1. INTRODUCTION
High adherence (consumption above 80% of prescribed doses) to antiretroviral therapy (ART) is necessary to achieve viral suppression and optimal therapeutic outcomes (Eisinger et al., 2019) in people living with HIV (PLHIV); yet meta-analyses show that global adherence is less than optimal, ranging from 53% to 62% (Marsh et al., 2019).
Although ART adherence is particularly important for adolescents who are entering the age of sexual debut, rates are as low as 28% in some countries (Hudelson and Cluver, 2015). Adolescents face various adherence challenges, including physical and psychological factors, disruption of daily routines, reliance on family support, and greater responsibility for medication-taking behaviors (Buchanan et al., 2012); all against the backdrop of their unique developmental stage. Adolescents in South Africa —where our research takes place—face additional challenges stemming from long-term racial segregation that contributes to violence, crime, poverty and family separation.
Interventions to improve ART adherence are sparse for adolescents compared to adults (Simoni et al., 2010), with few randomized controlled trials (RCTs) (Bain-Brickley et al., 2011). A recent systematic review by Ridgeway et al. (2018) concluded that studies on adolescent adherence in low-and-middle income countries (LMICs) are lacking in scope and quality.
Conditional economic incentives (CEIs), as a behavioral-structural intervention, have not been widely applied to improve ART adherence among adolescents or in generalized epidemic settings (Galárraga and Sosa-Rubí, 2019). CEIs have been successful for HIV risk reduction (Björkman Nyqvist et al., 2018; Operario et al., 2013), increasing HIV testing (Kranzer et al., 2018; Montoy et al., 2018), and improving linkage to care (El-Sadr et al., 2017). In the United States, several RCTs employing incentive-based interventions showed improved ART adherence among adults (Farber et al., 2013; Galárraga et al., 2013), suggesting that similar interventions could be effective for adolescents.
In the context of adherence behaviors, CEIs assume that adolescents (even more than adults) favor immediate rewards and discount future outcomes (Stoianova et al., 2018; Story et al., 2014). Providing incentives contingent upon a positive and measurable behavior, such as consuming ≥80% of daily doses of ART, or demonstrating reductions in viral load (via blood tests), can help alter this calculus by allowing recipients to experience an immediate, tangible benefit of a behavior rather than the delayed reward of positive health in the future. Given the unique adherence challenges facing adolescents living with HIV, tools that can elicit youth-centered preferences are critical for developing CEI interventions for this population.
Theoretical work points to potential unintended consequences of incentives eroding intrinsic motivation (Galárraga et al., 2013). Nevertheless, recent empirical literature suggests that incentives do not erode intrinsic motivation (Czaicki et al., 2018; Lohmann et al., 2018). The key to long-term sustainability, when incentives are used as short-term interventions, will be to habituate the use of incentives in conjunction with other interventions (Galárraga and Sosa-Rubí, 2019).
Discrete choice experiments (DCE) are widely used in environmental and development economics (Gibson et al., 2016), and hold promise for calibrating interventions to optimize adherence in adolescents (Johnson et al., 2013). DCEs help us understand how people make choices and trade-offs, and thus present an advantage over methods relying solely on questionnaires. DCEs elicit user preferences for a program or service based on a number of attributes, but methods for defining attributes are often poorly described (Coast et al., 2012; Coast and Horrocks, 2007). Increasing rigor and transparency surrounding attribute generation can ensure DCE design relevance and generalizability (De Brún et al., 2018).
This study uses a mixed methods design comprised of qualitative interviews and a DCE to explore youth-centered preferences for ART adherence programs in South Africa. Our qualitative approach helps elicit and understand adolescents’ preferences for attributes and levels of a future CEI intervention for ART adherence; a DCE estimates youth preferences for this intervention. This research contributes to two distinct areas: (a) DCEs in public health and HIV (de Bekker-Grob et al., 2012; Michaels-Igbokwe et al., 2014; Ostermann et al., 2015; Quaife et al., 2018); and (b) CEIs for behavior change and HIV management in LMICs (Bassani et al., 2013). To the best of our knowledge, this is the first DCE used to calibrate interventions that employ CEIs for ART adherence, and that focuses specifically on adolescents.
2. METHODS
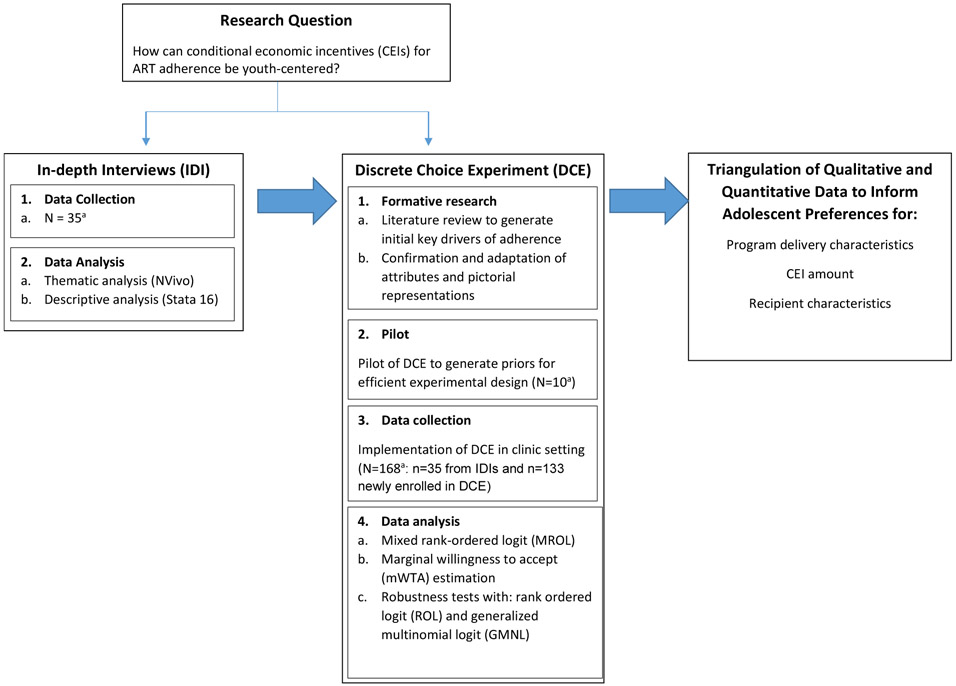
The rationale for using a mixed methods approach involving a DCE was grounded in the overall goals of conducting participant-engaged research, and comparing and contrasting data across methods in an integrated approach. Figure 1 summarizes the mixed methods study design. The overall study was conducted during 2017-2019 in South Africa’s Western Cape Province. All study procedures were approved by ethics committees at Brown University (Institutional Review Board, IRB/IAA#16-19) and University of Cape Town (Protocol #HREC 368/2016).
Figure 1.
Overview of mixed methods design
a Sample of young people 10-19 years
2.1. Qualitative phase
Study population.
We conducted in-depth interviews (IDIs) with n=35 adolescents living with HIV to explore acceptability of CEIs for ART adherence. Conducting IDIs is consistent with best practice recommendations for sensitive topics (Coast et al., 2012). Participants were recruited from adolescent HIV clinics using convenience sampling. Inclusion criteria were: (1) 10-19 years of age; (2) knowledge of HIV-positive status (self-report); and (3) currently on, or have been on, HIV treatment (self-report). Young persons living with HIV (YPLWH) who were not aware of their HIV status were excluded from participating in this research. The research team obtained written parental consent and adolescent assent. An additional n=12 YPLWH assented to participate but were excluded from the IDIs due to lack of parental consent (Appendix A).
Data collection.
All interviews were guided by a semi-structured protocol that we have successfully used to conduct qualitative research with adolescents in South Africa (Appendix B). Interviews were conducted in the participant’s preferred language (English or Xhosa), lasted 1-1.5 hours, and were digitally audiotaped. The protocol explored: (1) barriers to and facilitators of adherence; (2) acceptability of CEIs as an adherence intervention strategy; (3) predicted impacts of CEIs on behavior including on daily adherence; (4) preferred format and frequency of CEIs to optimize adherence behaviors; and (5) the durability of adherence after CEIs are removed. Each adolescent received 100 Rand (~US$7) for time and transport.
As part of the IDIs, we used ‘think aloud’ techniques as a form of cognitive interviewing (De Brún et al., 2018; Giles et al., 2016) to incorporate open-ended questions into the interviews. This semi-structured format allowed participants to brainstorm openly about their preferences for a potential CEI-based intervention.
Data analysis.
The epistemological stance was pragmatism (Shannon-Baker, 2016), focusing on facilitators that may make a difference for YPLWH from their own point of view. Data were transcribed verbatim, and translated into English if needed. We conducted thematic analysis of qualitative data using NVivo (QSR International, 2012). Analysis included open-coding, axial coding, and coding of marginal remarks and comparisons (Strauss and Corbin, 2008). Common words, phrases, sentences, and ideas were clustered to develop a codebook. All transcripts were double coded. Pieces of text were compiled across all interviews under specific codes and sub-codes. Meaning from these codes was formulated to produce thematic clusters to inform attribute selection for the DCE.
Using best practices for mixed methods research, we leveraged qualitative findings to design the discrete choice experiment (Cresswell and Plano Clark, 2017). Specifically, the qualitative findings allowed for generation of key attributes for the DCE, and also allowed for comparing and contrasting of similar and different findings across methods. This process of data triangulation informed the analytical process and enhanced interpretation of the mixed methods results. The qualitative portion of the study adhered to the COREQ criteria for the conduct of qualitative research (Tong et al., 2007).
2.2. Discrete Choice Experiment
Emerging themes from the qualitative data and findings from the literature informed the DCE design process (Figure 1). The DCE used random utility theory (RUT), assuming the existence of a latent construct called “utility” for each YPLWH (McFadden, 1974). RUT allows utility for individual i and alternative a (Uia) to be summarized by two components: a systematic (Via) component, and a random (εia) component (McFadden and Train, 2000):
| (1) |
The literature demonstrates that children and adolescents understand the elicitation methods and can make choices consistent with utility maximization (Guerriero et al., 2017; Harbaugh et al., 2001).
Attribute selection.
Attributes and levels were considered for inclusion if they had high frequency of occurrence during thematic analyses of the qualitative data. Attribute selection followed an informal, two-stage process (Coast et al., 2012) where the most frequently recurring themes from the qualitative analyses were first defined as an attribute, and then assigned a word or phrase to capture the essence of that attribute. Five attributes were selected, which is consistent with other DCEs (Goddard et al., 2018).
Attribute levels.
One attribute had 5 levels, one attribute had 4 levels and 3 attributes had 3 levels. Given that all possible combinations would generate a large number of scenarios (namely S=51 × 41× 33=540), a full factorial design was not feasible. Thus, we implemented a D-efficient partial factorial design based on the covariance matrix of the conditional logit model (Carlsson and Martinsson, 2003). We used the Stata SE (College Station, TX, version 16) dcreate procedure for implementation (Hole, 2017).
DCE design.
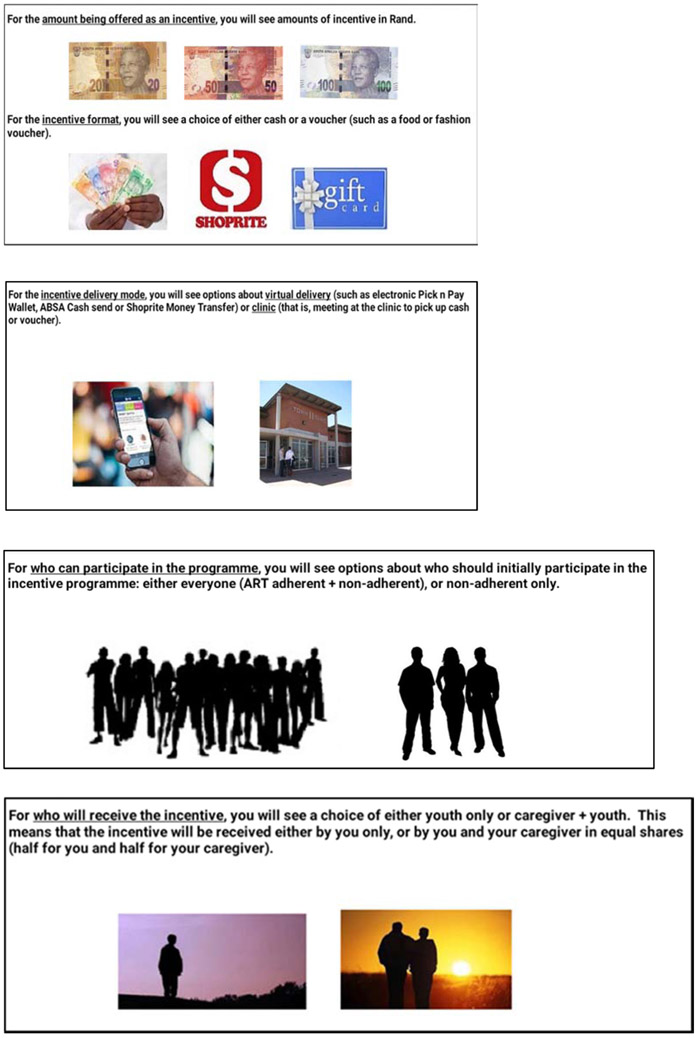
Respondents were asked to choose between different choice profiles that presented hypothetical CEI interventions for ART adherence (Figures 2 & 3). Profiles were made up of 5 attributes, each at an specific level. Three choice profiles were combined to form a choice task, in which participants were asked to select their preferred profile.
Figure 2.
Examples of computer-based sequential screens for choice scenario simulation for discrete choice experiment (DCE)
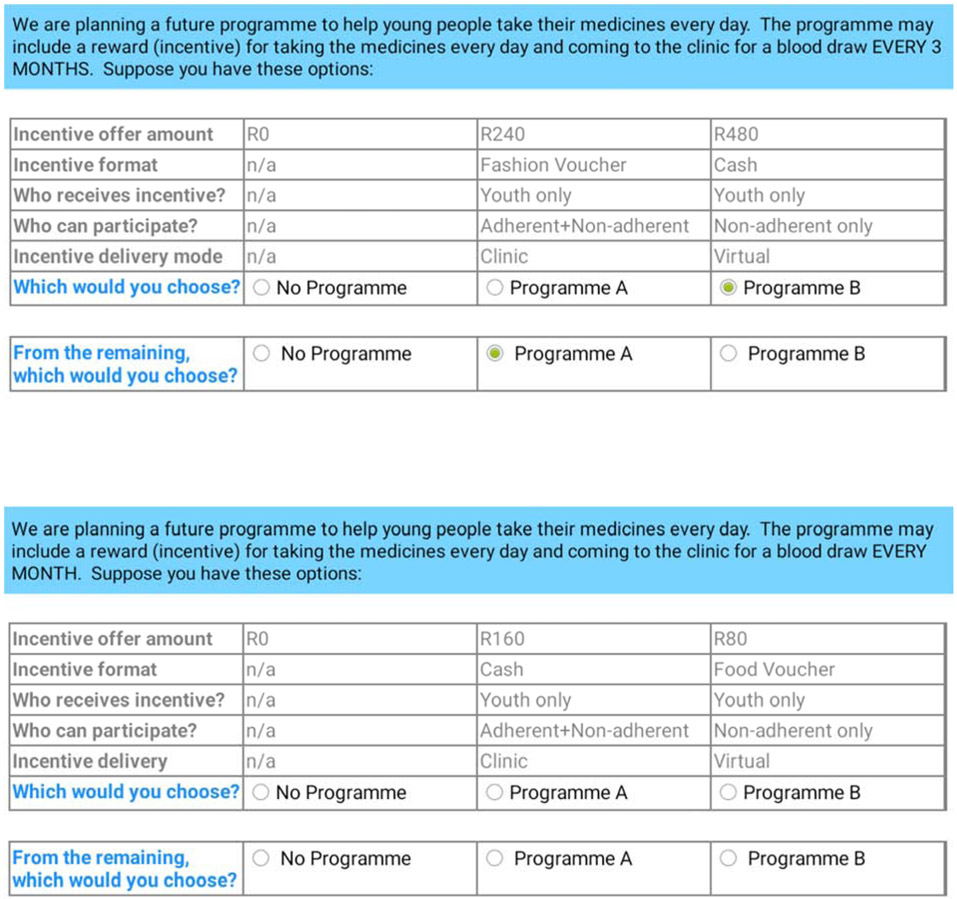
Figure 3.
Examples of computer-based choice scenarios for quarterly and monthly discrete choice experiments
The DCE assigned “unlabeled” alternatives in the choice sets, such that participants chose from random combinations of: Program A, Program B, or No Program. Unlabeled alternatives perform well in the health economics context (De Bekker-Grob et al., 2010). For each program type (with either monthly or quarterly visits), there were 540 scenarios in the full design; we used 5 blocks to allocate choice sets.
Number of profiles.
Each task included 3 choice alternatives: Program A, Program B, or No Program) (Figures 2 & 3). The No Program alternative represented the status quo (opt-out) option. The number of choice profiles was justified based on prior literature (Lancsar et al., 2017).
Number of tasks.
The total number of choice tasks (t=16) was chosen based on previous research concerning the number of questions that can be asked before reaching cognitive overload or respondent fatigue (Clark et al., 2014). We presented 8 scenarios for a monthly program and 8 scenarios for a quarterly program.
Framing.
For each respondent, we explained why we wanted their perspective via the DCE survey, emphasizing the importance of them teaching us how a future CEI program should be constructed. Research personnel also reviewed the study objectives, participation requirements and estimated time for survey completion. Respondents were encouraged to ask questions at any point during the experiment.
Elicitation format.
We used a best-best elicitation method (Ghijben et al., 2014; Lancsar et al., 2017). Respondents were first asked to select their best option from the 3 choice profiles (Program A, Program B, or No Program) based on the random attribute levels, and then to select their second-best option from the remaining 2 programs. This minimized cognitive burden, which was an important goal given the population and clinical focus of the research.
Instrument design and pilot testing.
We collected respondent information on socio-demographic characteristics, attitudes, and ART experience using a self-administered computer-based survey. Attributes and levels were derived from the qualitative data results, which also provided appropriate contextual information to ensure that the respondents understood the questions. Across participants, we randomized the order of the monthly vs. quarterly presentation. The computer-based DCE took approximately 40 minutes to complete.
During the design phase, we conducted pilot testing of the computerized DCE with n=10 adolescents who were patients of the clinic sites and who did not participate in the qualitative IDIs. To better assess young peoples’ acceptability of the DCE survey method, the validity of the attributes, and the respondents’ understanding of survey questions and attributes, pilot testing took an informal ‘think aloud’ approach whereby participants were encouraged to discuss their selections, ask questions as they completed the choice tasks and provide feedback on how the survey could be improved. Prior studies demonstrate the utility of the ‘think aloud’ approach during DCEs whereby participants verbalize their decision-making processes while simultaneously making choices on a computerized survey (Ryan et al., 2009; Whitty et al., 2014).
DCE sample size and population.
The same eligibility criteria used to enroll adolescents in the IDIs were used to enroll DCE participants. The minimum required sample size (N) was calculated based on the number of tasks (T), the alternatives (A) per task, and the number of analysis cells (c) as follows: N ≥ (500 × c) / (T × A). When considering main effects, c is equal to the largest number of levels for any one attribute. Solving with T=16, A=3, and c=5 our required sample size for the DCE was a minimum of N=52 respondents (de Bekker-Grob et al., 2015). The final sample size for the DCE was N=168 to allow exploration of heterogeneity by age.
Econometric analysis.
We assumed that the utility that individual i obtains from alternative a at choice scenario task t is given by:
| (2) |
where α are fixed coefficients on W, a vector of alternative-specific variables; β are random coefficients that vary over individuals in the population, and the vector X refers to the attributes of the alternatives; γ are fixed, alternative-specific coefficients on Z, a vector referring to characteristics of individual decision makers, including household characteristics (Appendix C); and εiat is a random term that follows a type-I extreme value distribution.
We analyzed the monthly and quarterly tasks together. We included a dummy variable that indicates if the task was quarterly=1 (and =0 if monthly). The variable YROFFER100s represented the yearly amount offered in South African Rand (in 100s) after transforming monthly OFFER×12, and quarterly OFFER×4. We used the best-best approach with an ‘exploded logit’ estimating it by expanding the data from each choice set into two choice subsets. The first contained three rows of data representing the three alternatives in the original set with the dependent variable (choice) =1 for the first-best and =0 for the remaining alternatives. The second sub choice set identified the second-best from the remaining two alternatives (Ghijben et al., 2014; Lancsar et al., 2017). Following the same logic as a mixed or random parameter logit, the best-best model can be estimated on ranked data by modelling the product of logits (Train, 2009) (Appendix D). We analyzed the ranked choice responses using a mixed rank-ordered logit model, which included normally distributed random parameters to allow for unobserved heterogeneity in latent preferences for a chosen Program compared with No Program. We included a constant term; yearly offer (R100s), age, years of formal education, asset index, travel time, ease of taking ART, and random block were modelled as continuous; other attributes were dummy coded. We used 1000 Hammersley sequence draws for the integration (Drukker and Gates, 2006; Ellis et al., 2019). Joint significance tests using Wald statistics determined if an attribute was jointly significant in the chosen program and the opt-out. Additional models —rank ordered logit and generalized multinomial logit— were used to check for robustness of main results. We used the Akaike and Bayesian information criteria to adjust for the number of parameters as diagnostic measures of model fit: the MROL model had the best performance, and thus was chosen as the main model. We plotted the average choice probabilities over the entire age range to visualize the participants’ overall choices.
We estimated the willingness to accept (WTA) for each attribute by calculating the marginal rate of substitution for each non-incentive attribute with the economic incentive attribute as reference. The WTA quantified the trade-offs that participants were willing to make across attributes in terms of the amount of incentives that they would be willing to sacrifice to keep that attribute in the program.
3. RESULTS
Table 1 shows the characteristics of the study population. One hundred and sixty-eight (N=168) youth completed the DCE, including the 35 adolescents who also participated in the IDIs and 133 newly enrolled participants (Appendix A). On average, youth were 15.4 years of age with 8 years of education. Half of participants identified as female; all self-identified as Black African. Adolescents were of low socio-economic status as measured by a 12-item asset index (Appendix C) and were food insecure (70%). Ease of taking ART was ranked at 4.1 (where 1=extremely hard; 2= Very hard; 3= Somewhat hard; 4= Not very hard; and 5=not hard at all). For about a quarter of participants (23.8%) it was at least somewhat hard to adhere to ART.
Table 1.
Characteristics of participants
| Variable | N± | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| Age (in years) | 168 | 15.4 | 2.4 | 10 | 19 |
| Female (=1) | 168 | 0.5 | 0.5 | 0 | 1 |
| Years of formal education | 168 | 8.0 | 2.6 | 1 | 13 |
| Index of assets owned in HH | 168 | 0.0 | 1.5 | −4.5 | 4.4 |
| Any food insecurity (=1) ¶ | 168 | 0.7 | 0.5 | 0 | 1 |
| Travel time to clinic‡ | 168 | 2.5 | 0.8 | 1 | 4 |
| Ease of taking ART ₫ | 168 | 4.1 | 1.0 | 1 | 5 |
Notes:
N includes the 35 adolescents who participated in in-depth interviews (IDIs) and were re-invited to participate in the discrete choice experiment (DCE).
Adolescents were considered to be food insecure (=1) if they responded “yes” to any of the following questions: Does your household ever run out of money to buy food? Do you ever cut the size of meals or skip meals because there is not enough money for food? Do you ever eat less than you should because there is not enough money for food? [Appendix C].
Travel time was coded as follows: 1 if less than 15 minutes; 2 if 15-30 minutes; 3 if 30 minutes to 1 hour; and 4 if more than 1 hour.
Ease of taking ART was a response to How difficult is it to take your antiretrovirals as prescribed? and coded as 1 if extremely hard; 2 if very hard; 3 if somewhat hard; 4 if not very hard; 5 if not hard at all.
HH=household; ART=antiretroviral treatment
3.1. Qualitative findings
3.1.1. Youth perspectives on CEIs for ART adherence
Adolescents felt that the use of CEIs could encourage youth to take responsibility for their medication-taking behaviors:
That [incentives period] is going to increase thingamajig – the number of children who are ‘eating’ ARVs. Because they would be getting motivated by the voucher that they will be getting. But now after that – [incentives period] - - they will – the number will have increased. But now if you have started them you can’t stop them again. If you’ve started them already. Because your body is [now] used to it. It’s – It’s already used to those pills. They will continue. Because their bodies would have become used to those pills.
Teen interview 9037
Though several interview participants noted that continuing to adhere to medications once a CEI program has ended may prove difficult for some adolescents, other respondents indicated that the CEI would help them get used to the routine of taking daily ART:
Because according to how I understand it, once you get yourself used to – like, within a year or so of drinking the pills, you will – like, drinking them on time, without skipping [doses], like that. Your body gets used to that, ‘Ok, at a certain time I’m going to drink the pills. ’
And once you tell yourself, nothing, like, distracts you from drinking the pills. So, I think it [the incentive] will help them. And as I had mentioned, [you know], indeed, she was whatsis – she was getting rewards, she was faced with the rewards -
Teen Interview 1031
Adolescents had several suggestions for optimizing adherence during the initiation of a future CEI program, and after the program has ended. First, the framing of the CEI intervention was important. Youth discussed that the purpose and intent of the CEI would need to be explained clearly so that recipients do not think of the CEI as a ‘bribe’:
No, you must not like [pay them]– which means you are bribing them to take their tablets. When you stop paying them then they’ll stop taking their tablets, so I think it’s best to advise them that they should take their medication properly. And they should also accept that they have this kind of illness.
Teen interview 9004
Second, respondents felt that youth should only participate in a CEI-based program if they are motivated and open to the idea of improving their ART adherence. One participant responded to the interviewer’s question about sustaining adherence after the incentive was discontinued:
R: They will stop taking tablets sister, they will stop taking their tablets.
Interviewer: Oh, okay will you also stop taking your ARVs when you…?
R: No, when I get used to them sister, I will take them.
The problem is that they will see now they are no more longer getting them. And they want to get it that’s why they take their tablets, so when they see that no the rewards are coming to an end; they will stop taking their tablets. …
And they go back to skipping them.
Teen Interview 5021
Sustaining adherence after the CEI program was terminated would only work if additional support was provided by those within the teenager’s network including family and others:
What I would say makes it easy for the youth to take their ARVs is that, if ever they get support from family, then there is nothing that will be difficult.
Teen interview 1010
3.1.2. Attributes of a future CEI adherence program
From the qualitative IDIs and literature review, five attributes emerged as likely to influence youth preferences for conditional economic incentives.
CEI Amount:
Various incentive amounts were suggested during the interviews. To ensure that these were not idealized amounts, we compared the amounts proposed during the interviews to other local standards such as social welfare programs and school vouchers (Coetzee, 2013). Suggested CEI amounts from the IDIs largely aligned with government social grants including, for example, the child support grant which issues a cash grant of R420 (~US$30) per month.
CEI Format:
There was a wide variation between interviews as to the form that the CEI should take. Perceived utility – how useful the incentive is for meeting daily needs – was a recurring factor when discussing the CEI format:
It should be cash … so that I can give it to my sister when I have to come to the hospital, and other times when I don’t have money to come. And when there is no food at home I will be able to get something quick to eat so that I can take my tablets.
Teen interview 5055
Maybe instead of a voucher you can give them a gift card to buy clothes, maybe buy a shirt or a jean and stuff like that… So that others at home wouldn’t feel as much you see being left out as much they can when they buy food, that would better.
Teen interview 2010
Safety in regards to broader health considerations also arose as an influencing factor:
Others… can end up doing bad things with that money that they receive. So - … Like, others - they drink alcohol, other - Others, they do drugs. The person doesn’t just declare to the doctor and say, ‘Ok, I’m now drinking alcohol, I – I’m smoking – I do stuff like that. ’
Teen Interview 1031
Incentive Recipient:
Cash transfer programs often deliver resources to both parents/guardians and adolescents (de Walque et al., 2017); however, some YPLWH indicated that if conditional incentives were to be used in an adherence program, they should be delivered directly to adolescents. It was critical that the power of decision-making and sense of ownership rest with adolescents:
I think that it [the voucher] should be given individually. It should be given like because if it’s given to the families – her family - the fact [is] they didn’t drink the pills; I’m the one who drank the pills, not the [family]. So, the money comes straight to me.
Teen interview 1025
Additionally, adolescents felt that delivery of CEIs to adolescents would re-inforce peer norms:
Mmm, I think that reward will help young people … to take their pills properly.
Mmm, yes, it can help them. … Like, if, like, the person was not drinking the pills properly … like, she was someone who cared about the outside, most of the time – she will change that, she will now care about her life.
Like, she will lag [behind] in the outside matters. She will want to pay attention to her pills and her life. So, I think it will change young people positively. …
[Because] they will be looking forward to – to change their lives, to drink their pills properly.
…. not the improper way they were drinking them in, if [that was the case].
Teen Interview 1031
Program participants:
Some adolescents felt CEIs would work best for adolescents who struggled with adherence. When asked who should participate in a future CEI program, adolescents stated:
It’s the one who is not ‘eating the pills ’
Teen interview 9037
It’s these who are not [taking] the treatment. So that they may also [pull up their socks and] ensure that they [take] the treatment. So that they can also get the reward.
Teen interview 9001
3.2. Results from the discrete choice experiment
Table 2 shows the attributes, description, and levels used in the discrete choice experiment. Adolescents were presented with two programs based on logistical feasibility, which would require either monthly or quarterly clinic visits. Monthly and quarterly visit timeframes were reflective of (1) the schedule of post-ART initiation clinic visits for adolescent patients of Groote Schuur Hospital (Fick et al., 2015), and (2) youth preferences that arose during the IDIs.
Table 2.
Attributes and levels included in the discrete choice experiment
| Attributes | Description | Levels | Number of Levels |
|---|---|---|---|
| 1. Conditional ¶ economic incentive (CEI) amount [yearly‡] | The yearly incentive offer to maintain high adherence to ART (i.e., take pills everyday) | (R0), R240, R480, R960, R1920 | 5 |
| 2. Incentive format | The type or presentation of the incentive | (n/a), cash, food voucher, fashion voucherO | 4 |
| 3. Delivery mode | How the incentive is distributed | (n/a), clinic, virtual/electronic deliveryO | 3 |
| 4. Participants | Who participates in the program | (n/a), adherent & non-adherent youth, non-adherent youth onlyO | 3 |
| 5. CEI recipient | Who receives the incentives§ | (n/a), YLPWH only, YPLWH and parent/caregiverO | 3 |
Notes: Levels in parentheses are the opt-out scenario.
CEI=conditional economic incentives (with conditionality based on viral load testing blood tests); R=South African Rand; ART=antiretroviral treatment as indicated for persons living with HIV; YPLWH=young person(s) living with HIV.
Tasks were originally divided into two parts: participants were asked about a program that requires them to come back to the clinic every month, and then separately they were asked about another potential program that requires them to come back every 3 months (the order of monthly vs. quarterly presentation was randomly varied). For the analysis, the monthly incentive was multiplied by 12 and the quarterly incentive by 4.
The incentive amount given to YPLWH only was specified as equal to the amount given to YPLWH and parent/guardian.
These levels were modelled as the base categories for the dummy-coded (=1) variables in the estimated mixed rank-ordered logit models (Table 3). [Appendix G shows attribute orthogonality and Appendix H shows level balance].
Table 3 shows the DCE results using a mixed rank-ordered logit (MROL) model using the complete ranking data coming from the best–best choices of respondents. In terms of alternative-specific variables, the coefficient on the yearly incentive offer is positive (0.147) and strongly significant, indicating that the probability of choosing an intervention program increases as the incentive offer increases. Similarly, the coefficient on CEI format being in cash is also positive (0.185) and significant indicating that participants (on average) would prefer cash (over a fashion voucher). On the other hand, the coefficient for food vouchers is not significant, indicating no difference in preferences between a food and a fashion voucher (though as explained below there is substantial heterogeneity, thus the null result may be occurring because there are respondents with opposing preferences). Program participants being both those adherent and non-adherent is positive (0.401) meaning that the probability of choosing an intervention program increases if the incentives are targeted to both adherent and non-adherent youth (as opposed to adherent-only youth). CEI delivery at the clinic is preferred (over virtual or electronic delivery) (0.134). Moreover, this mixed logit model reveals substantial heterogeneity as the computed standard deviations (second column) are large relative to the associated means of the random coefficients and these standard deviations are precisely estimated.
Table 3.
Estimated mixed rank-ordered logit (MROL) model#
| Variables^ | MROL choice coeff.§ |
MROL SD¶ |
MROL Program A coeff.‡ |
MROL Opt-out coeff.‡ |
|---|---|---|---|---|
| Alternative-specific variables | ||||
| Yearly offer (R100s) | 0.147*** (0.0119) |
|||
| CEI format is cash (=1) | 0.185** (0.0916) |
0.674*** (0.130) |
||
| CEI format is food voucher (=1) | 0.104 (0.0849) |
0.700*** (0.196) |
||
| CEI recipients are YPLWH only (=1) | −0.00621 (0.0797) |
0.615*** (0.108) |
||
| Program participants are adherent & non-adherent (=1) | 0.401*** (0.0919) |
0.722*** (0.107) |
||
| CEI is delivered at the clinic (=1) | 0.134* (0.0698) |
0.605*** (0.154) |
||
| Case-specific (individual) variables | ||||
| Age (in years) | −0.0248 (0.0473) |
0.556*** (0.208) |
||
| Female (=1) | 0.108 (0.125) |
0.00363 (0.468) |
||
| Years of formal education | 0.0350 (0.0460) |
−0.121 (0.182) |
||
| Index of assets owned in HH | 0.0493 (0.0408) |
0.0646 (0.194) |
||
| Any food insecurity (=1) | −0.0515 (0.142) |
0.687 (0.630) |
||
| Travel time to clinic | −0.0560 (0.0874) |
−0.661** (0.288) |
||
| Ease of taking ART | 0.0291 (0.0561) |
0.552** (0.222) |
||
| Other explanatory variables | ||||
| Quarterly (=1) | −0.200* (0.112) |
−0.170 (0.196) |
||
| Random block | −0.0614 (0.0400) |
0.0632 (0.160) |
||
| Order of presentation is first (=1) | 0.00469 (0.107) |
0.0558 (0.194) |
||
| Constant | 0.345 (0.617) |
−11.58*** (2.409) |
Notes: Robust standard errors in (parentheses)
p<0.01,
p<0.05,
p<0.1
Means of random coefficients for alternative-specific variables.
Standard deviation (SD) of the random coefficients for alternative-specific variables.
Using Program B as reference. A positive (negative) sign for an attribute means that level impacted positively (negatively) on utility and thus increased (reduced) the probability of choosing an alternative with that level.
Number of participants=168; number of observations=13,440; log-likelihood: −2093.
In the estimation, yearly offer (R100s), age, years of formal education, asset index, travel time, difficulty taking ART, and random block were modelled as continuous; other attributes are dummy coded (=1).
CEI=conditional economic incentive; R100s=South African Rand in 100s; YPLWH=young person living with HIV.
Case-specific variables have coefficients that vary across alternatives with those for Program B normalized to zero for the purposes of identification. In terms of case-specific (individual) variables, we do not see differences by gender or education level. Nevertheless, older participants are more likely to opt-out, as are those with greater ease of taking ART; while those having longer time travel to the clinic are less likely to opt-out.
In terms of other explanatory variables, presenting the tasks as a quarterly program did not have a significant effect at conventional levels. The random block that respondents answered and the order in which program type was presented did not affect results either.
Table 4 presents the marginal willingness to accept (mWTA) estimates for a standardized yearly program. From a maximum incentive amount of R1920 (~US$115), participants are willing to forgo up to R126 (~US$9) if the incentive is given in cash (instead of fashion voucher); up to R274(~US$19.6) if the incentive is allocated to adherent & non-adherent youth (instead of to adherent youth only); and up to R91 (~US$6.5) as long as the delivery location is at the clinic (as opposed to virtual or electronic pickup).
Table 4.
Marginal willingness to accept (mWTA) yearly economic incentives conditional on high adherence as verified by blood tests
| Attribute | Improvement in the attribute | mWTA/year (R100s, 95% CI)‡ |
|---|---|---|
| CEI format is in cash | CEI format is in cash instead of fashion voucher | −1.26* (−2.52 to −.003) |
| CEI format is food voucher | CEI format is as food voucher instead of fashion voucher | −0.71 (−1.87 to 0.45) |
| CEI recipients are YPLWH only | CEI recipients are YPLWH only instead of YPLWH and parents/caregivers | 0.04 (−1.02 to 1.11) |
| Program participants are adherent & non-adherent | Participants are adherent & non-adherent instead of non-adherent only | −2.74*** (−4.08 to −1.40) |
| CEI is delivered at the clinic | CEI is delivered at the clinic instead of virtually or electronically | −0.91* (−1.85 to 0.03) |
Notes:
Significant at the level of: p≤0.01,
p≤0.05,
p≤0.1
Computed using robust standard errors from mixed rank-ordered logit model presented in Table 3.
A negative coefficient indicates the incentive amount that a respondent is willing to forego to ensure a given attribute. CEI=conditional economic incentive; YPLWH=young person living with HIV; mWTA=marginal willingness to accept; R100s=South African Rand in 100s; CI=confidence interval.
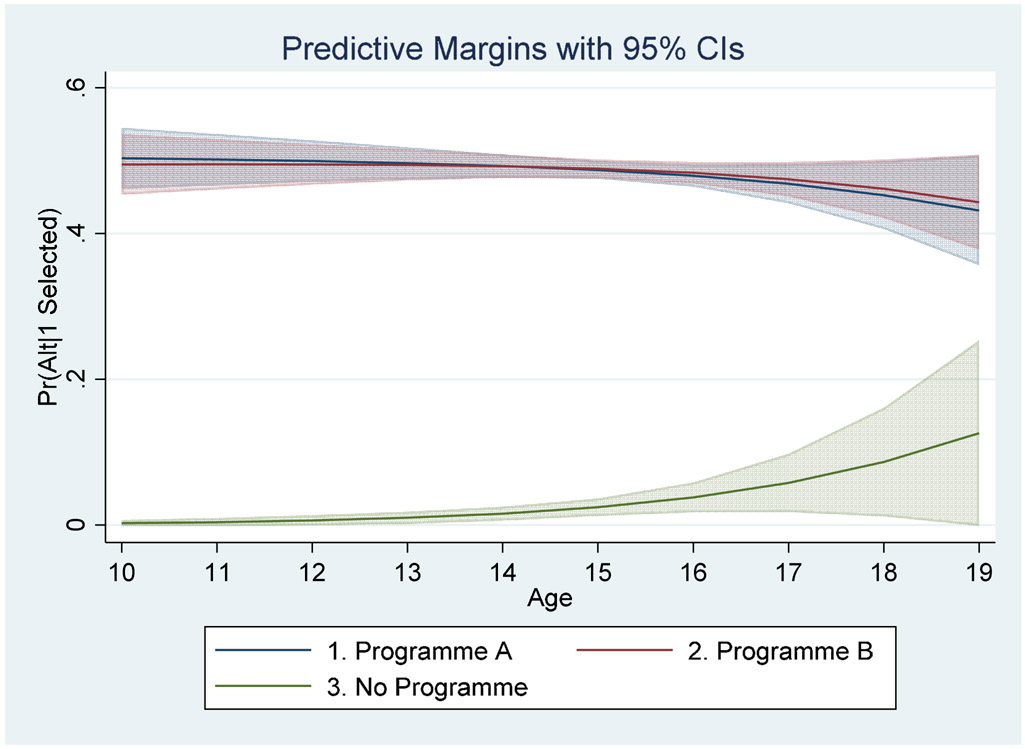
Figure 4 presents the averaged choice probabilities over the entire age range. Both Program A or Program B have (statistically) the same probability of being chosen: 44-50% depending on participants’ age. Thus, most participants would prefer a CEI program (A or B) (with a combined probability of 88-100%). On the contrary, the No Program (opt-out) option has a much lower probability (0-12%) of being chosen.
Figure 4.
Predictive Margins with 95% Confidence Intervals
3.3. Robustness Tests
Appendix E presents estimates for additional models. First, model A is the rank ordered logit (ROL); it shows some similar results as the main model but also differences. Model C is the GMNL, which also had qualitatively similar results as the MROL. The main difference between MROL and GMNL is one additional parameter (τ) allowing for scale heterogeneity. The τ parameter for the GMNL was 0.887 and was highly significant (SE=0.0662 with z=13.4), indicating unobserved heterogeneity. This heterogeneity can be described as scale heterogeneity; that is, with fixed attribute coefficients, the scale of the idiosyncratic error term is greater for some consumers than it is for others.
Appendix F shows the marginal willingness-to-accept estimates for all of the DCE models presented in Appendix E. In model A (ROL), participants are willing to forgo up to R143 (~US$10.21) if the incentive is in cash (instead of fashion voucher); and up to R265(~US$18.9) if the incentive is allocated all adherent & non-adherent youth (instead of to adherent youth only). Model B (MROL results) are the same as presented above in Table 4. Model C (using GMNL) shows that participants would be willing to forgo: R175 (~$12.5) to receive the incentive in cash; R227 (~$16.2) to receive a food voucher (instead of a fashion voucher); R199 (~$14.2) to have the incentive program open to both previously adherent and previously non-adherent youth; and R79 (~$5.6) if the incentive is delivered at the clinic (rather than virtually).
Appendix G presents the correlation matrix to check for orthogonality. The requirement is that levels for each attribute vary independently of each other. The pairwise correlation coefficients were generally low; thus, re-assuring that there was attribute level independence. Finally, Appendix H shows level balance. The level balance of the design applied in this study was generally good, though somewhat imbalanced towards the zero or N/A options. This is because the zero option was included in the active program choices, as well as in the opt-out, and because in the exploded dataset the zero option (or opt-out) was the most common one to be replicated (because 95-99% of initial first-best responses preferred a program over the opt-out).
4. DISCUSSION
Following best practices (Vass et al., 2017), we incorporate extensive qualitative research into a discrete choice experiment to inform future policy decisions regarding how conditional economic incentives can improve adolescent adherence to ART. This research indicates that South African youth would accept conditional economic incentives to help them overcome barriers to adherence. The youth understood and were sympathetic to the idea that adherence would be measured via blood samples (not just self-report), and that a potential consequence for non-adherence may be to lose the incentive. The optimal design of a CEI-based intervention for ART adherence should: (1) deliver CEIs in cash, (2) be available to youth who are adherent and also to youth who are non-adherent to ART, and (3) be delivered in a clinic-setting rather than virtually.
A few points merit discussion. First, economic theory predicts that the marginal utility of CEIs should be parallel for monthly and quarterly visits given equivalent incentives. Our findings are consistent with the theory. After controlling for travel time, the coefficient for quarterly visits was positive but not statistically significant. Following similar work (Terris-Prestholt et al. 2019; Quaife et al. 2018), we added socio-demographic variables and tested how these affect preferences. It is worth noting that older adolescents and those more easily adhering to ART were more likely to opt-out; while those traveling for the longest time to get to the clinic where less likely to do so.
Second, somewhat surprisingly, and despite qualitative findings showing the opposite, YPLWH do not strongly prefer to receive the incentives themselves, and could potentially share them with their parents or caregivers. This is in contrast to the theory of motivation which indicates that incentives, to be most effective, should be received by the individual who has to enact the behavior (Vlaev et al., 2019). If there is no strong preference for delivering CEIs directly to YPLWH, then an entire new area of research opens up to model the full household health production function. One related attribute that was generated during the IDIs, but not included in the DCE, was the potential to administer incentives to youth within a group setting. Where group-based economic incentives have been piloted in similar contexts, clinical attendance increased and perceived internal and external HIV stigma were reduced; no teasing or bullying from group members were reported (Barker et al., 2019; Galárraga et al., 2019). Lastly, in addition to attribute generation for the DCE, the qualitative data shed light on future areas for CEI development. When discussing the ideal format and delivery mode of incentives, youth focused on utility-related drivers such as the ability of a voucher incentive to purchase clothing, or cash incentives to pay for hospital visits or purchase household food. The emphasis on the usefulness of incentives within the context of daily life may imply that CEIs will need to align with youth-specific daily needs - rather than youth ‘desires’ – to be effective. Interview participants repeatedly stated that the purpose of the conditional economic incentive must be clearly explained so that youth do not interpret the incentive as a ‘bribe’ to change their behavior. Research in Uganda (Chamie et al., 2018) reinforces the importance of framing incentives as aiding rather than bribing behavior change. In this study, interviews suggested that CEIs can serve as a temporary reward until medication taking becomes a habit, which further supports explaining CEIs as a short-term mechanism to induce long-term habituation. Explicitly stating the intended goal of the incentive to adolescents – that it is difficult to form and maintain daily ART adherence and CEIs provide additional help to develop this habit – can offset feelings of being bribed. Framing CEIs as a tool for habit formation allows recipients to take control of their medication-taking behaviors while receiving added support, which is especially important for adolescents who are actively developing lifelong routines for their HIV care (Patton et al., 2016).
Strengths and limitations
This research contributes several innovations. First, this research is innovative from the point of view of interventions for adolescent HIV adherence. While one RCT testing CEIs for youth ART adherence is ongoing in Nigeria (Ekwunife et al., 2018), there is limited evidence on the effectiveness of service delivery interventions to support adolescent adherence (Bain-Brickley et al., 2011; Reisner et al., 2009) and no studies have used a DCE approach to inform the optimal design of such interventions. More generally, this study is innovative from the point of view of applying CEIs to promote youth behavior change. Given the unique developmental changes occurring during adolescence, incentives can reinforce or dissuade habit formation during this critical time period (Giles et al., 2016; Teslovich et al., 2014). Furthermore, the youth preferences elicited may be relevant beyond ART adherence, and should be explored within the context of other chronic disease interventions. Lastly, this study contributes to the existing literature from a methodological perspective. The use of (1) in-depth interviews led by trained experts and (2) a two-stage process for attribute generation is consistent with best practice recommendations for employing qualitative methods to inform discrete choice experiments (Coast and Horrocks, 2007). Triangulating findings from interviews, pilot testing and the systematic review served to ensure that the final attributes included in the DCE were context-appropriate and addressable through a single intervention. Integration of these findings with the DCE results also led to a deeper understanding of the study’s overall findings. Additionally, the use of conditional, mixed, and generalized multinomial logit models ensured robustness in estimating average preferences for the observed sample (Johnson et al., 2013). As seen in Figure 4, a program with incentives has a much larger probability of being chosen. Moreover, if there was status quo or left-to-right bias, the probability of choosing No Program would be overestimated (because it was shown at the left, and South Africans read from left to right). Thus, under the presence of status quo or left-to-right bias, the true probability of choosing No Program would be smaller, and that of choosing any program (A or B) would be even larger.
This study has limitations. The pooling of the monthly and quarterly tasks is a convenient modelling choice but it relies on the significance of a dummy indicator for quarterly visits, and hence is a limited test of poolability given that it is conditioned on all other parameters being the same across the two payment types. Moreover, we chose an experimental design where the adherence outcome was held constant and the potential payment varied. That is, the adolescents were instructed to think about the effort required to comply with the doctor’s recommended guidelines (i.e., ‘take your pills every day’). Thus, holding that desired outcome constant (Figure 3), the YPLWH decided on what level of compensation they would most prefer. Another alternative may be to ask participants about potential trade-offs between the rewards and consequences of not sufficiently adhering, in terms of the failure to receive the reward. Another limitation was that some willing participants could not be enrolled due to lack of guardian/parent consent. This was partially due to lengthy and complex consent and assent procedures at Groote Schuur Hospital. Given the limitation that missing parental consent placed on wider recruitment, the generalizability of our findings is limited to those from whom we could obtain consent. Similarly, the sample recruited for the IDIs and DCE was effectively a non-random (convenience) sample that may not be representative of the target population. Furthermore, some attributes that emerged during qualitative analysis were excluded from the DCE to limit respondent fatigue and because select attributes would be difficult to operationalize. For example, the duration of a potential ART adherence program arose during the IDIs but was not included as an attribute in the DCE. Programs that employ CEIs to improve ART adherence vary widely in duration and expense, offering as little as $0.40 per day for less than 6 months to as much as $10 a day over 2 years (McCoy et al., 2017; Silverman et al., 2019). Because program duration will depend on the availability of external funding mechanisms and political will, which are often outside the control of program developers, and because program duration was cited less frequently than other attributes during interviews, we opted to exclude program duration from the DCE. We also excluded hair analysis for adherence verification as a DCE attribute. This was because using hair analyses to verify ART adherence was deemed difficult to operationalize in the target population, where the majority of males and some females would not be able to provide long-enough hair strands for analysis. Lastly, important questions remain for future research: Will the incentives be cost-effective in the long-term? How much improvement in adherence behaviors can be expected from the incentive-based programs?
5. CONCLUSION
Adolescent preferences for programs that employ conditional economic incentives will be based on the optimal combination of amount, timing, delivery modality, and recipient. The use of short-term incentives in the critical age- and developmental-transition, when adolescents begin to take sole responsibility of their medication-taking behaviors, holds great promise for habituating adherence into adulthood.
Discrete choice experiments have strong external validity and high agreement with observed behaviors (Lancsar and Swait, 2014). Using qualitative methods to inform DCE design ensures that attributes are relevant for the target population and increases the generalizability of stated preferences (Coast et al., 2012). Using mixed methods in conjunction with other formative research can improve the efficacy and real world effectiveness of incentive-based programs for young people who are living with HIV, and should be considered for other chronic disease interventions.
Supplementary Material
Highlights.
Young persons living with HIV (YPLWH) endorse conditional economic incentives
YPLWH opine that incentives can help them overcome barriers to treatment adherence
They have strong preferences for higher incentive amounts in cash (vs. vouchers)
They would like to include both previously adherent and non-adherent youth
They have mild preferences for incentives delivered at the clinic (vs. virtually)
ACKNOWLEDGEMENTS
We are grateful for the unwavering support and guidance of Dr. Rudzani Muloiwa, Director of the Pediatric HIV Clinical Services at Groote Schuur Hospital. Computer-assisted questionnaires and programming was expertly done by Timothy Souza and Suzanne Sales. Data collection was done diligently by Mluleki and his team. Excellent research assistance provided by Marta Wilson-Barthes, Ariana Pather and Harini Balakrishnan.
Funding: U.S. National Institutes of Health (NIH) / National Institute of Allergy and Infectious Diseases (R21-AI118393 PIs: Galárraga/Hoare). The funding agency did not have any role in the design, implementation or decision to submit the study results for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Bain-Brickley D, Butler LM, Kennedy GE, Rutherford GW, 2011. Interventions to improve adherence to antiretroviral therapy in children with HIV infection. Cochrane Database Syst. Rev [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker D, Enimil A, Galárraga O, Bosomtwe D, Mensah N, Thamotharan S, Henebeng E, Brown L, Kwara A, 2019. In-Clinic Adolescent Peer Group Support for Engagement in Sub-Saharan Africa: A Feasibility and Acceptability Trial. J. Int. Assoc. Provid. AIDS Care 18, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassani DG, Arora P, Wazny K, Gaffey MF, Lenters L, Bhutta ZA, 2013. Financial incentives and coverage of child health interventions: a systematic review and meta-analysis. BMC Public Health 13, S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Björkman Nyqvist M, Corno L, de Walque D, Svensson J, 2018. Incentivizing Safer Sexual Behavior: Evidence from a Lottery Experiment on HIV Prevention. Am. Econ. J. Appl. Econ 10, 287–314. [Google Scholar]
- Buchanan AL, Montepiedra G, Sirois PA, Kammerer B, Garvie PA, Storm DS, Nichols SL, 2012. Barriers to Medication Adherence in HIV-Infected Children and Youth Based on Self- and Caregiver Report. Pediatrics 129, e1244–e1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlsson F, Martinsson P, 2003. Design techniques for stated preference methods in health economics. Health Econ. 12, 281–294. [DOI] [PubMed] [Google Scholar]
- Chamie G, Schaffer EM, Ndyabakira A, Emperador DM, Kwarisiima D, Camlin CS, Havlir DV, Kahn JG, Kamya MR, Thirumurthy H, 2018. Comparative effectiveness of novel nonmonetary incentives to promote HIV testing. AIDS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark MD, Determann D, Petrou S, Moro D, de Bekker-Grob EW, 2014. Discrete Choice Experiments in Health Economics: A Review of the Literature. Pharmacoeconomics 32, 883–902. [DOI] [PubMed] [Google Scholar]
- Coast J, Al-Janabi H, Sutton EJ, Horrocks SA, Vosper AJ, Swancutt DR, Flynn TN, 2012. Using qualitative methods for attribute development for discrete choice experiments: issues and recommendations. Health Econ. 21, 730–741. [DOI] [PubMed] [Google Scholar]
- Coast J, Horrocks S, 2007. Developing attributes and levels for discrete choice experiments using qualitative methods. J. Heal. Serv. Res. Policy 12, 25–30. [DOI] [PubMed] [Google Scholar]
- Coetzee M, 2013. Finding the benefits: Estimating the impact of the South African child support grant. South African J. Econ [Google Scholar]
- Cresswell JW, Plano Clark VL, 2017. Designing and conducting mixed methods research, 3rd ed. SAGE Publications, Thousand Oaks, CA. [Google Scholar]
- Czaicki NL, Dow WH, Njau PF, McCoy SI, 2018. Do incentives undermine intrinsic motivation? Increases in intrinsic motivation within an incentive-based intervention for people living with HIV in Tanzania. PLoS One 13, e0196616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bekker-Grob EW, Donkers B, Jonker MF, Stolk EA, 2015. Sample Size Requirements for Discrete-Choice Experiments in Healthcare: a Practical Guide. Patient - Patient-Centered Outcomes Res. 8, 373–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bekker-Grob EW, Hol L, Donkers B, Van Dam L, Habbema JDF, Van Leerdam ME, Kuipers EJ, Essink-Bot ML, Steyerberg EW, 2010. Labeled versus unlabeled discrete choice experiments in health economics: An application to colorectal cancer screening. Value Heal. 13, 315–323. [DOI] [PubMed] [Google Scholar]
- de Bekker-Grob EW, Ryan M, Gerard K, 2012. Discrete choice experiments in health economics: a review of the literature. Health Econ. 21, 145–172. [DOI] [PubMed] [Google Scholar]
- De Brún A, Flynn D, Ternent L, Price CI, Rodgers H, Ford GA, Rudd M, Lancsar E, Simpson S, Teah J, Thomson RG, 2018. A novel design process for selection of attributes for inclusion in discrete choice experiments: Case study exploring variation in clinical decision-making about thrombolysis in the treatment of acute ischaemic stroke. BMC Health Serv. Res 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Walque D. de, Fernald L, Gertler P, Hidrobo M, 2017. Cash Transfers and Child and Adolescent Development, in: Bundy D, Silva N, Horton S, Jamison D, Patton G (Eds.), Child and Adolescent Health and Development. The World Bank, Washington, DC. [PubMed] [Google Scholar]
- Drukker DM, Gates R, 2006. Generating Halton sequences using Mata. Stata J. 6, 214–228. [Google Scholar]
- Eisinger R, Dieffenbach C, Fauci A, 2019. HIV Viral Load and Transmissibility of HIV Infection: Undetectable Equals Untransmittable. JAMA 321, 451–452. [DOI] [PubMed] [Google Scholar]
- Ekwunife OI, Anetoh MU, Kalu SO, Ele PU, Eleje GU, 2018. Conditional economic incentives and motivational interviewing to improve adolescents’ retention in HIV care and adherence to antiretroviral therapy in Southeast Nigeria: study protocol for a cluster randomised trial. Trials 19, 710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sadr WM, Donnell D, Beauchamp G, Hall HI, Torian LV, Zingman B, Lum G, Kharfen M, Elion R, Leider J, Gordin FM, Elharrar V, Burns D, Zerbe A, Gamble T, Branson B, 2017. Financial Incentives for Linkage to Care and Viral Suppression Among HIV-Positive Patients. JAMA Intern. Med 177, 1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis AR, Howard K, Thomas KC, Bekker-Grob E.W. de, Ryan M, Lancsar E, Rose JM, 2019. Number of Halton draws required for valid random parameter estimation with discrete choice data, in: International Health Economics Association (IHEA) Meetings. Basel, Switzerland. [Google Scholar]
- Farber S, Tate J, Frank C, Ardito D, Kozal M, Justice AC, Scott Braithwaite R, 2013. A Study of Financial Incentives to Reduce Plasma HIV RNA Among Patients in Care. AIDS Behav. 17, 2293–2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fick C, Fairlie L, Moultrie H, Woollett N, Pahad K, Thomson K, Pleaner M, 2015. Working with adolescents living with HIV: A handbook for healthcare providers. Johannesburg: Wits RHI and Southern African HIV Clinicians Society. [Google Scholar]
- Galárraga O, Enimil A, Bosomtwe D, Cao W, Barker DH, 2019. Group-based economic incentives to improve adherence to antiretroviral therapy among youth living with HIV: safety and preliminary efficacy from a pilot trial. Vulnerable Child. Youth Stud 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galárraga O, Genberg BL, Martin RA, Barton Laws M, Wilson IB, 2013. Conditional Economic Incentives to Improve HIV Treatment Adherence: Literature Review and Theoretical Considerations. AIDS Behav. 17, 2283–2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galárraga O, Sosa-Rubí SG, 2019. Conditional economic incentives to improve HIV prevention and treatment in low-income and middle-income countries. Lancet HIV 6, 705–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghijben P, Lancsar E, Zavarsek S, 2014. Preferences for Oral Anticoagulants in Atrial Fibrillation: a Best-Best Discrete Choice Experiment. Pharmacoeconomics 32, 1115–1127. [DOI] [PubMed] [Google Scholar]
- Gibson JM, Rigby D, Polya DA, Russell N, 2016. Discrete Choice Experiments in Developing Countries: Willingness to Pay Versus Willingness to Work. Environ. Resour. Econ 65, 697–721. [Google Scholar]
- Giles EL, Becker F, Ternent L, Sniehotta FF, McColl E, Adams J, 2016. Acceptability of Financial Incentives for Health Behaviours: A Discrete Choice Experiment. PLoS One 11, e0157403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goddard FGB, Delea MG, Sclar GD, Woreta M, Zewudie K, Freeman MC, 2018. Quantifying user preferences for sanitation construction and use: Application of discrete choice experiments in Amhara, Ethiopia. Trop. Med. Int. Heal 23, 1364–1373. [DOI] [PubMed] [Google Scholar]
- Guerriero C, Cairns J, Bianchi F, Cori L, 2017. Are children rational decision makers when they are asked to value their own health? A contingent valuation study conducted with children and their parents. Health Econ. 27, e55–e68. [DOI] [PubMed] [Google Scholar]
- Harbaugh WT, Krause K, Berry TR, 2001. GARP for Kids: On the Development of Rational Choice Behavior. Am. Econ. Rev 91, 1539–1545. [Google Scholar]
- Hole AR, 2017. DCREATE: Stata module to create efficient designs. RePEC; https://econpapers.repec.org/software/bocbocode/S458059.htm (accessed 10.3.19). [Google Scholar]
- Hudelson C, Cluver L, 2015. Factors associated with adherence to antiretroviral therapy among adolescents living with HIV/AIDS in low- and middle-income countries: a systematic review. AIDS Care 27, 805–816. [DOI] [PubMed] [Google Scholar]
- Johnson FR, Lancsar E, Marshall D, Kilambi V, Muhlbacher A, Regier DA, Bresnahan BW, Kanninen B, Bridges JFP, 2013. Constructing Experimental Designs for Discrete-Choice Experiments: Report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Heal. 16, 3–13. [DOI] [PubMed] [Google Scholar]
- Kranzer K, Simms V, Bandason T, Dauya E, McHugh G, Munyati S, Chonzi P, Dakshina S, Mujuru H, Weiss HA, Ferrand RA, 2018. Economic incentives for HIV testing by adolescents in Zimbabwe: A randomised controlled trial. Lancet HIV 5, e79–e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancsar E, Fiebig DG, Hole AR, 2017. Discrete Choice Experiments: A Guide to Model Specification, Estimation and Software. Pharmacoeconomics 35, 697–716. [DOI] [PubMed] [Google Scholar]
- Lancsar E, Swait J, 2014. Reconceptualising the External Validity of Discrete Choice Experiments. Pharmacoeconomics 32, 951–965. [DOI] [PubMed] [Google Scholar]
- Lohmann J, Muula AS, Houlfort N, Allegri M. De, 2018. How does performance-based financing affect health workers’ intrinsic motivation? A Self-Determination Theory-based mixed-methods study in Malawi. Soc. Sci. Med 208, 1–8. [DOI] [PubMed] [Google Scholar]
- Marsh K, Eaton JW, Mahy M, Sabin K, Autenrieth CS, Wanyeki I, Daher J, Ghys PD, 2019. Global, regional and country-level 90–90–90 estimates for 2018. AIDS 33, S213–S226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy SI, Njau PF, Fahey C, Kapologwe N, Kadiyala S, Jewell NP, Dow WH, Padian NS, 2017. Cash vs. food assistance to improve adherence to antiretroviral therapy among HIV-infected adults in Tanzania. AIDS 31, 815–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFadden D, 1974. Conditional Logit Analysis of Qualitative Choice Behavior, in: Zarembka P (Ed.), Frontiers in Econometrics. Academic Press, New York, pp. 105–142. [Google Scholar]
- McFadden D, Train K, 2000. Mixed MNL Models for Discrete Response. J. Appl. Econom 15, 447–470. [Google Scholar]
- Michaels-Igbokwe C, Lagarde M, Cairns J, Terris-Prestholt F, 2014. Using decision mapping to inform the development of a stated choice survey to elicit youth preferences for sexual and reproductive health and HIV services in rural Malawi. Soc. Sci. Med 105, 93–102. [DOI] [PubMed] [Google Scholar]
- Montoy JCC, Dow WH, Kaplan BC, 2018. Cash incentives versus defaults for HIV testing: A randomized clinical trial. PLoS One 13, e0199833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Kuo C, Sosa-Rubí SG, Galárraga O, 2013. Conditional economic incentives for reducing HIV risk behaviors: Integration of psychology and behavioral economics. Heal. Psychol 32, 932–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostermann J, Brown DS, Mühlbacher A, Njau B, Thielman N, 2015. Would you test for 5000 Shillings? HIV risk and willingness to accept HIV testing in Tanzania. Health Econ. Rev [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, Arora M, Azzopardi P, Baldwin W, Bonell C, Kakuma R, Kennedy E, Mahon J, McGovern T, Mokdad AH, Patel V, Petroni S, Reavley N, Taiwo K, Waldfogel J, Wickremarathne D, Barroso C, Bhutta Z, Fatusi AO, Mattoo A, Diers J, Fang J, Ferguson J, Ssewamala F, Viner RM, 2016. Our future: a Lancet commission on adolescent health and wellbeing. Lancet 387, 2423–2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quaife M, Vickerman P, Manian S, Eakle R, Cabrera-Escobar MA, Delany-Moretlwe S, Terris-Prestholt F, 2018. The effect of HIV prevention products on incentives to supply condomless commercial sex among female sex workers in South Africa. Health Econ. 27, 1550–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Mimiaga MJ, Skeer M, Perkovich B, Johnson CV, Safren SA, 2009. A review of HIV antiretroviral adherence and intervention studies among HIV-infected youth. Top. HIV Med 17, 14–25. [PMC free article] [PubMed] [Google Scholar]
- Ridgeway K, Dulli LS, Murray KR, Silverstein H, Dal Santo L, Olsen P, Darrow de Mora D, McCarraher DR, 2018. Interventions to improve antiretroviral therapy adherence among adolescents in low- and middle-income countries: A systematic review of the literature. PLoS One 13, e0189770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan M, Watson V, Entwistle V, 2009. Rationalising the “irrational”: a think aloud study of discrete choice experiment responses. Health Econ. 18, 321–336. [DOI] [PubMed] [Google Scholar]
- Shannon-Baker P, 2016. Making Paradigms Meaningful in Mixed Methods Research. J. Mix. Methods Res 10, 319–334. [Google Scholar]
- Silverman K, Holtyn AF, Rodewald AM, Siliciano RF, Jarvis BP, Subramaniam S, Leoutsakos JM, Getty CA, Ruhs S, Marzinke MA, Fingerhood M, 2019. Incentives for Viral Suppression in People Living with HIV: A Randomized Clinical Trial. AIDS Behav. 23, 2337–2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Amico KR, Smith L, Nelson K, 2010. Antiretroviral Adherence Interventions: Translating Research Findings to the Real World Clinic. Curr. HIV/AIDS Rep 7, 44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoianova M, Tampke EC, Lansing AH, Stanger C, 2018. Delay discounting associated with challenges to treatment adherence and glycemic control in young adults with type 1 diabetes. Behav. Processes 157, 474–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story GW, Vlaev I, Seymour B, Darzi A, Dolan RJ, 2014. Does temporal discounting explain unhealthy behavior? A systematic review and reinforcement learning perspective. Front. Behav. Neurosci. 8, 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss A, Corbin J, 2008. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, 2nd ed, Basics of Qualitative Research Grounded Theory Procedures and Techniques. Sage Publications, Inc., London, UK. [Google Scholar]
- Teslovich T, Mulder M, Franklin NT, Ruberry EJ, Millner A, Somerville LH, Simen P, Durston S, Casey BJ, 2014. Adolescents let sufficient evidence accumulate before making a decision when large incentives are at stake. Dev. Sci [DOI] [PubMed] [Google Scholar]
- Tong A, Sainsbury P, Craig J, 2007. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Heal. Care 19, 349–357. [DOI] [PubMed] [Google Scholar]
- Train KE, 2009. Discrete Choice Methods with Simulation. Cambridge University Press. [Google Scholar]
- Vass C, Rigby D, Payne K, 2017. The Role of Qualitative Research Methods in Discrete Choice Experiments. Med. Decis. Mak 37, 298–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlaev I, King D, Darzi A, Dolan P, 2019. Changing health behaviors using financial incentives: a review from behavioral economics. BMC Public Health 19, 1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitty JA, Walker R, Golenko X, Ratcliffe J, 2014. A Think Aloud Study Comparing the Validity and Acceptability of Discrete Choice and Best Worst Scaling Methods. PLoS One 9, e90635. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.