncture and waitlist or exercise therapy groups (MD -1.61; 95%CI -1.92, -1.31; P < .00001; I2 = 72%; 133 participants; 2 trials), which were statistically significant, in favor of the control group[36,37] (Fig. 7).
Figure 7.
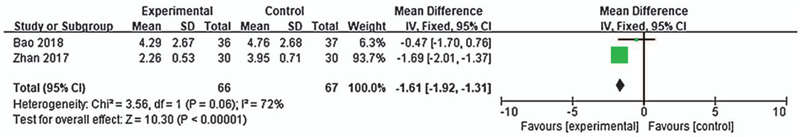
Forest plot of the effect of acupuncture on lymphedema (Arm circumference).
4. Discussion
The purpose of this review was to provide an overview of previous studies which investigated symptoms induced by BC treatments and to investigate the overall effectiveness of acupuncture. Nineteen studies were included in this review, and 7 studies were suitable for meta-analysis. The sample size of the included studies varied between 32 and 190, with 1,216 participants overall. These studies mentioned possible positive effects of acupuncture on BC treatment induced various symptoms, such as climacteric symptoms, pain, lymphedema, nausea, and miscellaneous symptoms. However, most of the authors suggested further confirmatory trials with conclusive evidence were needed, which indicates that there is still a lack of sufficient trials on acupuncture treatment as adjuvant therapy for BC. Overall, sixty distinct outcomes were measured in this review; the most frequently assessed outcomes were climacteric symptoms, pain, lymphedema, nausea and vomiting.
This study has several strengths. First, this study aimed to examine all of the acupuncture trials concerning the symptoms induced by BC treatment, in order to identify the efficacy of acupuncture treatment. Thus, we determined that the climacteric symptoms, pain, nausea, vomiting, lymphedema, cognitive impairment, gastrointestinal symptoms, and neuropathy were the main complaints in BC patients. Second, we reviewed a number of studies which were identified by a rigorous literature search strategy and we used standardized tools for reporting reviews and assessing bias.
Through this review, we learned that most of the studies were conducted in the United States, Europe, and China, while no studies have been published from Korea. In Korea, breast cancer is the second-most common cancer with a rapidly increasing incidence in Korean women. However, we identified a lack of evidence for the management of concomitant symptoms during BC treatment.
We also learned that most interventions have focused on manual acupuncture or EA. Interventions included enhanced self-care, auricular acupuncture, kinesio-therapy, exercises, symptomatic therapy, and umbilical application. However, due to the heterogeneity across the studies, they differed widely in terms of participant characteristics, duration, frequency of the interventions, and outcome measurement tools. Thus, we could not thoroughly evaluate the effectiveness of outcomes for measuring the benefit on certain symptoms. Only the change in affected arm circumference due to lymphedema was significantly different before and after treatment, which contradicts previous studies.[41,42] Such differences may be due to variations between measurement tools. With regard to climacteric symptoms, most of the studies reported a significant effect on general menopausal symptoms, but there was no improvement in the frequency and severity of hot flush, which is consistent with the results of previous studies.[43,44] Our findings with respect to musculoskeletal symptoms indicate that acupuncture may or may not alleviate pain and improve the function of the affected region. Conflicting with our data, a study on arthralgia previously reported that acupuncture reduced the pain and stiffness, but this was not statistically significant.[45] This difference may be due to the musculoskeletal symptoms which were not classified into body regions. Regarding nausea and vomiting, we found that acupuncture was associated with a statistically significant increase appetite and reduce the level of fatigue, anxiety, and depression. Further, studies on cognitive impairment and gastrointestinal symptoms demonstrated significant effects of acupuncture, including in cognitive function, levels of BDNF, incidence of diarrhea, constipation, nausea, and vomiting. However, there are no published studies to which these studies can be compared.
Despite the beneficial results of acupuncture treatment on various symptoms induced by BC treatment, most studies had a low level of reporting quality and a high heterogeneity in methodological quality. Furthermore, there are few studies in which specific symptoms are treated by acupuncture and subsequently evaluated.
This review has some limitations. First, there was no specific restriction on the study selection characteristics for breast cancer, such as stage of cancer, size of tumor, type of surgery, type of chemotherapy. Therefore, these findings only provide preliminary evidence for BC and further studies with a systematic methodology will be needed. Second, acupuncture points were not discussed because there was no similarity among the included trials. Our research team will analyze this topic using network meta-analysis in the near future. Third, although we searched all published studies concerning acupuncture for symptoms induced by BC treatment, we could not identify any studies in the Korean population. Thus, ethnic differences between countries should be examined in future comparative trials for appropriate planning in Korea. Despite these limitations, none of the studies reported severe adverse effects other than minor events, such as slight bleeding and/or bruising due to needle puncture.
This systematic review and meta-analysis of women being treated for breast cancer confirmed that acupuncture had no significant effect on the frequency and severity of hot flushes, but was associated with a significant reduction in general climacteric symptoms and an increase in quality of life. We conclude that acupuncture is not inferior, with respect to safety, to hormone therapy or other applied relaxation therapies in alleviating the symptoms of menopause.
5. Conclusions
There is currently insufficient evidence to conclude that acupuncture is of any benefit to patients suffering from symptoms caused by cancer treatment. Therefore, more rigorous studies are needed to clearly reveal the effectiveness of acupuncture in symptoms induced by BC treatment.
Acknowledgments
We thank Editage for English language editing. This manuscript was edited for English language by Editage.
Author contributions
BHJ and DSH designed the entire study. SJ and YK wrote the manuscript. All authors have read and consent to the publication of the manuscript.
Correction
The corresponding author has been changed from Bo-Hyoung Jang to Deok-Sang Hwang.
Footnotes
Abbreviations: AI = aromatase inhibitor, AT = acupuncture, AVLT = auditory-verbal learning test, BC = breast cancer, BDI = Beck depression inventory, BDNF = Brain-derived neurotrophic factor, BFI = brief fatigue inventory, BPI-SF = brief pain inventory - short form, C = control, CAM = complementary and alternative medicine, CDT = Clock-drawing test, CES-D = center for epidemiological studies depression scale, CRP = C reactive protein, DASH = disabilities of the arm, shoulder and hand score, EA = electro-acupuncture, ESR = Erythrocyte sedimentation rate, EXE = exemestane, F/U = follow-up, FACT-COG = Functional assessment of cancer treatment cognition, FACT-G = functional assessment of cancer therapy–general, FACT-NTX = neurotoxicity component of functional assessment of cancer therapy taxane scale, FACT-TAX = functional assessment of cancer therapy taxane scale, GCS = Greene climacteric scale, HADS = hospital anxiety and depression scale, HAQ-DI = health assessment questionnaire disability index, HFCS = Hot flush composite score, HFS = Hot flush score, HT = hormone therapy, I = intervention, KI = Kupperman's index, MenQoL = menopause specific quality of life, MLN = metastatic lymph node, M-SACRAH = modified score for the assessment and quantification of chronic rheumatoid affections of the hands, MYCaW = measure yourself concerns and wellbeing questionnaire, n.r. = not reported, NPS = neuropathic pain scale, PGWB = psychological and general well-being index, PRISMA = preferred reporting items for systematic reviews and meta-analyses protocols, PSQI = Pittsburgh sleep quality index, RCT = randomized control trial, RoB = Risk of Bias, SDMT = symbol digit modality test, SHBG = sex hormone binding globulin, TAM = tamoxifen, tgAI = third generation of AI, TMT-B = trail-making test part B, TROP = Tropisetron, VAS = visual analog scale, VFT = verbal fluency test, VNF = venlafaxine, W-BQ12 = wellbeing questionnaire, WHQ = Women's health questionnaire, WOMAC = Western Ontario and McMaster Universities osteoarthritis index.
How to cite this article: Jang S, Ko Y, Sasaki Y, Park S, Jo J, Kang NH, Yoo ES, Park NC, Cho Sh, Jang H, Jang BH, Hwang DS, Ko SG. Acupuncture as an adjuvant therapy for management of treatment-related symptoms in breast cancer patients: systematic review and meta-analysis (PRISMA-compliant). Medicine. 2020;99:50(e21820).
SJ and YK are the co-first author and contributed equally to this work.
All data generated or analyzed during this study are included in this published.
This study was supported by the Traditional Korean Medicine R&D Program funded by the Ministry of Health & Welfare through the Korea Health Industry Development Institute (KHIDI) (HB16C0072). The funding source had no influence in the design of the study, analysis, interpretation of the data, and writing the manuscript.
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Ginsburg O, Bray F, Coleman MP, et al. The global burden of women's cancers: a grand challenge in global health. Lancet 2017;389:847–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Fitzmaurice C, Allen C, Barber RM, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2017;3:524–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Kwekkeboom KL. Cancer symptom cluster management. Semin Oncol Nurs 2016;32:373–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dong ST, Butow PN, Costa DS, et al. Symptom clusters in patients with advanced cancer: a systematic review of observational studies. J Pain Symptom Manage 2014;48:411–50. [DOI] [PubMed] [Google Scholar]
- [5].Yeh CH, Chien L, Lin W, et al. Pilot randomized controlled trial of auricular point acupressure to manage symptom clusters of pain, fatigue, and disturbed sleep in breast cancer. Cancer Nurs 2015. [DOI] [PubMed] [Google Scholar]
- [6].Hu XD, Li Y, Peng YX, et al. Research progress of symptom clusters in cancer patients. J of Nurs Admin 2020;20:195–200. [Google Scholar]
- [7].Li Z, Zheng Z, Wang L, et al. Efficacy evaluation of heat-sensitive moxibustion for chemotherapy symptoms of large intestine cancer. Chin Acupunct Moxibust 2015;35:1010–3. [PubMed] [Google Scholar]
- [8].Jiao J, Luo ZQ, Zhang WM. Study for the effects of acupressure on symptom clusters for patients with advanced cancer. J Nurs Train 2015;30:2221–3. [Google Scholar]
- [9].Schapira MM, Mackenzie ER, Lam R, et al. Breast cancer survivors willingness to participate in an acupuncture clinical trial: a qualitative study. Support Care Cancer 2014;22:1207–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].DiGianni LM, Garber JE, Winer EP. Complementary and alternative medicine use among women with breast cancer. J Clin Oncol 2002;20:34S–8S. [PubMed] [Google Scholar]
- [11].Gerber B, Scholz C, Reimer T, et al. Complementary and alternative therapeutic approaches in patients with early breast cancer: a systematic review. Breast Cancer Res Treat 2006;95:199–209. [DOI] [PubMed] [Google Scholar]
- [12].Ernst E. Assessments of complementary and alternative medicine: the clinical guidelines from NICE. Int J Clin Pract 2010;64:1350–8. [DOI] [PubMed] [Google Scholar]
- [13].Joshi N, Araque H. Neurophysiologic basis for the relief of human pain by acupuncture. Acupunct Electrother Res 2009;34:165–74. [DOI] [PubMed] [Google Scholar]
- [14].Wong LYE, Wong CK, Leung PC, et al. The efficacy of herbal therapy on quality of life in patients with breast cancer: self-control clinical trial. Patient Prefer Adher 2010;4:223–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Xue D, Sun H, Li P-P. Long-term Chinese herbs decoction administration for management of hot flushes associated with endocrine therapy in breast cancer patients. Chin J Cancer Res 2011;23:74–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ma H, Sullivan-Halley J, Smith AW, et al. Estrogenic botanical supplements, health-related quality of life, fatigue, and hormone-related symptoms in breast cancer survivors: A HEAL study report. BMC Complement Altern Med 2011;2011:1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].De Oliveira Campos MP, Riechelmann R, Martins LC, et al. Guarana (Paullinia cupana) improves fatigue in breast cancer patients undergoing systemic chemotherapy. J Altern Complement Med 2011;17:505–12. [DOI] [PubMed] [Google Scholar]
- [18].Kim TH, Kang JW, Lee MS. Current evidence of acupuncture for symptoms related to breast cancer survivors A PRISMA-compliant systematic review of clinical studies in Korea. Medicine (Baltimore) 2018;97:e11793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. [DOI] [PubMed] [Google Scholar]
- [20].Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Elizabeth Nedstrand YW, Mats Hammar, Klaas, et al. Psychological well-being improves in women with breast cancer after treatent with applied relaxation or eletro-acupuncture for vasomotor symptom. J Psych Obstetr Gynecol 2006;27:193–9. [DOI] [PubMed] [Google Scholar]
- [22].Deng G, Vickers A, Yeung S, et al. Randomized, controlled trial of acupuncture for the treatment of hot flushes in breast cancer patients. J Clin Oncol 2007;25:5584–90. [DOI] [PubMed] [Google Scholar]
- [23].Walker EM, Rodriguez AI, Kohn B, et al. Acupuncture versus venlafaxine for the management of vasomotor symptoms in patients with hormone receptor-positive breast cancer: a randomized controlled trial. J Clin Oncol 2010;28:634–40. [DOI] [PubMed] [Google Scholar]
- [24].Frisk J, Kallstrom AC, Wall N, et al. Acupuncture improves health-related quality-of-life (HRQoL) and sleep in women with breast cancer and hot flushes. Support Care Cancer 2012;20:715–24. [DOI] [PubMed] [Google Scholar]
- [25].Liljegren A, Gunnarsson P, Landgren BM, et al. Reducing vasomotor symptoms with acupuncture in breast cancer patients treated with adjuvant Tamoxifen: a randomized controlled trial. Breast Cancer Res Treat 2012;135:791–8. [DOI] [PubMed] [Google Scholar]
- [26].Bao T, Cai L, Snyder C, et al. Patient-reported outcomes in women with breast cancer enrolled in a dual-center, double-blind, randomized controlled trial assessing the effect of acupuncture in reducing aromatase inhibitor-induced musculoskeletal symptoms. Cancer 2014;120:381–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hervik J, Mjaland O. Acupuncture for the treatment of hot flushes in breast cancer patients, a randomized, controlled trial. Breast Cancer Res Treat 2009;116:311–6. [DOI] [PubMed] [Google Scholar]
- [28].Hervik J, Mjaland O. Long term follow up of breast cancer patients treated with acupuncture for hot flushes. Springerplus 2014;3:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Grazia Lesi GR, Assunta Musti M, Stivanello E, et al. Acupuncture as an integrative approach for the treatment of hot flushes in women with breast cancer: a prospective multicenter randomized controlled trial (AcCliMaT). J Clin Oncol 2016;34:1795–802. [DOI] [PubMed] [Google Scholar]
- [30].Crew KD, Capodice JL, Greenlee H, et al. Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer. J Clin Oncol 2010;28:1154–60. [DOI] [PubMed] [Google Scholar]
- [31].Bao T, Cai L, Giles JT, et al. A dual-center randomized controlled double blind trial assessing the effect of acupuncture in reducing musculoskeletal symptoms in breast cancer patients taking aromatase inhibitors. Breast Cancer Res Treat 2013;138:167–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Oh B, Kimble B, Costa DS, et al. Acupuncture for treatment of arthralgia secondary to aromatase inhibitor therapy in women with early breast cancer: pilot study. Acupunct Med 2013;31:264–71. [DOI] [PubMed] [Google Scholar]
- [33].Giron PS, Haddad CA, Lopes de Almeida Rizzi SK, et al. Effectiveness of acupuncture in rehabilitation of physical and functional disorders of women undergoing breast cancer surgery. Support Care Cancer 2016;24:2491–6. [DOI] [PubMed] [Google Scholar]
- [34].Jane M, Beith BO, Mark D, et al. Electroacupuncture for nausea, vomiting, and myelosuppression in women receiving adjuvant chemotherapy for early breast cancer: a randomized controlled pilot trial. Med Acupunct 2012;24:241–8. [Google Scholar]
- [35].Pei-Shan H, Xiao-min W, Guo-Wang Y, et al. Prospective randomized controlled trial of treating and preventing chemotherapy-related nausea and vomiting on breast cancer patients with ‘experienced ten acupoints’. China J Trad Chin Med Pharm 2017;32:2805–7. [Google Scholar]
- [36].Zhan Jing LC-s. Clinical observation of abdominal acupuncture combining with upper limb functional exercise in treatment of patients with breast cancer-related upper limb lymphoedema. Chin J Woman Child Health Res 2017;28:570–2. [Google Scholar]
- [37].Bao T, Iris Zhi W, Vertosick EA, et al. Acupuncture for breast cancer-related lymphedema: a randomized controlled trial. Breast Cancer Res Treat 2018;170:77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Greenlee H, Crew KD, Capodice J, et al. Randomized sham-controlled pilot trial of weekly electro-acupuncture for the prevention of taxane-induced peripheral neuropathy in women with early stage breast cancer. Breast Cancer Res Treat 2016;156:453–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Tong T, Pei C, Chen J, et al. Efficacy of acupuncture therapy for chemotherapy-related cognitive impairment in breast cancer patients. Med Sci Monit 2018;24:2919–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Zhang ZY. Clinical study of abdominal acupuncture combined with umbilical patch for acute gastrointestinal adverse reactions after chemotherapy for breast cancer. Guide China Med 2018;16:187. [Google Scholar]
- [41].Chien TJ, Liu CY, Fang CJ. The effect of acupuncture in breast cancer-related lymphoedema (BCRL): a systematic review and meta-analysis. Integr Cancer Ther 2019;18:1534735419866910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Hou W, Pei L, Song Y, et al. Acupuncture therapy for breast cancer-related lymphedema: a systematic review and meta-analysis. J Obstet Gynaecol Res 2019;45:2307–17. [DOI] [PubMed] [Google Scholar]
- [43].Chien T-J, Hsu CH, Liu CY, et al. Effect of acupuncture on hot flush and menopause symptoms in breast cancer- A systematic review and meta-analysis. PLoS One 2017;12:e0180918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Wang XP, Zhang DJ, Wei XD, et al. Acupuncture for the relief of hot flashes in breast cancer patients: A systematic review and meta-analysis of randomized controlled trials and observational studies. J Can Res Ther 2018;14: Suppl S3: 600–8. [DOI] [PubMed] [Google Scholar]
- [45].Chien TJ, Liu CY, Chang YF, et al. Acupuncture for treating aromatase inhibitor-related arthralgia in breast cancer: a systematic review and meta-analysis. J Altern Complement Med 2015;21:251–60. [DOI] [PMC free article] [PubMed] [Google Scholar]


