Abstract
Background
Children with irritable bowel syndrome (IBS) have lower health-related quality-of-life (HRQOL) than healthy controls (HC). Abdominal pain and psychosocial distress are negatively associated with HRQOL, though their relative effect is unclear.
Aim
Compare the relative associations of abdominal pain and psychosocial distress with HRQOL in HC and IBS.
Study
Baseline abdominal pain, psychosocial distress, and HRQOL measures were obtained from HC and IBS pediatric clinical trial participants. Regression assessed which measures were most strongly associated with Physical and Psychosocial HRQOL separately by group. Interaction analyses examined group differences in the associations of abdominal pain and psychosocial distress with HRQOL.
Results
Eight-five HC and 213 children with IBS participated. Somatization was most strongly associated with Physical HRQOL in HC, and functional disability was most strongly related in IBS. With respect to Psychosocial HRQOL, somatization was most strongly associated for both HC and IBS; depression was also significantly associated in HC. The strength of association between somatization and Physical HRQOL differed between groups; the negative association was less pronounced for IBS than HC. The association between functional disability and both Physical and Psychosocial HRQOL differed significantly between groups; the negative associations were more pronounced for IBS than HC.
Conclusions
Multiple psychosocial distress measures, including somatization, were associated with HRQOL in children with IBS; HRQOL in HC was driven consistently by somatization, to the exclusion of other psychosocial concerns. The associations of somatization and functional disability with HRQOL are distinctly different between HC and IBS. This knowledge supports utilization of psychosocial interventions to improve overall well-being for children with IBS.
Keywords: irritable bowel syndrome, pediatrics, health-related quality of life, psychosocial distress
INTRODUCTION
Irritable bowel syndrome (IBS) is defined by the expert Rome Committee as a functional abdominal pain disorder characterized by chronic abdominal pain not attributable to an anatomic or biochemical abnormality and associated with changes in stool frequency and/or stool form.1, 2 About 20% of the pediatric population is affected and more than half of these children continue to have similar symptoms as adults, at a cost of 30 billion dollars annually in the United States.3–9
The overall burden of IBS can be gauged by many outcomes including symptomatology, healthcare utilization, daily functioning, and health-related quality-of-life (HRQOL).10, 11 HRQOL examines quality-of-life in the context of health and disease and is a multidimensional concept incorporating aspects of physical and mental well-being.12 Previous studies in children have shown that HRQOL is significantly lower in IBS than healthy controls (HC) and even trends lower for children with organic gastrointestinal (GI) diseases such as inflammatory bowel disease and gastroesophageal reflux disease.13, 14
Multiple lines of research in IBS show relationships between HRQOL and both abdominal pain and psychosocial distress.15–20 Not surprisingly, GI symptoms like abdominal pain and stomach discomfort when eating have been associated with decreased HRQOL in children with IBS.21 A recent meta-analysis of children with chronic pain emphasized a negative relationship between HRQOL and pain catastrophizing (i.e., predicting the worst and feeling helpless in response to an actual or anticipated painful event).22–24 Further, somatization, defined as “increased perception, awareness, and/or pathological interpretation of unpleasant physiological sensations,” is negatively associated with HRQOL in adults with functional GI disorders, independent of GI symptoms.25, 26
Abdominal pain severity and psychosocial distress are both associated with HRQOL, however their relative association with HRQOL is unknown in children with IBS. While one might assume that targeting pain would best improve HRQOL, adult studies comparing these factors in people with IBS and healthy controls suggests otherwise. Addante and colleagues explored the relative associations between HRQOL, GI symptoms, and various psychosocial factors in adults with IBS and HC. In contrast to healthy controls, they found psychosocial distress was more closely associated with poor HRQOL than physical symptoms in those with IBS.27 Understanding the relative contribution of abdominal pain severity and psychosocial distress is important to inform further intervention efforts to improve the overall well-being of children with IBS.
Our goal was to 1) examine the relative associations of abdominal pain severity, psychosocial distress, and somatization with HRQOL among children with and without IBS and (2) assess whether the associations among these measures and HRQOL differed between HC and IBS.
Materials and Methods
Study Sample
Baseline data from pediatric participants who had been enrolled in one of four IBS observational and intervention trials at Baylor College of Medicine/Texas Children’s Hospital were used in this study. Study participants were children ages 7 to 18 years old. Children were recruited from a large healthcare network based in Houston, TX, which is located in the southwest United States.28 Trained research coordinators reviewed medical charts for ICD-9 codes for potential participants with abdominal pain and IBS or well child, both groups without other chronic illness. Secondary review of medical and laboratory records was performed by an investigator (RJS) who ascertained no alternative GI illness accounted for or could potentially account for the abdominal pain symptom. Participants then were screened via telephone using a modified pediatric Rome III questionnaire2, 29 and retained in the IBS or HC groups if they met (or did not meet in the case of HC) criteria for IBS. Participants were ultimately classified as either HC or IBS based on symptoms recorded in a validated 2-week abdominal pain and stooling diary and Rome III criteria.2, 29–33 Participating HC did not meet criteria for Rome III defined functional abdominal pain or IBS or endorse any other chronic pain conditions. Caregivers provided their child’s age, gender, and race/ethnicity at enrollment. All clinical trial protocols were approved by Baylor College of Medicine’s Institutional Review Board. Consent was obtained from parents and assent from the children. All data utilized in this cross-sectional study were captured prior to any study intervention.
Measures
Health-Related Quality-of-Life Measures
HRQOL was measured using the child-report Pediatric Quality of Life Inventory 4.0™ Generic Core Scales,34 which has been widely used with healthy children and adolescents as well as those with acute and chronic illnesses. This instrument contains 23 items (e.g., In the past one month, how much of a problem has this been for you…It is hard for me to walk more than one block). Respondents respond to HRQOL items using a 5-point Likert scale ranging from “never (0)” to “almost always (4).”34 The instrument yields Physical, Emotional, Social, and School Functional Scales. The Psychosocial Health Summary Score is computed as the mean of the items included for the Emotional, Social, and School Functional Scales, and the Physical Health Summary Score is equivalent to the Physical Functioning Scale Score. Both the Physical and Psychosocial Health Summary Scores were used for this study, with higher scores indicating better HRQOL.
Abdominal Pain Measurement
As noted above, abdominal pain was recorded by participants through a validated 2-week abdominal pain and stooling diary.29–33 From the baseline diary, we captured both abdominal pain frequency and mean pain intensity over the 2-week period for each participant. When pain was endorsed, the participant was instructed to indicate the extent to which that pain interfered with activities using a 4-point Likert scale ranging from “no interference (0)” to “could not participate due to pain (3).” The mean pain interference rating during the 2-week period was calculated for each participant.28
Functional Disability
The Functional Disability Inventory measured the degree to which children have difficulty functioning due to their physical status.35, 36 On this validated questionnaire children rate the extent to which they had trouble with various activities (e.g., eating, sleeping, walking, playing, etc.) due to physical health within the last two weeks using a 5-point Likert scale ranging from “no trouble (0)” to “impossible (4).” Items are summed for a total score. Higher scores indicate more functional disability.
Pain Catastrophizing
Pain catastrophizing is a thinking pattern characterized by expecting the worst and feeling unable to do anything about it in response to actual or anticipated pain.23 Across the four studies from which these data were obtained, this construct was assessed using two different instruments. Responses from these two instruments were combined as described below to form a single measure of pain catastrophizing for these analyses.37
Two studies used the Pain Catastrophizing Scale (PCS-C), which is a validated 11-item survey using a 5-point Likert scale ranging from 0 to 4.38, 39 Subscales for this instrument include Rumination (cannot stop thinking about pain), Magnification (concern about the seriousness of the pain), and Helplessness (how overwhelming the pain is). All items were summed to generate a total score and then converted to a Z-score based on the study sample’s distribution. The other two studies used the Pain Response Inventory (PRI), which is a 60-item questionnaire designed to assess coping skills for children with chronic abdominal pain that contains items concerning pain catastrophizing. This instrument also uses a 5-point Likert scale ranging from 0 to 4.40, 41 For our constructed pain catastrophizing measure, we used 11 items from the Catastrophizing and Distract/Ignore subscales, which contained items that were similar or identical to the PCS-C Rumination, Magnification, and Helplessness dimensions noted above. To calculate the PRI-derived catastrophizing total score variable, we summed the 8-item responses from the PRI Catastrophizing Scale and reverse coded 3-item responses from the PRI Distract/Ignore Scale (items 34, 44, and 48; e.g., Try to think of something pleasant to take you mind off the pain). The 11 items then were summed and a total score was calculated. The total scores were converted into a Z score for this specific sample. We then compiled this data with the above PCS-C Z scores to create a single pain catastrophizing measure for all participants. Higher scores indicate more severe pain catastrophizing thoughts.
Anxiety and Depression
Anxiety and depression were measured using the Behavioral Assessment System for Children, Second Edition (BASC-2). This instrument is designed to assess the behavioral and emotional problems of children and adolescents using a 4-point Likert scale with responses ranging from “never (0)” to “almost always (3).”42 Item responses are summed for a raw score and then converted into a T–score based upon a large normative sample. The Anxiety and Depression Clinical Scales were used. Higher scores imply more severe psychosocial distress.
Somatization
The Children’s Somatization Inventory measures the frequency and severity of somatic symptoms taken from DSM-III-R criteria for somatization disorder43 and the somatization factor for the Hopkins Symptoms Checklist.44 Examples of items include “headaches,” “feeling low in energy”, and “muscle aches.” Participating children rated on a 5-point Likert scale (0- “not at all” to 4- “a whole lot”) the extent to which each of 35 symptoms have “bothered” them during the last 2 weeks. Total scores are calculated, with higher scores indicating more pronounced somatization.
Data Analysis
Similar to the adult HC and IBS study by Addante and colleagues,27 the associations of abdominal pain and psychosocial distress measures with Physical and Psychosocial HRQOL were assessed. Parametric tests were used for normal continuous data and Chi squared tests for categorical data. Cohen’s d measured the effect size differences for the Physical and Psychosocial HRQOL outcomes between groups for the abdominal pain and psychosocial measures. An alpha of 0.05 was utilized for these tests.
The correlations between all abdominal pain and psychosocial distress measures and Physical and Psychosocial HRQOL outcomes were calculated, and the partial correlation for these same measures adjusted for all demographics were evaluated. We then used multivariate linear regression models to calculate the regression coefficient, or beta, and compared the magnitude of the associations between abdominal pain and psychosocial distress measures on Physical and Psychosocial HRQOL (i.e., separate analyses for both dependent outcome variables) by sample group (i.e., HC and IBS groups). This process yielded four separate multivariate linear regression models. Abdominal pain and psychosocial distress measures that were identified as having problematic multi-collinearity, defined by a variance inflation factor (VIF) > 4, were removed from all further analyses. The respective unstandardized (B) and standardized (β) betas were calculated for each abdominal pain and psychosocial distress measure, and the coefficient of multiple determination (R2) for each model assessed the models’ goodness-of-fit.
The final analyses investigated whether the association between any abdominal pain or psychosocial distress measure and Physical and Psychosocial HRQOL significantly differed between the HC and IBS groups. Interaction analyses assessed whether the effect of each abdominal pain and psychosocial distress measure was different on both Physical and Psychosocial HRQOL by sample group (HC vs IBS). This process utilized the multivariate regression models noted above and added independent variable interactions to control for other independent measures. Based on Bonferroni adjustment for multiple tests, an alpha cutoff of 0.007 for these regression analyses was assigned.45 For each significant interaction identified, linear regression models for HC and IBS were graphed to demonstrate the difference in the associations. Regression analyses were conducted in SPSS Statistics 25 for Windows software (IBM Corporation, Armonk, NY) and the interaction regression model analysis and related graphs were created with SAS 9.4 for Windows (SAS Institute, Inc., Cary, NC).
RESULTS
This study included 85 and 213 participants for the HC and IBS groups, respectively. As would be expected, both Physical and Psychosocial HRQOL were significantly higher in HC participants compared to those with IBS (Table 1). Scores on all abdominal pain and psychosocial distress measures were lower for the HC group compared to IBS (Table 1). All demographic, abdominal pain, psychosocial distress measures were significantly correlated with both HRQOL outcomes, and these correlations remained after accounting for age, gender, and race/ethnicity (Supplemental Digital Content Table 1).
Table 1.
Healthy Controls and Irritable Bowel Syndrome Group Characteristics
| Healthy Controls (n=85) | IBS (n=213) | P-value | Cohen’s d | |
|---|---|---|---|---|
| Demographics | ||||
| Age (y) | 9.87 (2.01) | 10.85 (2.61) | 0.001 | |
| Gender, Female [n (%)] | 52 (61.2) | 132 (62.0) | 0.90 | |
| Race/Ethnicity [n (%)] | 0.79 | |||
| White, non-Hispanic | 43 (50.6) | 118 (55.4) | ||
| Black, non-Hispanic | 14 (16.5) | 31 (14.6) | ||
| Hispanic/Latino | 24 (28.2) | 51 (23.9) | ||
| Asian and More than One Race | 4 (4.7) | 13 (6.1) | ||
| HRQOL Measures | ||||
| Physical HRQOL | 90.70 (11.43) | 78.14 (18.46) | <0.001 | 0.81 |
| Psychosocial HRQOL | 87.04 (14.60) | 77.65 (16.43) | <0.001 | 0.60 |
| Abdominal Pain and Psychosocial Distress Measures | ||||
| Pain Frequency | 0.38 (0.58) | 14.19 (9.76) | <0.001 | 1.99 |
| Pain Intensity | 1.13 (1.94) | 3.29 (1.29) | <0.001 | 1.31 |
| Pain Interference | 0.19 (0.50) | 0.63 (0.48) | <0.001 | 0.90 |
| Somatization | 12.64 (12.77) | 27.95 (17.74) | <0.001 | 0.99 |
| Functional Disability | 4.18 (6.09) | 11.36 (9.33) | <0.001 | 0.91 |
| Pain Catastrophizing | −0.45 (0.92) | 0.17 (0.98) | <0.001 | 0.65 |
| Anxiety | 44.94 (9.53) | 51.50 (11.13) | <0.001 | 0.63 |
| Depression | 44.94 (6.82) | 47.79 (8.92) | 0.003 | 0.36 |
Mean values (SD) are shown unless otherwise noted.
IBS, irritable bowel syndrome; HRQOL, health-related quality-of-life
Multiple linear regression modeling determined which of the abdominal pain and psychosocial distress measures was most strongly associated with HRQOL outcomes. Collinearity was present for abdominal pain intensity (VIF=7.20 in Physical and Psychosocial HRQOL models) and pain interference (VIF=4.08 in the Physical and Psychosocial HRQOL models) in the HC group. Pain interference was therefore removed from all analyses because this measure notably overlapped with functional disability. After elimination of pain interference from all analyses, problematic multicollinearity among the remaining abdominal pain and psychosocial distress measures was no longer present.
The multivariate linear regression models predicting Physical HRQOL revealed that somatization (standardized β −0.55, p < 0.001) was the strongest predictor in the HC group (Table 2). For IBS, functional disability was the strongest predictor of Physical HRQOL (standardized β −0.37, p < 0.001), while somatization was also significantly predictive (standardized β −0.27, p < 0.001; Table 2).
Table 2.
Multivariate Linear Regression Models of Abdominal Pain and Psychosocial Distress Measures Predicting Physical Health-Related Quality-of-Life
| Healthy Control Group | |||
|---|---|---|---|
| Abdominal Pain and Psychosocial Distress Measures | Unstandardized B (95% CI) | Standardized β | P value |
| Pain Frequency | −2.15(−7.68 – 3.38) | −0.11 | 0.44 |
| Pain Intensity | 0.20 (−1.51 – 1.92) | 0.03 | 0.81 |
| Somatization | −0.49 (−0.68 – −0.30) | −0.55 | <0.001 |
| Functional Disability | −0.37 (−0.71 – −0.02) | −0.20 | 0.04 |
| Pain Catastrophizing | 0.35 (−2.01 – 2.71) | 0.03 | 0.77 |
| Anxiety | −0.07 (−0.33 – 0.20) | −0.06 | 0.62 |
| Depression | −0.13 (−0.49 – 0.22) | −0.08 | 0.46 |
| Coefficient of Multiple Determination (R2) | 0.57 | ||
| IBS Group | |||
| Pain Frequency | −0.02 (−0.23 – 0.19) | −0.01 | 0.83 |
| Pain Intensity | 1.91 (0.34 – 3.48) | 0.13 | 0.02 |
| Somatization | −0.28 (−0.42 – −0.15) | −0.27 | <0.001 |
| Functional Disability | −0.72 (−0.96 – −0.49) | −0.37 | <0.001 |
| Pain Catastrophizing | −2.61 (−4.97 – −0.24) | −0.14 | 0.03 |
| Anxiety | −0.05 (−0.27 – 0.17) | −0.03 | 0.67 |
| Depression | −0.16 (−0.42 – 0.11) | −0.08 | 0.25 |
| Coefficient of Multiple Determination (R2) | 0.48 | ||
Covariate includes age, gender, and race/ethnicity
Bold is the strongest relative measures(s) in the respective model.
CI, confidence interval; IBS, irritable bowel syndrome
With respect to psychosocial HRQOL for the HC group, both somatization and depression were significant predictors, and equally so ([both measures standardized β −0.43, p < 0.001]; Table 3). For the IBS group, somatization was the strongest predictor of psychosocial HRQOL (standardized β −0.28, p < 0.001). Other psychosocial distress measures that significantly predicted psychosocial HRQOL in the IBS group included anxiety (standardized β −0.27, p < 0.001), depression (standardized β −0.23, p < 0.001), and functional disability (standardized β −0.22, p < 0.001).
Table 3.
Multivariate Linear Regression Models of Abdominal Pain and Psychosocial Distress Measures Predicting Psychosocial Health-Related Quality-of-Life
| Healthy Control Group | |||
|---|---|---|---|
| Abdominal Pain and Psychosocial Distress Measures | Unstandardized B (95% CI) | Standardized β | P value |
| Pain Frequency | 2.08 (−3.24 – 7.40) | 0.08 | 0.44 |
| Pain Intensity | −1.01 (−2.65 – 0.64) | −0.13 | 0.23 |
| Somatization | −0.49 (−0.68 – −0.31) | −0.43 | <0.001 |
| Functional Disability | −0.10 (−0.43 – 0.23) | −0.04 | 0.56 |
| Pain Catastrophizing | 2.36 (0.09 – 4.63) | 0.15 | 0.04 |
| Anxiety | −0.31 (−0.57 – −0.05) | −0.20 | 0.02 |
| Depression | −0.91 (−1.26 – −0.57) | −0.43 | <0.001 |
| Coefficient of Multiple Determination (R2) | 0.76 | ||
| IBS Group | |||
| Pain Frequency | −0.04 (−0.19 – 0.12) | −0.02 | 0.66 |
| Pain Intensity | 0.53 (−0.65 – 1.70) | 0.04 | 0.38 |
| Somatization | −0.26 (−0.36 – −0.16) | −0.28 | <0.001 |
| Functional Disability | −0.39 (−0.57 – −0.21) | −0.22 | <0.001 |
| Pain Catastrophizing | −0.98 (−2.76 – 0.79) | −0.06 | 0.28 |
| Anxiety | −0.40 (−0.57 – −0.23) | −0.27 | <0.001 |
| Depression | −0.43 (−0.63 – −0.23) | −0.23 | <0.001 |
| Coefficient of Multiple Determination (R2) | 0.63 | ||
Covariate includes age, gender, and race/ethnicity
Bold is the strongest relative predictor(s) in the respective model.
CI, confidence interval; IBS, irritable bowel syndrome
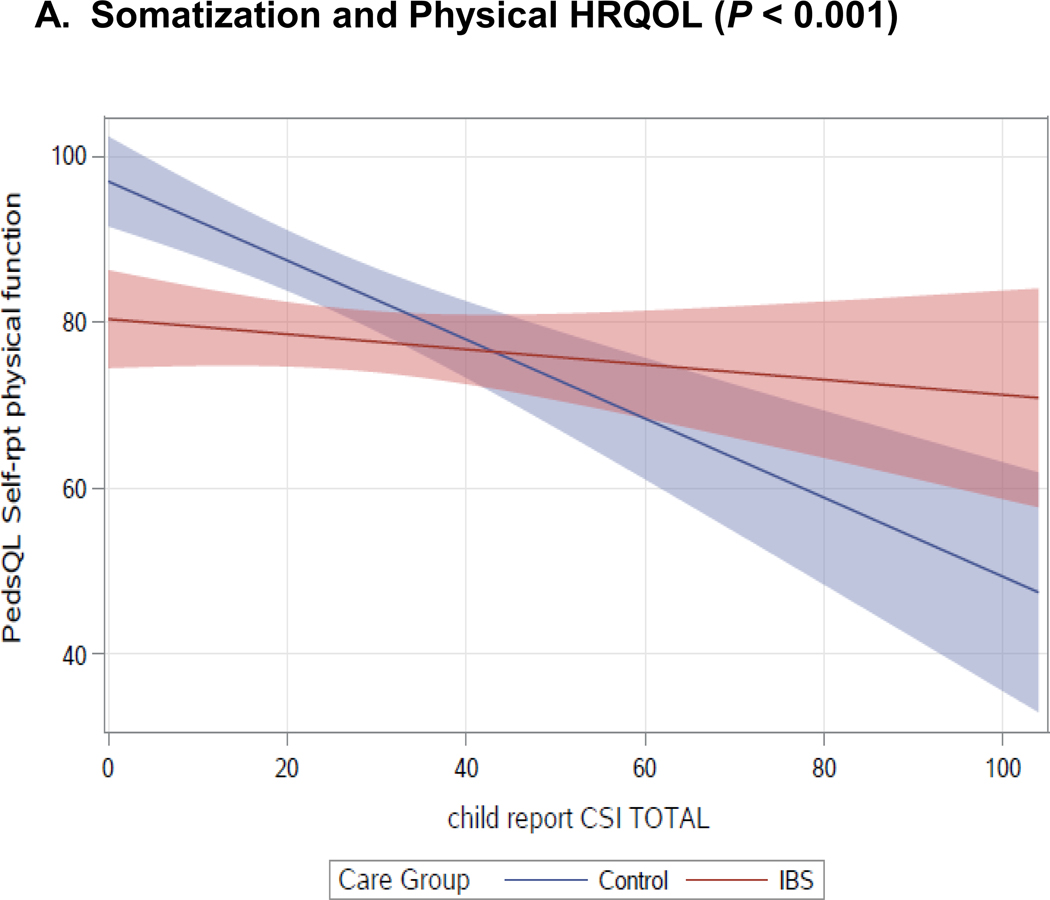
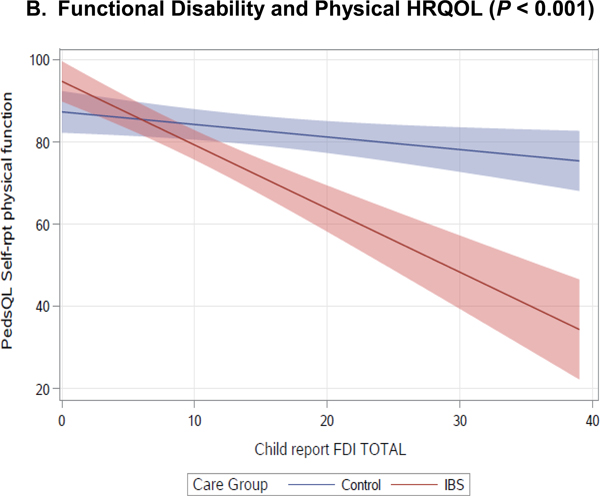
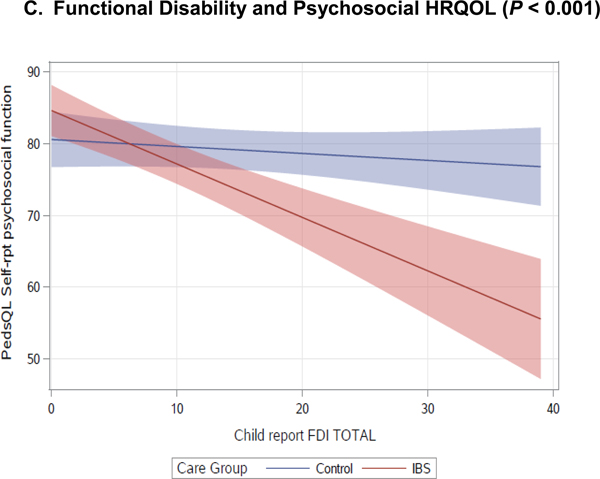
Finally, interaction analyses assessed group differences (HC vs IBS) in the associations of abdominal pain and psychosocial distress with Physical and Psychosocial HRQOL. Results revealed that the relationship between Physical HRQOL and both somatization and functional disability differed between HC and IBS groups. The association between psychosocial HRQOL and functional disability also differed between sample groups (Table 4). Figure 1 demonstrates these findings by illustrating the slope of the lines for the respective sample groups. Specifically, Figure 1A illustrates a larger reduction in Physical HRQOL as somatization increases for the HC group, whereas this reduction is less pronounced for those with IBS. Physical HRQOL (Figure 1B) and psychosocial HRQOL (Figure 1C) become poorer as functional disability increases for both the HC and IBS groups, but this is more pronounced in the IBS group.
Table 4.
Interaction P-values of Healthy Controls vs Irritable Bowel Syndrome Associations between Abdominal Pain and Psychosocial Distress Measures with Physical and Psychosocial Health-Related Quality-of-Life
| Abdominal Pain and Psychosocial Distress Measures | Physical HRQOL, P value | Psychosocial HRQOL, P value |
|---|---|---|
| Pain Frequency | 0.68 | 0.61 |
| Mean Pain Intensity | 0.93 | 0.57 |
| Somatization | <0.001 | 0.57 |
| Functional Disability | <0.001 | <0.001 |
| Pain Catastrophizing | 0.20 | 0.44 |
| Anxiety | 0.36 | 0.14 |
| Depression | 0.80 | 0.04 |
IBS, irritable bowel syndrome; HRQOL, health-related quality of life
Figure 1.
Linear Regression Models Comparing the Associations between Somatization and Functional Disability with Physical and Psychosocial Health-Related Quality-of-Life by Healthy Control and Irritable Bowel Syndrome Groups
CSI, Children’s Somatization Inventory; FDI, Functional Disability Inventory; HRQOL, health-related quality-of-life
DISCUSSION
This study explored the relative association of abdominal pain and psychosocial distress measures with HRQOL in a well-characterized cohort of children with IBS, while also exploring whether the nature of these relationships differed from HC. Our study compared the magnitude of the associations among an array of measures and HRQOL, which to our knowledge, is novel in a pediatric IBS population. In contrast to findings in adults,27 our results indicate that abdominal pain intensity and frequency are not strongly associated with HRQOL in children with IBS as compared with psychosocial distress46, suggesting that psychosocial factors may be a more impactful treatment target.
As would be expected, children with IBS experienced more abdominal pain, more psychosocial distress and reduced Physical and Psychosocial HRQOL compared to HC (Table 1). Poor Physical HRQOL was consistently associated with increased somatization for both HC and IBS participants. In fact among the multiple psychosocial distress measures, only somatization was significantly associated with Physical HRQOL in our analyses. Adult studies have also noted a significant association between somatization and HRQOL in IBS and HC27, as well as a better response to behavioral health interventions for those with IBS who have higher somatization.47 Our previous work also suggested a significant role of somatization in predicting both abdominal pain frequency37 and maintenance of pain in children with chronic abdominal pain.48 As such, referral for behavioral intervention like cognitive behavioral therapy, to address childhood somatization and its management by parents is an important consideration in the clinical management of pediatric IBS.
This study also compared differences between HC and children with IBS in the associations of Physical and Psychosocial HRQOL with various abdominal pain and psychosocial distress measures (Table 4). The role of somatization negatively impacting Physical HRQOL more strongly for HC than for IBS is a novel finding. Though our HC participants were thoroughly vetted by chart review and a 2-week abdominal pain and stooling diary, this sample may have other symptoms/diseases that may affect their Physical HRQOL. Perhaps these other conditions could play a role in why somatization is associated with Physical HRQOL. Further work is needed to discern whether somatization is a viable therapeutic target for those children without IBS who have decreased Physical HRQOL.
The role of functional disability was significantly different between HC and IBS groups for both Physical and Psychosocial HRQOL (Table 4 and Figures 1B and 1C), with functional disability having a greater negative impact on HRQOL for IBS. This same relationship has been observed in other adult chronic pain conditions such as rheumatoid arthritis, fibromyalgia, and back pain.49–51 These results again indicate that targeting the impact of symptoms on daily life through behavioral interventions, rather than a focus on ameliorating physical symptoms themselves, may be the more beneficial approach.
Limitations of the study include the cross-sectional nature of these data, resulting in the inability to determine direction of causation between the abdominal pain and psychosocial distress measures and both of the HRQOL outcomes. In addition, the created pain catastrophizing measure has not been validated, though the questions utilized were derived from two validated measures. Lastly, this study did not include a control group with abdominal pain attributed to an organic condition like inflammatory bowel disease or gastroesophageal reflux disease. Therefore, we cannot conclude that our study findings are unique for children with IBS and future studies should consider such a control group for comparison.
Strengths of the study include examining a diverse set of abdominal pain and psychosocial distress measures as they related to HRQOL. In addition, the sample size is relatively large and importantly, characterization of the cohort (HC vs IBS) was conducted using validated prospective diaries and our previously published algorithm that separates IBS from functional abdominal pain and non-IBS healthy controls.2, 29–33
In summary, our results indicate that despite greater abdominal pain and psychological distress in children with IBS relative to healthy children, only a few specific psychosocial distress measures are associated with lower Physical and Psychosocial HRQOL. Treatments targeting somatization and functional disability could improve HRQOL and may decrease morbidity in children with IBS.
Supplementary Material
Acknowledgments
Funding Source: This project was supported by a NIH Career Development Award K23 DK120928 to JMH; R01 NR013497, NR005337, RC2 NR013497 to RJS, Texas Medical Center Digestive Diseases Center (NIH P30 DK0563389), and the US Department of Agriculture/ARS under Cooperative Agreement 6250-51000-043. The contents of this publication do not necessarily reflect the views or policies of the USDA, nor does mention of trade names, commercial products, or organizations imply endorsement from the US Government.
Footnotes
Conflict of Interest: Dr. Varni holds the copyright and trademark of the Pediatrics Quality of Life Inventory™ (PedsQL) and receives compensation from the Mapi Research Trust, which is a nonprofit research institute that charges distribution fees to for-profit companies that use the PedsQL. There are no other conflicts of research relevant to this study.
Literature Cited
- 1.Hyams JS, Di Lorenzo C, Saps M, et al. Childhood Functional Gastrointestinal Disorders: Child/Adolescent. Gastroenterology. 2016;150:1456–1468.e1452. [Google Scholar]
- 2.Rasquin A, Di Lorenzo C, Forbes D, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130:1527–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korterink JJ, Diederen K, Benninga MA, et al. Epidemiology of pediatric functional abdominal pain disorders: a meta-analysis. PLoS One. 2015;10:e0126982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Apley J and Hale B. Children with recurrent abdominal pain: how do they grow up? Br Med J. 1973;3:7–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christensen MF and Mortensen O. Long-term prognosis in children with recurrent abdominal pain. Arch Dis Child. 1975;50:110–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Magni G, Pierri M and Donzelli F. Recurrent abdominal pain in children: a long term follow-up. Eur J Pediatr. 1987;146:72–74. [DOI] [PubMed] [Google Scholar]
- 7.Miele E, Simeone D, Marino A, et al. Functional gastrointestinal disorders in children: an Italian prospective survey. Pediatrics. 2004;114:73–78. [DOI] [PubMed] [Google Scholar]
- 8.Walker LS, Guite JW, Duke M, et al. Recurrent abdominal pain: a potential precursor of irritable bowel syndrome in adolescents and young adults. J Pediatr. 1998;132:1010–1015. [DOI] [PubMed] [Google Scholar]
- 9.Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500–1511. [DOI] [PubMed] [Google Scholar]
- 10.Drossman DA. Functional abdominal pain syndrome. Clin Gastroenterol Hepatol. 2004;2:353–365. [DOI] [PubMed] [Google Scholar]
- 11.Mohammad S, Di Lorenzo C, Youssef NN, et al. Assessment of abdominal pain through global outcomes and recent FDA recommendations in children: are we ready for change? J Pediatr Gastroenterol Nutr. 2014;58:46–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lipscomb J, Gotay CC and Snyder C. Outcomes assessment in cancer. Cambridge, UK; New York: Cambridge University Press; 2005. [Google Scholar]
- 13.Varni JW, Bendo CB, Nurko S, et al. Health-related quality of life in pediatric patients with functional and organic gastrointestinal diseases. J Pediatr. 2015;166:85–90. [DOI] [PubMed] [Google Scholar]
- 14.Youssef NN, Murphy TG, Langseder AL, et al. Quality of life for children with functional abdominal pain: a comparison study of patients’ and parents’ perceptions. Pediatrics. 2006;117:54–59. [DOI] [PubMed] [Google Scholar]
- 15.Whelan K, Martin LD, Staudacher HM, et al. The low FODMAP diet in the management of irritable bowel syndrome: an evidence-based review of FODMAP restriction, reintroduction and personalisation in clinical practice. J Hum Nutr Diet. 2018;31:239–255. [DOI] [PubMed] [Google Scholar]
- 16.Cong X, Ramesh D, Perry M, et al. Pain self-management plus nurse-led support in young adults with irritable bowel syndrome: Study protocol for a pilot randomized control trial. Res Nurs Health. 2018;41:121–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park JM, Choi MG, Kim YS, et al. Quality of life of patients with irritable bowel syndrome in Korea. Qual Life Res. 2009;18:435–446. [DOI] [PubMed] [Google Scholar]
- 18.Wang YT, Lim HY, Tai D, et al. The impact of irritable bowel syndrome on health-related quality of life: a Singapore perspective. BMC Gastroenterol. 2012;12:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Midenfjord I, Polster A, Sjovall H, et al. Anxiety and depression in irritable bowel syndrome: Exploring the interaction with other symptoms and pathophysiology using multivariate analyses. Neurogastroenterol Motil. 2019;31:e13619. [DOI] [PubMed] [Google Scholar]
- 20.Simren M, Tornblom H, Palsson OS, et al. Cumulative Effects of Psychologic Distress, Visceral Hypersensitivity, and Abnormal Transit on Patient-reported Outcomes in Irritable Bowel Syndrome. Gastroenterology. 2019;157:391–402 e392. [DOI] [PubMed] [Google Scholar]
- 21.Varni JW, Shulman RJ, Self MM, et al. Symptom Profiles in Patients With Irritable Bowel Syndrome or Functional Abdominal Pain Compared With Healthy Controls. J Pediatr Gastroenterol Nutr. 2015;61:323–329. [DOI] [PubMed] [Google Scholar]
- 22.Leung L Pain catastrophizing: an updated review. Indian J Psychol Med. 2012;34:204–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quartana PJ, Campbell CM and Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009;9:745–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller MM, Meints SM and Hirsh AT. Catastrophizing, pain, and functional outcomes for children with chronic pain: a meta-analytic review. Pain. 2018;159:2442–2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams AE, Czyzewski DI, Self MM, et al. Are child anxiety and somatization associated with pain in pain-related functional gastrointestinal disorders? Journal of health psychology. 2015;20:369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vu J, Kushnir V, Cassell B, et al. The impact of psychiatric and extraintestinal comorbidity on quality of life and bowel symptom burden in functional GI disorders. Neurogastroenterol Motil. 2014;26:1323–1332. [DOI] [PubMed] [Google Scholar]
- 27.Addante R, Naliboff B, Shih W, et al. Predictors of Health-related Quality of Life in Irritable Bowel Syndrome Patients Compared With Healthy Individuals. J Clin Gastroenterol. 2019;53:e142–e149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shulman RJ, Eakin MN, Jarrett M, et al. Characteristics of pain and stooling in children with recurrent abdominal pain. J Pediatr Gastroenterol Nutr. 2007;44:203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Czyzewski DI, Lane MM, Weidler EM, et al. The interpretation of Rome III criteria and method of assessment affect the irritable bowel syndrome classification of children. Aliment Pharmacol Ther. 2011;33:403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lane MM, Czyzewski DI, Chumpitazi BP, et al. Reliability and validity of a modified Bristol Stool Form Scale for children. J Pediatr. 2011;159:437–441 e431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.von Baeyer CL, Spagrud LJ, McCormick JC, et al. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children’s self-reports of pain intensity. Pain. 2009;143:223–227. [DOI] [PubMed] [Google Scholar]
- 32.Ragnarsson G and Bodemar G. Division of the irritable bowel syndrome into subgroups on the basis of daily recorded symptoms in two outpatients samples. Scand J Gastroenterol. 1999;34:993–1000. [DOI] [PubMed] [Google Scholar]
- 33.Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. [DOI] [PubMed] [Google Scholar]
- 34.Varni JW, Seid M and Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–812. [DOI] [PubMed] [Google Scholar]
- 35.Walker LS and Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. J Pediatr Psychol. 1991;16:39–58. [DOI] [PubMed] [Google Scholar]
- 36.Claar RL and Walker LS. Functional assessment of pediatric pain patients: psychometric properties of the functional disability inventory. Pain. 2006;121:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hollier JM, van Tilburg MAL, Liu Y, et al. Multiple psychological factors predict abdominal pain severity in children with irritable bowel syndrome. Neurogastroenterol Motil. 2019;31:e13509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Crombez G, Bijttebier P, Eccleston C, et al. The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. PAIN. 2003;104:639–646. [DOI] [PubMed] [Google Scholar]
- 39.Pielech M, Ryan M, Logan D, et al. Pain catastrophizing in children with chronic pain and their parents: Proposed clinical reference points and reexamination of the Pain Catastrophizing Scale measure. PAIN®. 2014;155:2360–2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Walker LS, Smith CA, Garber J, et al. Development and validation of the Pain Response Inventory for children. Psychological Assessment. 1997;9:392–405. [Google Scholar]
- 41.Stone AL, Walker LS, Laird KT, et al. Pediatric Pain Beliefs Questionnaire: Psychometric Properties of the Short Form. The Journal of Pain. 2016;17:1036–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reynolds CR and Kamphaus RW. BASC-2: Behavior Assessment System for Children Second Edition Manual. Circle Pines, MN: AGS Publishing; 2004. [Google Scholar]
- 43.Garber J, Walker LS and Zeman J. Somatization symptoms in a community sample of children and adolescents: Further validation of the Children’s Somatization Inventory. Psychological Assessment. 1991;3. [Google Scholar]
- 44.Derogatis LR, Lipman RS, Rickels K, et al. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19:1–15. [DOI] [PubMed] [Google Scholar]
- 45.Noble WS. How does multiple testing correction work? Nat Biotechnol. 2009;27:1135–1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Tilburg MA, Claar RL, Romano JM, et al. Role of Coping With Symptoms in Depression and Disability: Comparison Between Inflammatory Bowel Disease and Abdominal Pain. J Pediatr Gastroenterol Nutr. 2015;61:431–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Riehl ME, Kinnucan JA, Chey WD, et al. Nuances of the psychogastroenterology patient: A predictive model for gastrointestinal quality of life improvement. Neurogastroenterol Motil. 2019:e13663. [DOI] [PubMed] [Google Scholar]
- 48.Williams AE, Czyzewski DI, Self MM, et al. Are child anxiety and somatization associated with pain in pain-related functional gastrointestinal disorders? J Health Psychol. 2015;20:369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Manca A, Eldabe S, Buchser E, et al. Relationship between health-related quality of life, pain, and functional disability in neuropathic pain patients with failed back surgery syndrome. Value Health. 2010;13:95–102. [DOI] [PubMed] [Google Scholar]
- 50.Kurtze N, Gundersen KT and Svebak S. Quality of life, functional disability and lifestyle among subgroups of fibromyalgia patients: the significance of anxiety and depression. Br J Med Psychol. 1999;72 ( Pt 4):471–484. [DOI] [PubMed] [Google Scholar]
- 51.Guillemin F Functional disability and quality-of-life assessment in clinical practice. Rheumatology (Oxford). 2000;39 Suppl 1:17–23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.