Abstract
Background
Outpatient heart failure (HF) care involves intensive self-management (SM). Effective HF SM is associated with improved outcomes. Homelessness poses challenges to successful SM.
Objectives
To identify the ways in which homelessness may impede successful SM of HF and engagement with the healthcare system.
Methods
We conducted open-ended, semi-structured interviews with homeless adults with HF. Data were analyzed by a multidisciplinary team using a grounded theory approach.
Results
We interviewed 19 participants, 11 (58%) of whom were homeless at the time of interview. Interviews revealed a combination of influences on HF SM. Major themes included instability and lack of routine, tradeoffs between basic necessities and HF SM, and stigmatization by healthcare providers.
Conclusions
Anticipatory guidance aimed at the unique challenges faced by homeless individuals with HF may aid successful SM. HF providers should simplify medication regimes and engage in non-stigmatizing discourse. Larger-scale interventions include the creation of medical respite programs.
Keywords: heart failure, qualitative methods, social determinants, homelessness, health services research
Background
More than half a million people are homeless on any given night in the United States, and in several U.S. states, the number of homeless individuals is increasing.1 Cardiovascular disease (CVD) is a major cause of death among homeless adults. Mortality rates from CVD among the homeless are 2–3 fold higher than in the general population.2 Homeless individuals face a host of issues that may impact CVD mortality. These include concurrent mental illness, difficulty or delay in diagnosing CVD (e.g., due to lack of regular preventive care), and care fragmentation.3
Heart failure (HF) affects more than six million individuals in the United States, and its prevalence is rising.4 Outpatient HF care involves intensive self-management (SM): individuals with HF are expected to monitor weight gain, modulate dietary intake, adhere to complex medication regimens, and actively engage with nurses and physicians regarding their care.5 Improved HF SM is associated with improved HF outcomes,6 but for many patients, the complexity of SM behaviors makes it difficult to avoid exacerbations and readmission.7,8 A growing body of literature documents the challenges faced by homeless individuals in SM of chronic conditions such as diabetes mellitus, including difficulties with health prioritization and expenses.9 To our knowledge, no studies have examined the experiences of homeless individuals with HF. Given the rising prevalence of both homelessness and HF in the U.S., healthcare providers will increasingly encounter such patients in their clinical practice. Characterizing the experiences and perspectives of homeless persons with HF is critical to improving care for this vulnerable population.
To address these gaps in knowledge, we interviewed individuals 18 years and older who had experienced homelessness and been diagnosed with HF by a healthcare provider. We asked them to describe their experiences, including challenges they faced in prioritizing SM of HF, as well as interactions with healthcare providers and the healthcare system. We sought to identify their perspective on ways in which homelessness may impede successful SM of HF and engagement with the healthcare system.
Methods
Study Design and Sample
We conducted a qualitative study of individuals experiencing homelessness age 18 years and older who had been diagnosed with HF, based on standard clinical criteria,10 by a healthcare provider. We chose a qualitative approach, as we wished to describe complex phenomena that are challenging to measure using quantitative techniques.11 The use of qualitative methods in cardiovascular research is increasing, as health services researchers are beginning to recognize the unique contributions that such methods may provide in adding to our understanding of patients’ experiences with SM of chronic disease.12
The setting for our study was New Haven, Connecticut, a mid-sized city in the Northeastern United States. New Haven, like much of the U.S., suffers from a shortage of affordable housing. In 2018, Connecticut had the 9th highest housing wage (the hourly wage required to rent a 2-bedroom apartment without spending more than 30% of one’s income) in the US.13 Between 2017 and 2018, Connecticut experienced the second-largest percentage increase in the entire U.S. in the number of people experiencing homelessness.1
We used purposive sampling techniques to recruit participants from a variety of settings. We posted flyers throughout the city of New Haven (at public libraries, homeless shelters, social service offices, and other community organizations). In addition, in accordance with the principles of community-engaged research (CEnR), we engaged key stakeholders within the New Haven community to recruit participants.14 These included social workers at Yale-New Haven Hospital, Yale School of Medicine’s community research liaison, executive leadership at one of the city’s homeless shelters, and healthcare providers who treat homeless individuals within the shelter system as well as at one of New Haven’s federally qualified health centers (FQHCs).
In defining eligibility, we used the definition of homelessness provided by the Health Resources and Services Administration (HRSA) and used by many academic and policy organizations: “a homeless person is an individual without permanent housing who may live on the streets; stay in a shelter, mission, single room occupancy facilities, abandoned building or vehicle; or in any other unstable or nonpermanent situation.”15
We included participants in our study if they had experienced homelessness at any time following HF diagnosis. HF diagnosis was verified using Yale-New Haven Health’s electronic health record (EHR), which is shared by Yale-New Haven Hospital (the sole hospital within the City of New Haven, containing over 1500 beds16), its outpatient clinics, and New Haven’s FQHCs. HF diagnosis could thus have been made in a variety of clinical settings.
Data Collection and Measures
Between May 2018 and June 2019, the lead author conducted in-depth, in-person interviews consisting of open-ended, non-directive questions (Appendix). Interviews were conducted in settings of participants’ choosing, including public spaces such as the city library and municipal park, hospital rooms (with participants that were hospitalized at the time of interview), homeless shelters, and, for participants who had successfully transitioned from homelessness to stable housing, in their own residences.
The purpose of the interviews was to elicit individual perceptions and experiences regarding HF SM in the context of homelessness. After a thorough review of the literature, domains of inquiry were developed with the expertise of an interdisciplinary research team (two physicians with clinical and research expertise in cardiology [A.P. and E.S.], a public health researcher with research knowledge in homelessness, chronic disease SM, and qualitative methods [D.E.K.], a physician with research expertise in qualitative methods and CEnR [M.S.R.], and a community leader with two decades of experience in homeless services [A.C.]).
Interviews contained follow-up questions, known as probes, used to clarify or elaborate on participants’ responses.17 In keeping with a grounded theory approach,18 we collected data and conducted analyses in an iterative, ongoing manner, with the two processes taking place concurrently. To account for emerging themes, we continued to refine our interview guide as we conducted further interviews and analysis. We used the EHR to document participants’ age, sex, self-reported race, HF type (i.e., HF with reduced versus preserved ejection fraction), number of prior HF hospitalizations, and names and dosages of all guideline-directed HF medications. At the end of each interview, we also inquired about participants’ monthly income, including state-sponsored financial assistance.
We determined the size of our final sample according to the principle of thematic saturation, defined as the point at which novel themes or information ceased to emerge after sequential interviews.19 We achieved saturation after completion of 15 interviews, and then completed additional interviews to ensure that saturation was not determined prematurely.
The lead author conducted every interview. Interviews averaged 57 minutes in length. All interviews were digitally recorded and transcribed by a professional transcription service. The lead author reviewed each interview transcript to ensure transcription accuracy. The Yale University Institutional Review Board approved this study. All participants provided signed informed consent for their participation in this study.
Data Analysis
All 19 transcripts were initially coded independently by two team members (A.P. and M.S.R.). Selected transcripts were also independently read by E.S., A.C., D.B., and D.E.K.. Consistent with a grounded theory approach, our research team analyzed interview transcripts through an iterative and multi-stage coding process. We assigned codes to specific quotes, and, after reviewing the first few transcripts, we formulated an initial coding structure. As we conducted more interviews, we constantly compared sections of these transcripts with those that had been coded previously, to refine and develop concepts and to ensure uniform coding. We continued to refine our coding structure until no new concepts emerged.
Our analysis team consisted of researchers from diverse backgrounds, including cardiology, qualitative methodology, public health, and health services research. In addition, in keeping with the principles of CEnR and to add greater depth and context to our analysis,14 one member of our research team was a longtime resident of New Haven with personal experience of homelessness and chronic disease (D.B.), and another was executive director of Columbus House, Inc., an organization providing temporary shelter, transitional housing, medical respite services, and employment training to homeless individuals in New Haven (A.C.).
Through multiple group sessions, in order to ensure scientific rigor, we discussed applications of codes in an ongoing manner, reconciling differences in coding via negotiated consensus and checking our interpretations against each other’s and the data. The final coding structure that resulted from this process contained six primary codes capturing major categories, each with several subcodes capturing secondary concepts. We then used the coded data to develop themes in an established manner.20 We used Dedoose software (Version 8.2, SocioCultural Research Consultants, LLC, Los Angeles, CA) to facilitate data organization and retrieval.
Results
Participant Characteristics
Our sample included 19 individuals with a mean age of 56 years (range, 34–72; Table 1). The majority of participants were male (14, 74%). Eleven individuals (58%) were homeless at the time of interview. Nearly half of our sample self-identified as black (47%), 47% had a diagnosis of heart failure with reduced ejection fraction, and 100% reported Medicaid as their primary form of insurance. Mean number of prior HF hospitalizations was 8 (range, 0–37).
Table 1:
Participant characteristics (n = 19)
| Sex | |
| Male | 14 (74) |
| Female | 5 (26) |
| Race | |
| Black | 9 (47) |
| White | 9 (47) |
| Latino | 1 (5) |
| Age (years) | |
| Mean | 56 |
| Range | 34–72 |
| Homeless at time of interview | 11 (58) |
| HF type | |
| HFrEF | 9 (47) |
| HFpEF | 10 (53) |
| No. of prior HF hospitalizations | |
| Mean | 8 |
| Range | 0–37 |
| Participants with HFrEF prescribed GDMT | |
| BB | 9 (100) |
| ACEi/ARB/ARNi | 6 (67) |
| MRA | 5 (56) |
| Primary insurance | |
| Medicaid | 19 (100) |
| Monthly income (dollars) | |
| Mean | 780 |
| Range | 0–1379 |
Data are reported as n (%) unless otherwise specified. Abbreviations: HFrEF = heart failure with reduced ejection fraction, HFpEF = heart failure with preserved ejection fraction, GDMT = guideline-directed medical therapy, BB = beta blocker, ACEi = angiotensin converting enzyme inhibitor, ARB = angiotensin receptor blocker, ARNi = angiotensin II receptor blocker-neprilysin inhibitor, MRA = mineralocorticoid receptor antagonist. Percentages may not add up to 100% due to rounding.
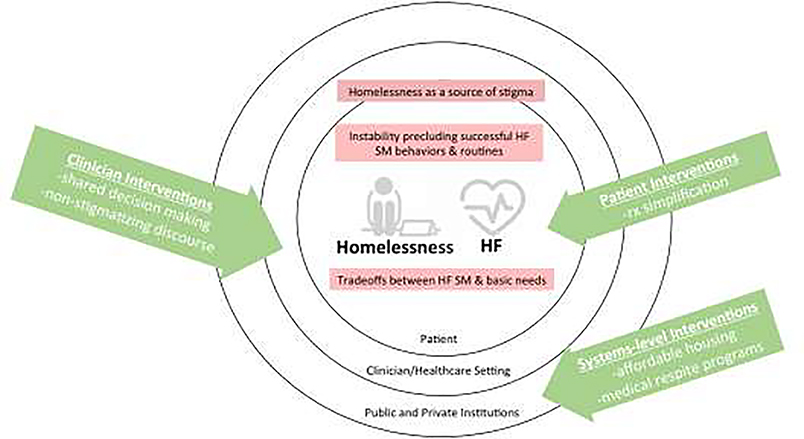
Three themes characterized the experiences of participants with HF and homelessness (Figure): instability, tradeoffs, and stigma.
Figure.
Three themes characterizing participants’ experiences with HF SM in the context of homelessness, along with possible sites of intervention.
Theme 1: Instability Due to Homelessness Impedes Successful HF SM Behaviors and Routines
The pervasive sense of instability that informed participants’ day-to-day experiences rendered them unable to engage in successful HF SM behaviors. As one participant described:
I was missing appointments because I had no transportation. I was missing appointments because I had nowhere to sleep at night…Wherever [I am] I carry a [tote bag] with my medicine in it…I’ll leave my tote bag there...I won’t come back for three, four days…Then when I go back, ‘Oh man, my medicine’…All my possessions got sold from the eviction warehouse. All my possessions got sold. Sleep apnea machine…Medicines, clothes, everything. (Participant 2, male, age 52)
In particular, difficulty establishing and maintaining SM routines was a common sentiment among participants. Many participants noted challenges with medication routines:
It’s hard to take the medication when you’re out there…You can’t make it to pharmacies…I take 12 different types of medications. Seven of them you have to have with food. So hence, the other four or five, I won’t even take…Actually, the only ones I would take is the torsemide and spironolactone so I can get...the [fluid] off of me. But the rest I won’t even take. (Participant 5, male, age 51)
Participants also described difficulties with other types of routinized HF SM behaviors, such as measuring daily weights:
I was in a room with 12 people…I didn’t have a scale…because you had to carry [the scale] every night to your bed, and you had to carry everything every morning back to the closet to lock it up for the day, so that could be difficult…because when I got out of the hospital I was really weak. (Participant 4, female, age 54)
Participants who were discharged to a medical respite program, however, described how respite provided structure and environmental constancy, emerging as a crucial source of stability and routine formation:
And now when I was in the medical respite, I had my meds with me, and the visiting nurses set me up with a box, Monday through Friday… [In medical respite] there’s a dresser in the room, the scale is right next to the dresser. First thing when I got up, the first thing I did was weigh myself, so that was every day, and I keep a record of it. (Participant 1, male, age 51)
Theme 2: Homelessness Creates Difficult Tradeoffs Between Basic Necessities and HF SM
Participants described difficult trade-offs between basic necessities and health needs. For many, the challenges of securing shelter took precedence over HF SM. As one participant noted:
When you get homeless…you have to think…’Where can I go close my eyes because I messed around and didn’t get to the shelter in time?…I got to go sit in one of the bus stop things and try to get me some sleep or kick back, get out of…the rain or snow’…[HF] is the last thing on your mind until you end up…the ambulance is picking you up, taking you to the hospital. Then that’s when…like, ‘Wow. I should’ve been taking care of myself.’ (Participant 12, male, age 61)
Another way in which participants described tradeoffs was by prioritizing “short-term thinking,” as opposed to planning for the future and making durable investments in their well-being. One participant explained it as follows:
…Meeting [the cardiologist] is important but it’s not as important as going to get that couple dollars to help sustain me for a couple of days. Now in reality, that’s a wrong decision. Because you could be a guy that could set me up on something better, something more long-term, something more stable…Sometimes when you’re thinking on the fly, you make the wrong decisions…This conversation might help me in the long run, but it ain’t going to get me nothing to eat tonight. It ain’t going to get me somewhere warm to stay tonight. It ain’t going to put no gas in this raggedy-ass car that won’t run…Thinking on the fly, sometimes you make the wrong decisions. (Participant 13, male, age 43)
Here, similar to its role in attenuating instability, the medical respite program again served a vital role for participants in our sample. A participant described how medical respite allowed him to view his health holistically, freeing him to make beneficial long-term decisions alongside engaging in successful HF SM:
When they sent me [to medical respite], I had a chance to save my money piece by piece. I didn’t need to do anything with it…it was helping with the savings. People were real nice. They got me on a regimen of taking my medication. Got me doing it right. They had me back and forth to appointments…I was making all my appointments. I was actually doing the medication, eating right, things like that. Changed…Feeling great. (Participant 5, male, age 51)
Theme 3: Stigmatization by Healthcare Providers Influences the Experiences of Homeless Individuals With HF Within the Healthcare System
Several participants described homelessness as a source of stigma that informed their interactions with the healthcare system. Even when participants were able to recognize symptoms of worsening HF, concerns about how they would be perceived by medical staff often prevented them from seeking timely HF care. When they did seek care, participants reported that they were treated without dignity:
…In the emergency room, they have no heart. When you’re homeless, they look down on you. The doctors, the nurses, the techs, the staff, period. The social workers were telling me, ‘This is not a hotel. Don’t think you’re gonna live here.’ I’m in heart failure…I’m half dead, and all you’re worried about is saying, ‘This isn’t a hotel.’ How dare you belittle me like that…None of my providers cared…What did they do? Nothing but treat me and send me back to the street. (Participant 16, male, age 58)
Stigma also made some participants hesitant to divulge their housing status to healthcare providers, out of fear that it would result in incomplete or inadequate care. As one participant noted:
I lied. I told my cardiologist that I had a place to live. She wasn’t gonna put in [the pacemaker]. Because I had no place to take care of myself. She wasn’t gonna put it in. I had her convinced that I lived somewhere. She put it in, and I got better….I went home to my tent…And I got scared…So, then, I went back to the hospital…And my daughter came. And told them the truth, that I was homeless. (Participant 6, female, age 64 years)
In contrast, other participants reported that when healthcare providers used non-stigmatizing language and actively inquired about their housing status, it elicited a sense of hope and greater self-efficacy in engaging in HF SM behaviors:
[My cardiologist] went to help me [obtain] assistance through social services and said, ‘He has a serious heart issue. And the fact that he is homeless has created an enormous amount of stress’…[My cardiologist] was the only one that…said, ‘Yes he does need help.’ Once she filled out proper paperwork, or went through channels, I…got a place [to live]…I felt like I was talking to a person and a doctor when I talked to [her]. Some of the other doctors I felt like I was talking to a used car salesman…[My cardiologist] put her foot in the ring, and…it triggered a response out of me that, ‘Okay she really does care.’ (Participant 10, male, age 55)
Discussion
In this qualitative study examining HF SM in the context of homelessness, we found three recurrent themes: difficulty executing successful HF SM behaviors and routines arising from lack of stability; frequent tradeoffs when attempting to prioritize HF SM and basic needs; and stigmatization by providers impacting HF care.
For participants in our sample, homelessness gave rise to a pervasive lack of stability and an inability to establish a daily routine. Routine, especially, plays a central role in successful SM of HF,21–23 and to our knowledge, our work represents the first study to directly address homelessness as a barrier to the formation of routine in HF SM. Many participants in our sample described difficulty in establishing a routine involving HF medications. As new evidence-based treatments have emerged, HF medication regimens have become increasingly complex,24 and prior studies have identified complex drug regimens as a barrier to medication adherence in HF.25–27 This may present an opportunity for HF clinicians caring for homeless individuals: simplifying drug regimens in concert with hospital pharmacists has been associated with improved medication adherence in several chronic conditions, including HF.28,29 Such an approach, when applied to homeless patients with HF, may reduce the treatment burden imposed on this vulnerable population.
Consistent with prior research into the experiences of low-income individuals with chronic illness,30,31 participants also had to engage in difficult tradeoffs. Specifically, participants commonly reported sacrificing HF SM in favor of necessities such as food and shelter. Long-term thinking about personal well-being was similarly supplanted by the need to attend to immediate material concerns. For some participants in our sample, these tradeoffs resulted in HF exacerbation and readmission.
While structured HF education has been shown to reduce risk of readmission,32 such education tends to focus on discrete domains of HF SM such as diet and activity.33 Clinicians, in providing HF education to homeless patients, should be attuned to the specific tradeoffs that these individuals may face. Our results suggest that clinicians may be able to augment routine HF education with anticipatory guidance tailored toward the unique challenges encountered by homeless individuals: for example, by providing instruction regarding diuretic titration or recognition of changes in HF symptomatology in the absence of reliable access to daily weights. Clinicians may also participate in shared decision making that incorporates social determinants of health such as housing.34 By discussing patient values and goals in a manner that takes into account their capacity to act given myriad constraints, providers may enhance homeless individuals’ engagement in successful HF SM.
Finally, participants frequently reported that stigma posed a barrier to successful HF SM. Previous qualitative studies have demonstrated that homeless patients feel “unwelcome,” “excluded,” and “depersonalized” in their encounters with healthcare providers.35–37 In our sample, stigma discouraged participants from seeking care and, at times, compelled them to conceal their housing status. The concept of stigma warrants further attention in the context of homelessness, as it may contribute to delays in the diagnosis and receipt of care for common conditions like HF. And as with other stigmatized conditions such as addiction,38,39 where researchers have recognized the importance of provider language in shaping attitudes and treatment decisions,40 our results suggest that for individuals with HF experiencing homelessness, non-stigmatizing discourse may be used to engender mutual respect and trust and, in the process, bolster their ability to participate in HF SM.
We thus find multiple modes of interaction between HF, homelessness, and SM behaviors, as well as multiple levels of opportunity to improve care for persons with HF experiencing homelessness (Figure). These include solutions involving individual providers and patients, like the ones we outline above. But there are additional, systems-level strategies that may be employed to improve care for this vulnerable population. Clinicians, in recognizing the centrality of housing as a key social determinant of health and the interplay between homelessness and health behaviors, may use their position to advocate for housing affordability and, more specifically, the construction of affordable housing units geared toward homeless patients with chronic disease.
Our results highlight one such effort in particular: the creation of medical respite programs. Municipalities across the country, through public-private parternships, have successfully implemented these medically-supervised environments,41 which are intended for homeless individuals who are too medically complex to stay in a shelter or on the street following hospital discharge. Medical respite units have been associated with lower hospital readmission rates,42,43 and may aid recovery after cardiac procedures.2 Indeed, in our study, participants who had been hospitalized for HF and discharged to medical respite were able to regain a sense of stability, form routines around HF SM behaviors, and experience freedom from difficult tradeoffs.
Limitations
Although our work provides important and novel insights into the experiences of homeless individuals with HF, there are several limitations. Our sample was limited to a single city in the United States; as such, results from our interviews may not reflect the experiences of individuals in other parts of the country. In particular, homeless individuals in states that did not expand Medicaid as part of the Affordable Care Act may experience greater difficulty in gaining insurance coverage and accessing health and social services.44 It is important to note, however, that homelessness and housing unaffordability are nationwide phenomena with structural economic causes,45 affecting cities and states of all sizes.1,13 For those participants who were no longer homeless at the time of interview, recall bias is a possible limitation. We minimized this bias by using extensive probing techniques to elicit a wide variety of factors associated with participant experiences with homelessness and HF SM. In addition, we used several established practices for ensuring rigorous data collection and analysis, including consistent use of the interview guide, digitally recording interviews, independent professional transcription, and uniform coding and analysis of the data.46,47
Conclusions
The prevalence of both homelessness and HF in the U.S. are rising. Understanding potential factors that shape the experiences of individuals with HF and homelessness is essential in creating interventions aimed at fostering successful SM behaviors in this population. Results from this qualitative study provide novel insights into the perceptions and difficulties in SM that homeless persons with HF face, along with potential opportunities for action. To improve outcomes for homeless persons with HF, individual clinicians and patients represent one important target. Concurrently engaging health system leadership and local and state officials to undertake larger-scale interventions, such as the creation of medical respite programs, represents another. Multilevel solutions involving patients, providers, health systems, and local and state authorities are necessary in addressing the growing and linked problems of homelessness and chronic CVD.
Supplementary Material
Highlights.
Heart failure (HF) involves intensive self-management
Homelessness poses a barrier to self-management of HF
Homeless persons with HF face instability, difficult tradeoffs, and stigma
Multilevel solutions are needed to address HF in homeless populations
Acknowledgments
Funding: This work was supported by CTSA Grant Number TL1 TR001864 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH).
Footnotes
Disclosures: The authors have no relationships or competing interests to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Henry M, Mahathey A, Morrill T, Robinson A, Shivji A, Watt R. Abt Associates (2018). The 2018 annual homeless assessment report (AHAR) to Congress. Part 1: Point-in-time estimates of homelessness. Washington, 2018. [Google Scholar]
- 2.Baggett TP, Liauw SS, Hwang SW. Cardiovascular Disease and Homelessness. Journal of the American College of Cardiology. 2018;71(22):2585–2597. [DOI] [PubMed] [Google Scholar]
- 3.Szerlip MI, Szerlip HM. Identification of cardiovascular risk factors in homeless adults. The American Journal of the Medical Sciences. 2002;324(5):243–246. [DOI] [PubMed] [Google Scholar]
- 4.Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics 2018 Update: A Report From the American Heart Association. Circulation. 2018;137(12):e67–e492. [DOI] [PubMed] [Google Scholar]
- 5.Lockhart E, Foreman J, Mase R, Heisler M. Heart failure patients’ experiences of a self-management peer support program: a qualitative study. Heart & Lung. 2014;43(4):292–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovascular Disorders. 2006;6:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dickson VV, Tkacs N, Riegel B. Cognitive influences on self-care decision making in persons with heart failure. American Heart Journal. 2007;154(3):424–431. [DOI] [PubMed] [Google Scholar]
- 8.Dickson VV, Riegel B. Are we teaching what patients need to know? Building skills in heart failure self-care. Heart & Lung. 2009;38(3):253–261. [DOI] [PubMed] [Google Scholar]
- 9.Keene DE, Guo M, Murillo S. “That wasn’t really a place to worry about diabetes”: Housing access and diabetes self-management among low-income adults. Soc Sci Med. 2018;197:71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jessup M, Abraham WT, Casey DE, et al. 2009 Focused Update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults. J Am Coll Cardiol. 2009;53(15):1343–1382. [DOI] [PubMed] [Google Scholar]
- 11.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311(6996):42–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Campbell DJ, Tam-Tham H, Dhaliwal KK, et al. Use of Mixed Methods Research in Research on Coronary Artery Disease, Diabetes Mellitus, and Hypertension: A Scoping Review. Circ Cardiovasc Qual Outcomes. 2017;10(1). [DOI] [PubMed] [Google Scholar]
- 13.Aurand A, Emmanuel D, Yentel D, Errico E, Gaby-Biegel J, Kerr E. Out of reach: the high cost of housing. The National Low Income Housing Coalition. 2018:1–284. [Google Scholar]
- 14.Richmond A, Aguilar-Gaxiola S, Perez-Stable EJ, et al. Proceedings of the 2017 Advancing the Science of Community Engaged Research (CEnR) Conference BMC Proceedings. 2019;13(Suppl 3):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Health Care for the Homeless Council. What is the official definition of homelessness? https://www.nhchc.org/faq/official-definitionhomelessness/.
- 16.D’Aquila R, Aseltyne WJ, Lopman A, Jweinat J, Ciaccio T, Comerford MJ. Yale-New Haven hospital’s planning and execution of a complex hospital acquisition. The American Journal of Medicine. 2013;126(8):744–752.e712. [DOI] [PubMed] [Google Scholar]
- 17.Patton MQ. Qualitative research and evaluation methods. Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- 18.Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. Aldine; Chicago, IL. 1967. [Google Scholar]
- 19.Morse JM. The significance of saturation. Sage Publications; Thousand Oaks, CA: 1995. [Google Scholar]
- 20.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res 2007;42(4):1758–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark AM, Spaling M, Harkness K, et al. Determinants of effective heart failure self-care: a systematic review of patients’ and caregivers’ perceptions. Heart. 2014;100(9):716–721. [DOI] [PubMed] [Google Scholar]
- 22.van der Wal MH, Jaarsma T, Moser DK, van Gilst WH, van Veldhuisen DJ. Qualitative examination of compliance in heart failure patients in The Netherlands. Heart & Lung 2010;39(2):121–130. [DOI] [PubMed] [Google Scholar]
- 23.Scotto CJ. The lived experience of adherence for patients with heart failure. Journal of Cardiopulmonary Rehabilitation. 2005;25(3):158–163. [DOI] [PubMed] [Google Scholar]
- 24.Hauptman PJ. Medication adherence in heart failure. Heart Failure Reviews. 2008;13(1):99–106. [DOI] [PubMed] [Google Scholar]
- 25.Forsyth P, Richardson J, Lowrie R. Patient-reported barriers to medication adherence in heart failure in Scotland. International Journal of Pharmacy Practice. 2019. October;27(5):443–450. [DOI] [PubMed] [Google Scholar]
- 26.Wu JR, Moser DK, Lennie TA, Burkhart PV. Medication adherence in patients who have heart failure: a review of the literature. The Nursing Clinics of North America. 2008;43(1):133–153; vii–viii. [DOI] [PubMed] [Google Scholar]
- 27.Milfred-LaForest SK, Chow SL, DiDomenico RJ, et al. Clinical pharmacy services in heart failure: an opinion paper from the Heart Failure Society of America and American College of Clinical Pharmacy Cardiology Practice and Research Network. Pharmacotherapy. 2013;33(5):529–548. [DOI] [PubMed] [Google Scholar]
- 28.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clinical Therapeutics. 2001;23(8):1296–1310. [DOI] [PubMed] [Google Scholar]
- 29.Sadik A, Yousif M, McElnay J. Pharmaceutical care of patients with heart failure. British Journal of Clinical Pharmacology. 2005;60(2):183–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chaufan C, Constantino S, Davis M. ‘It’s a full time job being poor’: understanding barriers to diabetes prevention in immigrant communities in the USA. Critical Public Health. 2012;22(2):147–158. [Google Scholar]
- 31.Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. The American Journal of Medicine. 2014;127(4):303–310.e303. [DOI] [PubMed] [Google Scholar]
- 32.Ruppar TM, Cooper PS, Mehr DR, Delgado JM, Dunbar-Jacob JM. Medication adherence interventions improve heart failure mortality and readmission rates: systematic review and meta-analysis of controlled trials. Journal of the American Heart Association. 2016;5(6):e002606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Specifications Manual for National Hospital Inpatient Quality Measures. 2018; https://www.jointcommission.org/specifications_manual_for_national_hospital_inpatient_quality_measures.aspx.
- 34.Enard KR, Hauptman PJ. Heart Failure, Shared Decision Making, and Social Determinants of Health: An Upstream Perspective. JAMA Cardiology. 2019. July 1;4(7):609–610. [DOI] [PubMed] [Google Scholar]
- 35.Martins DC. Experiences of homeless people in the health care delivery system: a descriptive phenomenological study. Public Health Nursing. 2008;25(5):420–430. [DOI] [PubMed] [Google Scholar]
- 36.Daiski I Perspectives of homeless people on their health and health needs priorities. Journal of Advanced Nursing. 2007;58(3):273–281. [DOI] [PubMed] [Google Scholar]
- 37.Wen CK, Hudak PL, Hwang SW. Homeless people’s perceptions of welcomeness and unwelcomeness in healthcare encounters. Journal of General Internal Medicine. 2007;22(7):1011–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brener L, Von Hippel W, Von Hippel C, Resnick I, Treloar C. Perceptions of discriminatory treatment by staff as predictors of drug treatment completion: utility of a mixed methods approach. Drug and Alcohol Review. 2010;29(5):491–497. [DOI] [PubMed] [Google Scholar]
- 39.Keyes K, Hatzenbuehler M, McLaughlin K, et al. Stigma and treatment for alcohol disorders in the United States. American Journal of Epidemiology. 2010;172(12):1364–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kelly JF, Westerhoff CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. International Journal of Drug Policy. 2010;21(3):202–207. [DOI] [PubMed] [Google Scholar]
- 41.Zerger S, Doblin B, Thompson L. Medical respite care for homeless people: a growing national phenomenon. Journal of Health Care for the Poor and Underserved. 2009;20(1):36–41. [DOI] [PubMed] [Google Scholar]
- 42.Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. American Journal of Public Health. 2006;96(7):1278–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kertesz SG, Posner MA, O’Connell JJ, et al. Post-hospital medical respite care and hospital readmission of homeless persons. Journal of Prevention & Intervention in the Community. 2009;37(2):129–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.“Five Ways Medicaid Expansion Is Helping Homeless Populations Ten Years After The ACA Became Law, “ Health Affairs Blog, February 27, 2020. [Google Scholar]
- 45.Katz MH. Homelessness-Challenges and Progress. JAMA. 2017;318(23):2293–2294. [DOI] [PubMed] [Google Scholar]
- 46.Lichtman JH, Leifheit-Limson EC, Watanabe E, et al. Symptom recognition and healthcare experiences of young women with acute myocardial infarction. Circulation: Cardiovascular Quality and Outcomes. 2015;8(2_suppl_1):S31–S38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sandelowski M The problem of rigor in qualitative research. Advances in Nursing Science. 1986. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.