Abstract
PURPOSE:
A health lifestyles approach holds promise for understanding change in women’s and men’s health behaviors and reducing gendered health disparities. The emerging theoretical and empirical literature on health lifestyles (individuals’ bundled health behaviors that are shaped by group-based identities and norms) helps elucidate complex disparities in health behaviors, but research is needed on how gender shapes the development of health lifestyles. This study proposed and assessed a dynamic multilevel framework for understanding health lifestyles that draws on insights from contemporary gender and life course scholarship.
DATA:
Using the transition from adolescence into adulthood as an empirical case, we analyzed US data from the National Longitudinal Study of Adolescent to Adult Health (Add Health; N=6,605), which followed adolescents through young adulthood, collecting information on their health behaviors and social contexts.
FINDINGS:
Latent class analyses showed that health lifestyles differed significantly by gender. Results supported the dynamic multilevel framework, finding more variation in health lifestyle behaviors within genders than between, high levels of change across ages, intersections of gender with age, and socioeconomic status as a structural pathway for gender’s influence.
CONCLUSION:
Taken together, these findings suggest that conceptualizing gender as a dynamic multilevel system intersecting with other social statuses is fruitful for understanding how health lifestyles form and change. These findings can inform more effective policies to change health behaviors.
Keywords: health lifestyle, gender, gender system, health behavior, Add Health, transition to adulthood
Introduction
The relationship between gender and health is complex, with mortality differences favoring women in many contexts but disparities in many morbidities favoring men (Bird & Rieker, 1999; Springer, Hankivsky, & Bates, 2012). Sometimes aligned with biological sex but transcending it, gender is “an institutionalized system of social practices for constituting people as two significantly different categories, men and women, and organizing social relations of inequality on the basis of that difference” (Ridgeway & Cornell, 2004:510). Gender differences in health behaviors have received considerable research attention—although nonbinary understandings of gender are woefully understudied, a problem our study reflects because of data limitations. A vast literature documents gender differences in prevalences of health behaviors (e.g., Byrnes, Miller, & Schafer, 1999; Pampel, 2001; Umberson, 1992). Cross-cultural variations in disparities suggest that social, and not just biological, factors are important for understanding gender differences in health behaviors. For example, gender disparities in cigarette smoking vary widely cross-nationally. In Sweden, nearly 20% more women than men smoke cigarettes, but these proportions are reversed in the United States, and in Japan about 4 times as many men as women smoke (Hitchman & Fong, 2011).
In the US context, Cockerham (2018) summarized research finding that women often engage in healthier behaviors than men, except for physical activity which favors men. Byrnes and colleagues (1999) found in a meta-analysis that on average, men engaged in riskier substance use, sexual activities, and driving. As Byrnes et al. noted, researchers’ portrayals of gender differences in health behaviors often downplay considerable differences across ages and social contexts. This focus on average gender differences and specific health behaviors does not attend to how an individual’s many health behaviors relate to each other, the social group memberships that may shape interrelated health behaviors, and the unique implications the bundling of health behaviors may have for health.
The relatively new, increasingly influential health lifestyles perspective (Cockerham, 2005; Frohlich & Potvin, 1999; Korp, 2008) has been proposed as a theoretical framework for understanding gendered health behaviors that addresses these shortcomings (Cockerham, 2018; Cockerham, Hinote, & Abbott, 2006). Health lifestyle theory views health lifestyles as the intersection of “life chances” and “life choices” (Cockerham, 2005). Gender is theorized as a sociodemographic factor that structures people’s life chances, providing them with specific lifestyle options according to social group memberships, among which they can choose. This perspective emphasizes the utility of examining health behaviors not singly as if they occur in a vacuum, but as bundles of health behaviors shaped by group-based identities, norms, and understandings of health (Cockerham, 2005; Krueger, Bhaloo, & Rosenau, 2009). Examining individuals’ many health behaviors together may help explain why specific health behaviors are often highly resistant to change and strongly influenced by social group memberships such as gender.
A new and growing body of research has used latent class analysis to identify prevalent health lifestyles among US adolescents and young adults (Burdette, Needham, Taylor, & Hill, 2017; Lawrence, Mollborn, & Hummer, 2017; Mize, 2017; Olson, Hummer, & Harris, 2017). Some studies have used a wide variety of health behaviors to operationalize lifestyles, while others have focused on a few specific domains. Across studies, health lifestyles are often discordant, combining healthier and unhealthier behaviors in the same person; typically involve unhealthier behaviors in young adulthood compared to adolescence; and predict health outcomes. Research on health lifestyles in childhood and adolescence has emphasized changes in influential social contexts as people age, with early family influences later joined by schools and peers (Mollborn & Lawrence, 2018). In the transition to adulthood, we further expect work contexts and transitions to adult roles to matter for health lifestyles (Benson, 2014). A life course approach to understanding health lifestyles thus has robust support, but scholarship on gender and health lifestyles is much less common.
We draw on insights from gender and life course scholarship to propose and assess a dynamic multilevel framework for understanding how gender shapes health lifestyles. Extant health lifestyle theory on gender is firmly rooted in the gender socialization perspective (Cockerham, 2018), which focuses on individuals being taught cultural messages around femininity and masculinity and which contemporary gender scholarship views as overly static and individual-focused. We develop a framework that includes gender-based socialization but also emphasizes change across the life course, incorporates meso- and macro-level influences, and considers intersections with other social statuses. We examine predominant health lifestyles among a nationally representative sample of young US women and men using latent class analyses, following them as they age from adolescence into early, then late, young adulthood, capitalizing on that life phase’s proximity to early socialization processes and frequent contextual changes (Rindfuss, 1991). The resulting insights may help explain gender disparities in health and could apply to other social statuses, improving broader understanding of health lifestyles.
Theory and Background
Although gender has been included as a demographic predictor in research on health lifestyles (rather than specific health behaviors), it has rarely been a primary focus in empirical research (see Cockerham et al., 2006; Olson et al., 2017; Södergren et al., 2014 for exceptions). Explicit theorizing how and why gender influences health lifestyles is even rarer. Cockerham (2018) proposed an enduring “gender-specific habitus,” a “cognitive map or mental set of perceptions routinely guiding and evaluating a person’s choices and options” (145) that develops early in life through gendered socialization. This socialization by parents as well as other adults, peers, and media results in innate behavior differences between women and men that transcend social class. Gendered norms and messages are communicated to children early in life, shaping their self-perceptions and behaviors (Weber et al., 2019). Through differential shaping of personal characteristics, gender generates internalized inequalities (England, 2016). Gender socialization and the internalization of masculinity and femininity have been linked to health and health behaviors (Mahalik, Burns, & Syzdek, 2007; Rosenfield & Mouzon, 2013), sometimes in explicit contrast to biological explanations for sex differences (Bird & Rieker, 1999). For example, socialization into hegemonic masculinity encourages men to engage in certain risky health behaviors (Springer & Mouzon, 2011). Importantly, many gender scholars have critiqued the socialization perspective as overly deterministic and not reflective of or helpful for understanding substantial empirical variations in behaviors within genders (e.g., Maccoby & Jacklin, 1974).
Contemporary gender scholarship often focuses on fluidity, context, and agency more than stability and socialization. We apply to health lifestyles three key insights theoretically developed and empirically supported by gender research (Grollman, 2014; Hamil-Luker & O'Rand, 2007; Moen & Chermack, 2005; Van Horne, Wiemann, Berenson, Horwitz, & Volk, 2009; Viner et al., 2012).
First, gender is a powerful multilevel system of social categorization that shapes individuals through institutional-, interactional-, and individual-level pathways (Risman, 2004). Materially, women’s access to socioeconomic resources, institutions, and social groups is limited compared to men. Socially, gender influences group-based identities, norms, and behaviors in interpersonal interactions, resulting in people “doing gender,” for example in the gendering of marital and parental roles adopted in adulthood (Umberson, Crosnoe, & Reczek, 2010; West & Zimmerman, 1987). In other words, the multilevel perspective views socialization as one small piece of the puzzle that is not rigidly deterministic of future behavior. In one example, Homan (2019) measured structural sexism at the macro, meso, and micro levels. Macrolevel structural sexism predicted worse health for women and men, mesolevel structural sexism within marriages benefitted men’s health and harmed women, and internalized sexism did not predict women’s or men’s health. This multilevel approach was fundamental for understanding gender and health.
Second, gender scholarship has long found that emphasizing gender differences in behavior obscures the fact that differences between genders in human behavior are greatly outweighed by differences within genders (Hyde, 2005). Changing social contexts and other social statuses shape how the multilevel gender system shapes individual lives (Risman, 2004). For example, Byrnes and colleagues’ (1999, p. 377) meta-analysis of gender and risk-taking included many health behaviors. They found that some risk-taking behaviors were more prevalent among women, others among men, and many gender differences shifted with age, concluding that risk taking does not appear to be a stable product of “masculine psychology.”
The third insight is the intersection of gender with other social statuses (Crenshaw, 1991; Schilt & Westbrook, 2009; Springer & Mouzon, 2011). The intersectionality perspective would not expect a gender-specific habitus to operate independently from intersecting characteristics such as age, socioeconomic status, sexuality, parental socioeconomic background, and race/ethnicity. For example, Armstrong, Hamilton, and Sweeney’s (2006) analysis of campus sexual assaults identified that gender’s intersection with social class, race, age, and sexual orientation increased particular college students’ risk for victimization. The power and privilege of upper-class, white-dominated fraternities with their own houses were fundamental for shaping the ecosystem of sexual assault, from physical spaces to normative expectations.
One of these social statuses—age—is a focus of the multidisciplinary life course perspective (Elder, Johnson, & Crosnoe, 2003), which like gender scholarship includes individual-level processes but also looks to meso- and macrolevel determinants of health (Corna, 2013). This perspective would expect gender and age to intersect in shaping health lifestyles. Gender disparities should emerge, change, or even reverse as people age. Life course research has shown that the transition into adulthood is particularly important to study because of rapid change in behaviors, social contexts, and social position and because of the transition’s “demographic density”—with frequent, often co-occurring changes in migration, fertility, marriage, schooling, and paid work (Benson, 2014; Rindfuss, 1991). Indeed, health lifestyles research examining the transition to adulthood has identified considerable change in individuals’ health lifestyles and their relationships to social characteristics (Burdette et al., 2017; Lawrence et al., 2017; Mize, 2017; Olson et al., 2017). For these reasons, we focus on the transition from adolescence to young adulthood, including changes in socioeconomic attainment and marital and parental roles, to understand the development of gendered health lifestyles.
The Current Study
Our analyses directly or indirectly assess several predictions derived from the above insights. First, health lifestyles are expected to be distinguishable by gender. Second, differences in understandings of gender, structural influences, and social contexts are expected to produce substantial variation in health lifestyles within genders. Third, the gendering of health lifestyles is expected to change with age, an example of intersections among social statuses. Fourth, gender is expected to shape health lifestyles in part through structural sexism (Homan, 2019) that limits gender equality at the macro, meso, and micro levels. Here, we focus on the gendering of socioeconomic attainment and marital and parental roles, which are often acquired in early adulthood.
Method
Data
Our analyses used longitudinal data from the US-based National Longitudinal Study of Adolescent to Adult Health (Add Health). These data portray a diverse, nationally representative cohort followed from adolescence to young adulthood, capturing detail on many health behaviors. Add Health’s school-based, stratified sample represents all US adolescents in grades 7 through 12 in 1994-95. Respondents completed an in-home interview in 1994-95 and follow-up waves. Wave I (adolescence) surveyed 20,745 adolescents in grades 7–12 (ages 11-19) in 1994-95. We did not use Wave II because only a subsample of individuals was re-interviewed. Wave III (early young adulthood) was conducted in 2001, when respondents were aged 18-28 (99% were 18-25). Wave IV (late young adulthood) surveyed respondents in 2007-08 at ages 24-34 (96% were 26-32). See Harris et al. (2019) or http://www.cpc.unc.edu/projects/addhealth for further details.
Measures
Health lifestyle behaviors.
Following several previous studies in taking a broad approach to operationalizing health lifestyles, we included health behaviors that were available in the data and developmentally appropriate for each age (and thus often changed as adolescents aged into adulthood), representing several domains. See Tables 1-3 for specific categories of each variable.
Table 1A.
Class-conditional response probabilities from latent class analyses for adolescent health lifestyles among MALES (Wave I)
| Male mean |
Femme mean |
Healthy | Mostly healthy, some substance |
Passive | Unhealthy, no substance |
Unhealthy, drinking |
Unhealth y, substanc e |
|
|---|---|---|---|---|---|---|---|---|
| 0.33 | 0.14 | 0.10 | 0.16 | 0.15 | 0.12 | |||
| Physical activity | ||||||||
| # activities (weekly) | ||||||||
| 0 | 0.29 | 0.45 | 0.17 | 0.22 | 0.75 | 0.24 | 0.28 | 0.39 |
| 1-2 | 0.30 | 0.32 | 0.28 | 0.19 | 0.19 | 0.38 | 0.40 | 0.33 |
| 3-15 | 0.41 | 0.23 | 0.55 | 0.58 | 0.06 | 0.38 | 0.33 | 0.29 |
| Screentime (weekly hours) | ||||||||
| 0-14 | 0.41 | 0.53 | 0.47 | 0.36 | 0.38 | 0.29 | 0.44 | 0.48 |
| 14.001-28 | 0.29 | 0.27 | 0.31 | 0.25 | 0.37 | 0.24 | 0.29 | 0.30 |
| 28.001-282 | 0.29 | 0.20 | 0.21 | 0.40 | 0.25 | 0.47 | 0.27 | 0.22 |
| Substance use | ||||||||
| Tobacco use | 0.31 | 0.33 | 0.05 | 0.54 | 0.13 | 0.21 | 0.57 | 0.74 |
| Marijuana use last 30 days | 0.18 | 0.16 | 0.00 | 0.29 | 0.01 | 0.02 | 0.13 | 0.99 |
| Other drug use last 30 days | 0.07 | 0.07 | 0.00 | 0.04 | 0.02 | 0.01 | 0.02 | 0.48 |
| Alcohol | ||||||||
| Nondrinker | 0.46 | 0.45 | 0.75 | 0.12 | 0.64 | 0.77 | 0.00 | 0.10 |
| Drinker | 0.11 | 0.14 | 0.13 | 0.07 | 0.27 | 0.10 | 0.07 | 0.05 |
| Drinker with HED/heavy/problem | 0.42 | 0.41 | 0.13 | 0.81 | 0.09 | 0.13 | 0.93 | 0.85 |
| Diet | ||||||||
| Ate 2 fruits and 2 veg | 0.16 | 0.17 | 0.26 | 0.14 | 0.02 | 0.10 | 0.11 | 0.11 |
| Usually eats breakfast | 0.80 | 0.74 | 0.91 | 0.87 | 0.69 | 0.83 | 0.67 | 0.64 |
| Safety | ||||||||
| Got in fight last year | 0.41 | 0.22 | 0.27 | 0.66 | 0.08 | 0.60 | 0.32 | 0.65 |
| Doesn't always wear helmet | 0.77 | 0.62 | 0.81 | 0.68 | 0.54 | 0.85 | 0.81 | 0.82 |
| Always wears seatbelt | 0.47 | 0.59 | 0.64 | 0.47 | 0.76 | 0.18 | 0.36 | 0.23 |
| Ever driven drunk | 0.09 | 0.06 | 0.00 | 0.06 | 0.00 | 0.00 | 0.29 | 0.33 |
| Healthcare | ||||||||
| Visited doctor | 0.67 | 0.68 | 0.79 | 0.78 | 0.43 | 0.57 | 0.61 | 0.61 |
| Visited dentist | 0.67 | 0.72 | 0.78 | 0.67 | 0.66 | 0.39 | 0.70 | 0.73 |
| Sleep | ||||||||
| 9+ hours sleep | 0.23 | 0.20 | 0.27 | 0.41 | 0.24 | 0.20 | 0.05 | 0.15 |
| Gets enough sleep | 0.74 | 0.67 | 0.86 | 0.94 | 0.72 | 0.71 | 0.52 | 0.53 |
| Sex | ||||||||
| Never had sex | 0.57 | 0.56 | 0.85 | 0.23 | 0.84 | 0.51 | 0.37 | 0.27 |
| Condom | 0.28 | 0.23 | 0.12 | 0.62 | 0.07 | 0.32 | 0.37 | 0.37 |
| Birth control, no condom | 0.03 | 0.05 | 0.01 | 0.00 | 0.01 | 0.02 | 0.07 | 0.06 |
| no contraception | 0.12 | 0.17 | 0.02 | 0.15 | 0.07 | 0.15 | 0.20 | 0.29 |
Source: Add Health
Notes: LCA adjust for clustering and weighting. N=3,174. Italicized means differ significantly by gender at p<.05.
Green/light gray cells represent significantly healthier behaviors than overall mean, red/dark gray significantly unhealthier, bolded are highest/lowest values.
Table 3A.
Class-conditional response probabilities from latent class analyses for late young adult health lifestyles among MALES (Wave IV)
| Male mean |
Female mean |
Healthy but drinking |
Mixed inactive, diet, sleep |
Unhealthy, substance |
|
|---|---|---|---|---|---|
| 0.29 | 0.37 | 0.34 | |||
| Physical activity | |||||
| # activities (weekly) | |||||
| 0 | 0.36 | 0.43 | 0.15 | 0.50 | 0.39 |
| 1-2 | 0.18 | 0.22 | 0.17 | 0.19 | 0.17 |
| 3-15 | 0.46 | 0.34 | 0.68 | 0.31 | 0.43 |
| Screentime (weekly hours) | |||||
| 0-14 | 0.39 | 0.49 | 0.46 | 0.40 | 0.33 |
| 14.001-28 | 0.32 | 0.28 | 0.36 | 0.32 | 0.28 |
| 28.001-282 | 0.29 | 0.22 | 0.19 | 0.28 | 0.39 |
| Walk/bike to work/class | 0.06 | 0.04 | 0.09 | 0.04 | 0.05 |
| Substance use | |||||
| Tobacco use | |||||
| No smoking, no chewing | 0.53 | 0.66 | 0.66 | 0.69 | 0.24 |
| Some smoking/chewing | 0.17 | 0.12 | 0.23 | 0.11 | 0.19 |
| Daily smoking/chewing | 0.30 | 0.22 | 0.11 | 0.21 | 0.56 |
| Marijuana use last 30 days | 0.21 | 0.12 | 0.16 | 0.00 | 0.48 |
| Other drug use last 30 days | 0.08 | 0.05 | 0.04 | 0.00 | 0.20 |
| Alcohol | |||||
| Nondrinker | 0.23 | 0.29 | 0.13 | 0.39 | 0.15 |
| Drinker | 0.19 | 0.28 | 0.19 | 0.28 | 0.09 |
| Drinker with HED/heavy | 0.58 | 0.43 | 0.68 | 0.33 | 0.75 |
| Nutrition | |||||
| Fast food 2+/week | 0.57 | 0.46 | 0.32 | 0.68 | 0.66 |
| SSB 7+/week | 0.63 | 0.53 | 0.32 | 0.74 | 0.78 |
| Safety | |||||
| Serious fight | 0.07 | 0.02 | 0.05 | 0.02 | 0.15 |
| Healthcare | |||||
| Visited doctor | 0.63 | 0.83 | 0.71 | 0.66 | 0.54 |
| Visited dentist | 0.52 | 0.62 | 0.71 | 0.51 | 0.38 |
| Sleep | |||||
| 7+ hours sleep | 0.69 | 0.76 | 0.80 | 0.66 | 0.64 |
| Sex | |||||
| Pay for sex | 0.03 | 0.01 | 0.01 | 0.01 | 0.06 |
| 2+ sex partners last year | 0.31 | 0.22 | 0.25 | 0.19 | 0.48 |
Source: Add Health.
Notes: LCA adjust for clustering and weighting. N=3,174. Italicized means differ significantly by gender at p<.05.
Green/light gray cells represent significantly healthier behaviors than overall mean, red/dark gray significantly unhealthier, bolded are highest/lowest values.
Physical activity: (1) a count of activities in the past week; (2) hours of screentime in the past week; (3) spending at least 40 hours/week seated for work and/or school (Wave III); (4) usually walking or biking to work and/or school (Wave IV). Substance use: (1-3) tobacco, marijuana, and illegal drug use in the past 30 days; (4) alcohol use in the last year (problem drinking was heavy episodic use, heavy use, or reporting one or more problems from drinking); (5) use of legal performance drugs or athletic performance supplements in the past 30 days (Wave III). Diet: (1) ate 2 vegetables and 2 fruits yesterday (Wave I); (2) usually eats anything for breakfast (Wave I), (3), eating no breakfasts per week compared to any (Wave III); (4) any disordered behaviors to lose weight (Wave III); (5) 0-1 fast food meals in the past week compared to more (Waves III-IV); (6) ≥7 sugary beverages in the past week (Wave IV). Safety: getting in a [Wave IV: “serious”] physical fight in the past year (Waves I, IV); (2) riding a bicycle or motorcycle without a helmet (Wave I), (3) always wearing a seatbelt (Wave I), (4) ever having driven drunk (Wave I). Healthcare: (1) having a doctor checkup in the past year, (2) visiting a dentist in the past year. Sleep: (1) sleep duration at or above recommended minimums, (2) reporting usually getting enough sleep (Wave I). Sexual risk: (1) never having had sex versus at most recent intercourse, using a condom, using other contraception but no condom, or not using any contraception (Wave I); (2) having 2 or more sex partners in the past year (Waves III-IV); (3) having paid for sex in the past year (Wave IV).
Other measures.
Analyses were split by gender, self-reported as male or female. Nonbinary gender options were not available, limiting our study’s contributions. Socioeconomic status in adolescence captured: (1) parents’ Wave I highest educational degree (using respondent reports if parent reports were missing); (2) household income-to-needs (ratio of household income to US Census-defined poverty threshold). Socioeconomic status in early young adulthood (Wave III) captured: (1) educational degree and enrollment; (2) personal earnings. In late young adulthood (Wave IV), socioeconomic status captured: (1) educational attainment; (2) household income-to-needs ratio. Family formation (Waves III and IV) combined marriage and parenthood. Wave I race/ethnicity used mutually exclusive categories: non-Hispanic White (referred to as White hereafter), non-Hispanic Black (referred to as Black), Hispanic, and other race/ethnicity (Asian/Pacific Islander, Native American/American Indian, or “other”).
Analytic Approach
Following previous research, we used latent class analysis (LCA; see Lanza et al. [2007]) to identify health lifestyles at each developmental stage: late adolescence (age 15-17), early young adulthood (20-24), and late young adulthood (26-31). LCA uses a set of observed indicators to identify a categorical latent variable that is assumed to explain all associations between indicators. LCA is best suited for health lifestyles research because it allows categorical health lifestyles to emerge from the data (Abel, 1991). We used PROC LCA in SAS (Lanza et al., 2007) and accounted for complex survey design and weighting. Because behaviors change substantially across these ages, we restricted all waves’ analyses to those aged 15 to 17 at Wave I. Tests of measurement invariance demonstrated that latent class models separated by age within Wave I better fit the data than pooled ages. Beyond the Wave I age limits and excluding pregnant or “probably pregnant” women (N=254; because pregnancy temporarily changes so many health behaviors, disrupting health lifestyles), all respondents with a valid weight were included (female N=3,431; male N=3,174). Analyses maintained all eligible cases at each wave using full information maximum likelihood (MI in Stata) to account for item missingness. In line with best practices for imputing variables with various distributions (Allison, 2001; White, Royston, & Wood, 2011), we used a chained equations (or fully conditional specification) approach, creating 10 datasets with all variables informing imputation, as well as adolescent body mass index, self-rated health, and depressive symptoms. Less than 4% of values were imputed for parent education, Wave III and IV educational attainment, and Wave III and IV family structure; larger proportions were imputed for adolescent household income (21% males, 24% females), Wave III earnings (14% males, 17% females), and Wave IV income (7% males, 6% females).
For each gender at each wave, we chose the best-fitting number of classes based on substantive interpretation and fit statistics including the G2, AIC, and BIC (see Table A2). We then predicted these class memberships based on current and past waves’ socioeconomic status, family formation, and race/ethnicity. We chose this stepwise approach because identifying classes and their associations concurrently would have produced health lifestyle classes that were conditional on the associations. Our approach of assigning class membership has misclassification bias that has been shown to produce underestimated associations (Bolck, Croon, & Hagenaars, 2004), likely making our significance tests conservative.
Results
First, we expected that health lifestyles are distinguishable by gender. Tests of measurement invariance (see Table A1) found that LCA stratified by gender better fit the data than pooled analyses at all three waves. Six health lifestyles classes emerged for adolescent. boys and four for girls (Wave I; age 15-17), four classes emerged for each gender in early young adulthood (Wave III; age 20-24), and three and four classes emerged respectively in late young adulthood (Wave IV; age 26-31). Tables 1-3 present means and class-conditional response probabilities, displaying patterns of health behaviors by gender and for each gendered latent class.
Our analyses identified distinct latent classes by gender, not only in the number of classes but also in their composition. For example, the combination of substance use with an individual’s other health behaviors differed by gender. Adolescent girls who did not use substances were concentrated in a single “healthy” lifestyle class (Table 1B). In contrast, boys who did not use substances were split across one healthy, one unhealthy, and one “passive” lifestyle class (Table 1A). Heavy or problem drinking co-occurred with marijuana and other drug use in a small class for both adolescent girls and boys. But for girls, problem drinking and safety concerns always co-occurred in those same classes, whereas they were sometimes distinct for boys. For boys, heavy/problem drinking was featured in an otherwise “mostly healthy” class. In contrast, binge drinking did not co-occur with mostly healthy behaviors for girls.
Table 1B.
Class-conditional response probabilities from latent class analyses for adolescent health lifestyles among FEMALES (Wave I)
| Female mean |
Male mean |
Healthy | Mixed active but sleep problems |
Unhealthy, inactive/diet |
Unhealthy, substance |
|
|---|---|---|---|---|---|---|
| 0.52 | 0.18 | 0.22 | 0.09 | |||
| Physical activity | ||||||
| # activities (weekly) | ||||||
| 0 | 0.45 | 0.29 | 0.44 | 0.27 | 0.60 | 0.51 |
| 1-2 | 0.32 | 0.30 | 0.32 | 0.34 | 0.30 | 0.34 |
| 3-15 | 0.23 | 0.41 | 0.25 | 0.39 | 0.10 | 0.15 |
| Screentime (weekly hours) | ||||||
| 0-14 | 0.53 | 0.41 | 0.53 | 0.66 | 0.42 | 0.61 |
| 14.001-28 | 0.27 | 0.29 | 0.29 | 0.23 | 0.24 | 0.27 |
| 28.001-282 | 0.20 | 0.29 | 0.18 | 0.11 | 0.35 | 0.12 |
| Substance use | ||||||
| Tobacco use | 0.33 | 0.31 | 0.05 | 0.58 | 0.54 | 0.96 |
| Marijuana use last 30 days | 0.16 | 0.18 | 0.00 | 0.25 | 0.17 | 0.94 |
| Other drug use last 30 days | 0.07 | 0.07 | 0.00 | 0.05 | 0.03 | 0.56 |
| Alcohol | ||||||
| Nondrinker | 0.45 | 0.46 | 0.74 | 0.05 | 0.26 | 0.00 |
| Drinker | 0.14 | 0.11 | 0.19 | 0.10 | 0.13 | 0.01 |
| Drinker with HED/heavy/problem | 0.41 | 0.42 | 0.07 | 0.84 | 0.61 | 0.99 |
| Diet | ||||||
| Ate 2 fruits and 2 veg | 0.17 | 0.16 | 0.20 | 0.23 | 0.05 | 0.16 |
| Usually eats breakfast | 0.74 | 0.80 | 0.80 | 0.78 | 0.62 | 0.65 |
| Safety | ||||||
| Got in fight last year | 0.22 | 0.41 | 0.11 | 0.20 | 0.43 | 0.30 |
| Doesn't always wear helmet | 0.62 | 0.77 | 0.63 | 0.70 | 0.52 | 0.66 |
| Always wears seatbelt | 0.59 | 0.47 | 0.71 | 0.66 | 0.35 | 0.37 |
| Ever driven drunk | 0.06 | 0.09 | 0.00 | 0.10 | 0.07 | 0.27 |
| Healthcare | ||||||
| Visited doctor | 0.68 | 0.67 | 0.67 | 0.79 | 0.58 | 0.71 |
| Visited dentist | 0.72 | 0.67 | 0.74 | 0.90 | 0.51 | 0.77 |
| Sleep | ||||||
| 9+ hours sleep | 0.20 | 0.23 | 0.22 | 0.12 | 0.23 | 0.18 |
| Gets enough sleep | 0.67 | 0.74 | 0.72 | 0.58 | 0.66 | 0.50 |
| Sex | ||||||
| Never had sex | 0.56 | 0.57 | 0.79 | 0.48 | 0.22 | 0.20 |
| Condom | 0.23 | 0.28 | 0.13 | 0.28 | 0.33 | 0.40 |
| Birth control, no condom | 0.05 | 0.03 | 0.02 | 0.05 | 0.07 | 0.16 |
| no contraception | 0.17 | 0.12 | 0.05 | 0.19 | 0.38 | 0.25 |
Source: Add Health.
Notes: LCA adjust for clustering and weighting. N=3,431. Italicized means differ significantly by gender at p<.05. Green/light gray cells represent significantly healthier behaviors than overall mean, red/dark gray significantly unhealthier, bolded are highest/lowest values.
Finally, there were gender differences in the prevalence of different lifestyle classes, as well as number and composition. For example, in late young adulthood (Table 3), two-thirds of women belonged to one of two mostly healthy lifestyle classes. Less than half that proportion (29%) of late young adult men belonged to the only mostly healthy class.
Second, we expected variation in health lifestyles within as well as between genders. Tables 1-3 present male and female means for each indicator, with italics representing statistically significant gender differences. We compared the magnitude of differences between women and men to means for that indicator for each of the gendered latent classes. Across all waves and most health behavior indicators, differences within genders were substantially larger than differences between genders represented by female and male means. For example, at Wave I, 29% of boys and 45% of girls were physically inactive. But within boys, lifestyle class means ranged from 17% to 75% inactive, and girls’ lifestyle class means ranged from 27% to 60% inactive, suggesting far greater variation within genders than between them. Although physical inactivity levels increased in early young adulthood and returned to a similar baseline in late young adulthood, the significant average gender difference remained and was outstripped by much more substantial variation across lifestyle classes within each gender.
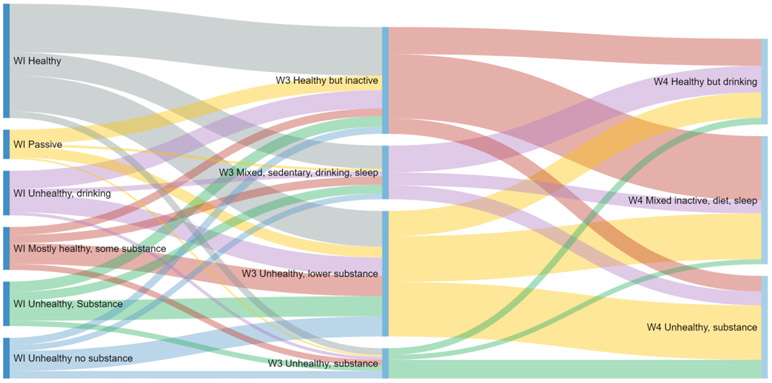
Third, we expected that the gendering of health lifestyles intersects with age. Figure 1 graphically depicts high levels of change in health lifestyles across the transition to adulthood, with relatively few respondents remaining in similar lifestyles across waves. For both women and men, in early young adulthood the majority of health lifestyle classes were mixed or unhealthy and involved high levels of problem drinking and/or other substance use. Most respondents (56% of women and 67% of men) were in these lifestyle classes, a considerable shift compared to adolescence, when the majority of girls and boys were in healthy and mostly healthy lifestyle classes. By late young adulthood, a gendered pattern had emerged, with most women in mostly healthy lifestyle classes, a pattern which was not similar for men. Across these life stages, only three health behaviors displayed a consistently significant gender difference: screentime favoring women, physical activities favoring men, and dentist visits favoring women. Other health behaviors displayed inconsistencies over time in their relationships with gender, solidifying into a well-recognized gendered pattern only in late young adulthood (though even that pattern, based on average behaviors, obscured much greater intragender variation across lifestyle classes).
Figure 1a.
Health Lifestyles at Waves I, III, IV: Males
Notes: Adjusted for complex sampling design. Standard errors in parentheses. N=3,147. Diagram created using SankeyMATIC (Bogart, 2017).
Source: Add Health.
Fourth, we expected structural sexism to shape health lifestyles in part through individuals’ socioeconomic status and family roles. Significance tests for gender differences in overall means (Table 4) show that although there were not gender differences in socioeconomic status in adolescence, they began to emerge across the transition to adulthood. In early young adulthood, a significantly higher proportion of men than women were not in school and had not received a Bachelor’s degree. By late young adulthood, this had translated into an educational disparity favoring women: 71% of women had education levels exceeding a high school diploma, compared to 60% of men. Yet despite higher educational attainment, women’s household incomes were substantially lower. Men’s average household income-to-needs ratio was 414% of the poverty line at Wave IV, compared to 369% for women. This disparity is noteworthy because the income-to-needs ratio adjusts for household size, thereby largely accounting for women’s higher prevalence of marriage and living with children.
Table 4.
Means for independent variables, across health lifestyles
| MALES (N=3,174) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WAVE I | WAVE III | WAVE IV | ||||||||||||
| Overall | Healthy | Mostly healthy, some substance |
Passive | Unhealthy, no substance |
Unhealthy, drinking |
Unhealthy, substance |
Healthy but inactive |
Mixed sedentary, drinking, sleep |
Unhealthy, lower substance |
Unhealthy, substance |
Healthy but drinking |
Mixed inactive, diet, sleep |
Unhealthy, substance |
|
| 33% | 14% | 10% | 16% | 15% | 12% | 33% | 18% | 37% | 12% | 29% | 37% | 34% | ||
| WI race/ethnicity | ||||||||||||||
| White | 0.68 | 0.68 | 0.65 | 0.73 | 0.52 | 0.75 | 0.72 | 0.58 | 0.79 | 0.70 | 0.72 | 0.73 | 0.63 | 0.69 |
| Black | 0.15 | 0.14 | 0.18 | 0.09 | 0.30 | 0.09 | 0.12 | 0.21 | 0.09 | 0.15 | 0.09 | 0.12 | 0.19 | 0.14 |
| Hispanic | 0.12 | 0.11 | 0.13 | 0.13 | 0.12 | 0.13 | 0.12 | 0.14 | 0.09 | 0.11 | 0.12 | 0.10 | 0.13 | 0.12 |
| Other | 0.05 | 0.07 | 0.04 | 0.06 | 0.06 | 0.04 | 0.03 | 0.06 | 0.04 | 0.04 | 0.07 | 0.05 | 0.05 | 0.05 |
| WI parent highest education | ||||||||||||||
| < High school | 0.12 | 0.09 | 0.15 | 0.11 | 0.16 | 0.13 | 0.13 | 0.16 | 0.04 | 0.12 | 0.11 | 0.07 | 0.15 | 0.13 |
| High school | 0.37 | 0.32 | 0.41 | 0.35 | 0.49 | 0.31 | 0.41 | 0.35 | 0.29 | 0.42 | 0.38 | 0.29 | 0.40 | 0.39 |
| Some college | 0.14 | 0.13 | 0.14 | 0.13 | 0.15 | 0.16 | 0.15 | 0.12 | 0.17 | 0.15 | 0.11 | 0.14 | 0.13 | 0.16 |
| BA | 0.25 | 0.28 | 0.24 | 0.24 | 0.16 | 0.25 | 0.23 | 0.24 | 0.32 | 0.21 | 0.28 | 0.31 | 0.21 | 0.23 |
| > BA | 0.12 | 0.17 | 0.06 | 0.15 | 0.04 | 0.15 | 0.09 | 0.13 | 0.17 | 0.10 | 0.11 | 0.20 | 0.10 | 0.08 |
| WI income/needs | 3.06 | 3.27 | 2.74 | 3.15 | 2.11 | 3.72 | 3.05 | 2.75 | 3.95 | 2.92 | 3.16 | 3.74 | 2.80 | 2.81 |
| WIII earnings WIII education | 8.73 | 8.76 | 8.67 | 8.71 | 8.84 | 8.67 | 8.74 | 8.78 | ||||||
| WIII education | ||||||||||||||
| BA degree | 0.09 | 0.10 | 0.16 | 0.06 | 0.06 | 0.17 | 0.08 | 0.04 | ||||||
| Some | ||||||||||||||
| college/enrolled | 0.30 | 0.32 | 0.43 | 0.23 | 0.29 | 0.41 | 0.29 | 0.23 | ||||||
| Not enrolled | 0.61 | 0.58 | 0.40 | 0.71 | 0.65 | 0.42 | 0.64 | 0.73 | ||||||
| WIII family structure | ||||||||||||||
| Married/kids | 0.08 | 0.10 | 0.03 | 0.09 | 0.05 | 0.05 | 0.09 | 0.08 | ||||||
| Married/no kids | 0.07 | 0.09 | 0.07 | 0.05 | 0.05 | 0.06 | 0.09 | 0.04 | ||||||
| Unmarried/kids | 0.06 | 0.06 | 0.03 | 0.07 | 0.04 | 0.03 | 0.05 | 0.09 | ||||||
| Unmarried/no kids | 0.80 | 0.75 | 0.87 | 0.79 | 0.87 | 0.86 | 0.76 | 0.79 | ||||||
| WIV income/needs | 4.14 | 5.11 | 3.94 | 3.56 | ||||||||||
| WIV highest education | ||||||||||||||
| < High school | 0.11 | 0.04 | 0.10 | 0.17 | ||||||||||
| High school | 0.29 | 0.19 | 0.32 | 0.33 | ||||||||||
| Some college | 0.31 | 0.28 | 0.30 | 0.34 | ||||||||||
| BA | 0.24 | 0.38 | 0.23 | 0.14 | ||||||||||
| > BA | 0.06 | 0.11 | 0.05 | 0.02 | ||||||||||
| WIV family structure | ||||||||||||||
| Married/kids | 0.28 | 0.26 | 0.36 | 0.18 | ||||||||||
| Married/no kids | 0.14 | 0.17 | 0.17 | 0.09 | ||||||||||
| Unmarried/kids | 0.10 | 0.06 | 0.11 | 0.12 | ||||||||||
| Unmarried/no kids | 0.48 | 0.51 | 0.37 | 0.60 | ||||||||||
| FEMALES (N=3,431) | ||||||||||||||
| WAVE I | WAVE III | WAVE IV | ||||||||||||
| Overall | Healthy | Mixed active but sleep problems |
Unhealthy, inactive/diet |
Unhealthy, substance |
Healthy but inactive |
Mixed sedentary, drinking |
Unhealthy, inactive/diet |
Unhealthy, substance |
Healthy but drinking |
Healthy but inactive/diet |
Mixed, substance |
Unhealthy | ||
| 52% | 18% | 22% | 9% | 44% | 17% | 28% | 11% | 26% | 41% | 7% | 26% | |||
| WI race/ethnicity | ||||||||||||||
| White | 0.68 | 0.63 | 0.81 | 0.66 | 0.83 | 0.59 | 0.83 | 0.70 | 0.78 | 0.77 | 0.62 | 0.70 | 0.72 | |
| Black | 0.16 | 0.19 | 0.06 | 0.22 | 0.06 | 0.21 | 0.05 | 0.17 | 0.11 | 0.07 | 0.21 | 0.13 | 0.17 | |
| Hispanic | 0.12 | 0.13 | 0.10 | 0.10 | 0.08 | 0.15 | 0.07 | 0.10 | 0.09 | 0.13 | 0.12 | 0.11 | 0.10 | |
| Other | 0.04 | 0.05 | 0.03 | 0.03 | 0.02 | 0.05 | 0.05 | 0.03 | 0.02 | 0.04 | 0.05 | 0.06 | 0.02 | |
| WI parent highest education | ||||||||||||||
| < High school | 0.13 | 0.12 | 0.07 | 0.20 | 0.17 | 0.17 | 0.07 | 0.13 | 0.09 | 0.10 | 0.14 | 0.11 | 0.16 | |
| High school | 0.38 | 0.35 | 0.37 | 0.46 | 0.35 | 0.37 | 0.26 | 0.46 | 0.41 | 0.28 | 0.40 | 0.32 | 0.46 | |
| Some college | 0.15 | 0.16 | 0.13 | 0.14 | 0.12 | 0.15 | 0.14 | 0.13 | 0.14 | 0.14 | 0.14 | 0.14 | 0.16 | |
| BA | 0.22 | 0.24 | 0.23 | 0.14 | 0.26 | 0.21 | 0.29 | 0.18 | 0.24 | 0.25 | 0.22 | 0.31 | 0.16 | |
| > BA | 0.12 | 0.13 | 0.20 | 0.05 | 0.10 | 0.10 | 0.24 | 0.10 | 0.11 | 0.23 | 0.10 | 0.12 | 0.06 | |
| WI income/needs | 3.02 | 3.02 | 3.68 | 2.43 | 3.15 | 2.68 | 4.46 | 2.60 | 3.04 | 3.81 | 2.70 | 3.40 | 2.67 | |
| WIII earnings | 8.58 | 8.55 | 8.51 | 8.58 | 8.81 | 8.62 | 8.47 | 8.41 | 8.79 | |||||
| WIII education | ||||||||||||||
| BA degre | 0.12 | 0.10 | 0.29 | 0.07 | 0.06 | 0.23 | 0.11 | 0.03 | 0.05 | |||||
| some | ||||||||||||||
| college/enrolled | 0.33 | 0.33 | 0.42 | 0.29 | 0.28 | 0.42 | 0.34 | 0.31 | 0.23 | |||||
| Not enrolled | 0.55 | 0.57 | 0.29 | 0.64 | 0.66 | 0.34 | 0.55 | 0.66 | 0.71 | |||||
| WIII family structure | ||||||||||||||
| Married/kids | 0.15 | 0.20 | 0.04 | 0.16 | 0.06 | 0.07 | 0.17 | 0.07 | 0.19 | |||||
| Married/no kids | 0.10 | 0.13 | 0.09 | 0.07 | 0.06 | 0.10 | 0.13 | 0.06 | 0.05 | |||||
| Unmarried/kids | 0.19 | 0.20 | 0.09 | 0.25 | 0.21 | 0.13 | 0.18 | 0.20 | 0.28 | |||||
| Unmarried/no kids | 0.56 | 0.47 | 0.78 | 0.52 | 0.67 | 0.71 | 0.52 | 0.67 | 0.48 | |||||
| WIV income/needs | 3.69 | 5.10 | 3.41 | 3.46 | 2.86 | |||||||||
| WIV highest education | ||||||||||||||
| < High school | 0.07 | 0.02 | 0.07 | 0.09 | 0.12 | |||||||||
| High school | 0.22 | 0.12 | 0.21 | 0.28 | 0.33 | |||||||||
| Some college | 0.35 | 0.31 | 0.35 | 0.38 | 0.36 | |||||||||
| BA | 0.26 | 0.37 | 0.26 | 0.22 | 0.15 | |||||||||
| > BA | 0.10 | 0.18 | 0.10 | 0.03 | 0.04 | |||||||||
| WIV family structure | ||||||||||||||
| Married/kids | 0.36 | 0.28 | 0.47 | 0.18 | 0.29 | |||||||||
| Married/no kids | 0.13 | 0.22 | 0.11 | 0.07 | 0.09 | |||||||||
| Unmarried/kids | 0.22 | 0.12 | 0.21 | 0.28 | 0.34 | |||||||||
| Unmarried/no kids | 0.28 | 0.38 | 0.20 | 0.48 | 0.27 | |||||||||
Source: Add Health.
Notes: Analyses adjust for complex sampling design. Italicized overall means differ significantly by gender at p<.05, bolded are significantly different from that gender’s mean.
In turn, Table 5 shows that these socioeconomic differences have important, though complicated, implications for gendered health lifestyles. The disproportionately male “not in school, no BA” category in early young adulthood was associated with higher odds of some riskier lifestyles and lower odds of others for both women and men, compared to the reference group. By late young adulthood, both income—which advantaged men—and educational attainment—which disadvantaged men—predicted higher odds of a healthier lifestyle for men compared to both less healthy classes. For women in late young adulthood, both income and educational attainment were protective against an unhealthy lifestyle compared to “healthy but drinking,” but socioeconomic measures did not consistently predict membership in the “mixed, substance use” class. In sum, our analyses suggest that gender shapes socioeconomic status, which in turn is associated with health lifestyles, suggesting a complex structural pathway for gender influence on health lifestyles.
Table 5.
Relative risk ratios and 95% CI from multinomial logistic regression, early young adult (Wave III) and late young adult (Wave IV) health lifestyles
| WAVE III MALES N=3,147 (Base outcome: Healthy but inactive) | ||||||
|---|---|---|---|---|---|---|
| Mixed sedentary, drinking, sleep |
Unhealthy, lower substance |
Unhealthy, substance | ||||
| WIII personal earnings WIII education (BA) | 1.00 | 1.00,1.00 | 1.00 | 1.00,1.00 | 1.00 | 1.00,1.00 |
| In school/some college | 0.91 | 0.56,1.49 | 1.24 | 0.72,2.15 | 1.50 | 0.79,2.82 |
| Not in school, no BA | 0.58 | 0.34,0.96 | 2.06 | 1.26,3.35 | 2.05 | 1.10,3.82 |
| WIII family structure (married/children) | ||||||
| Married/no children | 1.91 | 0.77,4.71 | 0.66 | 0.35,1.24 | 1.00 | 0.30,3.33 |
| Not married/children | 1.11 | 0.33,3.69 | 1.08 | 0.55,2.13 | 1.19 | 0.38,3.76 |
| Not married/no children | 2.81 | 1.32,5.95 | 1.50 | 0.96,2.36 | 3.08 | 1.37,6.91 |
| WAVE III FEMALES N=3,431 (Base outcome: Mostly healthy) | ||||||
| Mixed sedentary, drinking |
Unhealthy, inactive/diet |
Unhealthy, substance | ||||
| WIII personal earnings WIII education (BA) | 1.00 | 1.00,1.00 | 1.00 | 1.00,1.00 | 1.00 | 1.00,1.00 |
| In school/some college | 0.68 | 0.46,1.00 | 1.39 | 0.90,2.16 | 1.75 | 0.93,3.30 |
| Not in school, no BA | 0.45 | 0.27,0.75 | 2.07 | 1.33,3.23 | 3.74 | 1.77,7.88 |
| WIII family structure (married/children) | ||||||
| Married/no children | 2.65 | 1.20,5.84 | 0.81 | 0.45,1.48 | 2.14 | 0.98,4.67 |
| Not married/children | 2.40 | 1.20,4.79 | 1.55 | 0.99,2.43 | 3.75 | 1.89,7.46 |
| Not married/no children | 6.40 | 3.43,11.91 | 2.40 | 1.53,3.77 | 10.20 | 5.50,19.04 |
| WAVE IV MALES N=3,147 (Base outcome: Healthy but drinking) | ||||||
| Mixed inactive, diet, sleep | Unhealthy, substance | |||||
| WIV income-to-needs | 0.94 | 0.90,0.98 | 0.92 | 0.86,0.97 | ||
| WIV highest education (<HS) | ||||||
| High school | 0.72 | 0.38,1.37 | 0.60 | 0.30,1.18 | ||
| Some college/enrolled | 0.58 | 0.32,1.04 | 0.52 | 0.27,1.01 | ||
| BA degree | 0.53 | 0.27,1.07 | 0.29 | 0.13,0.67 | ||
| > BA | 0.39 | 0.17,0.91 | 0.22 | 0.08,0.59 | ||
| WIV family structure (married/children) | ||||||
| Married/no children | 1.06 | 0.74,1.53 | 1.38 | 0.81,2.36 | ||
| Not married/children | 1.00 | 0.55,1.80 | 1.95 | 1.06,3.59 | ||
| Not married/no children | 0.67 | 0.48,0.95 | 2.69 | 1.77,4.11 | ||
| WAVE IV FEMALES N=3,431 (Base outcome: Healthy but drinking) | ||||||
| Healthy but inactive/diet | Mixed, substance | Unhealthy | ||||
| WIV income-to-needs | 0.93 | 0.89,0.99 | 0.93 | 0.83,1.05 | 0.88 | 0.82,0.96 |
| WIV highest education (<HS) | ||||||
| High school | 0.51 | 0.23,1.16 | 0.37 | 0.14,0.98 | 0.53 | 0.25,1.10 |
| Some college/enrolled | 0.46 | 0.22,0.97 | 0.28 | 0.09,0.81 | 0.33 | 0.15,0.72 |
| BA degree | 0.63 | 0.26,1.53 | 0.33 | 0.08,1.33 | 0.33 | 0.12,0.88 |
| > BA | 0.59 | 0.25,1.41 | 0.09 | 0.02,0.39 | 0.22 | 0.08,0.61 |
| WIV family structure (married/children) | ||||||
| Married/no children | 0.41 | 0.23,0.73 | 0.91 | 0.39,2.14 | 1.12 | 0.63,1.99 |
| Not married/children | 0.83 | 0.55,1.25 | 2.42 | 1.10,5.31 | 2.10 | 1.27,3.47 |
| Not married/no children | 0.33 | 0.23,0.47 | 2.45 | 1.25,4.79 | 1.48 | 0.91,2.43 |
Source: Add Health.
Notes: Accounts for complex sampling design. Bolded values are significant at p<05. Models also include Wave 1 race/ethnicity, parent highest education, and income-to-needs ratio; all earlier waves’ health lifestyle classes for that gender; and (for Wave IV) Wave III personal earnings, education, and family structure.
Structural sexism may also shape gendered marital and parental roles, which can influence health lifestyles. Women were disproportionately likely to have these roles in young adulthood (Table 4), but family roles’ implications for health lifestyles varied substantially depending on gender, age, and type. In early young adulthood, the combination of marriage and parenthood was protective for some women’s and men’s health lifestyles. For women but not men, experiencing one of these roles in isolation sometimes predicted higher odds of having a riskier health lifestyle compared to having both. By late young adulthood, these relationships were more inconsistent, varying substantially between genders and by family roles and their combination. Results did not identify family roles as a clear pathway through which gender shapes health lifestyles; future research should use more direct mesolevel measures of structural sexism.
Discussion
We articulated and assessed a dynamic multilevel framework, rooted in the gender and life course literatures, for understanding how gender shapes the development of health lifestyles. The framework includes individual socialization and “gender-specific habitus” (Cockerham, 2018), but also expects differences in understandings of gender, structural influences, and social contexts to produce substantial variation in health lifestyles within genders. We analyzed nationally representative US data that followed young people from adolescence across the transition to adulthood—a life stage proximate to early life socialization and entailing substantial shifts in social contexts and roles.
Taken together, findings strongly support our dynamic multilevel framework, speaking to the benefits of drawing on gender and life course scholarship to develop a multifaceted answer to the question of how gender shapes health lifestyles and, ultimately, health outcomes. This study’s results suggest that to best understand gendered health lifestyles, research should conceptualize gender as: (1) a multilevel system ranging beyond individual-level socialization to incorporate interpersonal and structural mechanisms, which leads to effects that are (2) heavily structured by social contexts such as family, available resources, and work roles and (3) dependent on other social statuses such as age, race, sexual orientation, and socioeconomic status. Together, these implications emphasize that the gendering of health lifestyles is: (4) diverse, displaying considerable variation across individuals who identify with the same gender.
As an initial theoretical articulation and test, this study has limitations to address in future research. Our data examined one cohort using national data with widely spaced data collection; gendered health lifestyles might look different for other cohorts or in local contexts. Because of the observational data, associations identified may not be causal. Other health behaviors besides those measured here could be meaningful for health lifestyles. Our measure of gender was dichotomous; future work should consider more complex identities. Analyses explored stability and change, but similarities and differences can be hard to quantify across gender-stratified models when health behaviors vary across waves; future methodological work should address this issue.
This work has implications for research and policy. Because the gendering of health lifestyles is dynamic and varied, health lifestyles research should attend closely to life phase, articulate sources of variation within genders, and use longitudinal data when possible. The importance of a multilevel conceptualization of gender speaks to the need for health lifestyle data that better incorporate meso- and macrolevel factors together with individuals. Because gendered health lifestyles change so much, interventions may be effective later in life and not just at the time of initial gender socialization. And weakening the link between gender and socioeconomic status—for example by addressing gendered wage gaps and motherhood penalties, lower levels of compensation in female-dominated occupations, and the flight of women from male-dominated STEM fields—could lead to health lifestyle changes.
Our approach and findings expand understandings of gender disparities in health. Extant research on gender and discrete health behaviors points to riskier behaviors among men, whereas our study bundles behaviors together and looks within genders and over time. For both genders, unhealthy behaviors often cluster together in health lifestyles that likely result in greater health risks than can be identified by looking at single behaviors in isolation. These unhealthier lifestyles are particularly prevalent among young adult men, and many men shift between different lifestyles that represent varying bundles of health behavior risks. Many women also have unhealthier lifestyles, but a large proportion of women stably remain in healthier lifestyles across the transition to adulthood. Viewing health behaviors through this study’s life course-focused health lifestyles lens emphasizes the limitations of a stable, essentialist approach to understanding gendered health disparities. It also suggests that although time-varying bundles of health behaviors may be useful for explaining some gender disparities such as men’s mortality disadvantage, future research should also examine bundles across the life course to further understand gendered patterns in long-term chronic conditions or morbidities.
Although we focused on gender, this multilevel perspective may also be useful for understanding how other social statuses shape health lifestyles. In understanding racial disparities in health lifestyles, for example, race-based socialization explanations are unlikely to be useful as a primary theoretical lens. Instead, incorporating structural influences of race, its embeddedness in shifting social contexts, and its intersections with other social statuses using the dynamic multilevel framework will provide more leverage. Continuing to integrate insights from gender, life course, race, and other areas of research on inequalities may improve evolving understandings of health lifestyles.
Figure 1b.
Health Lifestyles at Waves I, III, IV: Females
Notes: Adjusted for complex sampling design. Standard errors in parentheses. N=3,431. Diagram created using SankeyMATIC (Bogart, 2017).
Source: Add Health.
Table 2A.
Class-conditional response probabilities from latent class analyses for early young adult health lifestyles among MALES (Wave III)
| Male mean |
Female mean |
Healthy but inactive |
Mixed sedentary, drinking, sleep |
Unhealthy, lower substance |
Unhealthy, substance |
|
|---|---|---|---|---|---|---|
| 0.33 | 0.18 | 0.37 | 0.12 | |||
| Physical activity | ||||||
| # activities (weekly) | ||||||
| 0 | 0.39 | 0.53 | 0.43 | 0.07 | 0.51 | 0.39 |
| 1-2 | 0.19 | 0.18 | 0.17 | 0.19 | 0.21 | 0.18 |
| 3-15 | 0.42 | 0.29 | 0.40 | 0.74 | 0.28 | 0.44 |
| Screentime (weekly hours) | ||||||
| 0-14 | 0.33 | 0.46 | 0.39 | 0.43 | 0.27 | 0.25 |
| 14.001-28 | 0.34 | 0.32 | 0.39 | 0.30 | 0.32 | 0.33 |
| 28.001-282 | 0.33 | 0.22 | 0.22 | 0.27 | 0.42 | 0.43 |
| 40 hours+ seated time | 0.13 | 0.14 | 0.16 | 0.23 | 0.07 | 0.09 |
| Substance use | ||||||
| Tobacco use | ||||||
| No smoking, no chewing | 0.57 | 0.64 | 0.83 | 0.60 | 0.43 | 0.29 |
| some smoking/chewing | 0.14 | 0.12 | 0.08 | 0.20 | 0.13 | 0.23 |
| Daily smoking/chewing | 0.29 | 0.24 | 0.10 | 0.20 | 0.44 | 0.49 |
| Marijuana use last 30 days | 0.28 | 0.17 | 0.01 | 0.30 | 0.34 | 0.81 |
| Other drug use last 30 days | 0.11 | 0.05 | 0.00 | 0.11 | 0.02 | 0.71 |
| Legal performance drugs | 0.16 | 0.01 | 0.03 | 0.41 | 0.09 | 0.36 |
| Alcohol | ||||||
| Nondrinker | 0.22 | 0.26 | 0.46 | 0.01 | 0.017 | 0.07 |
| Drinker | 0.09 | 0.17 | 0.21 | 0.05 | 0.02 | 0.00 |
| Drinker with HED/heavy/problem | 0.69 | 0.57 | 0.33 | 0.93 | 0.81 | 0.93 |
| Nutrition | ||||||
| Fast food (2+/week) | 0.65 | 0.54 | 0.65 | 0.45 | 0.7 | 0.77 |
| Breakfast (any vs. none) | 0.71 | 0.72 | 0.73 | 0.83 | 0.63 | 0.71 |
| Disordered behaviors to lose weight | 0.12 | 0.22 | 0.12 | 0.12 | 0.12 | 0.13 |
| Healthcare | ||||||
| Visited doctor | 0.53 | 0.75 | 0.64 | 0.62 | 0.41 | 0.52 |
| Visited dentist | 0.51 | 0.57 | 0.51 | 0.81 | 0.38 | 0.49 |
| Sleep | ||||||
| 7+ hours sleep | 0.68 | 0.78 | 0.72 | 0.64 | 0.65 | 0.71 |
| Sex | ||||||
| 2+ sex partners last year | 0.34 | 0.24 | 0.13 | 0.48 | 0.37 | 0.58 |
Source: Add Health.
Notes: LCA adjust for clustering and weighting. N=3,174. Italicized means differ significantly by gender at p<.05.
Green/light gray cells represent significantly healthier behaviors than overall mean, red/dark gray significantly unhealthier, bolded are highest/lowest values.
Table 2B.
Class-conditional response probabilities from latent class analyses for early young adult health lifestyles among FEMALES (Wave III)
| Female mean |
Male mean |
Healthy but inactive |
Mixed sedentary, drinking |
Unhealthy, inactive/diet |
Unhealthy, substance |
|
|---|---|---|---|---|---|---|
| 0.44 | 0.17 | 0.28 | 0.11 | |||
| Physical activity | ||||||
| # activities (weekly) | ||||||
| 0 | 0.53 | 0.39 | 0.54 | 0.22 | 0.70 | 0.49 |
| 1-2 | 0.18 | 0.19 | 0.21 | 0.19 | 0.12 | 0.20 |
| 3-15 | 0.29 | 0.42 | 0.24 | 0.59 | 0.17 | 0.31 |
| Screentime (weekly hours) | ||||||
| 0-14 | 0.46 | 0.33 | 0.49 | 0.60 | 0.37 | 0.39 |
| 14.001-28 | 0.32 | 0.34 | 0.30 | 0.35 | 0.32 | 0.34 |
| 28.001-282 | 0.22 | 0.33 | 0.21 | 0.05 | 0.31 | 0.27 |
| 40 hours+ seated time | 0.14 | 0.13 | 0.13 | 0.25 | 0.12 | 0.07 |
| Substance use | ||||||
| Tobacco use | ||||||
| No smoking, no chewing | 0.64 | 0.57 | 0.86 | 0.70 | 0.45 | 0.16 |
| some smoking/chewing | 0.12 | 0.14 | 0.05 | 0.19 | 0.15 | 0.24 |
| Daily smoking/chewing | 0.24 | 0.29 | 0.09 | 0.11 | 0.40 | 0.60 |
| Marijuana use last 30 days | 0.17 | 0.28 | 0.00 | 0.19 | 0.13 | 0.94 |
| Other drug use last 30 days | 0.05 | 0.11 | 0.01 | 0.01 | 0.00 | 0.38 |
| Legal performance drugs | 0.01 | 0.16 | 0.00 | 0.04 | 0.00 | 0.02 |
| Alcohol | ||||||
| Nondrinker | 0.26 | 0.22 | 0.48 | 0.00 | 0.15 | 0.07 |
| Drinker | 0.17 | 0.09 | 0.31 | 0.01 | 0.11 | 0.03 |
| Drinker with HED/heavy/problem | 0.57 | 0.69 | 0.21 | 0.99 | 0.74 | 0.90 |
| Nutrition | ||||||
| Fast food (2+/week) | 0.54 | 0.65 | 0.54 | 0.30 | 0.72 | 0.51 |
| Breakfast (any vs. none) | 0.72 | 0.71 | 0.76 | 0.92 | 0.57 | 0.62 |
| Disordered behaviors to lose weight | 0.22 | 0.12 | 0.16 | 0.18 | 0.29 | 0.31 |
| Healthcare | ||||||
| Visited doctor | 0.75 | 0.53 | 0.77 | 0.80 | 0.73 | 0.63 |
| Visited dentist | 0.57 | 0.51 | 0.59 | 0.82 | 0.45 | 0.45 |
| Sleep | ||||||
| 7+ hours sleep | 0.78 | 0.68 | 0.83 | 0.76 | 0.70 | 0.74 |
| Sex | ||||||
| 2+ sex partners last year | 0.24 | 0.34 | 0.10 | 0.31 | 0.33 | 0.48 |
Source: Add Health.
Notes: LCA adjust for clustering and weighting. N=3,431. Italicized means differ significantly by gender at p<.05.
Green/light gray cells represent significantly healthier behaviors than overall mean, red/dark gray significantly unhealthier, bolded are highest/lowest values.
Table 3B.
Class-conditional response probabilities from latent class analyses for late young adult health lifestyles among FEMALES (Wave IV)
| Female mean |
Male mean |
Healthy but drinking |
Healthy but inactive/diet |
Mixed, substance |
Unhealthy | |
|---|---|---|---|---|---|---|
| 0.26 | 0.41 | 0.07 | 0.26 | |||
| Physical activity | ||||||
| # activities (weekly) | ||||||
| 0 | 0.43 | 0.36 | 0.17 | 0.53 | 0.22 | 0.60 |
| 1-2 | 0.22 | 0.18 | 0.20 | 0.23 | 0.40 | 0.18 |
| 3-15 | 0.34 | 0.46 | 0.62 | 0.24 | 0.38 | 0.22 |
| Screentime (weekly hours) | ||||||
| 0-14 | 0.49 | 0.39 | 0.51 | 0.53 | 0.54 | 0.43 |
| 14.001-28 | 0.28 | 0.32 | 0.34 | 0.30 | 0.23 | 0.21 |
| 28.001-282 | 0.22 | 0.29 | 0.16 | 0.17 | 0.24 | 0.36 |
| Walk/bike to work/class | 0.04 | 0.06 | 0.09 | 0.02 | 0.08 | 0.01 |
| Substance use | ||||||
| Tobacco use | ||||||
| No smoking, no chewing | 0.66 | 0.53 | 0.74 | 0.87 | 0.24 | 0.35 |
| Some smoking/chewing | 0.12 | 0.17 | 0.19 | 0.02 | 0.33 | 0.16 |
| Daily smoking/chewing | 0.22 | 0.30 | 0.07 | 0.11 | 0.43 | 0.48 |
| Marijuana use last 30 days | 0.12 | 0.21 | 0.06 | 0.00 | 0.96 | 0.16 |
| Other drug use last 30 days | 0.05 | 0.08 | 0.02 | 0.00 | 0.36 | 0.07 |
| Alcohol | ||||||
| Nondrinker | 0.29 | 0.23 | 0.15 | 0.43 | 0.07 | 0.27 |
| Drinker | 0.28 | 0.19 | 0.21 | 0.44 | 0.15 | 0.13 |
| Drinker with HED/heavy | 0.43 | 0.58 | 0.64 | 0.14 | 0.78 | 0.60 |
| Nutrition | ||||||
| Fast food 2+/week | 0.46 | 0.57 | 0.18 | 0.54 | 0.33 | 0.65 |
| SSB 7+/week | 0.53 | 0.63 | 0.28 | 0.51 | 0.73 | 0.73 |
| Safety | ||||||
| Serious fight | 0.02 | 0.07 | 0.01 | 0.00 | 0.12 | 0.05 |
| Healthcare | ||||||
| Visited doctor | 0.83 | 0.63 | 0.91 | 0.86 | 0.65 | 0.74 |
| Visited dentist | 0.62 | 0.52 | 0.78 | 0.62 | 0.64 | 0.46 |
| Sleep | ||||||
| 7+ hours sleep | 0.76 | 0.69 | 0.84 | 0.75 | 0.76 | 0.71 |
| Sex | ||||||
| Pay for sex | 0.01 | 0.03 | 0.00 | 0.00 | 0.00 | 0.03 |
| 2+ sex partners last year | 0.22 | 0.31 | 0.18 | 0.08 | 0.50 | 0.38 |
Source: Add Health.
Green/light gray cells represent significantly healthier behaviors than overall mean, red/dark gray significantly unhealthier, bolded are highest/lowest values.
Gender and life course theories help predict health lifestyle formation and change.
Health lifestyle behaviors vary more within than between genders.
Health lifestyles change in gendered ways with age.
Socioeconomic status is a structural pathway for gender’s influence.
Health lifestyle is shaped by a dynamic, multilevel, intersectional gender system.
Acknowledgments
This research is based on work supported by a grant from the National Science Foundation (SES 1423524) and the National Institutes of Health under Ruth L. Kirschstein National Research Service Award (F32HD085599). Research funds were also provided by the NIH/NICHD funded CU Population Center (P2CHD066613). We are grateful to the NICHD-funded Carolina Population Center (P2CHD050924) and the Lund University Centre for Economic Demography for general support. This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available at the Add Health Web site (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis. We thank Richard Jessor, Fred Pampel, and Joshua Goode for their contributions to this study.
Appendix
Table A1.
Comparison of fit statistics for measurement invariance by gender
| G-squared | Degrees of Freedom | |||||
|---|---|---|---|---|---|---|
| Wave 1 | ||||||
| # classes | Model 1 | Model 2 | Difference | Model 1 | Model 2 | Difference |
| 2 | 40523 | 41784 | 1260 | 1769381 | 1769425 | 44 |
| 3 | 39808 | 40757 | 950 | 1769335 | 1769401 | 66 |
| 4 | 39272 | 40196 | 924 | 1769289 | 1769377 | 88 |
| 5 | 38853 | 39736 | 884 | 1769243 | 1769353 | 110 |
| 6 | 38494 | 39312 | 818 | 1769197 | 1769329 | 132 |
| 7 | 38194 | 39033 | 839 | 1769151 | 1769305 | 154 |
| Wave 3 | ||||||
| # classes | Model 1 | Model 2 | Difference | Model 1 | Model 2 | Difference |
| 2 | 27045 | 28274 | 1229 | 331697 | 331735 | 38 |
| 3 | 26365 | 27456 | 1091 | 331657 | 331714 | 57 |
| 4 | 25957 | 26937 | 980 | 331617 | 331693 | 76 |
| 5 | 25669 | 26499 | 829 | 331577 | 331672 | 95 |
| 6 | 25415 | 26200 | 785 | 331537 | 331651 | 114 |
| 7 | 25210 | 26002 | 793 | 331497 | 331630 | 133 |
| Wave 4 | ||||||
| # classes | Model 1 | Model 2 | Difference | Model 1 | Model 2 | Difference |
| 2 | 22479 | 23017 | 537 | 331697 | 331735 | 38 |
| 3 | 21643 | 22282 | 639 | 331657 | 331714 | 57 |
| 4 | 21315 | 21892 | 577 | 331617 | 331693 | 76 |
| 5 | 21053 | 21679 | 626 | 331577 | 331672 | 95 |
| 6 | 20841 | 21500 | 658 | 331537 | 331651 | 114 |
| 7 | 20626 | 21329 | 703 | 331497 | 331630 | 133 |
Notes: Models 1 and 2 are identical, except Model 2 includes measurement invariance for gender when Model 1 does not. Clustering is not used in either of these models, and gender is a grouping variable for both models. For all classes examined at all waves, interpretation of the G-squared statistic (as a chi-square value given the degrees of freedom) indicates a significant difference (p<.01), demonstrating improved model fit for measurement invariance compared to just using gender as a group.
Table A2.
Fit statistics for latent class analysis (LCA): Waves I, III, and IV
| MALES (N=3,174) | FEMALES (N=3,431) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Wave I | Classes | G2 | AIC | BIC | entropy | Classes | G2 | AIC | BIC | entropy |
| 2 | 19660 | 19750 | 20023 | 0.76 | 2 | 20840 | 20930 | 21207 | 0.76 | |
| 3 | 19334 | 19470 | 19882 | 0.73 | 3 | 20448 | 20584 | 21002 | 0.68 | |
| 4 | 19089 | 19271 | 19823 | 0.69 | 4 | 20156 | 20338 | 20897 | 0.70 | |
| 5 | 18872 | 19100 | 19792 | 0.65 | 5 | 19955 | 20183 | 20883 | 0.61 | |
| 6 | 18663 | 18937 | 19767 | 0.63 | 6 | 19811 | 20085 | 20927 | 0.65 | |
| 7 | 18500 | 18820 | 19790 | 0.67 | 7 | 16929 | 17235 | 18175 | 0.64 | |
| 8 | 18378 | 18744 | 19853 | 0.66 | 8 | 19533 | 19899 | 21022 | 0.70 | |
| 9 | 18377 | 18807 | 20111 | 0.66 | 9 | 19909 | 20339 | 21659 | 0.70 | |
| 10 | 18256 | 18734 | 20183 | 0.68 | 10 | 19770 | 20248 | 21715 | 0.73 | |
| Wave III | Classes | G2 | AIC | BIC | entropy | Classes | G2 | AIC | BIC | entropy |
| 2 | 14541 | 14619 | 14856 | 0.56 | 2 | 11914 | 11992 | 12231 | 0.72 | |
| 3 | 14219 | 14337 | 14695 | 0.59 | 3 | 11550 | 11668 | 12031 | 0.69 | |
| 4 | 14049 | 14207 | 14686 | 0.56 | 4 | 11315 | 11473 | 11958 | 0.61 | |
| 5 | 13894 | 14092 | 14692 | 0.56 | 5 | 11188 | 11386 | 11994 | 0.63 | |
| 6 | 13756 | 13994 | 14715 | 0.61 | 6 | 11068 | 11306 | 12037 | 0.61 | |
| 7 | 13664 | 13942 | 14784 | 0.62 | 7 | 10962 | 11240 | 12094 | 0.61 | |
| 8 | 13569 | 13887 | 14851 | 0.66 | 8 | 10863 | 11181 | 12157 | 0.63 | |
| 9 | 13492 | 13850 | 14935 | 0.61 | 9 | 10784 | 11142 | 12241 | 0.64 | |
| 10 | 13402 | 13800 | 15007 | 0.63 | 10 | 10708 | 11106 | 12328 | 0.68 | |
| Wave IV | Classes | G2 | AIC | BIC | entropy | Classes | G2 | AIC | BIC | entropy |
| 2 | 12592 | 12670 | 12907 | 0.5 | 2 | 9666 | 9744 | 9984 | 0.61 | |
| 3 | 12218 | 12336 | 12693 | 0.49 | 3 | 9201 | 9319 | 9681 | 0.55 | |
| 4 | 12076 | 12234 | 12713 | 0.58 | 4 | 9013 | 9171 | 9656 | 0.57 | |
| 5 | 11935 | 12133 | 12733 | 0.55 | 5 | 8894 | 9092 | 9700 | 0.64 | |
| 6 | 11815 | 12053 | 12775 | 0.56 | 6 | 8787 | 9025 | 9756 | 0.62 | |
| 7 | 11702 | 11980 | 12823 | 0.58 | 7 | 8694 | 8972 | 9825 | 0.63 | |
| 8 | 11609 | 11927 | 12891 | 0.60 | 8 | 8598 | 8916 | 9892 | 0.67 | |
| 9 | 11609 | 11927 | 12891 | 0.60 | 9 | 8505 | 8863 | 9962 | 0.66 | |
| 10 | 11434 | 11832 | 13039 | 0.62 | 10 | 8407 | 8805 | 10027 | 0.68 | |
Source: Add Health
Notes: Analyses adjust for complex sampling design. Shaded cells have best BIC fit.
References
- Abel T (1991). Measuring health lifestyles in a comparative analysis: Theoretical issues and empirical findings. Social Science & Medicine, 32(8), 899–908. [DOI] [PubMed] [Google Scholar]
- Allison PD (2001). Missing data (Vol. 136): Sage Publications. [Google Scholar]
- Armstrong EA, Hamilton L, & Sweeney B (2006). Sexual assault on campus: A multilevel, integrative approach to party rape. Social Problems, 53(4), 483–499. [Google Scholar]
- Benson J (2014). Transition to adulthood. In Handbook of child well-being: Theories, methods and policies in global perspective, 1763–1783. [Google Scholar]
- Bird CE, & Rieker PP (1999). Gender matters: an integrated model for understanding men's and women's health. Social Science & Medicine, 48(6), 745–755. [DOI] [PubMed] [Google Scholar]
- Bogart S (2017). SankeyMatic. [Google Scholar]
- Bolck A, Croon M, & Hagenaars J (2004). Estimating latent structure models with categorical variables: One-step versus three-step estimators. Political Analysis, 12(1), 3–27. [Google Scholar]
- Burdette AM, Needham BL, Taylor MG, & Hill TD (2017). Health lifestyles in adolescence and self-rated health into adulthood. Journal of Health and Social Behavior, 58(4), 520–536. [DOI] [PubMed] [Google Scholar]
- Byrnes JP, Miller DC, & Schafer WD (1999). Gender differences in risk taking: A meta-analysis. Psychological Bulletin, 125(3), 367–383. [Google Scholar]
- Cockerham WC (2005). Health lifestyle theory and the convergence of agency and structure. Journal of Health and Social Behavior, 46(1), 51–67. [DOI] [PubMed] [Google Scholar]
- Cockerham WC (2018). Health lifestyles and the search for a concept of a gender-specific habitus. Social Theory & Health, 16(2), 142–155. [Google Scholar]
- Cockerham WC, Hinote BP, & Abbott P (2006). Psychological distress, gender, and health lifestyles in Belarus, Kazakhstan, Russia, and Ukraine. Social Science & Medicine, 63(9), 2381–2394. [DOI] [PubMed] [Google Scholar]
- Corna LM (2013). A life course perspective on socioeconomic inequalities in health: A critical review of conceptual frameworks. Advances in Life Course Research, 18(2), 150–159. [DOI] [PubMed] [Google Scholar]
- Crenshaw K (1991). Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review 43(6), 1241–1299. [Google Scholar]
- Elder GH, Johnson MK, & Crosnoe R (2003). The emergence and development of life course theory In Handbook of the life course (pp. 3–19): Springer. [Google Scholar]
- England P (2016). Sometimes the social becomes personal: Gender, class, and sexualities. American Sociological Review, 81(1), 4–28. [Google Scholar]
- Frohlich KL, & Potvin L (1999). Collective lifestyles as the target for health promotion. Canadian Journal of Public Health, 90, S11–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grollman EA (2014). Multiple disadvantaged statuses and health: The role of multiple forms of discrimination. Journal of Health and Social Behavior, 55(1), 3–19. [DOI] [PubMed] [Google Scholar]
- Hamil-Luker J, & O'Rand AM (2007). Gender differences in the link between childhood socioeconomic conditions and heart attack risk in adulthood. Demography, 44(1), 137–158. [DOI] [PubMed] [Google Scholar]
- Harris KM, Halpern CT, Whitsel EA, Hussey JM, Killeya-Jones LA, Tabor J, & Dean SC (2019). Cohort profile: The national longitudinal study of adolescent to adult health (add health). International Journal of Epidemiology, 48(5), 1415–1415k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitchman SC, & Fong GT (2011). Gender empowerment and female-to-male smoking prevalence ratios. Bulletin of the World Health Organization, 89, 195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan P (2019). Structural sexism and health in the United States: A new perspective on health inequality and the gender system. American Sociological Review, 84(3), 486–516. [Google Scholar]
- Hyde JS (2005). The gender similarities hypothesis. American Psychologist, 60(6), 581. [DOI] [PubMed] [Google Scholar]
- Korp P (2008). The symbolic power of 'healthy lifestyles'. Health Sociology Review, 17(1), 18–26. [Google Scholar]
- Krueger PM, Bhaloo T, & Rosenau PV (2009). Health lifestyles in the United States and Canada: Are we really so different? Social Science Quarterly, 90(5), 1380–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Collins LM, Lemmon DR, & Schafer JL (2007). PROC LCA: A SAS procedure for latent class analysis. Structural Equation Modeling, 14(4), 671–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence EM, Mollbom S, & Hummer RA (2017). Health lifestyles across the transition to adulthood: Implications for health. Social Science & Medicine, 193, 23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maccoby EE, & Jacklin CN (1974). The psychology of sex differences. Stanford, CA: Stanford University Press. [Google Scholar]
- Mahalik JR, Burns SM, & Syzdek M (2007). Masculinity and perceived normative health behaviors as predictors of men's health behaviors. Social Science & Medicine, 64(11), 2201–2209. [DOI] [PubMed] [Google Scholar]
- Mize TD (2017). Profiles in health: Multiple roles and health lifestyles in early adulthood. Social Science & Medicine, 178, 196–205. [DOI] [PubMed] [Google Scholar]
- Moen P, & Chermack K (2005). Gender disparities in health: Strategic selection, careers, and cycles of control. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 60(Special_Issue_2), S99–S108. [DOI] [PubMed] [Google Scholar]
- Mollborn S, & Lawrence E (2018). Family, peer, and school influences on children’s developing health lifestyles. Journal of Health and Social Behavior, 59(1), 133–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson JS, Hummer RA, & Harris KM (2017). Gender and health behavior clustering among U.S. young adults. Biodemography and Social Biology, 63(1), 3–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pampel FC (2001). Cigarette diffusion and sex differences in smoking. Journal of Health and Social Behavior, 388–404. [PubMed] [Google Scholar]
- Ridgeway CL, & Correll SJ (2004). Unpacking the gender system: A theoretical perspective on gender beliefs and social relations. Gender & Society, 18(4), 510–531. [Google Scholar]
- Rindfuss RR (1991). The young adult years: Diversity, structural change, and fertility. Demography, 28(4), 493–512. [PubMed] [Google Scholar]
- Risman BJ (2004). Gender as a social structure: Theory wrestling with activism. Gender & Society, 18(4), 429–450. [Google Scholar]
- Rosenfield S, & Mouzon D (2013). Gender and mental health In Handbook of the sociology of mental health (pp. 277–296): Springer. [Google Scholar]
- Schilt K, & Westbrook L (2009). Doing gender, doing heteronormativity: "Gender normals," transgender people, and the social maintenance of heterosexuality. Gender & Society, 23(4), 440–464. [Google Scholar]
- Springer KW, Hankivsky O, & Bates LM (2012). Gender and health: relational, intersectional, and biosocial approaches. Social Science & Medicine, 74(11), 1661. [DOI] [PubMed] [Google Scholar]
- Springer KW, & Mouzon DM (2011). “Macho men” and preventive health care: Implications for older men in different social classes. Journal of Health and Social Behavior, 52(2), 212–227. [DOI] [PubMed] [Google Scholar]
- Sodergren M, Wang WC, Salmon J, Ball K, Crawford D, & McNaughton SA (2014). Predicting healthy lifestyle patterns among retirement age older adults in the WELL study: A latent class analysis of sex differences. Maturitas, 77(1), 41–46. [DOI] [PubMed] [Google Scholar]
- Umberson D (1992). Gender, marital status and the social control of health behavior. Social Science & Medicine, 34(8), 907–917. [DOI] [PubMed] [Google Scholar]
- Umberson D, Crosnoe R, & Reczek C (2010). Social relationships and health behavior across the life course. Annual Review of Sociology, 36, 139–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Horne BS, Wiemann CM, Berenson AB, Horwitz IB, & Volk RJ (2009). Multilevel predictors of inconsistent condom use among adolescent mothers. American Journal of Public Health, 99(S2), S417–S424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, & Currie C (2012). Adolescence and the social determinants of health. Lancet, 379(9826), 1641–1652. [DOI] [PubMed] [Google Scholar]
- Weber AM, Cislaghi B, Meausoone V, Abdalla S, Mejia-Guevara I, Loftus P, Gupta GR (2019). Gender norms and health: Insights from global survey data. Lancet, 393(10189), 2455–2468. [DOI] [PubMed] [Google Scholar]
- West C, & Zimmerman DH (1987). Doing gender. Gender & Society, 1(2), 125–151. [Google Scholar]
- White IR, Royston P, & Wood AM (2011). Multiple imputation using chained equations: issues and guidance for practice. Statistics in Medicine, 30(4), 377–399. [DOI] [PubMed] [Google Scholar]