Abstract
Introduction:
Sickle cell disease (SCD) stigma is a major community health issue. The challenges of caring for someone with SCD can be isolating and overwhelming. We explored stigma and its related factors for caregivers of pediatric patients with SCD in Kumasi, Ghana.
Methods:
Guided by the Ecological Systems Theory, we used in-depth interviews with a semi-structured guide to learn about the perception of stigmatization for Ghanaian caregivers of patients with SCD.
Results:
Overall, participants were knowledgeable about SCD. We identified three overarching themes including: 1) Blame for SCD; 2) Public misconception about SCD, and; 3) Shame for financial burden of SCD.
Discussion:
Findings demonstrate the need to design a SCD stigma reduction program for caregivers, their families and the community. Providers need to consider SCD stigma and interaction with multiple ecological levels including the family and community, health care system, culture, and health policy in Ghana. Findings can be used as a catalyst to explore the reduction of stigmatization in other sub-Saharan countries.
Keywords: Sickle cell disease (SCD), stigma, caregivers, Ecological Systems Theory, Ghana
Introduction
Sickle cell disease (SCD) affects millions worldwide with the greatest burden occurring in sub-Saharan Africa (Hood, McTate, Joffe, & Crosby, 2020; Tshilolo et al., 2019). In Ghana, where approximately 882,490 babies are born each year (Knoema, 2020), approximately 2% of newborns have SCD (Ohene-Frempong, Oduro, Tetteh, & Nkrumah, 2008). The disease is a genetically inherited disorder of the hemoglobin that can lead to serious health implications including recurrent infection, anemia, stroke, and both acute and chronic pain (Yawn et al., 2014).
Sickle cell-related stigma is increasingly becoming a major community health issue that is receiving more attention (Marsh, Kamuya, & Molyneux, 2011). Stigma is a mark of shame, disgrace or disapproval which results in an individual being rejected, discriminated against, and excluded from participating in a number of different areas of society (WHO, 2001). In a systematic review about the stigma of SCD, Bulgin and colleagues (2018), demonstrated the impact that stigma has on the lives and health of individuals with SCD, including hindering physiological and psychological wellbeing, having harmful social consequences, and impairing healthcare interactions. Stigma is something that is socially assigned (Major, Dovidio, Link, & Calabrese, 2018) and can stem from sources including institutions, healthcare providers, general public, family and friends (Bulgin, Tanabe, & Jenerette, 2018).
There is a paucity of research examining the experiences of caregivers of children with SCD in LMICs, particularly in Africa where the disease is most prevalent (Kuerten et al., 2020). Caregivers are often responsible for the physical care and emotional support of those with SCD and the challenges of caring for a loved one can be isolating and overwhelming (CDC, 2019). Evidence suggests that stigma and impairment in caregiver wellbeing can alter the quality of care in children with sickle cell disease (Bioku et al., 2020). Caregivers of children with SCD have reported challenges associated with the provision of physical, psychological and social care (Olwit, Mugaba, Osingada, & Nabirye, 2018; Wonkam et al, 2014). The chronicity of SCD could impair the quality of life of caregivers (Wonkam et al, 2014). The health and well-being of caregivers of patients with SCD contribute to the degree of treatment of sickle cell-related pain and the many clinical problems associated with the disease (Brown et al., 2010). In a study using the long interview method, Canadian mothers of African and Caribbean descent described how SCD stigma interacted with racism, contributed to social isolation, and prevented families from organizing as a group (Burnes, Antle, Williams, & Cook, 2008). Repeated hospitalization, altered body image and changes that come with the disease may affect self-esteem and the social life of caregivers and individuals with SCD (Olwit, Mugaba, Osingada, & Nabirye, 2018; Wonkam et al, 2014).
Even though caregivers play an important role in the lives of those with chronic diseases such as SCD, there is a gap in the literature about the perspectives of caregivers about stigma in SCD in Ghana. In this qualitative study, we used in-depth interviews to learn about the perception of stigmatization that Ghanaian caregivers experience for both themselves and the pediatric patients with SCD they care for. The aim of this paper was to explore stigma and its related factors, such as caregiver knowledge and public perception of SCD, for caregivers of pediatric patients with SCD in Kumasi, Ghana.
Methods
This cross-sectional, qualitative study was conducted between January and March 2020 in three outpatient clinics and inpatient hospitals in Kumasi, Ghana, to explore stigma and its related factors, including caregiver knowledge and public perception of SCD, for caregivers of patients with SCD.
Ethical Review
The study was cleared by the Ghana Health Service (GHS/ASH/AD4/Vol.6) and institutional review board approval was obtained before starting from the Kwame Nkrumah University of Science and Technology Committee on Human Research, Publication and Ethics (CHRPE/AP/001/20) and the University of Michigan (HUM00175765). Participants provided informed written consent or verbal consent if they were unable to read or write.
Study setting
Kumasi is located in the Ashanti Region of the West African nation of Ghana and is the country’s second largest city with a population of more than two million (World Population Review, 2020). Participants were interviewed at Suntreso Government Hospital, Kumasi Metropolitan Assembly Clinic, and the Komfo Anokye Teaching Hospital. Suntreso Government Hospital provides primary healthcare to approximately 519,439 residents of a sub-metropolitan area (Donkoh, Agyemang-Yeboah, Asmah, & Wiredu, 2019). At the Kumasi Metropolitan Assembly Clinic, the Sickle Cell Association of Ghana-Ashanti Regional Branch, supported by the National Health Learning Material Centre of the Ghana Health Service, offers monthly support group meetings for parents and caregivers and patients with SCD. The center offers administrative, organizational and educational support to the association and its members. The Komfo Anokye Teaching Hospital is a major academic medical center and their Sickle Cell Clinic is one of two large, established specialized pediatric SCD centers in Ghana (Kwarteng-Siaw, Paintsil, Toboh, Owusu-Ansah, & Green, 2017).
Participants
Participants were selected through purposive and snowball sampling. We spoke with healthcare staff or reviewed admission or clinic records to identify primary caretakers of pediatric patients under the age of 18 with SCD. Participants were approached face-to-face in the clinic/hospital or occasionally via mobile telephone after patients provided primary caregiver contact information and asked about their interest in completing an in-person interview regarding SCD. None of the participants refused to participate or dropped out, and all personal information collected was de-identified.
Data Collection
In-depth interviews were conducted by either the female PhD prepared primary investigator or one of the two locally trained, bachelor degree holding, male research assistants. Participants were given the option to speak in either English, the official language in Ghana, or the predominant local language, Ashanti Twi. To maintain confidentiality, only the participants and researchers were present during interviews.
A semi-structured interview guide written in English was used to collect the data. Questions in the interview guide were based on information included in scales to measure stigma from the sickle cell (Bediako et al., 2016; Leger, Wagner, & Odesina, 2018), mental illness (King et al., 2007), and HIV (Berger, Ferrans, & Lashley, 2001) literature. The interview guide included broad, open-ended questions to gather the perceptions of stigmatization by caregivers of patients with SCD. Example questions are shown in Table 1. The guide was pilot tested for context-in meaning with three caregivers and two providers, and no changes were deemed necessary.
Table 1:
Example interview guide questions about stigma for caregivers of patients with SCD
| Broad Stigma Topic | Questions |
|---|---|
| Knowledge of SCD |
|
| Discrimination and Disclosure |
|
| Public Perception |
|
| Social Exclusion |
|
All interviews were audio recorded, five interviews were translated to English, and transcribed verbatim. The research team discussed each transcript and attempted to clarify any areas that had ambiguous or unclear meaning. The primary investigator made field notes during and after each interview. The interviews lasted approximately half an hour. Data saturation was reached after five interviews.
Data Analysis
All the transcripts coded in English. The primary investigator reviewed transcripts for completeness and corrected any spelling or grammar errors. Four research team members, four fluent in English and three fluent in Ashanti Twi, coded the data. Coders communicated regularly via phone and email to discuss the development of coding, update the codebook as required and resolve any coding discrepancies. A password-encrypted shared google drive word document was used to manage the data. Findings were verified at follow-up clinic visits or over the phone with four of the participants about their own interview transcripts to ensure correct interpretation. Latent content analysis, guided by early versions of Bronfenbrenner’s Ecological Systems Theory (EST) (Bronfenbrenner, 1977, 1979, 1989), was used to underpin our qualitative study.
Social ecological analyses emphasize the dynamic interplay between situational and personal factors rather than focusing exclusively on environmental, biological, or behavioral determinants of well-being (Stokols, 1996). The EST acknowledges that the family is part of a much broader complex of systems and is concerned with the interaction of those systems (Leger, Wagner, & Odesina, 2018). Within the EST, the environment is conceived topologically as a nested arrangement of structures, each contained within the next (Bronfenbrenner, 1997). Moving from the innermost level to the outside, are the micro-, meso-, exo-, macro-, and chronosystem (Bronfenbrenner, 1989). In our operationalization of the EST for SCD stigma (Figure 1), the patient-caregiver dyad represents the microsystem. The mesosystem comprises the family and community surrounding the patient-caregiver dyad. The exosystem encompasses the health care system in Kumasi. The macrosystem incorporates culture. Lastly, the chronosystem includes health policy in Ghana pertaining to SCD.
Figure 1.
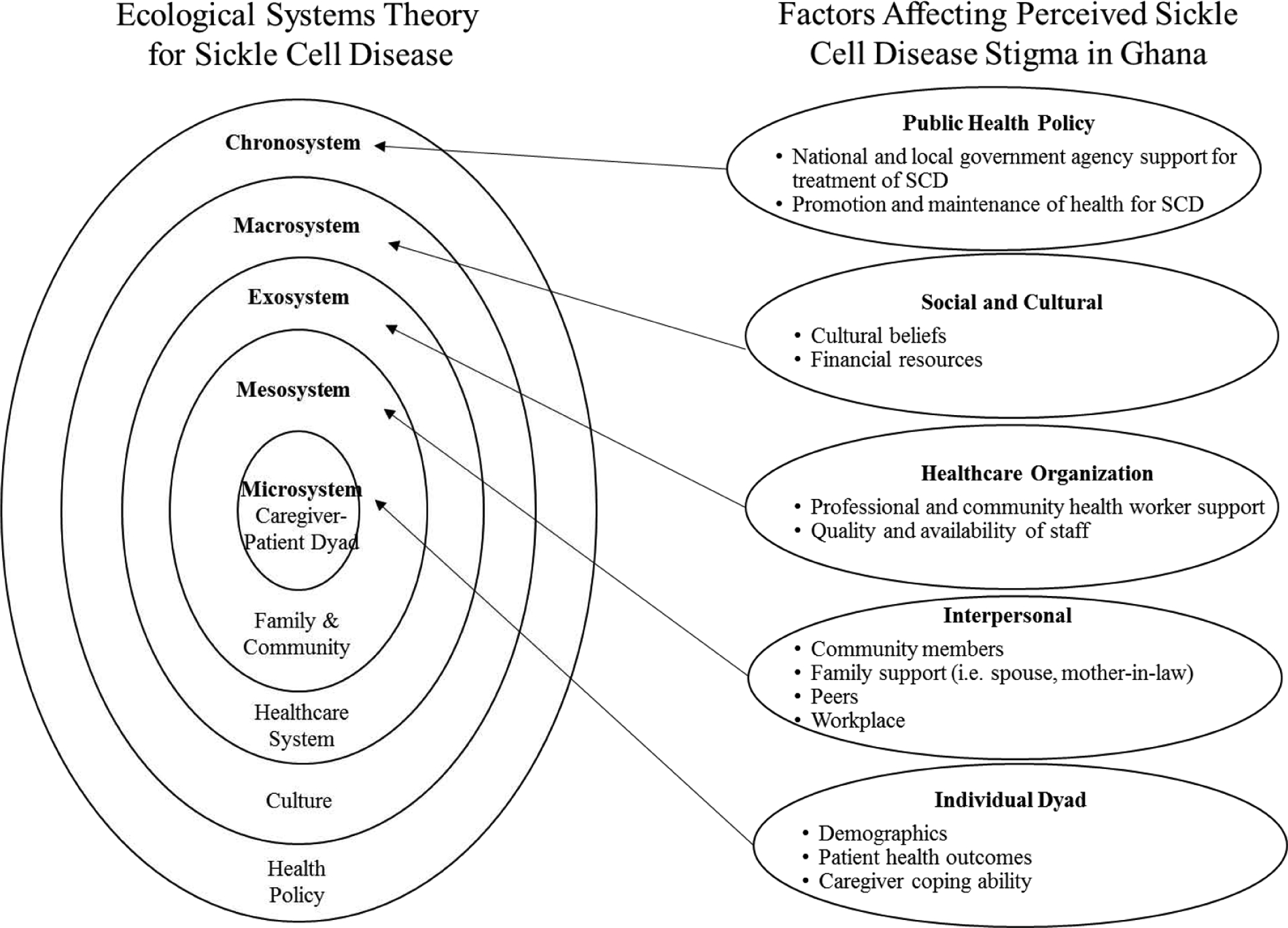
Operationalization of Ecological Systems Theory for Sickle Cell Disease Stigma (adapted from Berger, 2007; Buser, 2019; Stranger, 2011)
Results
Table 2 highlights demographic characteristics of the participants. Most were females and attained a senior secondary (grades 10–12) level of education. All participants were Christians from the Akan ethnic group. The majority of participants (n = 6) worked in sales or commerce.
Table 2.
Caregiver characteristics SCD Stigma
| Demographic Characteristic | Individual Interview (n = 10) |
|---|---|
| Sex | % (n) |
| Female, Male | 80% (8), 20% (2) |
| Age (years) | |
| Mean (SD), Range | 43.5 (8.0), 28 – 55 |
| Number of living children | |
| Mean (SD), Range | 3.1 (1.6), 1 – 6 |
| Marital status | |
| Married | 70% (7) |
| Separated/Divorced | 30% (3) |
| Education level | |
| Upper & Junior Primary | 20% (2) |
| Senior Secondary | 70% (7) |
| Tertiary | 10% (1) |
Every caregiver participant in our study reported experiencing SCD stigma. Participants identified negative societal attitudes towards children with SCD as the main prevailing factors contributing to stigmatization for caregivers. Overall, participants were knowledgeable about SCD and caregivers credited health education received from providers at sickle cell clinics for increasing their understanding of the disease. We identified three overarching themes from the data contributing to the perception of stigmatization by caregivers of patients with SCD including: 1) Blame for SCD; 2) Public misconception about SCD, and; 3) Shame for financial burden of SCD.
Blame for SCD
Caregivers discussed stigmatization attributed to beliefs among the general public that SCD results from a curse, or “brought disease”, known locally as “duabo” or “nto yare”. There is a widespread belief that the affected family committed a sin against the gods or someone is bewitching them. Others in the community believe that SCD is payback for the parents “doing bad things to other people”. One participant commented, “Some people perceive SCD as a generational problem passed down from olden-time family members. In our system, people can attribute such an instance of SCD to traditional or spiritual beliefs”. Another stated, “According to our beliefs, we understand that SCD is a devilish disease and acquired as a result of their parents’ sinful deed against God”. A participant commented:
You see, people are not so knowledgeable about this disease so they turn to say things out of ignorance such as SCD is caused by the evil spirit. People think that SCD is a devilish disease and most believe it is given to people by witches. This brings dishonor for our families and shame for our children with SCD.
Public misconception about SCD
While caregivers were knowledgeable about SCD, they observed that the general public is not knowledgeable about SCD and expressed dissatisfaction with what they feel is inadequate public health education. Participants would advocate for more local and national support for SCD and increased attention from the media to create awareness and change long-standing cultural beliefs and myths that people living with SCD are from the “marine spirit” and should be considered “devilish children”. A participant said, “Mostly those in the public have not come or attended any hospital for further explanation on SCD and they have a wrong perception on sickle cell and believe it is a devilish disease”. Another stated:
We are in the 21st century but some people in the community are still very ignorant about the disease and they say it has to be something spiritual. Sorry to say that some of our uneducated parents say a lot of things because they are not very educated and usually associate it with spiritual beliefs other than medical.
According to one participant:
I would say most of the public have low level of education on SCD and do not have people who would give them in-depth understanding on it. Some of them have heard about SCD but do not know what causes it and the acceptance of the condition in this society of ours is very low and causes rejection.
Shame for Financial burden of SCD
Participants frequently mentioned stigma associated with being shamed for the financial burden of caring for someone with SCD. Participants often talked about community members who believe that caregivers waste their money by spending it on children with SCD. Participants referred to the term, “sikabesa”, or “money will finish”. Sickle cell disease is seen to be a disease that involves a lot of money to manage and there is a widely held belief that the “spiritual enemy” can use SCD to drain the family finances. People perceive that someone with SCD will fall sick only to be taken to the hospital and waste the money of the family. As one caregiver noted, “Some think it’s just a waste of money by the parent to take care of such a person with SCD. So most neglect them”. A different participant stated, “Others even say this child always want to waste his or her parents’ money because they fall sick when there is money in the house”. More than one participant said that if there was more than one person with SCD in the family then it solidified the plan of the “spiritual enemy” to ruin the family financially. Another participant commented:
Sickle cell is a disease that requires a lot of money to be able to manage properly…It is a disease that wastes money, people term it ‘sikabesa’, because it finishes all the money of the parents and this becomes difficult to take care of them because of money issues.
Caregivers also cited the high cost of hydroxyurea and other drugs used to manage SCD. Most participants expressed concern because they cannot afford the necessary drugs for treatment. A couple of participants detailed having to sell personal belongings and still not being able to afford medications. One participant shared:
I wish we could get people to advocate for reduction on the prices of drugs and hydroxyurea we use for SCD person. Even before you are put on medications, the laboratory investigations are expensive. So the government should come out and help us or put it on the NHIS [National Health Insurance Scheme] because it is expensive for individuals.
Discussion
In this study exploring caregiver perceptions, participants expressed several concerns about stigma and its related factors as caregivers of pediatric patients with SCD in Kumasi, Ghana. Negative societal attitudes about SCD contributed to the perception of stigmatization by caregivers. The most significant concerns were feeling blamed for their child having the disease, public misconceptions about SCD, and being shamed for financial burdens. The ecological approach used to underpin the study sheds light on the importance of considering the stigmatization perceived by the caregiver and their interaction with multiple levels including the family and community, health care system in Kumasi, culture, and health policy in Ghana pertaining to SCD. When developing health care plans and interventions, it is important for healthcare providers to consider the stigma experienced by caregivers at these different levels.
Framed with the context of the Ecological Systems Theory, we identified linkages between themes at the micro- and mesosystem level as blame for SCD illustrates the stigmatizing mark placed on families in the Ghanaian context about cultural beliefs while public misconceptions demonstrate how these cultural beliefs at the macrosystem level impede the general public from becoming more knowledgeable of SCD. Increased knowledge might cause them to stop mystifying and dehumanizing individuals with SCD. The lack of knowledge and stigma indirectly and directly impedes advocacy for policies at the chronosystem level that could improve the overall care of SCD, relieve financial burden on caregivers, and result in improved health outcomes for patients with SCD.
Regarding blame and shame for financial burden, other researchers in Kumasi conducting in-depth interviews with fathers of patients with SCD found similar discourses associating sickle cell with blame related to supernatural beliefs about the cause of SCD and economic challenges (Dennis-Antwi, Culley, Hiles, & Dyson, 2011). Comparing our findings to other literature, we note that participants in our study are not alone in recognizing a public misconception and lack of knowledge about SCD. One study conducted in the capital of Ghana to evaluate pregnant women’s awareness of SCD and the factors that contribute to it found a deficit in the knowledge of SCD among pregnant women and recommended more public education on the disease (Obed et al., 2017). Researchers in western Ghana assessing knowledge of SCD found that only 53% of the individuals sampled (n=326) had knowledge of SCD in general and stressed the need for more emphasis to increase public awareness of SCD especially in schools, churches and the media (Orish, Onyeabor, Sanyaolu, & Iriemenam, 2014).
A strength of this study, guided by an ecological approach, is that it provides crucial, firsthand knowledge about stigma as perceived by caregivers in Ghana. Conversely, findings have limited generalizability as it focused on one region in central Ghana. Another limitation is a lack of gender balance in the sample. Since women were more likely to accompany their children to the health facilities for care, only two men were included in the sample. Furthermore, the study leaves out caregivers who did not accompany children to health facilities, these caregivers might have varying experiences of SCD stigma in Ghana.
There are several implications for healthcare providers emerging from this exploration of stigma and its related factors for caregivers of patients with SCD. Healthcare providers can better meet the needs of caregivers of patients with SCD by fostering an expanded social support network offering frequent in-person or consider on-line support group meetings for those with access to internet resources. Broader social support can potentially improve how caregivers cope with stigmatization associated with the shame of financial burden and blame for SCD. Expansion of programs to provide economic support for caregivers of patients with SCD would undoubtedly improve the wellness of entire families. Additionally, healthcare providers can advocate for improved educational programs to reduce public misconception and lack of knowledge about SCD. Finally, there should be government policy to financially support the care and management of SCD; for example, NHIS could pay for lab tests and medications and this can be a relief of the financial burden and its associated stigma.
In conclusion, our findings demonstrate the necessity of designing a SCD stigma reduction program in the Ghanaian setting for caregivers and their families. To avoid the potentially harmful effects of stigmatization, it is important for healthcare providers to design interventions, such as the use of community health workers, aimed at reducing the financial burden, blame, and public misconceptions about SCD. Our findings about caregiver perception of SCD stigma could be used as a catalyst to explore the reduction of stigmatization in other sub- Saharan countries.
Funding Sources:
Research reported in this publication was supported by the Fogarty International Center of the National Institutes of Health under grant number D43TW009345 awarded to the Northern Pacific Global Health Fellows Program. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
None to declare
Ethical Approval:
Institutional Review Board (IRB) approval was obtained before beginning the study from the Kwame Nkrumah University of Science and Technology Committee on Human Research, Publication and Ethics (CHRPE/AP/001/20), the University of Michigan (HUM00175765), and cleared by the Ghana Health Service (GHS/ASH/AD4/Vol.6).
Contributor Information
Julie M. Buser, Fogarty International Center, National Institutes of Health, Global REACH, University of Michigan Medical School, Victor Vaughan Building, 2nd Floor, 1111 East Catherine Street, Ann Arbor, MI 48109.
Ashura Bakari, Ghana Health Service, Suntreso Government Hospital, Kumasi, Ghana.
Abdul-Aziz Seidu, College of Public Health, Medical and Veterinary Sciences, James Cook University, Townsville, Queensland, Australia, Department of Population & Health, College of Humanities and Legal Studies, University of Cape Coast, Cape Coast, Ghana.
Alex Osei-Akoto, Department of Child Health School of Medical Sciences, Kwame Nkrumah University of Science & Technology, Kumasi, Ghana.
Vivian Paintsil, Komfo Anokye Teaching Hospital, Kumasi, Ghana.
Rexford Amoah, Ghana Health Service, Suntreso Government Hospital, Kumasi, Ghana.
Benjamin Otoo, Ghana Health Service, Suntreso Government Hospital. Kumasi, Ghana.
Cheryl A. Moyer, Global REACH, Departments of Learning Health Sciences and Obstetrics & Gynecology, Global REACH, University of Michigan Medical School, Victor Vaughan Building, 2nd Floor, 1111 East Catherine Street, Ann Arbor, MI 48109.
References
- Bediako SM, Lanzkron S, Diener-West M, Onojobi G, Beach MC, & Haywood C Jr (2016). The measure of sickle cell stigma: initial findings from the improving patient outcomes through respect and trust study. Journal of Health Psychology, 21(5), 808–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, & Lashley FR (2001). Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health, 24(6), 518–529. [DOI] [PubMed] [Google Scholar]
- Berger KS (2007). The developing person through the life span. New York: Worth Publishers. [Google Scholar]
- Bioku AA, Ohaeri JU, Oluwaniyi SO, Olagunju TO, Chaimowitz GA, & Olagunju AT (2020). Emotional distress among parent caregivers of adolescents with sickle cell disease: Association with patients and caregivers variables. Journal of Health Psychology, 1359105320935986. [DOI] [PubMed] [Google Scholar]
- Brown BJ, Okereke JO, Lagunju IA, Orimadegun AE, Ohaeri JU, & Akinyinka OO (2010). Burden of health-care of carers of children with sickle cell disease in Nigeria. Health & Social Care in the Community, 18(3), 289–295. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U (1977). Toward an experimental ecology of human development. American Psychologist, 32, 513–531. [Google Scholar]
- Bronfenbrenner U (1979). The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press. [Google Scholar]
- Bronfenbrenner U (1989). Ecological systems theory. Annals of Child Development, 6, 187–249. [Google Scholar]
- Bulgin D, Tanabe P, & Jenerette C (2018). Stigma of sickle cell disease: a systematic review. Issues in Mental Health Nursing, 39(8), 675–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnes DP, Antle BJ, Williams CC, & Cook L (2008). Mothers raising children with sickle cell disease at the intersection of race, gender, and illness stigma. Health & Social Work, 33(3), 211–220. [DOI] [PubMed] [Google Scholar]
- Buser J (2019). Cultural Practices, Knowledge, and Beliefs of Newborn Care and Health- Seeking in Rural Zambia (Doctoral dissertation).
- CDC. 2019. Caregivers and Sickle Cell Disease. Sickle Cell Disease (SCD). https://www.cdc.gov/ncbddd/sicklecell/features/sickle-cell-caregivers.html [Google Scholar]
- Dennis-Antwi JA, Culley L, Hiles DR, & Dyson SM (2011). ‘I can die today, I can die tomorrow’: lay perceptions of sickle cell disease in Kumasi, Ghana at a point of transition. Ethnicity & Health, 16(4–5), 465–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donkoh ET, Agyemang-Yeboah F, Asmah RH, & Wiredu EK (2019). Prevalence of cervical cancer and pre-cancerous lesions among unscreened women in Kumasi, Ghana. Medicine, 98(13). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood AM, McTate EA, Joffe NE, & Crosby LE (2020). Sickle Cell Disease In Clinical Handbook of Psychological Consultation in Pediatric Medical Settings (pp. 341–354). Springer, Cham. [Google Scholar]
- Jenerette CM, & Brewer C (2010). Health-related stigma in young adults with sickle cell disease. Journal of the National Medical Association, 102(11), 1050–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Dinos S, Shaw J, Watson R, Stevens S, Passetti F, … & Serfaty M (2007). The Stigma Scale: development of a standardised measure of the stigma of mental illness. The British Journal of Psychiatry, 190(3), 248–254. [DOI] [PubMed] [Google Scholar]
- Knoema. 2020. Ghana - Number of births. https://knoema.com/atlas/Ghana/topics/Demographics/Fertility/Number-of-births
- Kuerten BG, Brotkin S, Bonner MJ, Ayuku DO, Njuguna F, Taylor SM, & Puffer ES (2020). Psychosocial Burden of Childhood Sickle Cell Disease on Caregivers in Kenya. Journal of Pediatric Psychology, 45(5), 561–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwarteng-Siaw M, Paintsil V, Toboh CK, Owusu-Ansah A, & Green NS (2017). Assessment of Transition Readiness in Adolescents with Sickle Cell Disease and their Caretakers, A single institution experience. International Journal of Hematology Research, 3(1), 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leger RR, Wagner LD, & Odesina V (2018). Stigma in adults with sickle cell disease and family members: Scale development and pilot study in the USA and Nigeria. International Journal of Africa Nursing Sciences, 9, 23–29. [Google Scholar]
- Major B, Dovidio JF, Link BG, & Calabrese SK (2018). Stigma and its implications for health: Introduction and overview. Stigma, Discrimination, and health, 3–28. [Google Scholar]
- Marsh VM, Kamuya DM, & Molyneux SS (2011). ‘All her children are born that way’: gendered experiences of stigma in families affected by sickle cell disorder in rural Kenya. Ethnicity & Health, 16(4–5), 343–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obed SA, Asah-Opoku K, Aboagye S, Torto M, Oppong SA, & Nuamah MA (2017). Awareness of sickle cell trait status: a cross-sectional survey of antenatal women in Ghana. The American Journal of Tropical Medicine and Hygiene, 96(3), 735–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohene-Frempong K, Oduro J, Tetteh H, & Nkrumah F (2008). Screening newborns for sickle cell disease in Ghana. Pediatrics, 121(2), S120. [Google Scholar]
- Olwit C, Mugaba M, Osingada CP, & Nabirye RC (2018). Existence, triggers, and coping with chronic sorrow: a qualitative study of caretakers of children with sickle cell disease in a National Referral Hospital in Kampala, Uganda. BMC Psychology, 6(1), 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orish VN, Onyeabor OS, Sanyaolu AO, & Iriemenam NC (2014). Evaluating the knowledge of sickle cell disease and hemoglobin electrophoretic pattern among people living in Sekondi-Takoradi Metropolis, Ghana. Journal of Medicine in the Tropics, 16(2), 56. [Google Scholar]
- Stokols D (1996). Translating social ecological theory into guidelines for community health promotion. American Journal of Health Promotion, 10(4), 282–298. [DOI] [PubMed] [Google Scholar]
- Tshilolo L, Tomlinson G, Williams TN, Santos B, Olupot-Olupot P, Lane A, … & Ware RE (2019). Hydroxyurea for children with sickle cell anemia in sub-Saharan Africa. New England Journal of Medicine, 380(2), 121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yawn BP, Buchanan GR, Afenyi-Annan AN, Ballas SK, Hassell KL, James AH, … & Tanabe PJ (2014). Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA, 312(10), 1033–1048. [DOI] [PubMed] [Google Scholar]
- WHO. (2001). The World Health Report 2001: Mental health: new understanding, new hope. World Health Organization. [Google Scholar]
- Wonkam A, Mba CZ, Mbanya D, Ngogang J, Ramesar R, & Angwafo FF (2014). Psychosocial burden of sickle cell disease on parents with an affected child in Cameroon. Journal of Genetic Counseling, 23(2), 192–201. [DOI] [PubMed] [Google Scholar]
- World Population Review. (2020). Population of Cities in Ghana (2020). https://worldpopulationreview.com/countries/ghana-population/cities/


